Hearing Our Voices An Indigenous Trauma Aware Womens


- Slides: 37
Hearing Our Voices: An Indigenous Trauma Aware Women’s Practice Reproductive Health Curriculum 22 November 2019 www. nurture-north. org Lisa Bishop and Naana Jumah
Disclosures Lisa Bishop • Nothing to disclose Naana Jumah • Member of the OB/GYN LEG
Patient Encounter • You have a busy clinic with several new antenatal patients. To help make clinic more efficient, your colleague has a form for new antenatal patients to complete while they are waiting. The form contains most of the history found on the perinatal record. • Your clinic has been running behind schedule for the past few weeks, so you decide to try out your colleague’s antenatal form. • Your clinic assistant passes you the form for your next patient and there are quite a few blanks on the form. 3
Patient Encounter 4
Patient Encounter Continued You leave that appointment feeling frustrated and confused. The patient barely talked, she wouldn’t look at you and she hardly answered any questions. You hope that you can bring her out of her shell more at her next visit. 5
Patient Encounter Continued The patient does not return for her follow up appointment. 6
“Trauma is when we have encountered an out of control, frightening experience that has disconnected us from all sense of resourcefulness or safety or coping or love. ” ~Tara Brach, 2011
Trauma affects individuals of all ages, socio-economic status, cultures, religions and sexual orientations (including lesbian, gay, bisexual, transgender and two spirit*). *“Two-spirit” is an Aboriginal term referring to those who have both male and female spirits.
Families can be traumatized by an event happening to one or more of its members. Even people who did not directly experience the trauma can be impacted by it, especially if they have a close relationship to the individual who experienced the trauma.
Service providers can be traumatized after hearing the stories and witnessing the suffering of clients who have experienced trauma. This is called “vicarious trauma” or “trauma exposure response, ” and it happens when the provider is regularly confronted by traumatic content.
Communities can be traumatized when events effect any of its members.
Cultures can be traumatized when repeated denigration, attempts at assimilation and genocide occur.
Intergenerational Trauma “A collective complex trauma inflicted on a group of people who share a specific group identity or affiliation—ethnicity, nationality, and religious affiliation. It is the legacy of numerous traumatic events a community experiences over generations and encompasses the psychological and social responses to such events. ” Evans-Campbell, T. (2008). Historical trauma in American Indian/Native Alaska communities: A multilevel framework for exploring impacts on individuals, families, and communities. Journal of Interpersonal Violence, 23(3), 316 -338.
Impact of Traumatic Experiences
Trauma as a Worldview The impact of traumatic events does not simply go away when they are over. Instead, traumatic events are profound experiences that can shape the way a person sees themselves, others and the world.
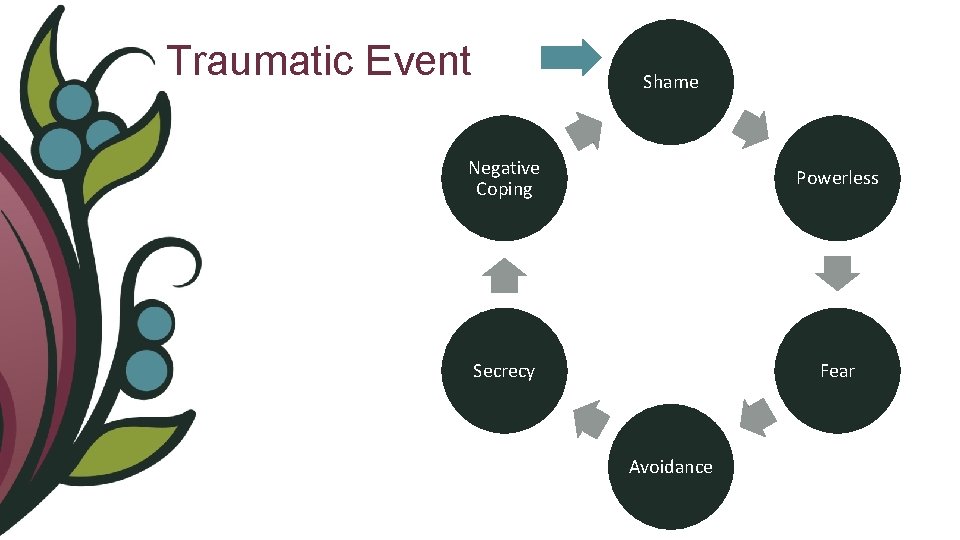
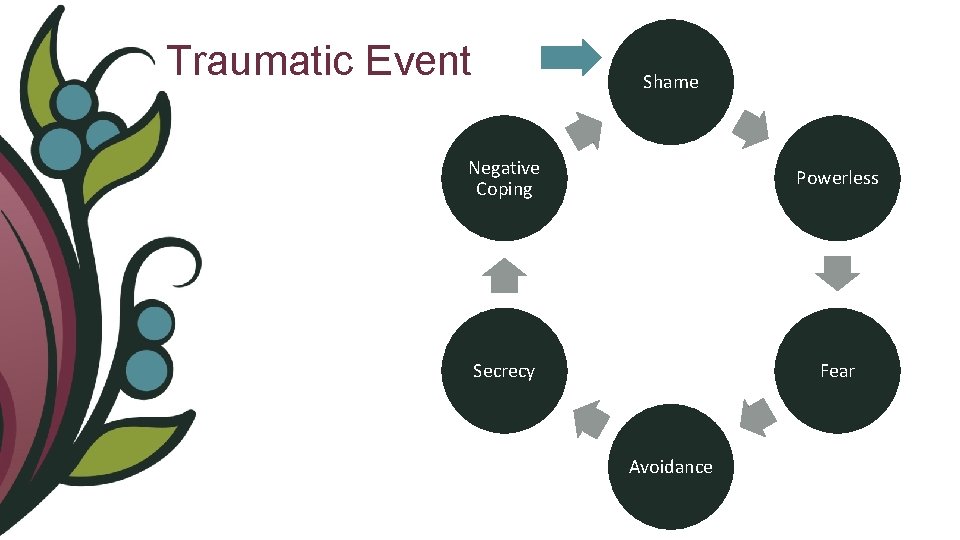
Traumatic Event Shame Negative Coping Powerless Secrecy Fear Avoidance
Neurobiology of Trauma The traumatic experience results in physiologic changes in areas of the brain responsible for emotion, memory and survival instincts (the amygdala and the hippocampus) and in areas that regulate emotions, decision making and personality (the prefrontal cortex) Bremner 2006. Traumatic stress and the brain. Dialogues in Clinical Neuroscience. 8(4): 445 -461
Trauma as a Survival Mechanism Blocking the traumatic experience from memory, or trying to avoid any reminders of the trauma is a survival mechanism. This results in a lack of integration of the traumatic experience, such that it becomes the experience in a person’s life, rather than one of many.
Trauma as a Framework for Life The trauma becomes the organizing principle from which the person lives their life always trying to cope with and/or avoid the impact of the trauma. This can be both a conscious and unconscious awareness/experience. This lack of processing of the trauma means that it is ever-present for the individual, and they feel as if the trauma happened yesterday when it could have been months or many years since.
Trauma and PTSD Most people who experience traumatic events do not go on to develop symptoms of Post-Traumatic Stress Disorder (PTSD). However, for many people, poor mental and physical health, depression and anxiety can become the greater challenge.
Trauma Aware Practice 21

Trauma as Public Health Issue
Trauma & Reproductive Health For patients who have experienced trauma, questions about pregnancy, sexual practices, sexually transmitted infections etc. can make the patient feel vulnerable. The process of explaining these intimate parts about themselves can cause the patient to be retraumatized both by the experience they had and the interaction with their health care provider. 23
Re-traumatization When re-traumatization happens, the system has failed the individual who has experienced trauma, and this can leave them feeling misunderstood, unsupported and even blamed. It can also perpetuate a damaging cycle that prevents healing and growth.
Creating Safer Spaces It is our responsibility as health and social service providers to create a safe space for our patients / clients. This includes recognizing that there is an inherent power imbalance between a care provider and a patient/client
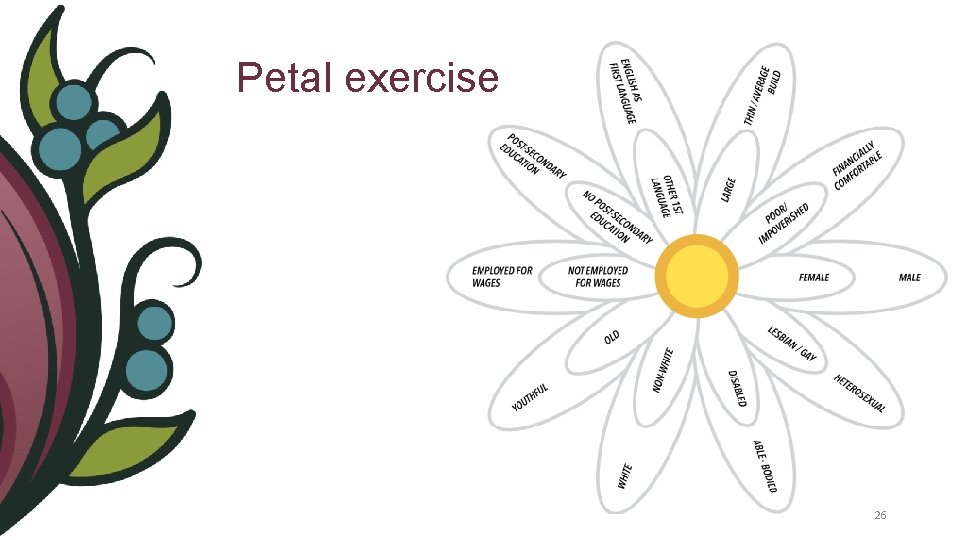
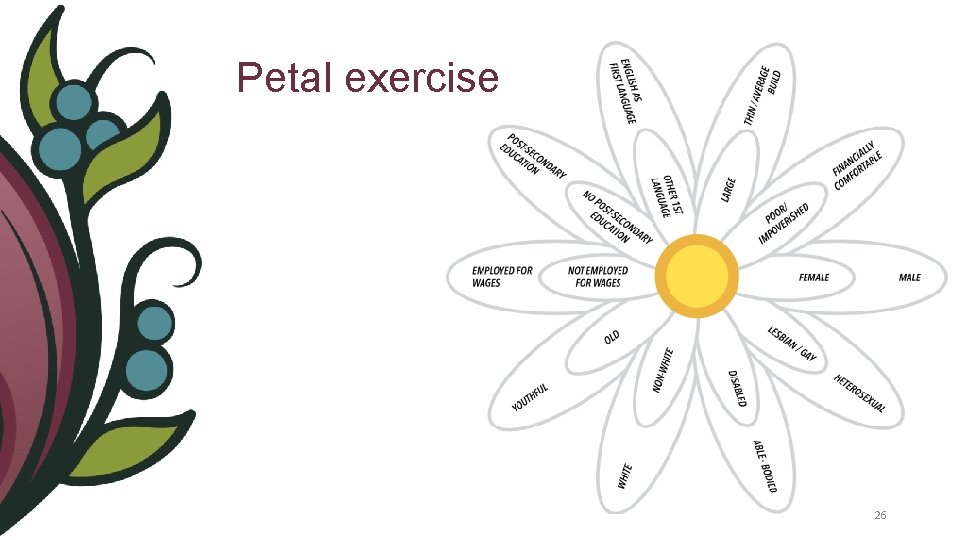
Petal exercise 26
Reframing the Conversation Viewing trauma as an injury shifts the conversation from asking “What is wrong with you? ” to “What has happened to you? ”
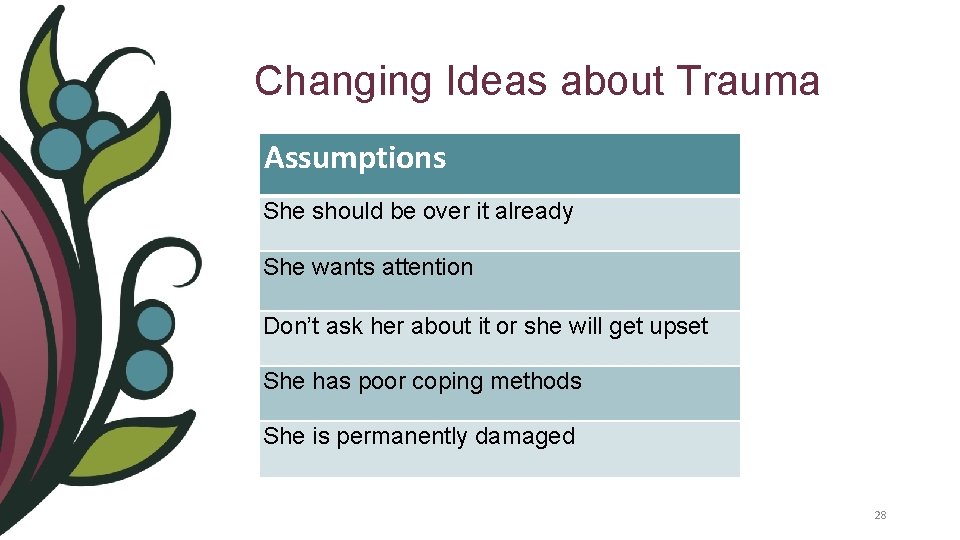
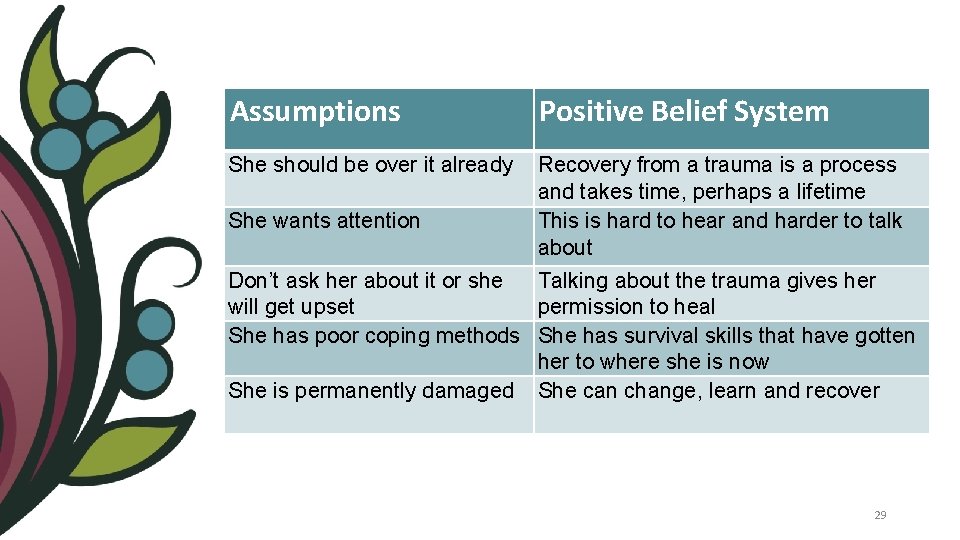
Changing Ideas about Trauma Assumptions She should be over it already She wants attention Don’t ask her about it or she will get upset She has poor coping methods She is permanently damaged 28
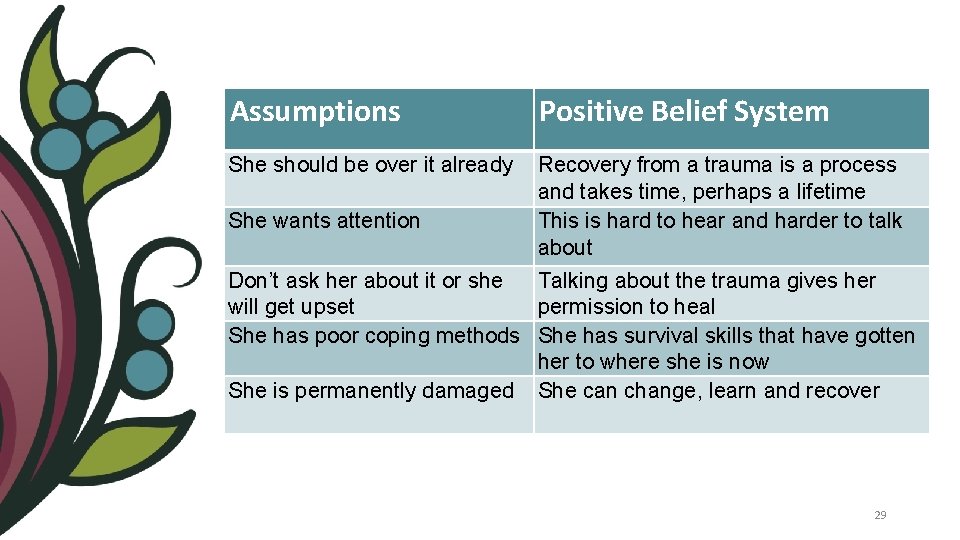
Assumptions Positive Belief System She should be over it already Recovery from a trauma is a process and takes time, perhaps a lifetime This is hard to hear and harder to talk about She wants attention Don’t ask her about it or she Talking about the trauma gives her will get upset permission to heal She has poor coping methods She has survival skills that have gotten her to where she is now She is permanently damaged She can change, learn and recover 29
Resilience & Recovery Just as we spend time and energy focusing on the impact of trauma, we must spend equal time on how people survived the experience, the strengths they have developed from having survived it, and how that resiliency has or will help in their recovery.
Resilience & Recovery Shows individuals who have experienced trauma that they do have the skills they need to heal and recover. To identify and access these skills, they need to reframe their coping behaviours and knowledge from weakness to strength. *** As service providers, we play a very important role in assisting individuals to develop a new trauma-informed lens of practice.
Self Compassion Validating resilience is important, even when past coping behaviours are now causing problems. Understanding a symptom as an adaptation reduces the guilt and shame that is so often associated with trauma. It also increases a person’s capacity for selfcompassion, and provides a guideline for developing new skills and resources so that new and better adaptations can be developed for the current situation (Elliot et al. , 2005).
Trauma Aware Basics • Develop rapport with your patient / client • Create a safe space for your patient / client • Let patients / clients know what you would like to talk about • Ask permission • Explain what you are doing • Don’t be afraid to ask about trauma. . . But for a purpose 33
Patient Encounter Revisited 34
Patient Encounter Debrief 35
Summary - Trauma Aware Care • Assume every women in your practice has experienced trauma • Recognize that there is an inherent power imbalance between the care provider and a patient/client • Make the distinction between who she is as a human being and what has happened to her • Work from a resilience-minded perspective helps people who have experienced trauma to realize that they do have the skills they need to heal and recover Trauma-informed, The Trauma Toolkit Second Edition, 2013. Klinic Community Health 36 Centre

Hearing Our Voices: An Indigenous Miigwetch! Women’s Thank you! Reproductive Health Curriculum www. nurture-north. org
 Womens shelter edmonton
Womens shelter edmonton Late night womens hour
Late night womens hour Womens community shelters
Womens community shelters Womens college kumbakonam
Womens college kumbakonam Women's rights
Women's rights Aylesbury womens aid
Aylesbury womens aid Scarborough womens centre
Scarborough womens centre Ballybeen womens centre
Ballybeen womens centre Womens college kumbakonam
Womens college kumbakonam Womens ministry activities
Womens ministry activities Female sex anatomy diagram
Female sex anatomy diagram Womens right
Womens right Girls lacrosse helmets
Girls lacrosse helmets Womens right
Womens right Womens rights
Womens rights Womens history month door
Womens history month door Differences between men's and women's soccer
Differences between men's and women's soccer Bristol womens voice
Bristol womens voice Hope for the silent voices
Hope for the silent voices Youth voices
Youth voices Hark ten thousand voices crying
Hark ten thousand voices crying Hark ten thousand voices crying
Hark ten thousand voices crying Stefanie klose
Stefanie klose Faces and voices of recovery uk
Faces and voices of recovery uk Many voices one world
Many voices one world What is voice
What is voice Young voices toronto
Young voices toronto Men's voices ireland
Men's voices ireland Characteristic of realism
Characteristic of realism 5 voices assessment
5 voices assessment The enjoyment of music 12th edition
The enjoyment of music 12th edition Have you heard the sound of the angel voices
Have you heard the sound of the angel voices Voices from the dust bowl
Voices from the dust bowl Verb.oo
Verb.oo Hark ten thousand voices crying
Hark ten thousand voices crying What is indigenous research
What is indigenous research Pristinity
Pristinity Indigenous education in nigeria
Indigenous education in nigeria