Infant Feeding Zero to Six Konnichiwa Suddenly youre





- Slides: 41
Infant Feeding Zero to Six
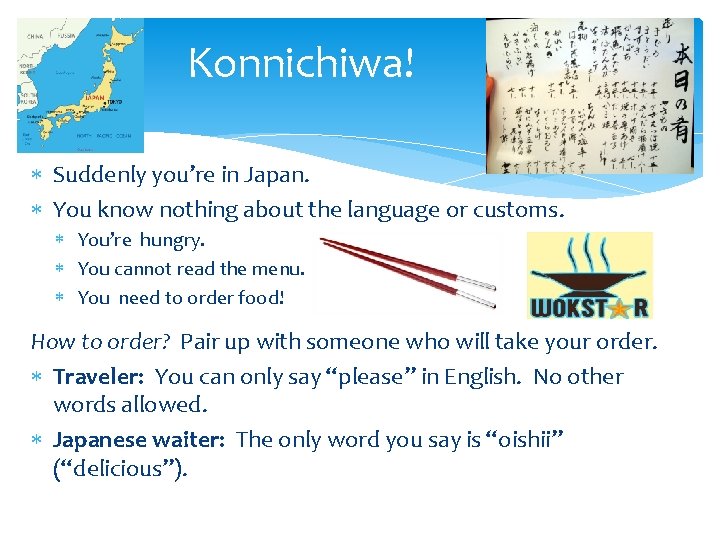
Konnichiwa! Suddenly you’re in Japan. You know nothing about the language or customs. You’re hungry. You cannot read the menu. You need to order food! How to order? Pair up with someone who will take your order. Traveler: You can only say “please” in English. No other words allowed. Japanese waiter: The only word you say is “oishii” (“delicious”).
Konnichiwa! You have 1 minute to order. When the facilitator calls time, the traveler tells the group what you were trying to order. Your Japanese waiter will tell the group what they would have brought based on your efforts to communicate. Ready, set, go…
Konnichiwa! Reflect: How difficult is it to express your thoughts without words? How frustrated did you feel when your partner didn’t understand? How relieved were you when your partner grasped what you wanted to say?

Konnichiwa! Conceptualize: What do babies try to communicate to us? How do parents recognize the cues or hints they’re being given? What are baby’s needs? How do appropriate responses support healthy growth and feeding skills?
Infant Feeding Zero to Six months Until the day of birth, mom’s body provides everything baby needs to grow and develop. Then mom’s attention and decisions are required to meet baby’s needs. AND also baby’s cooperation! How can WIC help?
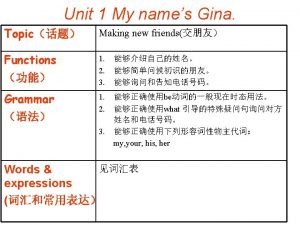
Today we’ll cover… 1. What do parents and caregivers need to know about… • • infant nutritional needs? infant developmental changes? 2. How do we assess and provide support for clients on the day of the WIC appointment? 3. How do we offer messages?
Objectives for Today 1. 2. 3. 4. Review evidence-based recommendations for infant growth and feeding Discuss how to recognize the needs and cues of infants based on their age, growth, and behaviors. Discuss how to connect recommendations with baby’s needs and behaviors Practice sharing messages with mom to address her concerns and baby’s needs
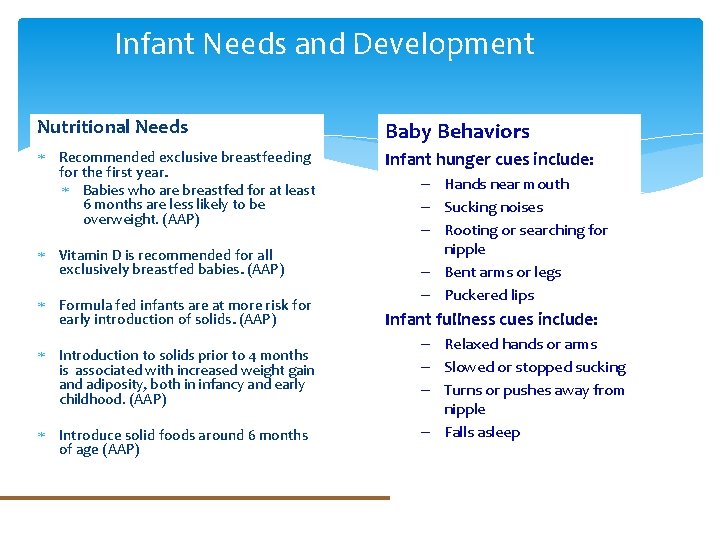
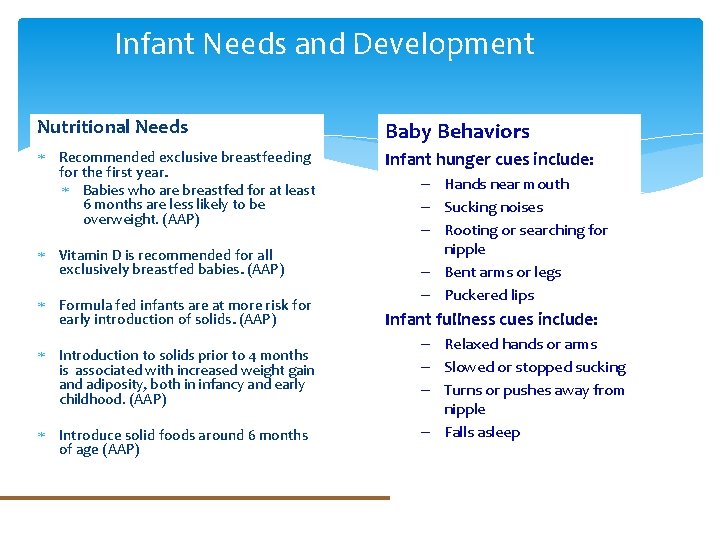
Infant Needs and Development Nutritional Needs Baby Behaviors Recommended exclusive breastfeeding for the first year. Babies who are breastfed for at least 6 months are less likely to be overweight. (AAP) Infant hunger cues include: Vitamin D is recommended for all exclusively breastfed babies. (AAP) Formula fed infants are at more risk for early introduction of solids. (AAP) Introduction to solids prior to 4 months is associated with increased weight gain and adiposity, both in infancy and early childhood. (AAP) Introduce solid foods around 6 months of age (AAP) – Hands near mouth – Sucking noises – Rooting or searching for nipple – Bent arms or legs – Puckered lips Infant fullness cues include: – Relaxed hands or arms – Slowed or stopped sucking – Turns or pushes away from nipple – Falls asleep
Infant Needs and Development The World Health Organization (WHO) recommends that infants start receiving complementary foods in addition to breast milk around six months of age. However, an infant’s age alone does not always determine readiness. Signs of readiness for solids include _____ (What are six signs of readiness? ) 1. 2. 3. 4. 5. 6.

Infant Needs and Development However, an infant’s age alone does not always determine readiness. Signs of readiness for solids include: 1. 2. 3. 4. 5. 6. Sitting up with support Holding head steady Putting fingers or toys in mouth Showing desire for food by opening mouth Turning head away when finished eating Keeping food in mouth and swallowing (also known as loss of the early tongue thrust reflex)
Infant Needs and Development A large CDC study of 1334 mothers tracked how early solids were started for infants. Over 50% of mothers who offered formula or a combination of breast milk and formula started solid foods before 4 months of age. 1. Based on this information, when do you feel it would be helpful to offer anticipatory guidance about starting solid foods? 2. What could you share to help parents assess whether their own baby was ready or not?

WIC Codes We know some feeding practices can increase risks to baby’s health. The Nutrition Risk Manual identifies evidence-based feeding risks for infants. These WIC Codes start with 411 and are followed with a decimal to indicate the specific risk. (411. 1, 411. 2, …)
WIC Codes – Feeding concerns Let’s take a look at some of the most commonly observed WIC Codes among infants. 1. For each code consider how to identify these behaviors among the clients you see. 2. After reviewing these codes we’ll look at some scenarios for practice.
WIC Codes – Feeding concerns 411. 3 Routinely offering complementary foods* or other substances that are inappropriate in type or timing. *Complementary foods are any foods or beverages other than human milk or infant formula. Examples of inappropriate complementary foods: - Adding sweet agents such as sugar, honey, or syrups to any beverage (including water) or prepared food, or used on a pacifier; and - Introducing any food other than human milk or iron-fortified infant formula before 4 months of age.
WIC Codes – Feeding concerns 411. 4 Routinely using feeding practices that disregard the developmental needs or stage of the infant. (411. 4 Example 1 of 4) • Inability to recognize, insensitivity to, or disregarding the infant’s cues for hunger and satiety (e. g. , forcing an infant to eat a certain type and/or amount of food or beverage or ignoring an infant’s hunger cues). What is an example of behavior that would fall under this description of 411. 4?
WIC Codes – Feeding concerns 411. 4 Routinely using feeding practices that disregard the developmental needs or stage of the infant. (411. 4 Example 2 of 4) • Feeding foods of inappropriate consistency, size, or shape that put infants at risk of choking. What is an example of behavior that would fall under this description of 411. 4?
WIC Codes – Feeding concerns 411. 4 Routinely using feeding practices that disregard the developmental needs or stage of the infant. (411. 4 Example 3 of 4) • Not supporting an infant’s need for growing independence with self-feeding (e. g. , solely spoon-feeding an infant who is able and ready to finger-feed and/or try self-feeding with appropriate utensils). What is an example of behavior that would fall under this description of 411. 4?
WIC Codes – Feeding concerns 411. 4 Routinely using feeding practices that disregard the developmental needs or stage of the infant. (411. 4 Example 4 of 4) • Feeding an infant food with inappropriate textures based on his/her developmental stage (e. g. , feeding primarily pureed or liquid foods when the infant is ready and capable of eating mashed, chopped or appropriate finger foods). What is an example of behavior that would fall under this description of 411. 4?
WIC Codes – Feeding concerns 411. 11 Routinely not providing dietary supplements recognized as essential by national public health policy when an infant’s diet alone cannot meet nutrient requirements. • Infants who are 6 months of age or older who are ingesting less than 0. 25 mg of fluoride daily when the water supply contains less than 0. 3 ppm fluoride. • Infants who are exclusively breastfed, or who are ingesting less than 1 liter (or 1 quart) per day of vitamin D-fortified formula, and are not taking a supplement of 400 IU of vitamin D. What is an example of behavior that would fall under this description of 411. 11?
Feeding Case Studies For the following two case studies, you will be given information about a baby at a WIC appointment. 1. Use what you know to assess the infant’s needs. Consider what mom shares in conversation. 2. Decide how to best respond balancing infant’s needs, mom’s interests and concerns.
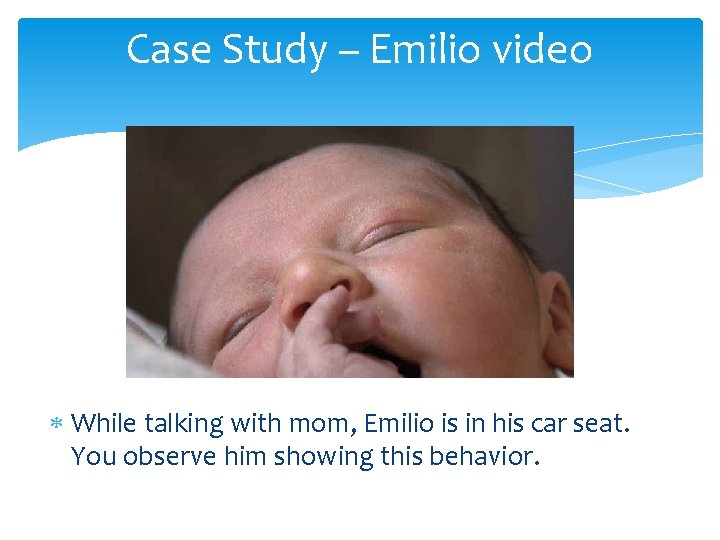
What about this baby? Here is what you see while talking with mom. (play video)
About this baby Baby Emilio is three months old What do you know about an infant’s nutritional needs at this age? What cues or behavior did you see? What do you know about infant sleep at this age?
Case Study - Emilio Mom brings 3 month Emilio for his first WIC appointment. His growth and weight are normal. Mom has been exclusively nursing. Counselor: What does baby do to tell you he’s hungry? Mom: He cries but it’s not always because he’s hungry. Counselor: How often does he nurse?
Case Study - Emilio Mom: He nurses at 7 am, 11 am, 3 pm, and 7 pm. And once during the night until morning. Counselor: What have you heard about how often infants need to eat? Mom: I know they’ll eat all the time if you let them. I can’t handle a baby that keeps crying until you do what they want all day long.
Case Study – Emilio video While talking with mom, Emilio is in his car seat. You observe him showing this behavior.
Case Study - Emilio How should the counselor respond to this mom? Choose a partner to role play as mom. 1. How does Emilio’s behavior show what he needs? 2. Practice discussing the feeding and growth needs for an exclusively nursing infant. 3. Remember to ask permission before offering a message. Check in with mom to see if it will work for her.
Case Study - Debrief Reflect on your discussion with Emilio’s mom: 1. How did you help mom understand Emilio’s cues? What needs could he be communicating? 2. How did you help mom understand the nutritional needs for an infant Emilio’s age? What worked well? What would you do differently next time?
Case Study - Debrief Reflect on your discussion with Emilio’s mom: 1. How did you help mom understand Emilio’s cues? What needs could he be communicating? 2. How did you help mom understand the nutritional needs for an infant Emilio’s age? What worked well? What would you do differently next time?

What about this baby? (What you see while talking with mom. ) **photo only**
Case Study - Eric Baby Eric is breastfed at home and mom bottlefeeds him in public. Mom arrives at a Nutrition Education appointment. You observe mom offer the bottle. Eric begins sucking and stops. Mom keeps moving the bottle across his lips until he takes it again. Again Eric sucks for a few seconds and stops. This happens repeatedly during the appointment.
Case Study - Eric 1. What does Eric’s behavior say about what he needs? 2. How can you bring Eric’s behavior to mom’s attention? 3. What information would you share to help Eric’s mom understand how his response tells her what he needs?
Case Study - Eric Counselor: What have you heard about hunger and fullness cues? Mom: I know they start rooting and sucking their hands when they’re hungry. Eric starts moving his head around on my chest when he wants to eat. And be pulls his head away and just looks around when he’s full.
Case Study - Eric Counselor: That’s good! Eric is lucky to have a mom who’s paying attention to what he needs. Can I share with you something I noticed Eric doing just now? Mom: Sure. Counselor: While we were talking and you gave him the bottle, he kept stopping until you moved it across his lips.
Case Study - Eric Mom: Yeah, I think he gets distracted in public. I have to remind him to keep eating. Counselor: Would it be okay if I offered some information that you might find helpful about bottle feeding? Mom: Okay (nods). Counselor: Sometimes babies show different fullness cues with the bottle than breastfeeding. (next page)
Case Study - Eric Counselor: While nursing babies have to help initiate the latch, the bottle nipple can be put into baby’s mouth even if they don’t want it. When bottle nipple touches their lips it triggers a reflex to open their mouth. If they stop sucking and seem content that’s a good sign of fullness. Mom: Oh I hadn’t thought about that. I usually try to get him to finish the bottle.
Case Study - Eric View this video to see the cues the Counselor observed while Eric was feeding: https: //www. quietyoutube. com/watch? v=1 ALUXZf 8 q 3 o (starts after 0: 10)
Case Study - Eric Counselor: • It sounds like his doctor is happy with his growth and his weight today is tracking perfectly. • Earlier you were telling me he nurses well and you’re pretty happy about how he’s doing. • We talked about how easy it is to keep offering the bottle after baby is content since by reflex they keep taking it. • Is there anything I left out, or that you want to discuss about Eric’s feeding and growth? Mom: No, that’s good.
Case Study - Eric At this point in the conversation, what would you do as the counselor to wrap things up and encourage mom to identify a behavior change that she feels would be helpful? 1. Find a partner. How can you suggest an appropriate next step for mom and close the conversation? Remember to ask permission before offering a message. Check in with mom to see if it will work for her. 2. Take turns playing the role of counselor with mom.
Infant Feeding Zero to Six Take Home Messages ü Babies are born with the skills and desire to tell parents what they need. ü Evidence based recommendations inform us about nutritional needs and key developmental stages for infants. ü Your assessment and skills can connect mom’s concerns and baby’s needs with evidence based education. ü Check in with mom to find out if it will work for her.

 Infant driven feeding readiness scale
Infant driven feeding readiness scale Enteral parenteral beslenme
Enteral parenteral beslenme Draw the core
Draw the core Random compliment generator
Random compliment generator If love is the answer you are wrong
If love is the answer you are wrong What to do when youre angry
What to do when youre angry And the tree was happy but not really
And the tree was happy but not really Youre my king
Youre my king How youre
How youre I hope you are doing well formal
I hope you are doing well formal Cybersmart definition
Cybersmart definition Tentative goal statement
Tentative goal statement Jesus youre my firm foundation
Jesus youre my firm foundation How do you know if you're asexual
How do you know if you're asexual How to write email writing
How to write email writing Zero defect zero effect
Zero defect zero effect Programmazione cnc simulator
Programmazione cnc simulator Zero one two three four five six seven eight nine
Zero one two three four five six seven eight nine Zero un deux trois quatre
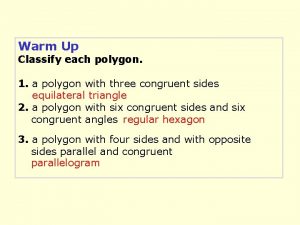
Zero un deux trois quatre Classify each polygon
Classify each polygon Stopped suddenly phrasal verb
Stopped suddenly phrasal verb I love u in swahili
I love u in swahili Literal language.
Literal language. When at rest on the launching pad the force
When at rest on the launching pad the force Athletes suddenly dying
Athletes suddenly dying Why did bruno's family suddenly moved house
Why did bruno's family suddenly moved house Past simple and past continuous form
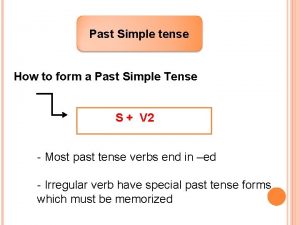
Past simple and past continuous form Fill in the blanks with present perfect continuous tense
Fill in the blanks with present perfect continuous tense Passage to india quiz
Passage to india quiz I was travelling
I was travelling Conservation of impulse
Conservation of impulse Catherine maguire infant mental health
Catherine maguire infant mental health Convent of the holy infant jesus
Convent of the holy infant jesus Baby reflexes chart
Baby reflexes chart Sex specific mortality rate
Sex specific mortality rate Decardron
Decardron Intraosseous meaning
Intraosseous meaning Phoenix infant academy
Phoenix infant academy Infant mortality rate formula
Infant mortality rate formula Denis browne bar
Denis browne bar Chest compression for infant 2 rescuer
Chest compression for infant 2 rescuer Infant industries apush
Infant industries apush