Extreme Pediatric Aerodigestive Medicine and Unsedated In Office





- Slides: 39

Extreme Pediatric Aerodigestive Medicine and Unsedated In Office Endoscopy: Monitoring Pediatric Esophagitis and Gastritis Using Unsedated Gastroscopy and Esophagoscopy Joel Friedlander Assistant Professor of Pediatrics Digestive Health Institute Aerodigestive Program
Disclosure/COI • This talk will discuss off-label use of medical and surgical • • devices that are authorized by the FDA I currently hold a patent on a currently-not available endoscope device. No other conflicts of interest
The Aerodigestive Conundrum The pursuit of more efficient, higher quality, less expensive care 4
The Aerodigestive Conundrum The pursuit of more efficient, higher quality, less expensive care Multiple procedural specialties Need for multiple procedures 5
The Aerodigestive/GI Conundrum The pursuit of more efficient, higher quality, less expensive care What Role Does Reflux Play? Multiple procedural specialties Need for multiple procedures 6
The Aerodigestive/GI Conundrum The pursuit of more efficient, higher quality, less expensive care How do we follow it up? Multiple procedural specialties What Role Does Reflux Play? Need for multiple procedures 7
The GI Background • Eosinophilic Esophagitis (Eo. E) and Reflux Esophagitis are increasingly common chronic inflammatory diseases that need to be addressed by the pediatric gastroenterologist and found in Aerodigestive clinics (often incidentally) • Assessment of esophageal mucosa is needed during diagnosis and subsequent therapeutic monitoring • Currently sedated endoscopy is the most common procedure used for evaluation of the esophagus and gastric mucosa Dellon ES, Gonsalves N, Hirano I, et al. ACG clinical guideline: Evidenced based approach to the diagnosis and management of esophageal eosinophilia and eosinophilic esophagitis (Eo. E). Am J Gastroenterol 2013; 108: 679 -92; quiz Greenhawt M, Aceves SS, Spergel JM, et al. The management of eosinophilic esophagitis. J Allergy Clin Immunol Pract 2013; 1: 332 -40; quiz 341 -2. Papadopoulou A, Koletzko S, Heuschkel R, et al. Management guidelines of eosinophilic esophagitis in childhood. J Pediatr Gastroenterol Nutr 2014; 58: 107 -18. Liacouras CA, Furuta GT, Hirano I, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol 2011; 128: 3 -20 e 6; quiz 21 -2 8
The GI Background • Endoscopy is expensive • Sedation requires monitoring and has risks • There is increased literature regarding potential risk of anesthesia in young children • Aerodigestive clinics desire assessment of the presence of reflux and improved lower cost care • Children with Eo. E need frequent endoscopy for targeting therapies and follow up Gleich SJ, Flick R, Hu D, et al. Neurodevelopment of children exposed to anesthesia: Design of the Mayo Anesthesia Safety in Kids (MASK) study. Contemp Clin Trials 2014; 41 C: 45 -54. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood) 2008; 27: 759 -69. 9
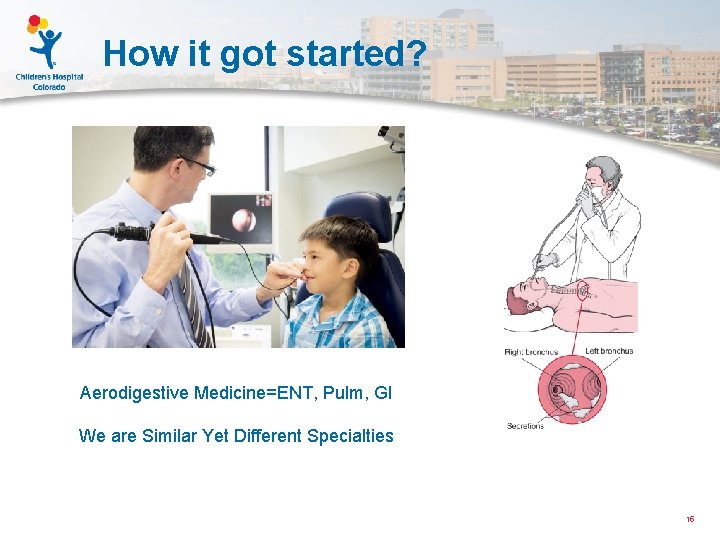
The GI Background • Unsedated endoscopy has been reported often in adults and minimally in pediatrics • Unsedated transnasal endoscopy (laryngoscopy) is performed routinely in pediatric otolaryngology and pulmonology clinics and by ENT/Pulmonary in Aerodigestive • Unsedated endoscopy is less expensive and potentially less risky than sedated endoscopy in a pediatric population Committee AT, Rodriguez SA, Banerjee S, et al. Ultrathin endoscopes. Gastrointest Endosc 2010; 71: 893 -8. Bishop PR, Nowicki MJ, May WL, et al. Unsedated upper endoscopy in children. Gastrointest Endosc 2002; 55: 624 -30. Wood RE. Evaluation of the upper airway in children. Curr Opin Pediatr 2008; 20: 266 -71 10
The GI Background • Unsedated endoscopy has been reported often in adults and minimally in pediatrics • Unsedated transnasal endoscopy (laryngoscopy) is performed routinely in pediatric otolaryngology and pulmonology clinics and by ENT/Pulmonary in Aerodigestive • Unsedated endoscopy is less expensive and potentially less risky than sedated endoscopy in a pediatric population Committee AT, Rodriguez SA, Banerjee S, et al. Ultrathin endoscopes. Gastrointest Endosc 2010; 71: 893 -8. Bishop PR, Nowicki MJ, May WL, et al. Unsedated upper endoscopy in children. Gastrointest Endosc 2002; 55: 624 -30. Wood RE. Evaluation of the upper airway in children. Curr Opin Pediatr 2008; 20: 266 -71 11
The Original Hypothesis Transnasal Esophagoscopy (TNE) is a safe and effective tool to monitor the mucosa of children with Eosinophilic Esophagitis 12
The Original Hypothesis Transnasal Esophagoscopy (TNE) is a safe and effective tool to monitor the mucosa of children with Eosinophilic Esophagitis (And Perhaps Reflux Esophagitis/Gastritis) 13
The Specific Aim of Original Study Evaluate the performance of TNE with biopsies using ultra-slim flexible endoscopes in assessing the esophageal mucosa of pediatric subjects with Eo. E. a. Assess parental and subject satisfaction b. Assess adequacy of biopsy samples c. Monitor for adverse events d. Assess duration and charges of procedure 14
How it got started? Aerodigestive Medicine=ENT, Pulm, GI We are Similar Yet Different Specialties 15

How it got started? Peds Bronchoscopes 2. 8 mm (1. 2 mm channel) 4 mm (2. 8 mm channel) Peds Gastroscopes 4. 9 -5. 5 mm (2 mm channel) 8. 6 mm-9. 2 mm (2. 8 mm channel) 16

How it got started? Peds Bronchoscopes 2. 8 mm (1. 2 mm channel) 4 mm (2. 8 mm channel) Peds Gastroscopes 4. 9 -5. 5 mm (2 mm channel) 8. 6 mm-9. 2 mm (2. 8 mm channel) Our Scopes are Very Similar 17
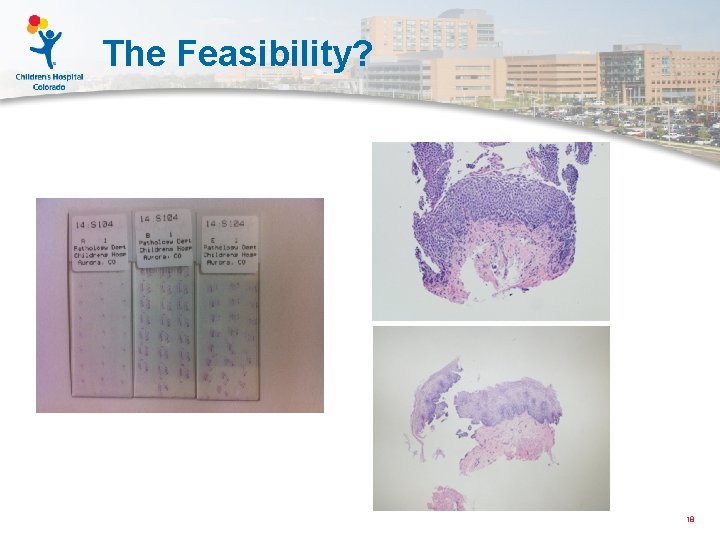
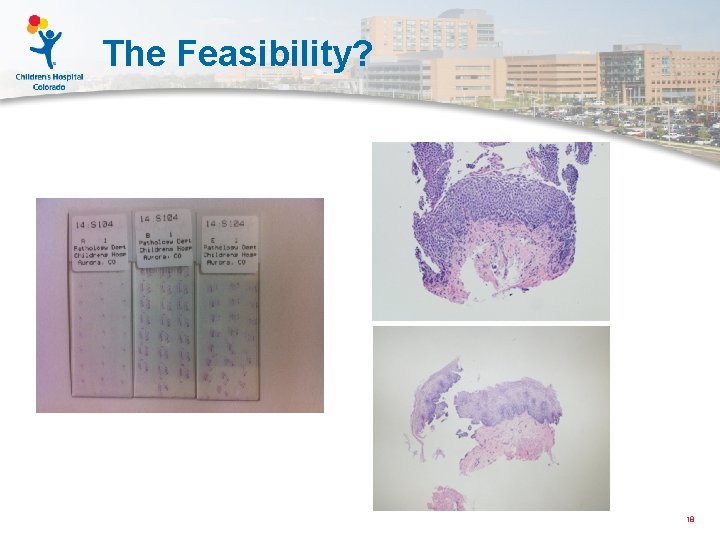
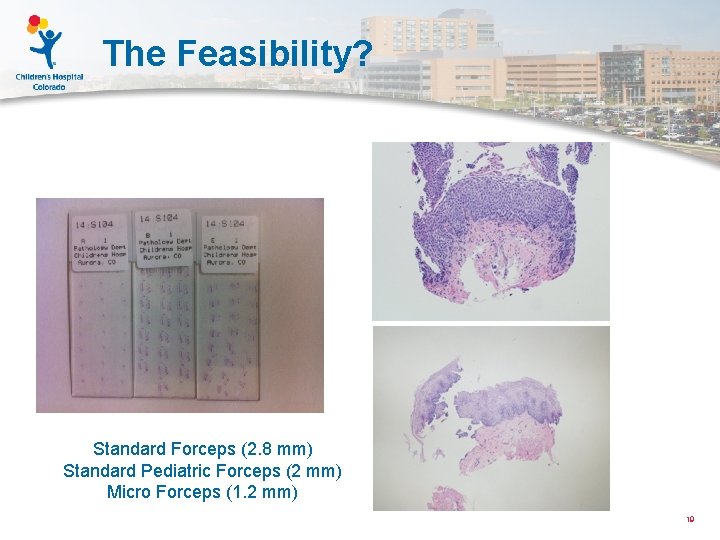
The Feasibility? 18
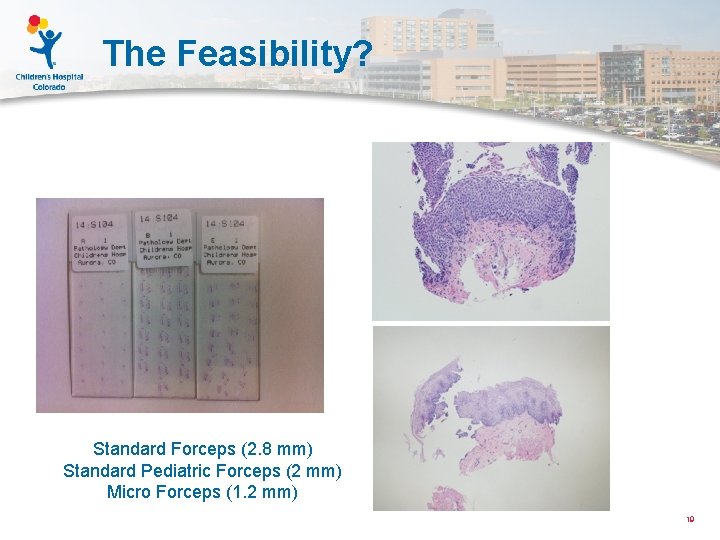
The Feasibility? Standard Forceps (2. 8 mm) Standard Pediatric Forceps (2 mm) Micro Forceps (1. 2 mm) 19
Study Design and Flow
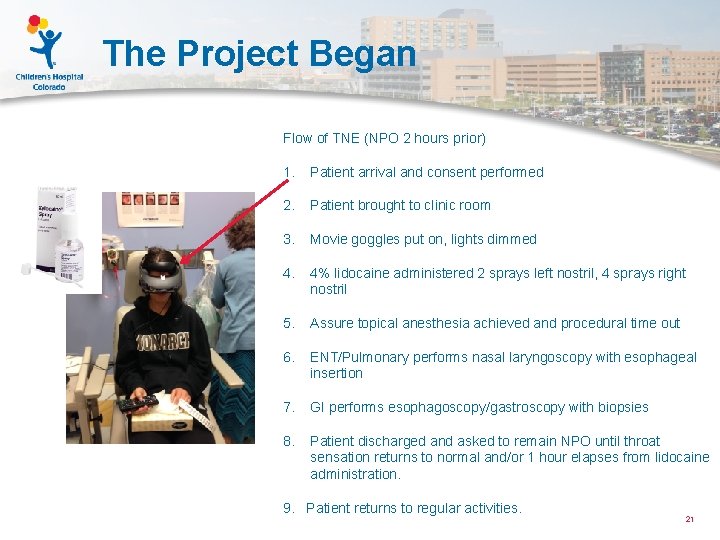
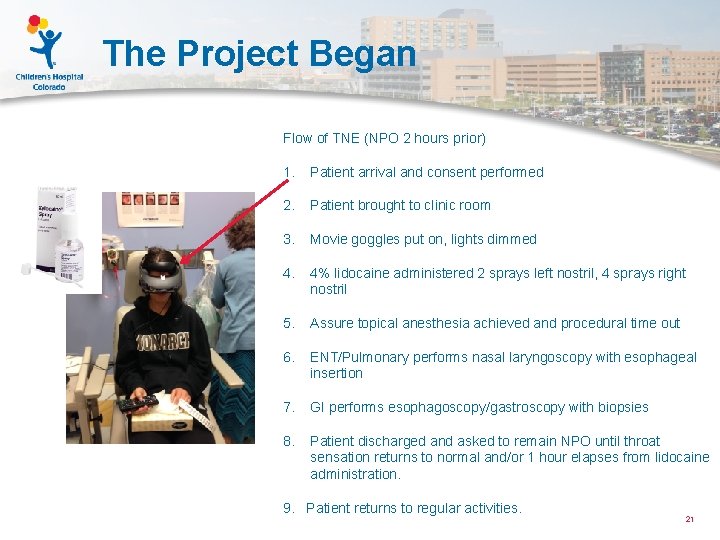
The Project Began Flow of TNE (NPO 2 hours prior) 1. Patient arrival and consent performed 2. Patient brought to clinic room 3. Movie goggles put on, lights dimmed 4. 4% lidocaine administered 2 sprays left nostril, 4 sprays right nostril 5. Assure topical anesthesia achieved and procedural time out 6. ENT/Pulmonary performs nasal laryngoscopy with esophageal insertion 7. GI performs esophagoscopy/gastroscopy with biopsies 8. Patient discharged and asked to remain NPO until throat sensation returns to normal and/or 1 hour elapses from lidocaine administration. 9. Patient returns to regular activities. 21
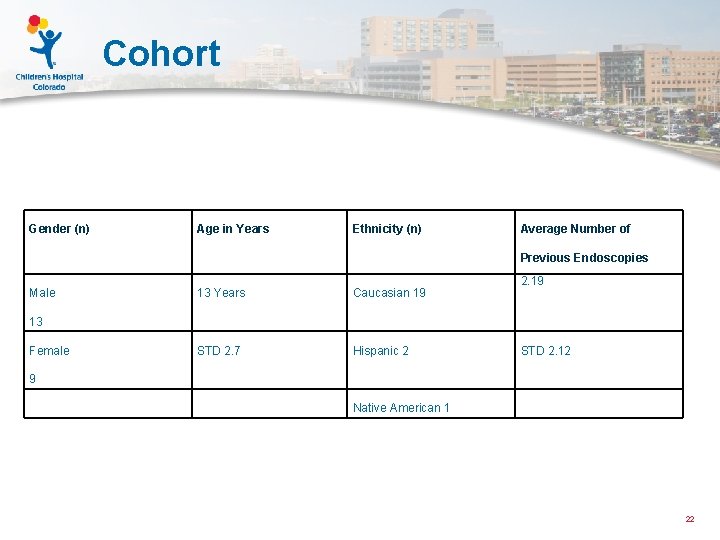
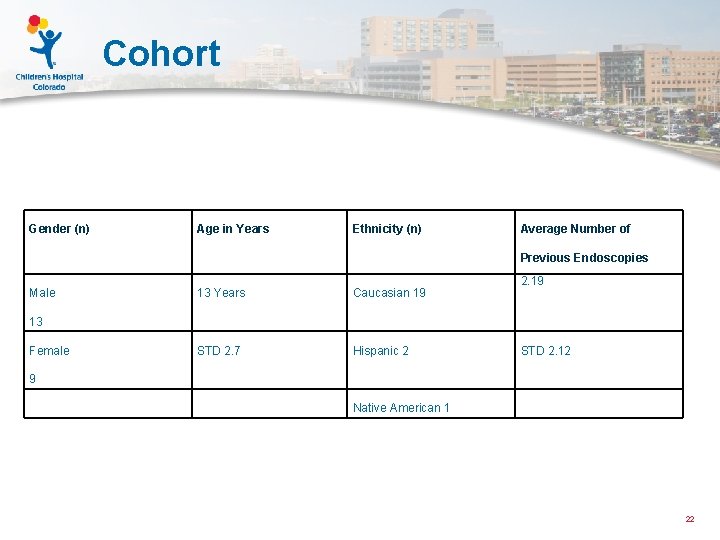
Cohort Gender (n) Age in Years Ethnicity (n) Average Number of Previous Endoscopies Male 13 Years Caucasian 19 STD 2. 7 Hispanic 2 2. 19 13 Female STD 2. 12 9 Native American 1 22
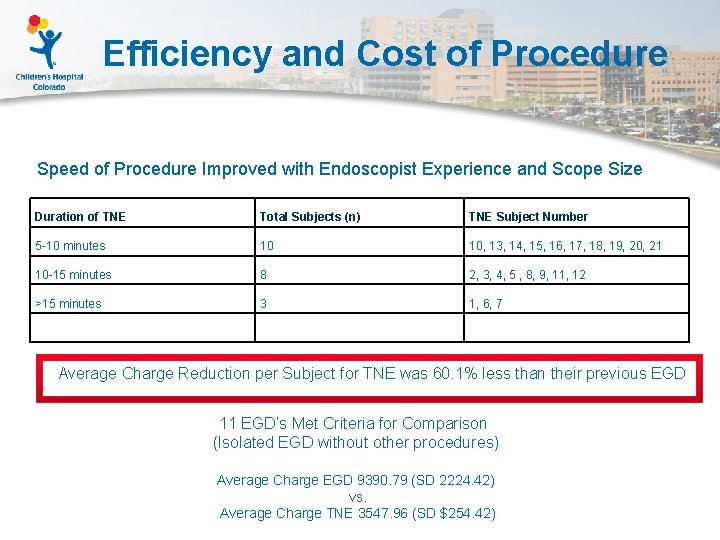
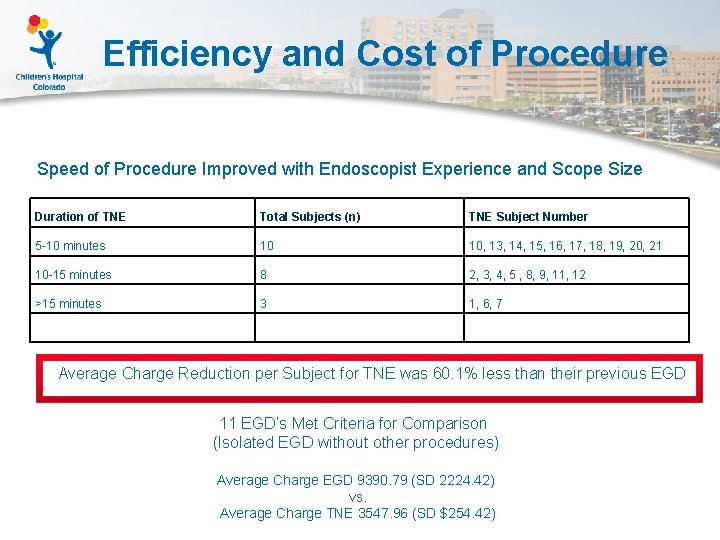
Efficiency and Cost of Procedure Speed of Procedure Improved with Endoscopist Experience and Scope Size Duration of TNE Total Subjects (n) TNE Subject Number 5 -10 minutes 10 10, 13, 14, 15, 16, 17, 18, 19, 20, 21 10 -15 minutes 8 2, 3, 4, 5 , 8, 9, 11, 12 >15 minutes 3 1, 6, 7 Average Charge Reduction per Subject for TNE was 60. 1% less than their previous EGD 11 EGD’s Met Criteria for Comparison (Isolated EGD without other procedures) Average Charge EGD 9390. 79 (SD 2224. 42) vs. Average Charge TNE 3547. 96 (SD $254. 42)

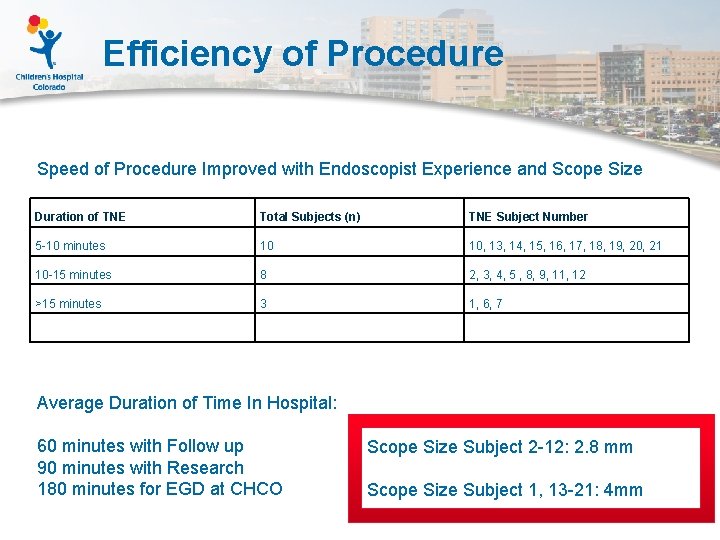
Efficiency of Procedure Speed of Procedure Improved with Endoscopist Experience and Scope Size Duration of TNE Total Subjects (n) TNE Subject Number 5 -10 minutes 10 10, 13, 14, 15, 16, 17, 18, 19, 20, 21 10 -15 minutes 8 2, 3, 4, 5 , 8, 9, 11, 12 >15 minutes 3 1, 6, 7 Average Duration of Time In Hospital: 45 -60 minutes with follow up 90 minutes with research 180 minutes for sedated EGD at CHCO
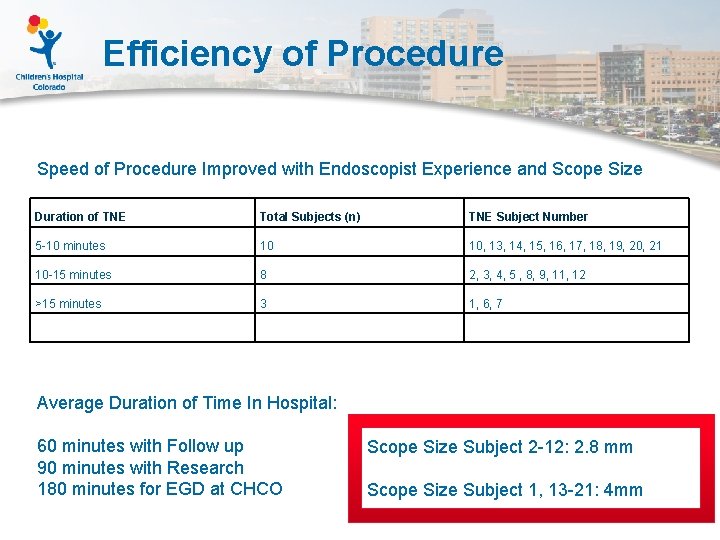
Efficiency of Procedure Speed of Procedure Improved with Endoscopist Experience and Scope Size Duration of TNE Total Subjects (n) TNE Subject Number 5 -10 minutes 10 10, 13, 14, 15, 16, 17, 18, 19, 20, 21 10 -15 minutes 8 2, 3, 4, 5 , 8, 9, 11, 12 >15 minutes 3 1, 6, 7 Average Duration of Time In Hospital: 60 minutes with Follow up 90 minutes with Research 180 minutes for EGD at CHCO Scope Size Subject 2 -12: 2. 8 mm Scope Size Subject 1, 13 -21: 4 mm
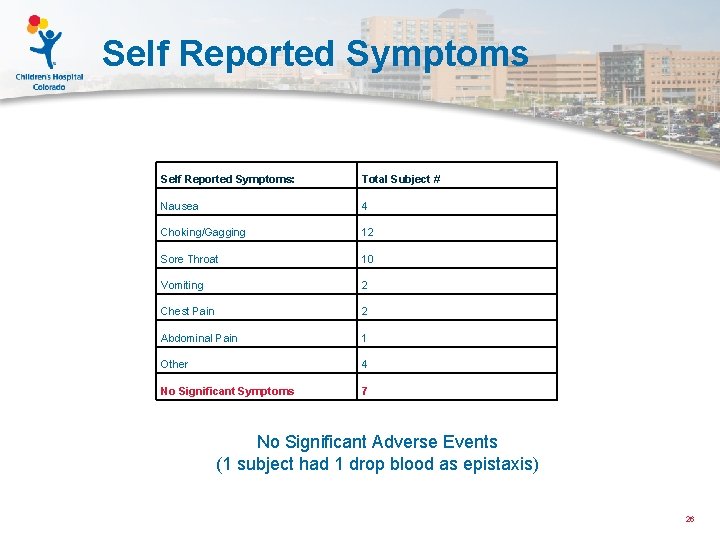
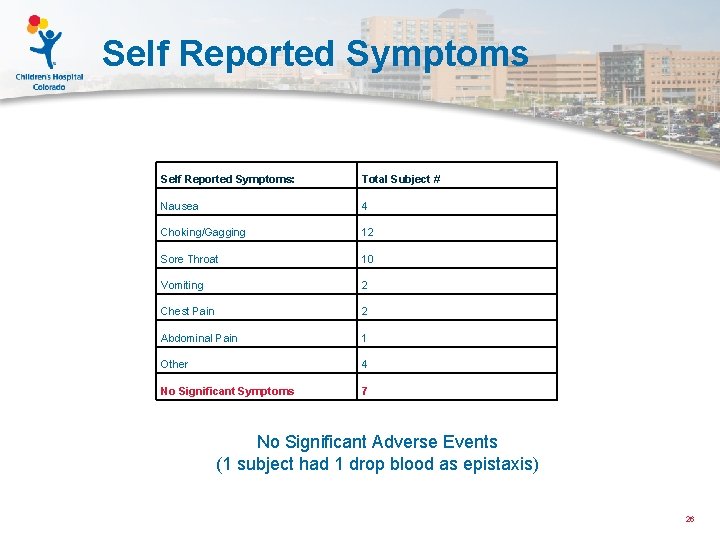
Self Reported Symptoms: Total Subject # Nausea 4 Choking/Gagging 12 Sore Throat 10 Vomiting 2 Chest Pain 2 Abdominal Pain 1 Other 4 No Significant Symptoms 7 No Significant Adverse Events (1 subject had 1 drop blood as epistaxis) 26
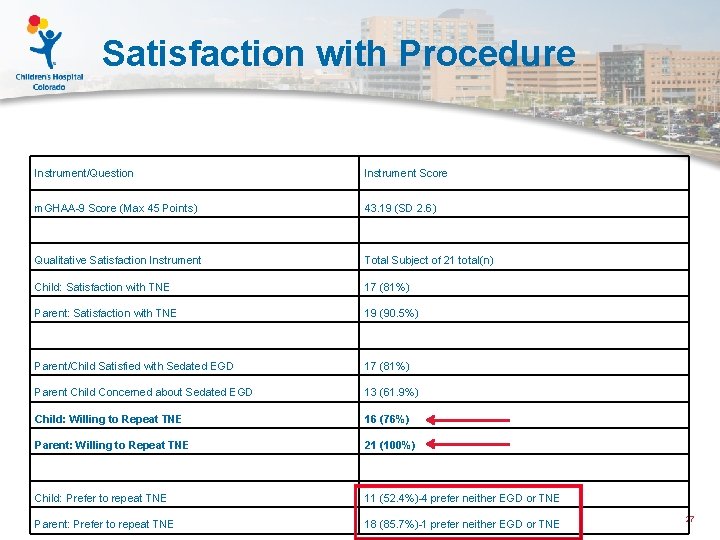
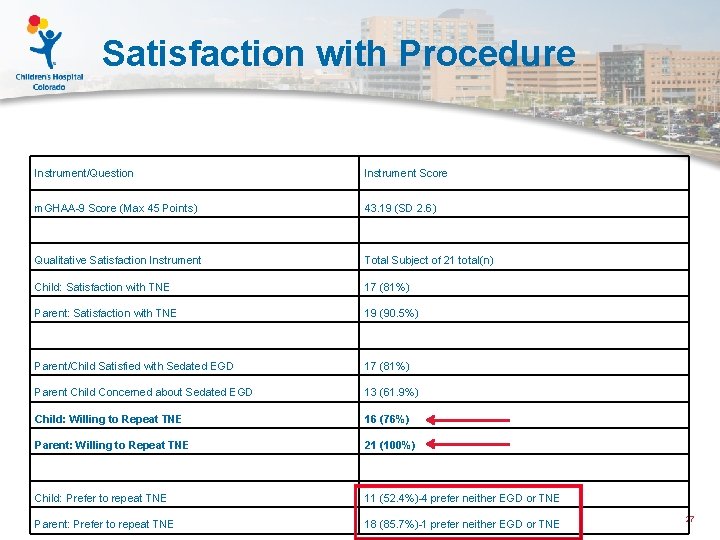
Satisfaction with Procedure Instrument/Question Instrument Score m. GHAA-9 Score (Max 45 Points) 43. 19 (SD 2. 6) Qualitative Satisfaction Instrument Total Subject of 21 total(n) Child: Satisfaction with TNE 17 (81%) Parent: Satisfaction with TNE 19 (90. 5%) Parent/Child Satisfied with Sedated EGD 17 (81%) Parent Child Concerned about Sedated EGD 13 (61. 9%) Child: Willing to Repeat TNE 16 (76%) Parent: Willing to Repeat TNE 21 (100%) Child: Prefer to repeat TNE 11 (52. 4%)-4 prefer neither EGD or TNE Parent: Prefer to repeat TNE 18 (85. 7%)-1 prefer neither EGD or TNE 27
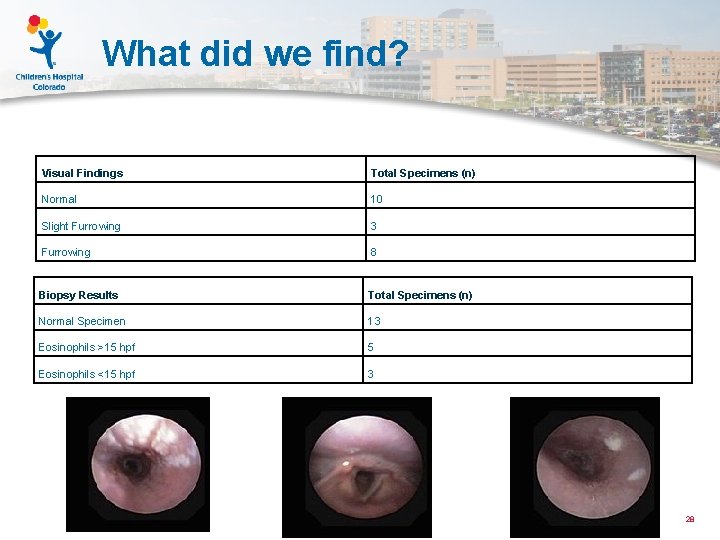
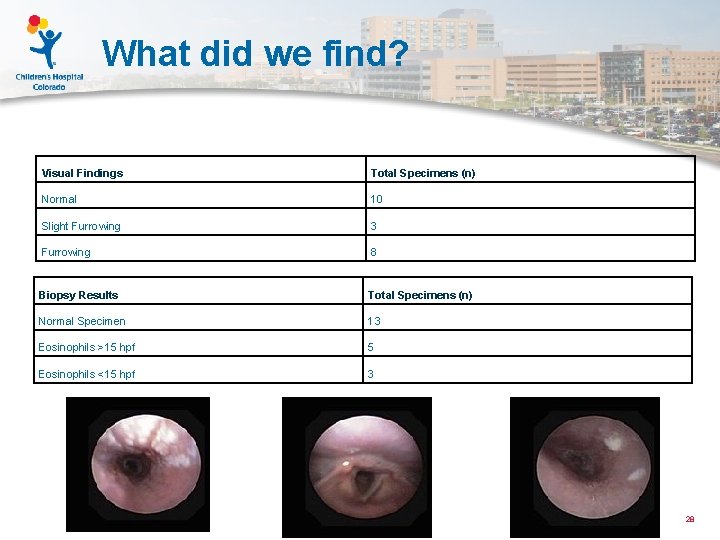
What did we find? Visual Findings Total Specimens (n) Normal 10 Slight Furrowing 3 Furrowing 8 Biopsy Results Total Specimens (n) Normal Specimen 13 Eosinophils >15 hpf 5 Eosinophils <15 hpf 3 28
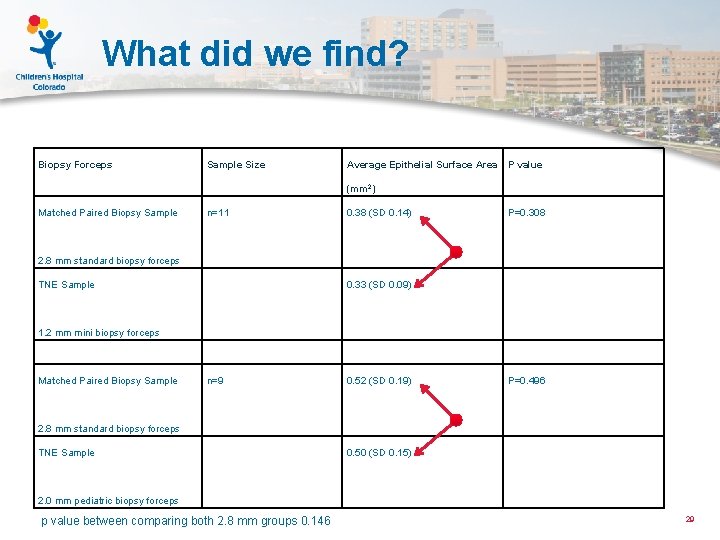
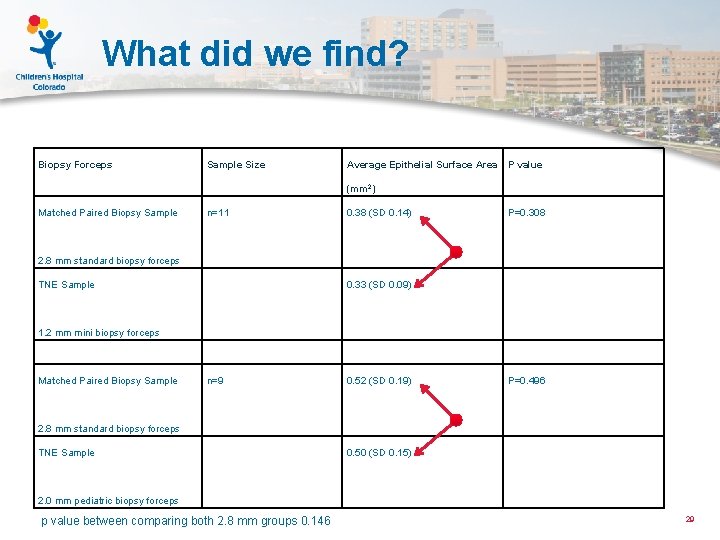
What did we find? Biopsy Forceps Sample Size Average Epithelial Surface Area P value (mm 2) Matched Paired Biopsy Sample n=11 0. 38 (SD 0. 14) P=0. 308 0. 33 (SD 0. 09) Matched Paired Biopsy Sample n=9 0. 52 (SD 0. 19) P=0. 496 0. 50 (SD 0. 15) 2. 8 mm standard biopsy forceps TNE Sample 1. 2 mm mini biopsy forceps 2. 8 mm standard biopsy forceps TNE Sample 2. 0 mm pediatric biopsy forceps p value between comparing both 2. 8 mm groups 0. 146 29

What did we find? Biopsy with Active Eo. E using 2. 8 mm forceps (Subject 2) Surface Area 0. 10 mm 2 Biopsy from same patient with Active Eo. E using 1. 2 mm forceps (Subject 2) Surface Area 0. 12 mm 2 30
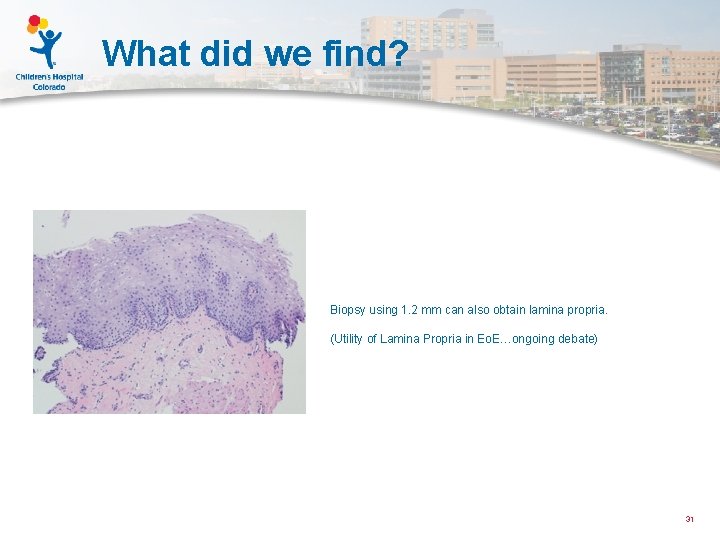
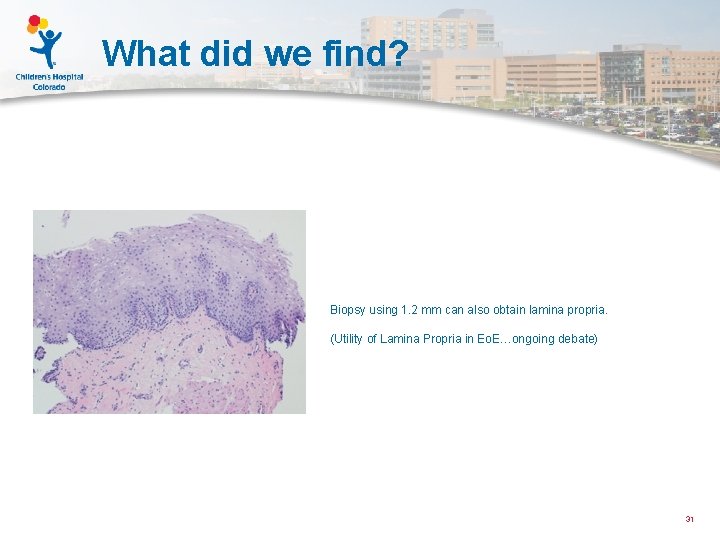
What did we find? Biopsy using 1. 2 mm can also obtain lamina propria. (Utility of Lamina Propria in Eo. E…ongoing debate) 31
Family Feedback 1. It did not require anesthesia, it took less time and it was not painful. 2. It was quick and he didn’t need to be under anesthesia. 3. Short duration of procedure. No anesthesia. Not Scary. Did have sore throat for 24 hours after. 4. She did not have to go under anesthesia 5. A lot less discomfort and time with endoscopies (TNE) 6. She was uncomfortable and in a lot of pain during and shortly after. Took to long 7. He did not have to be put to sleep which was great. 8. Minimally invasive 32
Conclusion and Future Conclusion: Unsedated TNE is an effective, preferred, lower cost procedure for monitoring the esophageal mucosal of children with Eo. E 33
What has happened since? Demographics: 5 years of age to 21 years of age Total # of TNE: 143 (March 2014 -October 2016, 122 Since January 2015) Adverse Events: None significant (3 scant epistaxis, 7 emesis) Specimen Evaluation: all adequate Being used for follow up of Barrett’s esophagus, Reflux Esophagitis, Eo. E, Gasrtitis, and TEF monitoring. Ongoing follow up study of specimen adequacy and use in other conditions on 34
What has happened since? Refinements: 1. New distraction techniques 2. New topical anesthesia methods 3. Newer scope technologies 4. Disposable Micro Forceps 5. Improving work flow 6. Training of others 7. Expansion and modification of in office procedures to other areas 35
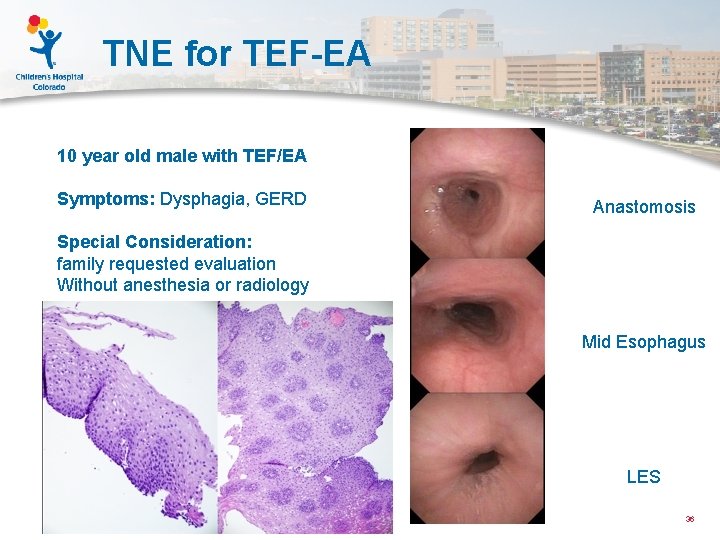
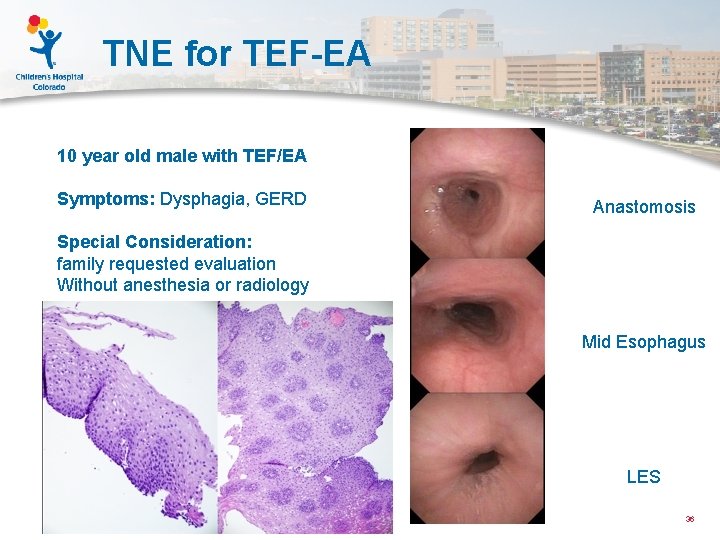
TNE for TEF-EA 10 year old male with TEF/EA Symptoms: Dysphagia, GERD Anastomosis Special Consideration: family requested evaluation Without anesthesia or radiology Mid Esophagus LES 36
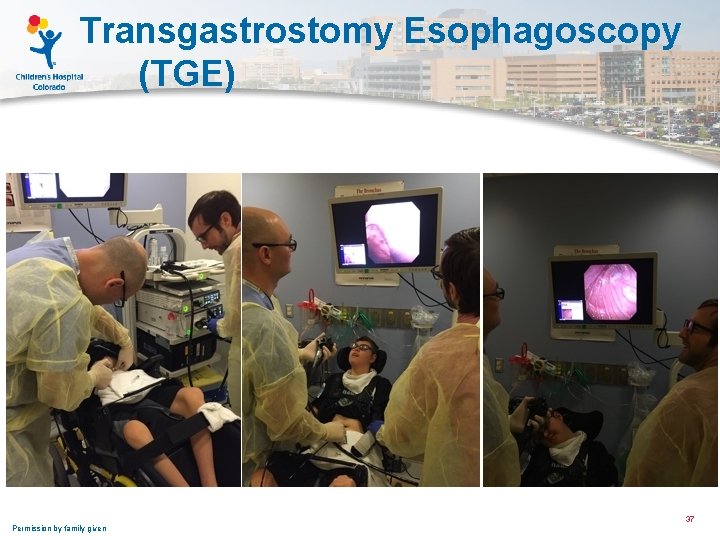
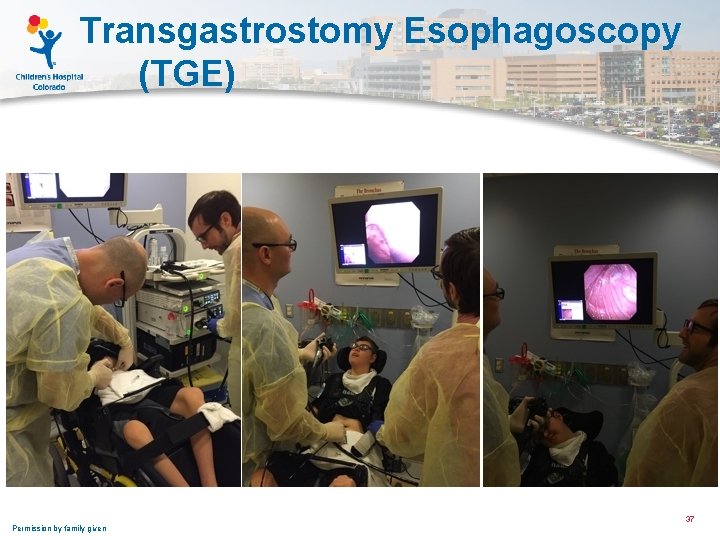
Transgastrostomy Esophagoscopy (TGE) Permission by family given 37
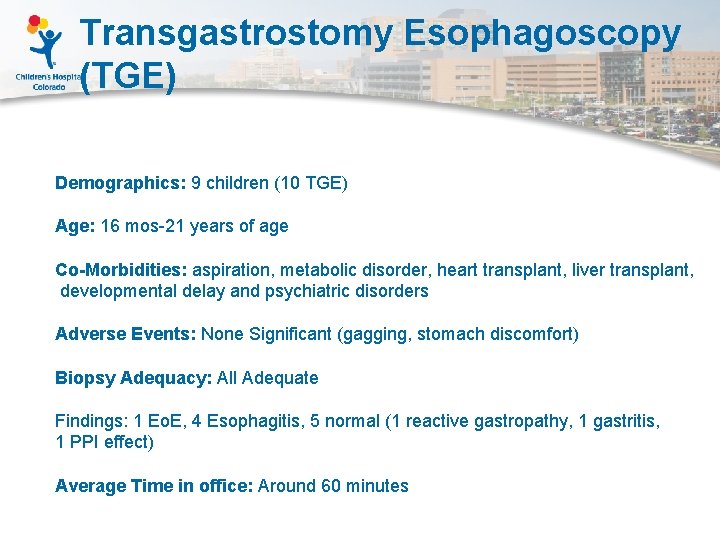
Transgastrostomy Esophagoscopy (TGE) Demographics: 9 children (10 TGE) Age: 16 mos-21 years of age Co-Morbidities: aspiration, metabolic disorder, heart transplant, liver transplant, developmental delay and psychiatric disorders Adverse Events: None Significant (gagging, stomach discomfort) Biopsy Adequacy: All Adequate Findings: 1 Eo. E, 4 Esophagitis, 5 normal (1 reactive gastropathy, 1 gastritis, 1 PPI effect) Average Time in office: Around 60 minutes
Thank You and Questions Aerodigestive Team Ben Corbett Emily Deboer Jacklyn Deck Robin Deterding Sparrow Helland Jenny Maybee Krystal Mesenbrink Jeremy Prager Bethany Thomas Todd Wine Nora Janosy Melissa Brooks Clint Smith GEDP Team Dan Atkins David Fleischer Glenn Furuta Calies Menard-Katcher DHI Team David Brumbaugh Robert Kramer Ron Sokol Ed Hoffenberg 39
 Scott schraff ent
Scott schraff ent Long shot vs wide shot
Long shot vs wide shot Factory office plan
Factory office plan Pediatric first aid for caregivers
Pediatric first aid for caregivers Aya addema xxx
Aya addema xxx Restricted utilitarianism
Restricted utilitarianism Extreme and mean ratio
Extreme and mean ratio Fear factor success and risk in extreme sports
Fear factor success and risk in extreme sports Extreme fear and apprehension
Extreme fear and apprehension Extreme programming
Extreme programming Unc chapel hill hematology oncology
Unc chapel hill hematology oncology Miami pediatric nephrology seminar
Miami pediatric nephrology seminar Define pediatric dentistry
Define pediatric dentistry Headache red flags
Headache red flags Pediatric seizures
Pediatric seizures Wikimedia
Wikimedia Pediatric maintenance fluids 4-2-1 rule
Pediatric maintenance fluids 4-2-1 rule Pediatric vision scanner
Pediatric vision scanner Pediatric urologist atlanta ga
Pediatric urologist atlanta ga Pediatric heart rate chart
Pediatric heart rate chart Cavity class 4
Cavity class 4 Trends in pediatric nursing 2020
Trends in pediatric nursing 2020 Common pediatric medications
Common pediatric medications Volutrol
Volutrol Hematocrit normal
Hematocrit normal Pediatric exercise physiology
Pediatric exercise physiology Pediatric hematology/oncology board review questions
Pediatric hematology/oncology board review questions H and ts of cardiac arrest
H and ts of cardiac arrest Pediatric bls algorithm
Pediatric bls algorithm Basic life support sequence
Basic life support sequence Good respiration rate
Good respiration rate Headss assessment
Headss assessment Ticls pediatric
Ticls pediatric Nf1pn
Nf1pn Modern concept of paediatric nursing
Modern concept of paediatric nursing Modern concept in child health care
Modern concept in child health care Mary bridge neurology clinic
Mary bridge neurology clinic Pediatric coma scale
Pediatric coma scale Dr br vacher
Dr br vacher Iv fluid computation
Iv fluid computation