High Altitude Illness David Gonzales MD Medicine You




- Slides: 32
High Altitude Illness David Gonzales, MD
Medicine You Will Probably Never Use in Texas Guadalupe Peak, 8, 749 feet Might as well be in New Mexico
Outline Challenges of High Altitude Physiologic Response to Hypobaric Hypoxia High Altitude Syndromes Acute Mountain Sickness/ High Altitude Cerebral Edema High Altitude Pulmonary Edema
Oxygen = Good Amount of oxygen available to breathe is a function of the percentage of oxygen in the air and barometric pressure. Earth’s atmosphere is 21% oxygen Barometric pressure at sea level = 760 mm Hg Pressure of inspired oxygen =149 mm Hg
Less oxygen = bad Denver = 5000 feet Pi. O 2 = 124 mm Hg Santa Fe = 7000 feet Pi. O 2 = 115 mm Hg Highest human habitation = 18, 000 ft. Pi. O 2 = 73 mm Hg Mt. Everest = 29, 528 ft Pi. O 2 = 42 mm Hg (about ¼ that of sea level)
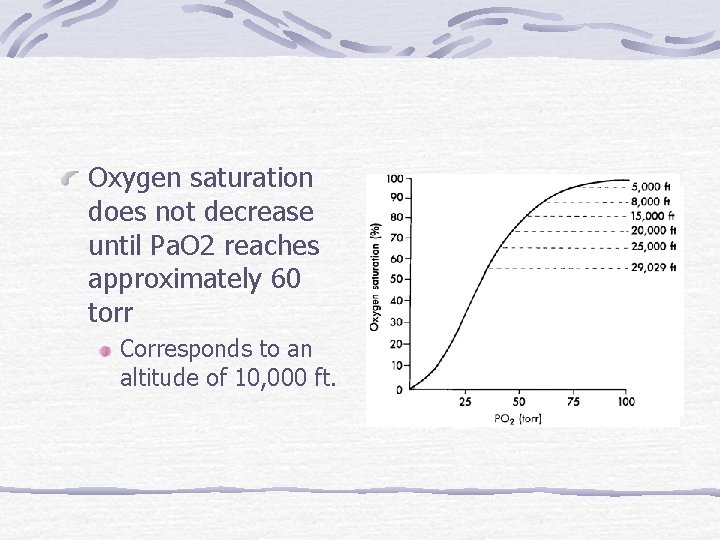
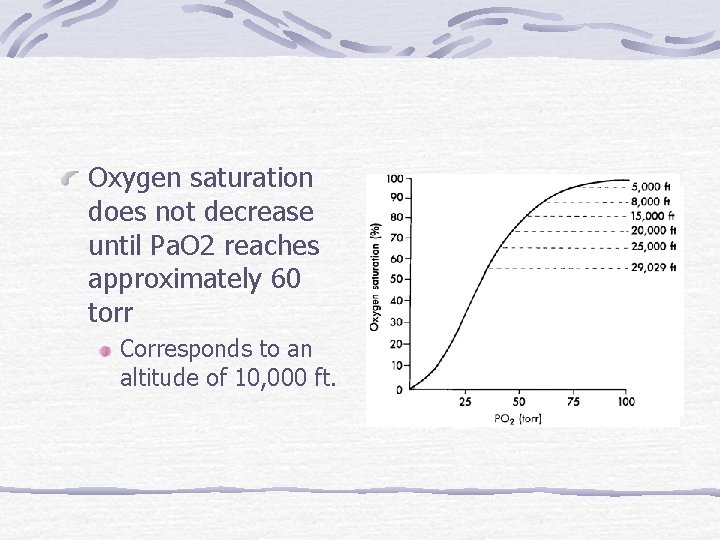
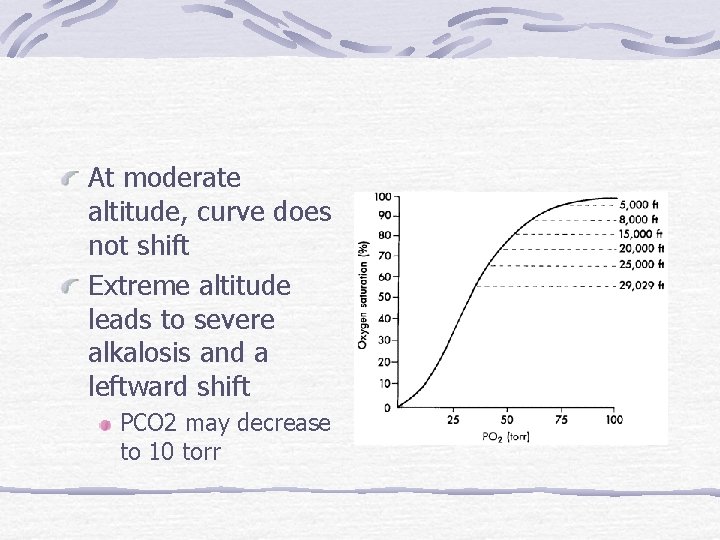
Oxygen saturation does not decrease until Pa. O 2 reaches approximately 60 torr Corresponds to an altitude of 10, 000 ft.
Physiologic Response to Hypoxia Acclimatization A gradual process (days to weeks) whereby individuals respond to hypoxia in order to adapt and increase performance Rate varies among individuals Mediated through sympathetic nervous system
Ventilatory Response Carotid body senses decreased Pa. O 2; signals medulla to increase ventilation Respiratory alkalosis ensues, decreasing ventilation Subsequent HCO 3 diuresis occurs through the kidney and ventilation subsequently increases again This process stabilizes after 4 -7 days, provided altitude does not change
Cardiovascular Response Heart rate increases, leading to a moderate rise in cardiac output Pulmonary artery pressure increases secondary to hypoxic vasoconstriction Cerebral blood flow increases These last 2 adaptations may become pathologic (more on this later)
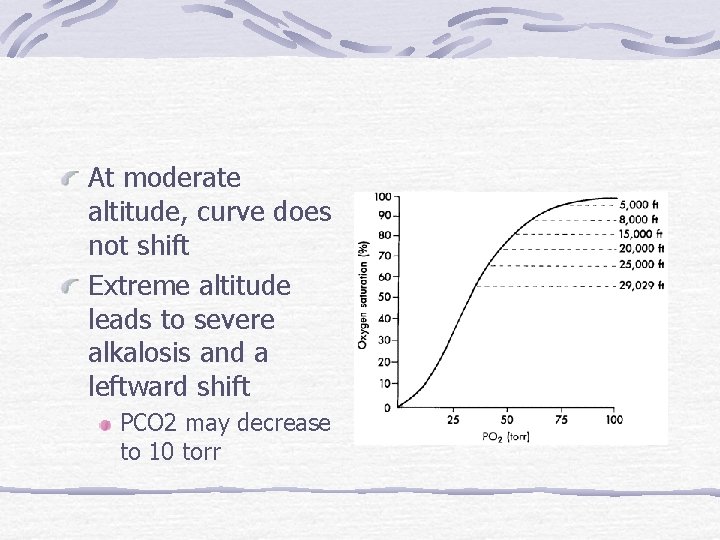
At moderate altitude, curve does not shift Extreme altitude leads to severe alkalosis and a leftward shift PCO 2 may decrease to 10 torr
Pathologic Syndromes Acute Mountain Sickness (AMS) A headache + (any of the following) Nausea/vomiting Fatigue Dizziness Sleep disturbance



Diagnosis Suspect in non-acclimatized persons above 8, 200 feet Rapid ascent
AMS Pathophysiology Not so much hypoxia, rather your body’s response to it Lag time between onset of symptoms; acclimatization cures
Pathophysiology of AMS Low ventilatory response increases risk Fluid retention Evidence suggests vasogenic cerebral edema plays a central role, however cellular mechanisms not yet elucidated Big brain, small skull
Treatment of AMS Prevention is best treatment Avoid abrupt ascent to sleeping altitudes >10, 000 feet Don’t increase sleeping altitude by more than 2000 ft. per night Climb high, sleep low philosophy Acetazolamide (Diamox) 125 to 250 mg po bid Carbonic anhydrase inhibitor Diuresis Metabolic acidosis increased breathing Decreases CSF production
Treatment of AMS Supportive analgesics, antiemetics Diamox to hasten acclimatization Minimize exertion Low flow oxygen if available Consider dexamethasone Failure of symptoms to improve with treatment or progression of symptoms despite 24 hours of acclimatization is an indication to descend.
High Altitude Cerebral Edema (HACE) A progression of AMS to a severe, lifethreatening condition AMS + Ataxia Altered consciousness Severe lassitude Cerebral edema is cytotoxic rather than vasogenic
High Altitude Cerebral Edema (HACE) Cellular swelling thought to be caused in part by NMDA-receptor mediated calcium influx. Trial using magnesium infusion (an NMDA blocker) were clinically unsuccessful in treating AMS; prophylaxis with Mg citrate only caused diarrhea
Treatment of HACE Early recognition is key Oxygen 2 -4 liters Dexamethasone Immediate Descent
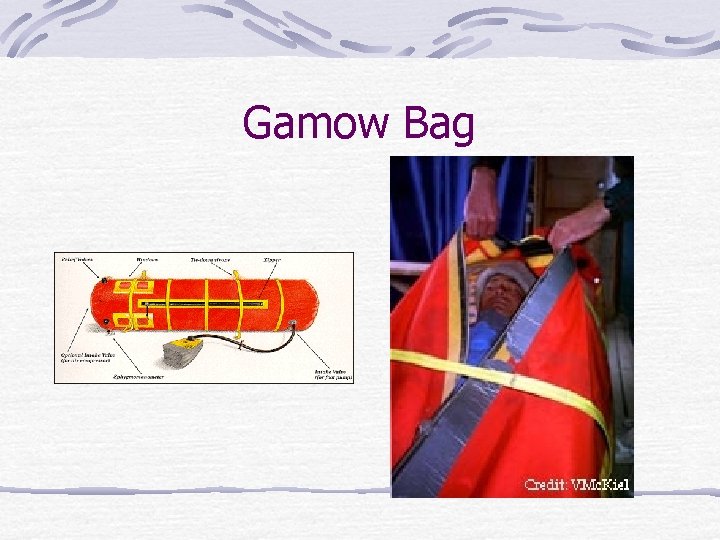
Gamow Bag An impermeable bag that can be inflated to simulate a lower altitude Patient placed inside but reassessed periodically HAPE = 2 to 4 hours of treatment HACE = 4 to 6 hours of treatment
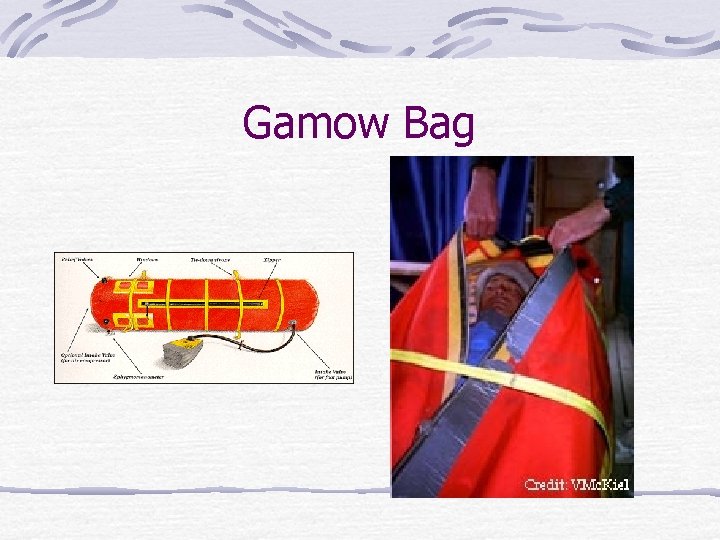
Gamow Bag

Portable Altitude Chamber Zipper placement makes it easier to use than Gamow Low, low price of $1, 200
High Altitude Pulmonary Edema (HAPE) Most common cause of high-altitude related death Easily treated/prevented with prompt recognition <1 in 10, 000 in Colorado skiers 1 in 50 in climbers on Mt. Mc. Kinley Risk factors include individual susceptibility, rapid ascent, exertion, altitude reached
Manifestations of HAPE Decreased exercise performance Dyspnea at rest; often occurs during sleep AMS (50%) Dry cough Cyanosis RLL crackles Pink, frothy sputum (late sign)
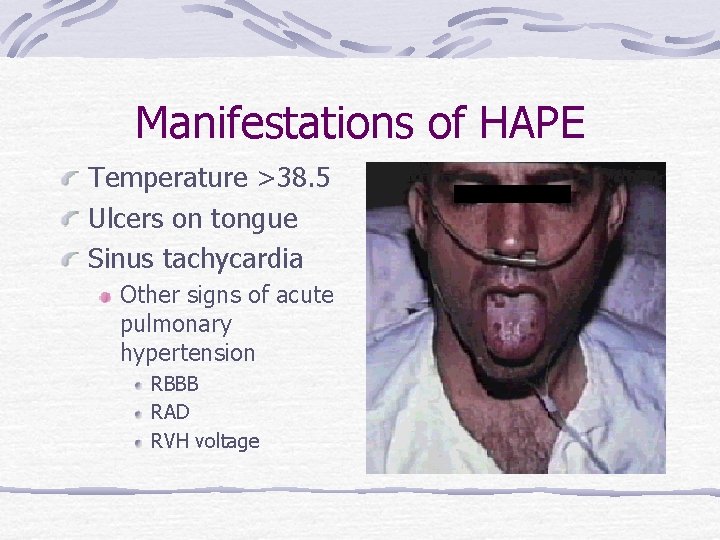
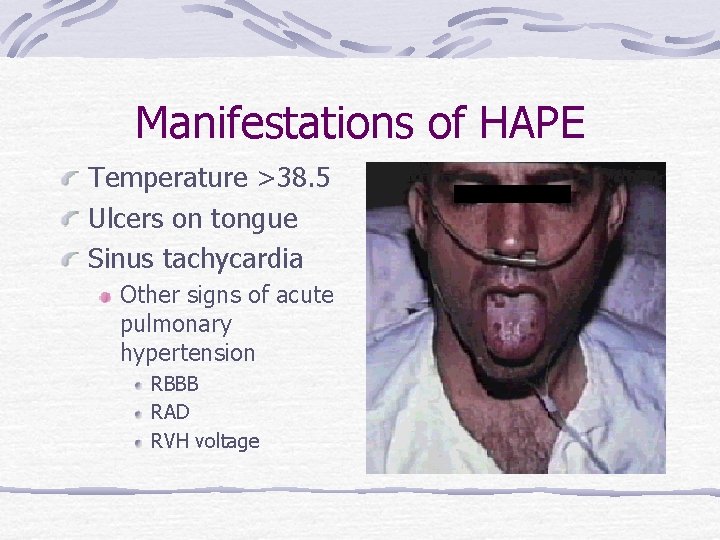
Manifestations of HAPE Temperature >38. 5 Ulcers on tongue Sinus tachycardia Other signs of acute pulmonary hypertension RBBB RAD RVH voltage
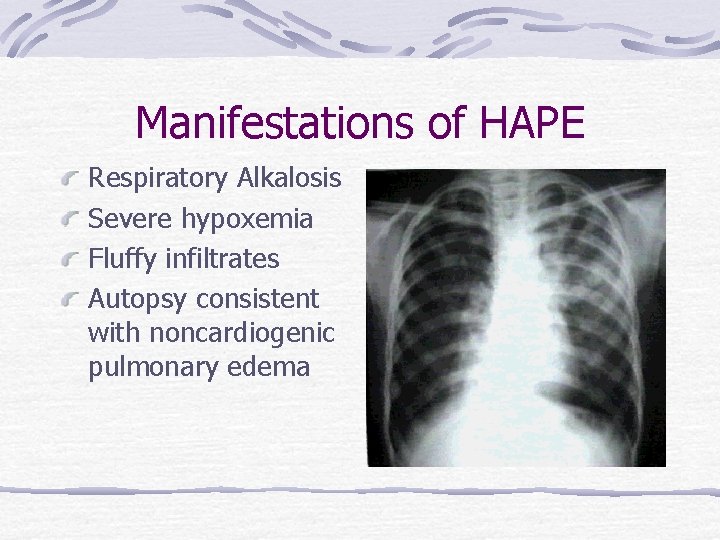
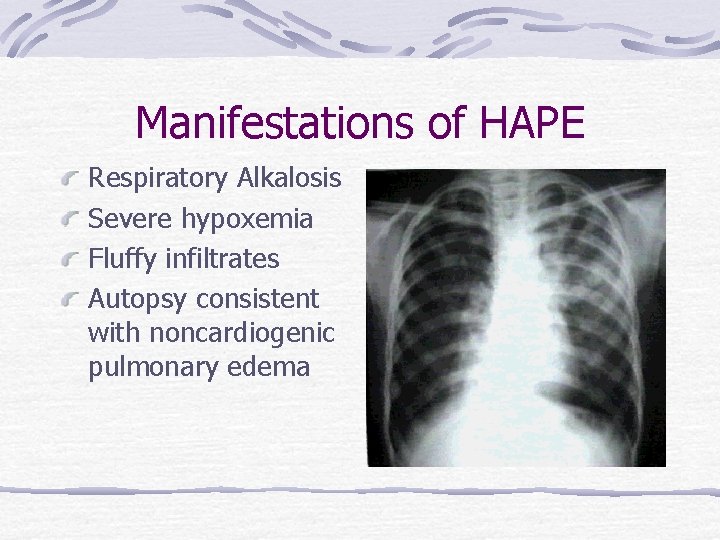
Manifestations of HAPE Respiratory Alkalosis Severe hypoxemia Fluffy infiltrates Autopsy consistent with noncardiogenic pulmonary edema
Pathophysiology of HAPE Pulmonary Hypertension-A fact of life at high altitude Global hypoxic pulmonary vasoconstrictor response When is it pathologic? Increased Capillary Permeability Shear forces vs. endothelial dysfunction Decreased HVR Role in nighttime hypoxia
Treatment of HAPE Early recognition should lead to evacuation/descent This will limit severity and hasten recovery O 2 if available; Gamow bag Vasodilators as adjuncts Nifedipine Salmeterol Ounce of prevention
Summary Altitude acclimatization is a highly individualized process Mild AMS is best treated supportively HACE and HAPE require more aggressive treatment Common sense and adequate preparation go a long way
 Lhaaso
Lhaaso Lijack
Lijack David mechanic illness behaviour
David mechanic illness behaviour Ilan ang katangian ng pananaliksik
Ilan ang katangian ng pananaliksik Tourbillon de passions mauricio gonzáles
Tourbillon de passions mauricio gonzáles 3 reformas de alfredo gonzales flores
3 reformas de alfredo gonzales flores Adolfo gonzales chief probation officer
Adolfo gonzales chief probation officer Neal martin maura gonzales
Neal martin maura gonzales Image processing place
Image processing place Propiedades fisicas y quimicas del fosforo
Propiedades fisicas y quimicas del fosforo Geisha gonzales
Geisha gonzales Speedy gonzales
Speedy gonzales Vladimeir gonzales
Vladimeir gonzales Bidy gonzales plant
Bidy gonzales plant Speedy gonzales sounds
Speedy gonzales sounds Mercedes gonzales
Mercedes gonzales Glaucio gonzales
Glaucio gonzales Verbal order read back
Verbal order read back Indicated altitude
Indicated altitude Aerodrome physical characteristics
Aerodrome physical characteristics Lateral faces of cone
Lateral faces of cone Soti
Soti Sun path angle
Sun path angle Indicated altitude
Indicated altitude Properties of median of isosceles triangle
Properties of median of isosceles triangle Medians and altitudes of triangles
Medians and altitudes of triangles Pascaline pey
Pascaline pey Minimum safe altitude vfr
Minimum safe altitude vfr Medians and altitudes of a triangle
Medians and altitudes of a triangle Chapter 9 geometry
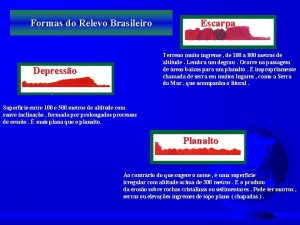
Chapter 9 geometry Formada por morros pontiagudos cristas
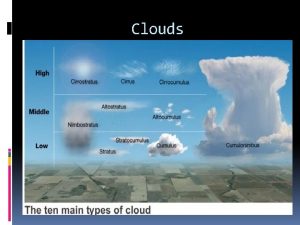
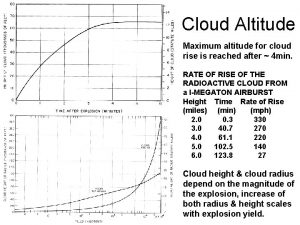
Formada por morros pontiagudos cristas Low altitude cloud
Low altitude cloud Continentalidade
Continentalidade