Formation of Urine Filtration Each nephron has its

- Slides: 19
Formation of Urine
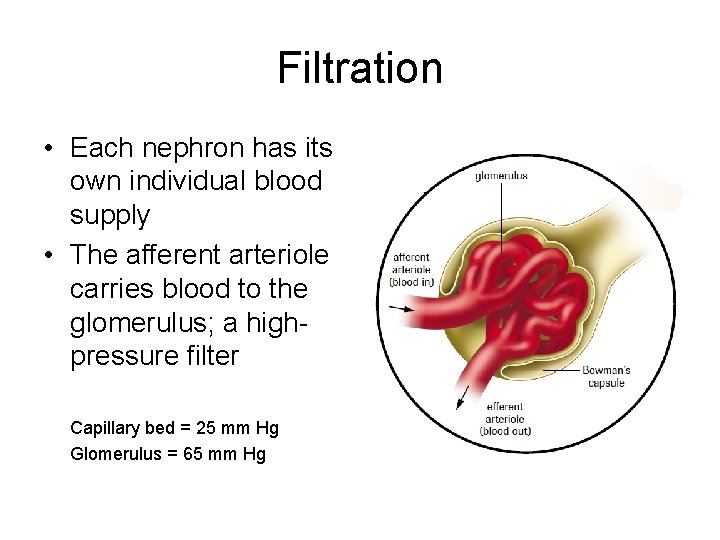
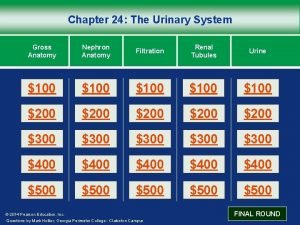
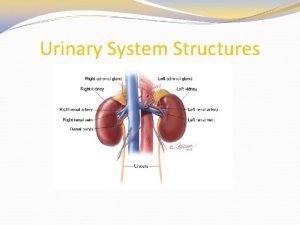
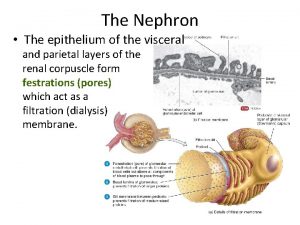
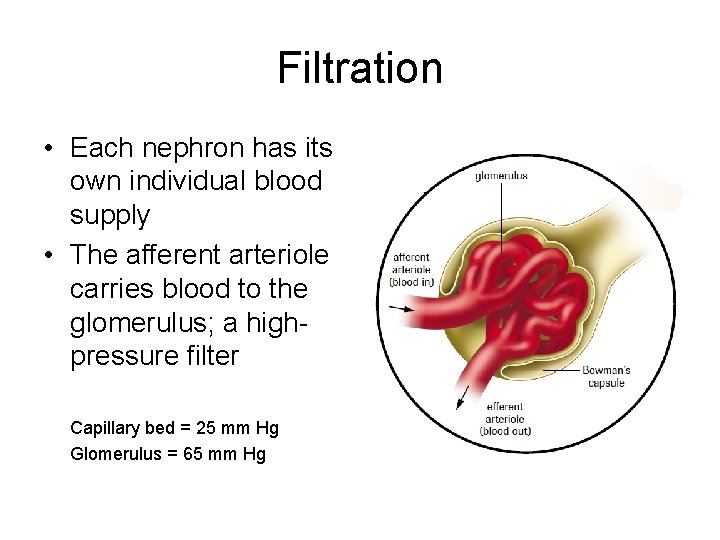
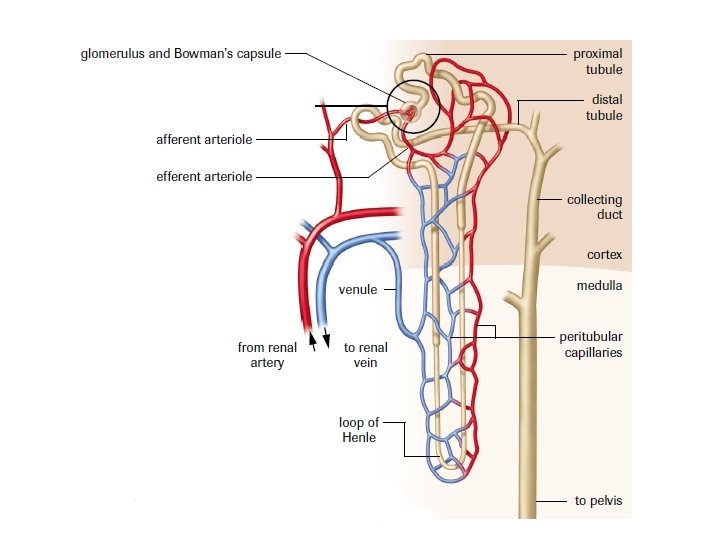
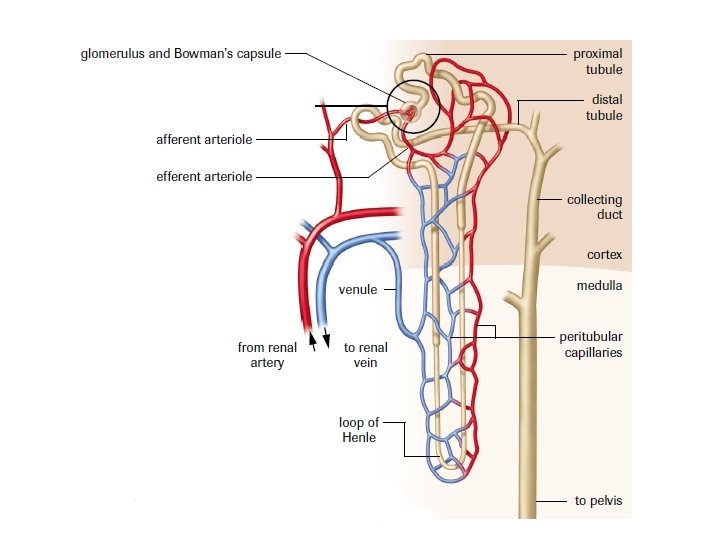
Filtration • Each nephron has its own individual blood supply • The afferent arteriole carries blood to the glomerulus; a highpressure filter Capillary bed = 25 mm Hg Glomerulus = 65 mm Hg
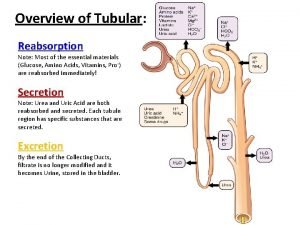
Urine Formation The formation of urine occurs as the result of three processes. 1. Filtration- the movement of fluids from the blood into the Bowman’s capsule 2. Reabsorption – the transfer of essential solutes and water from the nephron back into the blood 3. Secretion – the movement of materials from the blood back into the nephron
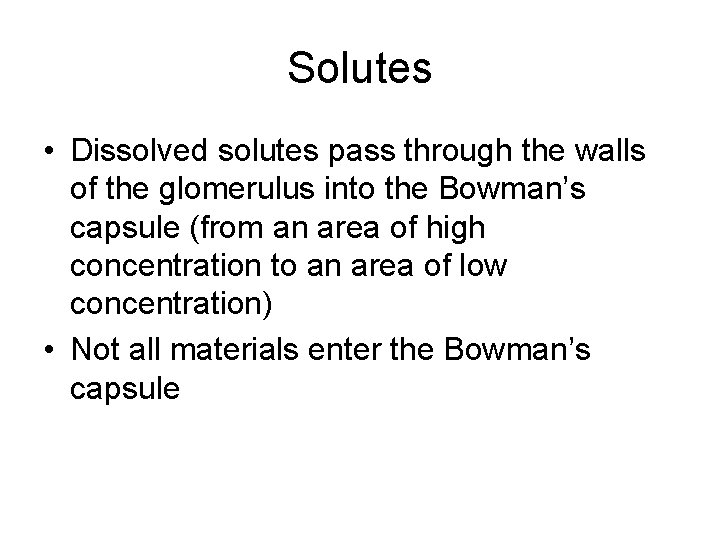
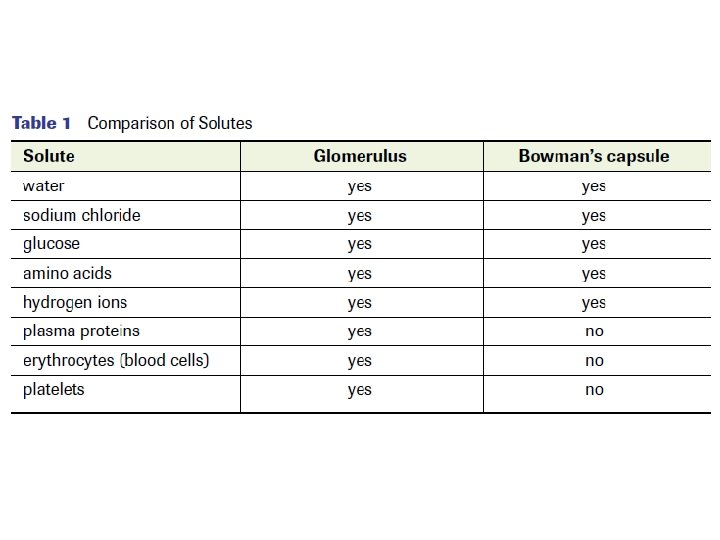
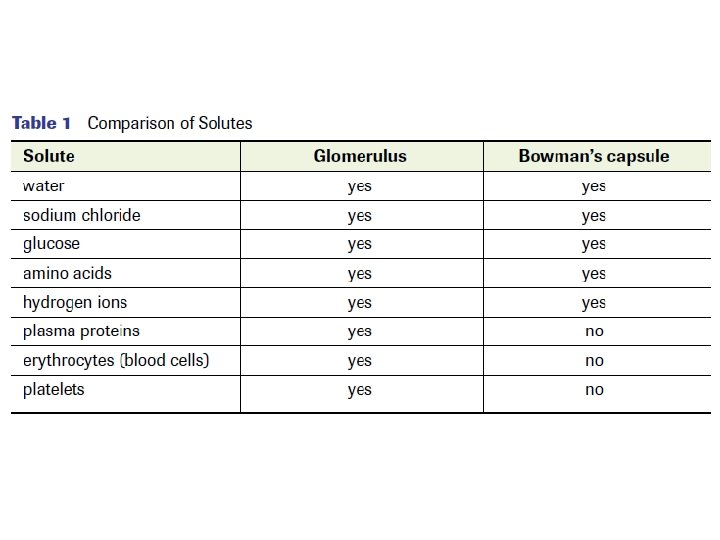
Solutes • Dissolved solutes pass through the walls of the glomerulus into the Bowman’s capsule (from an area of high concentration to an area of low concentration) • Not all materials enter the Bowman’s capsule
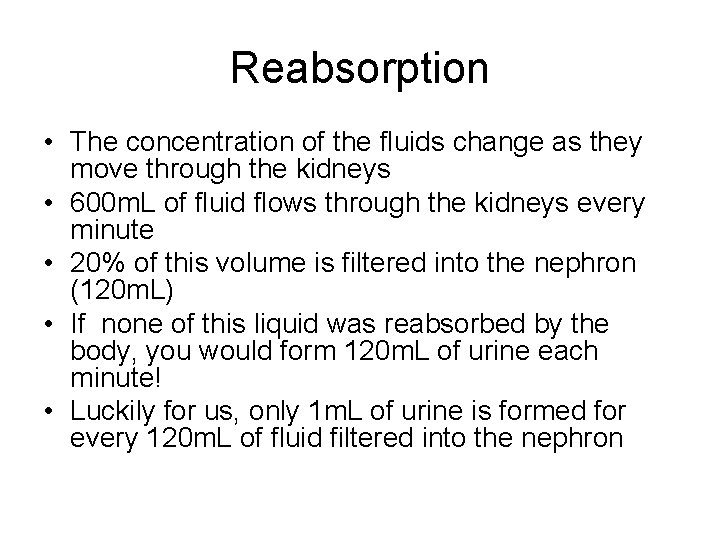
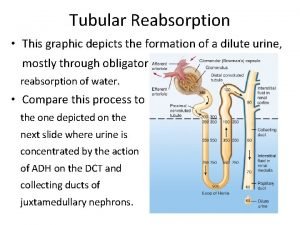
Reabsorption • The concentration of the fluids change as they move through the kidneys • 600 m. L of fluid flows through the kidneys every minute • 20% of this volume is filtered into the nephron (120 m. L) • If none of this liquid was reabsorbed by the body, you would form 120 m. L of urine each minute! • Luckily for us, only 1 m. L of urine is formed for every 120 m. L of fluid filtered into the nephron
• Where does the rest of the 119 m. L volume go? • It is (selectively) reabsorbed!
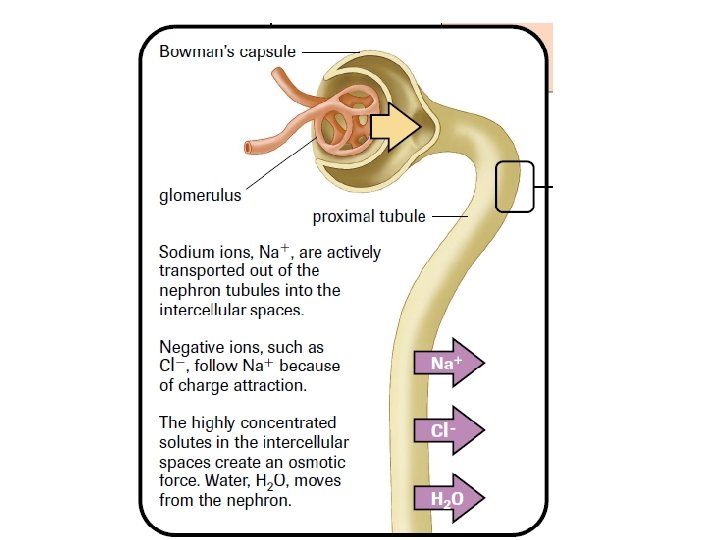
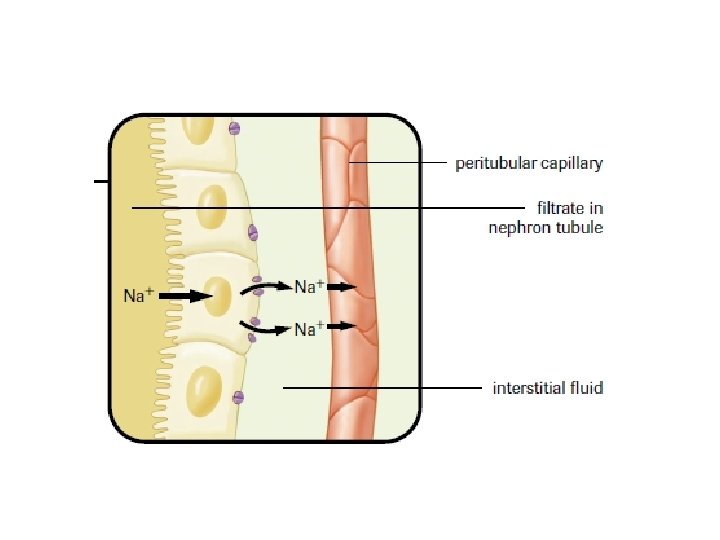
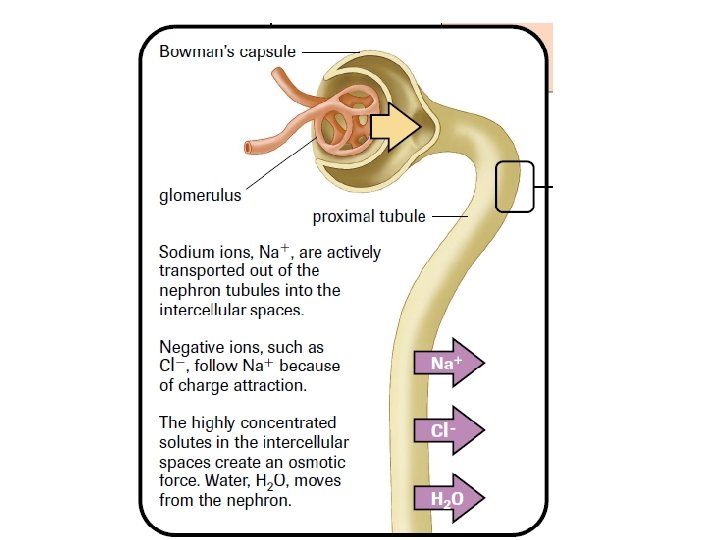
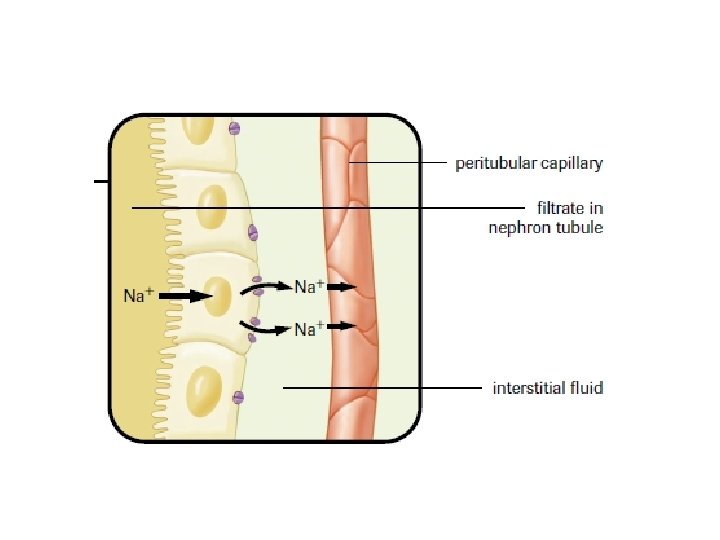
Selective Reabsorption • Occurs by both active and passive transport • Mitochondria provide energy for the active transport • Carrier molecules move Na+ ions across the cell membranes of the cells that line the nephron • Negative ions, such as Cl- and HCO 3 - follow positive Na+ ions because of charge attraction
• Other molecules are actively transported from the proximal tubule into the surrounding capillaries • Glucose and amino acids attach to specific carrier molecules which shuttle them out of the nephron
Threshold Level - The maximum amount of material that can be moved across the nephron • Once threshold level has been reached, the excess solute is excreted in the urine
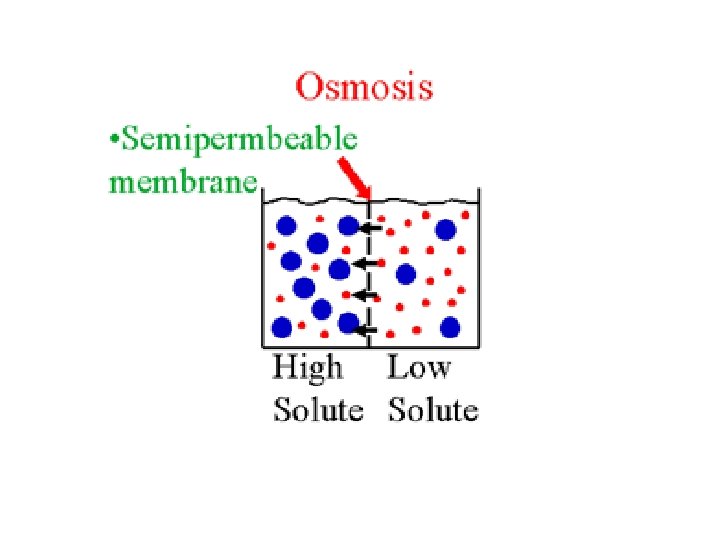
Osmotic Gradient • As solutes move out of the nephron into the capillaries, an osmotic gradient is created • This means that there is a greater concentration of solutes on the outside of the nephron compared to the inside • Water moves out of the nephron by osmosis (high [ ] to low [ ])
• A Second osmotic force is created by the proteins that still remain in the blood stream • Recall: these proteins are too large to be filtered into the Bowman’s capsule • This helps draw water from the interstitial fluid into the blood Interstitial fluid – fluid that surrounds the body’s cells

• As water is reabsorbed and removed from the nephron, the remaining solutes in the tubules become more concentrated
Secretion – is the movement of wastes from the blood into the nephron • Nitrogen-containing wastes, excess H+ ions, and minerals such as K+ ions are examples of substances secreted • Secretion occurs by active transport
 Cake filtration equation
Cake filtration equation Urine filtration
Urine filtration Dari hasil tes ternyata pak jaka mengandung glukosa
Dari hasil tes ternyata pak jaka mengandung glukosa Kdigo aki classification
Kdigo aki classification Introduction of urinary system
Introduction of urinary system Introduction of excretory system
Introduction of excretory system Urine formation introduction
Urine formation introduction Proximal convoluted tubule
Proximal convoluted tubule Urine formation video
Urine formation video Each season has its own beauty
Each season has its own beauty When glucose spills over into the urine, it has
When glucose spills over into the urine, it has Formation initiale vs formation continue
Formation initiale vs formation continue Atrial natriuretic peptide
Atrial natriuretic peptide Figure 15-3 is a diagram of the nephron
Figure 15-3 is a diagram of the nephron Where does reabsorption occur in the nephron
Where does reabsorption occur in the nephron Juxtamedullary nephrons and cortical nephrons
Juxtamedullary nephrons and cortical nephrons Zac efron on a nephron
Zac efron on a nephron Where does secretion occur in nephron
Where does secretion occur in nephron Transcellular
Transcellular Tubular secretion in nephron
Tubular secretion in nephron