Infectious Disease Emergencies Carol Sulis MD Associate Professor










- Slides: 38
Infectious Disease Emergencies Carol Sulis, MD Associate Professor of Medicine Boston University School of Medicine Hospital Epidemiologist, Boston Medical Center Emergency Lecture Series Boston Medical Center, Boston, MA 7/5/13
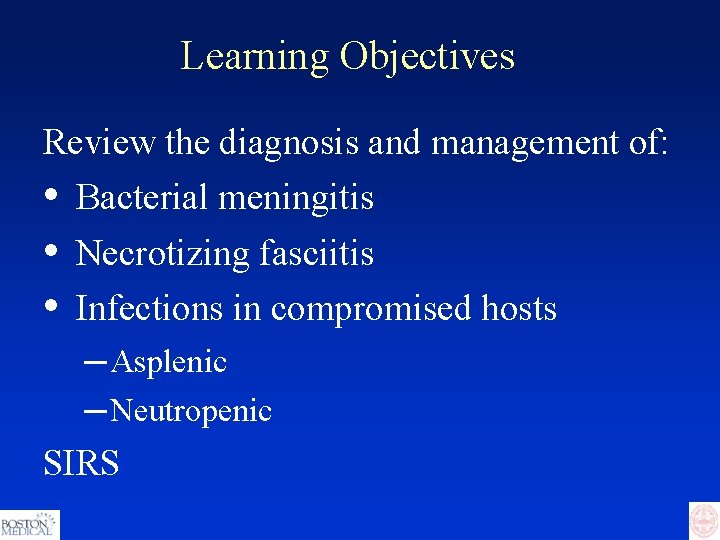
Learning Objectives Review the diagnosis and management of: • • • Bacterial meningitis Necrotizing fasciitis Infections in compromised hosts ─ Asplenic ─ Neutropenic SIRS
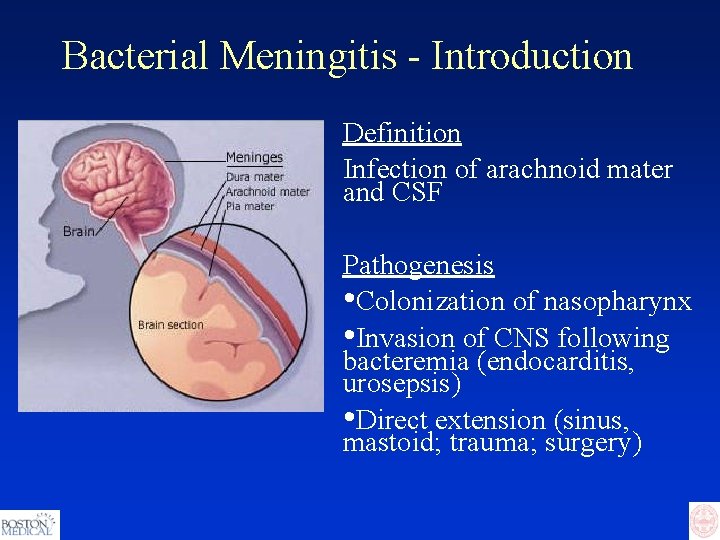
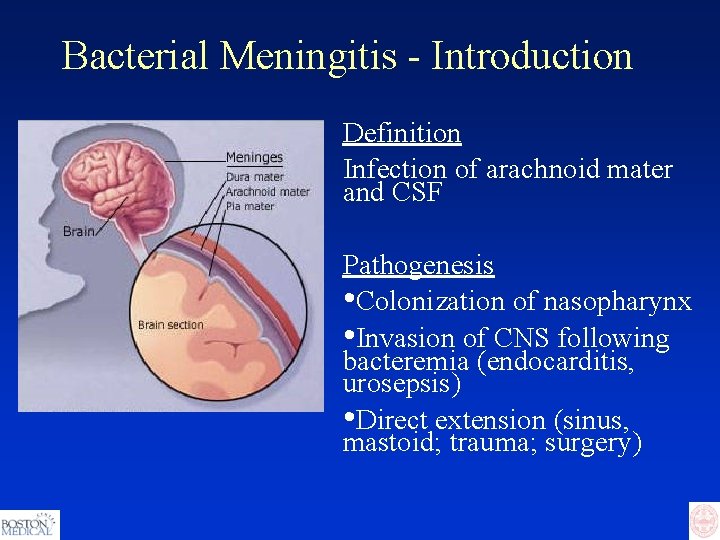
Bacterial Meningitis - Introduction Definition Infection of arachnoid mater and CSF Pathogenesis • Colonization of nasopharynx • Invasion of CNS following bacteremia (endocarditis, urosepsis) • Direct extension (sinus, mastoid; trauma; surgery)
Bacterial Meningitis - Epidemiology Common causes in adults: • • • Streptococcus pneumoniae – 60% Neisseria meningitidis – 20% Hemophilus influenzae type B – 10% Listeria monocytogenes (<1, >50) – 6% Group B streptococcus – 4%
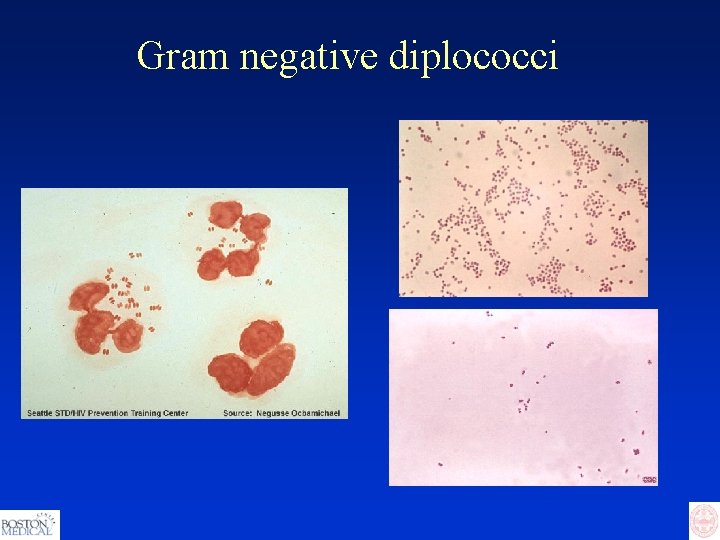
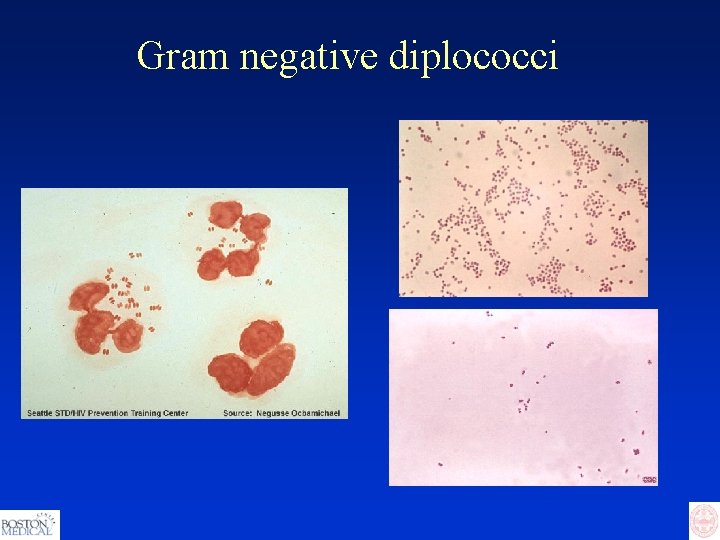
Gram negative diplococci
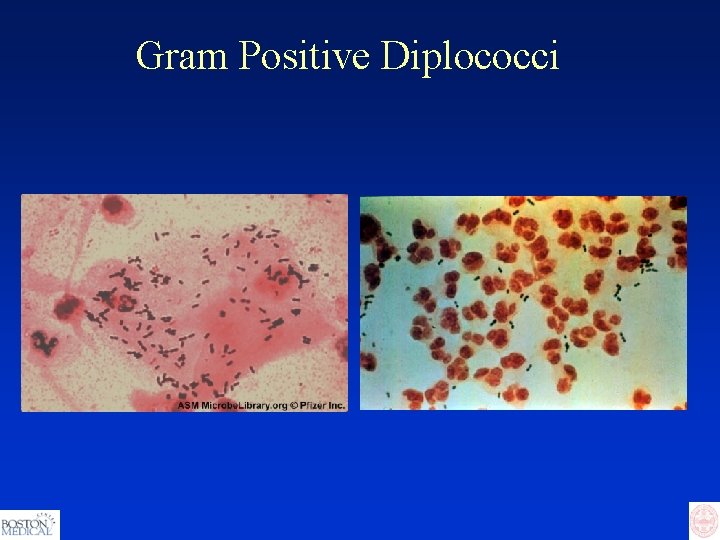
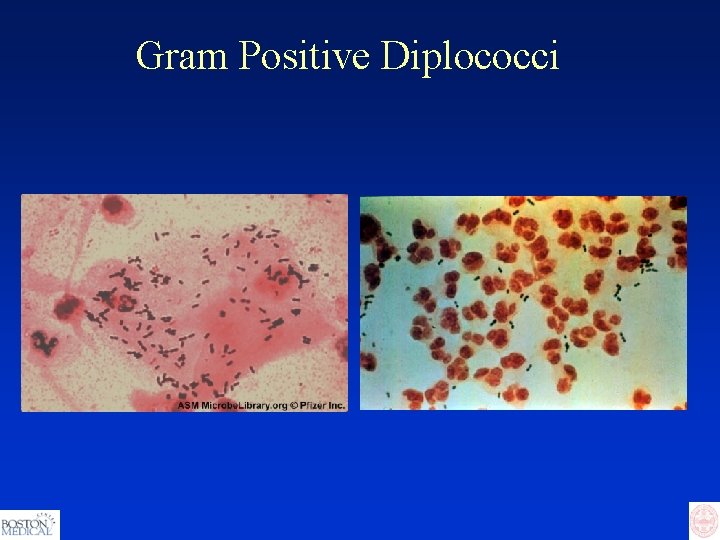
Gram Positive Diplococci
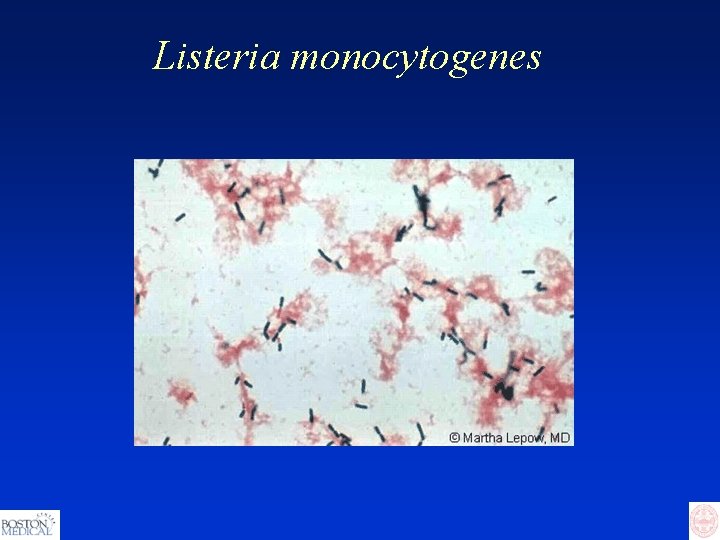
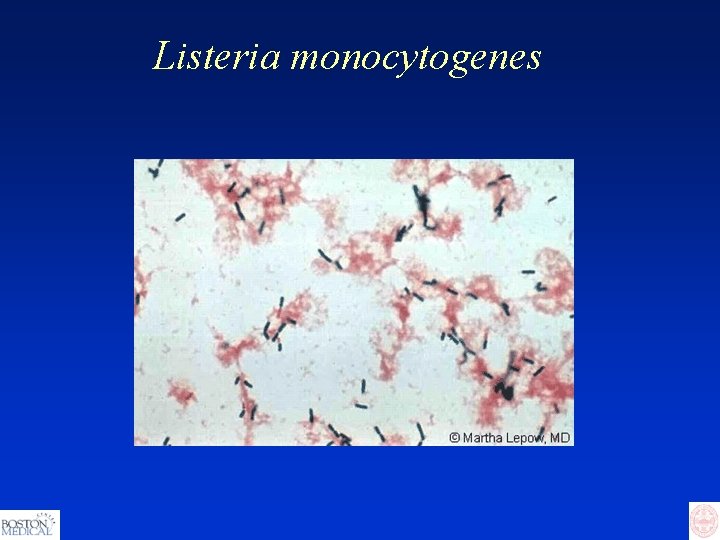
Listeria monocytogenes
Bacterial Meningitis – Clues from History Recent URI Otorrhea/rhinorrhea Petechial rash Recent travel to endemic area Exposure to meningitis case Recent head trauma IVDU HIV Other immunocompromising condition
Bacterial Meningitis - Clinical Classic triad: • Fever +/- headache • Nuchal rigidity • Change in mental status ─ Confusion/lethargy 75% ─ Obtunded 25% • Complications: ─ Focal neuro deficits including CN palsy (1/3) ─ Seizure (1/3) ─ Papilledema
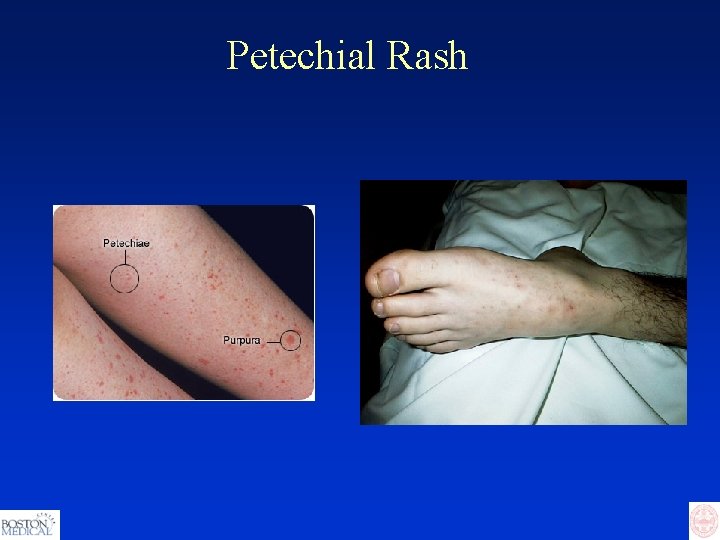
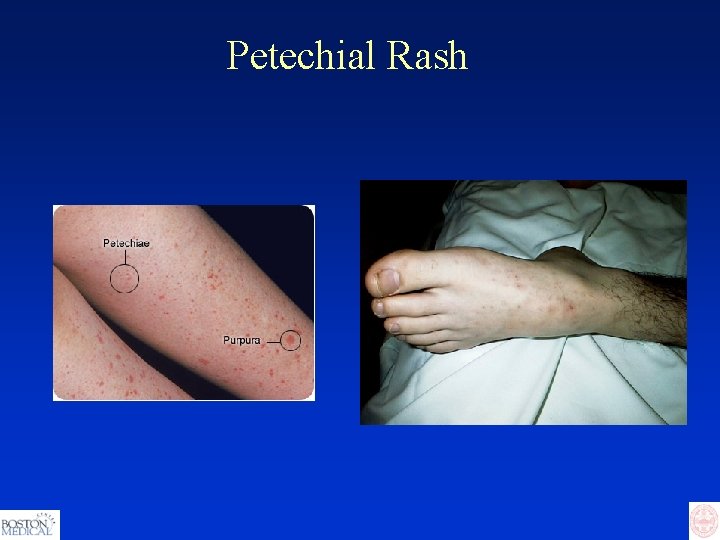
Petechial Rash

Petechiae and Purpura
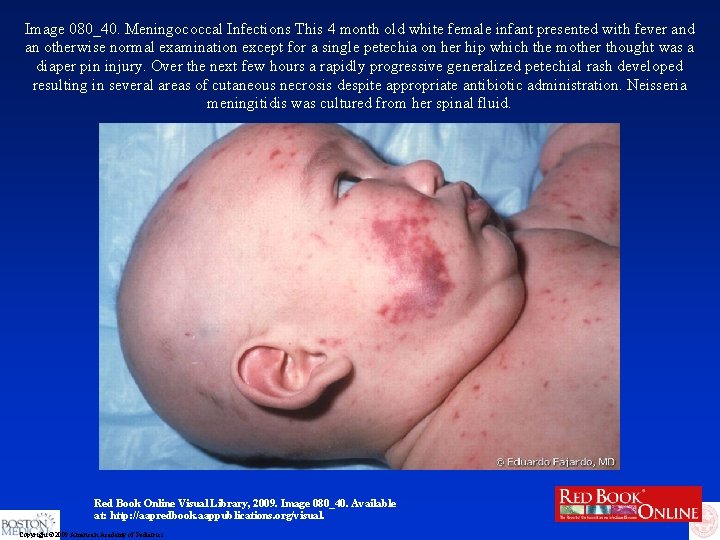
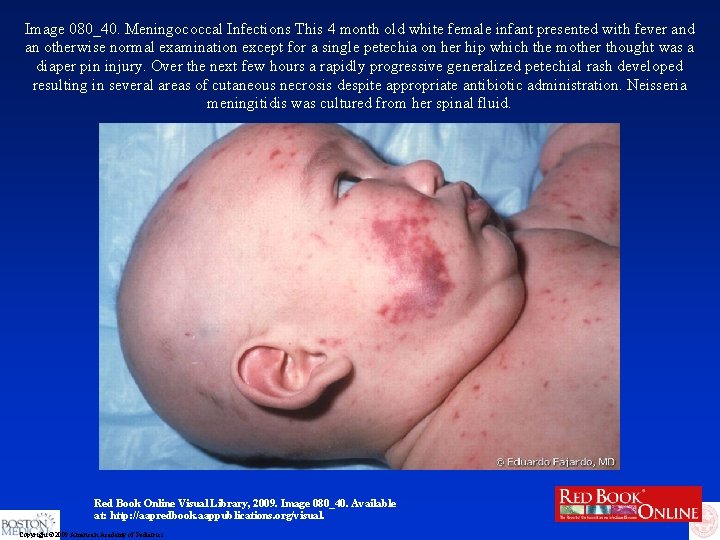
Image 080_40. Meningococcal Infections This 4 month old white female infant presented with fever and an otherwise normal examination except for a single petechia on her hip which the mother thought was a diaper pin injury. Over the next few hours a rapidly progressive generalized petechial rash developed resulting in several areas of cutaneous necrosis despite appropriate antibiotic administration. Neisseria meningitidis was cultured from her spinal fluid. Red Book Online Visual Library, 2009. Image 080_40. Available at: http: //aapredbook. aappublications. org/visual. Copyright © 2009 American Academy of Pediatrics

Purpura fulminans
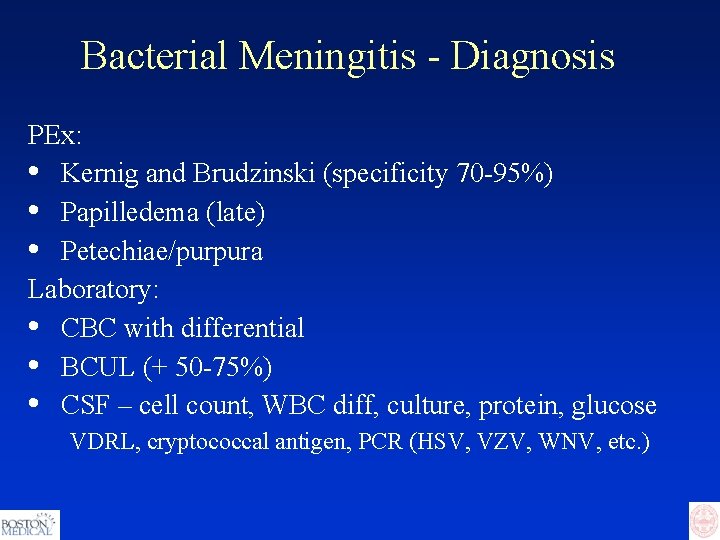
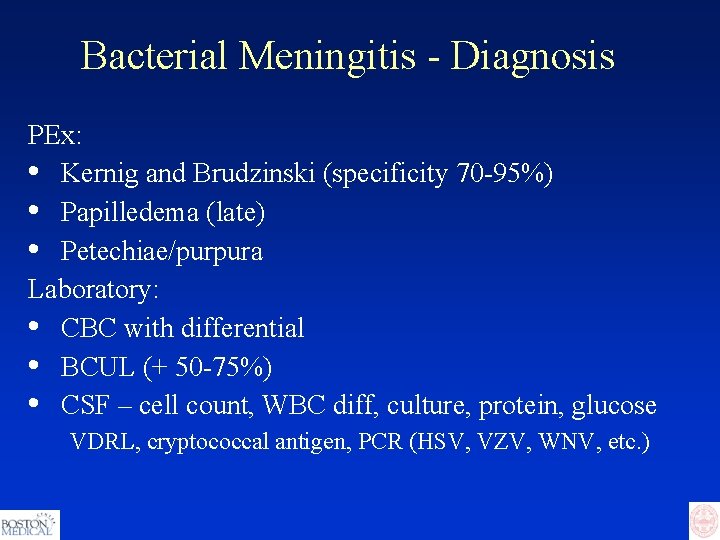
Bacterial Meningitis - Diagnosis PEx: • Kernig and Brudzinski (specificity 70 -95%) • Papilledema (late) • Petechiae/purpura Laboratory: • CBC with differential • BCUL (+ 50 -75%) • CSF – cell count, WBC diff, culture, protein, glucose VDRL, cryptococcal antigen, PCR (HSV, VZV, WNV, etc. )
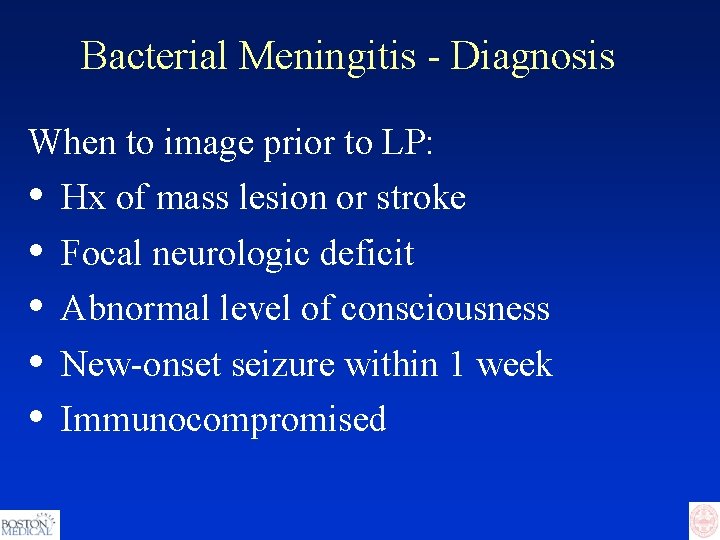
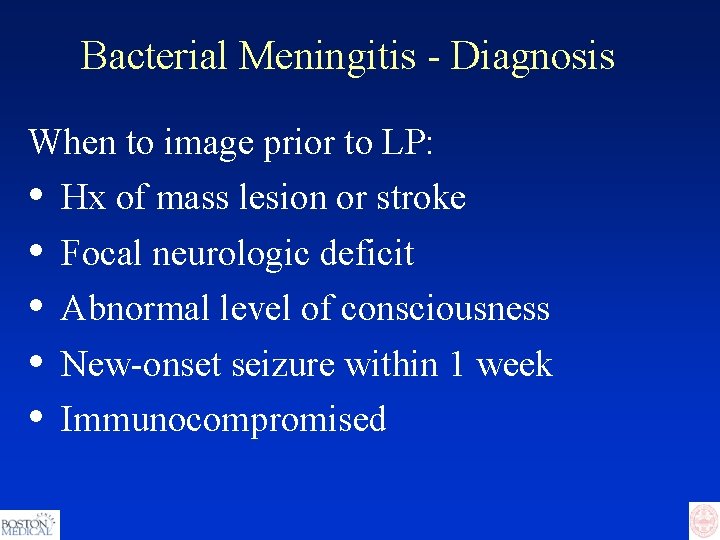
Bacterial Meningitis - Diagnosis When to image prior to LP: • • • Hx of mass lesion or stroke Focal neurologic deficit Abnormal level of consciousness New-onset seizure within 1 week Immunocompromised
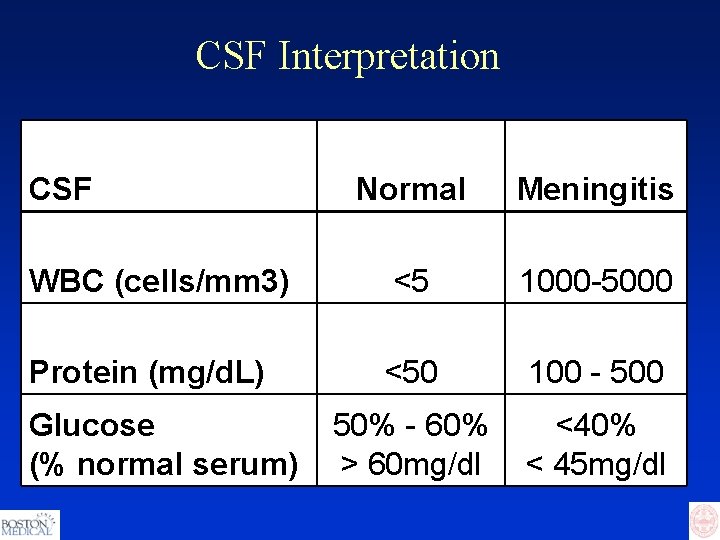
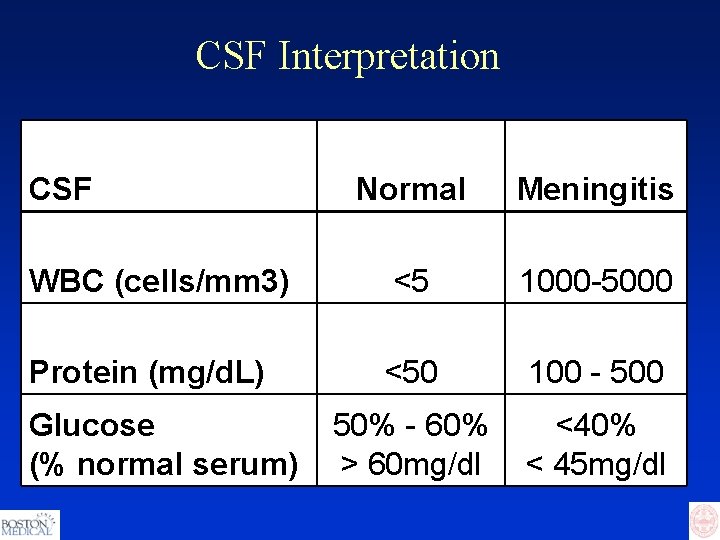
CSF Interpretation CSF Normal Meningitis WBC (cells/mm 3) <5 1000 -5000 Protein (mg/d. L) <50 100 - 500 50% - 60% > 60 mg/dl <40% < 45 mg/dl Glucose (% normal serum)
Bacterial Meningitis - Treatment Ceftriaxone + vancomycin +/- ampicillin Chloramphenicol if allergic Decadron Droplet precautions
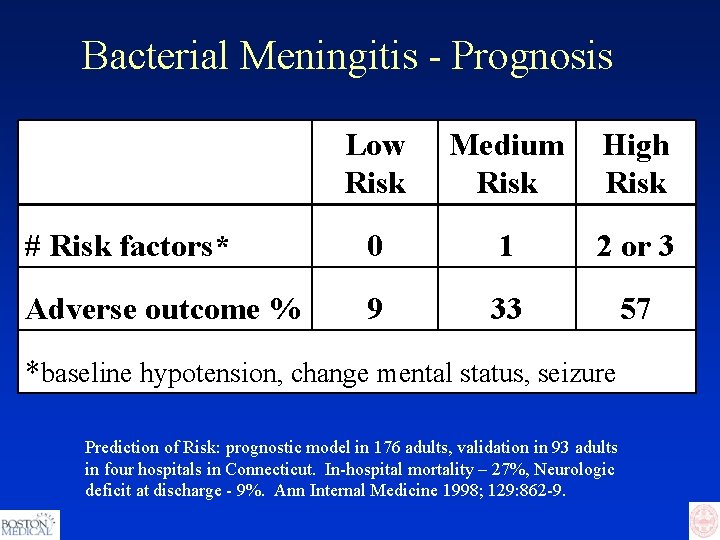
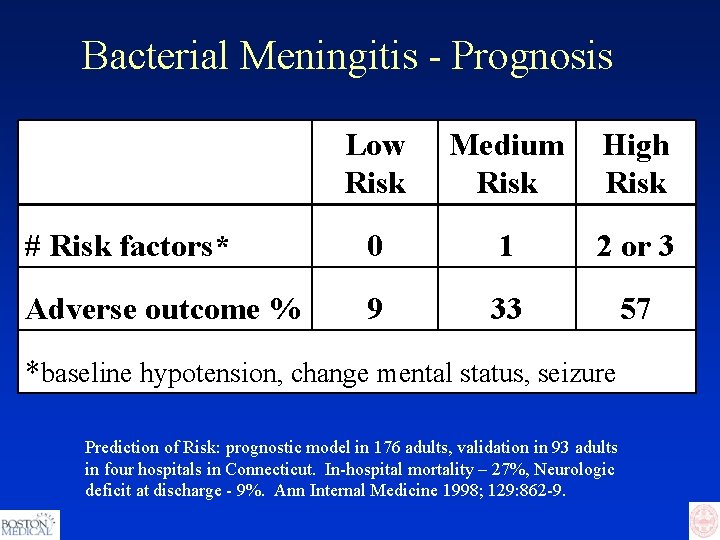
Bacterial Meningitis - Prognosis Low Risk Medium Risk High Risk # Risk factors* 0 1 2 or 3 Adverse outcome % 9 33 57 *baseline hypotension, change mental status, seizure Prediction of Risk: prognostic model in 176 adults, validation in 93 adults in four hospitals in Connecticut. In-hospital mortality – 27%, Neurologic deficit at discharge - 9%. Ann Internal Medicine 1998; 129: 862 -9.
Bacterial Meningitis - Prevention Vaccines Chemoprophylaxis
Necrotizing Fasciitis Introduction • Fulminant tissue destruction • Thrombosis • Bacterial spread along fascial planes • Sparse inflammatory cell infiltrate • Systemic toxicity • High mortality
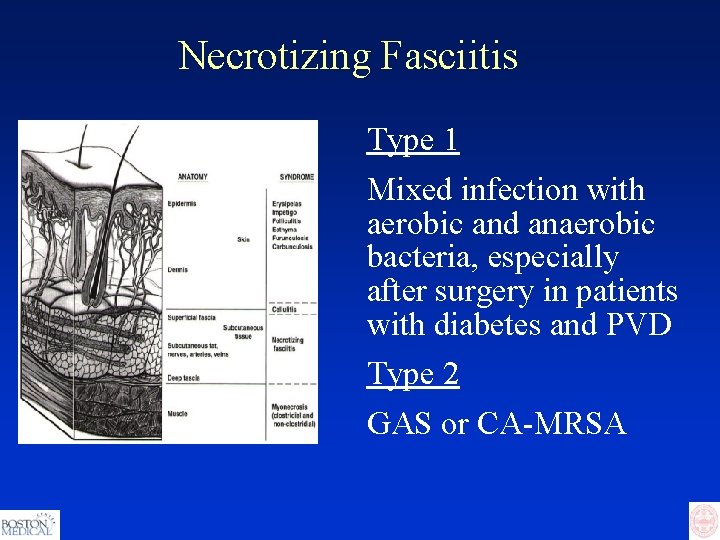
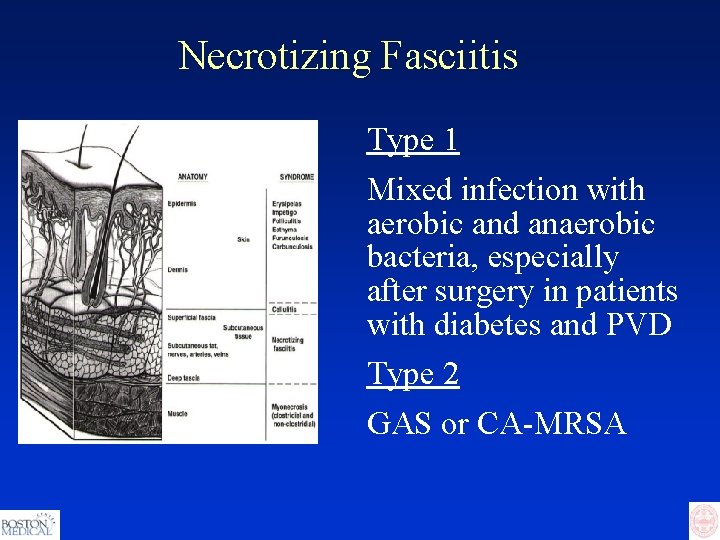
Necrotizing Fasciitis Type 1 Mixed infection with aerobic and anaerobic bacteria, especially after surgery in patients with diabetes and PVD Type 2 GAS or CA-MRSA
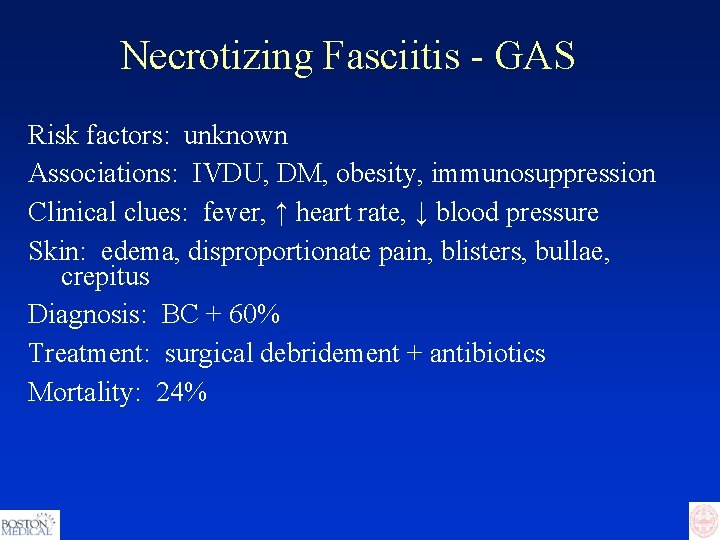
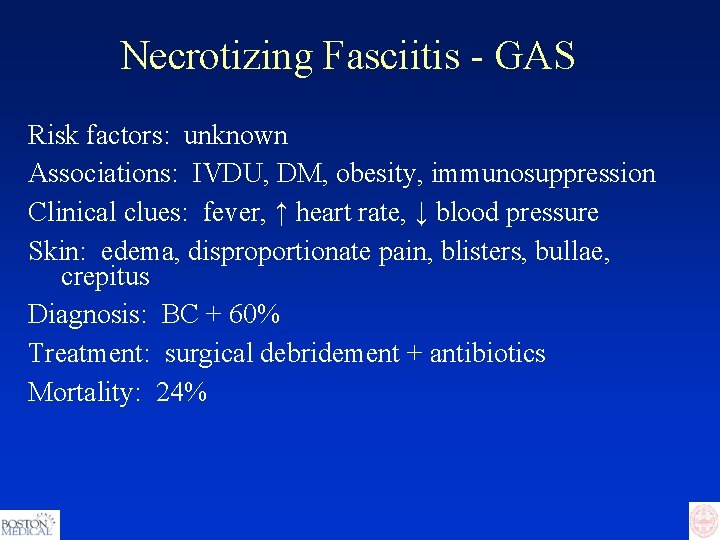
Necrotizing Fasciitis - GAS Risk factors: unknown Associations: IVDU, DM, obesity, immunosuppression Clinical clues: fever, ↑ heart rate, ↓ blood pressure Skin: edema, disproportionate pain, blisters, bullae, crepitus Diagnosis: BC + 60% Treatment: surgical debridement + antibiotics Mortality: 24%

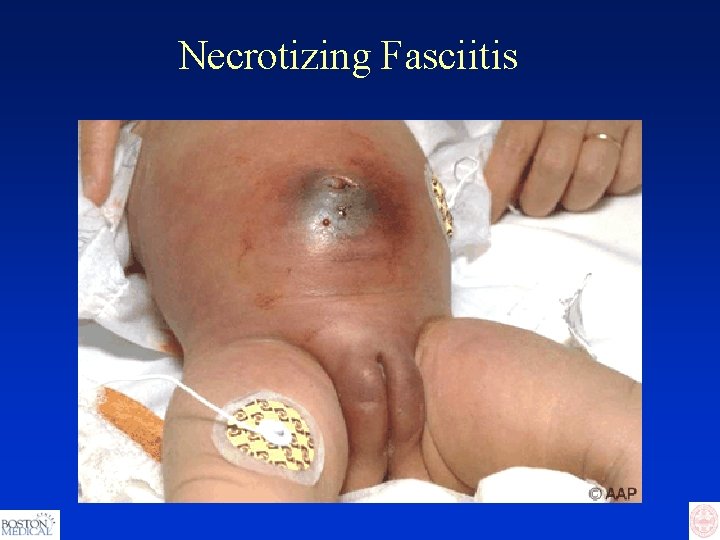
Image 151_22. Varicella-Zoster Infections Varicella complicated by necrotizing fasciitis. A blood culture was positive for group A streptococcus. The disease responded to antibiotics and surgical debridement followed by primary surgical closure. Red Book Online Visual Library, 2009. Image 151_22. Available at: http: //aapredbook. aappublications. org/visual. Copyright © 2009 American Academy of Pediatrics
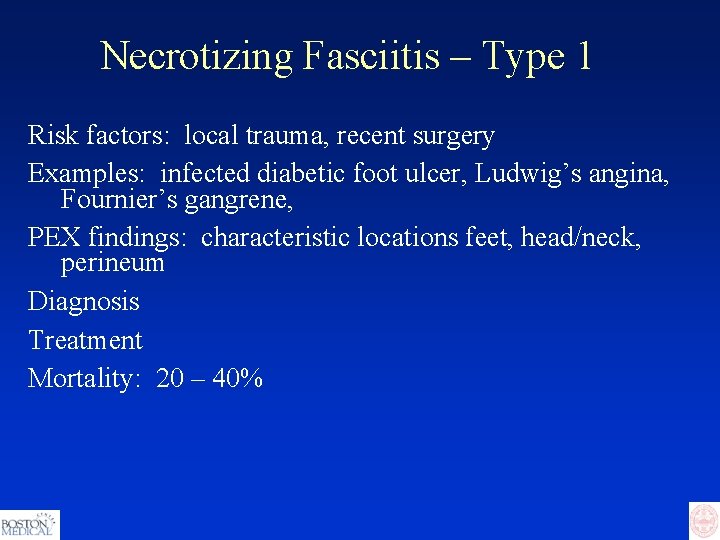
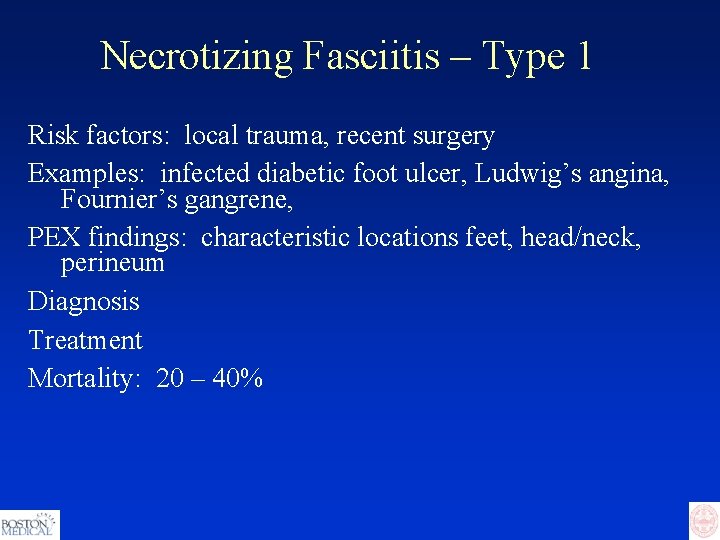
Necrotizing Fasciitis – Type 1 Risk factors: local trauma, recent surgery Examples: infected diabetic foot ulcer, Ludwig’s angina, Fournier’s gangrene, PEX findings: characteristic locations feet, head/neck, perineum Diagnosis Treatment Mortality: 20 – 40%
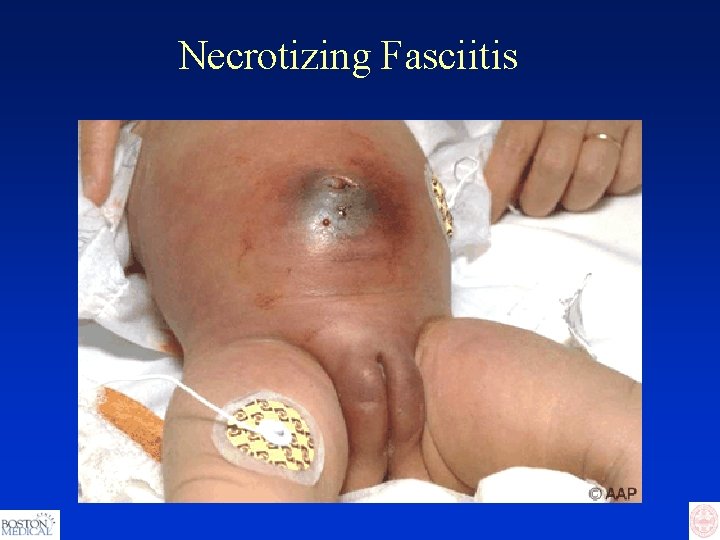
Necrotizing Fasciitis
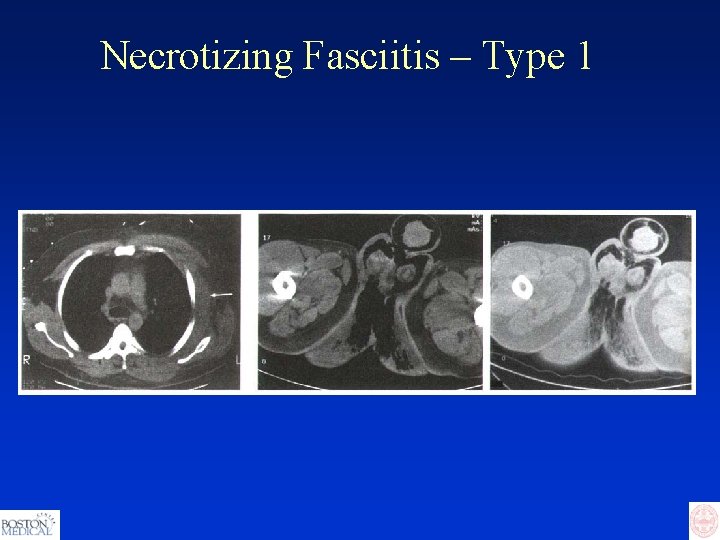
Necrotizing Fasciitis – Type 1

Necrotizing Fasciitis – Type 1
Cases from BMC


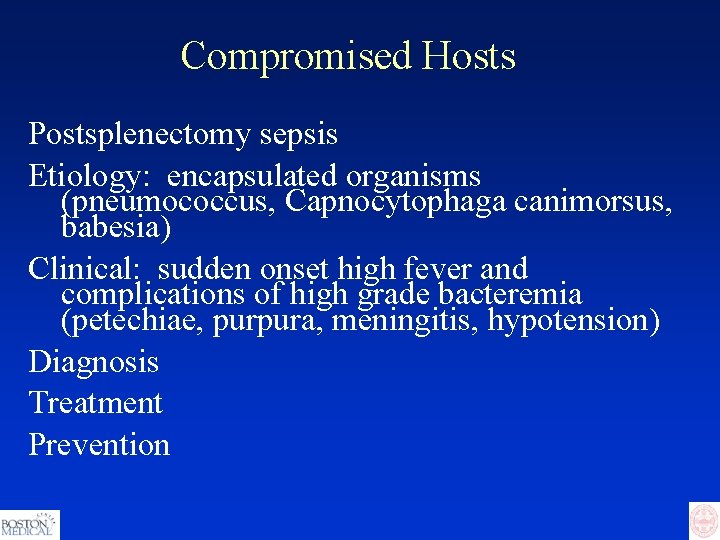
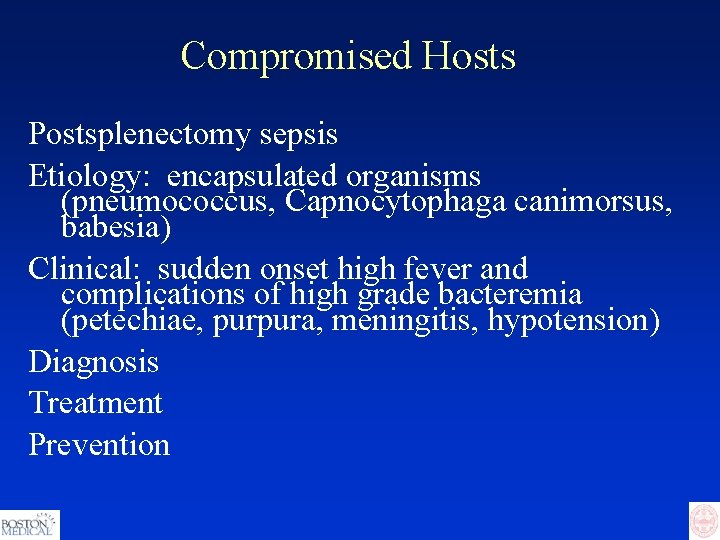
Compromised Hosts Postsplenectomy sepsis Etiology: encapsulated organisms (pneumococcus, Capnocytophaga canimorsus, babesia) Clinical: sudden onset high fever and complications of high grade bacteremia (petechiae, purpura, meningitis, hypotension) Diagnosis Treatment Prevention
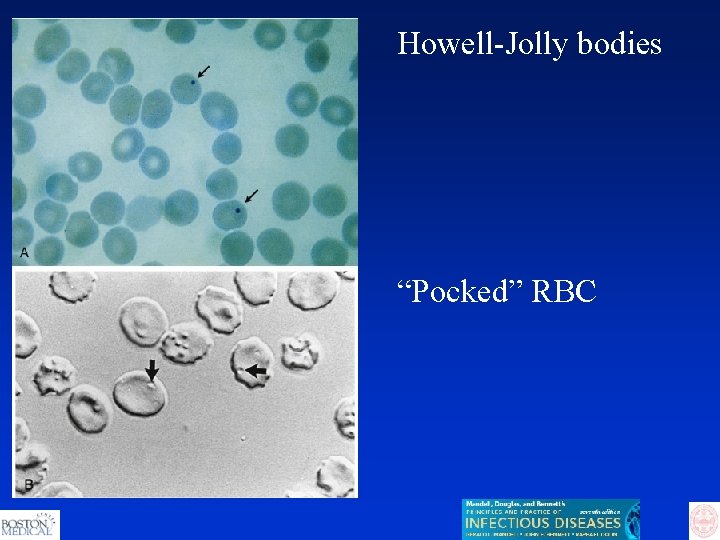
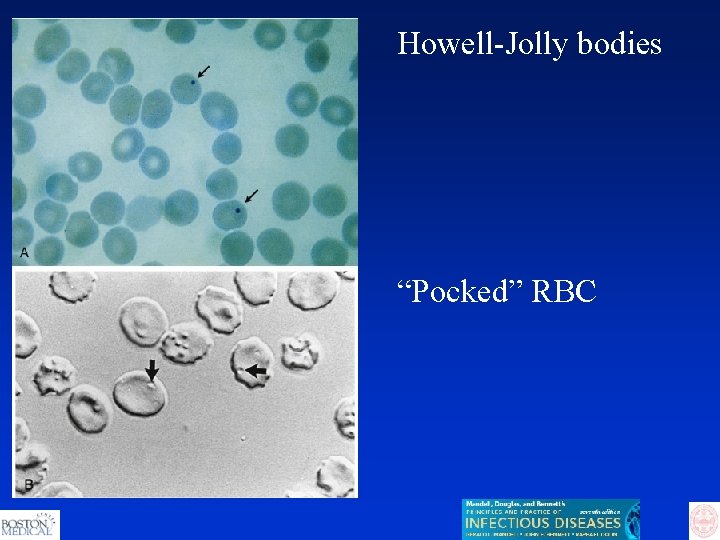
Howell-Jolly bodies “Pocked” RBC


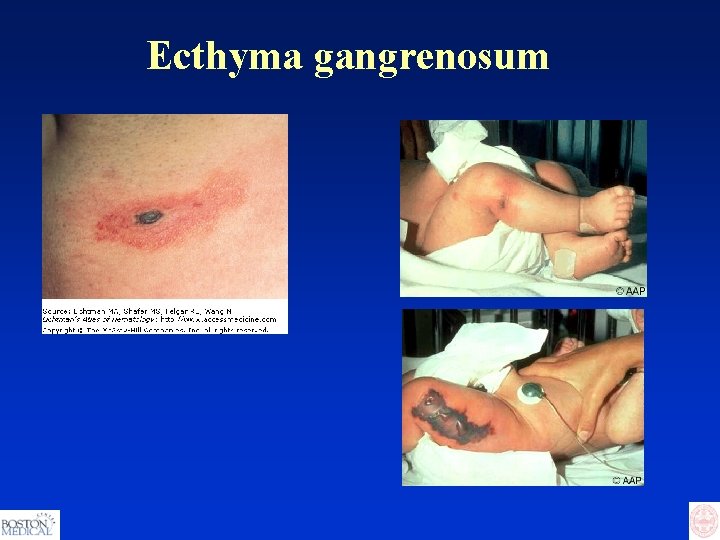
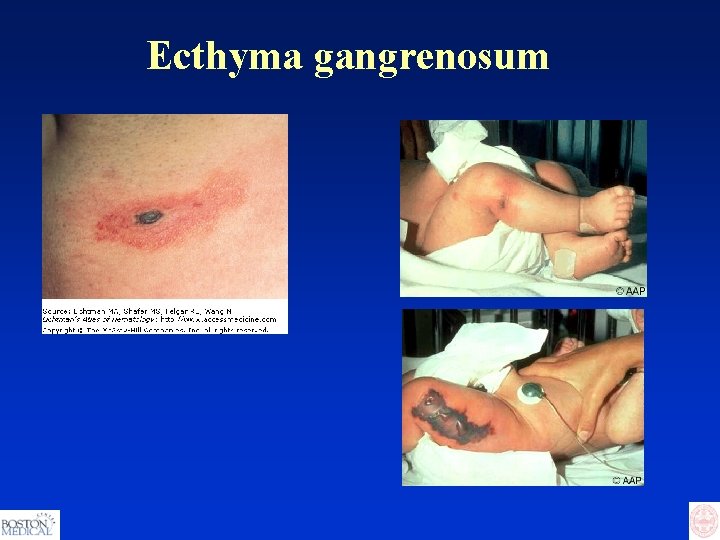
Ecthyma gangrenosum

Clostridium difficile
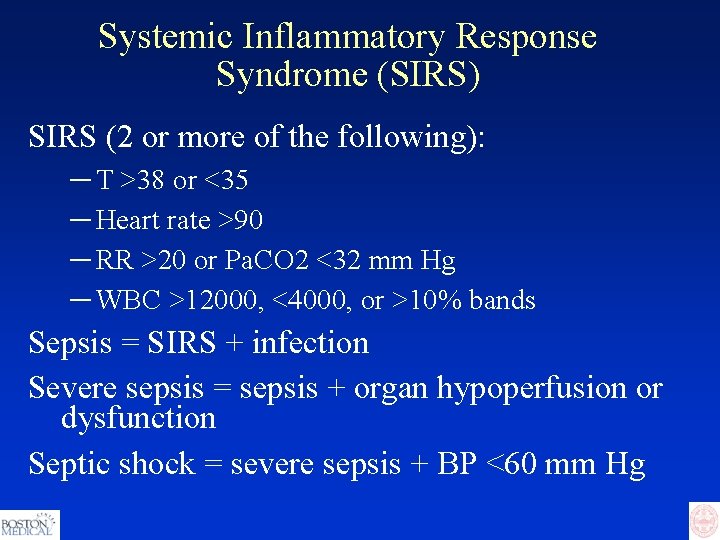
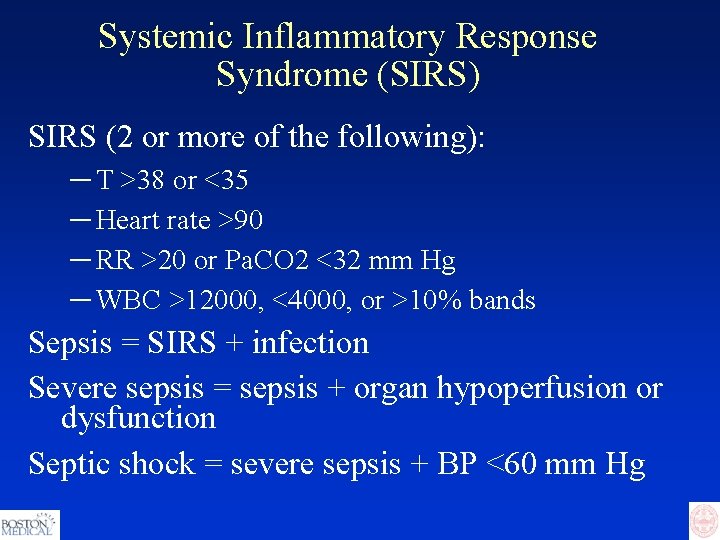
Systemic Inflammatory Response Syndrome (SIRS) SIRS (2 or more of the following): ─ T >38 or <35 ─ Heart rate >90 ─ RR >20 or Pa. CO 2 <32 mm Hg ─ WBC >12000, <4000, or >10% bands Sepsis = SIRS + infection Severe sepsis = sepsis + organ hypoperfusion or dysfunction Septic shock = severe sepsis + BP <60 mm Hg

 Promotion from assistant to associate professor
Promotion from assistant to associate professor Iis alghero
Iis alghero Stridor
Stridor Stages of infection
Stages of infection Infectious disease
Infectious disease Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control Hennepin county infectious disease manual
Hennepin county infectious disease manual Stages of infectious disease
Stages of infectious disease Viruses are the smallest infectious agents
Viruses are the smallest infectious agents Infectious disease quality controls
Infectious disease quality controls Underpinning theory
Underpinning theory Professor carol dweck
Professor carol dweck Communicable disease and non communicable disease
Communicable disease and non communicable disease Mebosha
Mebosha Blood smear
Blood smear Quizlet
Quizlet Icd 10 morbus hansen
Icd 10 morbus hansen Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Ebv
Ebv Infectious stunting syndrome
Infectious stunting syndrome Papillomitosis
Papillomitosis Epidemiological triad of malaria
Epidemiological triad of malaria Infectious nucleic acid
Infectious nucleic acid Hpps symbols
Hpps symbols Psychiatric emergencies
Psychiatric emergencies Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Chapter 12 behavioral emergencies
Chapter 12 behavioral emergencies Chapter 23 gynecologic emergencies
Chapter 23 gynecologic emergencies Chapter 18 neurologic emergencies
Chapter 18 neurologic emergencies Qut security emergency extension number
Qut security emergency extension number Oncological emergencies wikipedia
Oncological emergencies wikipedia Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Chapter 32 environmental emergencies
Chapter 32 environmental emergencies Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Immunologic emergencies
Immunologic emergencies Gems diamond geriatric
Gems diamond geriatric During a psychiatric emergency the emt should be able to
During a psychiatric emergency the emt should be able to Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed