Gout ASAD KHAN CONSULTANT RHEUMATOLOGIST HEART OF ENGLAND




- Slides: 26

Gout ASAD KHAN CONSULTANT RHEUMATOLOGIST HEART OF ENGLAND NHS FOUNDATION TRUST
Overview Background Diagnosis Risk factors Acute treatment Long-term treatment Pseudogout
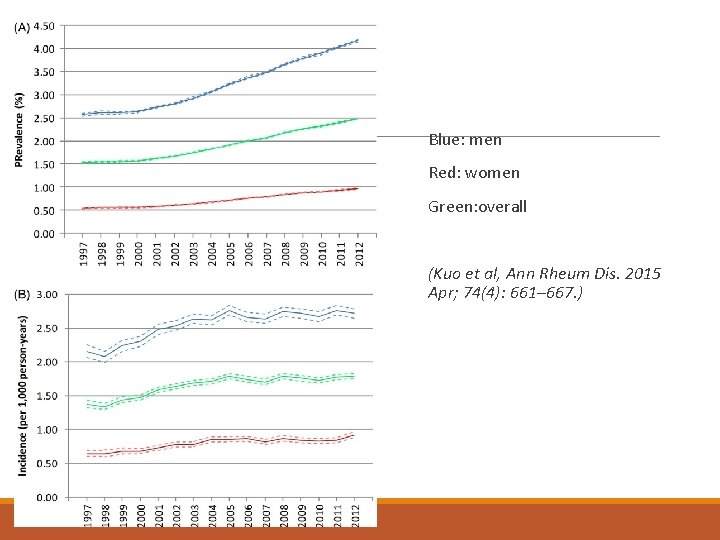
Gout Inflammatory arthritis due to monosodium urate crystal deposition Presents with acute self-limiting attacks of severe pain Chronic – causes tophaceous deposits, joint damage and chronic pain Rising prevalence (2. 49% in 2012) Curable!
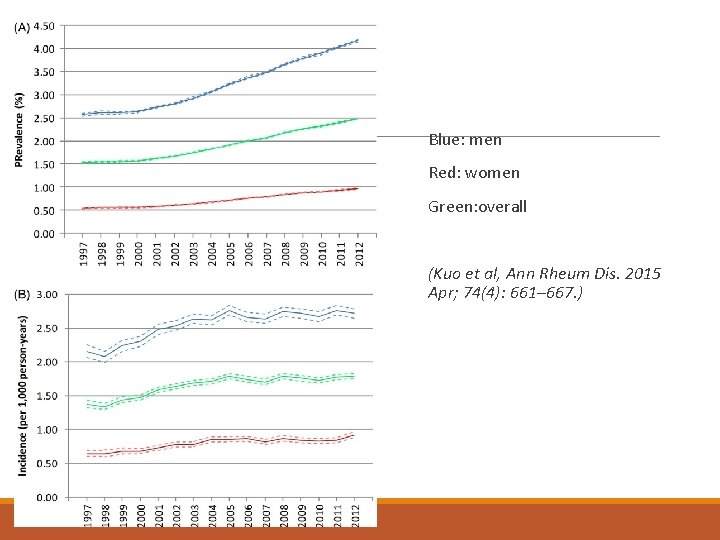
Blue: men Red: women Green: overall (Kuo et al, Ann Rheum Dis. 2015 Apr; 74(4): 661– 667. )
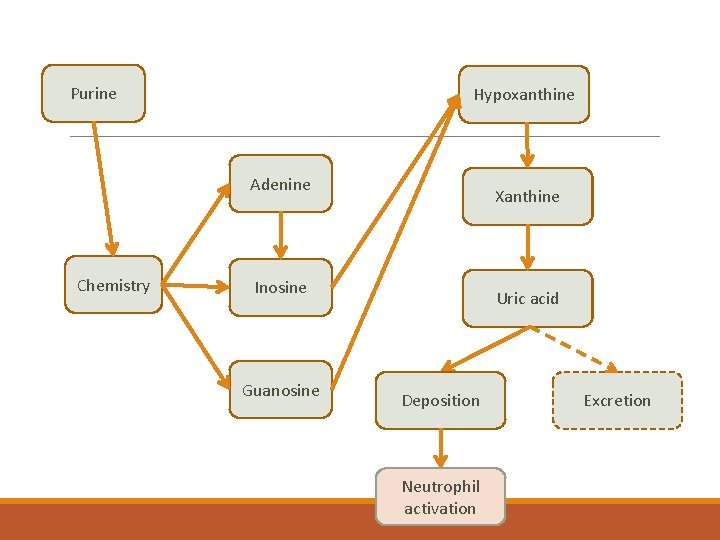
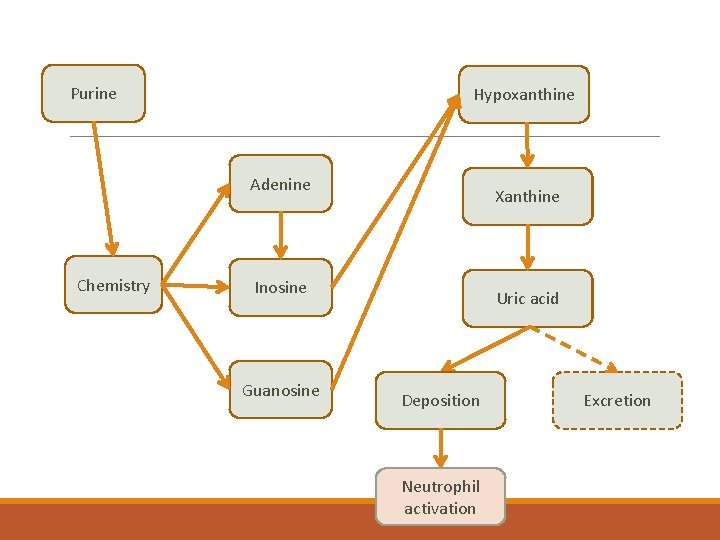
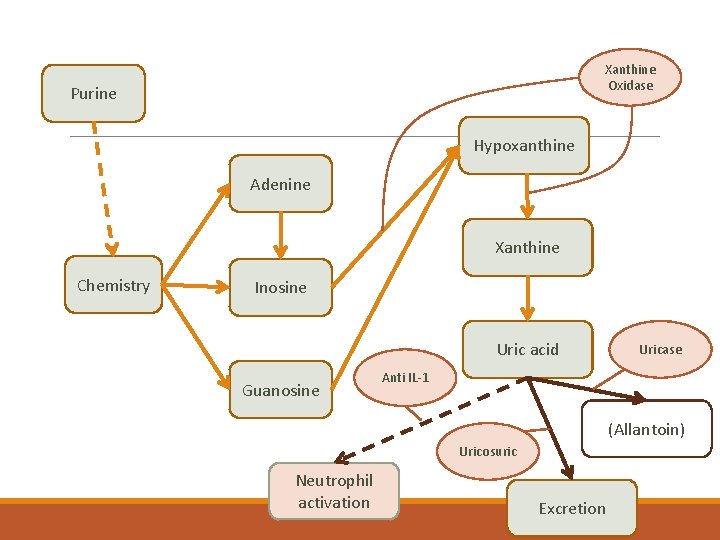
Purine Hypoxanthine Adenine Chemistry Xanthine Inosine Guanosine Uric acid Deposition Neutrophil activation Excretion
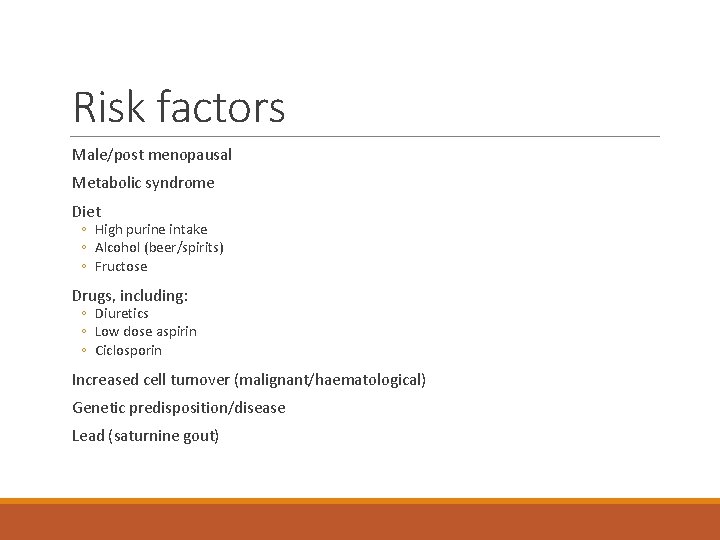
Risk factors Male/post menopausal Metabolic syndrome Diet ◦ High purine intake ◦ Alcohol (beer/spirits) ◦ Fructose Drugs, including: ◦ Diuretics ◦ Low dose aspirin ◦ Ciclosporin Increased cell turnover (malignant/haematological) Genetic predisposition/disease Lead (saturnine gout)
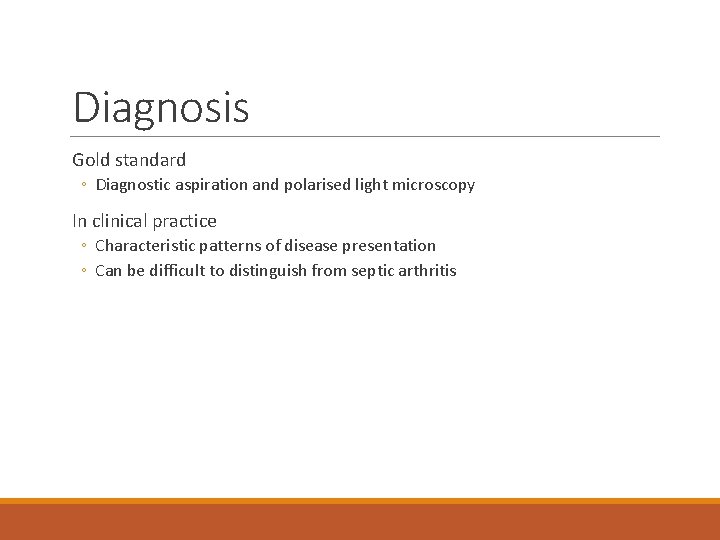
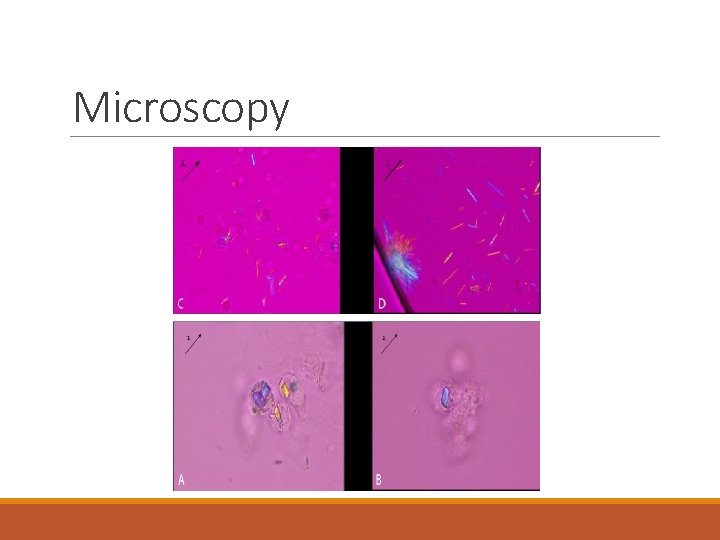
Diagnosis Gold standard ◦ Diagnostic aspiration and polarised light microscopy In clinical practice ◦ Characteristic patterns of disease presentation ◦ Can be difficult to distinguish from septic arthritis
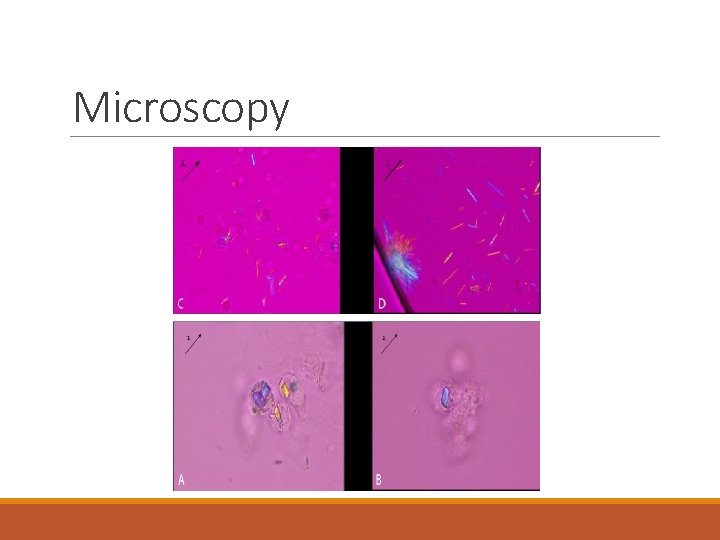
Microscopy
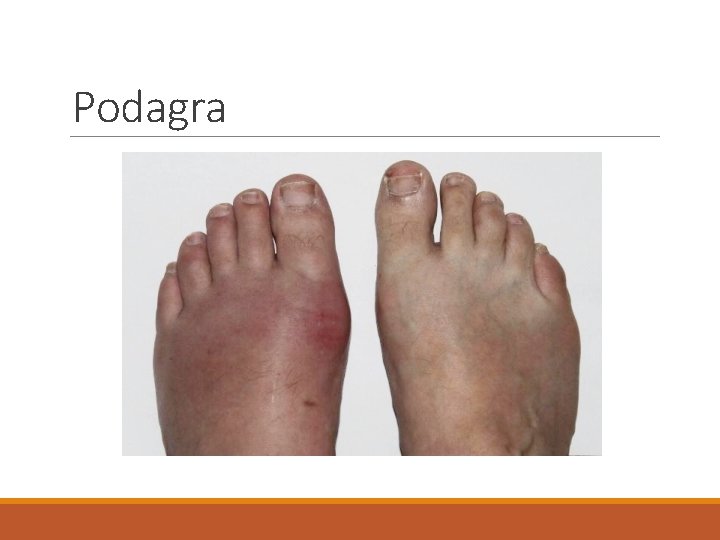
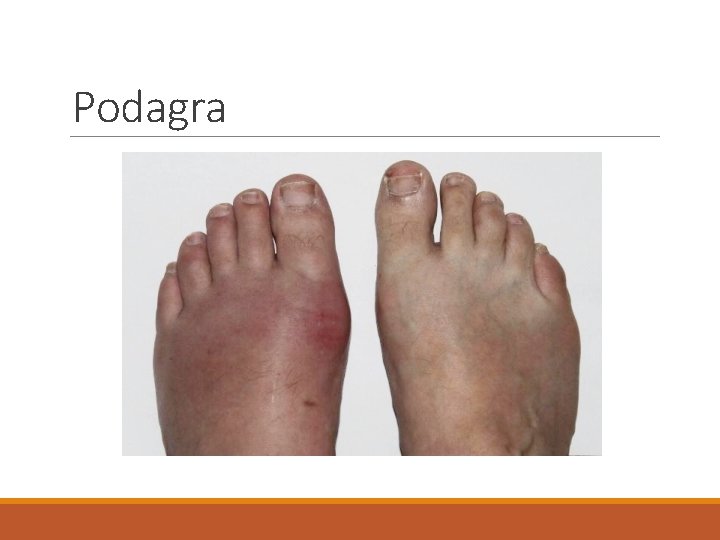
Podagra

Tophi
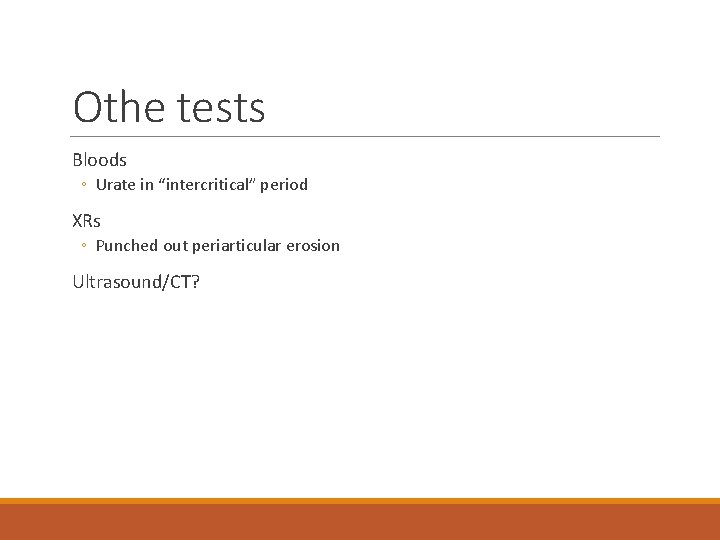
Othe tests Bloods ◦ Urate in “intercritical” period XRs ◦ Punched out periarticular erosion Ultrasound/CT?

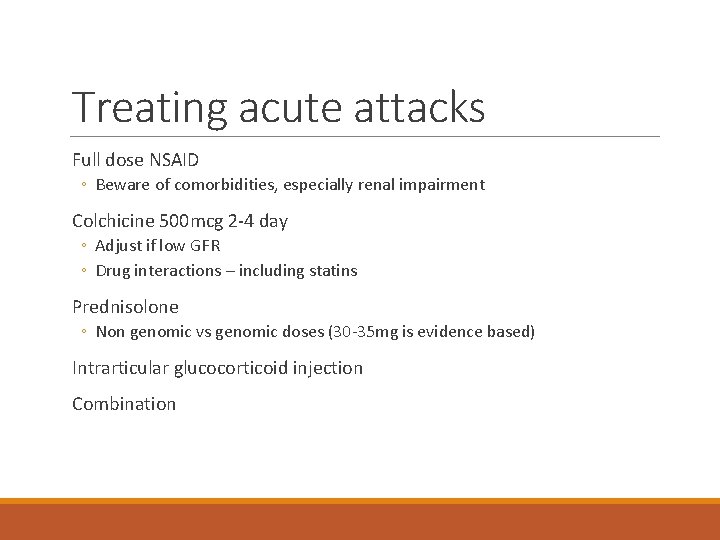
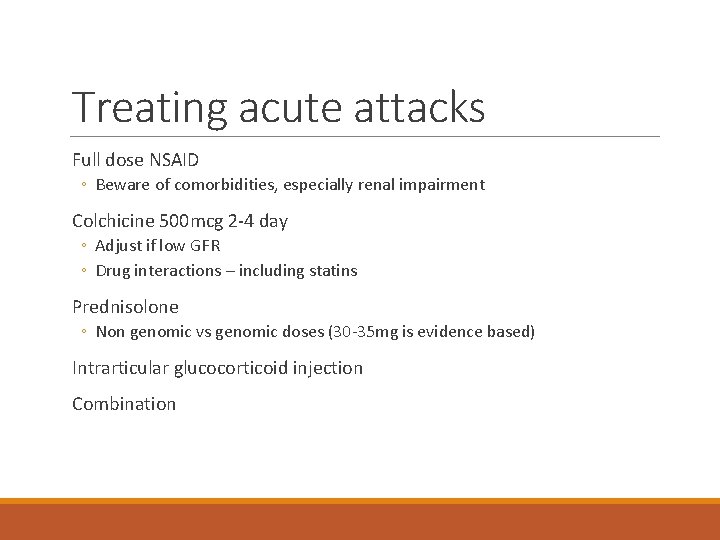
Treating acute attacks Full dose NSAID ◦ Beware of comorbidities, especially renal impairment Colchicine 500 mcg 2 -4 day ◦ Adjust if low GFR ◦ Drug interactions – including statins Prednisolone ◦ Non genomic vs genomic doses (30 -35 mg is evidence based) Intrarticular glucocorticoid injection Combination
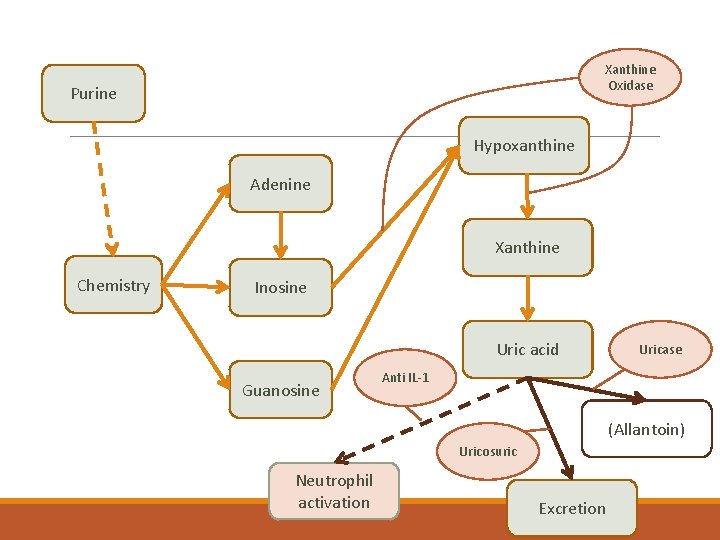
Xanthine Oxidase Purine Hypoxanthine Adenine Xanthine Chemistry Inosine Uric acid Guanosine Uricase Anti IL-1 (Allantoin) Uricosuric Neutrophil activation Excretion
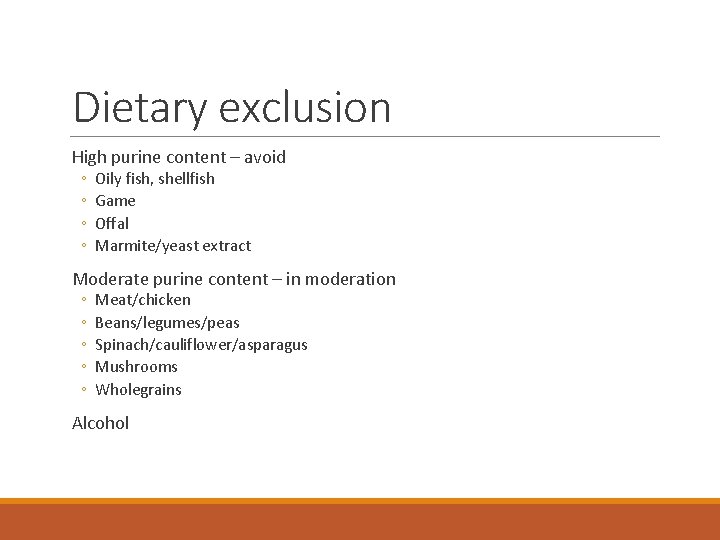
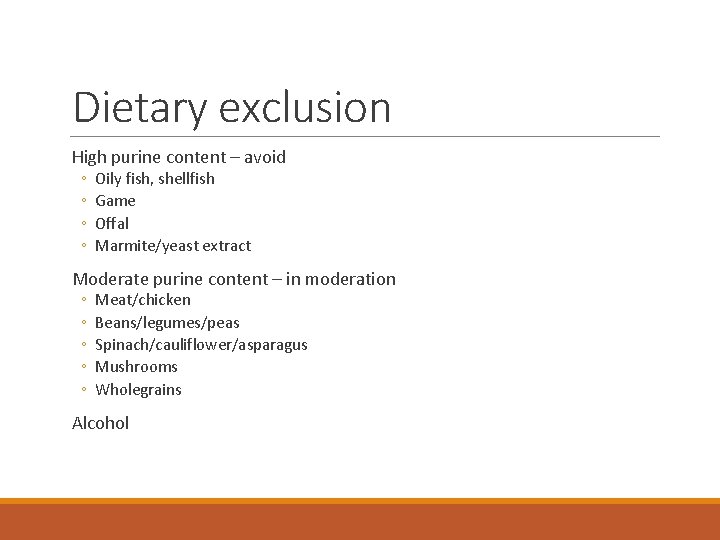
Dietary exclusion High purine content – avoid ◦ ◦ Oily fish, shellfish Game Offal Marmite/yeast extract Moderate purine content – in moderation ◦ ◦ ◦ Meat/chicken Beans/legumes/peas Spinach/cauliflower/asparagus Mushrooms Wholegrains Alcohol
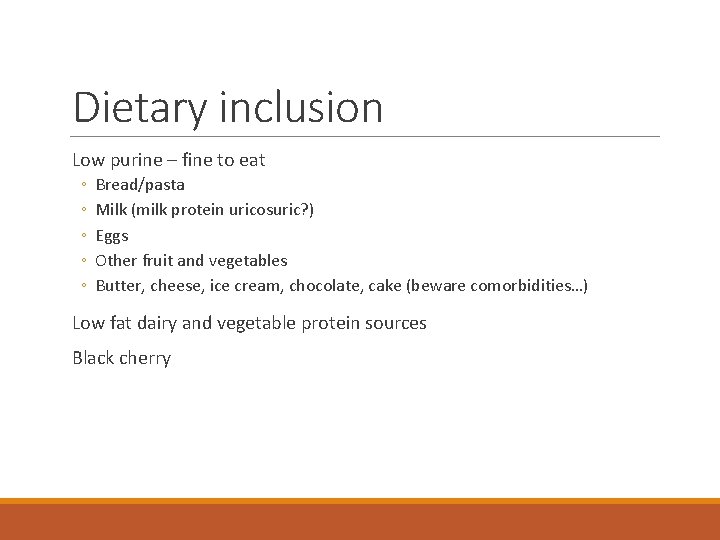
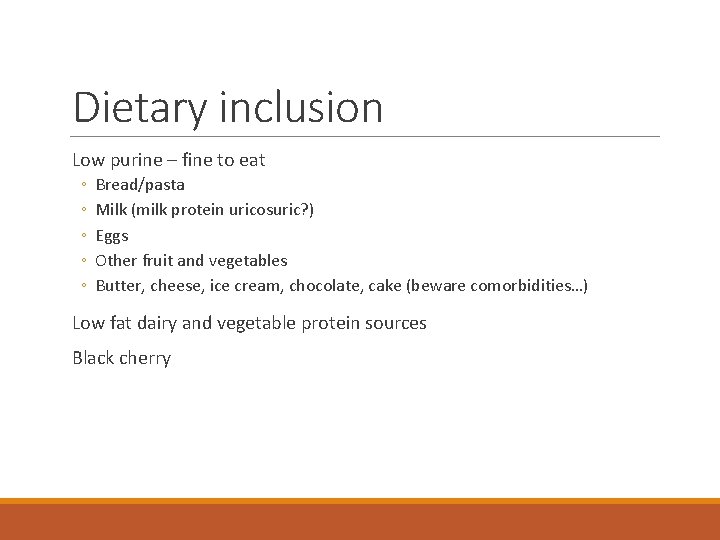
Dietary inclusion Low purine – fine to eat ◦ ◦ ◦ Bread/pasta Milk (milk protein uricosuric? ) Eggs Other fruit and vegetables Butter, cheese, ice cream, chocolate, cake (beware comorbidities…) Low fat dairy and vegetable protein sources Black cherry
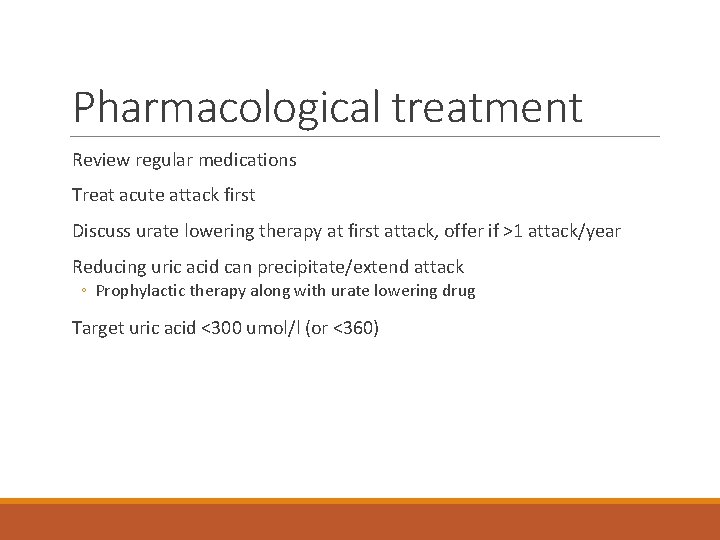
Pharmacological treatment Review regular medications Treat acute attack first Discuss urate lowering therapy at first attack, offer if >1 attack/year Reducing uric acid can precipitate/extend attack ◦ Prophylactic therapy along with urate lowering drug Target uric acid <300 umol/l (or <360)
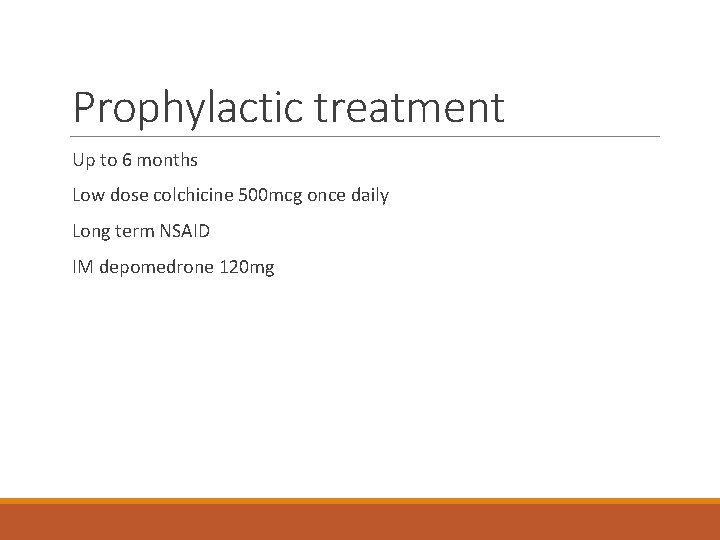
Prophylactic treatment Up to 6 months Low dose colchicine 500 mcg once daily Long term NSAID IM depomedrone 120 mg
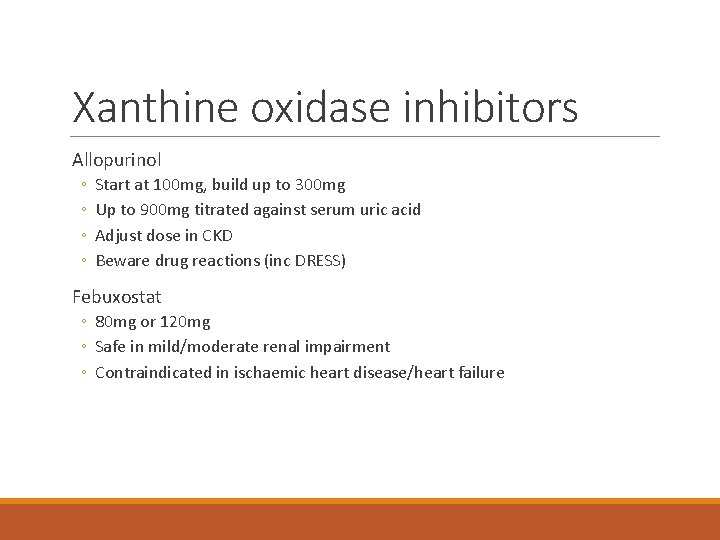
Xanthine oxidase inhibitors Allopurinol ◦ ◦ Start at 100 mg, build up to 300 mg Up to 900 mg titrated against serum uric acid Adjust dose in CKD Beware drug reactions (inc DRESS) Febuxostat ◦ 80 mg or 120 mg ◦ Safe in mild/moderate renal impairment ◦ Contraindicated in ischaemic heart disease/heart failure
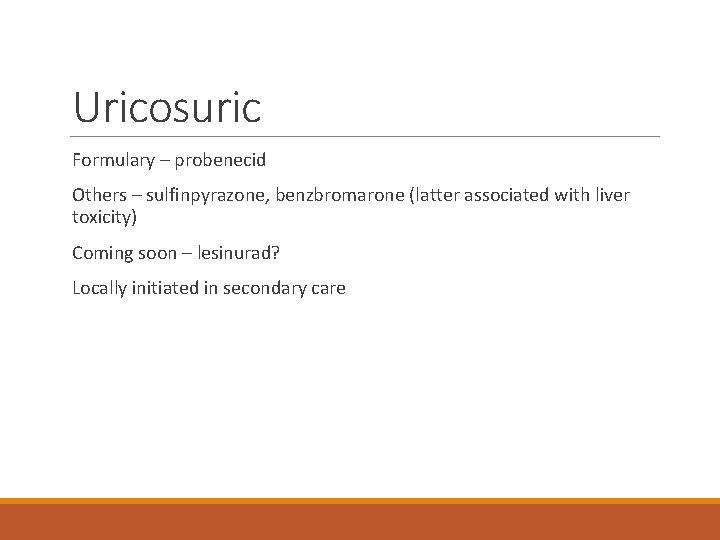
Uricosuric Formulary – probenecid Others – sulfinpyrazone, benzbromarone (latter associated with liver toxicity) Coming soon – lesinurad? Locally initiated in secondary care
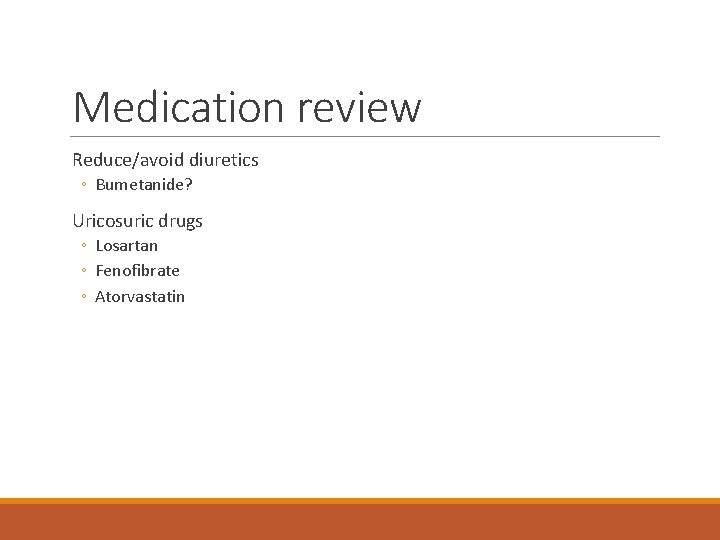
Medication review Reduce/avoid diuretics ◦ Bumetanide? Uricosuric drugs ◦ Losartan ◦ Fenofibrate ◦ Atorvastatin
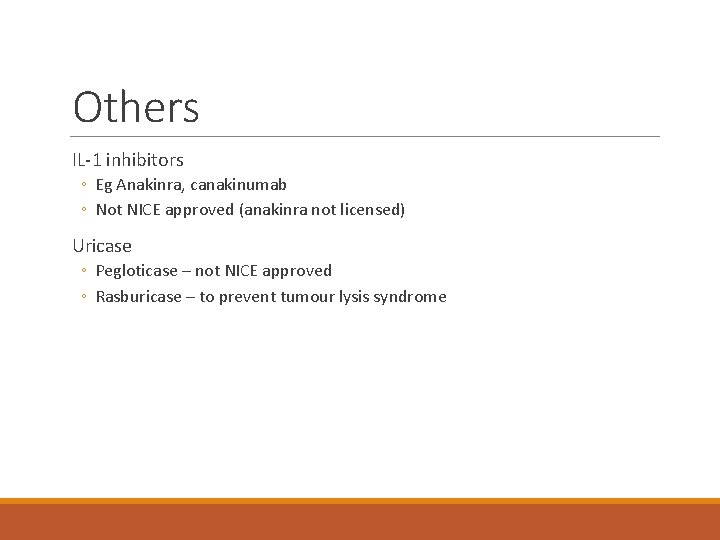
Others IL-1 inhibitors ◦ Eg Anakinra, canakinumab ◦ Not NICE approved (anakinra not licensed) Uricase ◦ Pegloticase – not NICE approved ◦ Rasburicase – to prevent tumour lysis syndrome
Uric acid and cardiovascular risk Noted association between gout and cardiovascular disease Is serum uric acid an independent risk factor? Trend of association with: ◦ ◦ Hypertension IHD/heart failure CKD Diabetes Only proven associations: gout, nephrolithiasis Is low serum uric acid harmful? ◦ Reactive oxygen species scavenger, possible association with neurodegenerative diseases Currently – raised serum uric acid not an indication for treatment But diagnosis of gout should prompt for assessment of cardiovascular risk
Pseudogout Calcium pyrophosphate crystal deposition Large joints – knee, wrist, hip Risk factors ◦ ◦ Age Hyperparathyroidism Haemochromatosis Other calcium haemostasis disoders Acute attacks – treat as for gout Prophylaxis – none available

(University of California, San Diego)
Summary Commonest inflammatory arthritis Generally diagnosed by pattern of disease rather than joint aspiration Treatment: ◦ Acute ◦ Followed by urate lowering therapy ◦ Lifestyle ◦ Pharmacological ◦ With prophylaxis See BSR (2017) and EULAR (2016) guidelines
 Rheumatologist carefirst bcbs
Rheumatologist carefirst bcbs Rheumatologist vsp
Rheumatologist vsp Dr forghani rheumatologist
Dr forghani rheumatologist Dr susan wallis rheumatologist
Dr susan wallis rheumatologist Dr eugene lim rheumatologist
Dr eugene lim rheumatologist Model asad
Model asad Ad/as diagram
Ad/as diagram Asad model
Asad model Asad modellen
Asad modellen Asad samar
Asad samar Kasisky test
Kasisky test Model asad
Model asad Asad model
Asad model Asad software
Asad software Lecturer asad ali
Lecturer asad ali Model asad
Model asad Mariane asad doyle
Mariane asad doyle Asad model
Asad model Asad rahmani
Asad rahmani Asad model
Asad model Szok podazowy
Szok podazowy Gout
Gout Is gout like arthritis
Is gout like arthritis Gout criteria
Gout criteria Spinal dysraphism
Spinal dysraphism Analglesia
Analglesia Hydrocodone and gout
Hydrocodone and gout