Endocrine investigation of a case of adrenal insufficiency


- Slides: 22
Endocrine investigation of a case of adrenal insufficiency
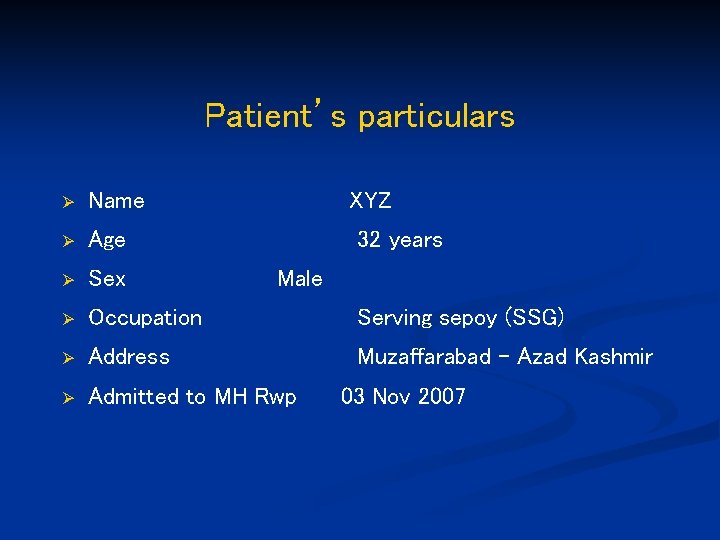
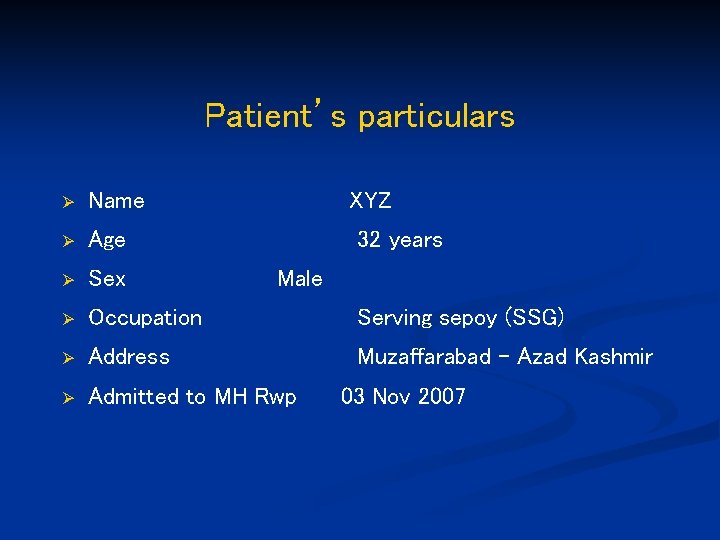
Patient’s particulars Ø Name XYZ Ø Age Ø Sex Ø Occupation Serving sepoy (SSG) Ø Address Muzaffarabad - Azad Kashmir Ø Admitted to MH Rwp 32 years Male 03 Nov 2007
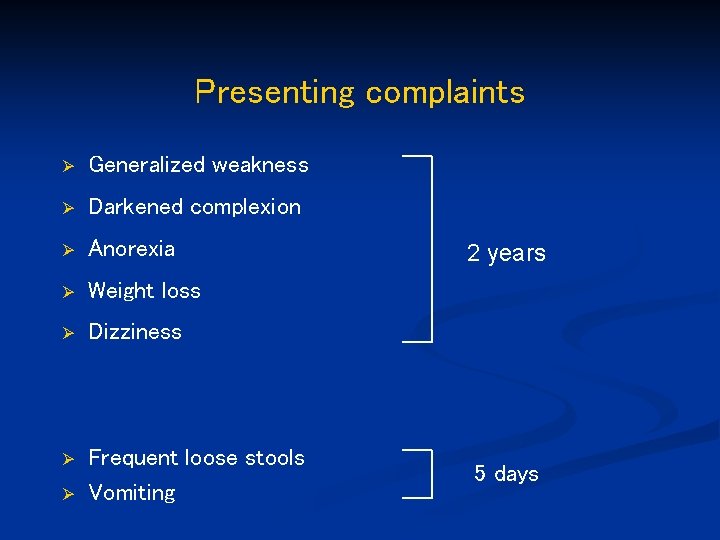
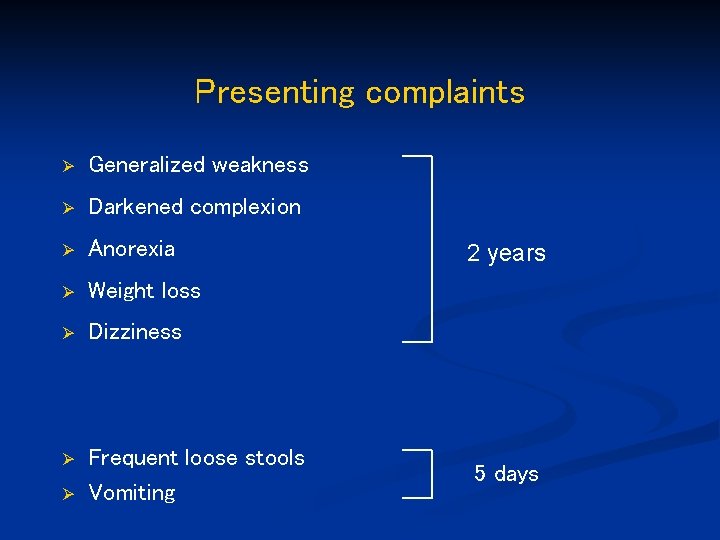
Presenting complaints Ø Generalized weakness Ø Darkened complexion Ø Anorexia Ø Weight loss Ø Dizziness Ø Frequent loose stools Vomiting Ø 2 years 5 days
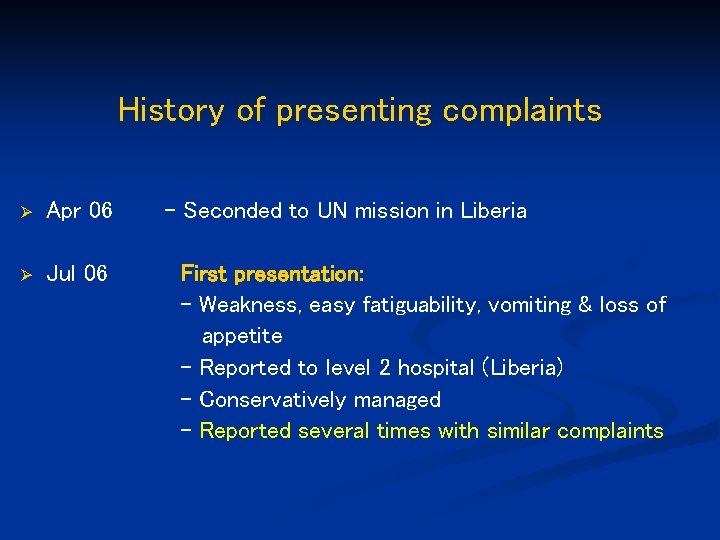
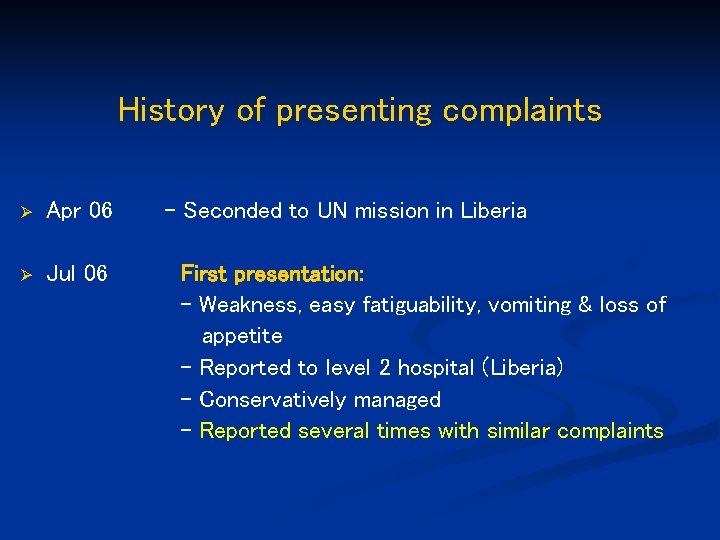
History of presenting complaints Ø Apr 06 Ø Jul 06 - Seconded to UN mission in Liberia First presentation: - Weakness, easy fatiguability, vomiting & loss of appetite - Reported to level 2 hospital (Liberia) - Conservatively managed - Reported several times with similar complaints
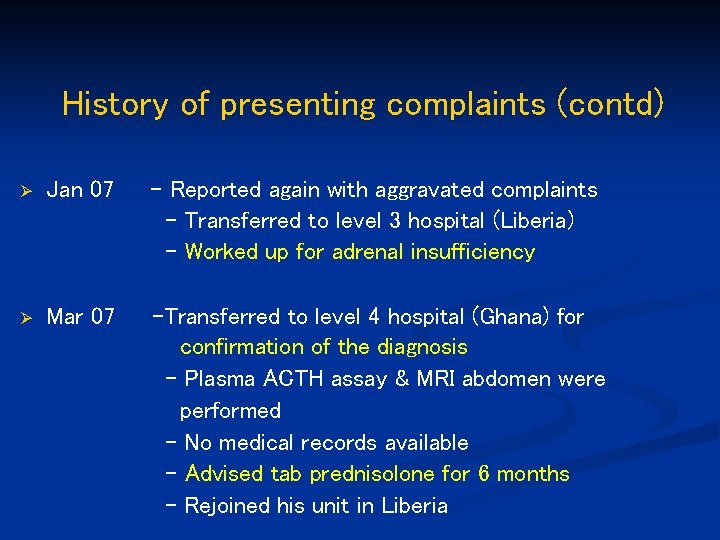
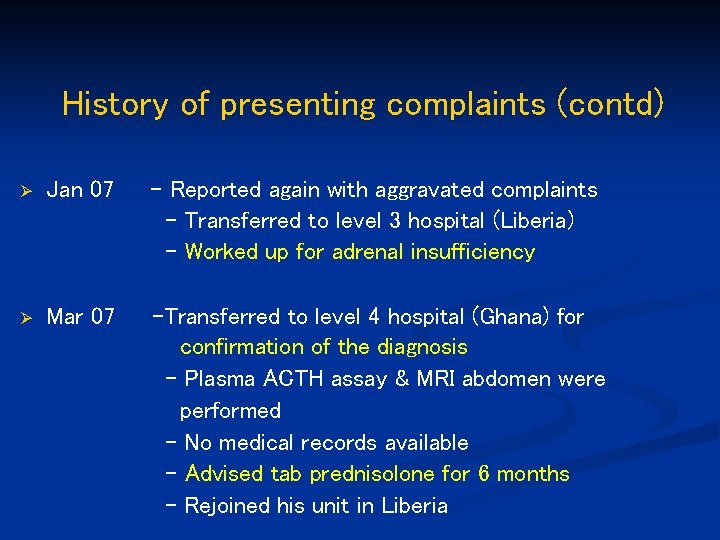
History of presenting complaints (contd) Ø Jan 07 - Reported again with aggravated complaints - Transferred to level 3 hospital (Liberia) - Worked up for adrenal insufficiency Ø Mar 07 -Transferred to level 4 hospital (Ghana) for confirmation of the diagnosis - Plasma ACTH assay & MRI abdomen were performed - No medical records available - Advised tab prednisolone for 6 months - Rejoined his unit in Liberia
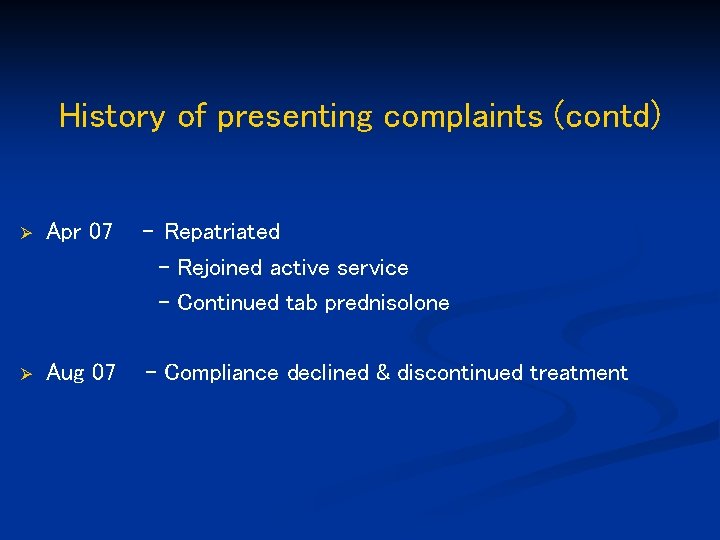
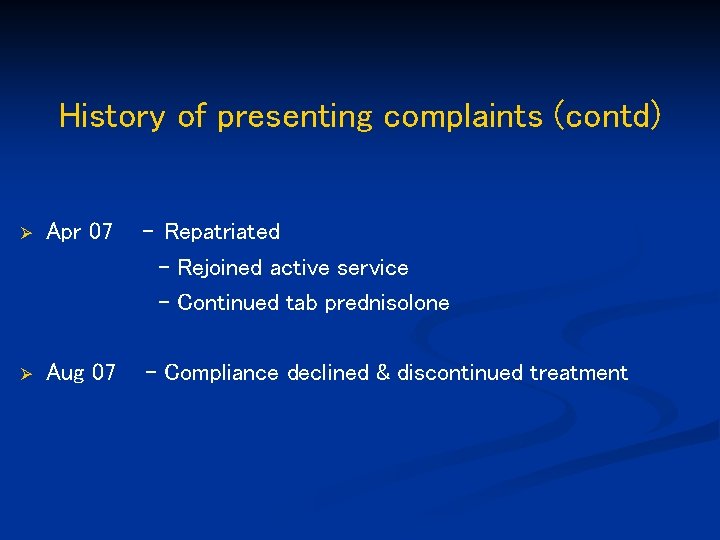
History of presenting complaints (contd) Ø Apr 07 - Repatriated - Rejoined active service - Continued tab prednisolone Ø Aug 07 - Compliance declined & discontinued treatment
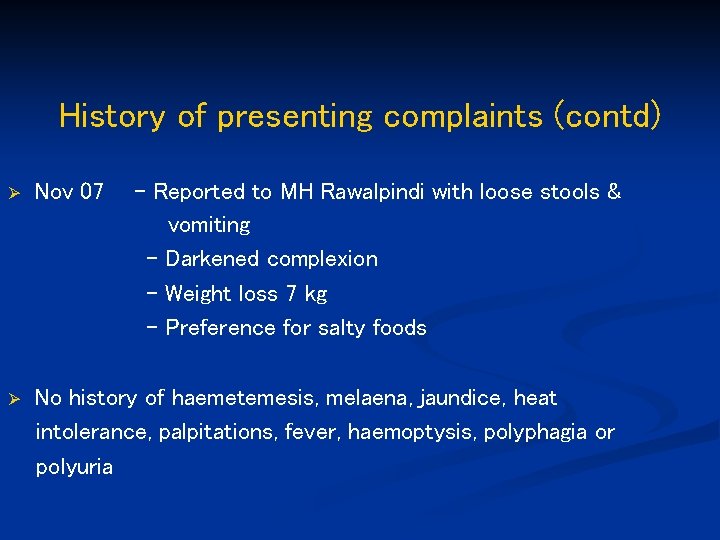
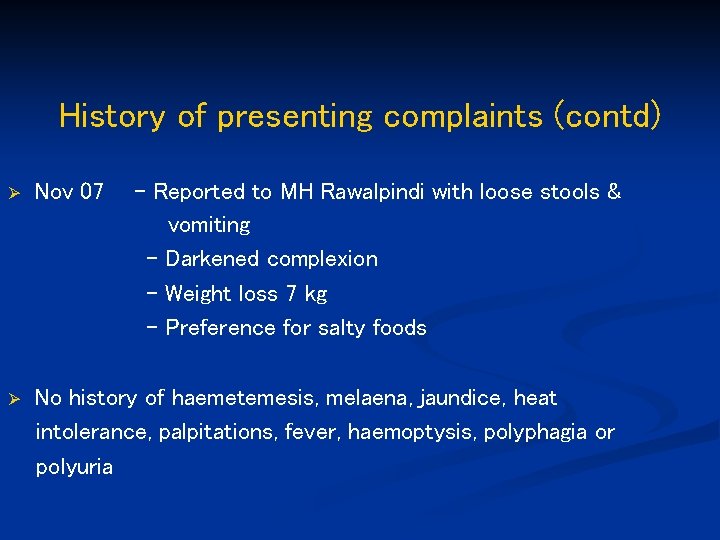
History of presenting complaints (contd) Ø Nov 07 - Reported to MH Rawalpindi with loose stools & vomiting - Darkened complexion - Weight loss 7 kg - Preference for salty foods Ø No history of haemetemesis, melaena, jaundice, heat intolerance, palpitations, fever, haemoptysis, polyphagia or polyuria
History (contd) Ø Ø Ø Past history Family history Personal history Dietary history Drug history Not contributory
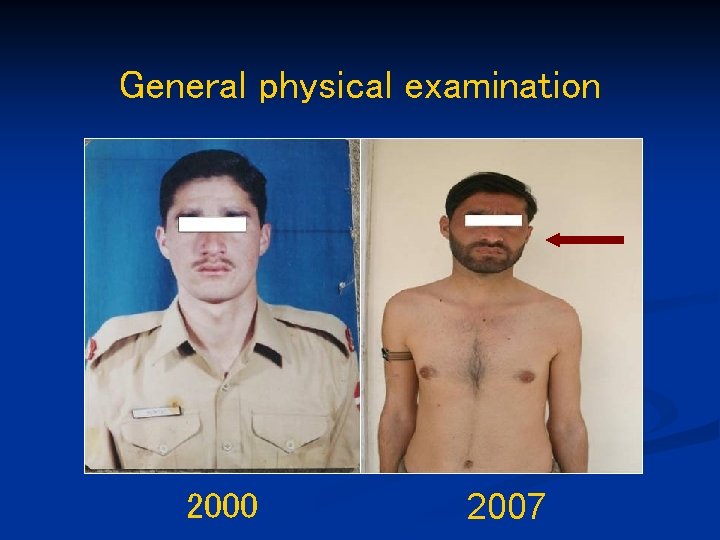
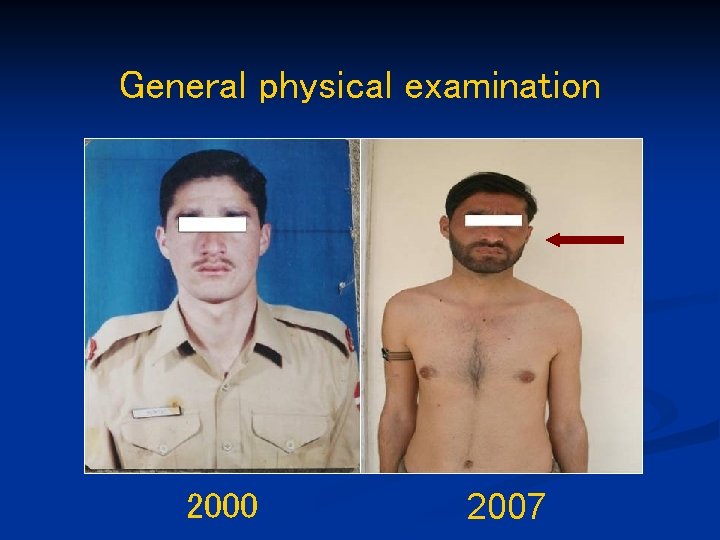
General physical examination 2000 2007
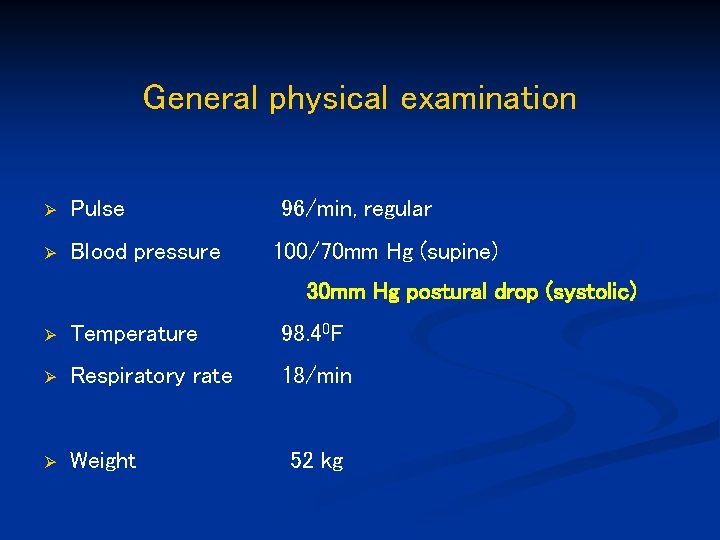
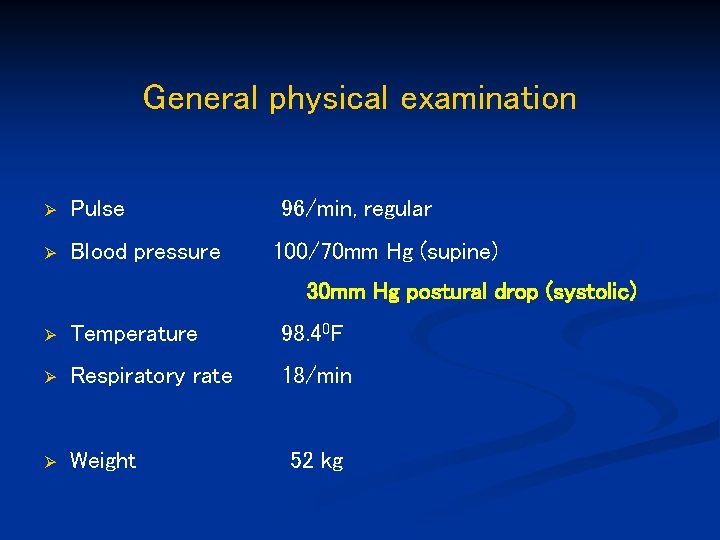
General physical examination Ø Pulse Ø Blood pressure 96/min, regular 100/70 mm Hg (supine) 30 mm Hg postural drop (systolic) Ø Temperature 98. 40 F Ø Respiratory rate 18/min Ø Weight 52 kg
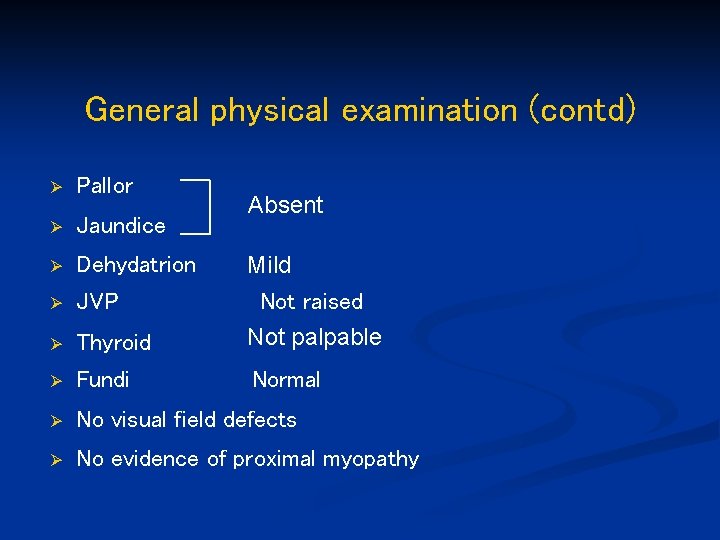
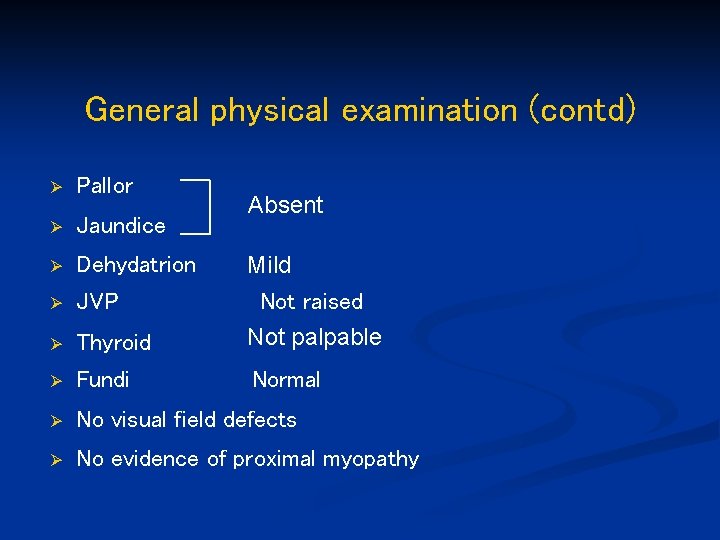
General physical examination (contd) Ø Pallor Ø Jaundice Ø Dehydatrion Mild Ø JVP Ø Thyroid Not raised Not palpable Ø Fundi Normal Ø No visual field defects Ø No evidence of proximal myopathy Absent
Systemic examination Ø Central nervous system Ø Cardiovascular system Ø Respiratory system Ø Gastrointestinal system Unremarkable

Provisional diagnosis Adrenal insufficiency
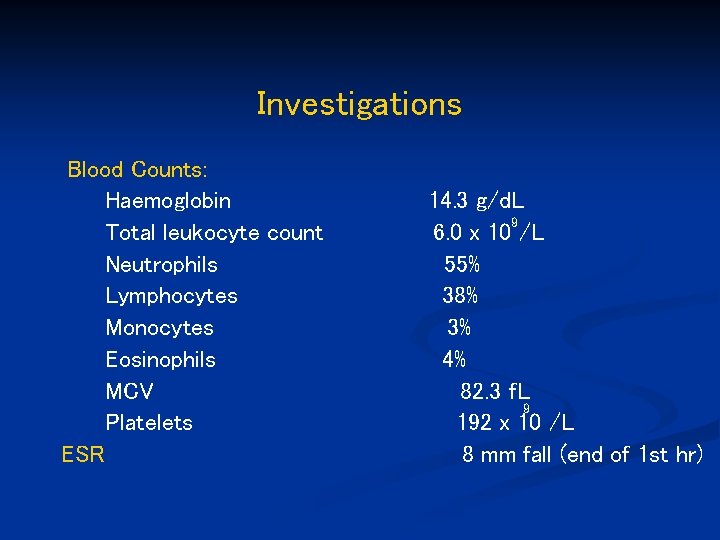
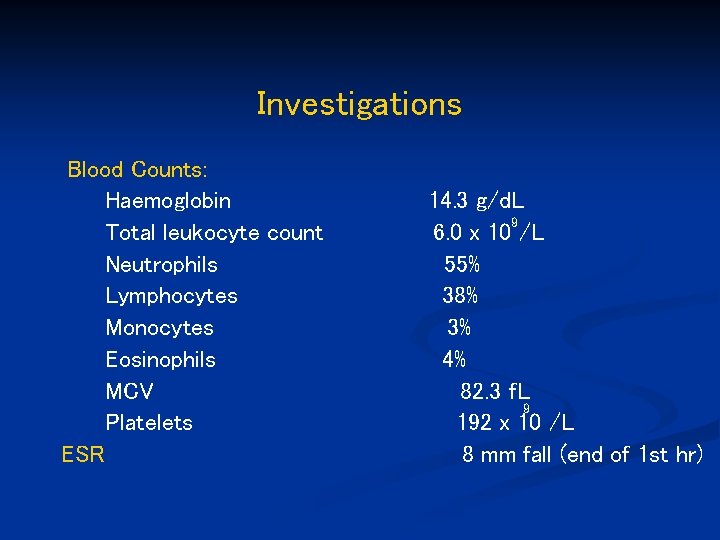
Investigations Blood Counts: Haemoglobin Total leukocyte count Neutrophils Lymphocytes Monocytes Eosinophils MCV Platelets ESR 14. 3 g/d. L 9 6. 0 x 10 /L 55% 38% 3% 4% 82. 3 f. L 9 192 x 10 /L 8 mm fall (end of 1 st hr)
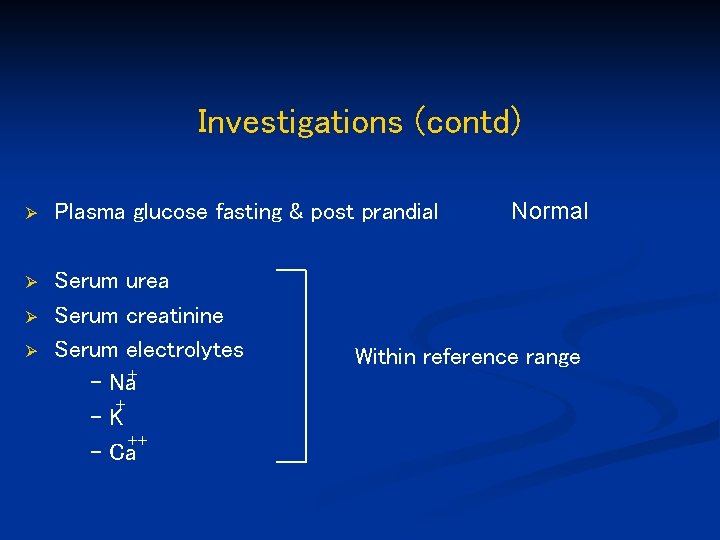
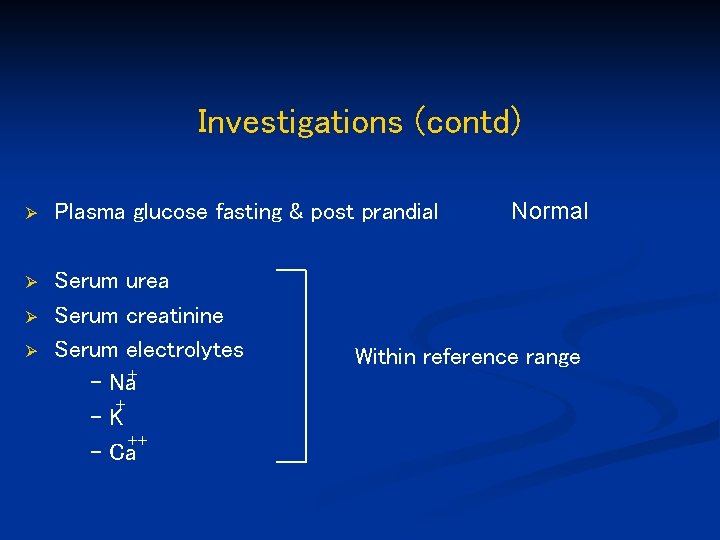
Investigations (contd) Ø Plasma glucose fasting & post prandial Ø Serum urea Serum creatinine Serum electrolytes - Na+ + -K - Ca++ Ø Ø Normal Within reference range
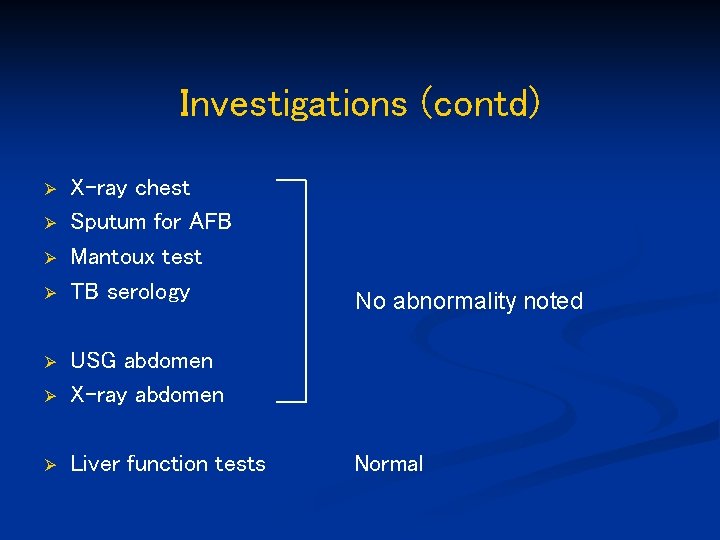
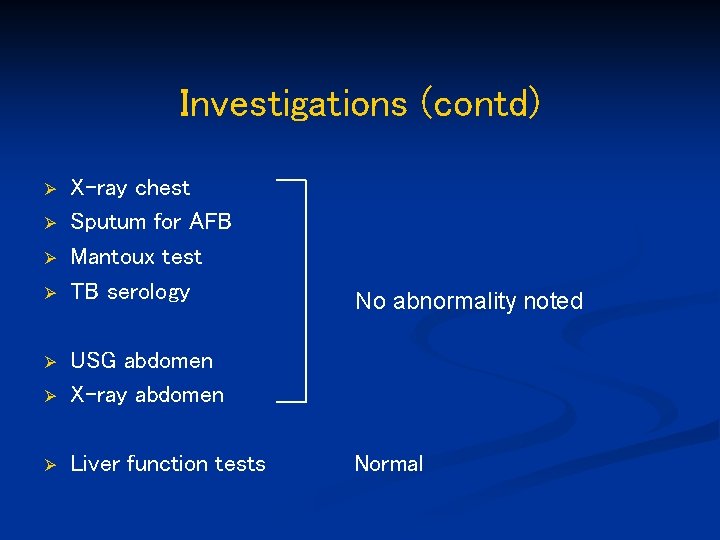
Investigations (contd) Ø Ø X-ray chest Sputum for AFB Mantoux test TB serology Ø USG abdomen X-ray abdomen Ø Liver function tests Ø No abnormality noted Normal

Investigations (contd) Ø Ø Ø Serum cortisol Plasma ACTH Serum Plasma Serum TSH PTH FSH LH 9. 0 >1000 (5 -25) (8 -79) µg/d. L pg/m. L Within reference range
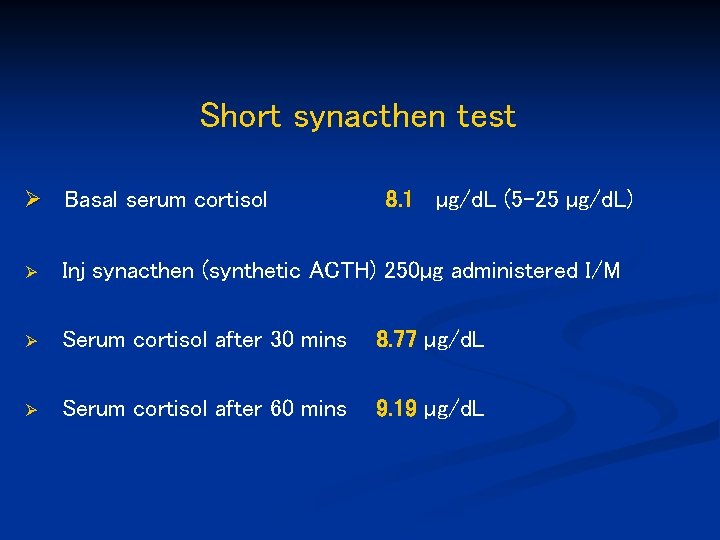
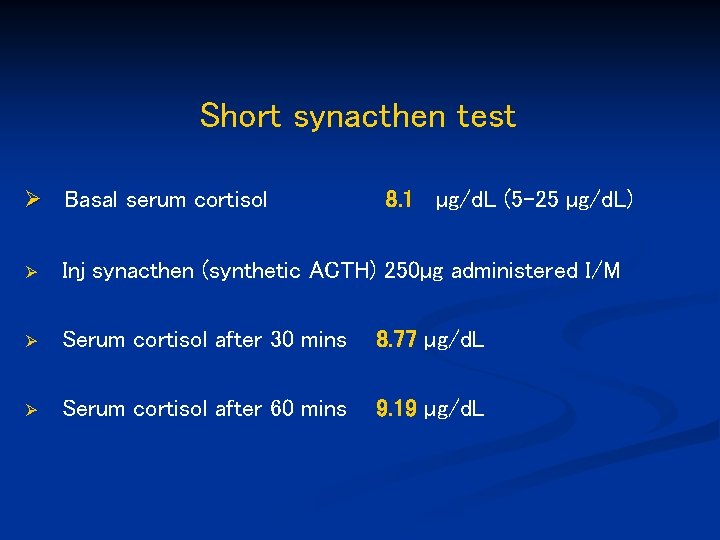
Short synacthen test Ø Basal serum cortisol 8. 1 µg/d. L (5 -25 µg/d. L) Ø Inj synacthen (synthetic ACTH) 250µg administered I/M Ø Serum cortisol after 30 mins 8. 77 µg/d. L Ø Serum cortisol after 60 mins 9. 19 µg/d. L
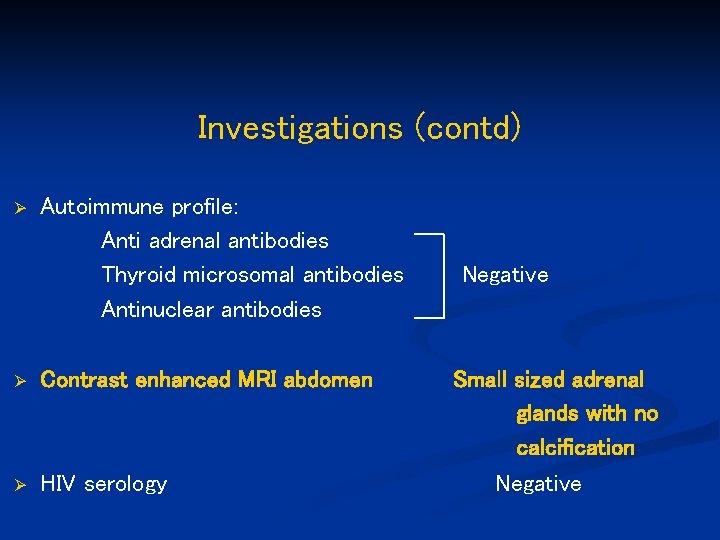
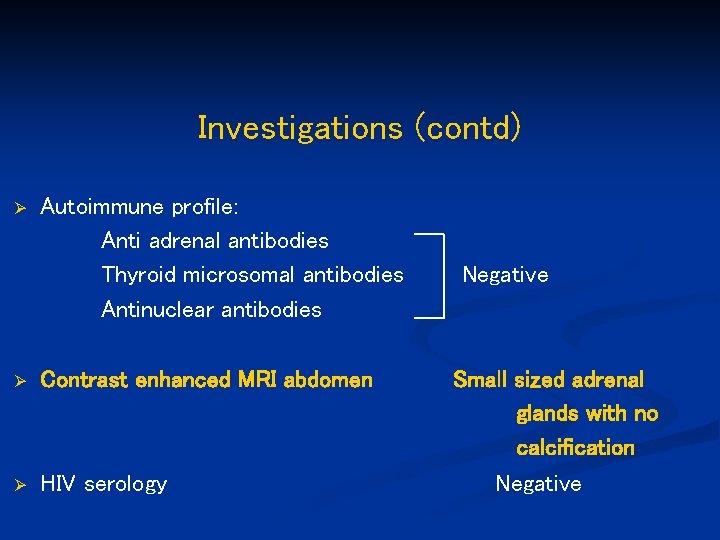
Investigations (contd) Ø Autoimmune profile: Anti adrenal antibodies Thyroid microsomal antibodies Antinuclear antibodies Ø Contrast enhanced MRI abdomen Ø HIV serology Negative Small sized adrenal glands with no calcification Negative
Final diagnosis Idiopathic adrenal insufficiency
Management Ø Inj ciprofloxacin 500 mg I/V twice daily Replacement therapy: Ø Tab prednisolone 10 mg (morning) and 5 mg (evening) Ø Tab fludrocortisone 0. 05 mg once daily
Follow up Ø Appetite has improved Ø Gained 4 kg of weight Ø No postural variation in blood pressure
 Passive insufficiency
Passive insufficiency Divergence insufficiency
Divergence insufficiency Eye lesions
Eye lesions How to diagnose epi
How to diagnose epi Convergence insufficiency latham
Convergence insufficiency latham Pseudo convergence insufficiency
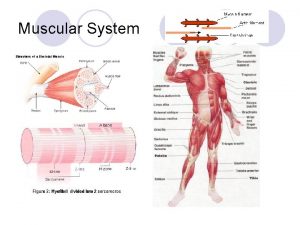
Pseudo convergence insufficiency Muscle movement
Muscle movement Chello.hu
Chello.hu Best case worst case average case
Best case worst case average case Larynx dissection
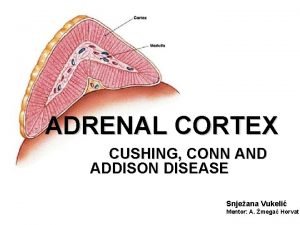
Larynx dissection Adrenal medulla cortex
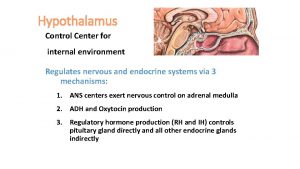
Adrenal medulla cortex Craniosacral region
Craniosacral region Hymen
Hymen Hypoglycemic shock
Hypoglycemic shock Adrenal korteks hormonları
Adrenal korteks hormonları The adrenal medullae secrete
The adrenal medullae secrete Conn vs addison
Conn vs addison Estadiamento de tanner
Estadiamento de tanner Adrenal gland regions
Adrenal gland regions Virilisation in females
Virilisation in females Adrenal kriz acilci
Adrenal kriz acilci Addison's disease vs cushing's syndrome
Addison's disease vs cushing's syndrome Adrenal gland
Adrenal gland