Dementia muddling along Steve Iliffe Professor of Primary

- Slides: 36
Dementia: muddling along? Steve Iliffe Professor of Primary Care for Older People University College London Kent Academic Primary Care Unit Wednesday June 10 th 2015
What is dementia? • A complex multi-factorial syndrome. Querfurth H , Laferla M Alzheimer’s Disease N. Engl J Med 2010; 362: 329 -44 • Memory loss plus one other impaired cognitive domain • No rocket science (except scanning) 2
Scale of the problem • Prevalence of dementia syndrome may double by 2040? • Costs of health & social care for people with dementia exceed those for cancer, heart disease and stroke combined Alzheimer’s Society 3
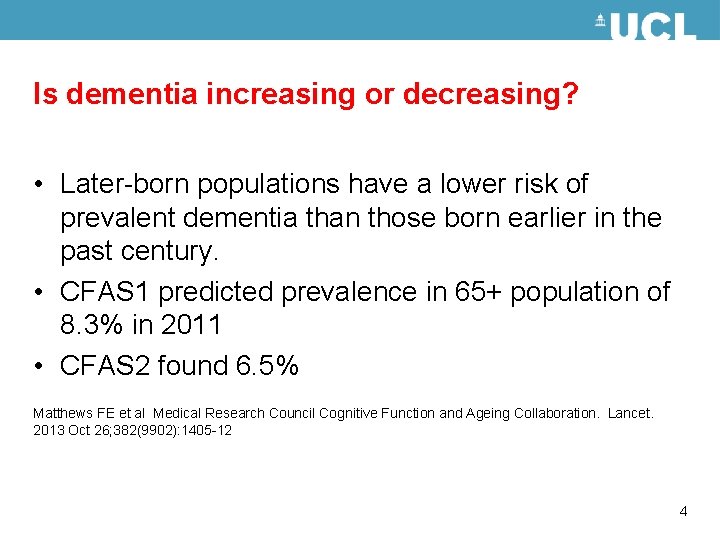
Is dementia increasing or decreasing? • Later-born populations have a lower risk of prevalent dementia than those born earlier in the past century. • CFAS 1 predicted prevalence in 65+ population of 8. 3% in 2011 • CFAS 2 found 6. 5% Matthews FE et al Medical Research Council Cognitive Function and Ageing Collaboration. Lancet. 2013 Oct 26; 382(9902): 1405 -12 4
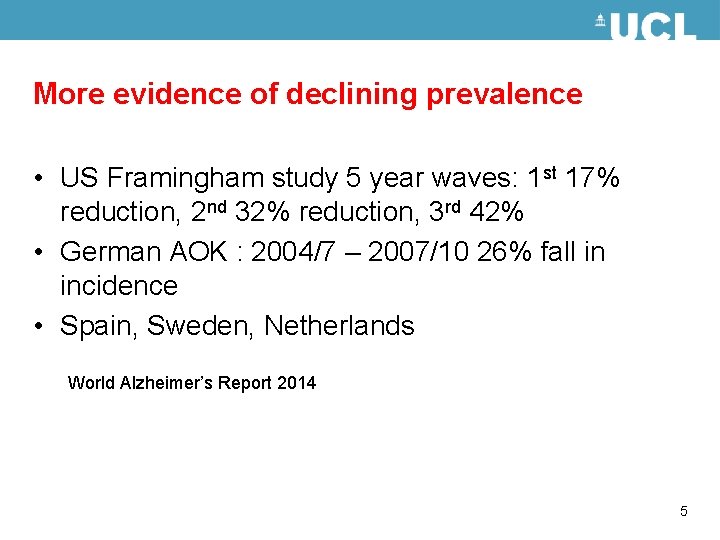
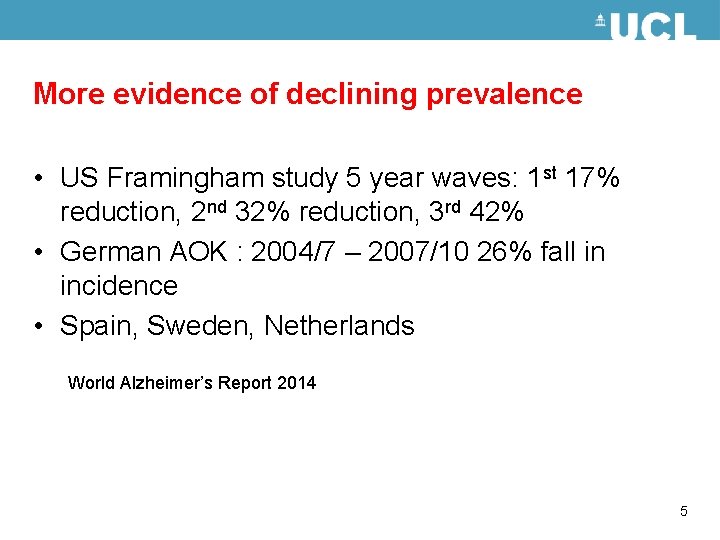
More evidence of declining prevalence • US Framingham study 5 year waves: 1 st 17% reduction, 2 nd 32% reduction, 3 rd 42% • German AOK : 2004/7 – 2007/10 26% fall in incidence • Spain, Sweden, Netherlands World Alzheimer’s Report 2014 5
Recognition How do you know you are cognitively normal? 6
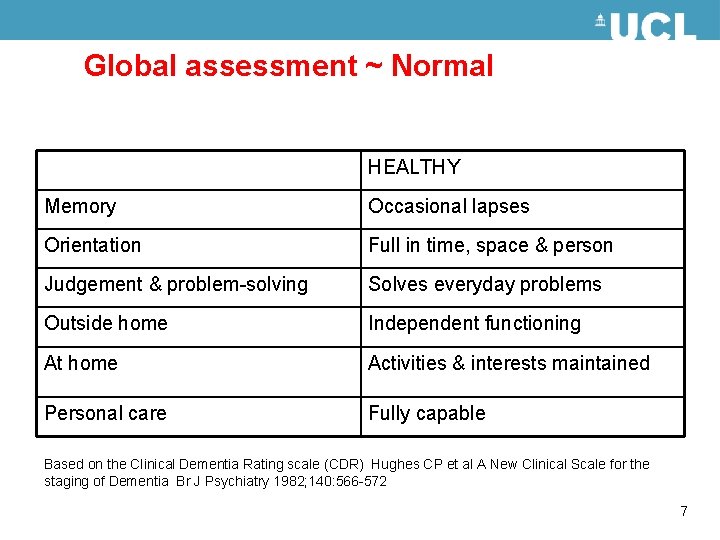
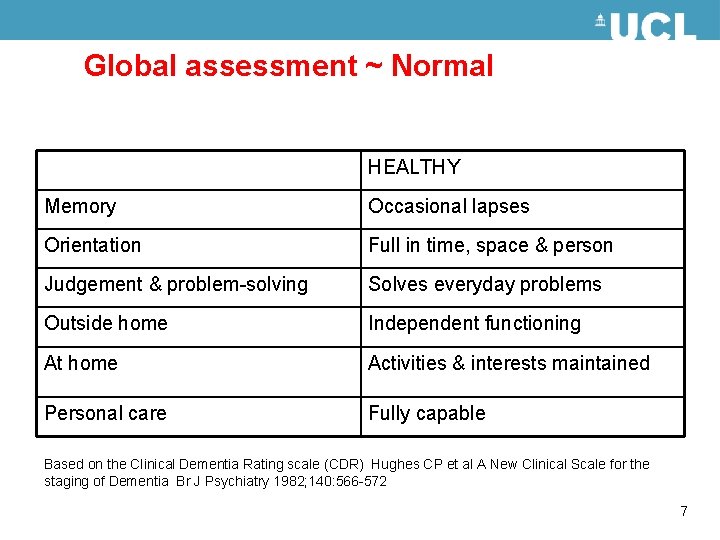
Global assessment ~ Normal HEALTHY Memory Occasional lapses Orientation Full in time, space & person Judgement & problem-solving Solves everyday problems Outside home Independent functioning At home Activities & interests maintained Personal care Fully capable Based on the Clinical Dementia Rating scale (CDR) Hughes CP et al A New Clinical Scale for the staging of Dementia Br J Psychiatry 1982; 140: 566 -572 7
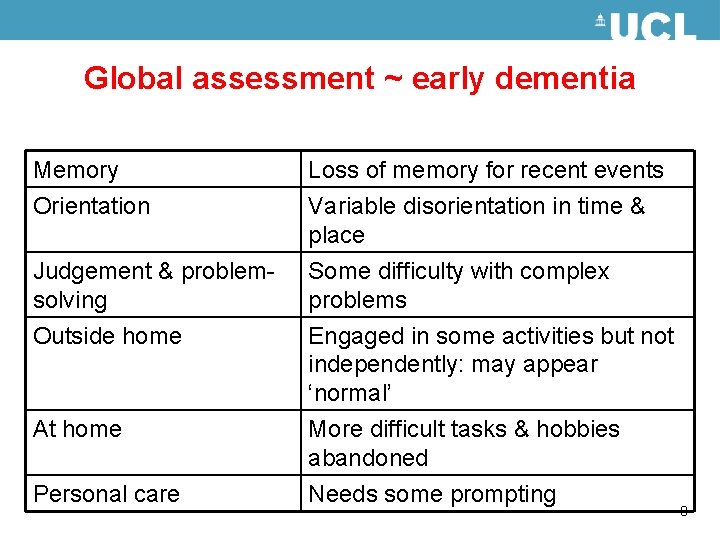
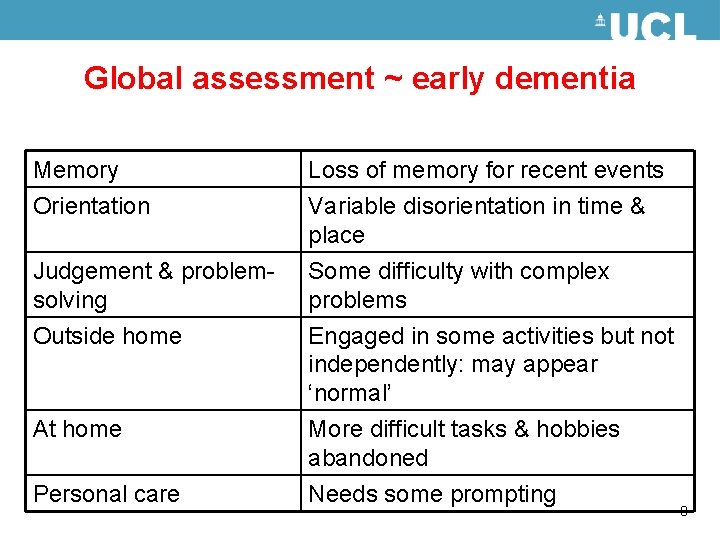
Global assessment ~ early dementia Memory Loss of memory for recent events Orientation Variable disorientation in time & place Judgement & problemsolving Outside home Some difficulty with complex problems Engaged in some activities but not independently: may appear ‘normal’ At home More difficult tasks & hobbies abandoned Personal care Needs some prompting 8
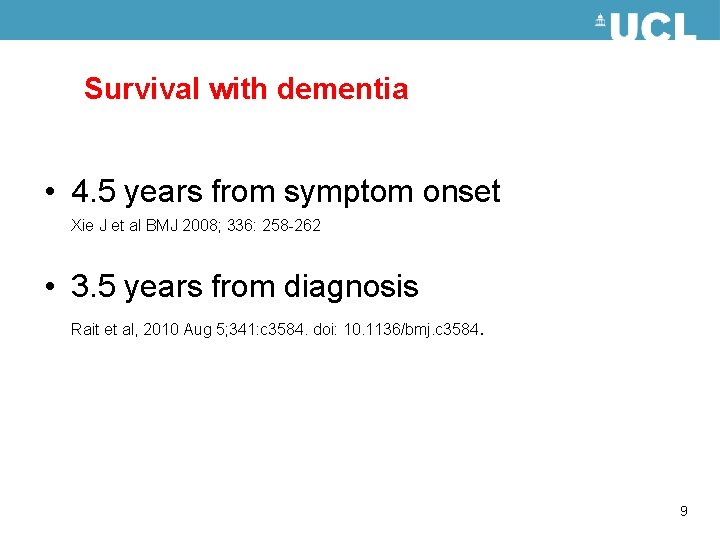
Survival with dementia • 4. 5 years from symptom onset Xie J et al BMJ 2008; 336: 258 -262 • 3. 5 years from diagnosis Rait et al, 2010 Aug 5; 341: c 3584. doi: 10. 1136/bmj. c 3584 . 9
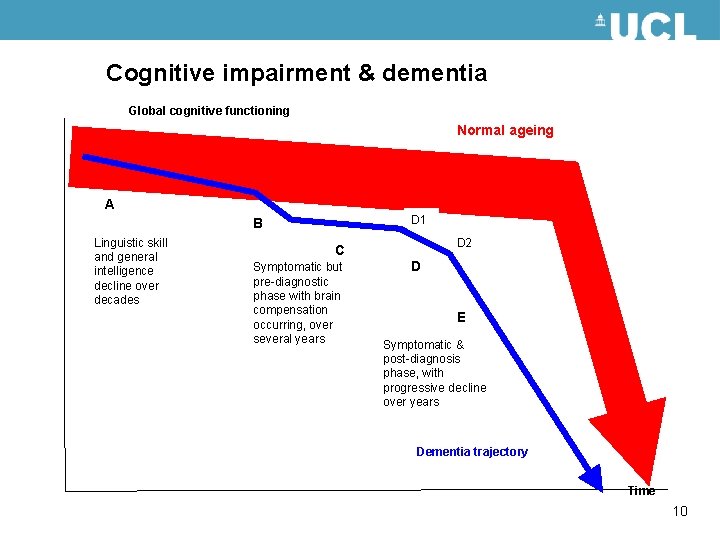
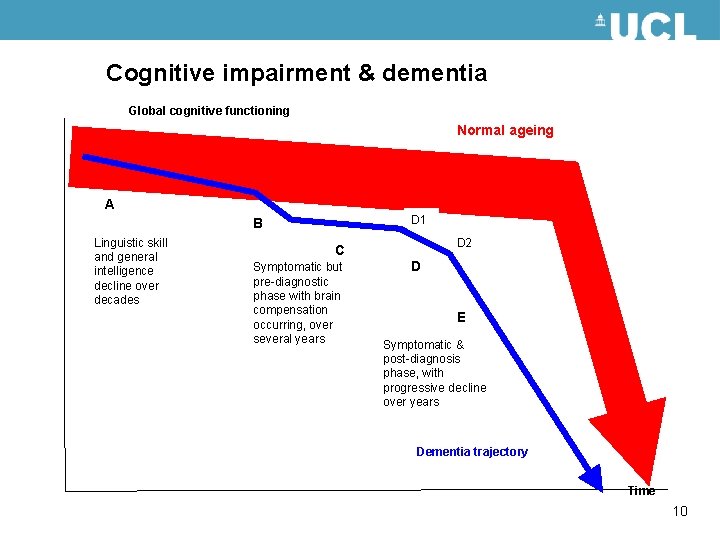
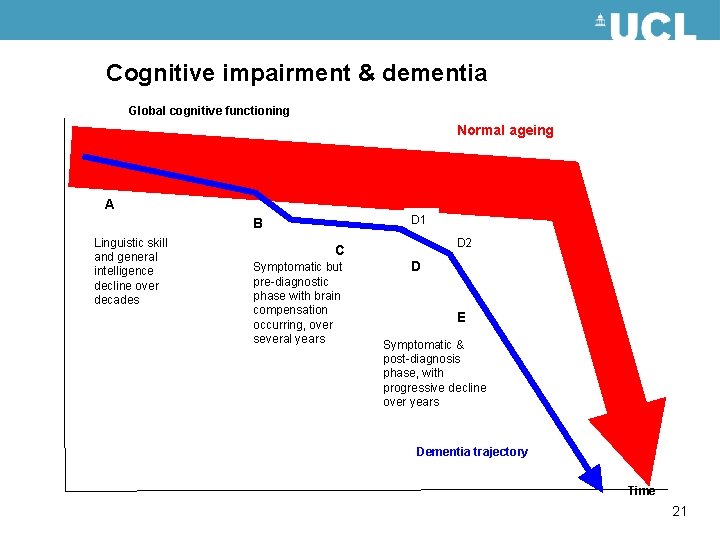
Cognitive impairment & dementia Global cognitive functioning Normal ageing A D 1 B Linguistic skill and general intelligence decline over decades D 2 C Symptomatic but pre-diagnostic phase with brain compensation occurring, over several years D E Symptomatic & post-diagnosis phase, with progressive decline over years Dementia trajectory Time 10
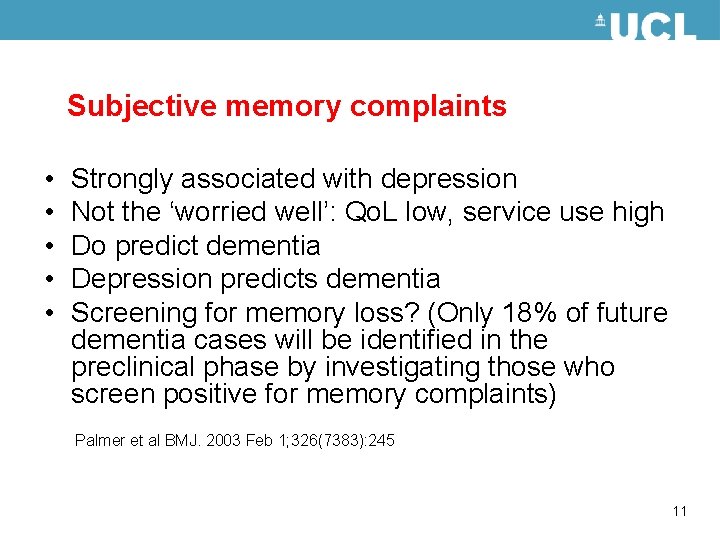
Subjective memory complaints • • • Strongly associated with depression Not the ‘worried well’: Qo. L low, service use high Do predict dementia Depression predicts dementia Screening for memory loss? (Only 18% of future dementia cases will be identified in the preclinical phase by investigating those who screen positive for memory complaints) Palmer et al BMJ. 2003 Feb 1; 326(7383): 245 11
The scale of subjective memory complaints • 60% of middle-aged people reported forgetfulness that hindered them significantly • 70% with SMC were very worried about it Commissaris et al Patient Education and Counselling 1998; 34(01): 25 -32 • 25 to 50% of older people • increases with age • 43% in people aged 65 -74, 88% in over 85 s Larrabee & Crook Int Psychogeriatrics 1994; 6(01): 95 -104 12
How do older people with SMC differ from their peers? • • Advanced age Female gender Depressed mood Anxious/phobic/obsessive personality Iliffe S & Pealing L Subjective memory complaints: a clinical review BMJ 2010: 340: c 1425 13
NICE/SCIE Guidelines 2006: recognition • • Informant history Cognitive function tests Blood screen (FBC, thyroid function) Scanning 14
Cognitive assessment • • • Mini-Mental State Examination (MMSE) 6 CIT GPCog TYM test Verbal fluency Clock drawing 15
GPCog 1 1. GPCOG measures both memory and executive function 1, 2 2. Sensitivity 85%, specificity 86% in the detection of dementia 1 3. More sensitive at detecting dementia than the MMSE 2 4. Suitable for use in primary care 3 -6 5. GPCOG patient interview + informant interview 1. Brodaty H et al. J Am Geriatr Soc 2002; 50(3): 530 -534. 2. Euro. Co. De 2009. http: //www. alzheimer-europe. org/Our. Research/European Collaboration-on-Dementia/Diagnosis-and-treatment-of-dementia 2/Assessment. 3. Lorentz WJ et al. Can J Psychiatry 2002; 47(8): 723 -733. 4. Milne A et al. Int Psychogeriatr 2008; 20(5): 911 -926. 5. Brodaty H et al. Am J Geriatr Psychiatry 2006; 14(5): 391 -400. 6. Ismail Z et al. Int J Geriatr Psychiatry 2010; 25(2): 111 -120. 16
GPCog patient interview 1. Name and address for subsequent recall test: 2. Time Orientation: What is the date? 3. Clock Drawing (visuospatial functioning) 4. Information: news event 5. Recall: Brodaty H et al. J Am Geriatr Soc 2002; 50(3): 530 -534 17
GPCog informant interview Difficulties: 1. Remembering things that have happened recently? 2. Recalling conversations a few days later? 3. Finding the right word? 4. With managing money (e. g. , paying bills, budgeting)? 5. Manage medication independently? 6. Using transport? 18
Verbal Fluency Test • The animal fluency test requires the patients to name as many items as they can in one minute 1 • Naming less than 15 novel items is indicative of AD 1 • Measures semantic fluency 1 • Can be used in a primary care setting 2 • Sensitivity 87% and specificity 96% in the detection of AD 1 • similar sensitivity and specificity to MMSE 1. Canning SJ et al. Neurology 2004; 62(4): 556 -562. 2. Kilada S et al. Alzheimer Dis Assoc Disord 2005; 19(1): 8 -16. 19
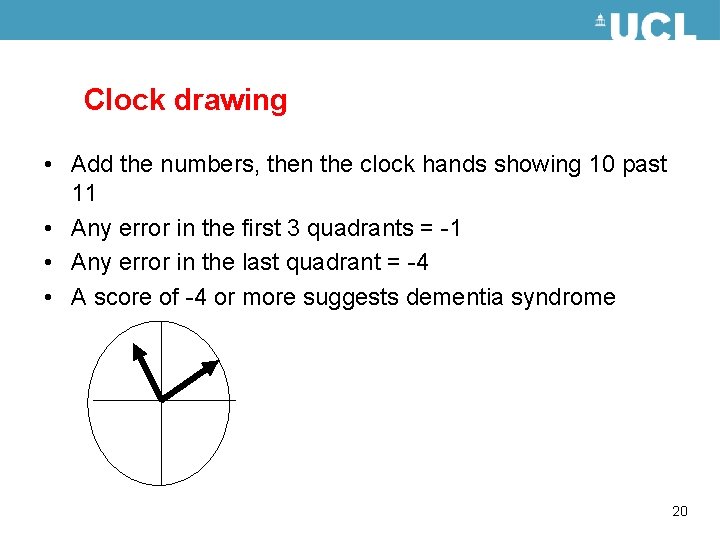
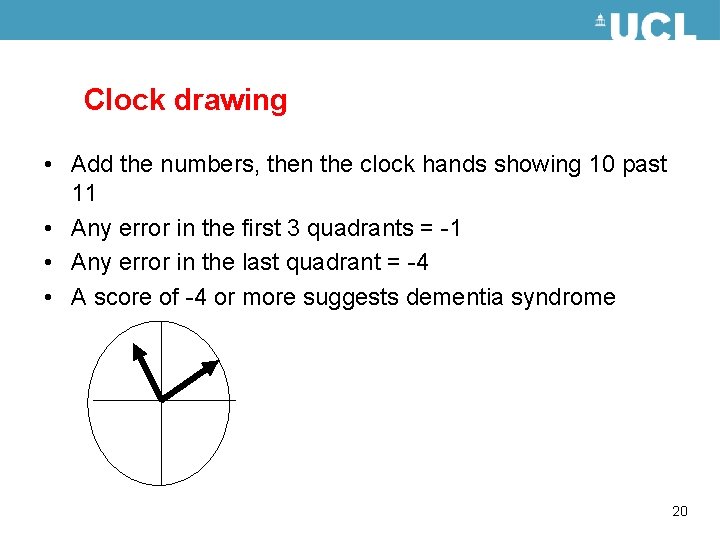
Clock drawing • Add the numbers, then the clock hands showing 10 past 11 • Any error in the first 3 quadrants = -1 • Any error in the last quadrant = -4 • A score of -4 or more suggests dementia syndrome 20
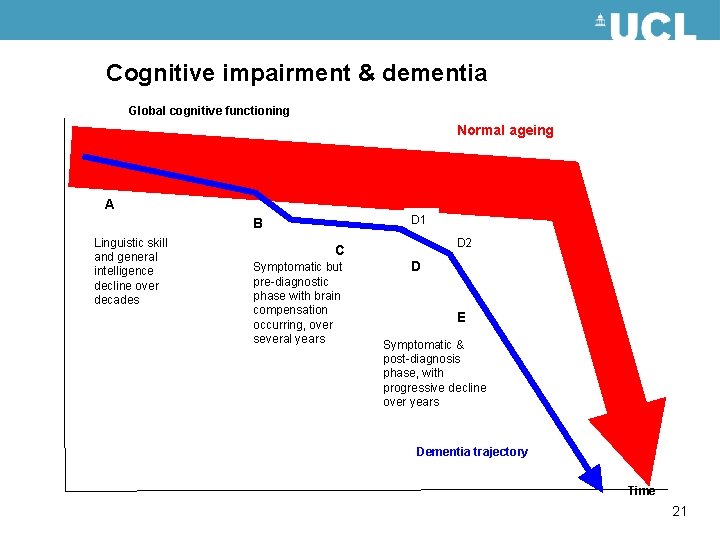
Cognitive impairment & dementia Global cognitive functioning Normal ageing A D 1 B Linguistic skill and general intelligence decline over decades D 2 C Symptomatic but pre-diagnostic phase with brain compensation occurring, over several years D E Symptomatic & post-diagnosis phase, with progressive decline over years Dementia trajectory Time 21

Psychosocial support • • • Regular doctor-initiated contact Review global assessment Manage co-morbidities Review support needed Carer’s health Robinson L et al for the DENDRON Primary Care Clinical Studies Group Primary care & dementia: 2 Case management, carer support & the management of behavioural and psychological symptoms IJGP 2009; Nov 27 [Epub ahead of print] 22
Psychosocial interventions 1 Need to overcome catastrophic thinking and depressive withdrawal: • Focussing on the individual and their family’ beliefs and attitudes about dementia Typical fears: • Other people ‘finding out’ the diagnosis, • Rapid deterioration in abilities, • Socially embarrassing behaviour; • Loss of involvement in life and care planning. 23
Psychosocial interventions 2 Reframing dementia as a disability • acknowledges anger • re-labelling of ‘stupidities’ as ‘difficulties’ • focus on things they still can do 24
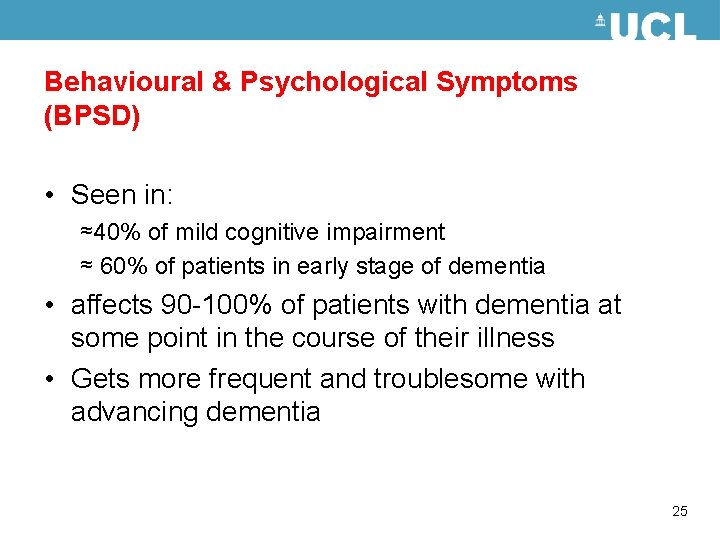
Behavioural & Psychological Symptoms (BPSD) • Seen in: ≈40% of mild cognitive impairment ≈ 60% of patients in early stage of dementia • affects 90 -100% of patients with dementia at some point in the course of their illness • Gets more frequent and troublesome with advancing dementia 25
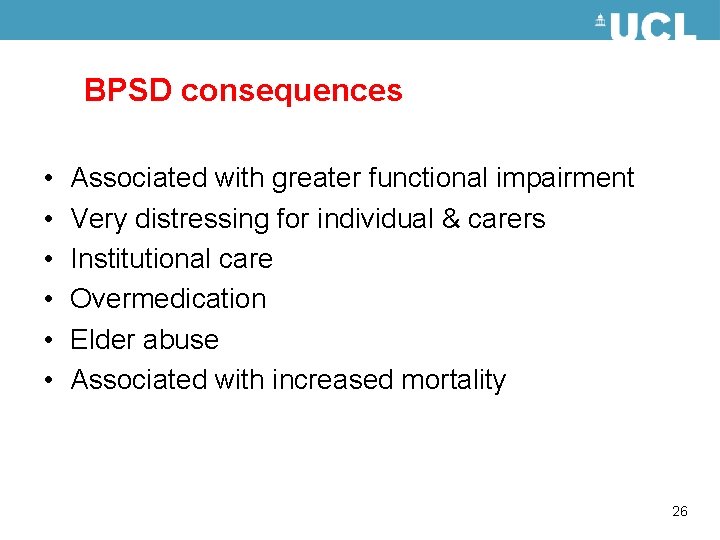
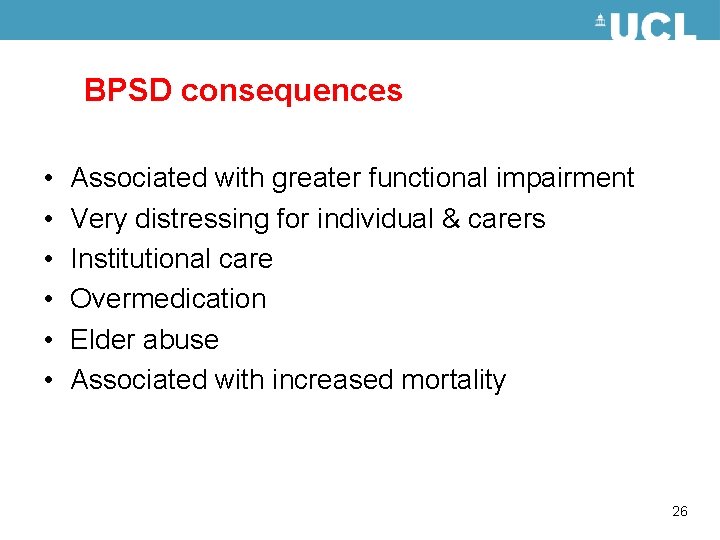
BPSD consequences • • • Associated with greater functional impairment Very distressing for individual & carers Institutional care Overmedication Elder abuse Associated with increased mortality 26
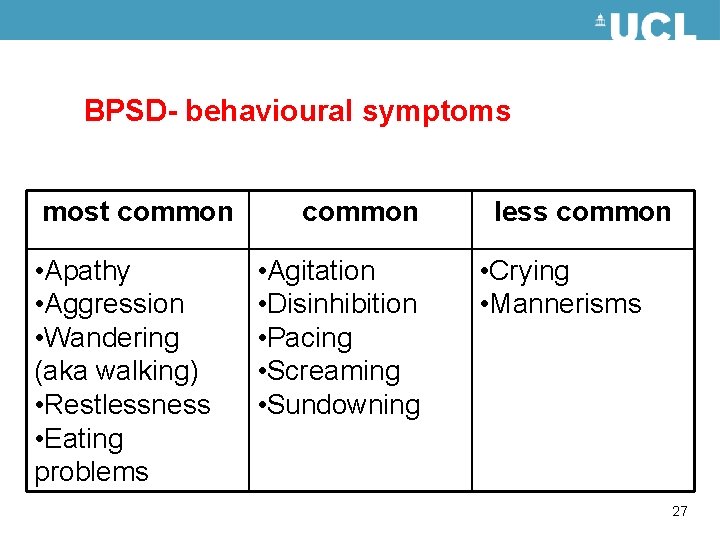
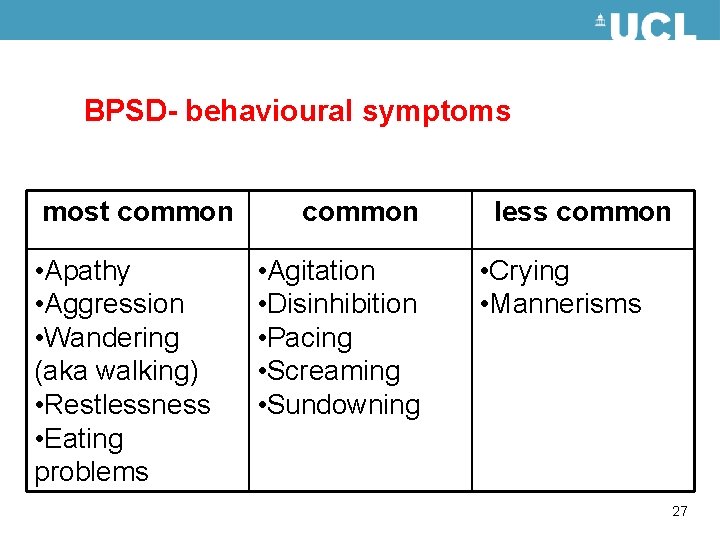
BPSD- behavioural symptoms most common • Apathy • Aggression • Wandering (aka walking) • Restlessness • Eating problems common • Agitation • Disinhibition • Pacing • Screaming • Sundowning less common • Crying • Mannerisms 27
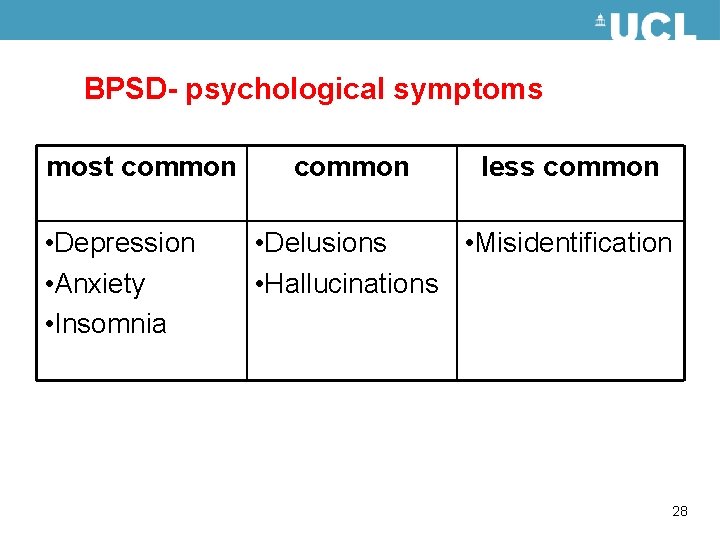
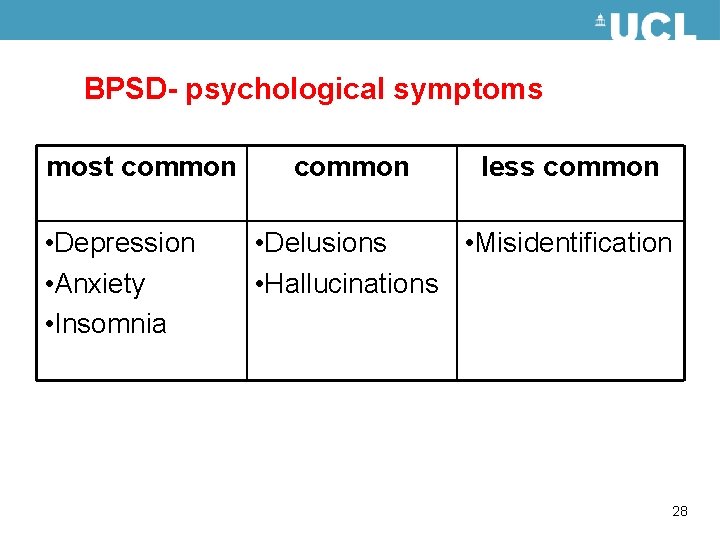
BPSD- psychological symptoms most common • Depression • Anxiety • Insomnia common less common • Delusions • Misidentification • Hallucinations 28
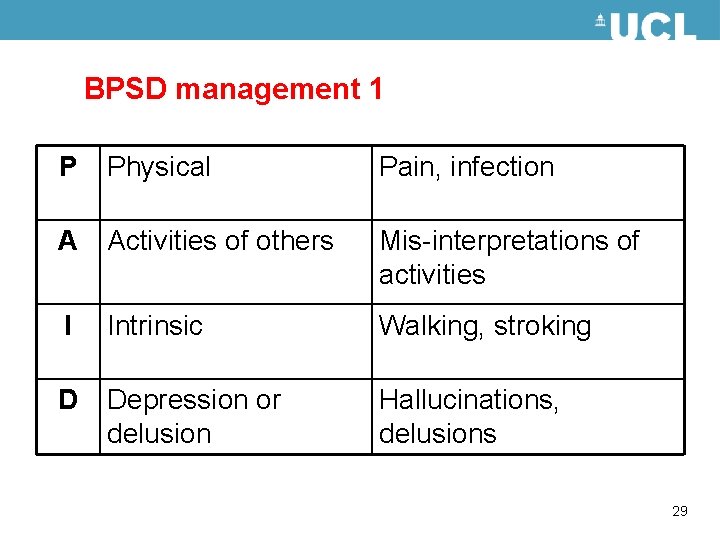
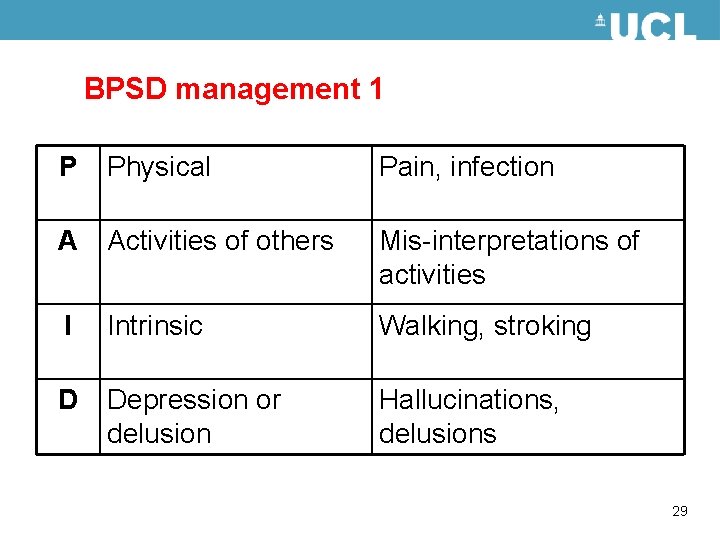
BPSD management 1 P Physical Pain, infection A Activities of others Mis-interpretations of activities I Intrinsic Walking, stroking D Depression or delusion Hallucinations, delusions 29
BPSD management 2 • Drug treatment – – Last resort Should target specific symptoms Specialist initiation Regular review 30
End of Life care • Capacity to make decisions • Advance decisions • Co-morbidities (pain) Goodman C et al End of life care for community dwelling older people with dementia: an integrated review Int J Geriatric Psychiatr 2009; 31
Mental Capacity Always assume capacity, act in best interests, with least restriction. A person is thought to be unable to make specific decisions if he or she is unable to: • Understand the information relevant to the decision, • Retain that information, • Use that information to make a decision, • Communicate a decision (by any means). 32
Advance decisions An advance decision cannot be used to: • Refuse basic nursing care essential to comfort • Refuse the offer of food or drink by mouth • Refuse measures designed to maintain comfort − for example, painkillers • Demand treatment that a healthcare team considers inappropriate • Refuse treatment for mental disorder if the person is or is liable to be detained under the Mental Health Act 1983 • Ask for anything that is against the law (euthanasia) 33
Dementia syndrome: Core business for general practice • • • Continuity of contact Population reach Pattern recognition Problem solving not protocol driven Systematised care 34
What is the role of the Specialist? • Uncertain diagnosis, ‘red flag’ symptoms/signs, sub-typing • Access to treatments (Alzheimer’s disease) & support • Management problems: anti-psychotic drugs • Education 35
Thank you for listening! http: //www. journalslibrary. nihr. ac. uk/pgfar/volume-3/issue-3 EVIDEM Educational interventions in general practice Management of BPSD with exercise Continence management in dementia Assessing mental capacity End of Life care and dementia s. iliffe@ucl. ac. uk 36
 Lindblom science of muddling through
Lindblom science of muddling through Eliminating muddling mindset
Eliminating muddling mindset Promotion from assistant to associate professor
Promotion from assistant to associate professor Ronald wayne biography
Ronald wayne biography Wendylett sheets 1 carer
Wendylett sheets 1 carer Bookcase analogy dementia
Bookcase analogy dementia Chapter 49 confusion and dementia
Chapter 49 confusion and dementia Difference between delirium and dementia table
Difference between delirium and dementia table Dementia pictures
Dementia pictures Frontotemporal dementia
Frontotemporal dementia Promoting excellence in dementia care
Promoting excellence in dementia care Dementia 2015
Dementia 2015 Strength based dementia care
Strength based dementia care Difference between dementia and delirium
Difference between dementia and delirium Dementia treatments and interventions near patterson
Dementia treatments and interventions near patterson Rocking chair therapy for dementia patients
Rocking chair therapy for dementia patients Receptive language
Receptive language Epilepsy
Epilepsy Dementia pugilistica
Dementia pugilistica Life story work dementia
Life story work dementia Confusion dementia and alzheimer disease chapter 19
Confusion dementia and alzheimer disease chapter 19 Dementie
Dementie Unit 40 dementia care
Unit 40 dementia care Rarly signs of dementia
Rarly signs of dementia 3 zones of space and awareness dementia
3 zones of space and awareness dementia Pool activity level pdf
Pool activity level pdf Risk factor dementia
Risk factor dementia Bath city forum
Bath city forum Dementia
Dementia Living well with dementia scotland
Living well with dementia scotland Barbara's story dementia
Barbara's story dementia Dementia
Dementia Enriched model of dementia care
Enriched model of dementia care Trasodone
Trasodone Confusion dementia and alzheimer's disease
Confusion dementia and alzheimer's disease 850 000 steps for dementia
850 000 steps for dementia Enriched model of dementia care
Enriched model of dementia care