Honchi Yip Department of Surgery North District Hospital
- Slides: 30
Hon-chi Yip Department of Surgery North District Hospital BCT for multifocal multicentric breast cancer Is it contraindicated?
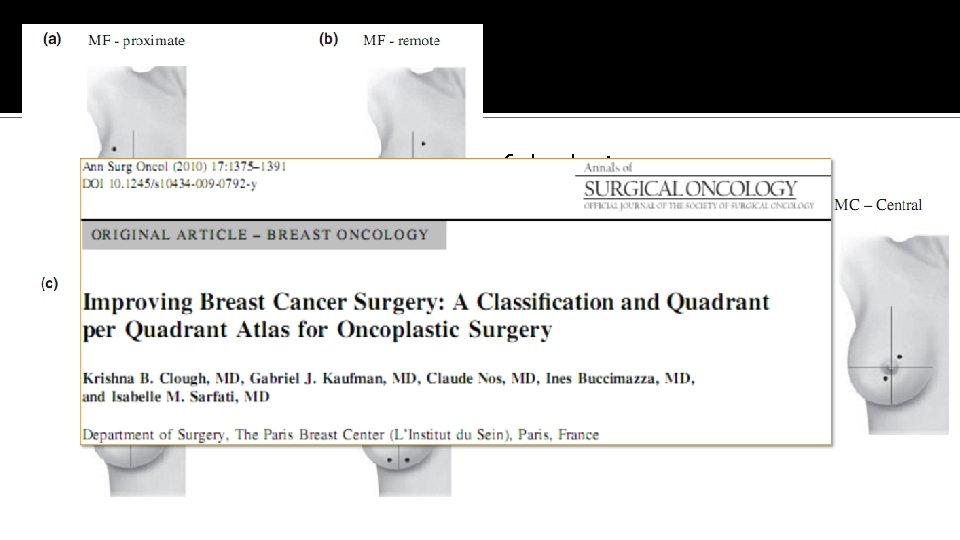
Multifocal / multicentric breast cancer �Definition Multifocal (MF) – multiple tumors in same quadrant (>5 cm apart) Multicentric (MC) – multiple tumors in different quadrants Not based on anatomy of breast �Increasingly detected due to the widespread use of MRI breast
Pathophysiology of multifocality and multicentricity 1. Monoclonal proliferation of a single mammary carcinoma 2. Multiple independent synchronous tumors in the same breast
Breast conservation therapy �Wide local excision + radiotherapy �Established treatment modality for early stage breast cancer No difference in overall, disease-free survival Improved body image and lifestyle score �National Institutes of Health (NIH) Consensus Conference statement 1990 BCT as preferred surgical treatment of women with early stage breast cancer NIH Consensus Conference. JAMA 1991; 265(3): 391 -5
Multifocal / multicentric breast cancer �Traditionally contraindicated for BCT �Landmark trials for BCT – NSABP B-06, EORTC, Milan etc Exclusion criteria – Multifocal or multicentric disease Increased difficulty to obtain negative margin Potential increase risk of recurrence Fisher B et al. N Engl J Med 2002; 347: 1233– 1241. Veronesi U et al. N Engl J Med 2002; 347: 1227– 1232. van Dongen JA et al. J Natl Cancer Inst 2000; 92: 1143– 1150.
Development of oncoplastic surgery (OPS) �Allow wide excision for BCT without compromising the natural shape of the breast �Integration of plastic surgery techniques for immediate breast reshaping �Oncologic efficacy (margin status & recurrence) compare favorably with traditional BCT Results of 298 OPS treated breast cancer ▪ 5 year overall survival 94. 6%, DFS 93. 7% Staub G et al. Ann Chir Plast Esthet. 2007; 53(2): 124– 34. �Recent enthusiasm on BCT in MF / MC disease
Important issues 1. Oncological considerations Effect on overall survival Effect on disease recurrence, esp. locoregional 2. Technical considerations Complete excision, negative margin Satisfactory cosmetic result
Oncological considerations �Lack of level 1 evidence �What are the available evidence in the literature? �Medline and Pub. Med search – keywords: ‘‘Multifocal’’ or ‘‘Multicentric’’ or ‘‘Breast Conservation’’ or ‘‘Mastectomy’’ ‘‘Breast Cancer’’ or ‘‘Ductal Carcinoma In-Situ (DCIS)’’
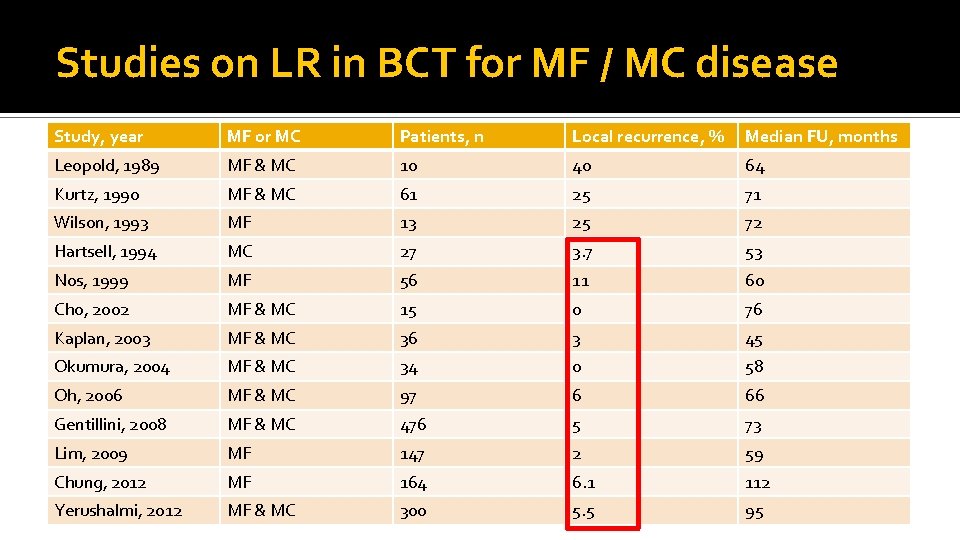
Local recurrence
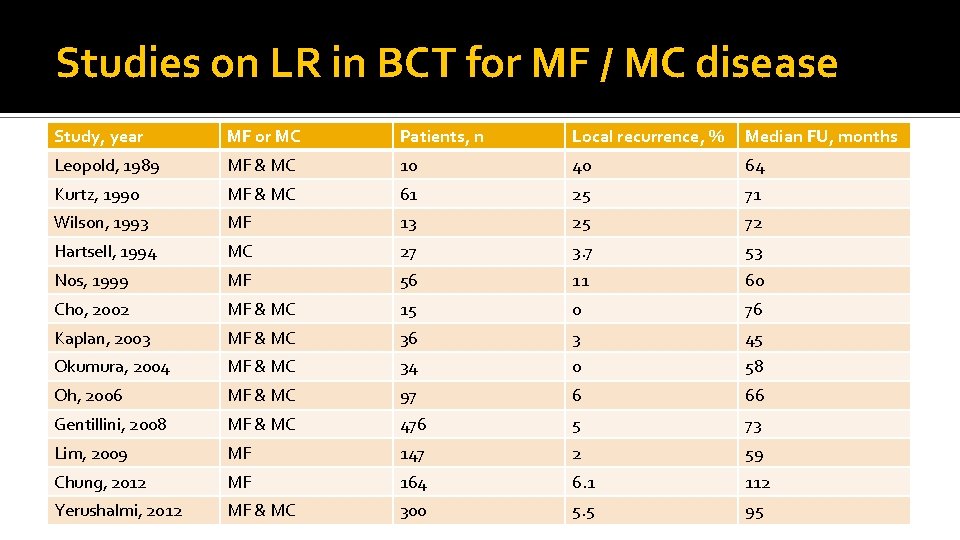
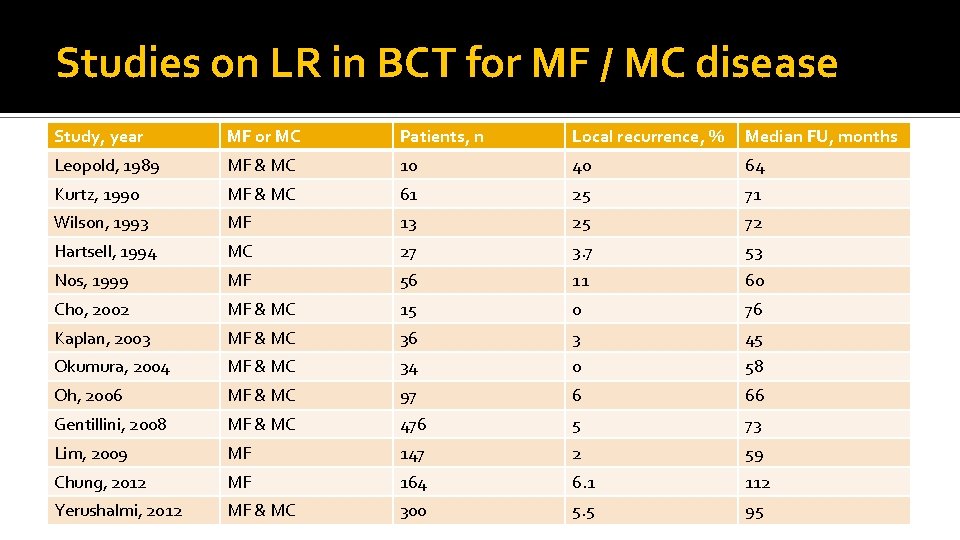
Studies on LR in BCT for MF / MC disease Study, year MF or MC Patients, n Local recurrence, % Median FU, months Leopold, 1989 MF & MC 10 40 64 Kurtz, 1990 MF & MC 61 25 71 Wilson, 1993 MF 13 25 72 Hartsell, 1994 MC 27 3. 7 53 Nos, 1999 MF 56 11 60 Cho, 2002 MF & MC 15 0 76 Kaplan, 2003 MF & MC 36 3 45 Okumura, 2004 MF & MC 34 0 58 Oh, 2006 MF & MC 97 6 66 Gentillini, 2008 MF & MC 476 5 73 Lim, 2009 MF 147 2 59 Chung, 2012 MF 164 6. 1 112 Yerushalmi, 2012 MF & MC 300 5. 5 95
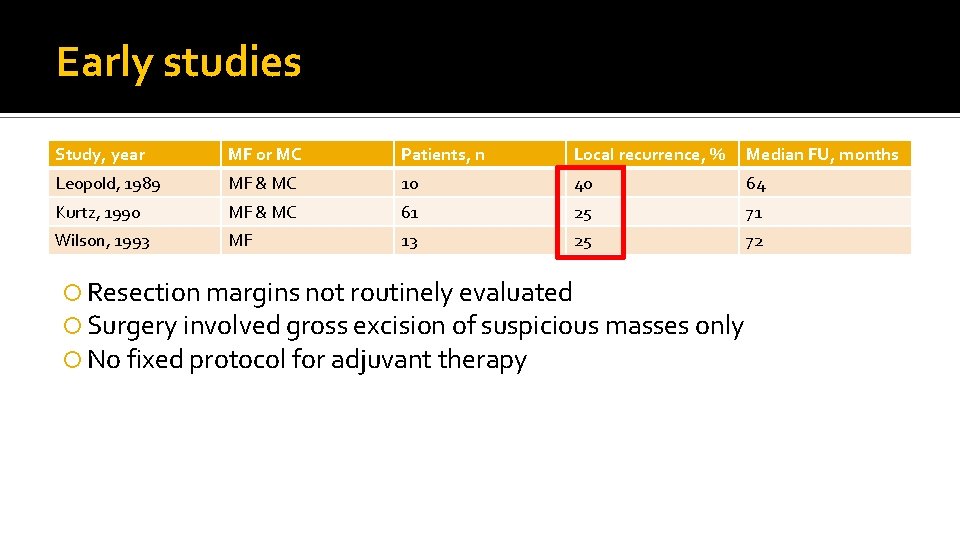
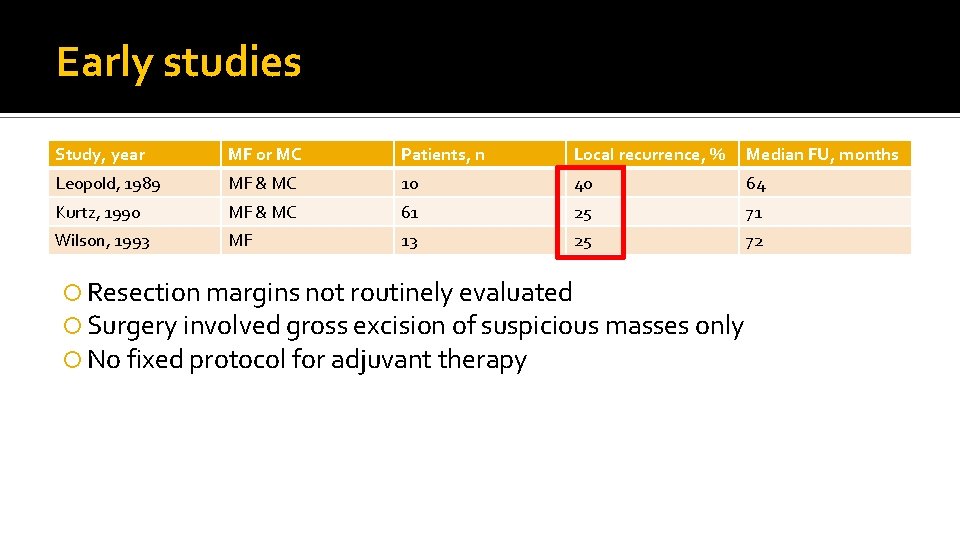
Early studies Study, year MF or MC Patients, n Local recurrence, % Median FU, months Leopold, 1989 MF & MC 10 40 64 Kurtz, 1990 MF & MC 61 25 71 Wilson, 1993 MF 13 25 72 Resection margins not routinely evaluated Surgery involved gross excision of suspicious masses only No fixed protocol for adjuvant therapy
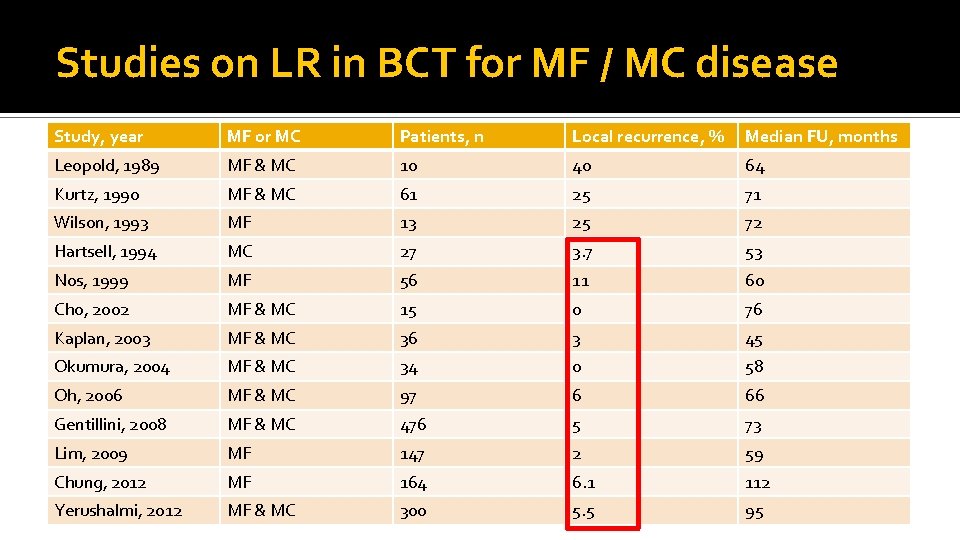
Studies on LR in BCT for MF / MC disease Study, year MF or MC Patients, n Local recurrence, % Median FU, months Leopold, 1989 MF & MC 10 40 64 Kurtz, 1990 MF & MC 61 25 71 Wilson, 1993 MF 13 25 72 Hartsell, 1994 MC 27 3. 7 53 Nos, 1999 MF 56 11 60 Cho, 2002 MF & MC 15 0 76 Kaplan, 2003 MF & MC 36 3 45 Okumura, 2004 MF & MC 34 0 58 Oh, 2006 MF & MC 97 6 66 Gentillini, 2008 MF & MC 476 5 73 Lim, 2009 MF 147 2 59 Chung, 2012 MF 164 6. 1 112 Yerushalmi, 2012 MF & MC 300 5. 5 95
Unifocal vs multifocal CA breast Prognostic implication
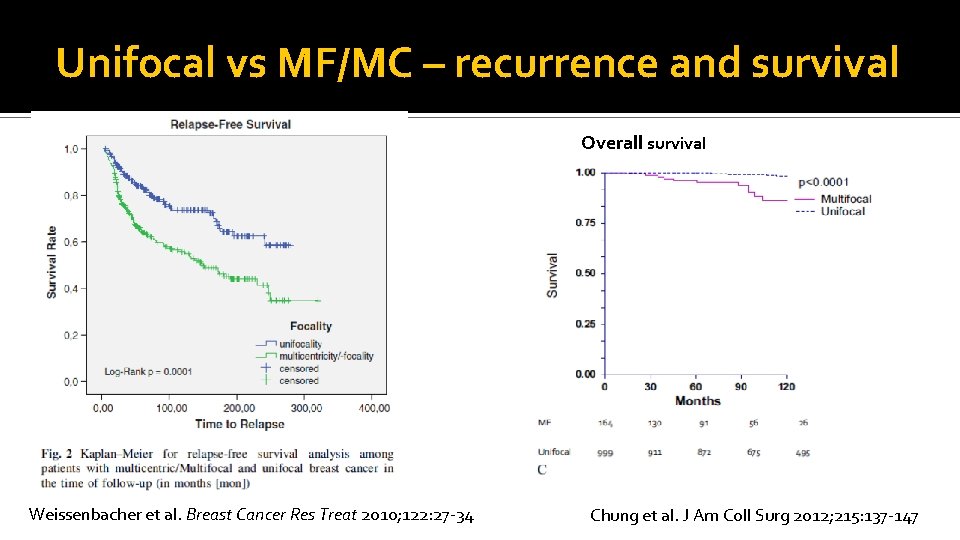
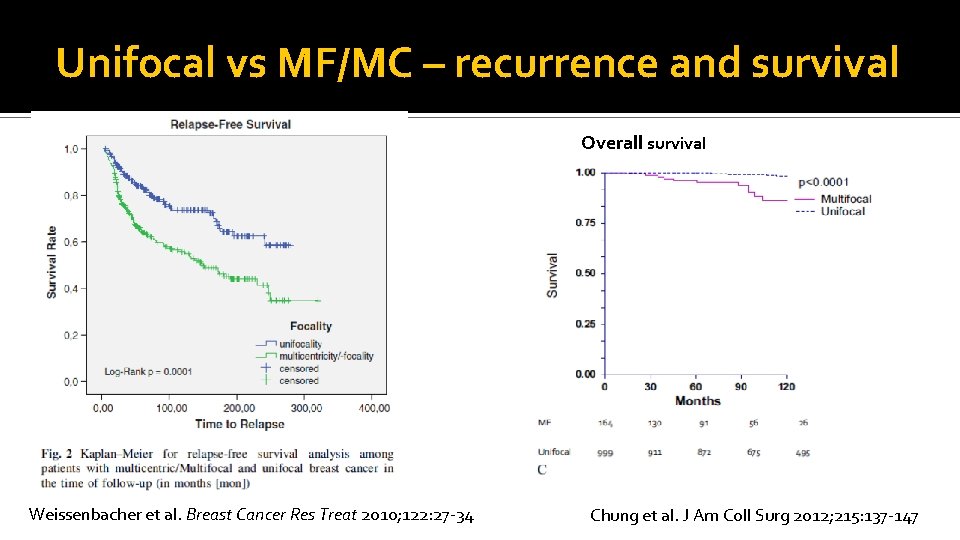
Unifocal vs MF/MC – recurrence and survival Overall survival Weissenbacher et al. Breast Cancer Res Treat 2010; 122: 27 -34 Chung et al. J Am Coll Surg 2012; 215: 137 -147
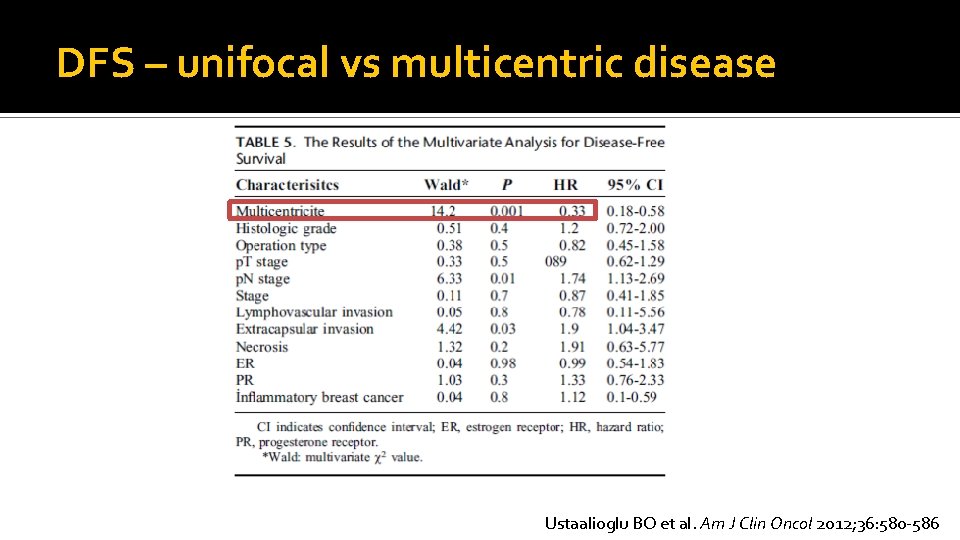
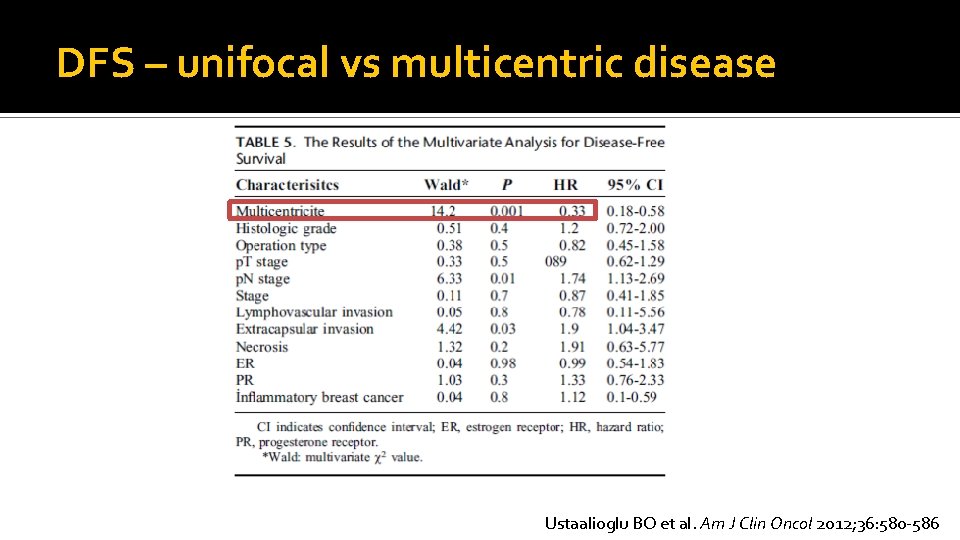
DFS – unifocal vs multicentric disease Ustaalioglu BO et al. Am J Clin Oncol 2012; 36: 580 -586
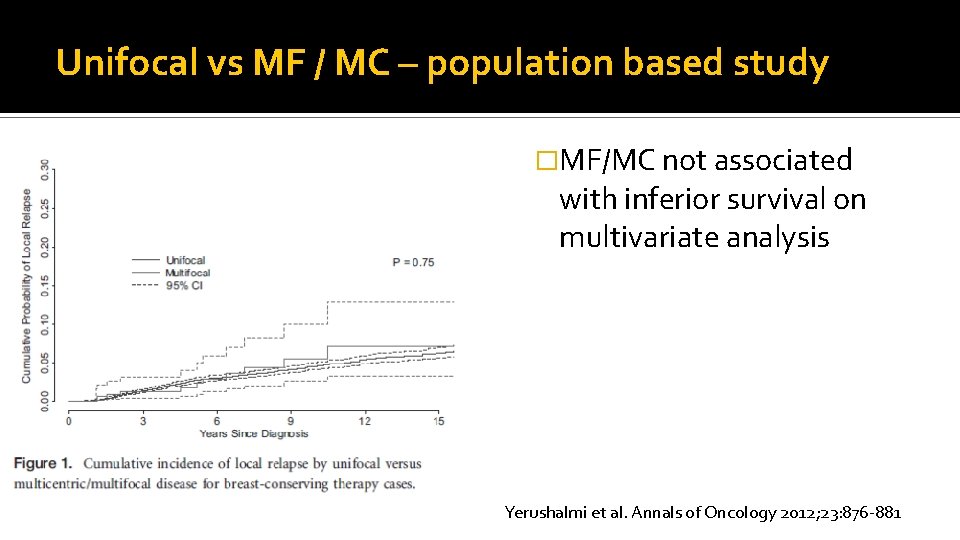
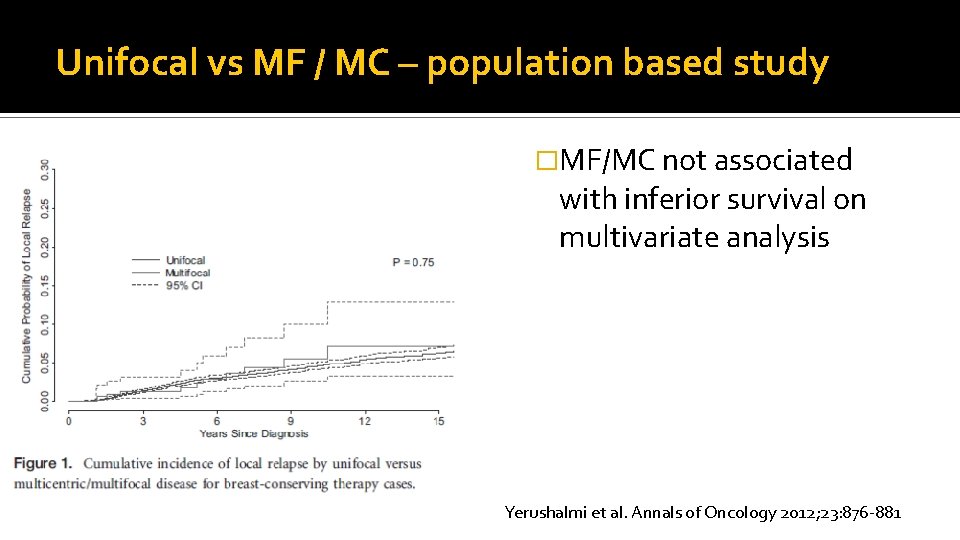
Unifocal vs MF / MC – population based study �MF/MC not associated with inferior survival on multivariate analysis Yerushalmi et al. Annals of Oncology 2012; 23: 876 -881
MF / MC breast cancer – survival �No comparative survival data on BCT vs mastectomy in MF / MC disease
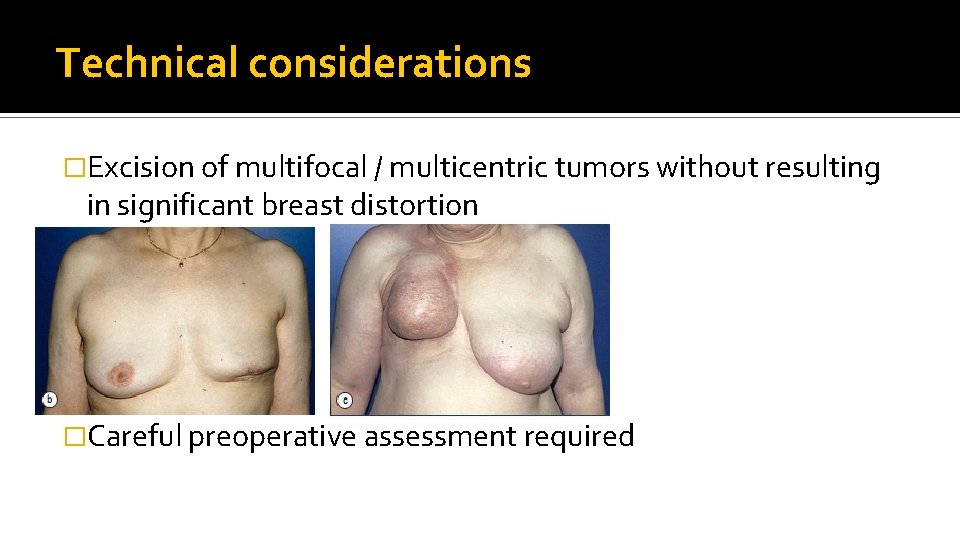
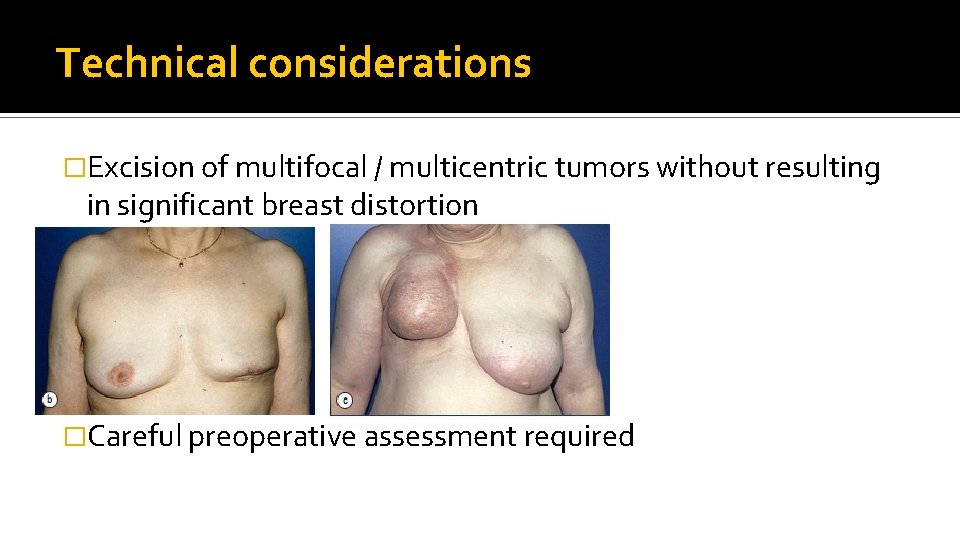
Technical considerations �Excision of multifocal / multicentric tumors without resulting in significant breast distortion �Careful preoperative assessment required
Role of MRI breast in preoperative assessment �Routine use of MRI breast in preoperative staging for early CA breast is controversial �Meta-analysis showed that MRI could identify additional multifocal / multicentric foci that preclude breast conservation �Possibility of false positive finding, unnecessary mastectomy Houssami et al. J Clin Oncol 2008; 26: 3248 -58 �RCT showed no improvement in reoperation rate L Turnbull et al. Lancet 2010; 375: 563 -71
Role of MRI �Possible role in confirmed MF / MC disease to rule out additional tumor foci and define extent of disease?
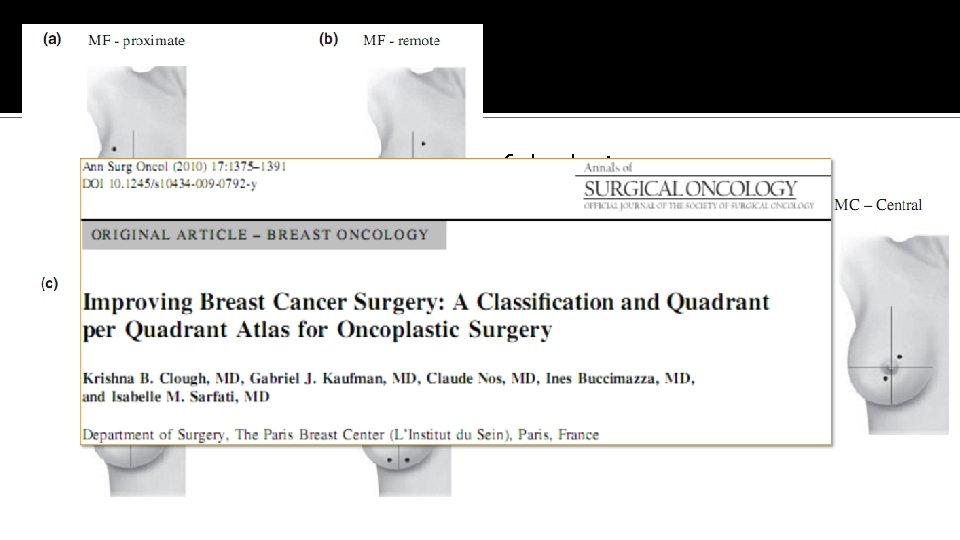
Choice of approach �Size, location and distribution of the lesions �Breast volume, ptosis �Surgeon preference �Single vs multiple wide local excisions �Choice of breast restoration Oncoplastic surgical techniques
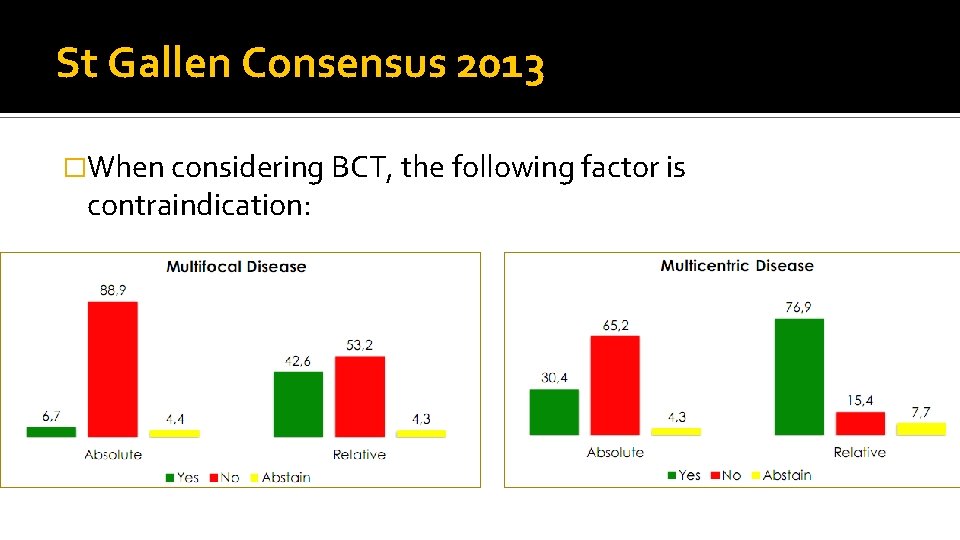
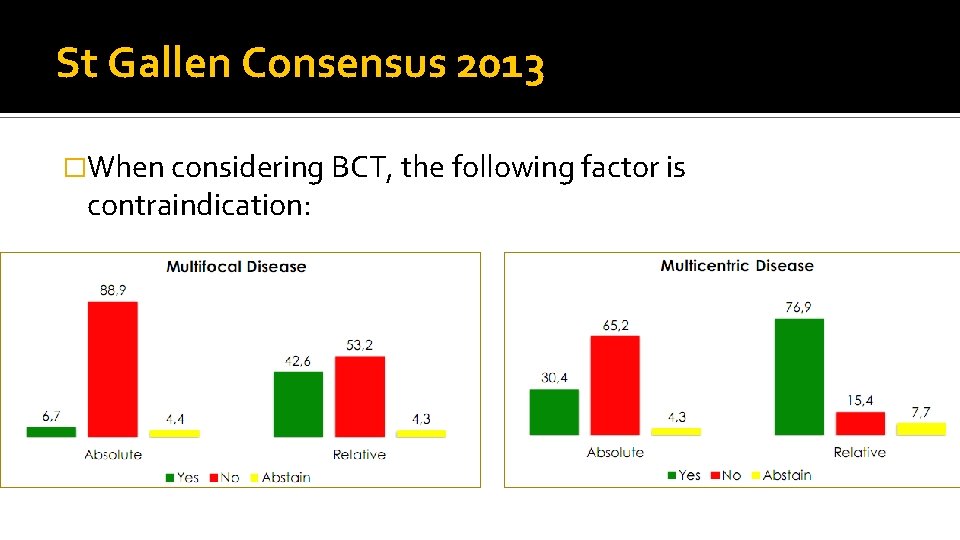
St Gallen Consensus 2013 �When considering BCT, the following factor is contraindication:
Conclusion �BCT is not absolutely contraindicated in cases of multifocal or multicentric breast cancers �Acceptable recurrence rate and survival can be obtained with adequate tumor excision and adjuvant therapy �Therapeutic strategy should be individualized based on the feasibility of wide local excision with negative margins and patient’s preference
The end
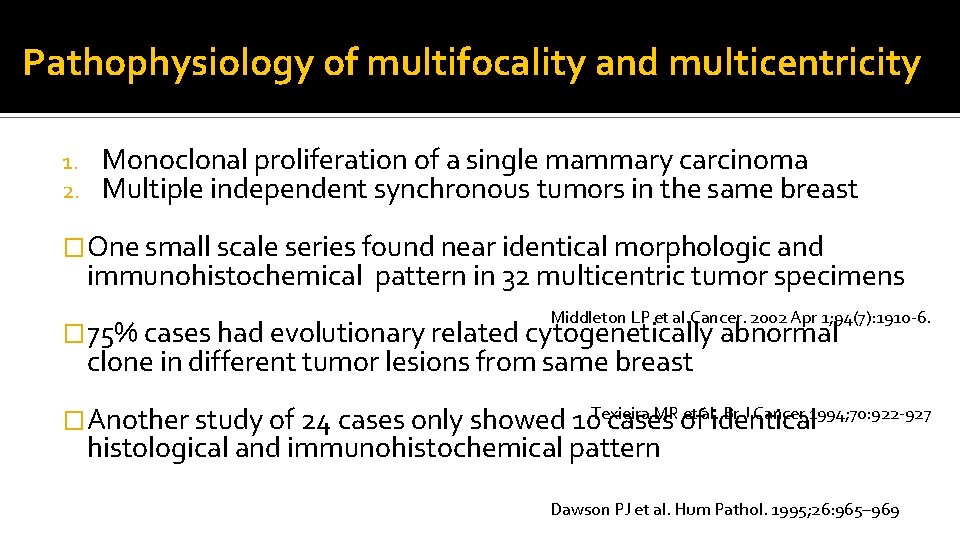
Pathophysiology of multifocality and multicentricity 1. 2. Monoclonal proliferation of a single mammary carcinoma Multiple independent synchronous tumors in the same breast �One small scale series found near identical morphologic and immunohistochemical pattern in 32 multicentric tumor specimens Middleton LP et al. Cancer. 2002 Apr 1; 94(7): 1910 -6. � 75% cases had evolutionary related cytogenetically abnormal clone in different tumor lesions from same breast Texieira MR et al. Br J Cancer 1994; 70: 922 -927 �Another study of 24 cases only showed 10 cases of identical histological and immunohistochemical pattern Dawson PJ et al. Hum Pathol. 1995; 26: 965– 969
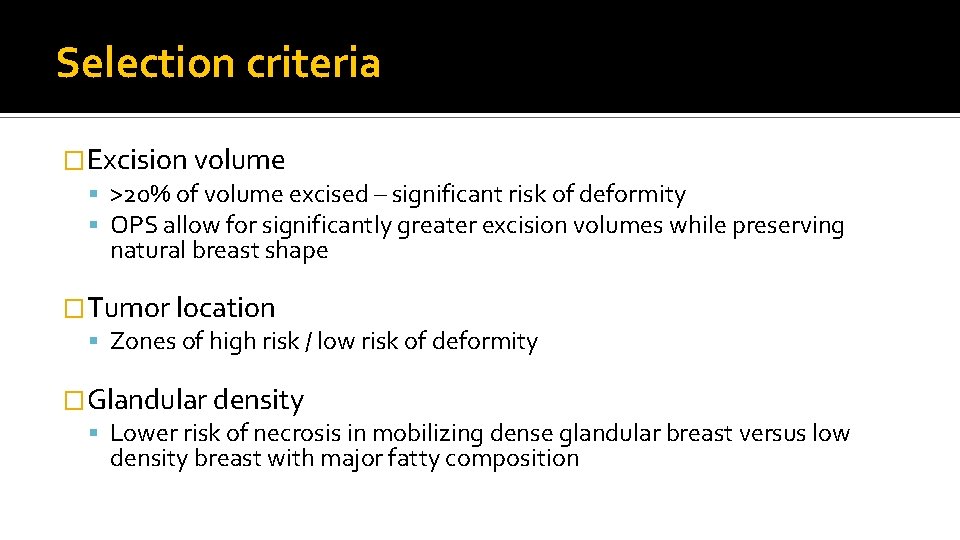
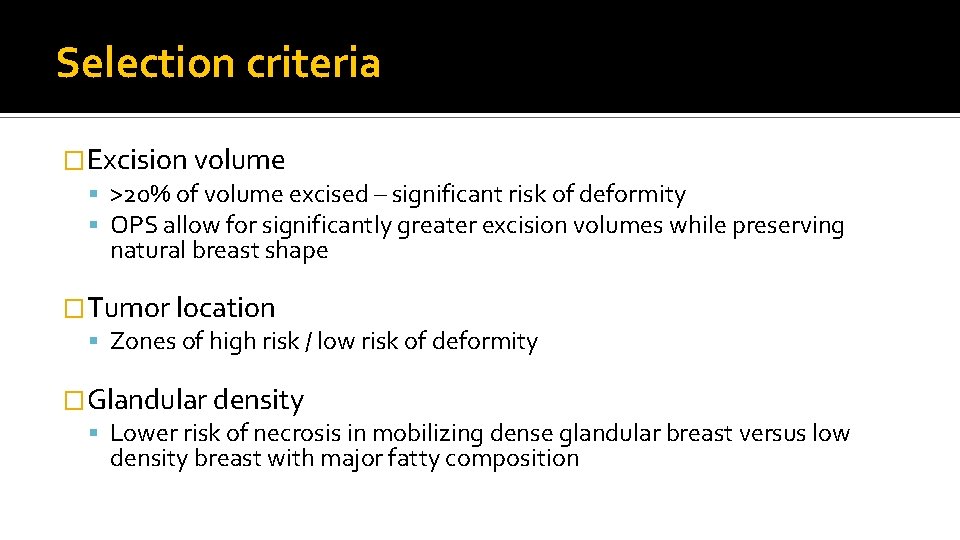
Selection criteria �Excision volume >20% of volume excised – significant risk of deformity OPS allow for significantly greater excision volumes while preserving natural breast shape �Tumor location Zones of high risk / low risk of deformity �Glandular density Lower risk of necrosis in mobilizing dense glandular breast versus low density breast with major fatty composition
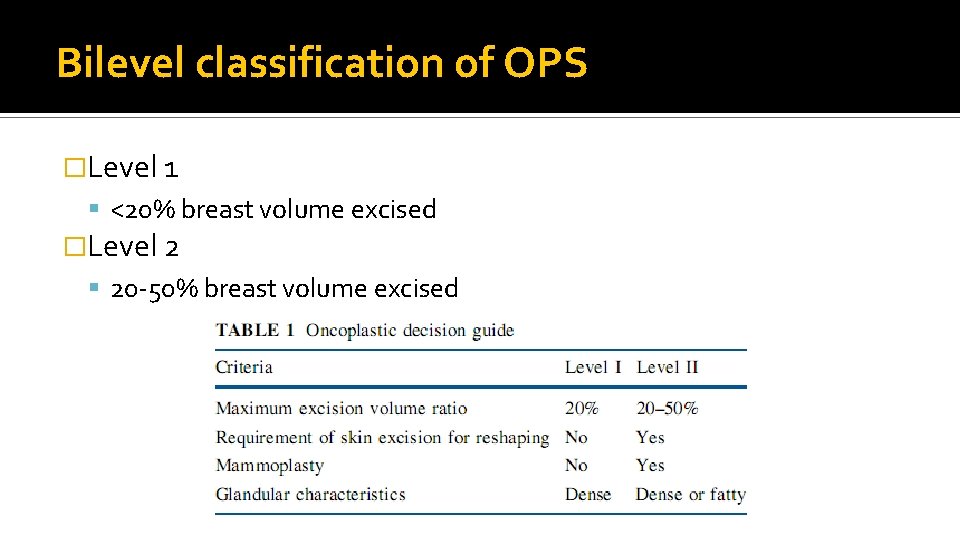
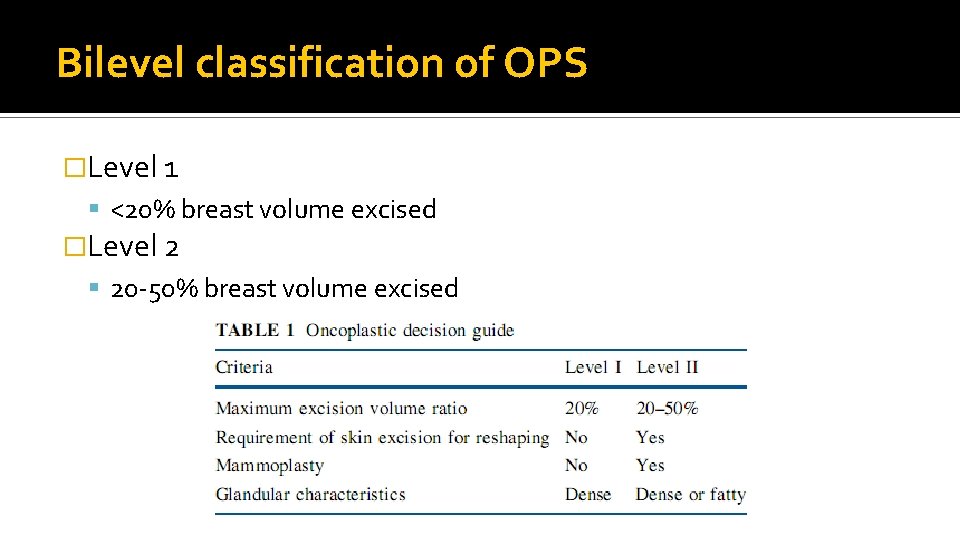
Bilevel classification of OPS �Level 1 <20% breast volume excised �Level 2 20 -50% breast volume excised
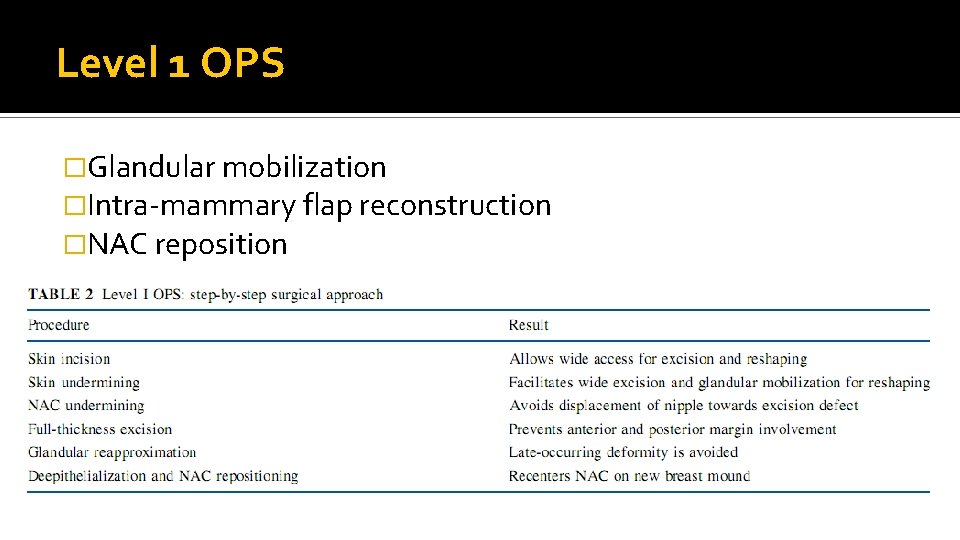
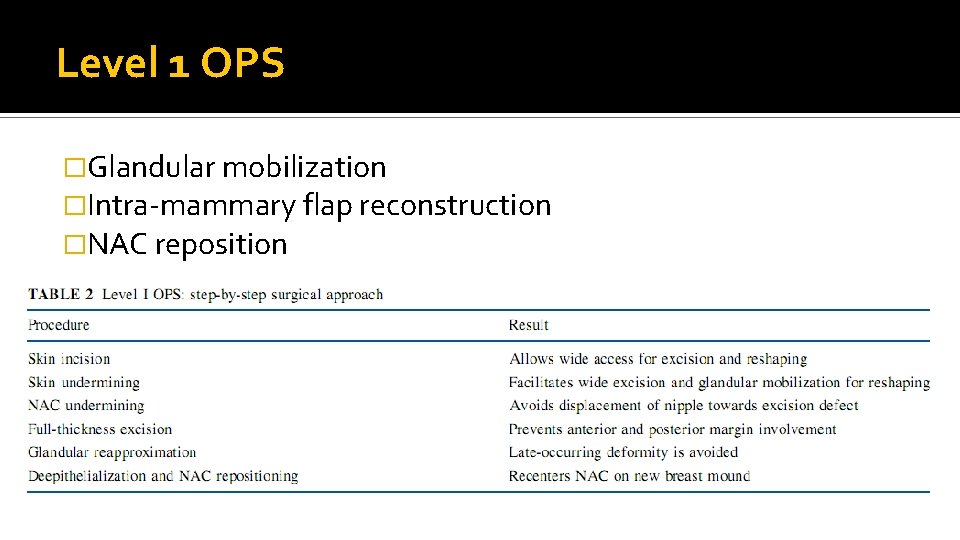
Level 1 OPS �Glandular mobilization �Intra-mammary flap reconstruction �NAC reposition
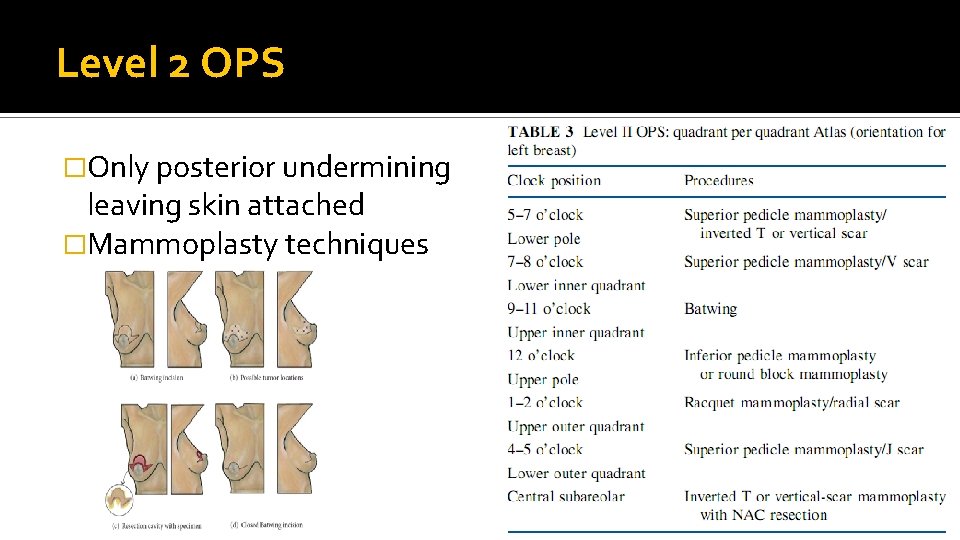
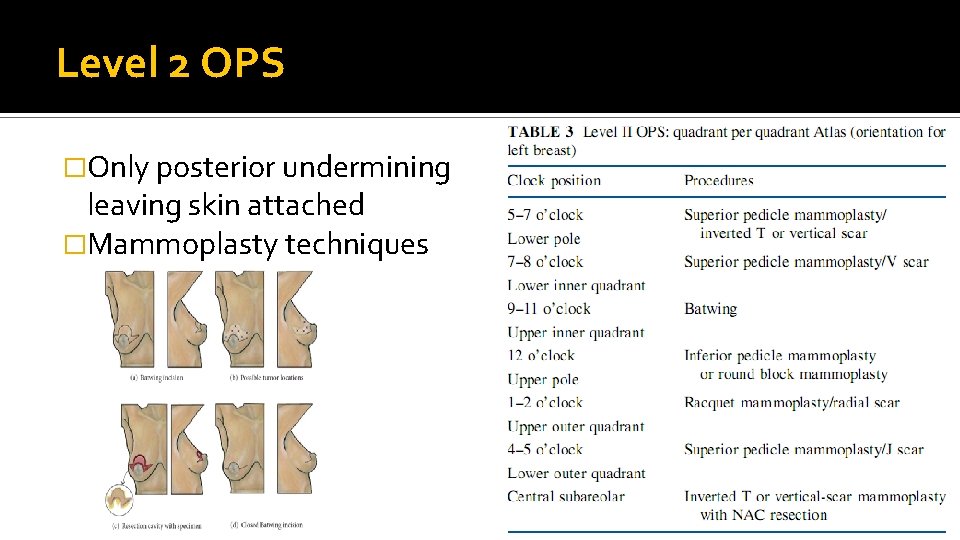
Level 2 OPS �Only posterior undermining leaving skin attached �Mammoplasty techniques
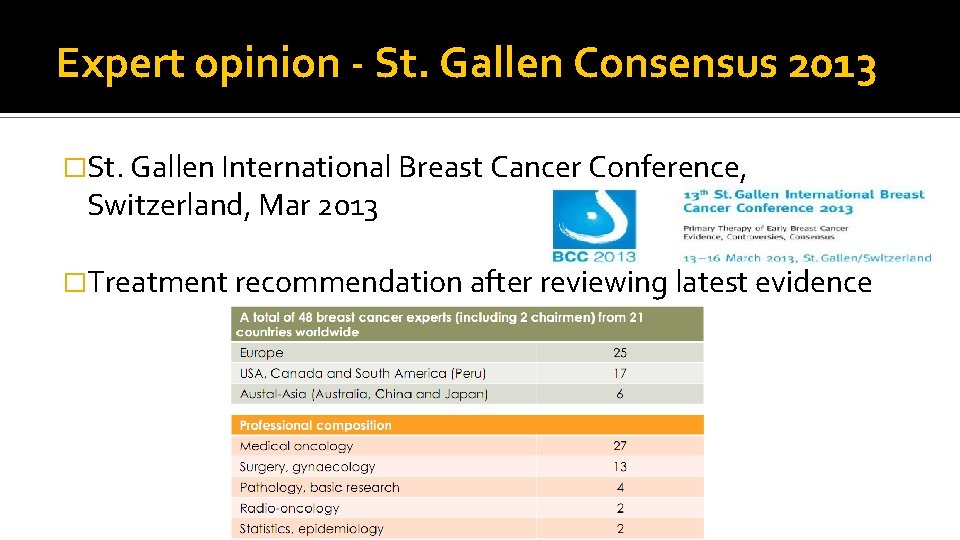
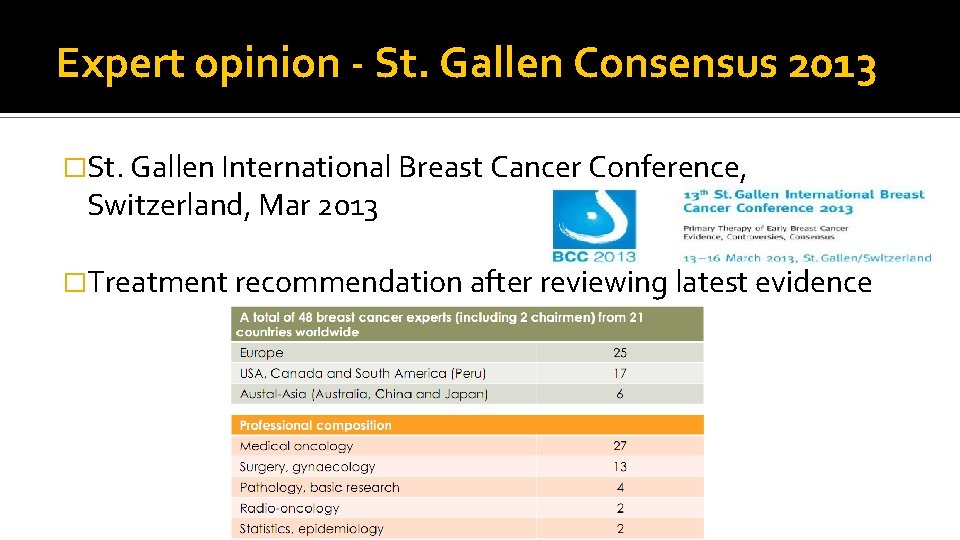
Expert opinion - St. Gallen Consensus 2013 �St. Gallen International Breast Cancer Conference, Switzerland, Mar 2013 �Treatment recommendation after reviewing latest evidence
 Gde mission and vision
Gde mission and vision North central district health department ct
North central district health department ct Milada cosmetic surgery hospital
Milada cosmetic surgery hospital Ospital ng maynila address
Ospital ng maynila address Wvu department of surgery
Wvu department of surgery Yip sir
Yip sir Yipsir
Yipsir Tommy yip
Tommy yip Yipsir
Yipsir Yipsir
Yipsir Michael chun
Michael chun Yip sir social work
Yip sir social work Yip sir
Yip sir Diarusis
Diarusis Kalabo district
Kalabo district Benzie-leelanau county health department
Benzie-leelanau county health department North mason school levy
North mason school levy Proof of tenure
Proof of tenure Blood type map
Blood type map Northern suburban special education district
Northern suburban special education district Geoweb property viewer
Geoweb property viewer Requirements and abilities required for hospital pharmacist
Requirements and abilities required for hospital pharmacist Hesf1
Hesf1 Hospital pharmacy organizational chart
Hospital pharmacy organizational chart Flagler hospital billing department
Flagler hospital billing department North middlesex hospital pharmacy
North middlesex hospital pharmacy North palm beach police
North palm beach police North west department of public works and roads vacancies
North west department of public works and roads vacancies Geoweb north vancouver
Geoweb north vancouver True north vs magnetic north
True north vs magnetic north North east and north cumbria ics map
North east and north cumbria ics map