Introduction to Physical Therapy Occupational Therapy and Common


- Slides: 30
Introduction to Physical Therapy, Occupational Therapy, and Common Orthotics in Musculoskeletal Medicine Hassen Berri DO University of Michigan Sports Medicine Fellow
Discussion Focus • Gain a general understanding of PT/OT • PT/OT Scripts- Important characteristics • Common orthotics and other pearls for common musculoskeletal problems
Very General Differences: PT and OT • OT can focus on fine motor tasks, ergonomics, posture, ADLs, IADLs, lymphedema, work specific tasks, and upper extremity function, especially hand function • PT can focus on gross motor tasks, manual therapy, core strength, larger muscle groups, compound movements, gait, and balance
What is PT/OT for MSK Medicine? • Designed to encourage the healing process and enhance or regain function, quality of life, and decrease pain. • This is done through EDUCATION, modalities, physical manipulation, joint ROM & flexibility training, neuromuscular retraining, strengthening etc. with progression to HEP • These are also things you can place in a therapy script!
General principles • Muscles not used will shorten and antagonists may lengthen • This may cause asymmetries throughout the body leading to more of the above • Muscles that are shortened or overly lengthened for a prolonged period of time don’t fire as well, and become weak • Muscles cause motion about a joint and also provide static and dynamic support for joints as they go through their ROM
Which patients should do PT/OT • Patients with time, resources, and motivation • Patients that you feel need some supervision and extra attention • Patient’s afraid to move or hurt themselves • Patients who have not did well with home exercises alone • Patient’s who you want to trial modalities/orthotics/equipment
EDUCATION • Should usually be the primary focus of these visits (limited visits, copays, short-lived results) • Teaching stretches, exercises, proper form, and other pearls on how to use equipment, and being self-sufficient when therapy is over • Depending on patient and pathology, may take only 1 -2 sessions • Results are dependent on completion and continuation of home program
Physical Manipulation • • • Facilitated positonal release Myofascial release Massage Muscle Energy Techniques HVLA (high velocity, low amplitude)
Joint ROM and Flexibility Passive vs Active ROM To get a baseline and monitor progress Goal of restoring pain free active ROM To prevent joint contractures To help tolerance of motion, reduce postimmobilization stiffness/pain POSSIBLE FACTORS • Intrinsic joint capsule, scar tissue, fascia, surrounding ligaments, tendons, muscles, and other anatomic barriers etc. • • •
Neuromuscular Retraining • Muscles not firing optimally/synchronously and movements about a joint are suboptimal SECONDARY TO: - Biomechanical factors (loss of ROM) - Neurologic- neurologic injury/recovery - Pain inhibition - Disuse/abuse/misuse of neuromuscular system
Strengthening • • • Isometric- easiest on joints Concentric- best for isolation Eccentric- tendon remodeling, muscle damage Open chain exercises: no fixed distal contact Closed chain exercises: fixed distal contact
Modalities Ice Heat US TENS unit Laser Etc. Overall palliative; weak evidence that this makes the patient much better. • Overall not a good use of a therapy if modalities is the majority of sessions • Can be useful in doing “no harm” • •
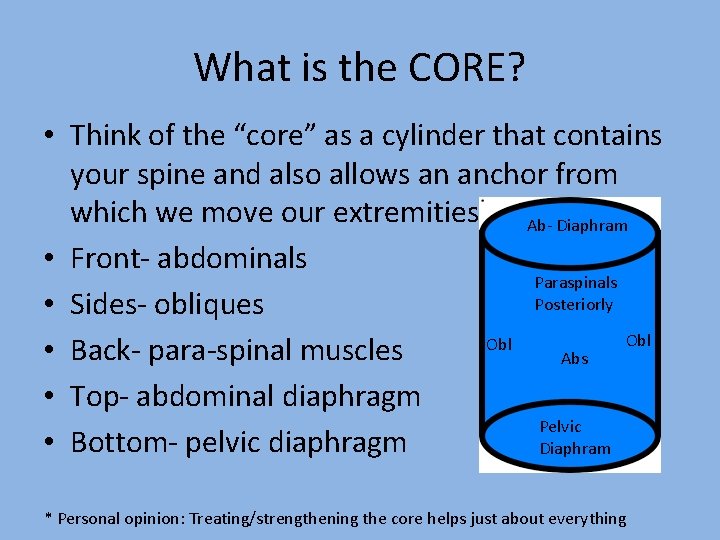
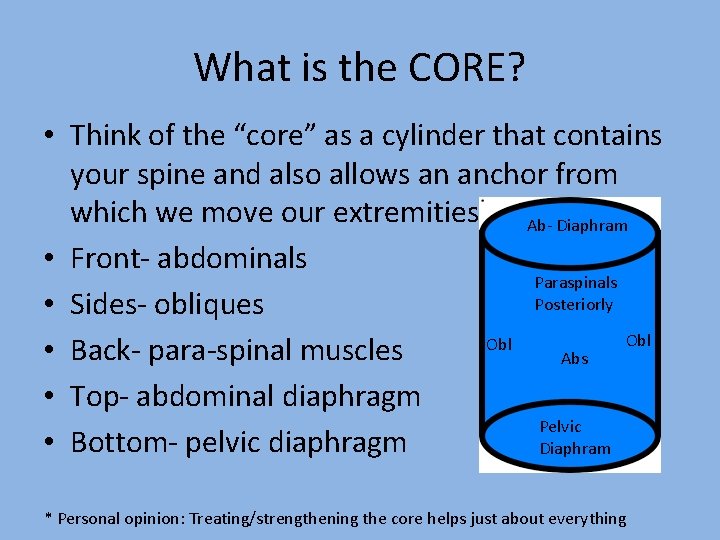
What is the CORE? • Think of the “core” as a cylinder that contains your spine and also allows an anchor from which we move our extremities Ab- Diaphram • Front- abdominals Paraspinals Posteriorly • Sides- obliques Obl • Back- para-spinal muscles Abs • Top- abdominal diaphragm Pelvic • Bottom- pelvic diaphragm Diaphram * Personal opinion: Treating/strengthening the core helps just about everything
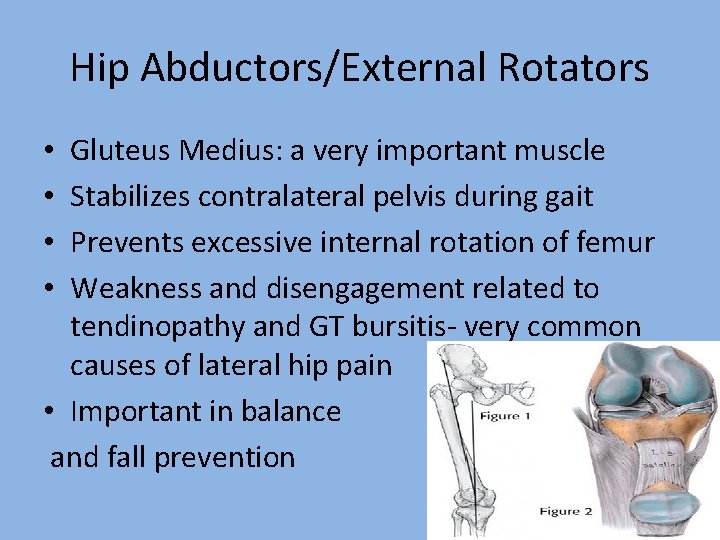
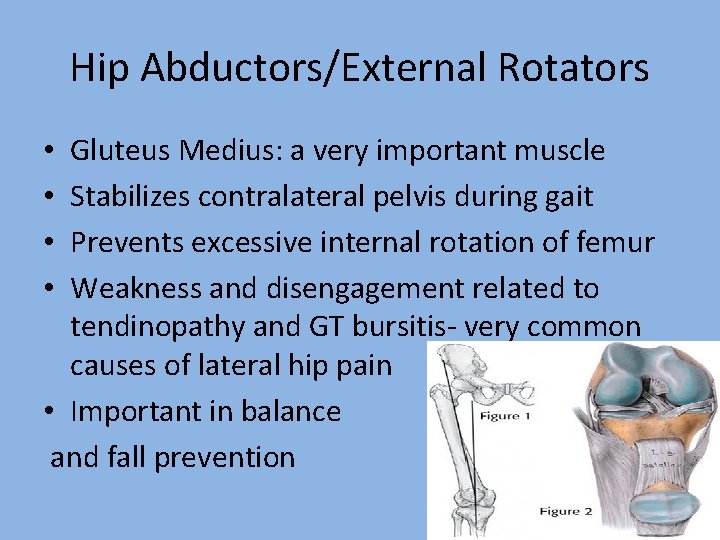
Hip Abductors/External Rotators Gluteus Medius: a very important muscle Stabilizes contralateral pelvis during gait Prevents excessive internal rotation of femur Weakness and disengagement related to tendinopathy and GT bursitis- very common causes of lateral hip pain • Important in balance and fall prevention • •
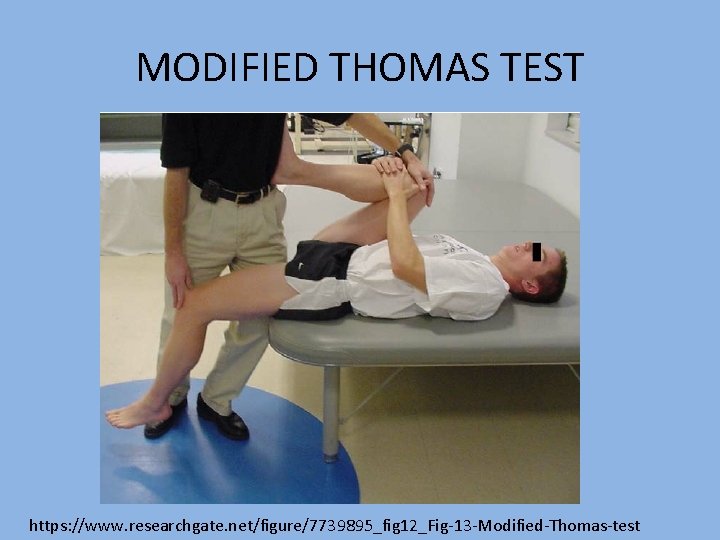
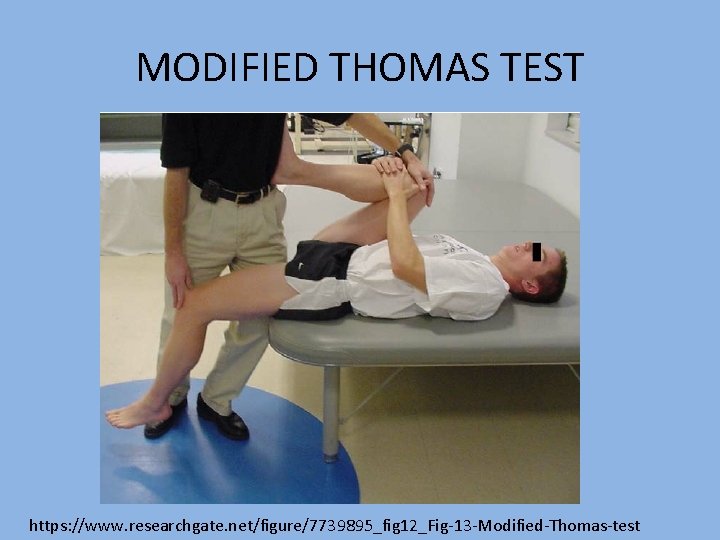
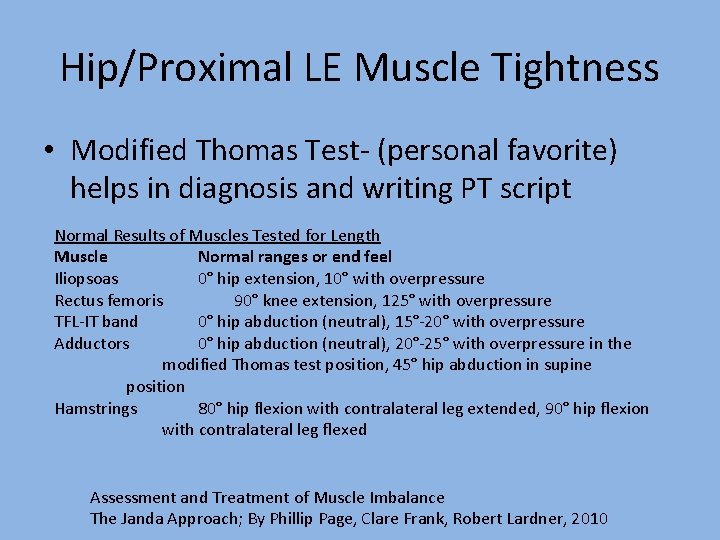
MODIFIED THOMAS TEST https: //www. researchgate. net/figure/7739895_fig 12_Fig-13 -Modified-Thomas-test
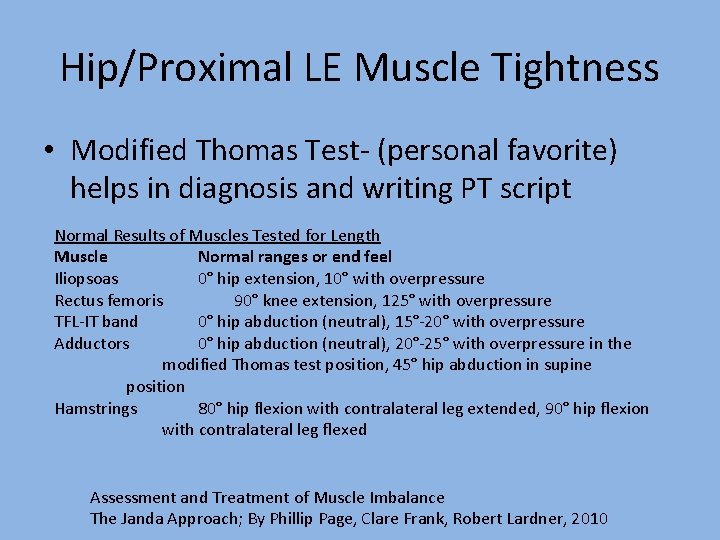
Hip/Proximal LE Muscle Tightness • Modified Thomas Test- (personal favorite) helps in diagnosis and writing PT script Normal Results of Muscles Tested for Length Muscle Normal ranges or end feel Iliopsoas 0° hip extension, 10° with overpressure Rectus femoris 90° knee extension, 125° with overpressure TFL-IT band 0° hip abduction (neutral), 15°-20° with overpressure Adductors 0° hip abduction (neutral), 20°-25° with overpressure in the modified Thomas test position, 45° hip abduction in supine position Hamstrings 80° hip flexion with contralateral leg extended, 90° hip flexion with contralateral leg flexed Assessment and Treatment of Muscle Imbalance The Janda Approach; By Phillip Page, Clare Frank, Robert Lardner, 2010
Example PT/OT script • Dx: (eg. ) Right Patellofemoral syndrome • Tx desired: “please Evaluate and Treat, please include: IT band, Hip flexor and quadriceps stretching program. Also include hip abductor, Quad and hamstring strengthening after neuromuscular retraining to ensure adequate firing and Muscle activation, Progress to HEP” • Freq: 1 -3 times per week • Duration: 1 -2 months
Orthotics • Definition: braces, splints, and other devices fabricated for: - Immobilization - Protection/alignment preservation - Pain mitigation/comfort - ROM/contracture prevention - Etc. • Does not include prosthetics or assistive devices
Low back pain • +/- lumbar corset to be worn occassionally • May help with symptoms by increasing intraabdominal pressure thus increasing support • May help by providing some propioceptive feedback • Home traction unit? • SI joint pain? - SI joint belt with walking n Google Images

Knee Osteoarthritis • Medial compartment: knee sleeve, medial offloading brace, lateral wedge in shoe • Lateral compartment: knee sleeve, lateral offloading brace, medial wedge • Patellofemoral compartment- knee sleeve, patellar J-brace
Carpal Tunnel Syndrome • CTS wrist splints to be worn during sleep (neutral to 20 degrees extn) • Avoidance of compression of carpal tunnel • Avoid prolonged and forceful wrist extn/flxn
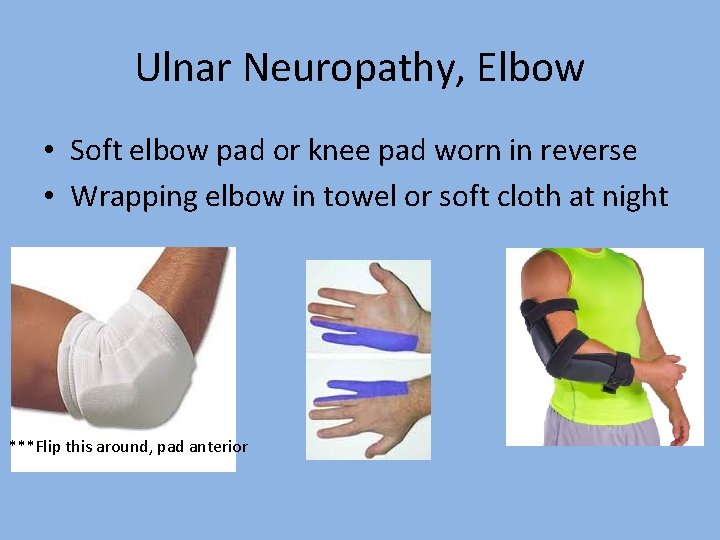
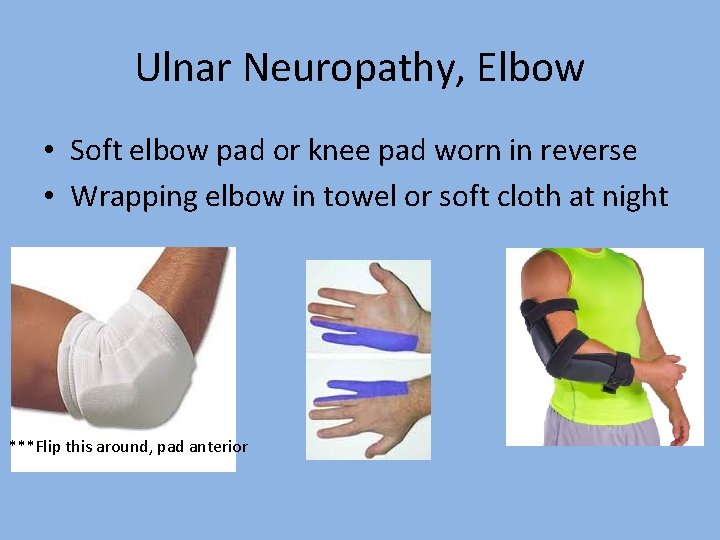
Ulnar Neuropathy, Elbow • Soft elbow pad or knee pad worn in reverse • Wrapping elbow in towel or soft cloth at night ***Flip this around, pad anterior
Patellofemoral pain, MCC anterior knee pain in runners • Knee sleeve vs Patellar J brace • Semi-rigid arch supports for overpronators • Work on biomechanical abnormalities detected on exam in therapy/home exercises • Common targets: Core, Glut max/med, IT band, hip flexors, VM etc.
Shin Splints/tibial stress syndrome • OTC compression sleeves and relative rest • Arch supports for pes planus and over pronators • Intrinsic foot muscle strengthening, eccentric plantarflexion strengthening • Relative rest from running, pain as guide

Plantar fasciitis Semi-rigid arch supports OTC (Power-step) Night splinting sock/dorsi-flexion splint Don’t walk anywhere barefooted Avoid flip-flops Stretch gastrocs/soleus/achilles and plantarfascia • Intrinsic foot muscle strengthening • • •
Pes Planus into adulthood • Asymptomatic? No Orthotic indicated usually • Consider arch supports if they have low back, hip, knee, ankle, leg, foot pain • May signal peripheral neuropathy so consider testing sensation • Intrinsic foot muscle strengthening may help
Initial tx: suspect metatarsal stress fracture or high ankle sprain • Aircast walking boot vs NWB w crutches initial management • Clues this may be a high ankle sprain: squeeze test, passive dorsiflexion/eversion pain, pain over the distal syndesmosis
Distal phalanx, non-displaced simple fracture • Hard soled shoe, or post-op shoe • Why- decrease motion through site of injury
Conclusions/Closing Thoughts • A better understanding and utilization of PT will help your patients • A better physical therapy script will ensure key targets are being addressed and insurance covers • Utilization of orthotics for MSK pathologies can be very helpful
Thank you