Clinical Examination for Splinting Somaya Malkawi Ph D






- Slides: 57
Clinical Examination for Splinting Somaya Malkawi, Ph. D University of Jordan Occupational Therapy Department

History, interviews, chart review, reports Part 1 11/10/2020
Obtaining a history You should obtain the history from medical charts, surgical, radiologic reports Physician’s referral or prescription Age, gender, diagnosis Past medical history and dates of occurrence Occupation Pertinent medical history (e. g. diabetes, epilepsy, kidney, gout) UE dysfunction is due to orthopedic or neurological or trauma affecting soft tissue such as burn, tendon laceration) Anatomic structure involved at surgery Protocol : different and decide on the rehabilitation program and timing 11/10/2020
Interview Impact of condition on functioning, family, economic status, social/emotional wellbeing Co-histories from family, parents, friends, caregivers Check questions page 77 Habits, stress, obesity
observation In the initial process of evaluation while interviewing your client, use your observation skills! Nonverbal communication (facial expressions and body language) mood, emotions, and motivation. Use of the involved UE and trunk: some clients may exaggerate their impairment (guarding or less AROM) Check points to observe on (page 77) or (form 51) Posture of whole UE. . Asymmetry Resting hand posture: 10 – 15 wrist flex/ 10 UD / 15— 20 MCP flex 11/10/2020 Slight flexion and abd of thumb
palpation Muscle tone (PROM) ask pt to relax muscles Muscle symmetry (compare right and left) Scar density Tendon nodules Masses (ganglia) Skin temperature Wear sterile gloves

Assessments Part 2 11/10/2020
Pain No equipment is necessary. During initial evaluation; use a pain scale. Numeric analogue scale (1, 2, 3, … 10). Visual analogue scale (10 cm vertical line). Verbal rating scale (no pain, mild, moderate…). Graphic representation (point out pain on a body chart) (fig 5 -3) Pain questionnaires (e. g. Mc. Gill pain questionnaire) usually used by pain management centers. 11/10/2020
Methods Obtain a written description of the pain including the following factors: Level of pain: see previous slide. Location of pain: have the client point out his or her pain on a body chart and rate them (referred pain: palpation of one area results in pain in another area). Type of pain: throbbing ( )ﻧﺎﺑﺾ , aching, sharp, stabbing, shooting, burning, or hypersensitivity to light touch. Frequency of pain: constant or intermittent! What seem to cause the pain? What is pain associated with (e. g. AROM). Children’s report of pain (table 5 -3) 11/10/2020
Skin Color Temperature Texture Muscle atrophy Scarring Edema Hair pattern Sweating Watch for Fragile skin. . older people , steroids, diabetes) Skin allergies (bandages , adhesive, latex Monitor rashes after prescription

Wound assessment If the wound is closed; skip to scar assessment, if the wound is open, assess the following: Size: length and width using a ruler, do not touch the wound by the ruler except was sterile. What about future measurements? Depth: use sterile cotton swap only if pt is comfortable Color: wound are red, yellow, black, or any of them together. We love the red wound! 1. Red: Red uninfected, definite borders, granulation tissue present, apparent revascularization 11/10/2020
Wound assessment 2. Yellow: Yellow wound may have odor, draining and purulent, semi-liquid slough, usually in the late inflammatory stage, epithelialization will be delayed due to infection. dominant cellular activity is the macrophage (Pac Man), 3. Black: Black Presence of Escher (necrotic tissue) will increase the work required by the macrophage and delay healing. 11/10/2020
Wound assessment Drainage: mild, moderate, or heavy? 1. Serous: clear, white or slightly yellow, indicator of healthy open wound. Ø If infection is suspected, refer client back to the referring physician. 11/10/2020
Wound assessment Amount of discharge Oder of discharge: means infection, if present refer client back to the referring physician. Temperature: use thermometers or temperature tapes to measure the temperature of an area near the wound and compare it with an intact area. Ø Always observe the wound for the cardinal signs of infection: redness, swelling, increased temperature and pain. stages of wound healing and splinting precautions (next class) read chapter 11/10/2020
Scar assessment In assessing scar, consider the following: Ø Color: deep red lighter with time. Size: length x width. Flat/raised: the scar itself maybe flat or raised, if raised describe it in terms of mild or moderate. Sometimes their will be a lump under the skin which is a combination between scar and fluid, commonly it appears on the dorsum of the hand or on the wrist: describe it by location, size, and height. Adhesions: adhesions of superficial scar to underlying fascia and tendons. Can be seen during active movements. Observe and palpate and describe by mild, moderate, or sever or simply by raising the skin (the scar tissue) 11/10/2020
Scar assessment Precautions: Respect the healing of a new scar the tissue to which it may adhere. Do not move the scar if when a portion of the wound is still open. Do not aggressively attempt to move the scar within the first week after suture removal. Do not manipulate a scar strongly in the treatment or assessment of scar over a tendon in the early stages of healing. 11/10/2020
ROM Assessment Part 5 11/10/2020
Vascular status assessment Part 6 11/10/2020
Vascular status assessment Blood flow to the hand may be affected by proximal injuries or diagnoses, e. g. : Injury to the hand itself. Conditions such as Raynaud's phenomenon. 11/10/2020
Observation Consider the following: Color: White grayish (pallor): (pallor) arterial interruption. Congested purple blue: blue venous blockage. Dusky blue: blue chronic venous insufficiency. Red: Red venous problem or inflammatory phase of healing or infection. 11/10/2020
Observation Trophic changes (texture of the skin and nails) which can be the result of sympathetic nerve or vascular changes: Dry/moist. Shiny/dull. Pain: in 2/3 of clients with UE vascular problems. Aching, cramping, tightness, or cold intolerance. May be associated with vibration, cold, or repetition. 11/10/2020
Palpation tests of vascular status Capillary Refill Test: 1. firmly press on the distal portion of the volar finger or finger nail. 2. Until it turns white. 3. Release and count seconds. § Normal refill time is less than 2 seconds. 11/10/2020
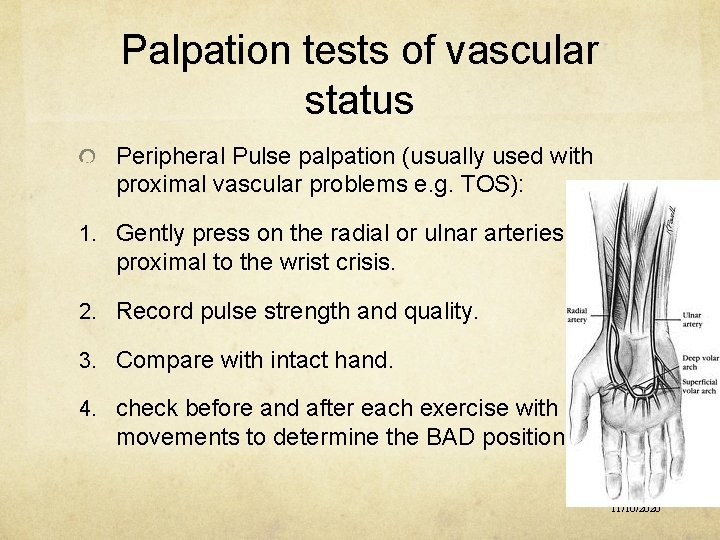
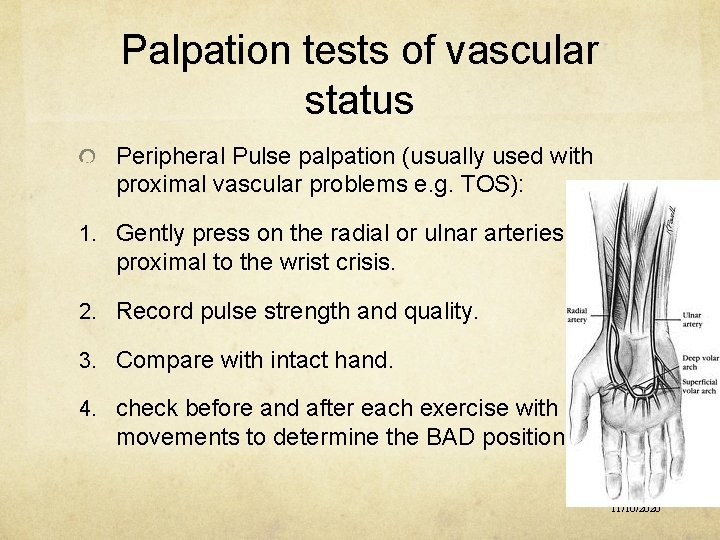
Palpation tests of vascular status Peripheral Pulse palpation (usually used with proximal vascular problems e. g. TOS): 1. Gently press on the radial or ulnar arteries just proximal to the wrist crisis. 2. Record pulse strength and quality. 3. Compare with intact hand. 4. check before and after each exercise with certain movements to determine the BAD position. 11/10/2020
Surface temperature assessment If forearm temperature is at least 4 degrees warmer than the fingertips temperature then vascular problems are expected. In testing for Raynaud’s phenomenon: 1. Test baseline temperature. 2. Test after being in a warm room for 30 minutes. 3. Record time of temperature returning to baseline. 4. Test after being immersed in ice for 20 seconds. 5. Record time of temperature returning to baseline. § Normal time is 10 minutes, Raynaud’s phenomenon patients may take 20 – 45 minutes. 11/10/2020
Assessment of Swelling Part 7 11/10/2020
Swelling Inflammatory swelling is a normal body response to injury, surgery or trauma, bringing good cells for healing. Normal reduction of edema begins within 2 weeks post surgery/trauma/injury but may take months to complete. Edema that does not decrease gradually and stays longer than 2 weeks is a problem!! it becomes more like gel interferes with joint and tendon motion �UE function. Inflammatory edema that occur after injury, surgery or insult starts as fluids spongy fibrotic!!. So what? ? Resistant to methods aimed at reducing the swelling 11/10/2020
swelling You should consider: Amount of swelling: Volumetric displacement. Circumferential measurement. Characteristics of edema: observation. Palpation. 11/10/2020
Volumetric displacement Equipments: Tank. Collection beaker. Graduated cylinder. Methods: See picture next slide. Notes: After measuring the affected hand, compare it to the intact hand, a difference of 10 -ml is significant and shows a systematic increase in volume. 11/10/2020
Volumetric displacement Precautions: This method must not be used with: open wounds, unstable vascular status, casts, external fixators, etc. Discussion: To increase test reliability, repeat the test 3 times and average. To increase test reliability, mark the forearm at the edge of water! Web-space between fingers. 11/10/2020
Circumferential measurement Equipments: Tape measure with finger loop (standardize location in relation to anatomic landmarks, standardize tension!). Methods: Apply tape measure. Tighten. Record reading. Discussion: To increase reliability: standardize location in relation to anatomic landmarks, standardize tension, and have the same therapist do the test all times. Compare to intact hand. 11/10/2020

observation Look for and document using a checklist including: Shininess. Dryness. Loss of joint creases. Skin color (erythematic, erythematic cyanosis, cyanosis or pallor). pallor 11/10/2020
Assessment of Sensation Part 8 11/10/2020
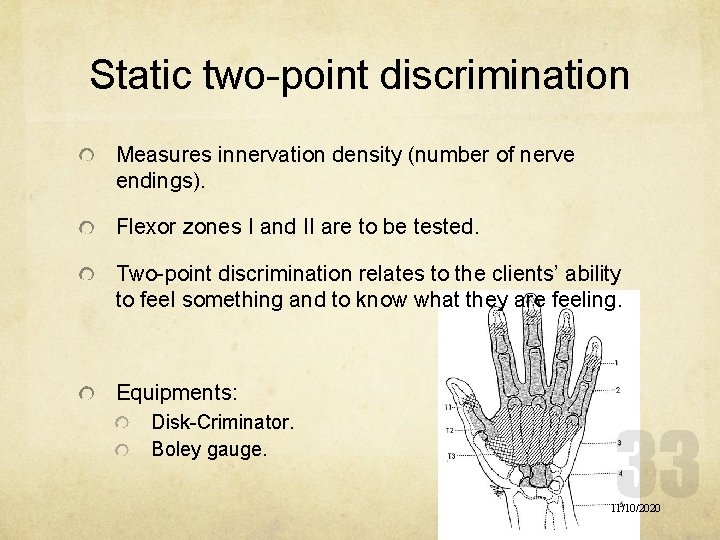
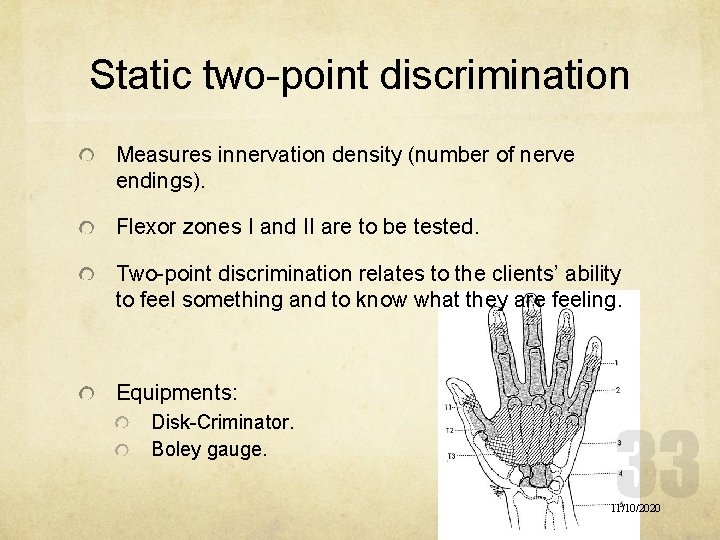
Static two-point discrimination Measures innervation density (number of nerve endings). Flexor zones I and II are to be tested. Two-point discrimination relates to the clients’ ability to feel something and to know what they are feeling. Equipments: Disk-Criminator. Boley gauge. 11/10/2020
Static two-point discrimination Methods: Ask patient to respond by “two” or “one”. Support client’s hand. Occlude the client vision. Start with 5 mm. Force must be applied to the point of blanching, in a longitudinal direction, and perpendicular to the skin. If patient recognizes 5 mm increase distance, vice versa. Begin distally and progress proximally. 11/10/2020
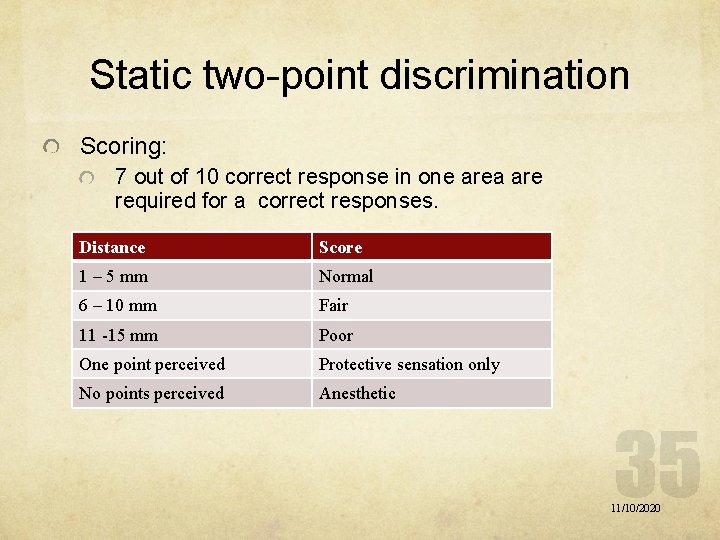
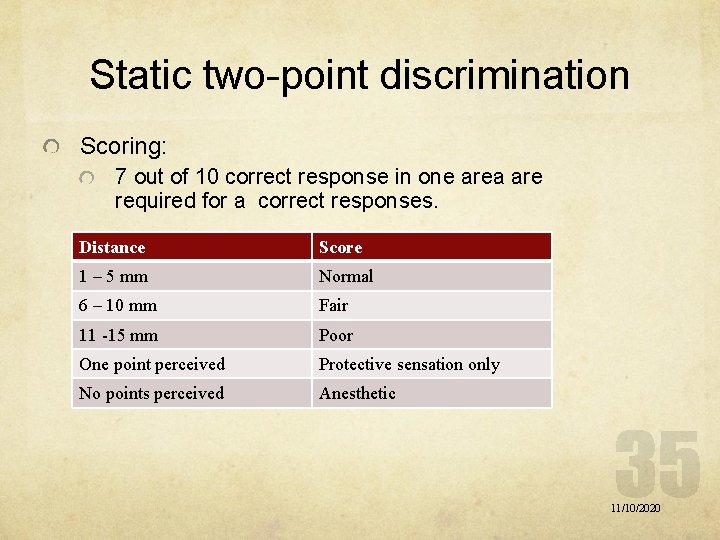
Static two-point discrimination Scoring: 7 out of 10 correct response in one area are required for a correct responses. Distance Score 1 – 5 mm Normal 6 – 10 mm Fair 11 -15 mm Poor One point perceived Protective sensation only No points perceived Anesthetic 11/10/2020
Moving two-point discrimination Always returns earlier than static two-point discrimination. Measures progress in return of sensation following nerve injury. Equipments: Disk-Criminator. Boley gauge. 11/10/2020
Moving two-point discrimination Methods: Ask patient to respond by “two” or “one”. Support client’s hand. Occlude the client vision. Start with 5 mm. Moving force must be applied to the point of blanching, in a longitudinal direction, and perpendicular to the skin, along the finger tip only. Begin proximally and progress distally. Begin with 5 – 8 mm and increase or decrease as needed. 11/10/2020
Moving two-point discrimination Scoring: 7 out of 10 correct response in one area are required for a correct responses. 2 mm is considered normal moving two-point discrimination. 11/10/2020

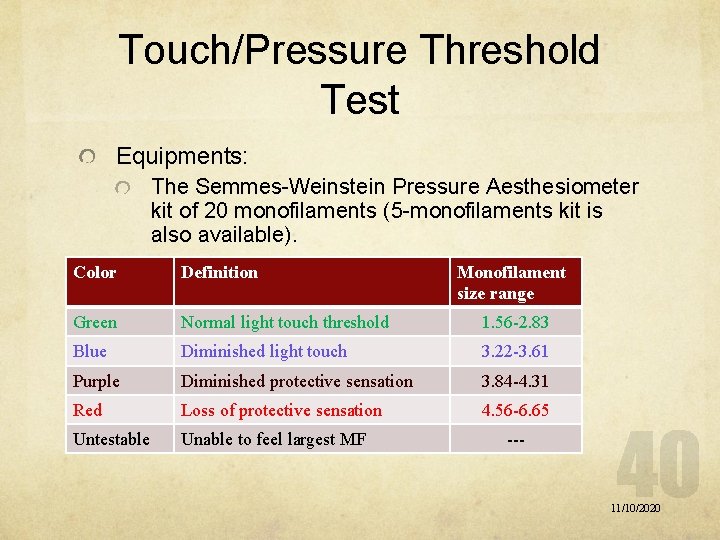
Touch/Pressure Threshold Test Recovers earlier than two-point discrimination sensation. Effective in identifying sensory impairments due to nerve compressions. Equipments: The Semmes-Weinstein Pressure Aesthesiometer kit of 20 monofilaments (5 -monofilaments kit is also available). 11/10/2020
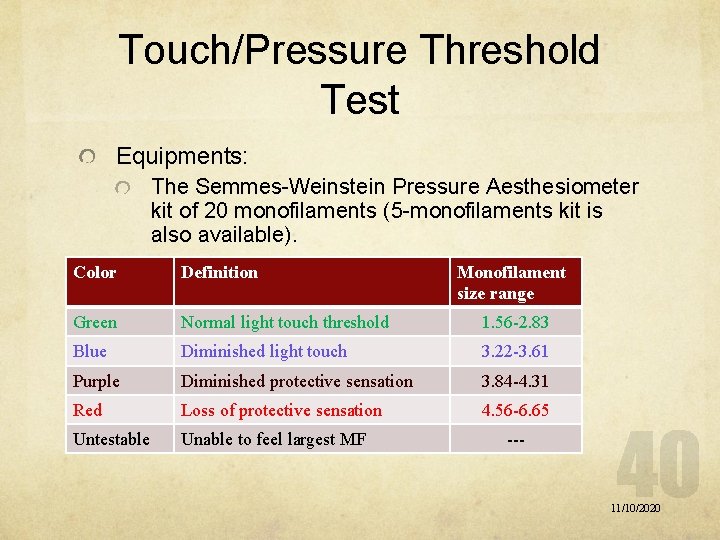
Touch/Pressure Threshold Test Equipments: The Semmes-Weinstein Pressure Aesthesiometer kit of 20 monofilaments (5 -monofilaments kit is also available). Color Definition Monofilament size range Green Normal light touch threshold 1. 56 -2. 83 Blue Diminished light touch 3. 22 -3. 61 Purple Diminished protective sensation 3. 84 -4. 31 Red Loss of protective sensation 4. 56 -6. 65 Untestable Unable to feel largest MF --- 11/10/2020
Touch/Pressure Threshold Test Methods: Explain the test to client. Support the hand in a putty. Occlude client’s vision. Ask the patient to respond with “touch” when he/she feels a touch. Begin with the largest green MF. If responded continue to smaller, if no response continue to larger MF. For green and blue MFs, apply the filament must be applied 3 times, 1 correct response is good enough. All other large MFs must be applied once for each trial. Distal to proximal. 11/10/2020
Touch/Pressure Threshold Test Filament must be applied perpendicular to the skin until it bends. Apply in 1 -1. 5 seconds hold for 1. 5 seconds lift in 1 -1. 5 seconds. Record on a hand chart (MF size and color). 11/10/2020
Localization of light touch The last sensory stimulus to return. Has a significant importance after nerve repair. Equipments: Smallest MF recognized earlier. Determined by the previous test. Cotton ball. 11/10/2020
Localization of light touch Methods: Explain the test to client. Support the hand in a putty. Occlude client’s vision. Touch the hand somewhere and dot it on a chart. Ask the patient to respond by opening his/her eyes and point out where you’ve touch him/her. If the response was correct do not draw any thing on the chart. If the client pointed out the stimulus in another place than given, draw an arrow from the dot you’ve drawn toward the place he/she pointed out. 11/10/2020
Assessment of coordination Part 9 11/10/2020
Coordination assessment O’Connor dexterity test. Nine-hole Peg test. Jebsen-Taylor hand function test. Minnesota rate of manipulation test. Crawford small parts dexterity test. Purdue peg board. 11/10/2020
Assessment of strength Part 10 11/10/2020
contraindications As simple as this: is the testing going to damage a healing process (fracture, ligament repair, tendon laceration, tendon transfer, etc)? So do not perform strength testing except when resistance is approved by referring physician. 11/10/2020

Grip strength test Always use the Jamar grip dynamometer. Do not ignore calibration! Testing setting: Client seated. Shoulder adducted. Elbow flexed to 90 degrees. Forearm neutral. Place dynamometer in the client’s hand. Provide gentle support at the base of the dynamometer. Instruct client squeeze smoothly not jerkily. Allow wrist extension during grip. 11/10/2020
Grip strength test Methods and procedures: Standard grip test: 3 trials on the 2 nd handle setting. Five-level grip test: 1 trial on each handle setting, when curve is a flat line or shows up/down/up/down waves lack of maximal efforts. Rapid change grip test: therapist alternate the dynamometer between hands for 10 trials for each hand. Thought to prevent client from self-limiting his grip strength!!!!! There are normative data, BUT compare to the intact hand if possible. 11/10/2020
Pinch strength test Use the pinchmeter. Testing setting: Client seated. Shoulder adducted. Elbow flexed to 90 degrees. Forearm neutral. Place pinchmeter in the client’s hand. Instruct client to squeeze smoothly not jerkily. 11/10/2020
Pinch strength test Methods and procedures, proceed as following: Lateral pinch (key pinch): pinchmeter between radial side of the index and the thumb. Three-point pinch (three jaw chuck pinch): pinchmeter between the pulp of the thumb and the pulps of the index and middle fingers. Two-point pinch (tip to tip pinch): between the tip of the index and the tip of the thumb. Ask the patient to pinch as hard as possible. 11/10/2020
MMT You’ve already learned that. Note: thumb and fingers tendon repairs are sufficiently strong to test until after 14 weeks after surgery. 11/10/2020
Splinting precautions Part 11 11/10/2020
Splint precautions Form 5 -2 Check off sheet 11/10/2020
Assessment of functional use Part 11 11/10/2020
Functional use DASH 11/10/2020
 Somaya arianfar
Somaya arianfar Soft and scotch splinting
Soft and scotch splinting Principles of pop
Principles of pop Peronus
Peronus Cow physical exam
Cow physical exam Ospe and osce
Ospe and osce Grunt test cattle
Grunt test cattle Objective structured clinical examination
Objective structured clinical examination Clinical performance examination
Clinical performance examination Grunt test cow
Grunt test cow Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Bamse för de yngsta
Bamse för de yngsta Bat mitza
Bat mitza Hur stor skarns är det för ett barn att få cancer
Hur stor skarns är det för ett barn att få cancer Jag har nigit för nymånens skära text
Jag har nigit för nymånens skära text Strategi för svensk viltförvaltning
Strategi för svensk viltförvaltning Romarriket tidslinje
Romarriket tidslinje Boverket ka
Boverket ka Ledningssystem för verksamhetsinformation
Ledningssystem för verksamhetsinformation Typiska drag för en novell
Typiska drag för en novell Stål för stötfångarsystem
Stål för stötfångarsystem Tack för att ni har lyssnat
Tack för att ni har lyssnat Texter för hinduer tantra
Texter för hinduer tantra Centrum för kunskap och säkerhet
Centrum för kunskap och säkerhet Läkarutlåtande för livränta
Läkarutlåtande för livränta Påbyggnader för flakfordon
Påbyggnader för flakfordon Inköpsprocessen steg för steg
Inköpsprocessen steg för steg Sura för anatom
Sura för anatom Egg för emanuel
Egg för emanuel Standardavvikelse
Standardavvikelse Rutin för avvikelsehantering
Rutin för avvikelsehantering Treserva lathund
Treserva lathund Myndigheten för delaktighet
Myndigheten för delaktighet Presentera för publik crossboss
Presentera för publik crossboss Tack för att ni lyssnade
Tack för att ni lyssnade Debattinlägg mall
Debattinlägg mall Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Tack för att ni har lyssnat
Tack för att ni har lyssnat Hur ser ett referat ut
Hur ser ett referat ut Karttecken
Karttecken Vad är vanlig celldelning
Vad är vanlig celldelning Byggprocessen steg för steg
Byggprocessen steg för steg Rbk-mätning
Rbk-mätning Formel för lufttryck
Formel för lufttryck Var 1721 för stormaktssverige
Var 1721 för stormaktssverige Vad är densitet
Vad är densitet Elektronik för barn
Elektronik för barn Tack för att ni har lyssnat
Tack för att ni har lyssnat Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Mjälthilus
Mjälthilus Trög för kemist
Trög för kemist Delegerande ledarskap
Delegerande ledarskap Större och mindre tecken
Större och mindre tecken Kassaregister ideell förening
Kassaregister ideell förening Blomman för dagen drog
Blomman för dagen drog Returpilarna
Returpilarna