Distinction of Primary Ovarian Mucinous Tumors and Mucinous



- Slides: 29
Distinction of Primary Ovarian Mucinous Tumors and Mucinous Tumors Metastatic to the Ovary A Practical Approach With Guidelines for Prediction of Primary Site for Metastases of Uncertain Origin Russell Vang, MD, and Brigitte M. Ronnett, MD Pathology Case Reviews • Volume 11, Number 1, January/February 2006
CASE PRESENTATION l 33 y/o, female l A right ovarian cyst l No history of cervical diseases l laparoscopic salpingo-oophorectomy l spongy and papillary tissue measuring 12. 5 cm in aggregate
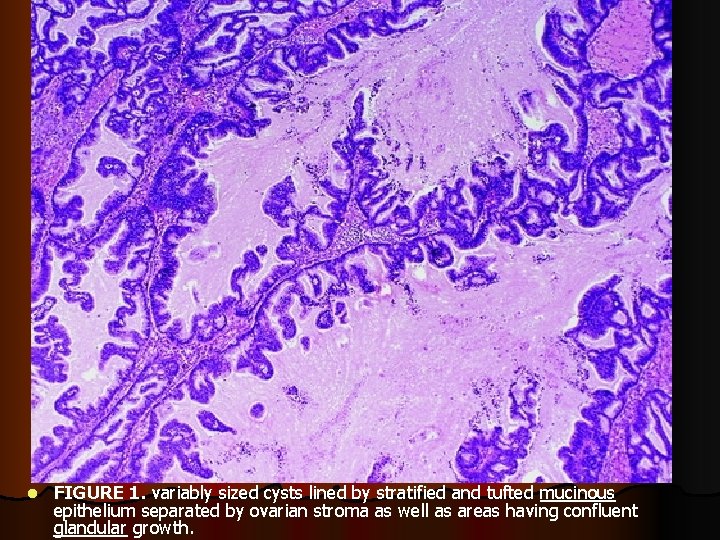
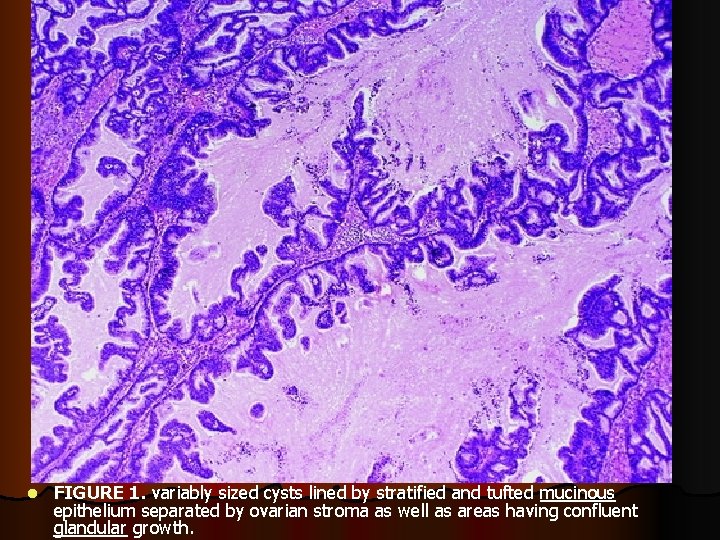
FIGURE 1 l FIGURE 1. variably sized cysts lined by stratified and tufted mucinous epithelium separated by ovarian stroma as well as areas having confluent glandular growth.
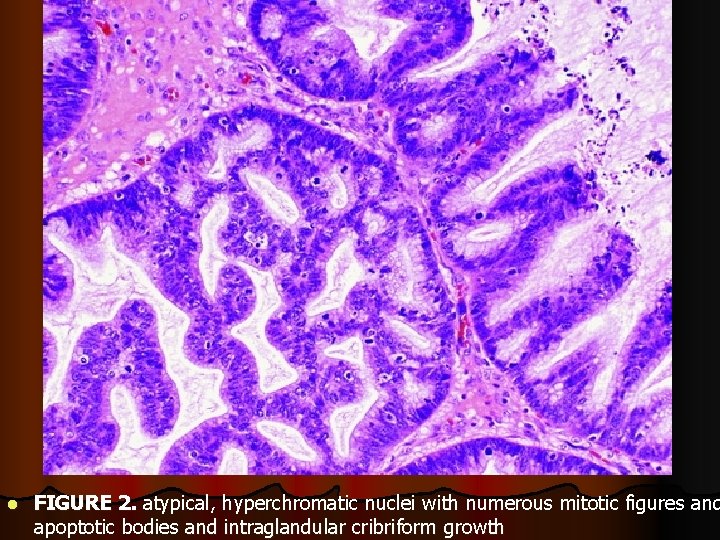
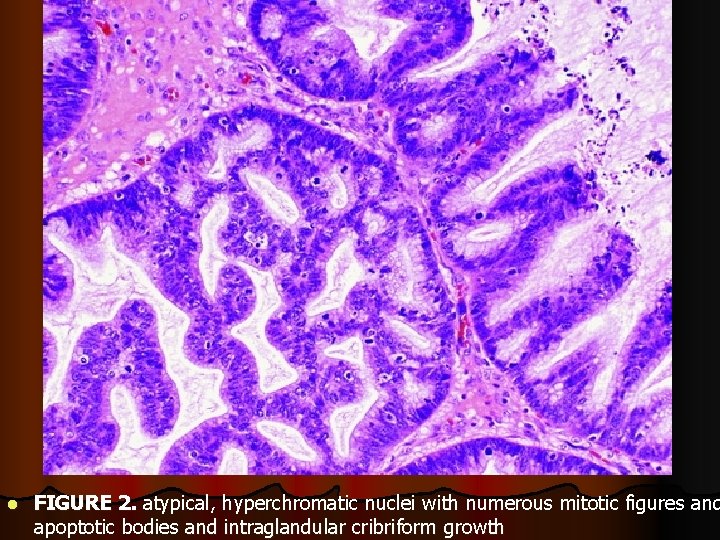
l FIGURE 2. atypical, hyperchromatic nuclei with numerous mitotic figures and apoptotic bodies and intraglandular cribriform growth
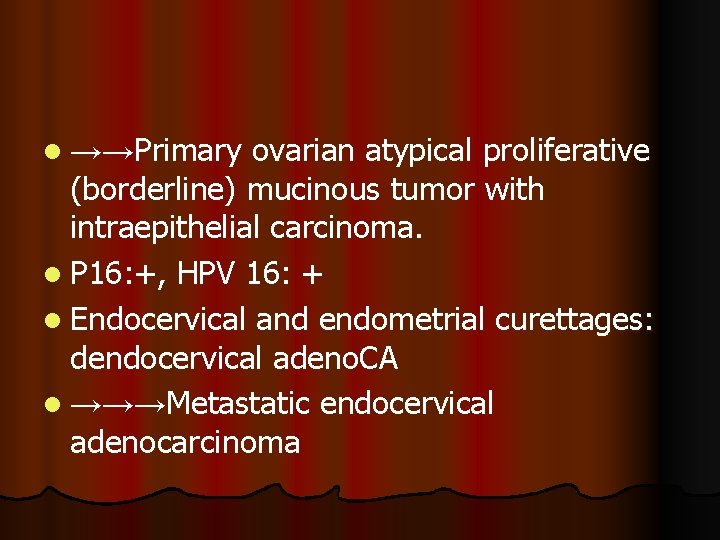
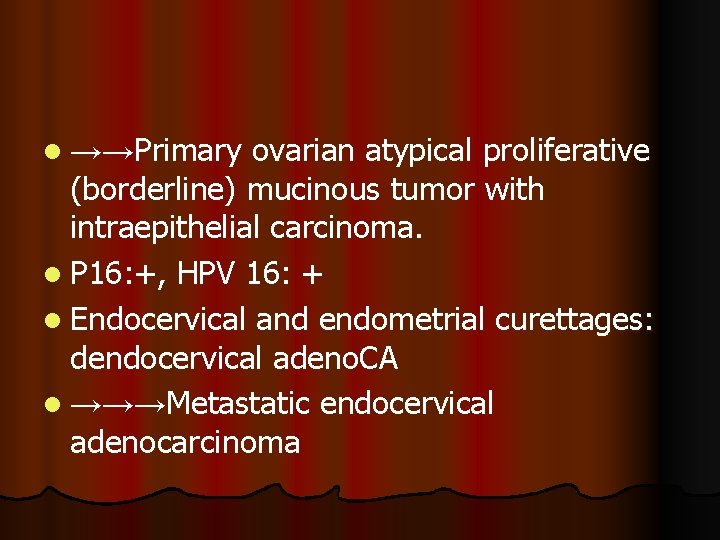
l →→Primary ovarian atypical proliferative (borderline) mucinous tumor with intraepithelial carcinoma. l P 16: +, HPV 16: + l Endocervical and endometrial curettages: dendocervical adeno. CA l →→→Metastatic endocervical adenocarcinoma
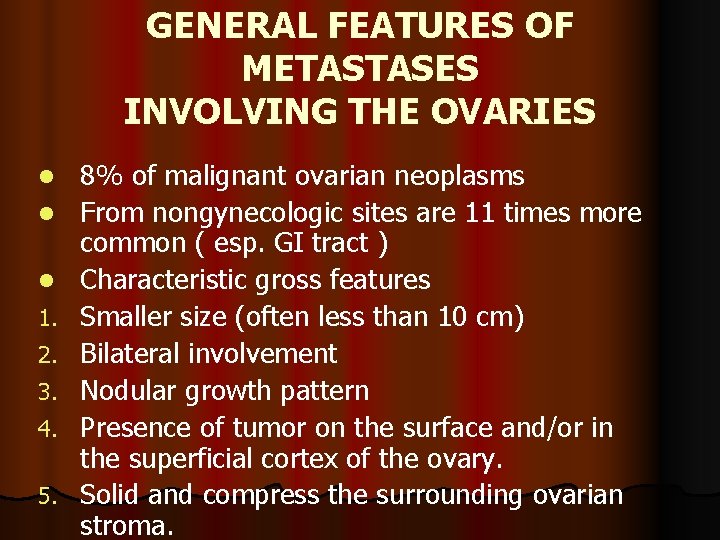
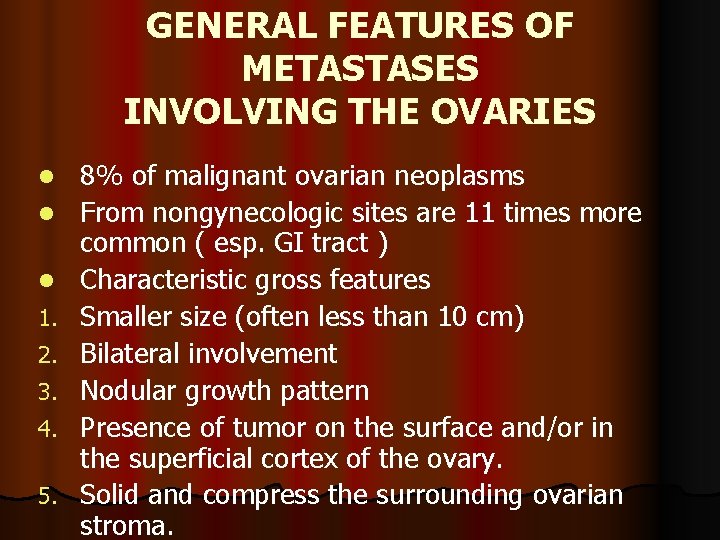
GENERAL FEATURES OF METASTASES INVOLVING THE OVARIES l l l 1. 2. 3. 4. 5. 8% of malignant ovarian neoplasms From nongynecologic sites are 11 times more common ( esp. GI tract ) Characteristic gross features Smaller size (often less than 10 cm) Bilateral involvement Nodular growth pattern Presence of tumor on the surface and/or in the superficial cortex of the ovary. Solid and compress the surrounding ovarian stroma.
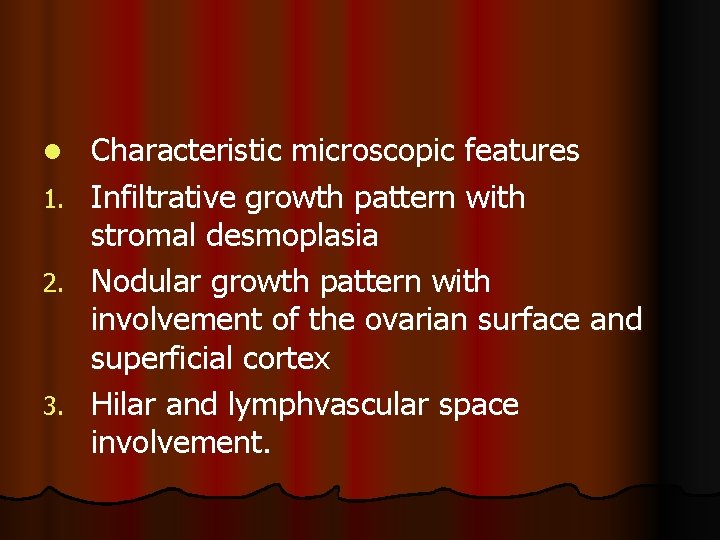
l 1. 2. 3. Characteristic microscopic features Infiltrative growth pattern with stromal desmoplasia Nodular growth pattern with involvement of the ovarian surface and superficial cortex Hilar and lymphvascular space involvement.
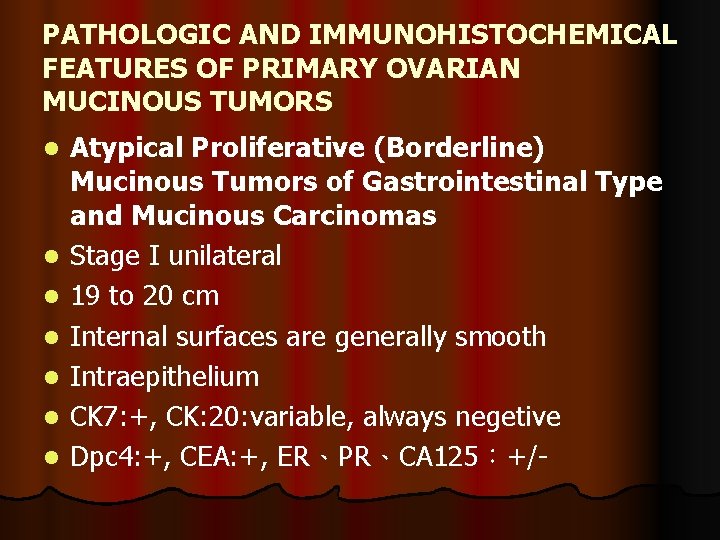
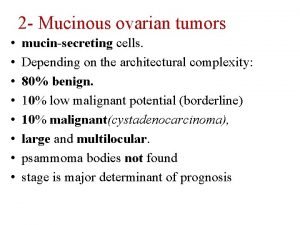
PATHOLOGIC AND IMMUNOHISTOCHEMICAL FEATURES OF PRIMARY OVARIAN MUCINOUS TUMORS l l l l Atypical Proliferative (Borderline) Mucinous Tumors of Gastrointestinal Type and Mucinous Carcinomas Stage I unilateral 19 to 20 cm Internal surfaces are generally smooth Intraepithelium CK 7: +, CK: 20: variable, always negetive Dpc 4: +, CEA: +, ER、PR、CA 125:+/-
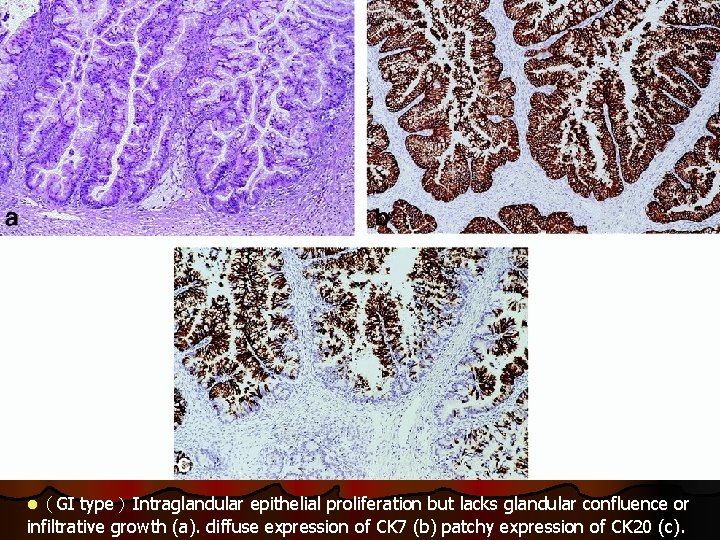
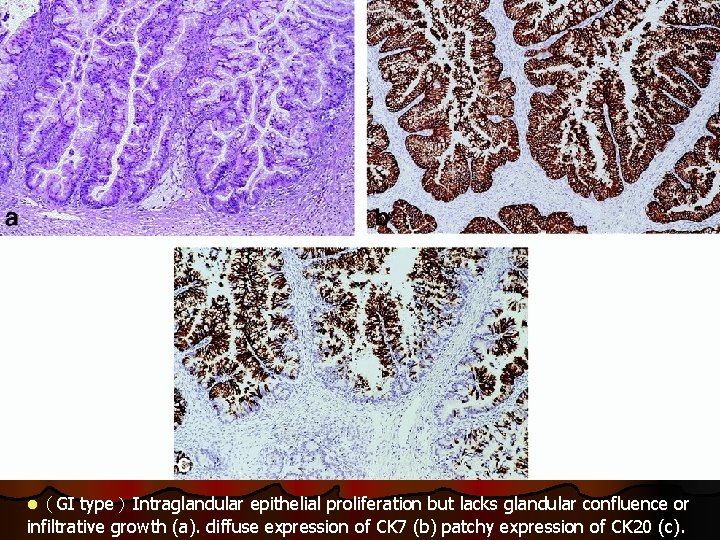
l(GI type)Intraglandular epithelial proliferation but lacks glandular confluence or infiltrative growth (a). diffuse expression of CK 7 (b) patchy expression of CK 20 (c).
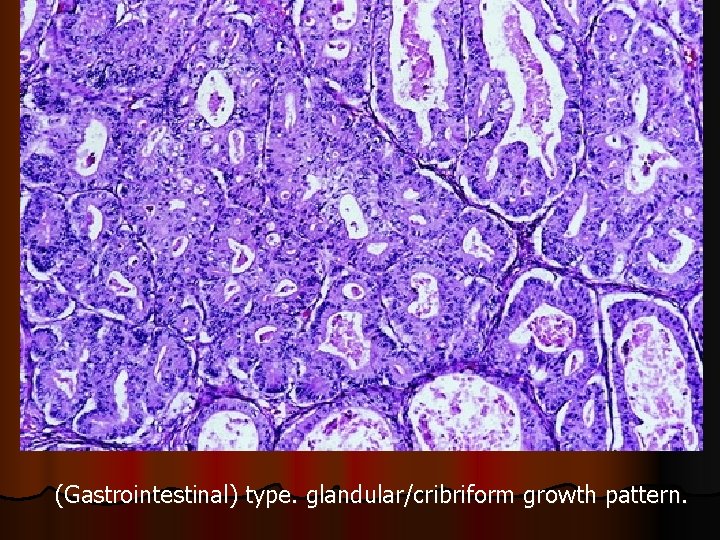
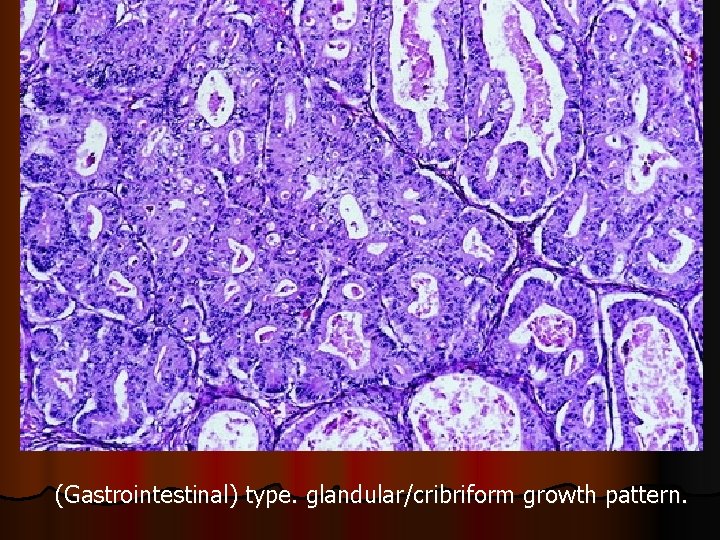
(Gastrointestinal) type. glandular/cribriform growth pattern.
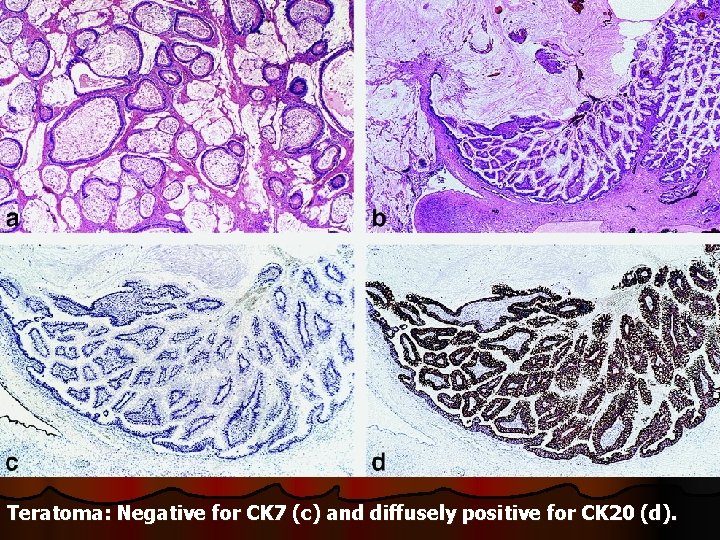
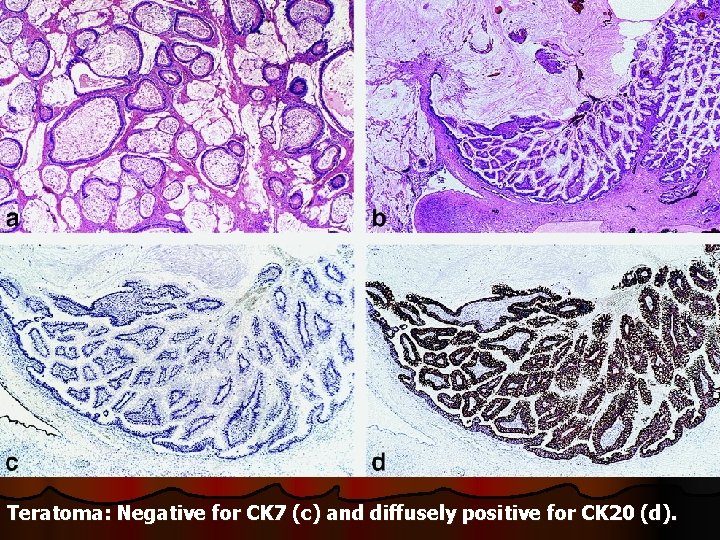
Teratoma: Negative for CK 7 (c) and diffusely positive for CK 20 (d).
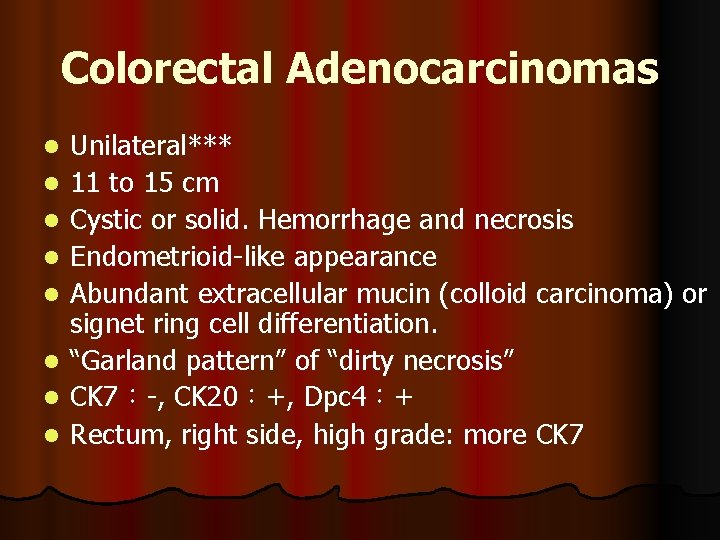
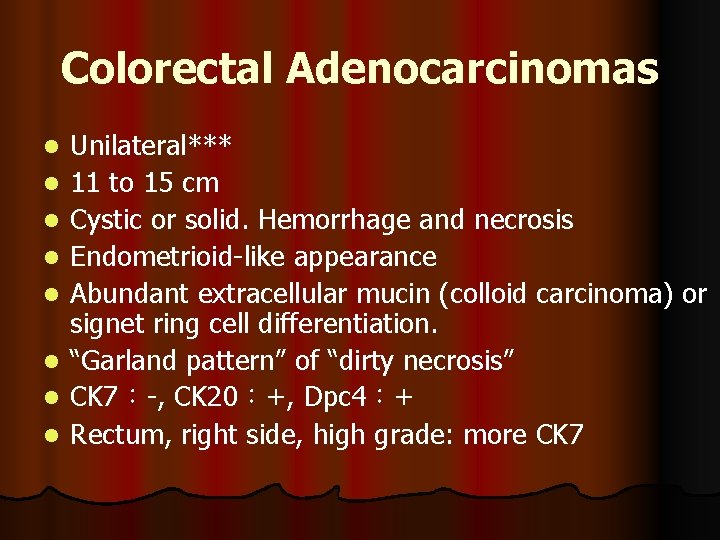
Colorectal Adenocarcinomas l l l l Unilateral*** 11 to 15 cm Cystic or solid. Hemorrhage and necrosis Endometrioid-like appearance Abundant extracellular mucin (colloid carcinoma) or signet ring cell differentiation. “Garland pattern” of “dirty necrosis” CK 7:-, CK 20:+, Dpc 4:+ Rectum, right side, high grade: more CK 7
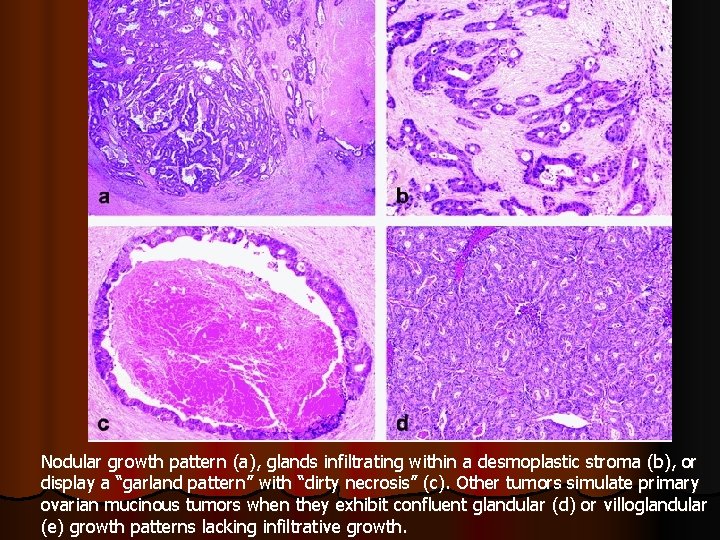
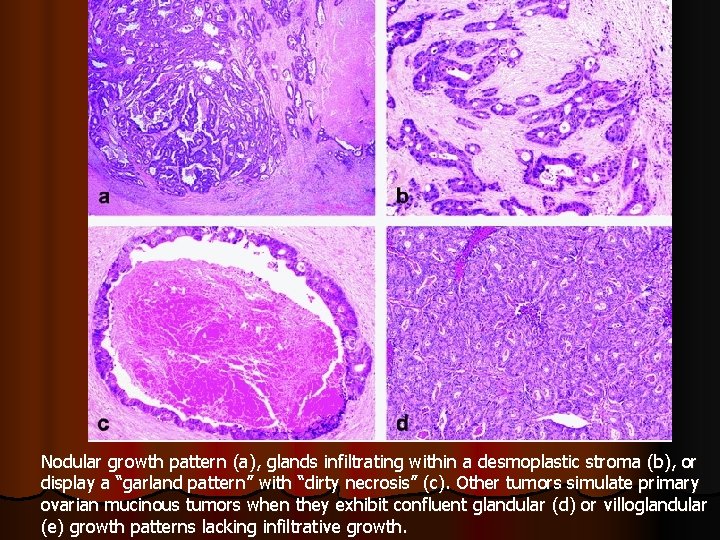
Nodular growth pattern (a), glands infiltrating within a desmoplastic stroma (b), or display a “garland pattern” with “dirty necrosis” (c). Other tumors simulate primary ovarian mucinous tumors when they exhibit confluent glandular (d) or villoglandular (e) growth patterns lacking infiltrative growth.
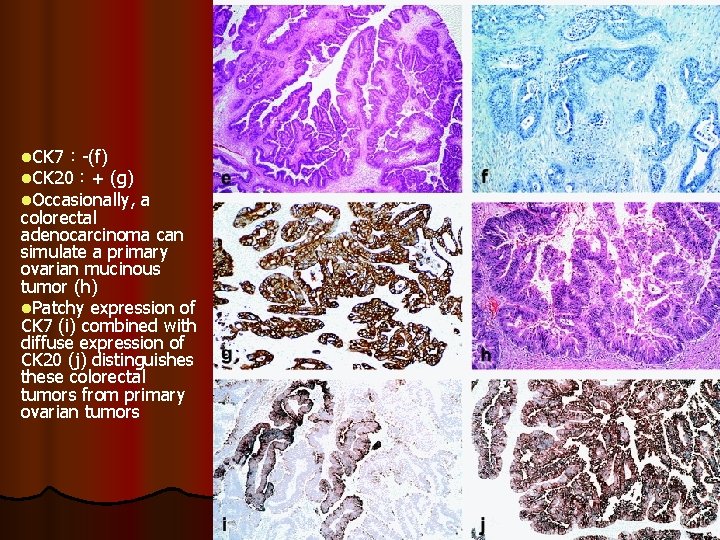
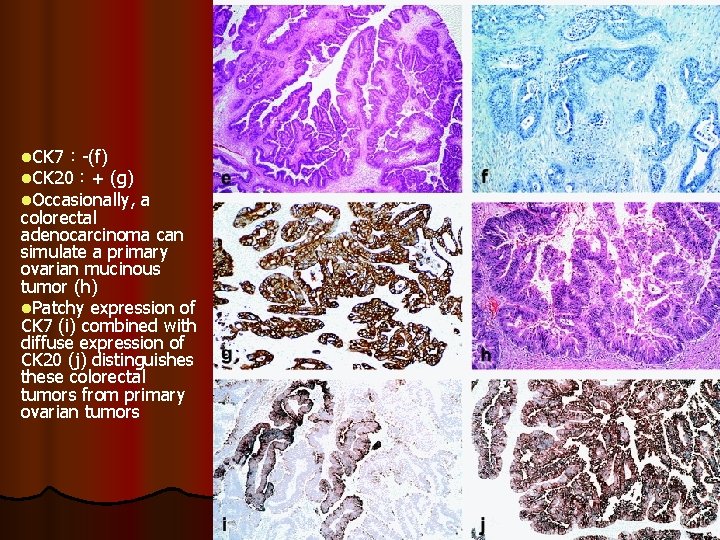
l. CK 7:-(f) l. CK 20:+ (g) l. Occasionally, a colorectal adenocarcinoma can simulate a primary ovarian mucinous tumor (h) l. Patchy expression of CK 7 (i) combined with diffuse expression of CK 20 (j) distinguishes these colorectal tumors from primary ovarian tumors
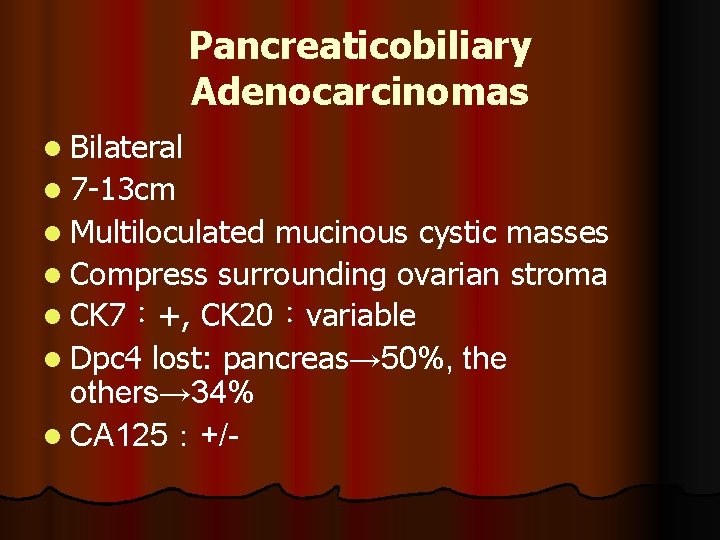
Pancreaticobiliary Adenocarcinomas l Bilateral l 7 -13 cm l Multiloculated mucinous cystic masses l Compress surrounding ovarian stroma l CK 7:+, CK 20:variable l Dpc 4 lost: pancreas→ 50%, the pancreas others→ 34% l CA 125:+/-
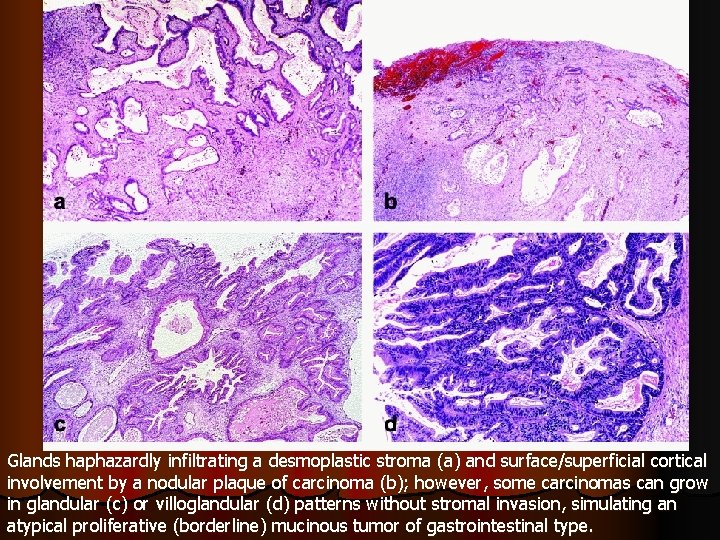
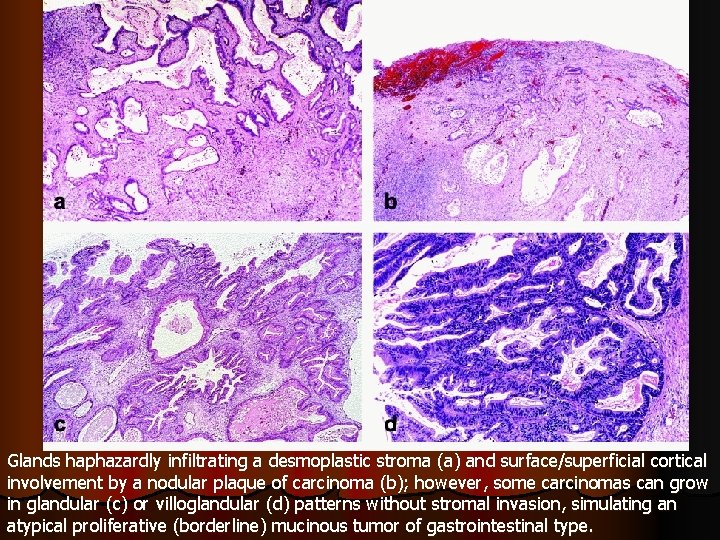
Glands haphazardly infiltrating a desmoplastic stroma (a) and surface/superficial cortical involvement by a nodular plaque of carcinoma (b); however, some carcinomas can grow in glandular (c) or villoglandular (d) patterns without stromal invasion, simulating an atypical proliferative (borderline) mucinous tumor of gastrointestinal type.
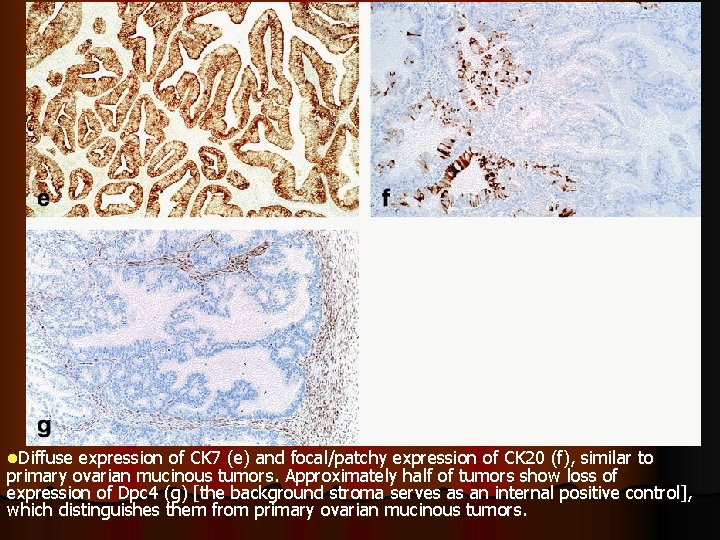
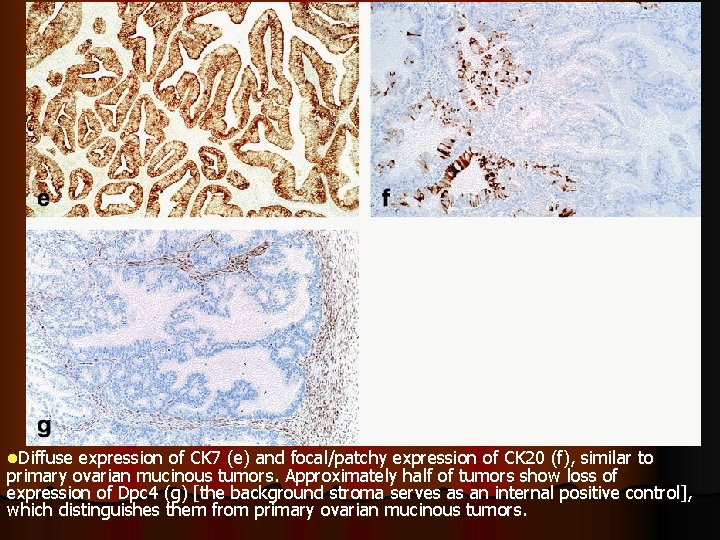
l. Diffuse expression of CK 7 (e) and focal/patchy expression of CK 20 (f), similar to primary ovarian mucinous tumors. Approximately half of tumors show loss of expression of Dpc 4 (g) [the background stroma serves as an internal positive control], which distinguishes them from primary ovarian mucinous tumors.
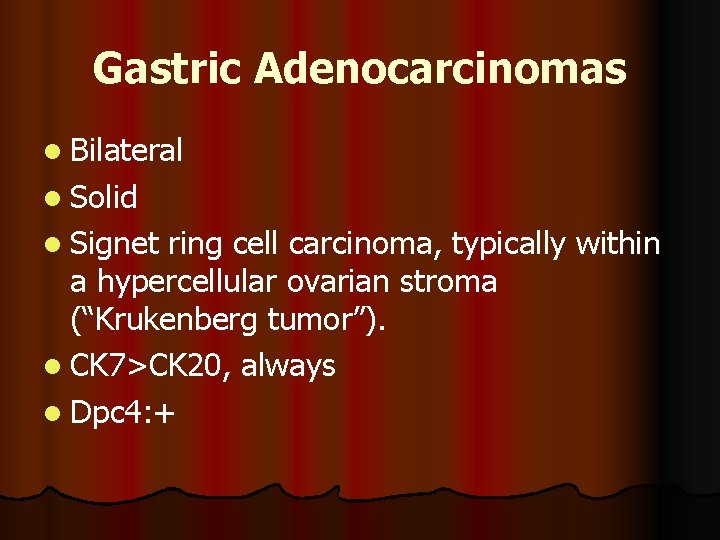
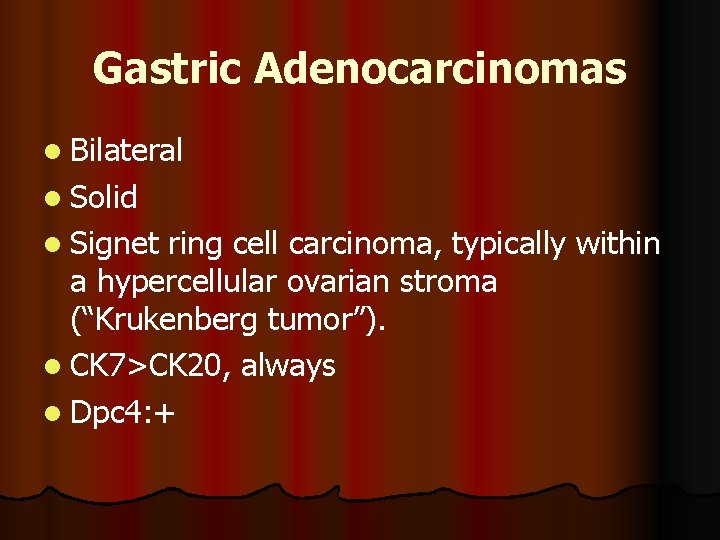
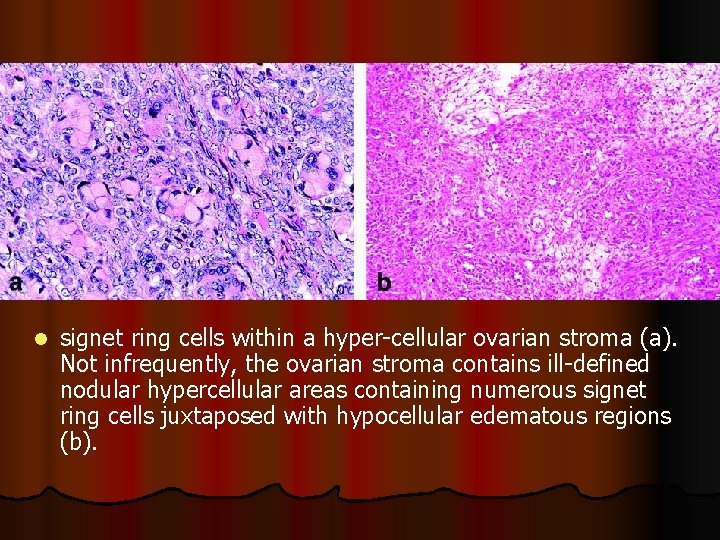
Gastric Adenocarcinomas l Bilateral l Solid l Signet ring cell carcinoma, typically within a hypercellular ovarian stroma (“Krukenberg tumor”). l CK 7>CK 20, always l Dpc 4: +
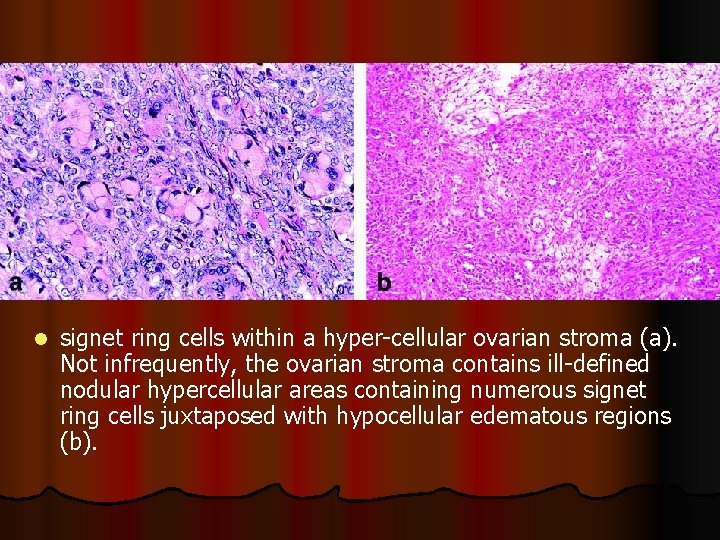
l signet ring cells within a hyper-cellular ovarian stroma (a). Not infrequently, the ovarian stroma contains ill-defined nodular hypercellular areas containing numerous signet ring cells juxtaposed with hypocellular edematous regions (b).
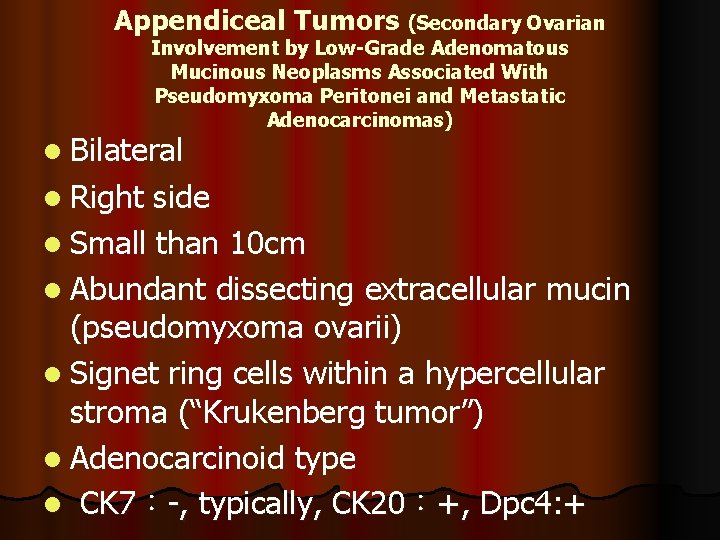
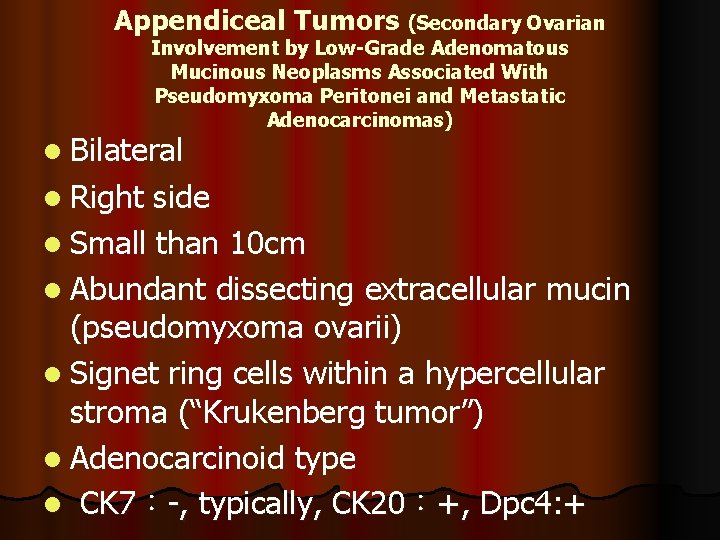
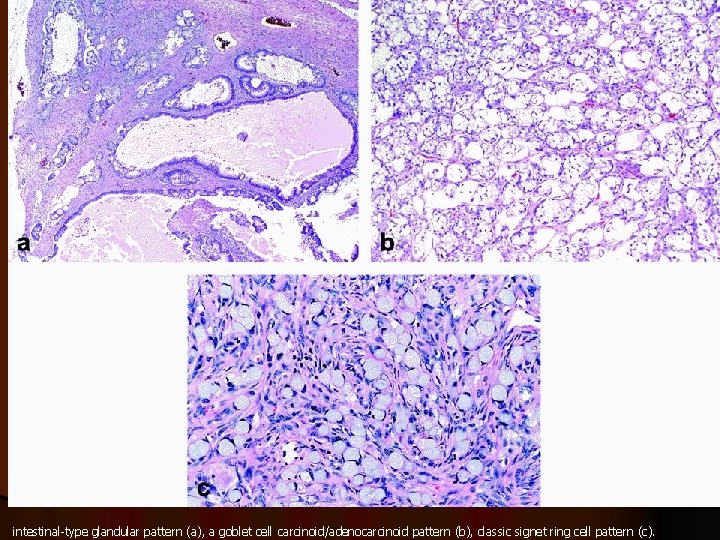
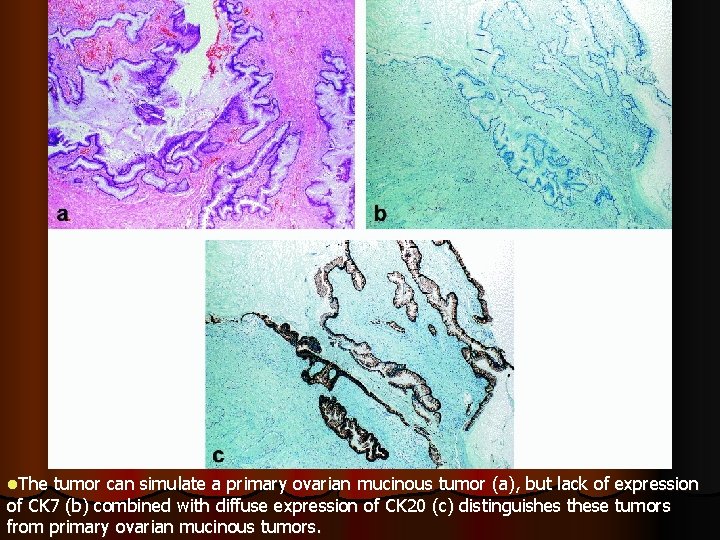
Appendiceal Tumors (Secondary Ovarian Involvement by Low-Grade Adenomatous Mucinous Neoplasms Associated With Pseudomyxoma Peritonei and Metastatic Adenocarcinomas) l Bilateral l Right side l Small than 10 cm l Abundant dissecting extracellular mucin (pseudomyxoma ovarii) l Signet ring cells within a hypercellular stroma (“Krukenberg tumor”) l Adenocarcinoid type l CK 7:-, typically, CK 20:+, Dpc 4: +
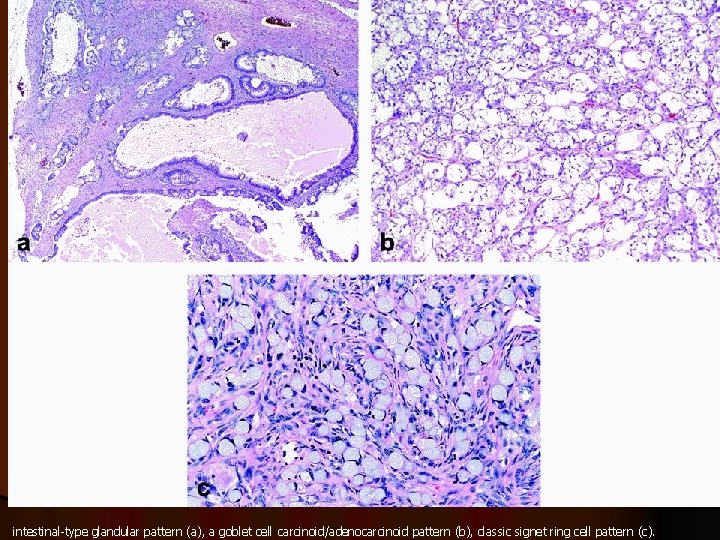
intestinal-type glandular pattern (a), a goblet cell carcinoid/adenocarcinoid pattern (b), classic signet ring cell pattern (c).
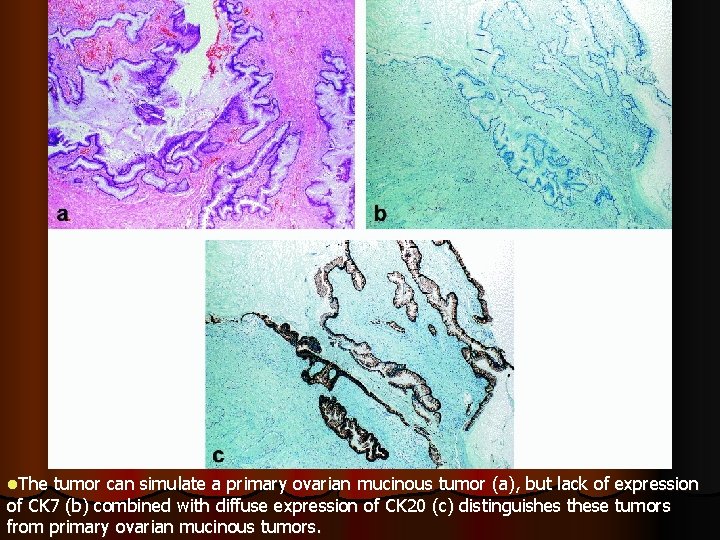
l. The tumor can simulate a primary ovarian mucinous tumor (a), but lack of expression of CK 7 (b) combined with diffuse expression of CK 20 (c) distinguishes these tumors from primary ovarian mucinous tumors.
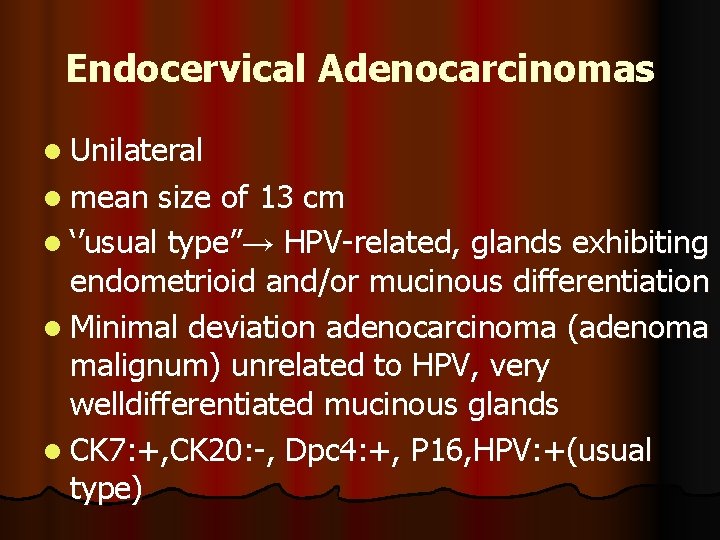
Endocervical Adenocarcinomas l Unilateral l mean size of 13 cm l ‘’usual type”→ type” HPV-related, glands exhibiting endometrioid and/or mucinous differentiation l Minimal deviation adenocarcinoma (adenoma malignum) unrelated to HPV, very welldifferentiated mucinous glands l CK 7: +, CK 20: -, Dpc 4: +, P 16, HPV: +(usual type)
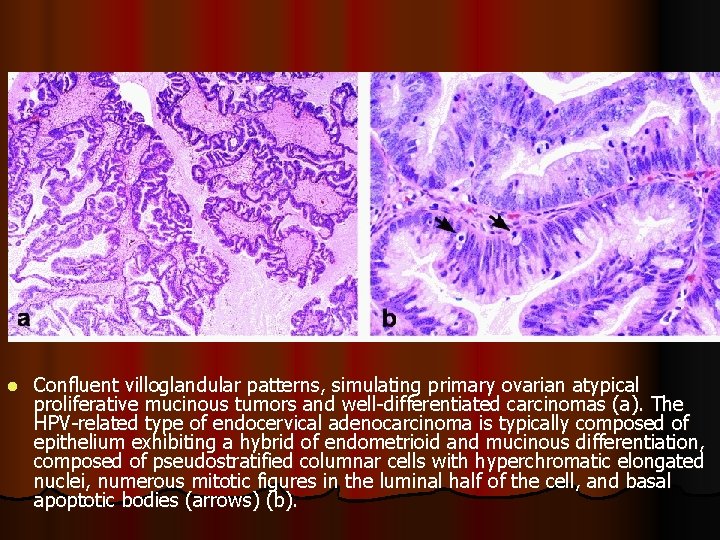
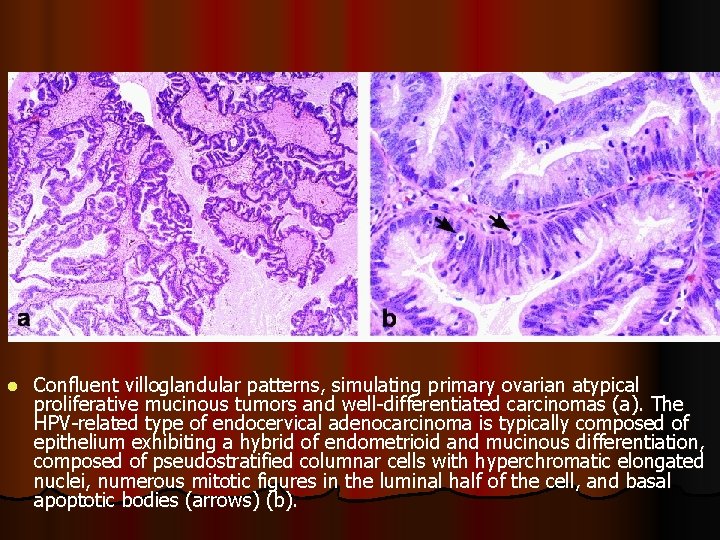
l Confluent villoglandular patterns, simulating primary ovarian atypical proliferative mucinous tumors and well-differentiated carcinomas (a). The HPV-related type of endocervical adenocarcinoma is typically composed of epithelium exhibiting a hybrid of endometrioid and mucinous differentiation, composed of pseudostratified columnar cells with hyperchromatic elongated nuclei, numerous mitotic figures in the luminal half of the cell, and basal apoptotic bodies (arrows) (b).
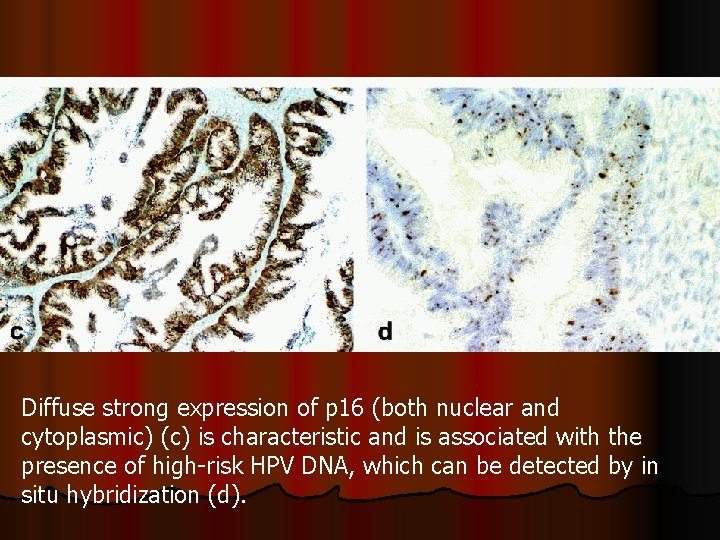
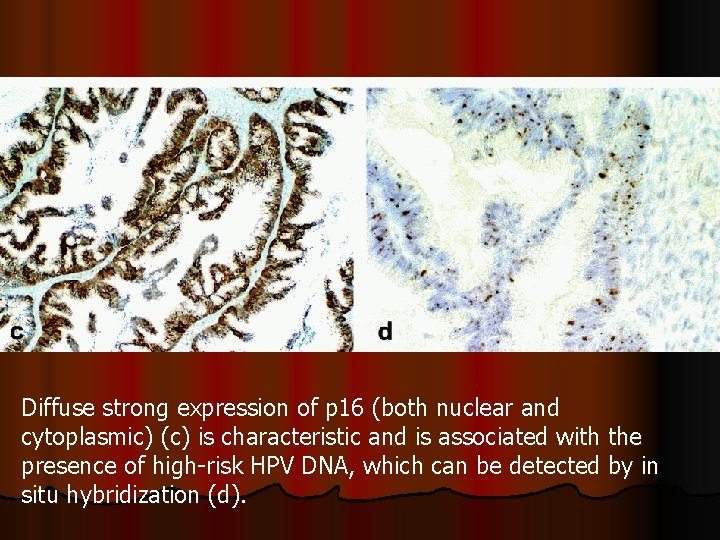
Diffuse strong expression of p 16 (both nuclear and cytoplasmic) (c) is characteristic and is associated with the presence of high-risk HPV DNA, which can be detected by in situ hybridization (d).
GUIDELINES FOR DISTINGUISHING PRIMARY OVARIAN MUCINOUS TUMORS FROM METASTATIC MUCINOUS TUMORS IN THE OVARY AND FOR PREDICTING PRIMARY SITE FOR METASTATIC CARCINOMAS OF UNKNOWN ORIGIN Intraoperative Consultation l Whether the patient has had any other documented tumors l Extraovarian disease, bilateral tumor, gross or microscopic nodularity, garland pattern necrosis, or signet ring cells→ cells gastrointestinal tract l Mucinous ascites (pseudomyxoma peritonei) →evaluate and remove the appendix.



 Exocrine tumors of pancreas
Exocrine tumors of pancreas Malignant and benign tumors
Malignant and benign tumors Benign and malignant tumors
Benign and malignant tumors Teratoma
Teratoma Benign tumors in the uterus
Benign tumors in the uterus Response evaluation criteria in solid tumors (recist)
Response evaluation criteria in solid tumors (recist) Triangle de codman
Triangle de codman How many bones
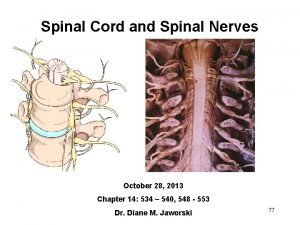
How many bones Spinal cord tumors
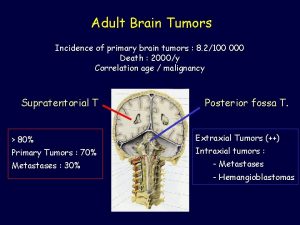
Spinal cord tumors Brain tumors
Brain tumors Chest wall tumors
Chest wall tumors Syringimyelia
Syringimyelia Classification of tumors
Classification of tumors Classification of tumors
Classification of tumors Odontogenic tumors classification
Odontogenic tumors classification Enneking staging
Enneking staging Odontogenic tumors
Odontogenic tumors Ameloblastoma rtg
Ameloblastoma rtg Thyroid grading system
Thyroid grading system The distinction between right and wrong lies at the
The distinction between right and wrong lies at the The proper distinction between law and gospel
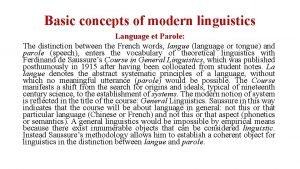
The proper distinction between law and gospel Concept of langue and parole
Concept of langue and parole Difference between counselling and guidance
Difference between counselling and guidance The proper distinction between law and gospel
The proper distinction between law and gospel Pierre bourdieu distinction
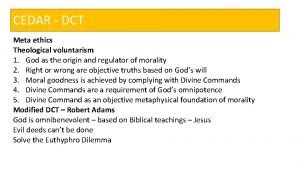
Pierre bourdieu distinction Meta ethics vs normative ethics
Meta ethics vs normative ethics Ovarian functions
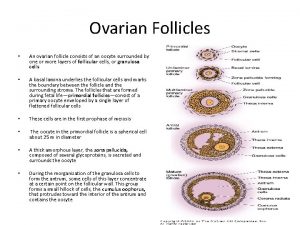
Ovarian functions Figure 16-7 is a sectional view of the ovary
Figure 16-7 is a sectional view of the ovary Ca 125
Ca 125 Ovarian cyst rupture discharge look like
Ovarian cyst rupture discharge look like