A Curious Case of NMO Transverse Myelitis Mystery
- Slides: 1
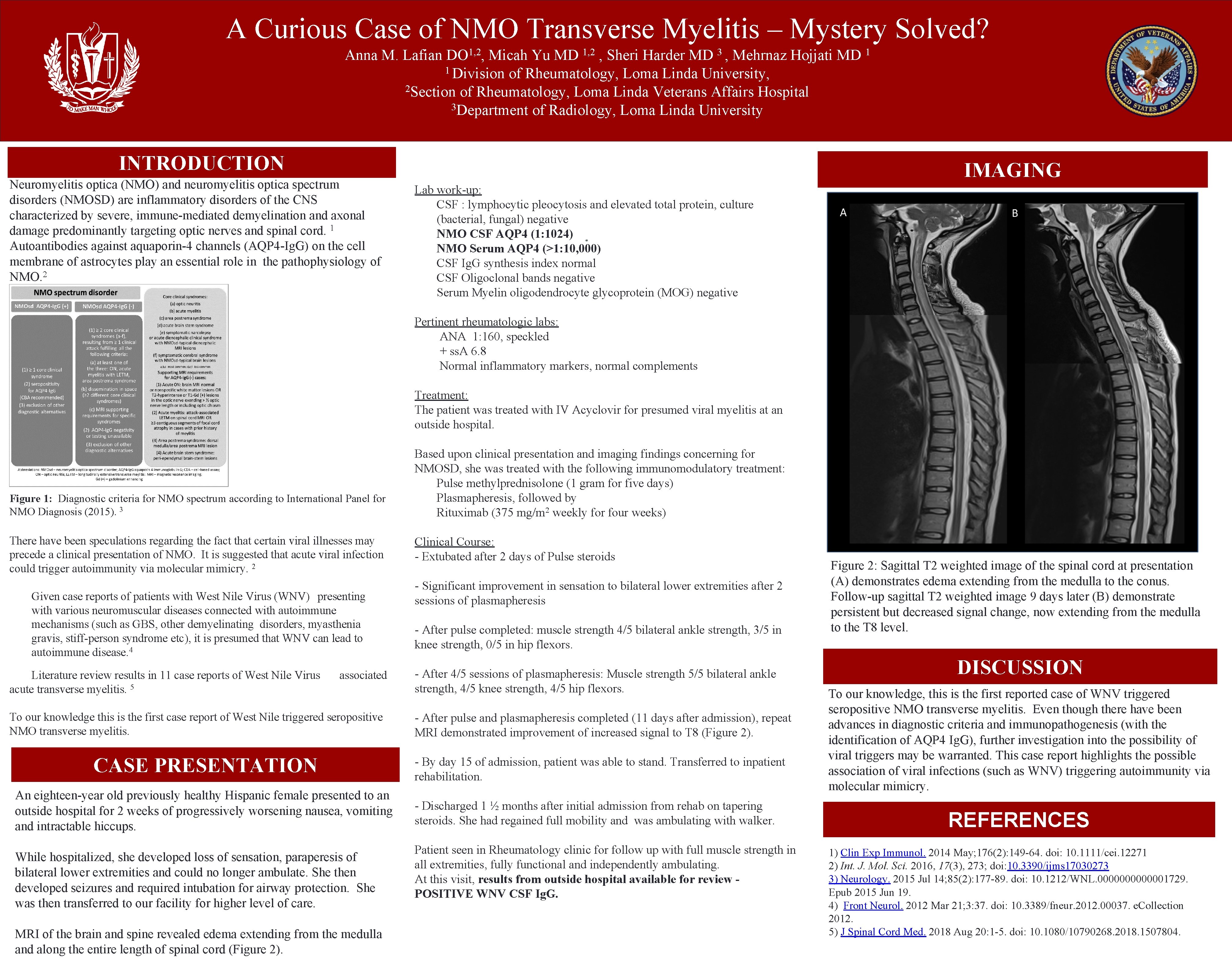
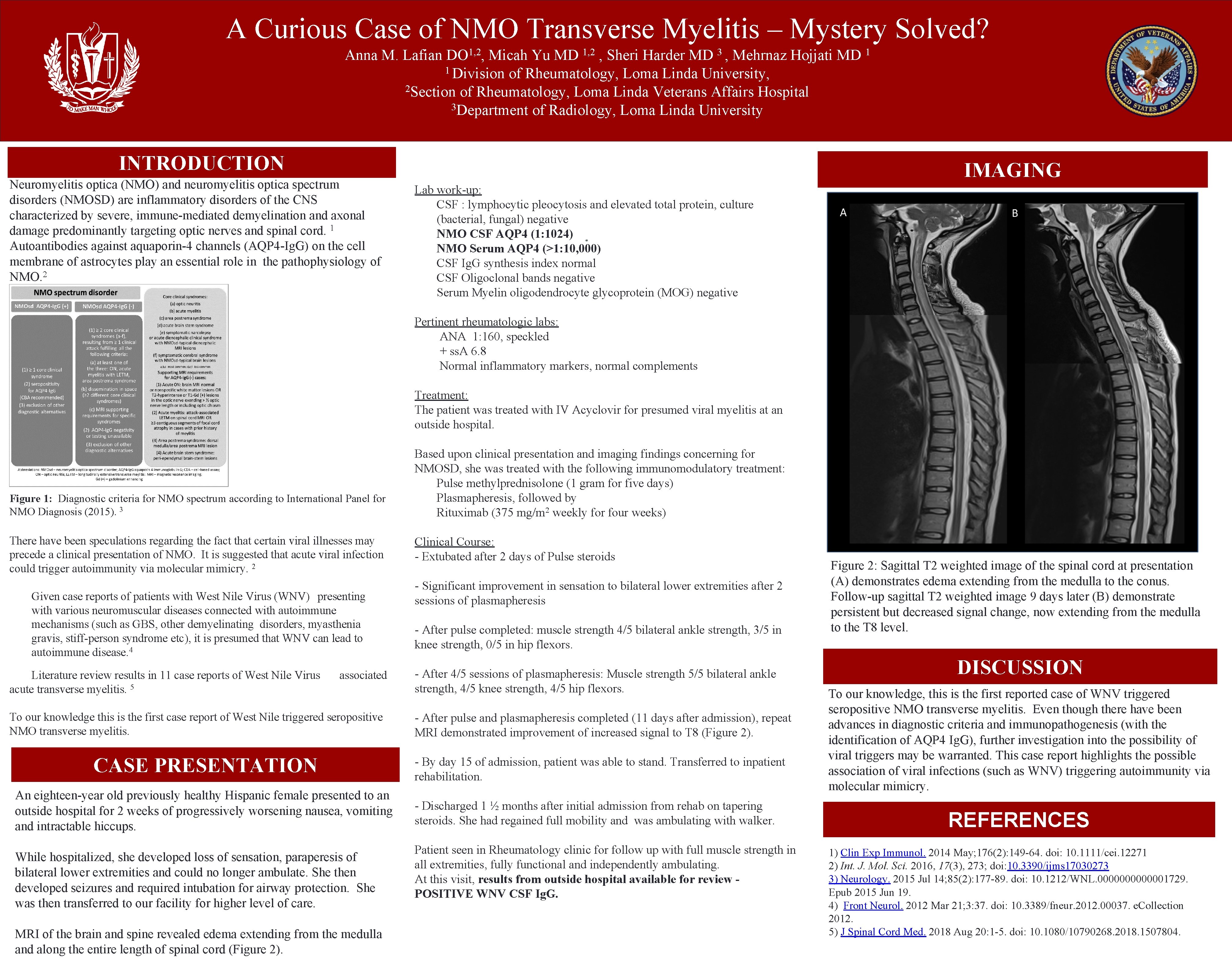
A Curious Case of NMO Transverse Myelitis – Mystery Solved? Anna M. Lafian DO 1, 2, Micah Yu MD 1, 2 , Sheri Harder MD 3 , Mehrnaz Hojjati MD 1 1 Division of Rheumatology, Loma Linda University, 2 Section of Rheumatology, Loma Linda Veterans Affairs Hospital 3 Department of Radiology, Loma Linda University INTRODUCTION Neuromyelitis optica (NMO) and neuromyelitis optica spectrum disorders (NMOSD) are inflammatory disorders of the CNS characterized by severe, immune-mediated demyelination and axonal 1 damage predominantly targeting optic nerves and spinal cord. Autoantibodies against aquaporin-4 channels (AQP 4 -Ig. G) on the cell membrane of astrocytes play an essential role in the pathophysiology of NMO. 2 IMAGING Lab work-up: CSF : lymphocytic pleocytosis and elevated total protein, culture (bacterial, fungal) negative NMO CSF AQP 4 (1: 1024) NMO Serum AQP 4 (>1: 10, 000) CSF Ig. G synthesis index normal CSF Oligoclonal bands negative Serum Myelin oligodendrocyte glycoprotein (MOG) negative Pertinent rheumatologic labs: ANA 1: 160, speckled + ss. A 6. 8 Normal inflammatory markers, normal complements Treatment: The patient was treated with IV Acyclovir for presumed viral myelitis at an outside hospital. Figure 1: Diagnostic criteria for NMO spectrum according to International Panel for NMO Diagnosis (2015). 3 There have been speculations regarding the fact that certain viral illnesses may precede a clinical presentation of NMO. It is suggested that acute viral infection could trigger autoimmunity via molecular mimicry. 2 Given case reports of patients with West Nile Virus (WNV) presenting with various neuromuscular diseases connected with autoimmune mechanisms (such as GBS, other demyelinating disorders, myasthenia gravis, stiff-person syndrome etc), it is presumed that WNV can lead to autoimmune disease. 4 Literature review results in 11 case reports of West Nile Virus acute transverse myelitis. 5 associated To our knowledge this is the first case report of West Nile triggered seropositive NMO transverse myelitis. CASE PRESENTATION An eighteen-year old previously healthy Hispanic female presented to an outside hospital for 2 weeks of progressively worsening nausea, vomiting and intractable hiccups. While hospitalized, she developed loss of sensation, paraperesis of bilateral lower extremities and could no longer ambulate. She then developed seizures and required intubation for airway protection. She was then transferred to our facility for higher level of care. MRI of the brain and spine revealed edema extending from the medulla and along the entire length of spinal cord (Figure 2). Based upon clinical presentation and imaging findings concerning for NMOSD, she was treated with the following immunomodulatory treatment: Pulse methylprednisolone (1 gram for five days) Plasmapheresis, followed by Rituximab (375 mg/m 2 weekly for four weeks) Clinical Course: - Extubated after 2 days of Pulse steroids - Significant improvement in sensation to bilateral lower extremities after 2 sessions of plasmapheresis - After pulse completed: muscle strength 4/5 bilateral ankle strength, 3/5 in knee strength, 0/5 in hip flexors. - After 4/5 sessions of plasmapheresis: Muscle strength 5/5 bilateral ankle strength, 4/5 knee strength, 4/5 hip flexors. - After pulse and plasmapheresis completed (11 days after admission), repeat MRI demonstrated improvement of increased signal to T 8 (Figure 2). - By day 15 of admission, patient was able to stand. Transferred to inpatient rehabilitation. - Discharged 1 ½ months after initial admission from rehab on tapering steroids. She had regained full mobility and was ambulating with walker. Patient seen in Rheumatology clinic for follow up with full muscle strength in all extremities, fully functional and independently ambulating. At this visit, results from outside hospital available for review POSITIVE WNV CSF Ig. G. Figure 2: Sagittal T 2 weighted image of the spinal cord at presentation (A) demonstrates edema extending from the medulla to the conus. Follow-up sagittal T 2 weighted image 9 days later (B) demonstrate persistent but decreased signal change, now extending from the medulla to the T 8 level. DISCUSSION To our knowledge, this is the first reported case of WNV triggered seropositive NMO transverse myelitis. Even though there have been advances in diagnostic criteria and immunopathogenesis (with the identification of AQP 4 Ig. G), further investigation into the possibility of viral triggers may be warranted. This case report highlights the possible association of viral infections (such as WNV) triggering autoimmunity via molecular mimicry. REFERENCES 1) Clin Exp Immunol. 2014 May; 176(2): 149 -64. doi: 10. 1111/cei. 12271 2) Int. J. Mol. Sci. 2016, 17(3), 273; doi: 10. 3390/ijms 17030273 3) Neurology. 2015 Jul 14; 85(2): 177 -89. doi: 10. 1212/WNL. 0000001729. Epub 2015 Jun 19. 4) Front Neurol. 2012 Mar 21; 3: 37. doi: 10. 3389/fneur. 2012. 00037. e. Collection 2012. 5) J Spinal Cord Med. 2018 Aug 20: 1 -5. doi: 10. 1080/10790268. 2018. 1507804.