Joint Hospital Grand Round Topic Intraductal papillary mucinous
- Slides: 23
Joint Hospital Grand Round Topic: Intraductal papillary mucinous neoplasm (IPMN) of Pancreas Dr. Chui Lap Bun Prince of Wales Hospital 16 th January, 2010
Introduction More pancreatic cystic lesions are being detected. ¢ Evolution from small benign cystic neoplasms may be very slow and some had high malignant potential and therefore allow selective treatment according to morphological characteristics. ¢
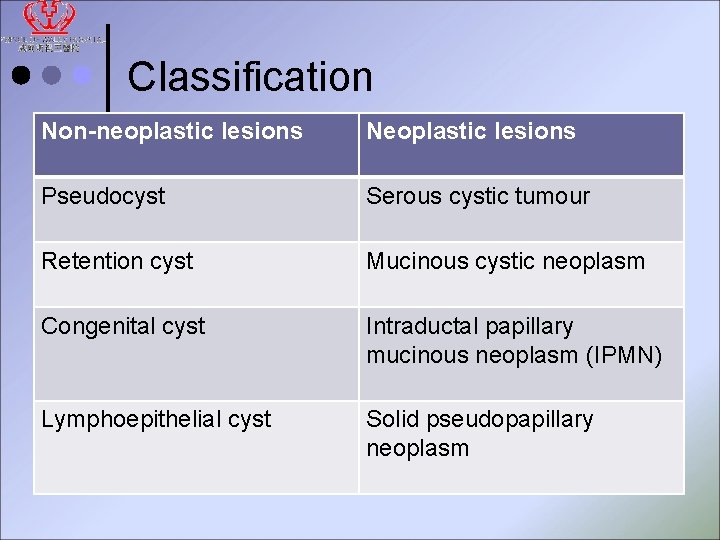
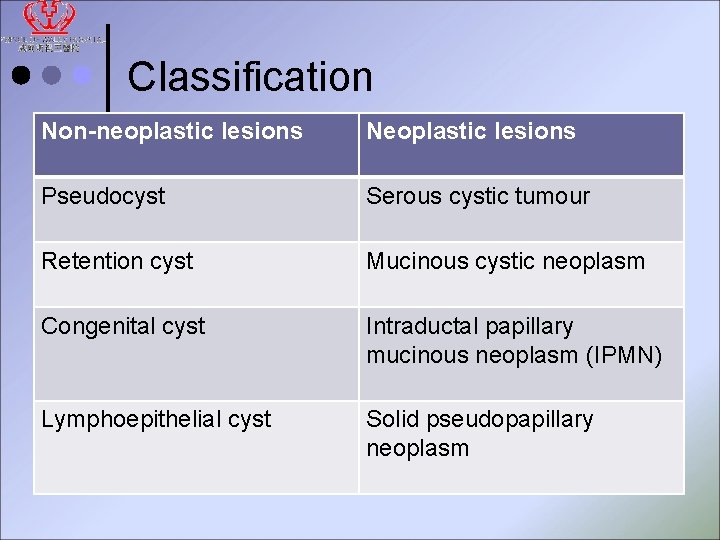
Classification Non-neoplastic lesions Neoplastic lesions Pseudocyst Serous cystic tumour Retention cyst Mucinous cystic neoplasm Congenital cyst Intraductal papillary mucinous neoplasm (IPMN) Lymphoepithelial cyst Solid pseudopapillary neoplasm
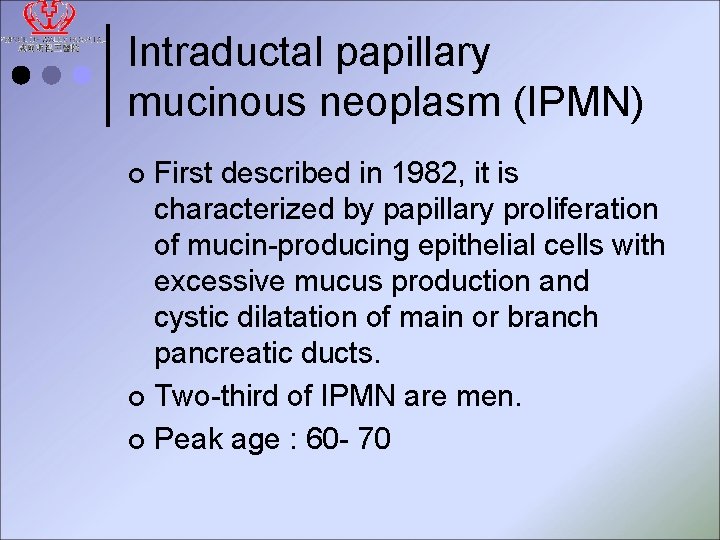
Intraductal papillary mucinous neoplasm (IPMN) First described in 1982, it is characterized by papillary proliferation of mucin-producing epithelial cells with excessive mucus production and cystic dilatation of main or branch pancreatic ducts. ¢ Two-third of IPMN are men. ¢ Peak age : 60 - 70 ¢
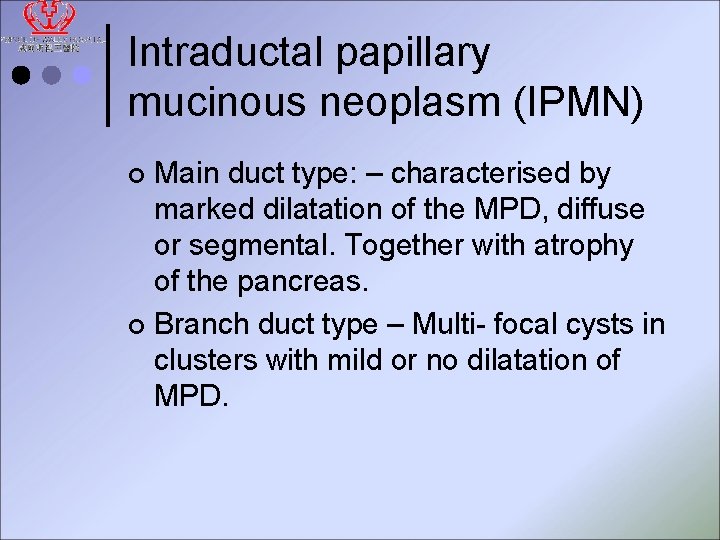
Intraductal papillary mucinous neoplasm (IPMN) Main duct type: – characterised by marked dilatation of the MPD, diffuse or segmental. Together with atrophy of the pancreas. ¢ Branch duct type – Multi- focal cysts in clusters with mild or no dilatation of MPD. ¢
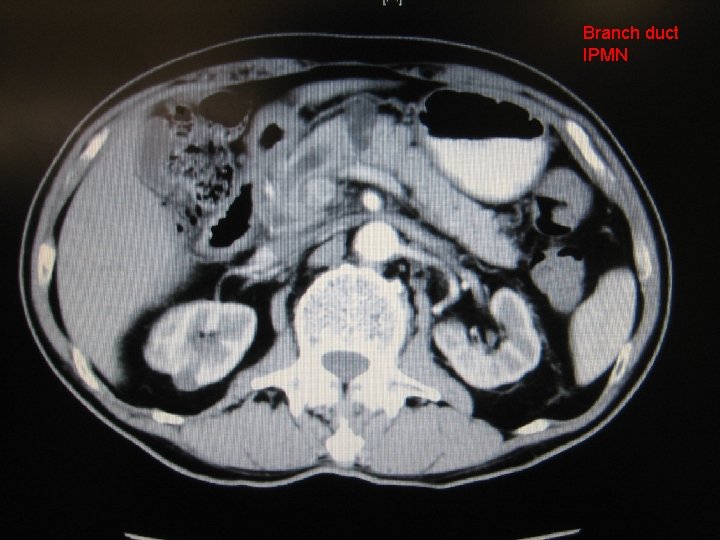
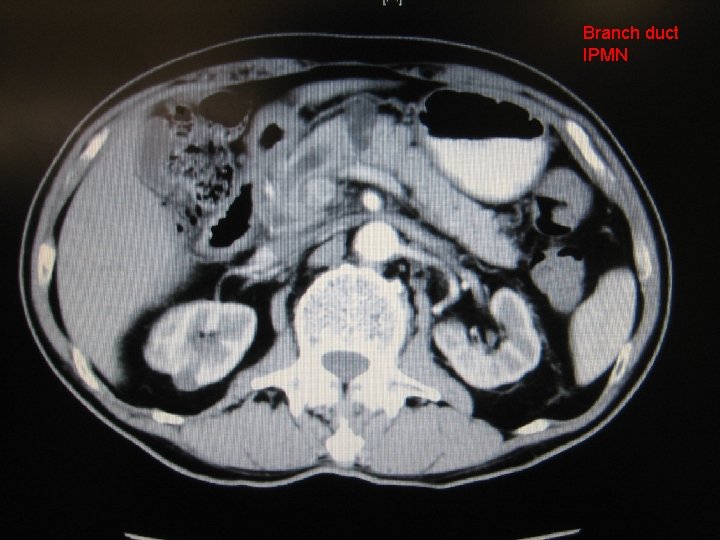
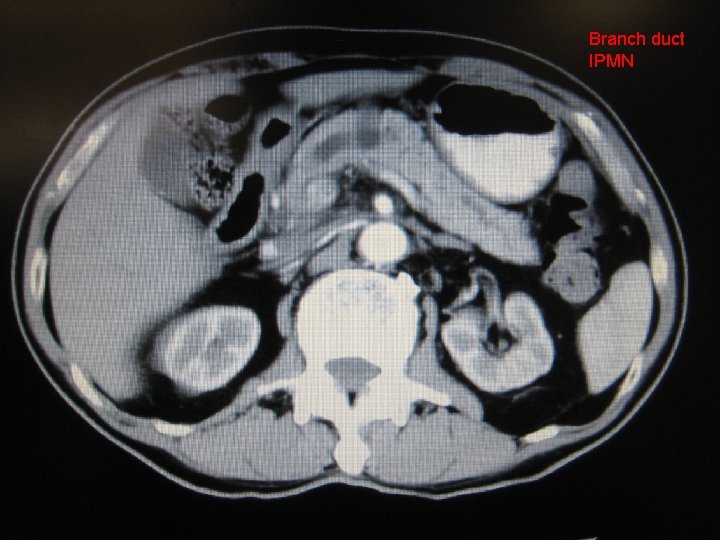
CT Branch duct IPMN
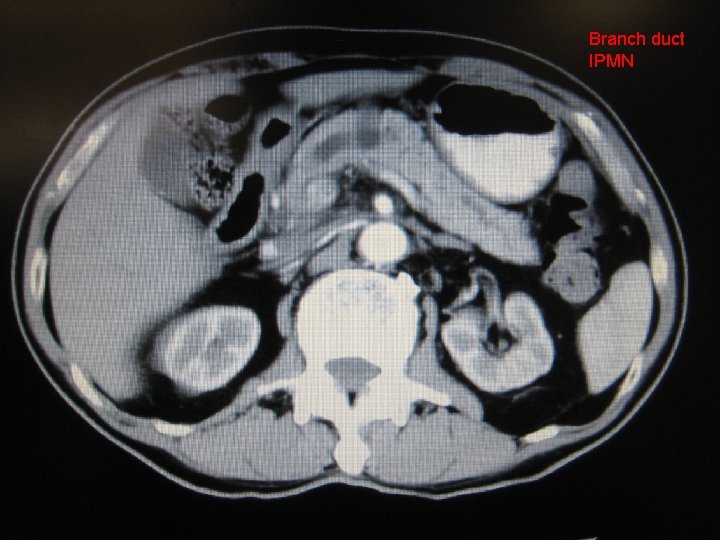
Branch duct IPMN
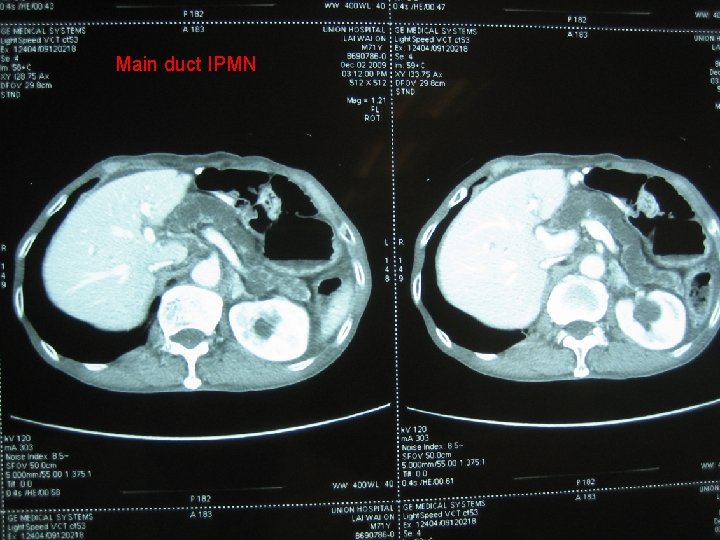
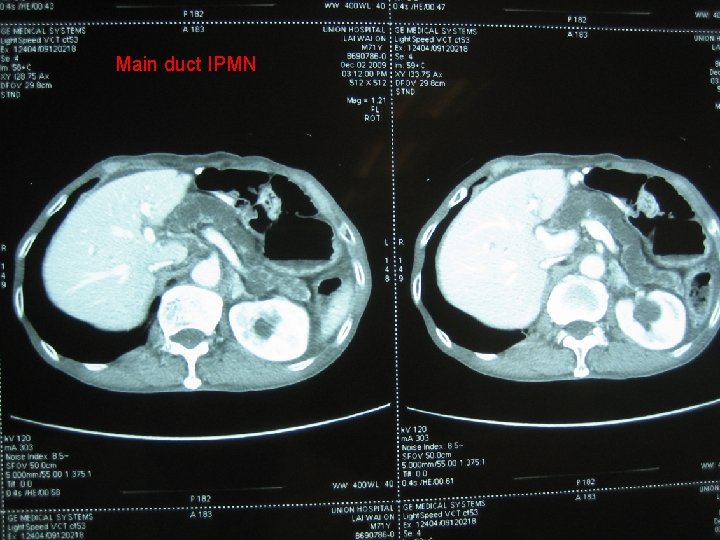
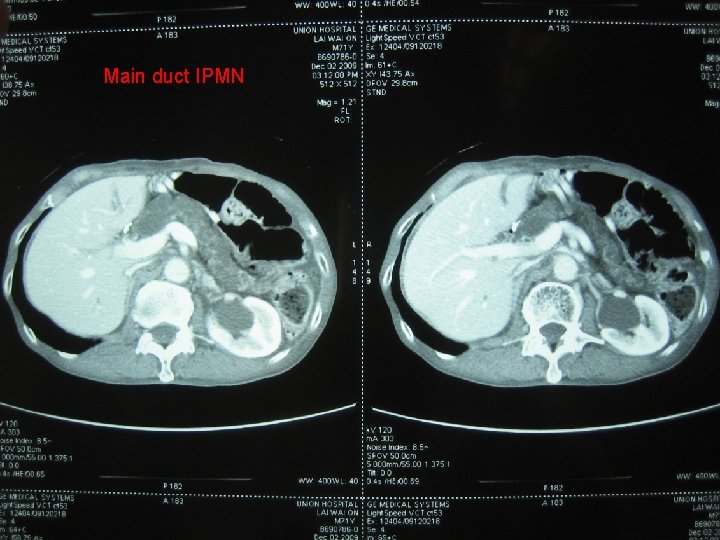
Main duct IPMN
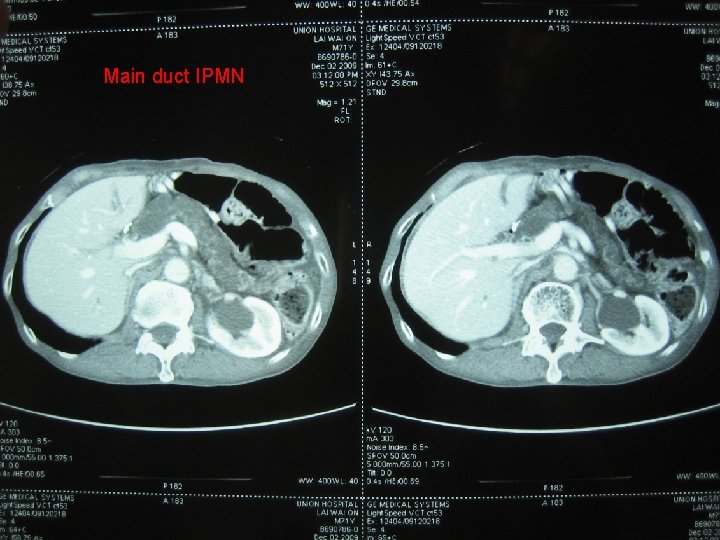
Main duct IPMN
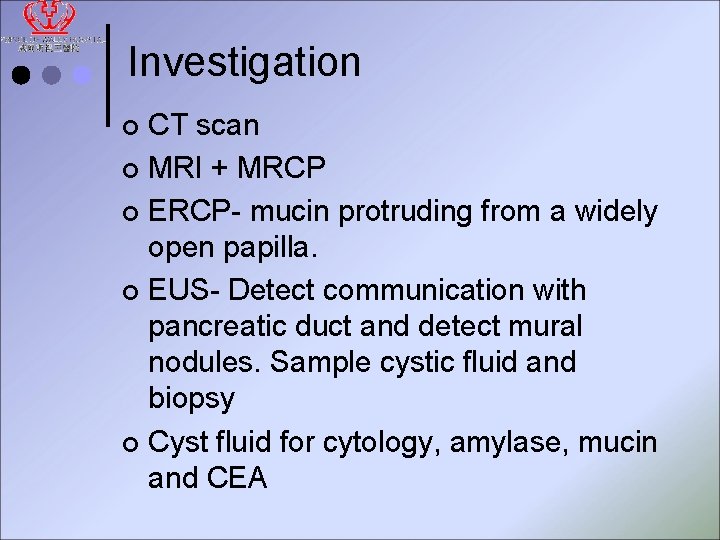
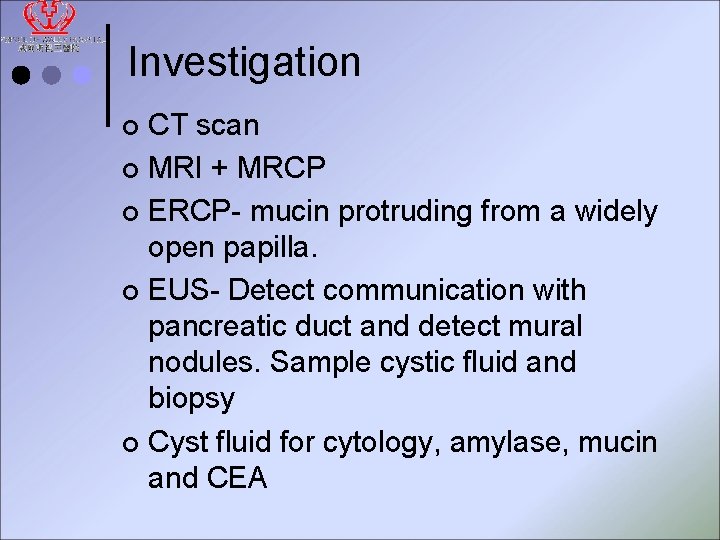
Investigation CT scan ¢ MRI + MRCP ¢ ERCP- mucin protruding from a widely open papilla. ¢ EUS- Detect communication with pancreatic duct and detect mural nodules. Sample cystic fluid and biopsy ¢ Cyst fluid for cytology, amylase, mucin and CEA ¢
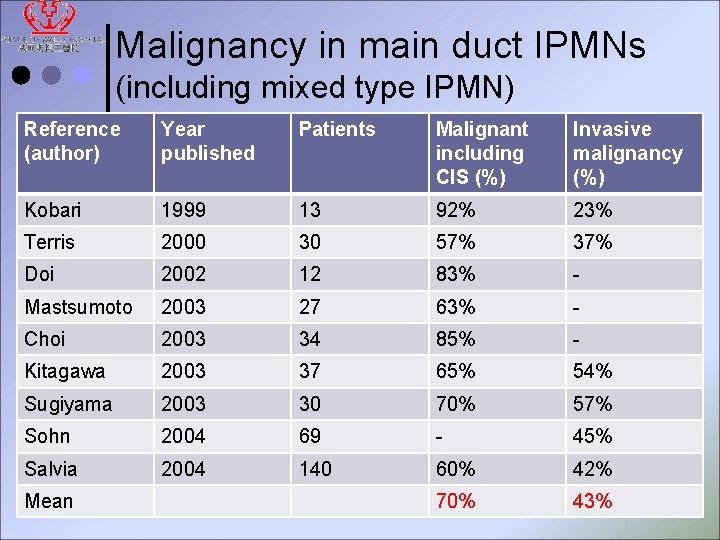
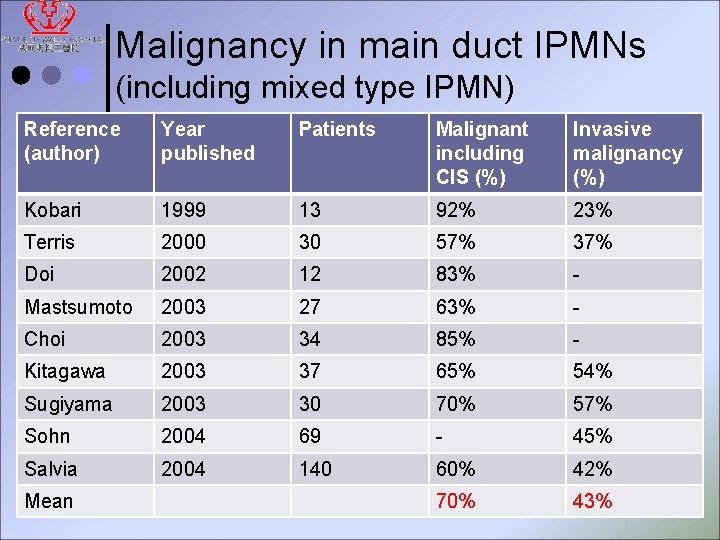
Malignancy in main duct IPMNs (including mixed type IPMN) Reference (author) Year published Patients Malignant including CIS (%) Invasive malignancy (%) Kobari 1999 13 92% 23% Terris 2000 30 57% 37% Doi 2002 12 83% - Mastsumoto 2003 27 63% - Choi 2003 34 85% - Kitagawa 2003 37 65% 54% Sugiyama 2003 30 70% 57% Sohn 2004 69 - 45% Salvia 2004 140 60% 42% 70% 43% Mean
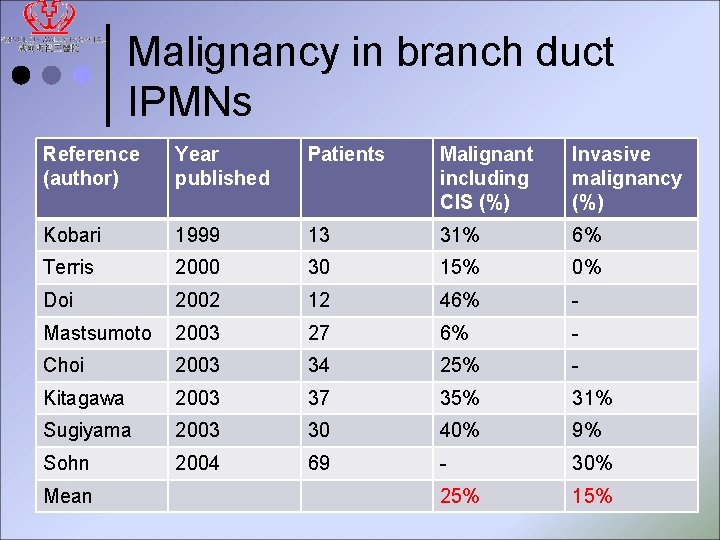
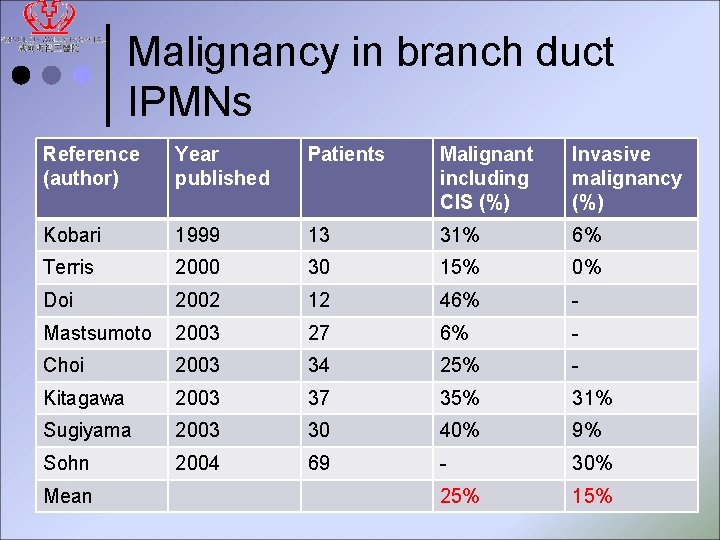
Malignancy in branch duct IPMNs Reference (author) Year published Patients Malignant including CIS (%) Invasive malignancy (%) Kobari 1999 13 31% 6% Terris 2000 30 15% 0% Doi 2002 12 46% - Mastsumoto 2003 27 6% - Choi 2003 34 25% - Kitagawa 2003 37 35% 31% Sugiyama 2003 30 40% 9% Sohn 2004 69 - 30% 25% 15% Mean
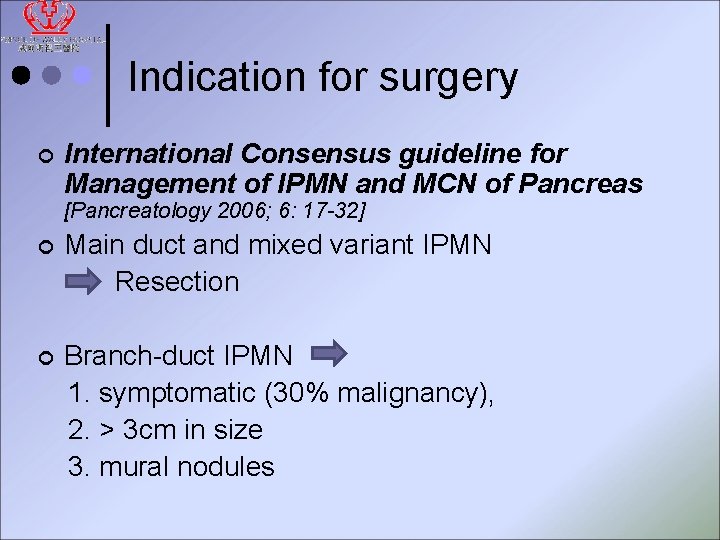
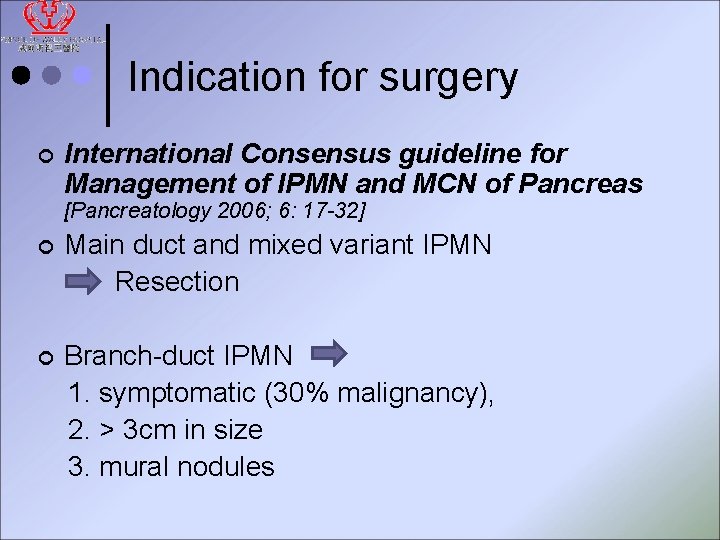
Indication for surgery ¢ International Consensus guideline for Management of IPMN and MCN of Pancreas [Pancreatology 2006; 6: 17 -32] ¢ Main duct and mixed variant IPMN Resection ¢ Branch-duct IPMN 1. symptomatic (30% malignancy), 2. > 3 cm in size 3. mural nodules
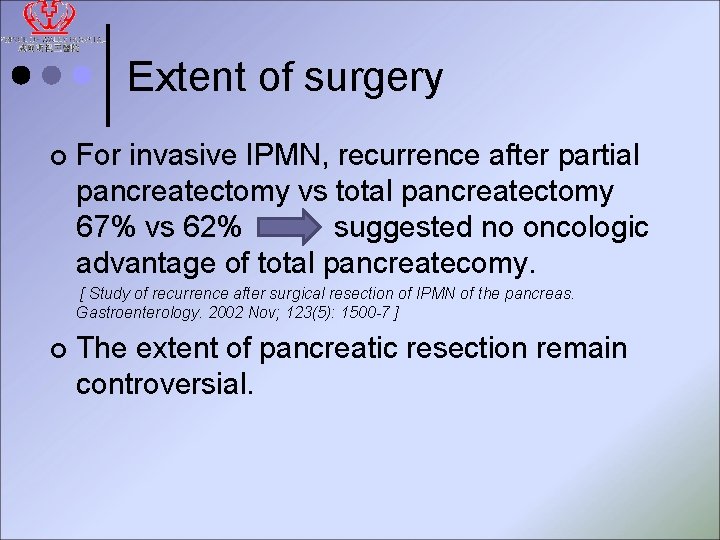
Extent of surgery ¢ For invasive IPMN, recurrence after partial pancreatectomy vs total pancreatectomy 67% vs 62% suggested no oncologic advantage of total pancreatecomy. [ Study of recurrence after surgical resection of IPMN of the pancreas. Gastroenterology. 2002 Nov; 123(5): 1500 -7 ] ¢ The extent of pancreatic resection remain controversial.
Extent of surgery Risk of recurrence Vs. the morbidity of total pancreatectomy. ¢ Routine total pancreatectomy for IPMN is not recommended. ¢ Total pancreatectomy should only be reserved for patients with resectable but extensive IPMN which involves the whole pancreas. ¢
Frozen section Microscopic extension of neoplastic cells beyond visible boundaries of the main lesion is common. ¢ IPMNs can be multifocal and the margin frequently involved at the time of resection ¢ Positive Margin (LD, MD, HD, invasive) Resect more? ? ¢
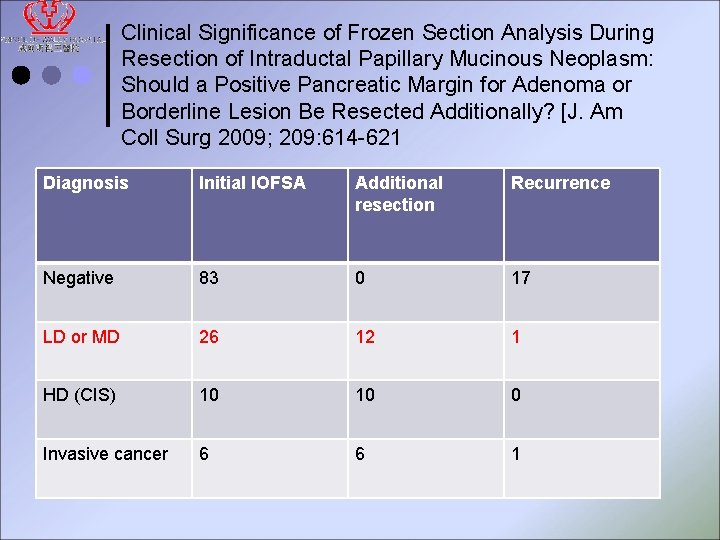
Frozen section ¢ Clinical Significance of Frozen Section Analysis During Resection of Intraductal Papillary Mucinous Neoplasm: Should a Positive Pancreatic Margin for Adenoma or Borderline Lesion Be Resected Additionally? [J. Am Coll Surg 2009; 209: 614 -621 IPMN with CIS or invasive carcinoma: complete resection if possible. ¢ IPM adenoma or borderline lesion: might not need further resection ¢
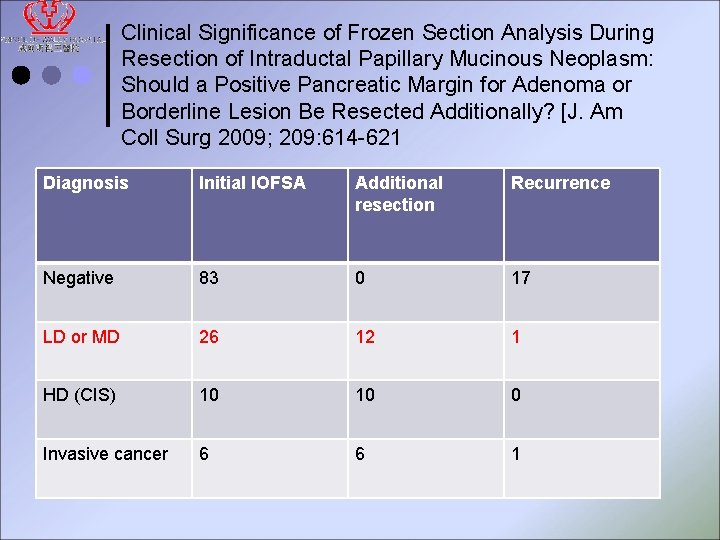
Clinical Significance of Frozen Section Analysis During Resection of Intraductal Papillary Mucinous Neoplasm: Should a Positive Pancreatic Margin for Adenoma or Borderline Lesion Be Resected Additionally? [J. Am Coll Surg 2009; 209: 614 -621 Diagnosis Initial IOFSA Additional resection Recurrence Negative 83 0 17 LD or MD 26 12 1 HD (CIS) 10 10 0 Invasive cancer 6 6 1
Follow up plan Slow growing ¢ Residual tumour may develop into carcinoma ¢ New IPMN arise from ramnant ¢ Time of recurrence ranged from 8 -62 months ¢ Need regular FU imaging
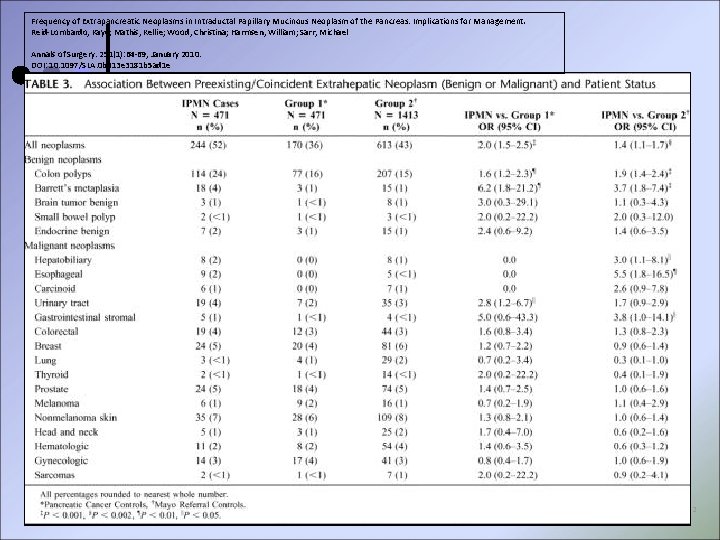
Synchronous and metachronous malignancy ¢ 23. 6 – 32% IPMNs associated with extrapancreatic malignant neoplasm, including gastric, biliary, colorectal and lung malignancy. [ Yamaguchi et, al. Osanai et al. , Augiyama et al. ] ¢ Mayo clinic: IPMN patients with more benign and malignant neoplasms compared with controls– screening colonoscopy should be considered in all patients with IPMN. [Ann Surg 2010; 251: 64 -69]
Conclusion ¢ ¢ IPMN of the pancreas is uncommon but important because it is slow growing with significant malignant potential. Main duct type should be resected. Branch duct type with tumour > 3 cm, mural nodule or positive symptoms warrants surgical resection. High incidence of extrapancreatic malignancies and pancreatic ductal carcinoma.
~Thank you~ Q&A
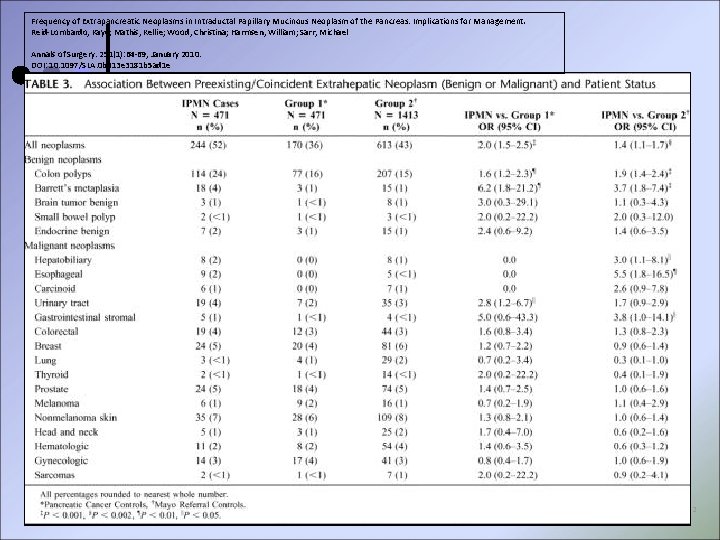
Frequency of Extrapancreatic Neoplasms in Intraductal Papillary Mucinous Neoplasm of the Pancreas: Implications for Management. Reid-Lombardo, Kaye; Mathis, Kellie; Wood, Christina; Harmsen, William; Sarr, Michael Annals of Surgery. 251(1): 64 -69, January 2010. DOI: 10. 1097/SLA. 0 b 013 e 3181 b 5 ad 1 e 2
 Exocrine tumors of pancreas
Exocrine tumors of pancreas Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Esophgeal varices
Esophgeal varices Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Papillary layer function
Papillary layer function Papillary renal cell carcinoma
Papillary renal cell carcinoma Pulmonary valve sheep heart
Pulmonary valve sheep heart Endocrine histology
Endocrine histology Breast papillary carcinoma
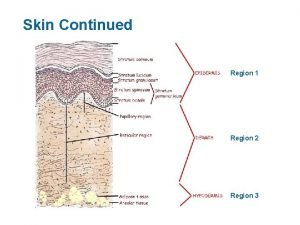
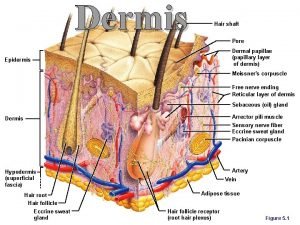
Breast papillary carcinoma Papillary dermis
Papillary dermis Papillary duct
Papillary duct Proximal convoluted tubule
Proximal convoluted tubule Integumentary system histology labeled
Integumentary system histology labeled Anaplastic squamous cell carcinoma
Anaplastic squamous cell carcinoma Superficial papillary layer
Superficial papillary layer Papillary layer
Papillary layer Papillary muscle
Papillary muscle Papillae of skin
Papillae of skin Function of macula densa
Function of macula densa Coronary sulcus
Coronary sulcus