Intraductal Papillary Mucinous Neoplasm IPMN of the Pancreas
- Slides: 24
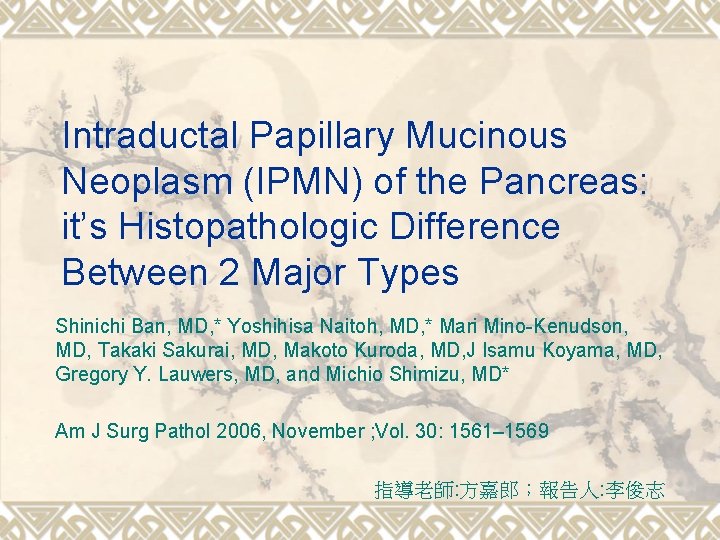
Intraductal Papillary Mucinous Neoplasm (IPMN) of the Pancreas: it’s Histopathologic Difference Between 2 Major Types Shinichi Ban, MD, * Yoshihisa Naitoh, MD, * Mari Mino-Kenudson, MD, Takaki Sakurai, MD, Makoto Kuroda, MD, J Isamu Koyama, MD, Gregory Y. Lauwers, MD, and Michio Shimizu, MD* Am J Surg Pathol 2006, November ; Vol. 30: 1561– 1569 指導老師: 方嘉郎;報告人: 李俊志
Introduction v IPMN is characterized by a predominantly noninvasive growth pattern with mucin production and cystic duct dilatation. v The distinction between IPMN and pancreatic intraepithelial neoplasia (Pan. IN) , which is the common precursor of invasive carcinomas
Introduction v 1. 2. v 1999, Yonezawa Villous dark cell type--- resembles colorectal villous; MUC 2 (+); intestinal type Papillary clear cell type--- resembles gastric foveolar epi. MUC (-); gastric type have not been fully described.
Introduction v 1. 2. 3. 4. Mucin profiles MUC 1 --- membrane-bound mucin MUC 2 --- secretory mucins, intestinal MUC 5 AC--- secretory mucins, gastric foveolar MUC 6 --- secretory mucins, pyloric gland.
Introduction v 1. 2. 3. GOALS: Evaluate the distribution of the IPMNs and their derived invasive carcinomas Refine their differences of gastric-type and intestinal-type--- regard to their histopathologic characteristics and mucin profiles Better characterize the gastric type
Materials and Methods v 1. 2. 3. 4. 5. Patients’ data--- 80 cases: M/F(49/31) Mean age(65. 3 y/o, 37 -83 y/o); From 1983 to 2003; from 4 hospitals (Saitama Medical School, Japan; Kyoto University Hospital, Japan; Fujita Health University, Japan, and Massachusetts General Hospital, USA) Exclusion: IPMNs of other type (ex: pancreatobiliary, oncocytic) and IPMN-like lesions
Materials and Methods v based on 1. WHO classification on tumors of the digestive system international consensus guidelines for IPMN and mucinous cystic neoplasms (MCNs) 2. v v Gastric type--- clear/lightly eosinophilic; columnar; round to ovoid nuclei; no/minimal pseudostratified Intestinal type--- dark eosinophilic; columnar; oval to spindle nuclei; pseudostratified
Materials and Methods v 1. 2. 3. 4. 5. 6. 7. 8. Evaluation of 8 histologic features: distribution--- main duct or branch duct histologic grade---benign/borderline/noninvasive intraluminal nodular growth pyloric glandlike structures low-grade Pan. IN-like complex within the tumor, atrophy of the surrounding pancreas tissue mucous lake formation occurrence of invasive carcinoma.
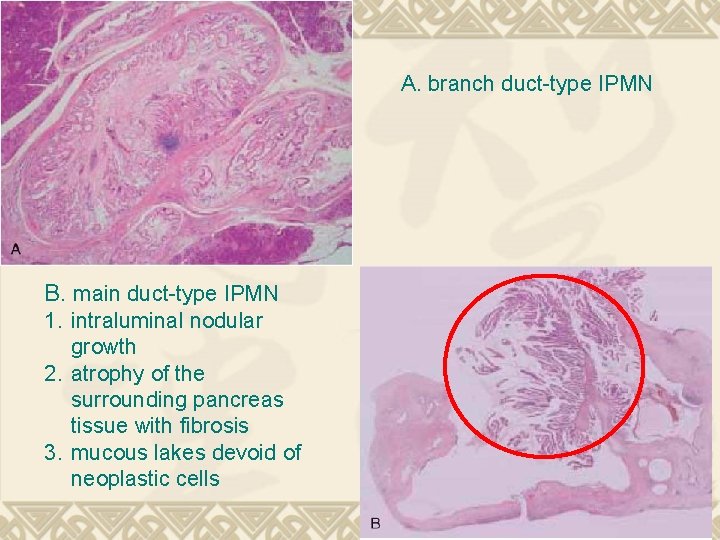
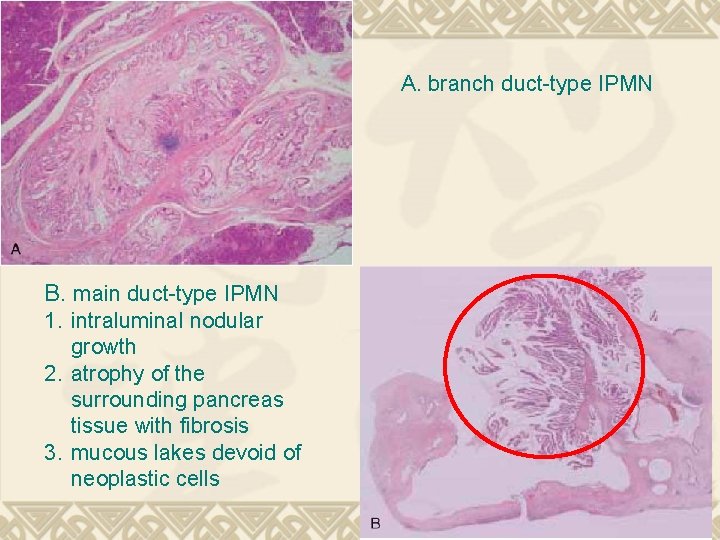
A. branch duct-type IPMN B. main duct-type IPMN 1. intraluminal nodular growth 2. atrophy of the surrounding pancreas tissue with fibrosis 3. mucous lakes devoid of neoplastic cells
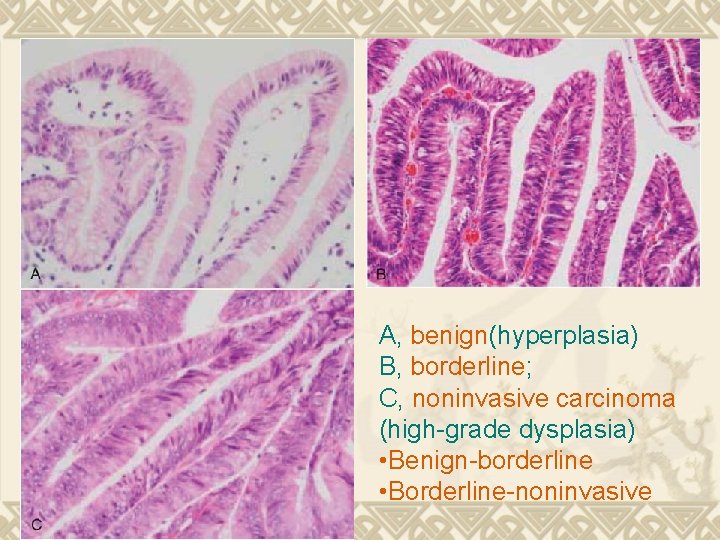
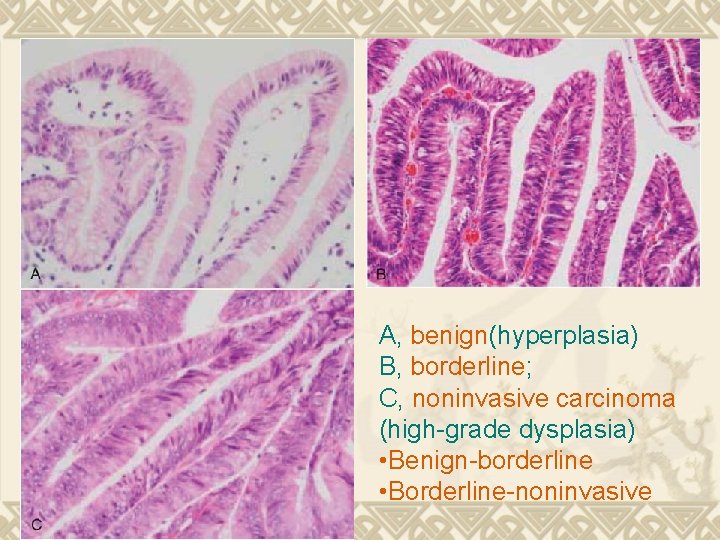
A, benign(hyperplasia) B, borderline; C, noninvasive carcinoma (high-grade dysplasia) • Benign-borderline • Borderline-noninvasive
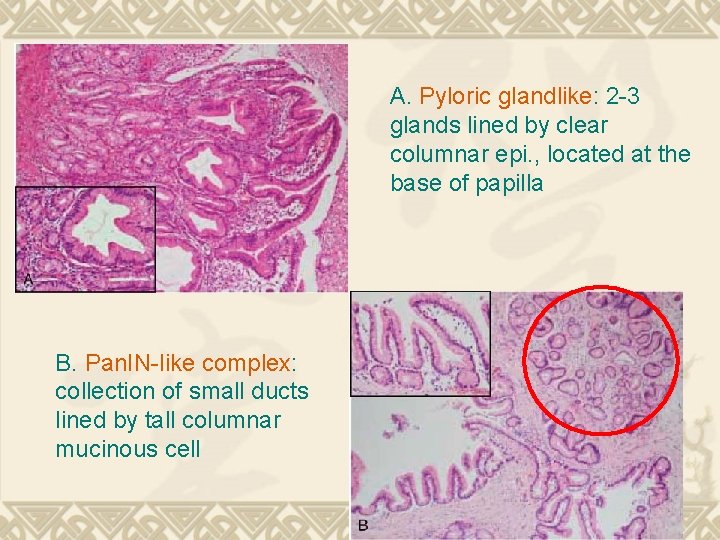
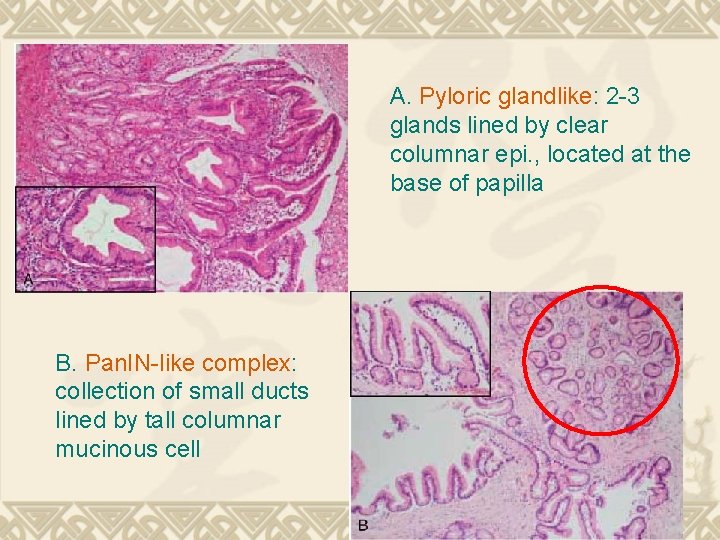
A. Pyloric glandlike: 2 -3 glands lined by clear columnar epi. , located at the base of papilla B. Pan. IN-like complex: collection of small ducts lined by tall columnar mucinous cell
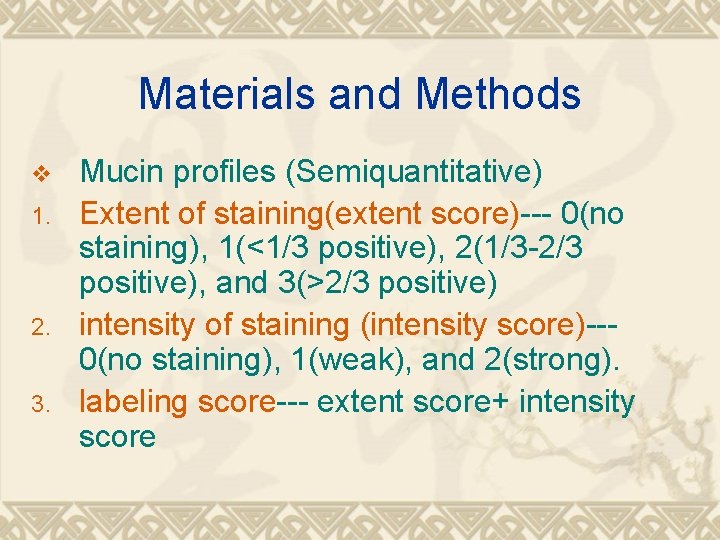
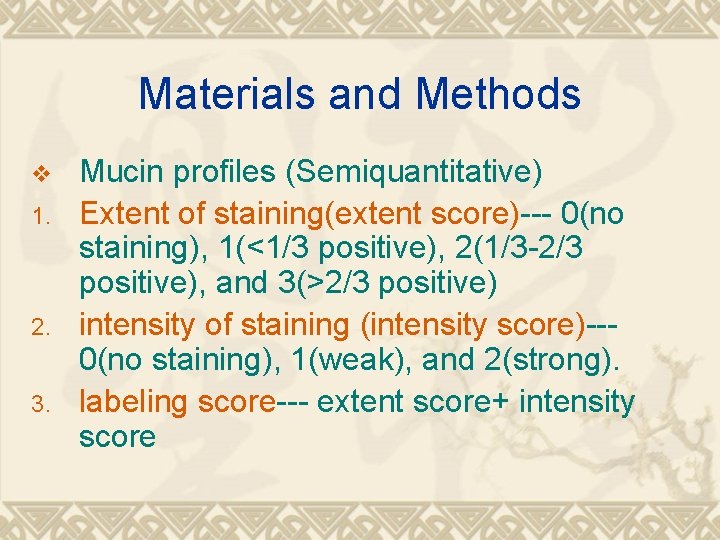
Materials and Methods v 1. 2. 3. Mucin profiles (Semiquantitative) Extent of staining(extent score)--- 0(no staining), 1(<1/3 positive), 2(1/3 -2/3 positive), and 3(>2/3 positive) intensity of staining (intensity score)--0(no staining), 1(weak), and 2(strong). labeling score--- extent score+ intensity score
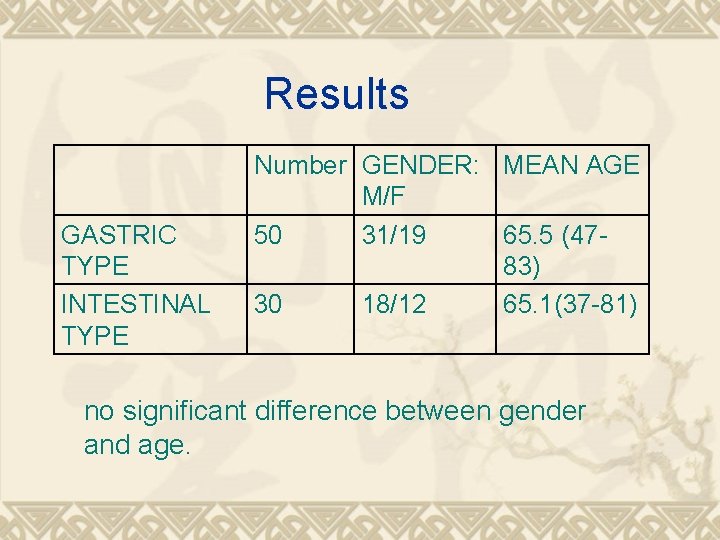
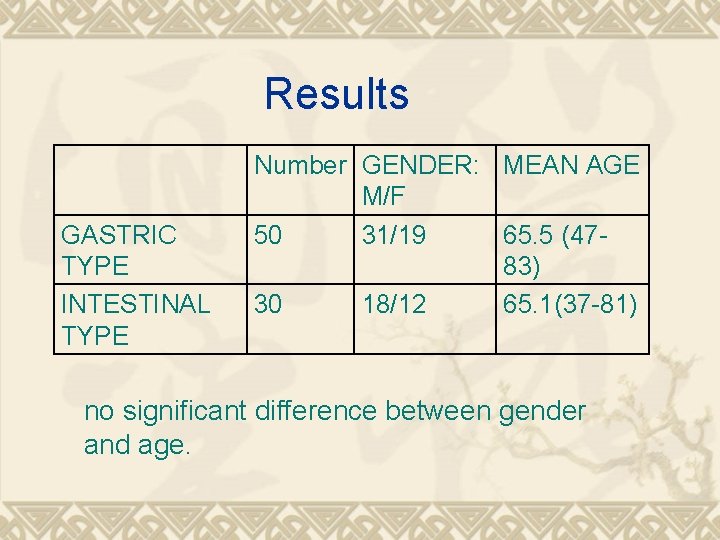
Results GASTRIC TYPE INTESTINAL TYPE Number GENDER: MEAN AGE M/F 50 31/19 65. 5 (4783) 30 18/12 65. 1(37 -81) no significant difference between gender and age.
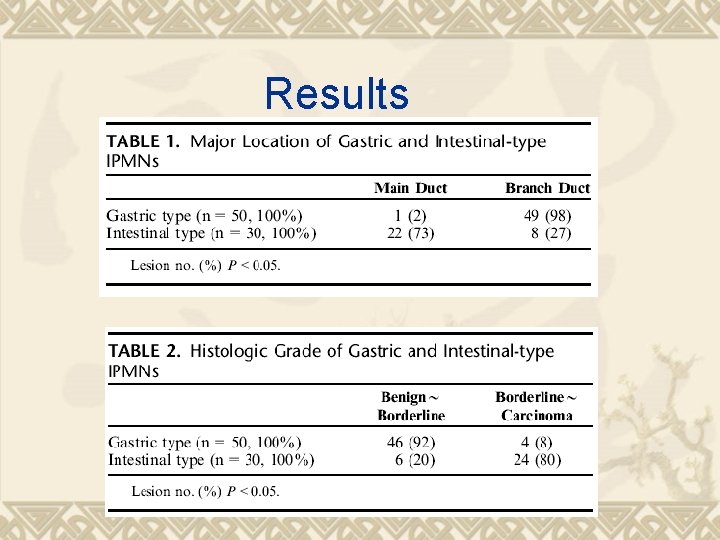
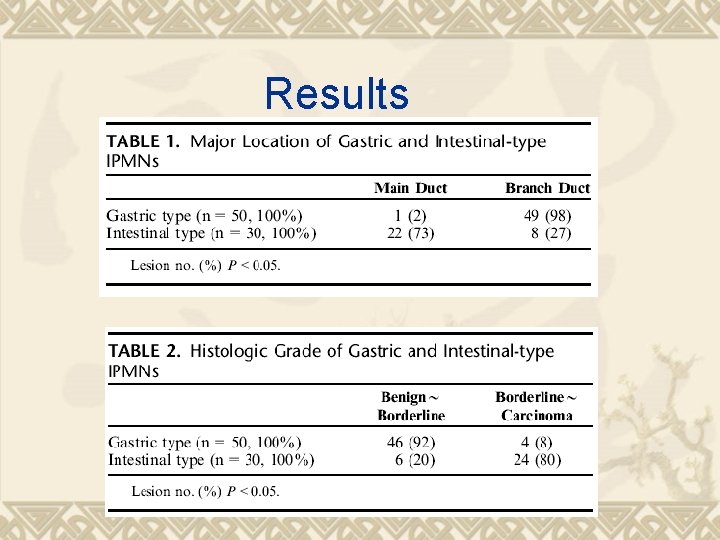
Results
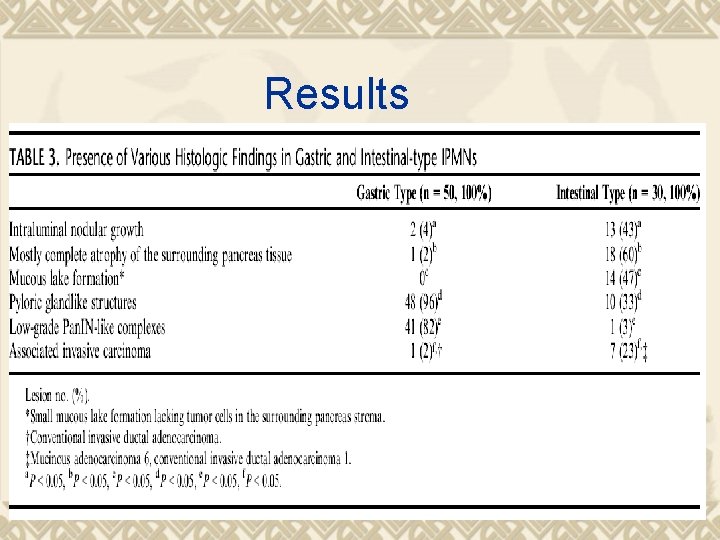
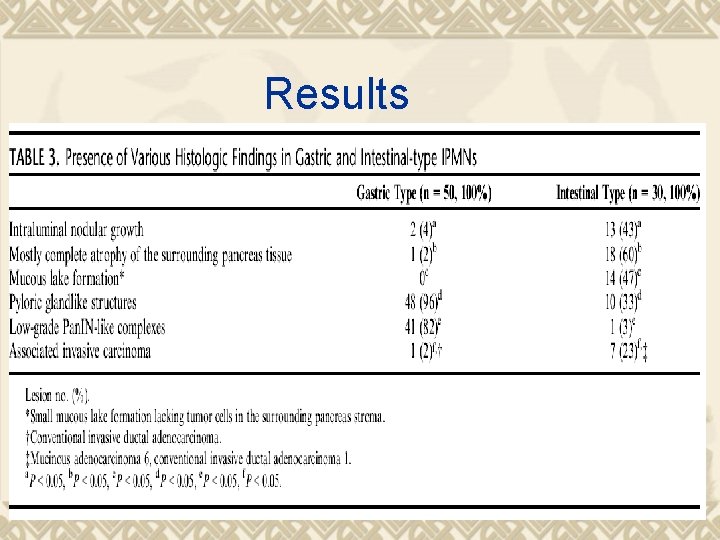
Results
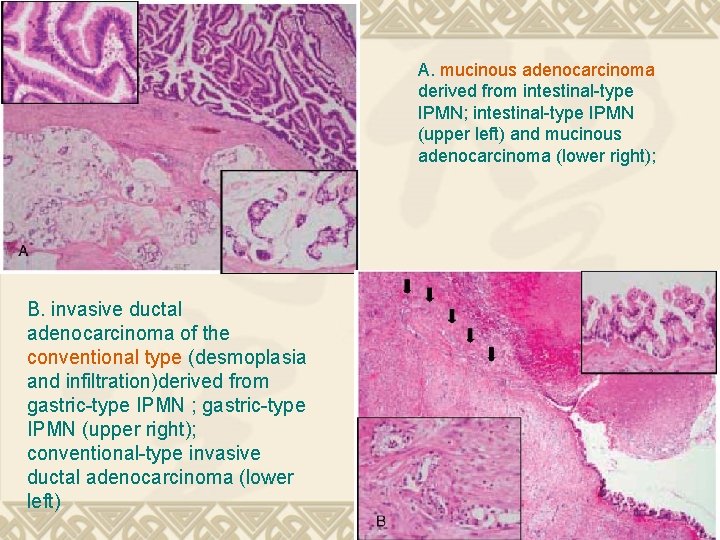
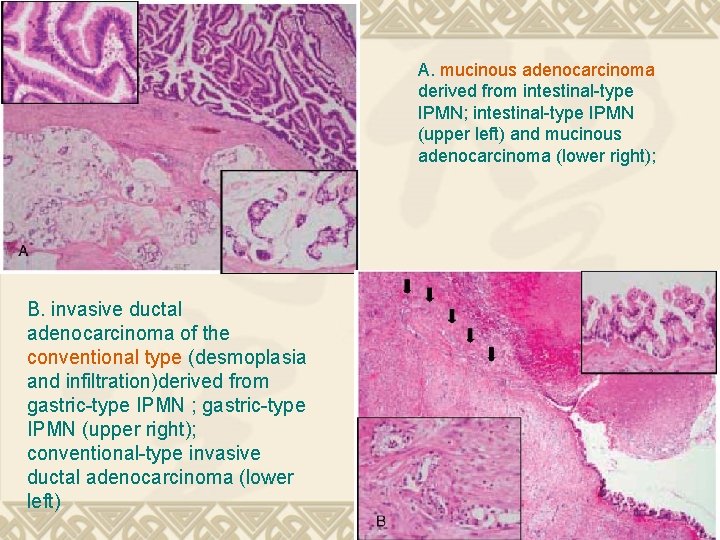
A. mucinous adenocarcinoma derived from intestinal-type IPMN; intestinal-type IPMN (upper left) and mucinous adenocarcinoma (lower right); B. invasive ductal adenocarcinoma of the conventional type (desmoplasia and infiltration)derived from gastric-type IPMN ; gastric-type IPMN (upper right); conventional-type invasive ductal adenocarcinoma (lower left)
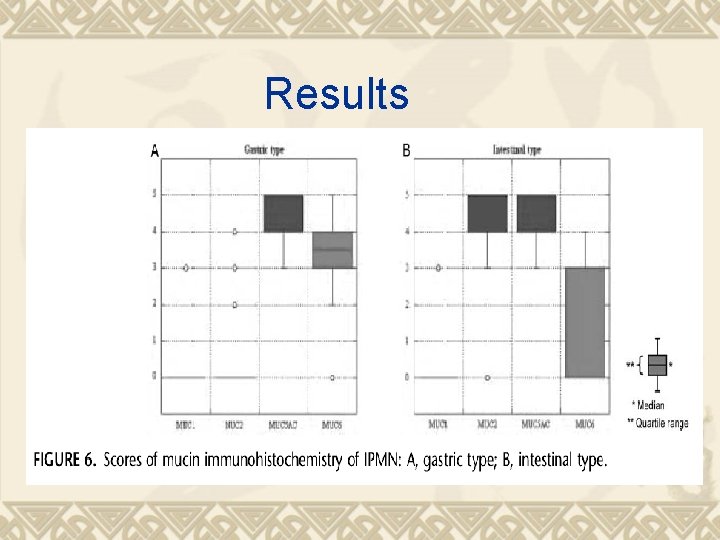
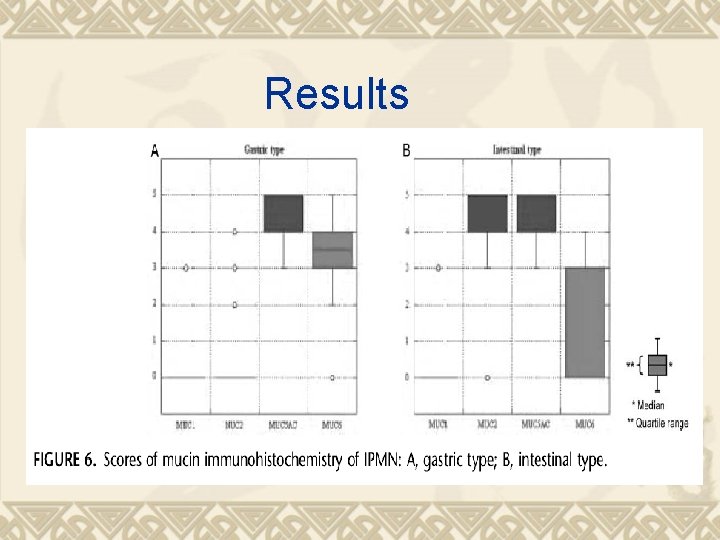
Results
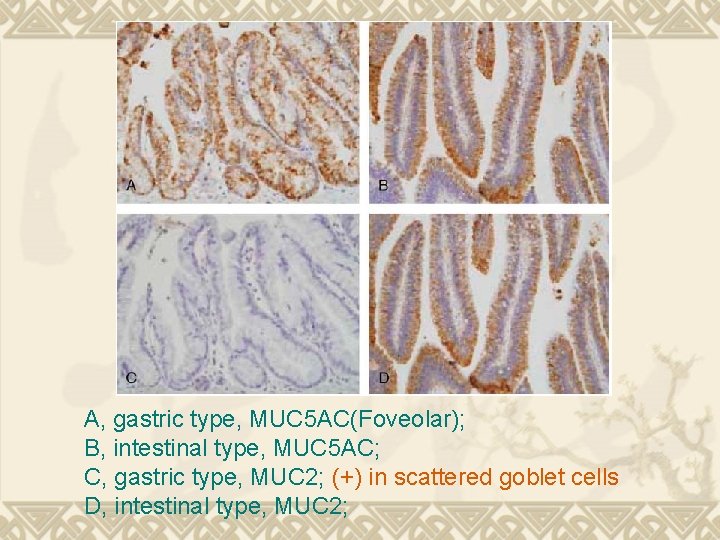
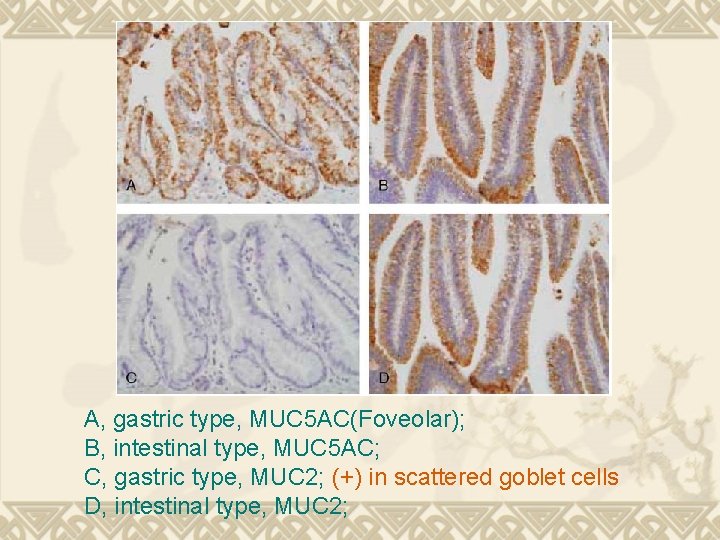
A, gastric type, MUC 5 AC(Foveolar); B, intestinal type, MUC 5 AC; C, gastric type, MUC 2; (+) in scattered goblet cells D, intestinal type, MUC 2;
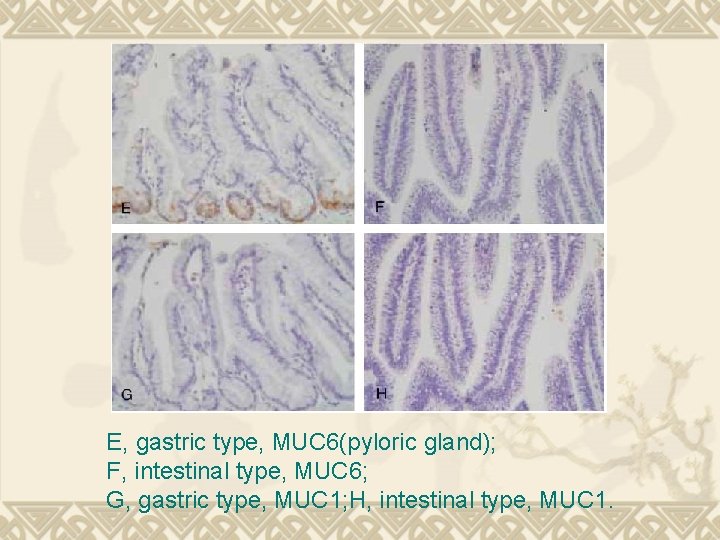
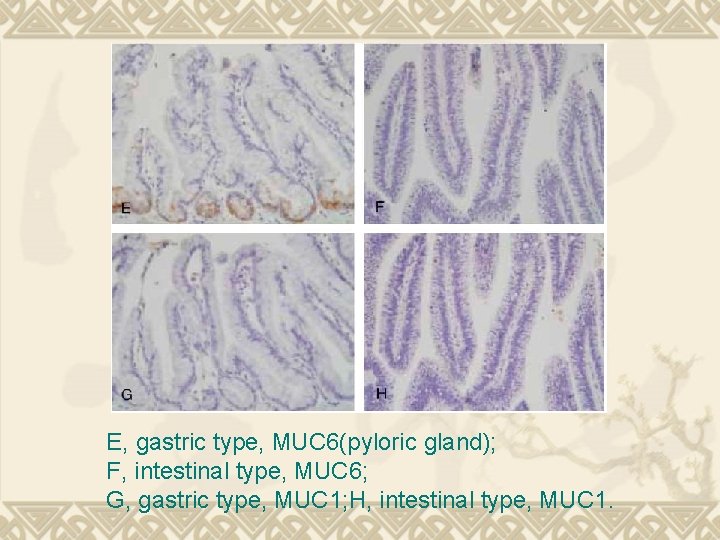
E, gastric type, MUC 6(pyloric gland); F, intestinal type, MUC 6; G, gastric type, MUC 1; H, intestinal type, MUC 1.
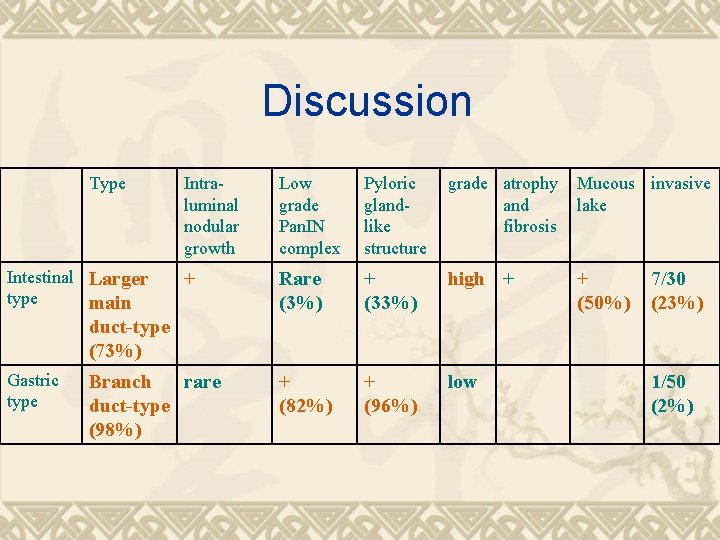
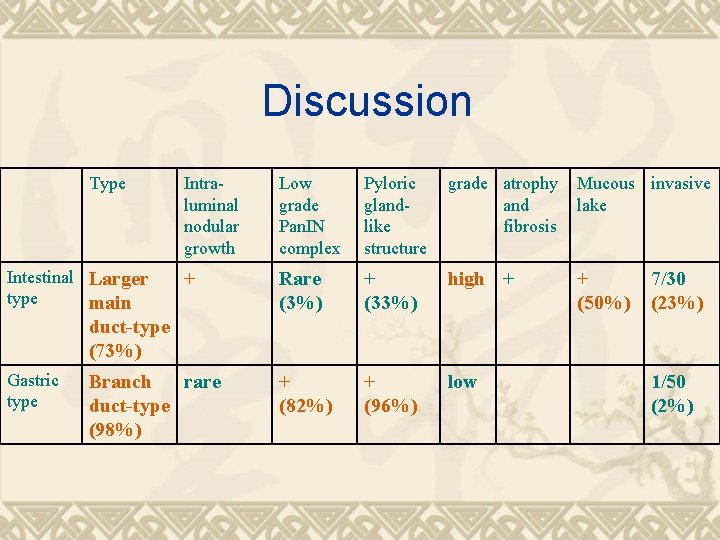
Discussion Type Intestinal Larger type main Intraluminal nodular growth Low grade Pan. IN complex Pyloric glandlike structure grade atrophy and fibrosis Mucous invasive lake + Rare (3%) + (33%) high + + (50%) + (82%) + (96%) low 7/30 (23%) duct-type (73%) Gastric type Branch rare duct-type (98%) 1/50 (2%)
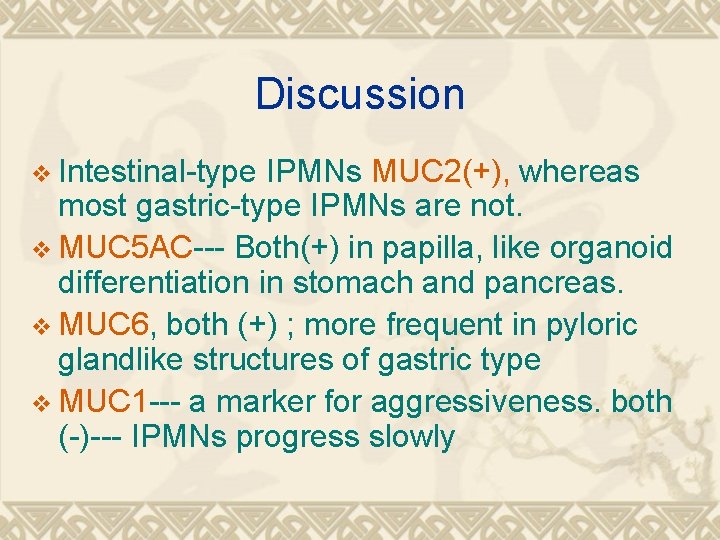
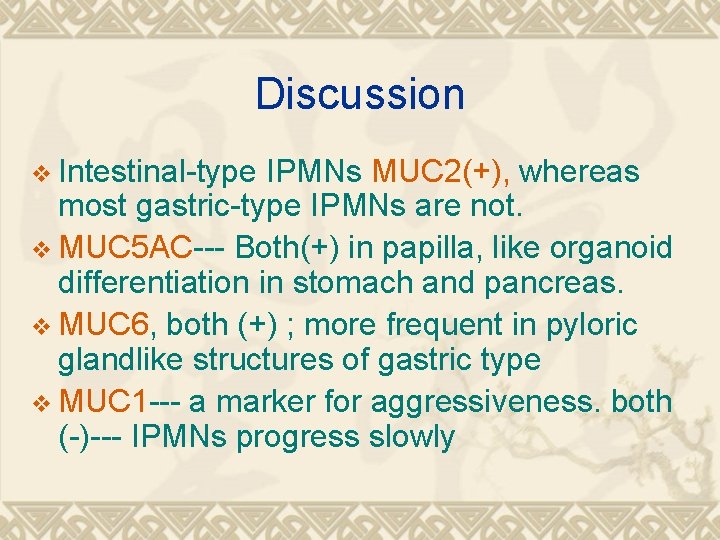
Discussion v Intestinal-type IPMNs MUC 2(+), whereas most gastric-type IPMNs are not. v MUC 5 AC--- Both(+) in papilla, like organoid differentiation in stomach and pancreas. v MUC 6, both (+) ; more frequent in pyloric glandlike structures of gastric type v MUC 1 --- a marker for aggressiveness. both (-)--- IPMNs progress slowly
Discussion v 1. 2. Malignant change: intestinal >gastric Mucin pools --- associated with mucinous adenocarcinoma in intestinaltype IPMNs; lead to muconodular infiltration, like occurred in invasive colorectal villous tumors; sign of invasive Gastric-type IPMNs--- conventional type
Discussion v 1. 2. 3. 4. 5. Gastric-type IPMNs V. S Low-grade Pan. IN Both have “pyloric gland-like structures” and “low-grade Pan. IN-like complex” Both are MUC 5 AC+/MUC 2 Both have genetic alterantions associated with ductal carcinoma, ex: K-ras, p 53, DPC 4/Smad 4, p 16 (more common in Low-grade Pan. IN) Low-grade Pan. IN gastric-type IPMNs Further molecular studies still needed
Discussion v 1. 2. Two hypothesis Gastric type, which being called “null-type” by Adsay et al, may progress to intestinal type or others Different phathogenesis between the two types --- different mode of spreading through the pancreatic ductal system Gastric type --- low-grade Pan. IN-like complex Intestinal type --- involving small ducts with complete atrophy of surrounding parenchyma
 Ipmn
Ipmn Operacja ipmn
Operacja ipmn Pancreatoblastoma
Pancreatoblastoma Malignant neoplasm of the blood-forming organs
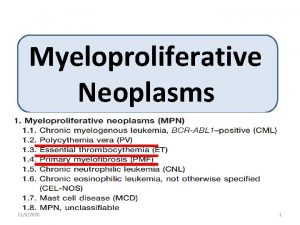
Malignant neoplasm of the blood-forming organs Myeloproliferative neoplasm
Myeloproliferative neoplasm Plasma cell neoplasm
Plasma cell neoplasm Malignant neoplasm of liver
Malignant neoplasm of liver Benign neoplasm of ovary d27 artinya
Benign neoplasm of ovary d27 artinya Myeloproliferative syndrome
Myeloproliferative syndrome Kode icd 10 tumor leher
Kode icd 10 tumor leher Neoplasia
Neoplasia Bronchogenic neoplasm
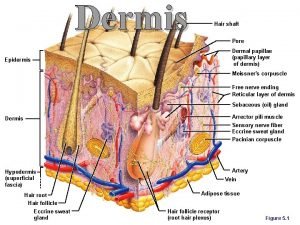
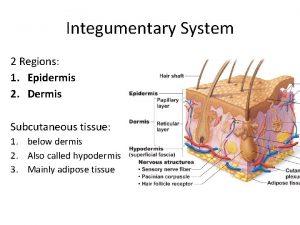
Bronchogenic neoplasm Stratum germinativum
Stratum germinativum Mesangial
Mesangial Longitudinal sulcus heart
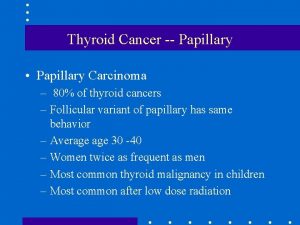
Longitudinal sulcus heart Papillary carcinoma
Papillary carcinoma Dermal papillae
Dermal papillae Pericardiu
Pericardiu Hair root plexus
Hair root plexus Follicular adenoma
Follicular adenoma Stratum corneum
Stratum corneum Renal cell carcinoma
Renal cell carcinoma Uneven junction of the dermis with the epidermis
Uneven junction of the dermis with the epidermis Papillary layer function
Papillary layer function Pulmonary valve sheep heart
Pulmonary valve sheep heart