Medical Staff Orientation 1 Welcome to Memorial Hospital






















- Slides: 83

Medical Staff Orientation 1

Welcome to Memorial Hospital! This orientation tutorial is being presented to provide you with important information about Memorial and certain regulatory requirements. We hope you find it informative. 2
T Mission • Our mission is to build a healthier community. • We are a public institution dedicated to the provision of quality health care services for citizen of the Hospital District and such other persons as may be accommodated. • Memorial serves as a responsive, comprehensive health care resource for its patients, Medical Staff, and the health care consumers of the community served by the Hospital and its affiliated organizations. Hospital By-Laws, Article I 3

T Shared Vision • We believe in a future where the Hospital and Medical Staff work collaboratively to provide our community with not just quality care, but care that sets the benchmark for quality. • As the Hospital of Choice for our community, we need to provide our patients with access to the care they need by providing a medical staff with adequate numbers of specialists, primary care physicians and locations that are both convenient and responsive to our community. • We believe that we must keep our facilities up-to-date and provide our caregivers with technology to improve the care that they give with both information systems and equipment. We must provide an infrastructure that supports constant clinical improvements and safety, and provides for active physician involvement. We must also provide a collegial workplace for our staff and physicians, where all team members are treated with respect. • We acknowledged that we cannot achieve this future without adequate financial resources. • We believe that in order to maximize our financial standing we need physician involvement as we strategize about revenue enhancement, payer relationships and effective care processes • We believe that strong alignment between Memorial Hospital and our Medical Staff, both private and employed, needs to be the foundation on which we build a shared future. Hospital By-Laws, Article I 4
Basic Obligations of Staff Membership Staff members, regardless of assigned staff category, and practitioners exercising privileges under these Bylaws, shall: • Provide their patients with care at the level of quality and safety consistent with recognized standards of healthcare • Abide by the Medical Staff Bylaws and all other lawful standards, policies and rules of the medical staff • Discharge such staff, committee, department, and hospital functions for which they are responsible by staff category assignment, appointment, election or otherwise • Prepare and complete the medical and other required records for all patients they admits or in any way provides care to in the hospital at the time of discharge, and sign such records within 30 days after discharge • Pledge to provide or arrange for continuous, appropriate and timely medical coverage and care for patients for whom they are responsible • Participate in continuing medical education activities consistent with Mississippi State Board of Medical Licensure Continuing Medical Education requirements and report said participation to the Medical Staff 5
Medical Staff Code of Conduct Medical staff member conduct is governed according to these medical staff bylaws. This Code of Conduct shall not be construed so as to prohibit a public or private employer of a member of the Medical Staff from negotiating additional behavior or conduct terms in contracts of employment with members of the Medical Staff; however, compliance with such additional terms, if any, and their enforcement are beyond the scope of this Code. APPROPRIATE CONDUCT: The following kinds of conduct by medical staff members are not restricted by these bylaws: • Advocating for patients in an appropriate, respectful and professional manner. • Criticism that is meant to improve care in an appropriate, respectful and professional manner. • Legitimate business activities that may or may not compete with the hospital. Medical Staff By-laws Article 13 6
Medical Staff Code of Conduct ACTIONABLE CONDUCT: Medical staff member conduct is actionable under these bylaws if harassment can reasonably be considered to be directed against any individual at the Hospital on the basis of: • race • religion • color • national origin • ancestry • physical disability • mental disability • medical disability • age • marital status • sex or sexual orientation AND/OR • verbal, visual or physical abuse, directed against any individual at the Hospital including: • another medical staff member • house staff • hospital employee • contractor • volunteer • patient or visitor. Medical Staff By-laws Article 13 7
Memorial Code of Conduct Memorial is committed to maintaining an environment based on mutual respect, civility and positive personal relationships that contributes to the healing and comfort of our patients and their families, and enhances personal growth and job satisfaction for our staff. Staff at Memorial will: • Embrace the Hospital's Service Standards: Service, Teamwork, Attitude and Respect. • Be cooperative with others. Demonstrate good teamwork principles. Recognize that our organization is only successful if we are successful as a team. • Communicate in a timely and professional manner, and in an appropriate setting. • Provide constructive criticism or comments in a respectful manner. • Always be respectful of patients and their families. Give clear instructions when necessary for the care of patients and families. • Respond positively to requests for assistance if the requested assistance is within the individual's scope of practice. • Always adhere to principles of patient confidentiality. • Be understanding that a variety of experience levels exist, and tolerant of those who are learning. • Maintain self control and utilize appropriate conflict resolution strategies when confronted by people who are angry. Leadership Policy I. 41 8
Memorial Code of Conduct Staff at Memorial will not (included, but not limited to): • Behave in a manner that would humiliate, intimidate, degrade or belittle another individual. • Engage in behavior that is disrespectful and/or abusive toward patients, families, visitors or other Hospital staff. • Shout, yell, slam or throw objects in anger or disgust. • Engage in behavior that interferes with therapeutic environment and operations of the Hospital. • Be critical of performance and/or competency in an inappropriate location or when not aimed at performance improvement. • Make inappropriate physical contact with another individual that is unwanted, threatening or intimidating. Leadership Policy I. 41 9
Conflict of Interest • The purpose of the policy is to define those situations where the interests of employees are in conflict with the interests or operations of the Hospital. • The Hospital desires to administer its affairs honestly and economically and in a manner above question. • Conflict of interest may arise from a situation in which: • An individual’s private interests, usually of an economic nature, conflict with or raise a reasonable question of concern with the activities of the Hospital. • As used in this policy, terms are defined by, and set forth, in 25 -4103, Mississippi Code 1973, as amended. Leadership Policy I. 08 10

Medical Staff Policy Conflict of Interest • It is the policy of the Medical Staff that its members have an obligation to avoid ethical, legal and financial or other conflicts of interest to ensure their activities and interests do not conflict with their obligations under the Medical Staff Bylaws. • It is the policy of the Medical Staff that whenever one of its committees or departments considers business or makes decision regarding an organization, entity or individual in which a member of the Medical Staff, one of its committees or departments has conflict the following must occur: 11
Medical Staff Policy Conflict of Interest Continued A. The interested member, if in attendance at the meeting where the matter is being considered, must disclose the conflict to the Presiding Officer; B. The Presiding Officer may then ask the interested member to leave the meeting during the discussion. The member must leave the meeting, if asked, but may make a statement or answer questions before leaving; C. The remaining members at the meeting may then consider the matter and vote upon it as usual but excluding the vote of the interested person. 12
Disclosure of Unanticipated Outcomes • Physicians and other healthcare givers have a professional/ethical obligation to disclose outcomes, including unanticipated, adverse outcomes, to patients, and where appropriate, to patients’ families. • The responsible provider or his/her designee informs the patient, and when appropriate the patient’s family, about these outcomes of care. • When a disclosable event/outcome occurs: A. The responsible provider or his/her designee should be notified immediately. B. The responsible provider should: 1. Address immediate physical and emotional healthcare and safety needs; 2. Discuss additional diagnostic and/or therapeutic treatment as appropriate. C. The responsible provider should clearly document in the medical record: 1. The known objective facts about the unanticipated adverse outcome; 2. A summary of the discussion with the patient/family, and 3. The treatment offered and/or given and follow-up treatment plans. Leadership Policy I. 37 13
The Disclosure Process 1. Verify all pertinent facts and discoveries. 2. Meet with involved caregivers and the Risk Manager or administrative representative on duty to coordinate the disclosure discussion. Consider having a witness. 3. Tell the patient/family the known objective facts at the time of disclosure pending further investigation. 4. Convey empathy, compassion, and regret for the patient/family’s situation. Under no circumstances imply that the hospital will assume liability for the unanticipated adverse outcome. 5. Do not make excuses or assign blame. Avoid speculation or disclosing information protected by Quality Assurance/Peer Review and/or legal privileges that exist. Unanticipated adverse outcomes are not always presentable and the root cause and outcome of the unanticipated adverse outcome may not be fully known at the time disclosure is made. 6. Offer support and assistance that address patient/family religious, cultural, and linguistic needs where appropriate. Social workers, chaplains, interpreters, and customer relations assistance is available as needed. 7. Keep the patient/family involved in subsequent treatment plans and discussions and continue to address their questions and concerns. 8. Caregivers should document the disclosure discussions in the medical record, including the facts and the pertinent points that were communicated, any response, and/or other discussion and the names of those present. Leadership Policy I. 37 14
T Illness or Impairment The impaired practitioners guidelines define the term "impaired" to mean the inability of a practitioner to practice medicine with reasonable skill or safety to patients by reason of one or more of the following: • Mental illness as defined by DSM IV-TRI diagnosis and any current review of this document. • Physical illness or impairment, including but not limited to deterioration through the aging process, or loss of motor skills • Excessive use or abuse of drugs, including alcohol • Other non-specified impairment A copy of the Impaired Practitioners Guidelines may be obtained from Medical Staff Services, or may be found on the hospital intranet home page, listed under Medical Staff Documents as IMPAIRED PRACTITIONERS GUIDELINES. 15
Confidentiality of Information submitted, collected or prepared by any representative of this or any other health care facility or organization or medical staff for the purpose of evaluating, monitoring or improving the quality and efficiency of patient care, reducing morbidity and mortality, contributing to teaching or clinical research, or determining that health care services are professionally indicated or were performed in compliance with the recognized standards of healthcare shall, to the fullest extent permitted by law, be confidential. Said information shall not be disseminated to anyone other than a representative or other health care facility or organization of health professionals engaged in an official, authorized activity for which the information is needed, nor be used in any way except as provided herein or except as otherwise specifically required by law. Such confidentiality shall also extend to information of like kind that may be provided by third parties. This information shall not become part of any particular patient's record. It is expressly acknowledged by each Memorial Hospital-Medical Staff practitioner that violation of the confidentiality provided herein is grounds for immediate and permanent revocation of staff membership and clinical privileges or specified services. Medical Staff By-Laws Sec 5. 3 16
HIPAA Protected Health Information • PHI is information that identifies an individual; relates to the individual’s health, healthcare treatment or healthcare payment; and is maintained or disclosed electronically, on paper and/or orally. It includes identification, physical and mental conditions, treatment, clinical test results, financial information, demographic information, etc. • Individual identifiers include: • Name • Full face photographs • Social Security number • Biometric identifiers ( e. g. , fingerprints) • Medical record number • Health Plan number • Geographic location, except for state • Account number • All dates, except for year • License number • All ages over 89 • Vehicle identification • Telephone number • Device identifiers • Fax number • URLs & IP addresses • E-mail address • Any other unique number or code Patients have the right to: • Request restrictions on certain uses or disclosure of their medical information. • Request communication in a certain way or at a certain location. • Inspect and obtain a copy of any medical record that providers use to make decisions about them and their treatment. This includes the legal medical record, their billing records and may extend to other shadow and research records, if not included in the legal record. This right is subject to certain specific exceptions. • Add an addendum to or correct their medical record. The request may be denied for certain specific reasons, but the patient will be provided with a written explanation for the denial and information, regarding further rights they may have at the time of denial. • Request an "accounting of disclosures" – that is, a list describing with whom and why their medical information has been shared with outside parties. This list must even include those disclosures that are required by law. • Receive a copy of the Notice of Privacy Practices. • Complain to Memorial and/or to HHS, if they believe the organization violated their privacy 17
Conditions Present at Admission (POA) • POA indicator is a reporting data element required by CMS for patient diagnoses on in-patient visits to reflect whether each diagnosis was present on admission or not. • POA is defined as present at the time the order for inpatient admission occurs. Conditions that develop during an outpatient encounter, including emergency department, observation or out-patient surgery, are considered present on admission. • POA indicators are appended to each ICD-10 -CM code reported for patient’s conditions and diagnoses documented in the medical record by physicians/providers. • POA data will be used for measuring hospital performance, public reporting, and payment. 18
Advance Directives • Mississippi’s Uniform Health Care Decisions Act of 1998 recognizes advance directives for health care. • An advance directive can be an individual instruction or a Power of Attorney for Health Care. • Employees of health care facilities may not witness an advance directive for health care. • When the physician objects to the implementation of a patient's advance directive, and/or healthcare decision and the advance directive and/or decision in question complies with hospital policy and procedure, the director of the unit (or designee) will assist in transfer of the patient to another physician. Patient Care Policy IV. 03 19
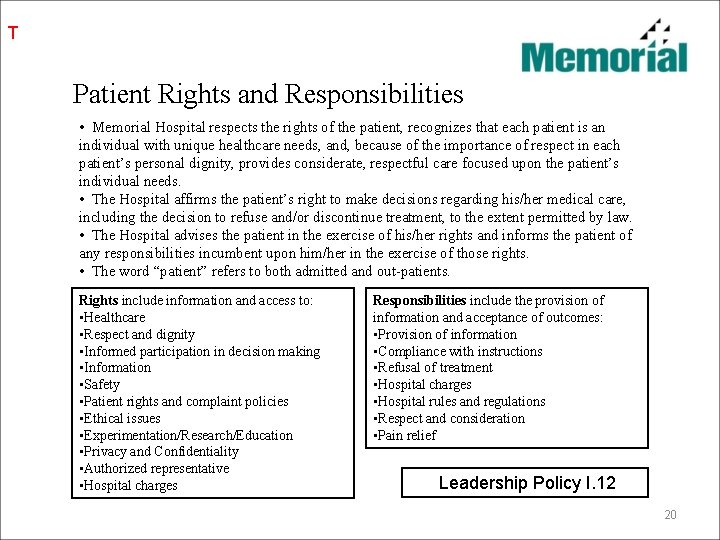
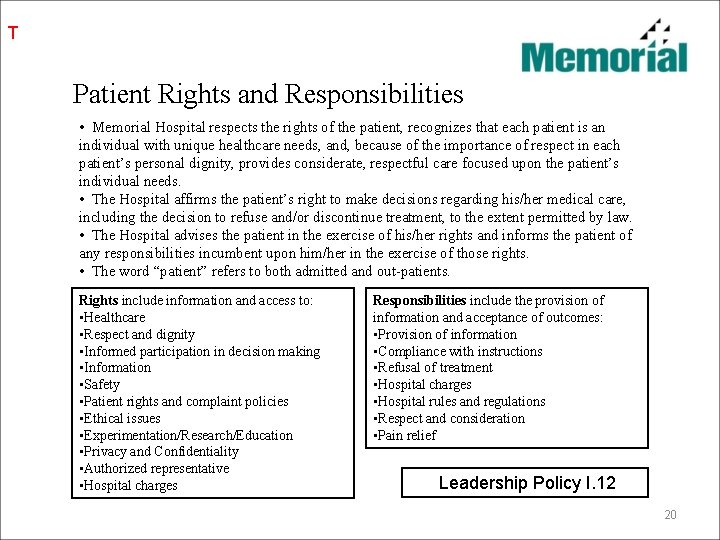
T Patient Rights and Responsibilities • Memorial Hospital respects the rights of the patient, recognizes that each patient is an individual with unique healthcare needs, and, because of the importance of respect in each patient’s personal dignity, provides considerate, respectful care focused upon the patient’s individual needs. • The Hospital affirms the patient’s right to make decisions regarding his/her medical care, including the decision to refuse and/or discontinue treatment, to the extent permitted by law. • The Hospital advises the patient in the exercise of his/her rights and informs the patient of any responsibilities incumbent upon him/her in the exercise of those rights. • The word “patient” refers to both admitted and out-patients. Rights include information and access to: • Healthcare • Respect and dignity • Informed participation in decision making • Information • Safety • Patient rights and complaint policies • Ethical issues • Experimentation/Research/Education • Privacy and Confidentiality • Authorized representative • Hospital charges Responsibilities include the provision of information and acceptance of outcomes: • Provision of information • Compliance with instructions • Refusal of treatment • Hospital charges • Hospital rules and regulations • Respect and consideration • Pain relief Leadership Policy I. 12 20

Informed Consent A. The responsible physician or dentist shall obtain and document proper informed consent as a prerequisite to any procedure or treatment for which it is appropriate. B. Information to be supplied by the doctor to the patient shall include: • an explanation of his/her condition, • a description of the proposed treatment or procedure, • an explanation potential risk and benefits, • an explanation of the potential problems following the treatment or procedure, • an explanation of the potential success or failure, a description of the likely consequences of not performing the treatment or procedure • a description of any reasonable significant alternative to the proposed treatment or procedure. C. The patient shall have an opportunity to have their questions answered by the physician performing the procedure. Medical Staff Rules and Regulations: Medical Records Rule 9 Patient Care Policy: IV. 08 21
Physician Responsibility for Initial and Continued Patient Care • A patient admitted to the hospital shall be evaluated within the first twentyfour (24) hours by either the admitting physician or his/her designated substitute physician and shall be seen every calendar day thereafter. • Each attending physician shall provide adequate coverage for his patients. • Each physician must assure timely, adequate professional care for his patients in the hospital by being personally available through an alternate physician with equivalent clinical privileges. • Failure of an attending physician to meet these requirements may result in loss of clinical privileges. Medical Staff Rules and Regulations: Medical Records Rule 9 and General Patient Care Rule 5 22
Consults • Any qualified medical staff physician with clinical privileges at Memorial Hospital at Gulfport can be called for consultation within his area of expertise. • The attending physician is primarily responsible for requesting consultation when indicated and for calling in a qualified consultant. 1. Should be answered within 24 hours of receipt or notification 2. If consult is refused, the attending physician should be notified as soon as possible • When a STAT physician consult is ordered on a patient there will be: 1. Physician to physician contact – the ordering physician will contact the consulted physician to inform him of the request and provide a brief patient history AND 2. RN to physician contact –the RN caring for the patient will also contact the consulted physician to inform him of the consult, to answer any questions regarding the patient’s condition, and to obtain any order. AND 3. Nursing staff to physician office staff contact- the procedure for office notification that would be done for routine consults should also be followed. Medical Staff Rules and Regulations: Conduct of Care 4. 23
Use of Electronic Medical Record A) Medical staff members shall have electronic access to clinical data related to patients treated by themselves or members of their practice group in the capacity of attending physician, consultant or surgeon via individual physician issued passwords which are not to be shared or disclosed at anytime. B) Medical staff member may complete medical record entries electronically via use of an individual physician issued password and personal identification number (PIN) which is not to be shared or disclosed at anytime. The PIN number shall constitute the full representation of the physician electronic signature. Sharing or intentional disclosure of passwords or PIN numbers constitutes grounds for initiation of corrective action as provided in the Medical Staff Bylaws. C) A medical record shall not be considered complete until all entries have been dated, timed and authenticated. All medical records shall be completed within thirty (30) days of discharge or date of service. Medical Staff Rules& Regulations: General Patient Care Rule 17 24

Completion of History and Physical Examination A) Medical history and physical examination must be completed no more than thirty (30) days before or twenty-four (24) hours after admission or registration, but prior to surgery or a procedure requiring anesthesia services. The medical history and physical examination must be completed and documented by a physician, an oral-maxillofacial surgeon, or other qualified licensed practitioner in accordance with State law and hospital policy. B) An updated examination of the patient, including any changes in the patient’s condition, be completed and documented within twenty-four (24) hours after admission or registration, but prior to surgery or a procedure requiring anesthesia services, when the medical history and physical examination are completed within thirty (30) days before admission or registration. The updated examination of the patient, including any changes in the patient’s condition, must be completed and documented by a privileged physician, an oral-maxillofacial surgeon, or other qualified licensed practitioner in accordance with State law and hospital policy. C) The content of complete and focused history and physical examinations is delineated in the rules and regulations Medical Staff Bylaws: Section 9. 5 -2 25

Integrity of Dictations • Having voice recognition software has allowed for immediate access to important documentation needed for the safe and efficient care of our patients. • We would ask that each of you take the time to review and correct your documents prior to signing. • Remember that when you correct your document you are actually training the software which reduces the chance of the error occurring the next time. • We are aware that you may choose to put a disclaimer regarding voice recognition on your dictations. While there is no problem adding that verbiage, please understand that there is no legal protection provided by this addition of this disclaimer to the document and you are ultimately responsible for the accuracy therein. MEC Action 1 -19 -2016 26

Chain of Command The Chain of Command may be initiated whenever an employee is unable to resolve an immediate clinical, administrative, or safety issue that may affect patient care. Chain of Command for physician issues is as follows: 1. Ordering Physician 2. Attending Physician 3. Medical Staff Department Chairman 4. Chief of Staff or Designee 5. Hospital Chief Executive Officer Medical Staff Rules and Regulations: Conduct of Care 5. 27

Focus Professional Performance Evaluation (FPPE) A. All initial appointments and increases in clinical privileges shall have their first five (5) cases proctored. B. When an increase for clinical privileges is requested and there is no one on the medical staff who currently holds the clinical privilege being requested an external review of the cases will be required. External reviews may also be initiated in cases where conflicts of interest occur. If practitioner is currently performing procedures at another institution, then a letter telling us they are competent could be accepted. C. The methods for proctoring are determined by the Department Chair and include: � Concurrent Chart Review � Retrospective Chart Review � Direct Observation* *With Direct Observation proctoring, the case cannot be scheduled unless the proctor is secured and verified. The proctor may not serve as the first assistant on any surgical procedure. D. The medical staff member may select their proctor; Medical Staff Department Chair will determine if proctor is appropriate prior to the beginning of the process. If no proctor is obtained for direct observation proctoring the Medical Staff Department Chair will be responsible. E. The proctor will forward any of the following outcomes to the Department Chair for review: 1) Unexpected Death 2) Major complication as result of morbidity or increase in length of stay 3) Patient Safety Concern 4) Repetition of complication similar in nature F. Physicians will be notified of the proctoring process via: Initial Appointment Application Letter Request for Modification of Clinical Privilege Form Medical Staff Rules and Regulations 28
Ongoing Professional Practice Evaluation (OPPE) The ongoing maintenance of medical staff clinical privileges is required. The OPPE will look at performance data for practitioners with privileges on an ongoing basis to allow them to take steps to improve performance on a timely basis. The data elements are determined and approved by the Medical Executive Committee with input from the individual Medical Staff Departments. This data will be reviewed by the respective Department Chair (or designee) every nine (9) months for the purpose of determining whether to continue, limit or revoke privileges. Recommendations for limitation or revoking of privileges shall be forwarded to the Medical Executive Committee. The evaluation shall be housed in the practitioner’s peer review file. Data Elements: • Technical Quality of Care • Quality of Service • Peer and Co- worker Relationships • Citizenship • Resource Utilization • Patient Safety Medical Staff Rules and Regulations 29
Medical Staff Officers Chief of Staff – Alton Dauterive, M. D. Vice- Chief of Staff –Charles Slonaker, M. D. Secretary-Treasurer - Joseph Bosarge, M. D. 30
Medical Staff Committees • Medical Executive Committee (MEC) • Credentials • Medical Quality Review (MQRC) • Continuing Medical Education • Joint Conference • Medical Staff Wellness • Bylaws • Executive Operations/Planning Committee Additional committee functions include, but are not limited to: • Pharmacy and Therapeutics • Ethics Each multi-disciplinary committee shall report to: • MEC • MQRC • other medical staff entity, if so designated by the MEC • to any other hospital entity designated by the CEO. Medical Staff By-Laws 31
Chief Medical Officer: Larry Couvillon, MD Chief Medical Information Officer: David Northington, DO 32
Clinical Effectiveness Program • • Service Line Teams Lead by Medical Directors Multidisciplinary Active involvement in medical management of patients, department operations, best practice and evidence based medicine 33
Clinical Effectiveness Program • Current Teams – Surgery – Medicine – Pediatrics – Cardiovascular – Perinatal – Neuro/Ortho/Rehab – Emergency Medicine – Critical Care 34
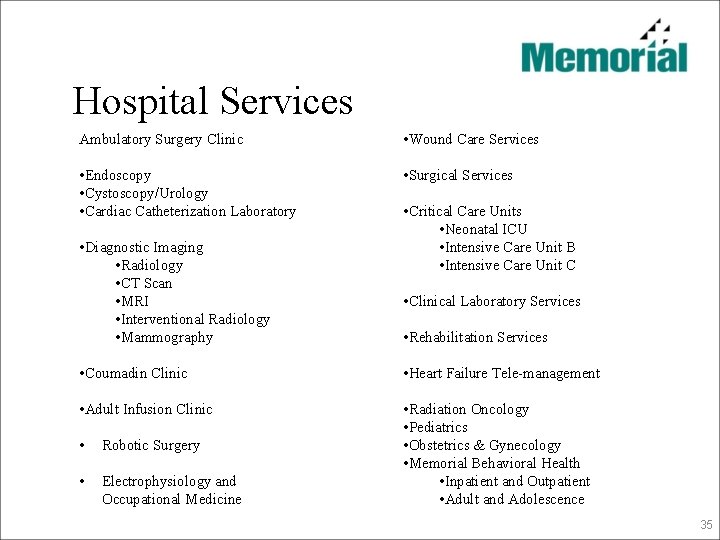
Hospital Services Ambulatory Surgery Clinic • Wound Care Services • Endoscopy • Cystoscopy/Urology • Cardiac Catheterization Laboratory • Surgical Services • Diagnostic Imaging • Radiology • CT Scan • MRI • Interventional Radiology • Mammography • Critical Care Units • Neonatal ICU • Intensive Care Unit B • Intensive Care Unit C • Clinical Laboratory Services • Rehabilitation Services • Coumadin Clinic • Heart Failure Tele-management • Adult Infusion Clinic • Radiation Oncology • Pediatrics • Obstetrics & Gynecology • Memorial Behavioral Health • Inpatient and Outpatient • Adult and Adolescence • Robotic Surgery • Electrophysiology and Occupational Medicine 35
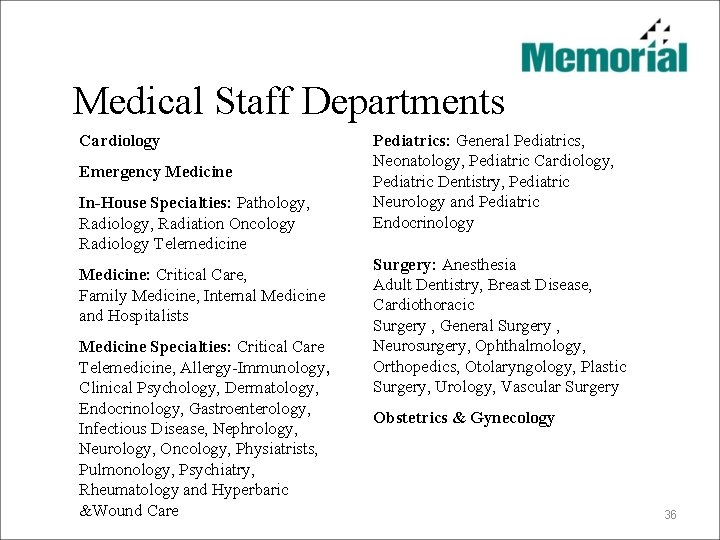
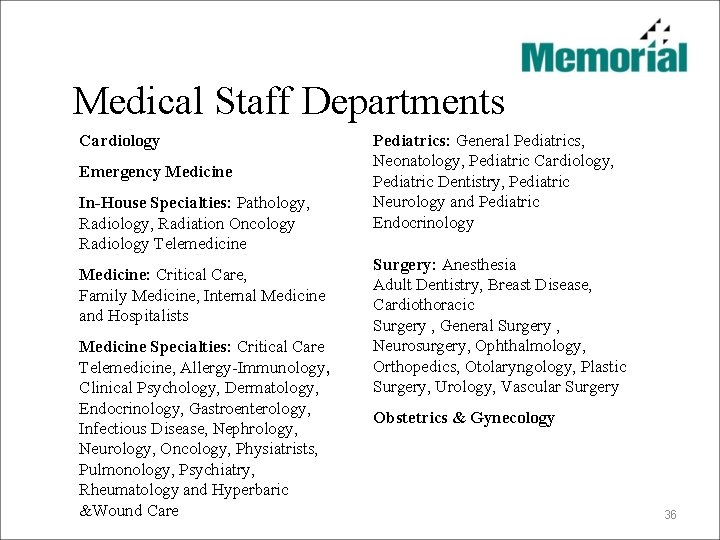
Medical Staff Departments Cardiology Emergency Medicine In-House Specialties: Pathology, Radiology, Radiation Oncology Radiology Telemedicine Medicine: Critical Care, Family Medicine, Internal Medicine and Hospitalists Medicine Specialties: Critical Care Telemedicine, Allergy-Immunology, Clinical Psychology, Dermatology, Endocrinology, Gastroenterology, Infectious Disease, Nephrology, Neurology, Oncology, Physiatrists, Pulmonology, Psychiatry, Rheumatology and Hyperbaric &Wound Care Pediatrics: General Pediatrics, Neonatology, Pediatric Cardiology, Pediatric Dentistry, Pediatric Neurology and Pediatric Endocrinology Surgery: Anesthesia Adult Dentistry, Breast Disease, Cardiothoracic Surgery , General Surgery , Neurosurgery, Ophthalmology, Orthopedics, Otolaryngology, Plastic Surgery, Urology, Vascular Surgery Obstetrics & Gynecology 36
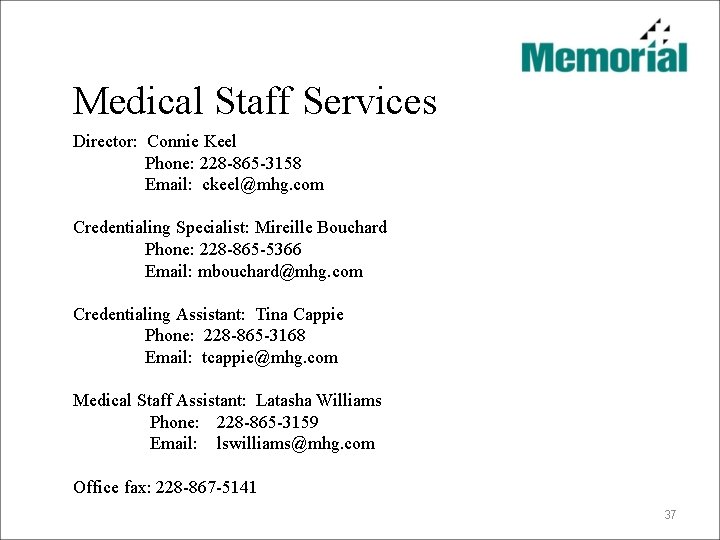
Medical Staff Services Director: Connie Keel Phone: 228 -865 -3158 Email: ckeel@mhg. com Credentialing Specialist: Mireille Bouchard Phone: 228 -865 -5366 Email: mbouchard@mhg. com Credentialing Assistant: Tina Cappie Phone: 228 -865 -3168 Email: tcappie@mhg. com Medical Staff Assistant: Latasha Williams Phone: 228 -865 -3159 Email: lswilliams@mhg. com Office fax: 228 -867 -5141 37
Rules and Regulations Medical Staff By-laws A complete listing of Medical Staff Rules, Regulations and By-Laws were provided on separate electronic media and should be reviewed as a part of the overall process of orientation. 38

Patient Safety Quality of Care 39
T Reporting Safety/Quality Concerns APR. 09. 02. 01 of The Joint Commission Hospital Accreditation Standards Manual indicates that “any individual who provides care, treatment, and services can report concerns about safety or the quality of care to The Joint Commission without retaliatory action from the hospital”. Hospital Accreditation Standards 2012 The Hospital provides a policy and procedure for reporting unusual events and situations in order to monitor, evaluate and improve the quality/performance of medical services offered and the environment of care: • A reportable event or situation is any circumstance that is unexpected within the normal operations of the institution or the anticipated disease/treatment process of a patient. • The subjects of reportable events include patients, visitors, contract/agency staff, and others. • Events are reported electronically via MIDAS, located on each computer. Leadership Manual I. 30 40
Performance Improvement • The purpose of the Quality Assessment and Performance Improvement program is to coordinate the hospital's efforts to maintain or improve the performance of organizational and patient care services. The program is designed to objectively and systematically measure organizational and patient care functions and processes to identify areas where performance improvement efforts could lead to improved patient outcomes/safety and/or improve the value of services provided. • The Medical Staff, in accordance with currently approved medical staff bylaws, shall be accountable for the quality care provided by those individuals with clinical privileges. • The MEC shall receive reports from and assure the appropriate functioning of the medical staff committees. Leadership Policy I. 23 41
CMS’ Value Based Purchasing Program for FY 2016 The outcomes from the areas identified by Medicare regarding the Program have significant financial implications for facility reimbursement. The results can result in up to a 1% re-imbursement return on Medicare accounts. Experience of Care Domain (HCAHPS) (weighted 30 %): • Communication with Nurses • Communication with Doctors • Responsiveness of Hospital Staff • Pain Management • Communication about Medicines • Cleanliness and Quietness of Hospital Environment • Discharge Information • Overall Rating of Hospital. Outcomes Domain (weighted 30 %): • Mortality Measures • Hospital Acquired Condition (HAC) Measures • AHRQ Patient Safety Indicators (PSIs), Inpatient Quality Indicators (IQIs) Composite Measures Efficiency Domain (weighted 20%) • Medicare spending per beneficiary 42
CMS’ Value Based Purchasing Program for FY 2016 Experience of Care Domain (HCAHPS) (weighted 30 %): • The following slide lists a sample of questions that are asked of the patient at the time of the survey post-discharge. • Questions are scored on a 1 – 5 Likert type scale with Always being the 5 rating. Consideration for re-imbursements under the Value Based Purchasing Program is only given for answers that indicate “Always” or a 5 rating. • Percentages that are reported will be evaluated only on the “Always” responses. • Additional questions relate to cleanliness, noise levels, and the likelihood that a patient would recommend the facility for care to others. 43
CMS’ Value Based Purchasing Program for FY 2016 • How often did nurses treat you with courtesy and respect? • How often did nurses listen carefully to you? • How often did nurses explain things in a way you could understand? • How often did doctors treat you with courtesy and respect? • How often did doctors listen carefully to you? • How often did doctors explain things in a way you could understand? • How often was your pain well controlled? • How often did the hospital staff do everything they could to help you with your pain? • How often did hospital staff tell you what the medicine was for? • How often did hospital staff describe possible side effects in a way you could understand? • Did hospital staff talk with you about whether you would have the help you needed when you left the hospital? • Did you get information in writing about what symptoms or health problems to look out for after you left the hospital? 44

. Meaningful Use • Health Information Technology for Economic and Clinical Health Act (HITECH Act or “The Act”) is part of the American Recovery and Reinvestment Act of 2009 (ARRA). • ARRA is commonly known as the Stimulus Bill. • ARRA contains close to $20 billion worth of incentives related to health care information technology in general (e. g. creation of a national health care infrastructure) and contains specific incentives designed to accelerate the adoption of electronic health record (EHR) systems among providers. • Those funds require providers to demonstrate Meaningful Use (“MU”) of said technology, prior to receiving the incentive funds. 45
Meaningful Use Memorial embarked in an aggressive effort to achieve MU status as early as possible to: • Begin the process of moving to an electronic based medical record or HER. • Use components of an HER to improve care. • Begin to create an environment enabling remote and mobile EHR access for physicians. • Offset the cost of acquiring and implementing EHR systems by receiving financial incentive provided in HITECH / ARRA. • Avoid HITECH / ARRA penalties that effect providers who do not meet MU by 2015. 46
Meaningful Use • Memorial achieved MU Stage 1 in the inpatient setting and with over 90% of clinic based eligible providers. • Memorial is in the top 10% of US hospitals in the deployment of EHR technology – source: HIMSS (Healthcare Information Management Systems Society) • Three stages of the reporting requirements Stage 1: 2011 and 2012 - electronic data capture Stage 2: 2013 and 2014 - improve processes Stage 3: 2015 - improve outcomes • Incentive payments paid 2011 -2015, and diminish for participants who begin meeting MU after 2012. Penalties begin in 2015 - reduction in Medicare payments. • If not a “meaningful” user by CY 2015 No incentive payments Penalties will be applied Hospitals -reduction in Market Basket updates Physicians -reduction in fee schedule 2015 - 1% reduction 2016 - 2% reduction 2017 - 3% reduction 2018 - HHS Secretary has discretion 47
Clinical Effectiveness Program (CEP) committees are an integral component of the Quality Assessment/ Process Improvement function. CEP teams are provider led functions that are focused on clinical and operational process improvement within various clinical disciplines: • Critical Care • Emergency Medicine • Surgery • Neuroscience • Mother/Baby • Pediatrics • Medicine • Cardiovascular 48

T Pain Assessment and Management Pain management refers to on-going assessment and treatment of patients experiencing acute or chronic pain. The cycle of pain management includes: • Pain screening/assessment • Pain assessment • Intervention • Re-assessment • Patient education Medication Management Manual Policy VIII. 08 49
T National Patient Safety Goals Included for consideration in regard to NPSG as published by The Joint Commission: • Using full name and date of birth as acceptable forms of patient identification. • Labeling specimen containers in the presence of the patient. • Reducing errors involving the transfusion of blood or blood products. • Critical results reported to provider within one hour. • Medication labeling on and off a sterile field. Applicable to all areas that would work from a sterile field i. e. surgery, interventional radiology, cardiac cath lab. • Safety when administering anti-coagulation therapy. • Medication Reconciliation upon discharge from any patient encounter. • Hand hygiene and Infection Control • Awareness of : 1. Multiple Drug Resistant Organism’s (MDRO) 2. Central Line-Associated Blood Stream Infections (CLABSI) 3. Surgical Site Infection (SSI) 4. Catheter-Associated Urinary Tract Infection (CAUTI) • Identification of patient with risk of suicide • Universal Protocol as applicable to all procedural areas. 50
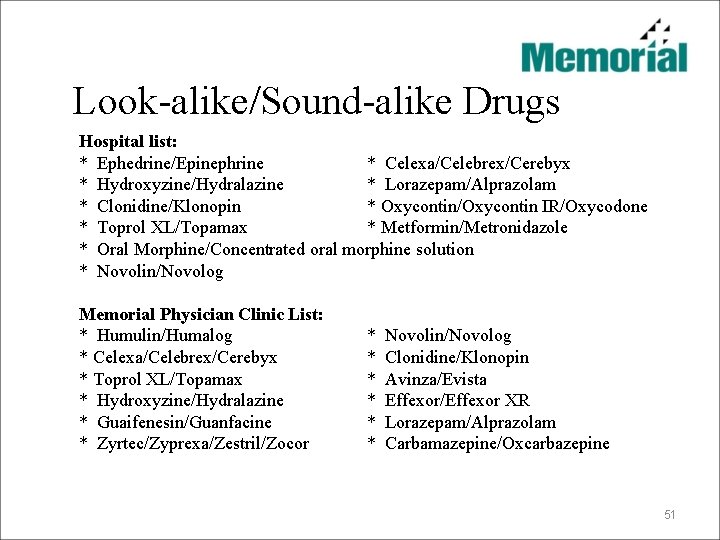
Look-alike/Sound-alike Drugs Hospital list: * Ephedrine/Epinephrine * Celexa/Celebrex/Cerebyx * Hydroxyzine/Hydralazine * Lorazepam/Alprazolam * Clonidine/Klonopin * Oxycontin/Oxycontin IR/Oxycodone * Toprol XL/Topamax * Metformin/Metronidazole * Oral Morphine/Concentrated oral morphine solution * Novolin/Novolog Memorial Physician Clinic List: * Humulin/Humalog * Celexa/Celebrex/Cerebyx * Toprol XL/Topamax * Hydroxyzine/Hydralazine * Guaifenesin/Guanfacine * Zyrtec/Zyprexa/Zestril/Zocor * Novolin/Novolog * Clonidine/Klonopin * Avinza/Evista * Effexor/Effexor XR * Lorazepam/Alprazolam * Carbamazepine/Oxcarbazepine 51
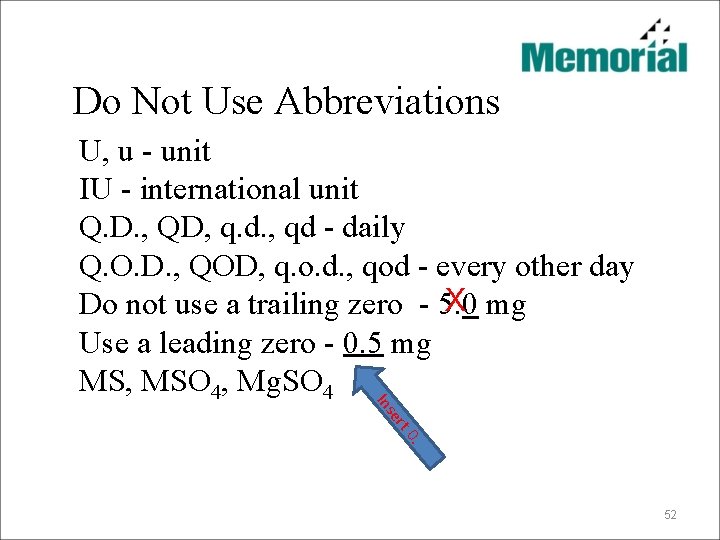
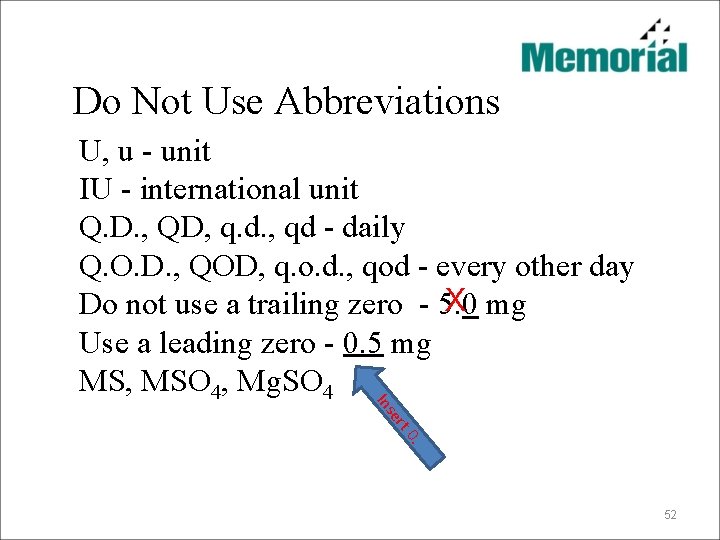
Do Not Use Abbreviations 0. t er Ins U, u - unit IU - international unit Q. D. , QD, q. d. , qd - daily Q. O. D. , QOD, q. o. d. , qod - every other day X Do not use a trailing zero - 5. 0 mg Use a leading zero - 0. 5 mg MS, MSO 4, Mg. SO 4 52
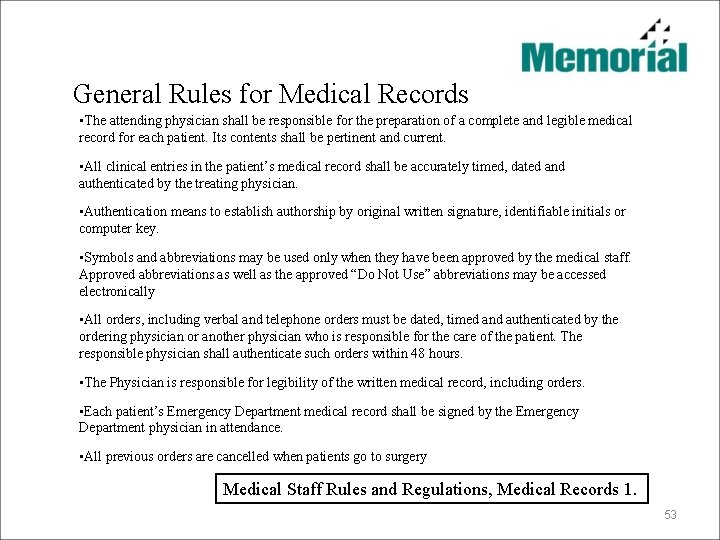
General Rules for Medical Records • The attending physician shall be responsible for the preparation of a complete and legible medical record for each patient. Its contents shall be pertinent and current. • All clinical entries in the patient’s medical record shall be accurately timed, dated and authenticated by the treating physician. • Authentication means to establish authorship by original written signature, identifiable initials or computer key. • Symbols and abbreviations may be used only when they have been approved by the medical staff. Approved abbreviations as well as the approved “Do Not Use” abbreviations may be accessed electronically • All orders, including verbal and telephone orders must be dated, timed and authenticated by the ordering physician or another physician who is responsible for the care of the patient. The responsible physician shall authenticate such orders within 48 hours. • The Physician is responsible for legibility of the written medical record, including orders. • Each patient’s Emergency Department medical record shall be signed by the Emergency Department physician in attendance. • All previous orders are cancelled when patients go to surgery Medical Staff Rules and Regulations, Medical Records 1. 53

Telephone/Verbal Orders • By practical application, verbal orders are strongly discouraged except in situations where no other option is readily available (code 7/provider “scrubbed in”). • Telephone orders are understood to be necessary under certain circumstances, however, also discouraged if not necessary for safe and adequate patient care. • Hospital personnel who are licensed or registered may accept telephone or verbal orders. Telephone and verbal orders should “read back” for clarity before the hospital staff will carry out the order. q write down the order q read back the written order q receive confirmation from the individual who gave the order • Telephone or verbal orders should be date, timed, and authenticated by the physician or his or designee within 48 hours of being given. Patient Care Policy IV. 34 54
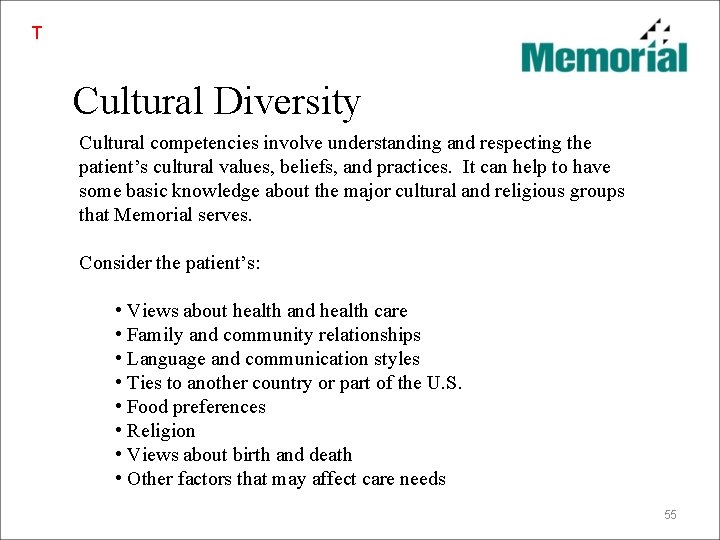
T Cultural Diversity Cultural competencies involve understanding and respecting the patient’s cultural values, beliefs, and practices. It can help to have some basic knowledge about the major cultural and religious groups that Memorial serves. Consider the patient’s: • Views about health and health care • Family and community relationships • Language and communication styles • Ties to another country or part of the U. S. • Food preferences • Religion • Views about birth and death • Other factors that may affect care needs 55
T Special Population Groups At Memorial our focus populations are: Patients needing communication assistance who cannot: • See well • Hear well • Speak or process language • Speak or understand English Bariatric patients: • Those who weigh more than 100 pounds over the desired weight • Have a BMI greater than 40 56

Abuse and Neglect • Memorial Hospital at Gulfport will identify, then report, all cases of suspected abuse, neglect, or exploitation to the appropriate state agency. • Any incident of suspected abuse, neglect, or exploitation should be reported immediately to the appropriate designated delegate. Delegates include: • At Memorial Behavioral Health (MBH) - The Director of Performance Improvement or designee • At the main campus, and all other areas of the hospital - the social worker; there is a rotating "on-call" service in Social Services to handle all calls after hours. Patient Care Policy IV. 11 57
Abuse and Neglect It is important that staff be able to recognize potential signs of abuse, neglect, and/or exploitation of patients. This could potentially be inflected by anyone - a family member, caregiver, friend or hospital employee. The following are the steps which will take place once the call to report the problem is made to the designated delegate. • The designated delegate will interview, in person, the individuals involved to assess the situation. • The designated delegate will coordinate the assessment of the situation and verbal and written reporting requirements with the applicable manager/director of the area and the Manager of Quality/Resource Management or designee. • A verbal report is made to the appropriate state agency within 24 hours. • A written report is sent to the state within 24 -72 hours, depending on the agency requirement. Patient Care Policy IV. 11 58
Organ Donation Policy • Provides guidelines for viable organ/tissue donation when appropriate for patients and their families while maintain ing patient and family dignity, privacy and safety. • The staff of Memorial Hospital recognizes the need for identification of potential organ and tissue donors in Mississippi. • Transplantation can be an effective treatment for some patients. • We participate by providing facilities, personnel and procedures for the recovery of organs and tissue • Mississippi Organ Recovery Agency (MORA) and Mississippi Lyons Eye Bank (MLEB) are the recognized agencies responsible for consent, evaluation and recovery of appropriate organs and/or tissues. Procedures are detailed in Patient Care Policy IV. 05 and attachments A-C. 59

End of Life Considerations Attitudes to Promote Dignity and Respect for the Dying Patient • The patient has a right to be treated with dignity as a living person until the time of death. • The patient has the right to compassionate and competent care delivered by his or her caretakers. • The patient has a right to have his or her symptoms treated to promote relief, including pain. • The patient has the right to express his or her needs without judgment of a caretaker. • The patient has a right to the correct information and honest responses regarding his or her medical condition and care. • The patient has the right for his or her body to be treated respectfully after death occurs. Patient Care Policy IV. 56 60
Rapid Response Team… The Roadrunners • The activation of the Rapid Response Team (RRT) provides a means for additional assessment and interventions to prevent a decline in the patient’s condition. • Any staff member, patient or family member can request assistance from the RRT when rapid assessment and intervention are deemed necessary for a declining patient based on clinical criteria. • The RRT consists of an ICU RN, respiratory therapist, Nursing Supervisor and the primary RN caring for the patient. • Criteria include changes in blood pressure, respirations, heart rate, level of consciousness, shortness of breath, chest pain, decrease in urine output, when the care giver or other feels that something is just not right. Clinical Support Manual, Clinical Support 01. 107 61
T Restraints • Memorial Hospital is committed to preventing, reducing, and striving to eliminate the use of restraints through the use of preventive strategies, use of alternatives, and reallocation of staffing and other resources whenever possible and appropriate. • Restraints may only be used when less restrictive interventions have not been effective in protecting the patient or others. • Patients should not be placed in restraints as a means of coercion, discipline, convenience or retaliation by the staff. • For non-violent, non-self destructive (Medical) patients, restraints may be necessary to promote healing and prevent the confused patient from removing medically necessary catheters and tubes. Patient Care Policy IV. 06 62
T Restraints – continued • When the physician’s order indicates the conditions under which restraints can be discontinued, the order can remain in effect until those conditions are met. • Once restraints are removed, another order is necessary to reapply them. • When orders do not specify indications for discontinuation, orders are effective until the end of the next calendar day. • Orders for restraints to manage violent or self-destructive behavior (Behavioral Health) that jeopardizes the immediate safety of the patient, staff members, or others shall remain in effect until the patient’s behavior or situation is evaluated to no longer require them, but no longer than 4 hours for adults, 2 hours for 9 to 17 year olds, and 1 hours for children under 8 years old. Patient Care Policy IV. 06 63

T Waived Testing • Point of Care testing (POCT) refers to the analytical testing performed outside the clinical lab, but within the organization. • Patient test results from Memorial Hospital at Gulfport are documented in the patient’s medical record. Clinical use of result is consistent with the hospital’s policies and the manufacturer’s recommendation for the test. • Unless otherwise stated, competency and documentation are overseen and maintained by nursing services. Current competency methods for the above tests include at least two of the following: 1. Performing a test on an unknown specimen 2. Observation by a supervisor or qualified personnel 3. The monitoring of each user’s quality control performance 4. A written test that is specific to the method • Documentation of the identity of staff members who perform testing or who supervise testing is kept by the lab and/or nursing service. Supervision of testing is under the direction of the RN’s or RN designee. Laboratory Reference Guide. 10 / TJC HAS Waived Testing 64

Infection Control and Prevention 65
T Infection Control Program • The Infection Control Program is hospital-wide, encompassing all patient care, and patient support departments and services including in-patient, out-patient, behavioral health, and ambulatory services, and physician clinics. • The Program includes information and direction for executing evidence based outcome procedures and for conformation with advisory/regulatory agencies including, but not limited to: • The Joint Commission • Occupational Health and Safety Agency • Centers for Disease Control and Prevention • Institute for Healthcare Improvement The Infection Control Plan covers subjects including: • Hand Hygiene – includes ongoing monitoring of the use of alcohol-based hand cleanser and the use of soap and water for hand hygiene. • Standard Precautions • Isolation • Blood-borne Pathogen Exposure Control Plan • TB Control Plan • Employee Health Infection Control Manual 66
T Isolation Precautions Transmission based precautions are to be used for patients documented or suspected to be infected with highly transmissible or epidemiologically important pathogens for which additional precautions beyond standard precautions are needed to interrupt transmission. There are three types of transmission-based precautions: 1. Contact Precautions 2. Droplet Precautions 3. Airborne. Precautions They may be combined together as needed for diseases that have multiple routes of transmission. When used either singularly or in combination, they are to be used in addition to standard precautions. Infection Control Manual 67
T Multiple Drug Resistant Organisms Goals: • Reduce or prevent health-care associated infections from MDROs • Educate staff about: • Educate patients/families who are infected or colonized with an MDRO Healthcare associated infections (HAIs) MDROs Prevention Strategies: • Hand hygiene • Contact precautions • Cleaning and disinfecting • Educate staff upon hire and annually • Patient/family education (utilize Krames educational handouts) 68

T Central Line-Associated Bloodstream Infections (CLABSI) Goals: • Implement best practices for preventing CLABSIs - includes both short and long term central and peripherally inserted venous access devices (Central lines and PICC lines) Strategies: • Implement policies and practices aimed at reducing the risk of CLABSIs • Institute for Healthcare Improvement Central Line Insertion Bundles • Educate staff upon hire and annually • Patient/family education (utilize Krames educational handouts) 69
T Surgical Site Infections (SSI) • An infection of a surgical incision that occurs within 30 days after the operative procedure; also includes infection of surgical implants, which can be counted up to 1 year post-op Goals: • Implement best practices for preventing surgical site infections (SSIs) Strategies: • Implement policies and practices aimed at reducing the risk of SSIs • Educate staff upon hire and annually • Patient/family education prior to all surgical procedures (utilize Krames educational handouts) 70
T Catheter Associated Urinary Tract Infections (CAUTI) • This is a new National Patient Safety Goal for 2012 and is expected to be fully implemented, per the Joint Commission, by January 1, 2013. • Insert indwelling catheters according to established evidence-based guidelines: o Insert catheters only for appropriate indications o Leave catheters in place only as long as medically needed • Manage indwelling urinary catheters according to established evidencebased guidelines. • Measure and monitor catheter-associated urinary tract infection prevention processes and outcomes in high volume areas. (This goal is not applicable to pediatric populations. ) 71
T Universal Protocol The three components of Universal Protocol include: • Pre procedure verification • Marking the operative site (when applicable) • Time out 72
T Universal Protocol Pre-procedure Verification of correct person, procedure, and site should occur: • when the procedure is scheduled • at the time of admission/entry • at pre-admission testing or assessment The verification should occur with the patient involved, awake and alert, if possible, and before the patient leaves the pre-op area or enters the procedure room. 73
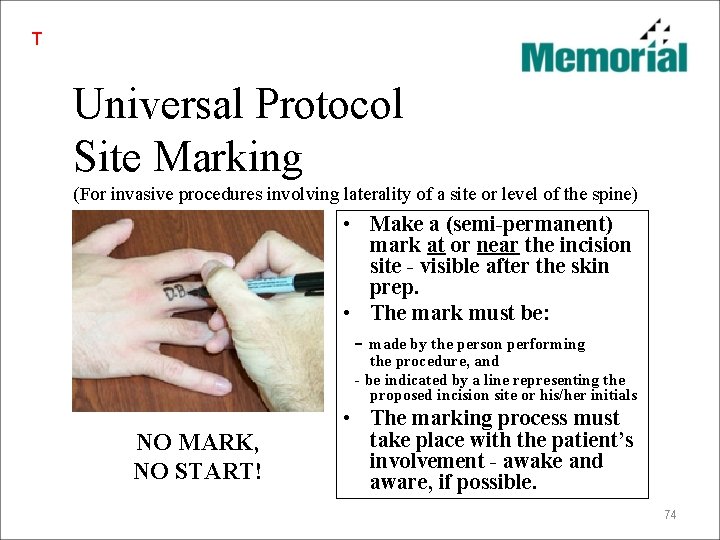
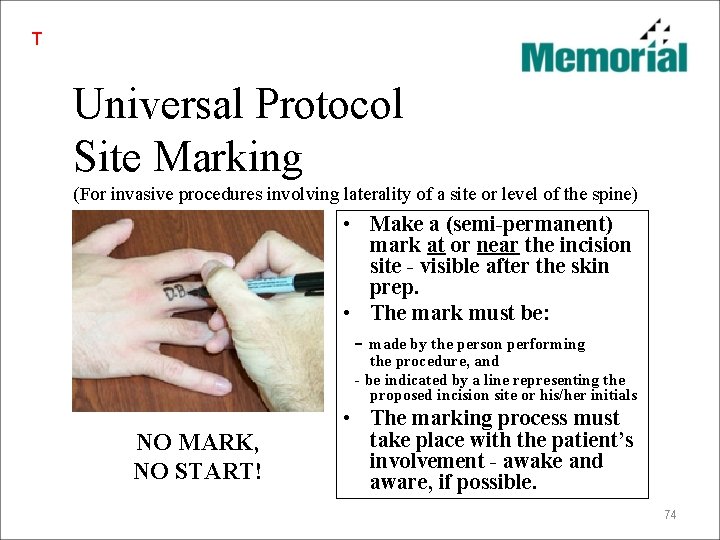
T Universal Protocol Site Marking (For invasive procedures involving laterality of a site or level of the spine) • Make a (semi-permanent) mark at or near the incision site - visible after the skin prep. • The mark must be: - made by the person performing the procedure, and - be indicated by a line representing the proposed incision site or his/her initials NO MARK, NO START! • The marking process must take place with the patient’s involvement - awake and aware, if possible. 74

T Universal Protocol Time Out Before starting an invasive procedure, conduct a final assessment process, known as “Time Out” to confirm: • Correct patient • Correct site • Correct procedure Other elements that may be addressed include: • Relevant images and results displayed • The need for antibiotics or fluids for irrigation • Safety precautions based on patient history or medication use • Consent form, accurate and completed • Correct patient position *The “time out” involves all members of the procedure team, and requires interactive verbal communication to ensure confirmation of the above elements. 75

Safety/Security 76
T All components of emergency and/or security operations can be found by accessing the Emergency Operations Plan of Memorial Hospital of Gulfport and should be reviewed by all employees. Security Hospital security during abnormal situations is critical to both staff and patient safety. No Hospital can expect to operate effectively without the expectations that security programs and procedures are in place. Security is especially critical during prolonged emergencies that are generated as a result of terrorism or other unlawful activities. The ability to control personnel movement into and out of the Hospital is paramount to efficiency and effectiveness. Hospital security during routine or non-emergency situations can be handled with minimal staffing, but such staffing must consist of personnel who are trained for such duties. Based on established agreements, security of the Hospital during normal operations will be performed by security personnel. However, during abnormal or emergency situations, augmentation of security personnel may be supported by other designated hospital employees or by local law enforcement agencies. Emergency Operations Plan: Safety and Security 77
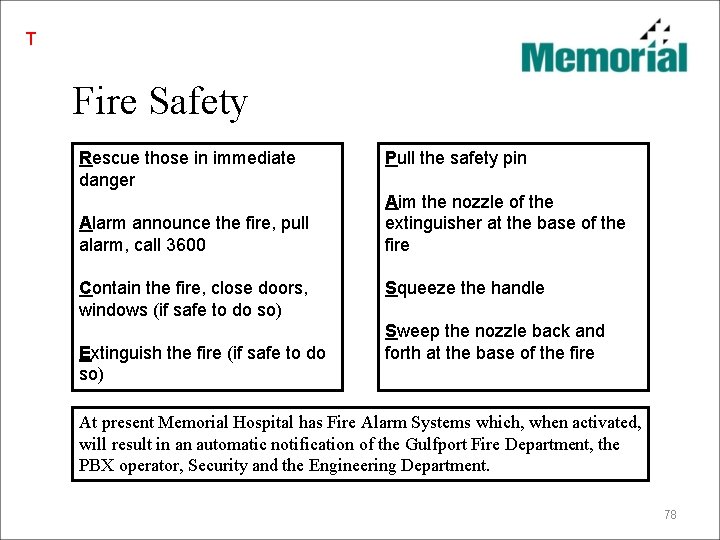
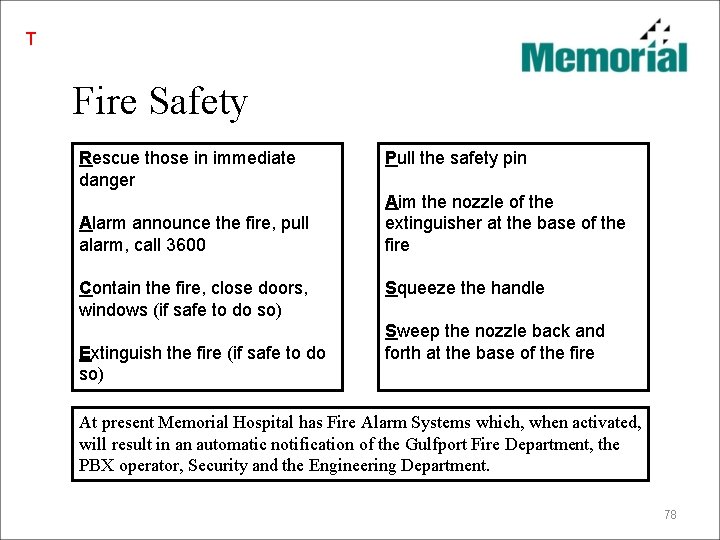
T Fire Safety Rescue those in immediate danger Alarm announce the fire, pull alarm, call 3600 Contain the fire, close doors, windows (if safe to do so) Extinguish the fire (if safe to do so) Pull the safety pin Aim the nozzle of the extinguisher at the base of the fire Squeeze the handle Sweep the nozzle back and forth at the base of the fire At present Memorial Hospital has Fire Alarm Systems which, when activated, will result in an automatic notification of the Gulfport Fire Department, the PBX operator, Security and the Engineering Department. 78
T Hurricane Alert Status MHG Hurricane Alert Status (HAS) When a major tropical storm or a hurricane threatens the Mississippi Gulf Coast, the Hospital President/CEO or his designee may place the hospital in a Hurricane Alert Status, depending on the projected landfall and severity of the storm. When HAS is implemented, all departments will activate the Hurricane Alert Status Tasking as outlined in the Disaster Management Plan. Incident Annex: Tropical Cyclones 79

T Hurricane Alert Status You are reminded that you are responsible for: • Arranging appropriate call coverage if your name appears on the schedule for unreferred call during the dates of a hurricane’s projected landfall. • Arranging appropriate coverage for your private patients. You are also responsible for the above immediately following the storm. • If you are on the unreferred call list for any dates surrounding possible landfall of a hurricane, Medical Staff Services will be contacting you to relay important information you will need before reporting to the hospital. Incident Annex: Tropical Cyclones 80
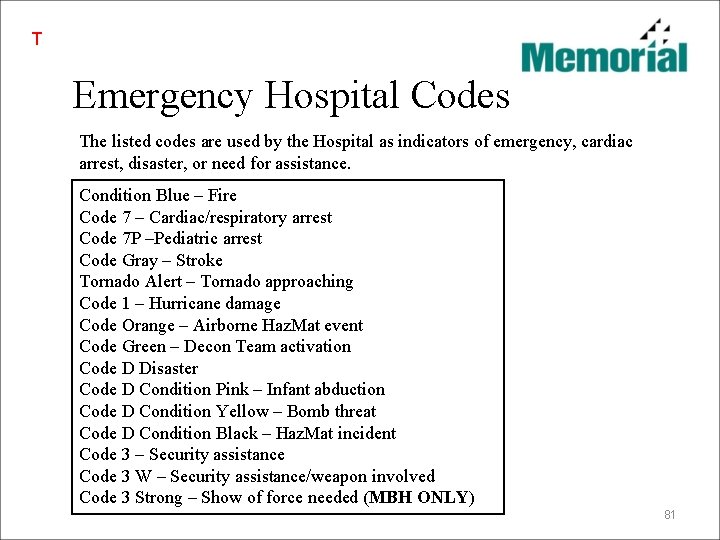
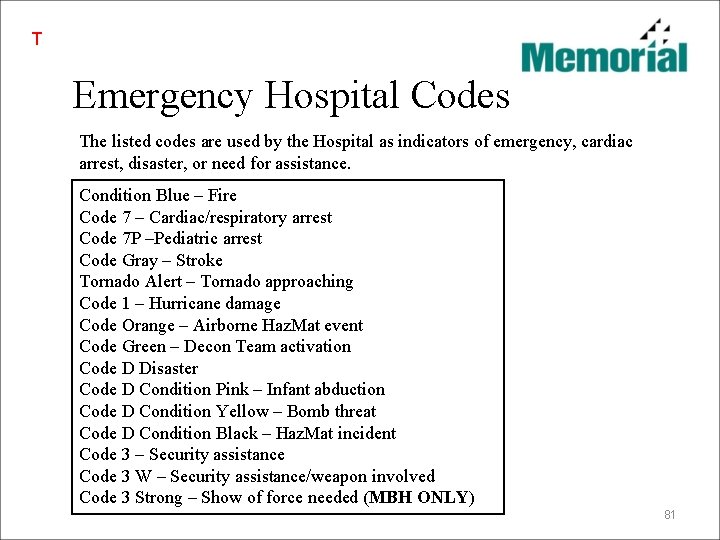
T Emergency Hospital Codes The listed codes are used by the Hospital as indicators of emergency, cardiac arrest, disaster, or need for assistance. Condition Blue – Fire Code 7 – Cardiac/respiratory arrest Code 7 P –Pediatric arrest Code Gray – Stroke Tornado Alert – Tornado approaching Code 1 – Hurricane damage Code Orange – Airborne Haz. Mat event Code Green – Decon Team activation Code D Disaster Code D Condition Pink – Infant abduction Code D Condition Yellow – Bomb threat Code D Condition Black – Haz. Mat incident Code 3 – Security assistance Code 3 W – Security assistance/weapon involved Code 3 Strong – Show of force needed (MBH ONLY) 81

• Additional information regarding the specific operations of various clinical areas will be provided as determined by Clinical Directors. • Training for Computerized Physician Order Entry (CPOE) will also be scheduled. • Slides identified with a “T” in the upper left hand corner represent information required by The Joint Commission for hospital orientation. 82
I, ___________, hereby attest Print Name I have reviewed the content of the Medical Staff Orientation _____________________ Signature _____________________ Date Please return this signed document to Medical Staff Services with your completed application for Medical Staff Membership and Clinic Privileges For questions, please contact Pat Warner, Librarian At 228 -865 -3616 or pwarner@mhg. com 83
 Torrance memorial human resources
Torrance memorial human resources Deepak memorial hospital
Deepak memorial hospital Quentin burdick memorial hospital
Quentin burdick memorial hospital Memorial christian hospital
Memorial christian hospital Chipping norton war memorial hospital
Chipping norton war memorial hospital Shaukat khanum memorial cancer hospital and research centre
Shaukat khanum memorial cancer hospital and research centre Mackay memorial hospital
Mackay memorial hospital Umass memorial pharmacy
Umass memorial pharmacy 100 bedded hospital staff requirements
100 bedded hospital staff requirements Lynfield mount hospital
Lynfield mount hospital Objective of hospital pharmacy
Objective of hospital pharmacy Ethnocentric polycentric
Ethnocentric polycentric Ucsf
Ucsf Florida association of medical staff services
Florida association of medical staff services Northside hospital new hire orientation
Northside hospital new hire orientation Green eggs early childhood centre
Green eggs early childhood centre Welcome to parent orientation
Welcome to parent orientation Welcome to parent orientation
Welcome to parent orientation Welcome speech for kindergarten parent orientation
Welcome speech for kindergarten parent orientation Welcome welcome this is our christmas story
Welcome welcome this is our christmas story Tcm hospital malaysia
Tcm hospital malaysia Kaohsiung medical university hospital
Kaohsiung medical university hospital Ninewells hospital and medical school
Ninewells hospital and medical school Six sigma at academic medical hospital case analysis
Six sigma at academic medical hospital case analysis National ambulatory medical care survey
National ambulatory medical care survey Doctors in north central washington
Doctors in north central washington Ptal california medical board
Ptal california medical board Gbmc medical records
Gbmc medical records Hepburn osteometric board
Hepburn osteometric board Cartersville medical center medical records
Cartersville medical center medical records Voluntary health agencies
Voluntary health agencies Wiggins library
Wiggins library Wwjh
Wwjh Eucharistic prayer
Eucharistic prayer Turning point suffragist memorial
Turning point suffragist memorial Hubert kairuki memorial university faculty of medicine
Hubert kairuki memorial university faculty of medicine Anton anderson tunnel
Anton anderson tunnel Jan marek memorial
Jan marek memorial Keshav sita memorial foundation trust
Keshav sita memorial foundation trust Suvinil nó de marinheiro
Suvinil nó de marinheiro Entrudo memorial do convento
Entrudo memorial do convento Dennis h mahan memorial bridge
Dennis h mahan memorial bridge Memorial tree tags
Memorial tree tags Memorial middle school la joya isd
Memorial middle school la joya isd Memorial do convento capitulos
Memorial do convento capitulos Trinity beach memorial
Trinity beach memorial Lincoln memorial university college of veterinary medicine
Lincoln memorial university college of veterinary medicine Alison weir
Alison weir Anzac day quotes and poems
Anzac day quotes and poems Jefferson monument 5 whys
Jefferson monument 5 whys Torrance memorial cardiac rehab
Torrance memorial cardiac rehab Memorial cards ballincollig
Memorial cards ballincollig Barnhill
Barnhill International health agencies
International health agencies What are toponyms ap human geography
What are toponyms ap human geography American gothic painting
American gothic painting William knibb memorial high school
William knibb memorial high school Queen isabella memorial bridge
Queen isabella memorial bridge Larissa gordon
Larissa gordon Masaryk memorial cancer institute
Masaryk memorial cancer institute Chang pui chung memorial school
Chang pui chung memorial school St malachy's memorial high school
St malachy's memorial high school National military memorial park
National military memorial park Manchester memorial elementary school
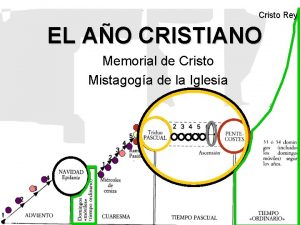
Manchester memorial elementary school Memorial de cristo
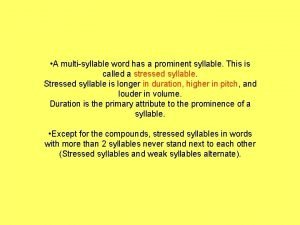
Memorial de cristo Memorial stressed syllable
Memorial stressed syllable Mustang way
Mustang way Geological engineering ubc
Geological engineering ubc Arrival form mun
Arrival form mun Olcott memorial higher secondary school
Olcott memorial higher secondary school Autism background
Autism background Jefferson memorial root cause analysis
Jefferson memorial root cause analysis Jefferson memorial root cause analysis
Jefferson memorial root cause analysis Pro fide et patria
Pro fide et patria Liu po shan memorial college
Liu po shan memorial college Leonardo sarao picture
Leonardo sarao picture Memorial square coalville
Memorial square coalville Slslib
Slslib Vimy ridge memorial
Vimy ridge memorial Fanwood memorial
Fanwood memorial Black childrens memorial
Black childrens memorial Satish chandra memorial school
Satish chandra memorial school Bbc bitesize maccaig
Bbc bitesize maccaig The tanaka memorial
The tanaka memorial