CURRENT RADIOLOGICAL TREATMENT OF COLORECTAL METASTASES WHAT CAN


- Slides: 48
CURRENT RADIOLOGICAL TREATMENT OF COLORECTAL METASTASES WHAT CAN WE DO AND SHOULD WE BE DOING IT? Alexander Spiers Royal Devon & Exeter Hospital
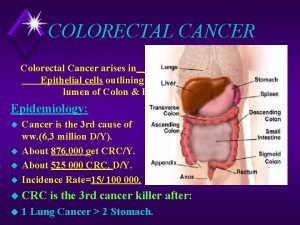
Introduction � Discussion will be limited to metastatic disease in liver and lung Commonest sites for deposits Main areas where Radiological Intervention is applicable The talk is slanted to my own practice
� Review of available techniques Ablation �Radiofrequency (RFA) �Microwave (MWA) �Cryoablation �Electroporation (IRE) Embolisation �Bland Embolisation �Trans-arterial chemotherapy �Trans-Arterial chemoembolisation(TACE) �Drug-eluting bead TACE (DEB-TACE) Radioactive microparticles (SIRT) �Yttrium-90 radioembolisation (Y-90) Combination Therapies – where does Radiology fit in? �Surgery, Systemic Chemotherapy, Stereotactic Radiotherapy
� What is the evidence for these Radiological interventions? How do they compare with chemotherapy, surgery or SABR Have they been compared? � Concept of Oligometastatic Disease Is it valid What is the evidence for Surgical Lung Metastasectomy?
Ablation Technologies � RFA Alternating Current (450 -500 k. Hz). Ionic agitation results in frictional heating. � Lung is a more favourable environment than liver due to insulation provided by surrounding air � Blood vessels act as a heat sink – vessels >3 mm diameter often cause prolongation of RFA procedure and may result in incomplete ablation (see later). � 60 C � � MWA 915 MHz and 2. 45 GHz � Dielectric hysteresis � Faster and larger ablation zone than RFA � 90 C �
Ablation Technologies � Cryoablation � � Rapid cooling results in extracellular and intracellular ice crystal formation causing osmotic dehydration of cells and membrane damage respectively (We think!) Irreversible Electroporation (IRE) � utilizes high-voltage millisecond electrical pulses applied through adjustable needles to increase cell membrane permeability, which results in cell death and necrosis Faroja et al. Radiology: Volume 266: Number 2—February 2013
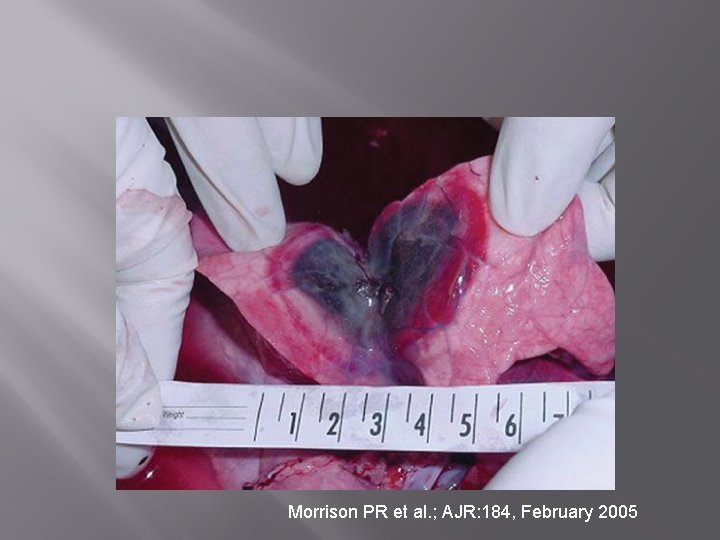
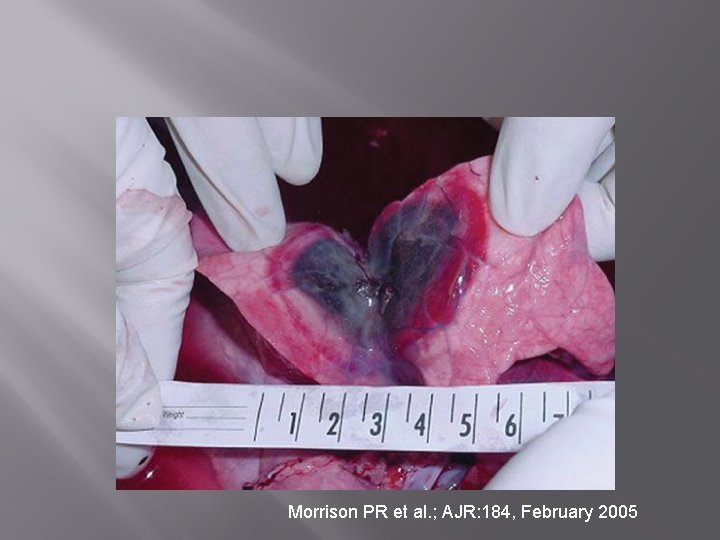
Morrison PR et al. ; AJR: 184, February 2005
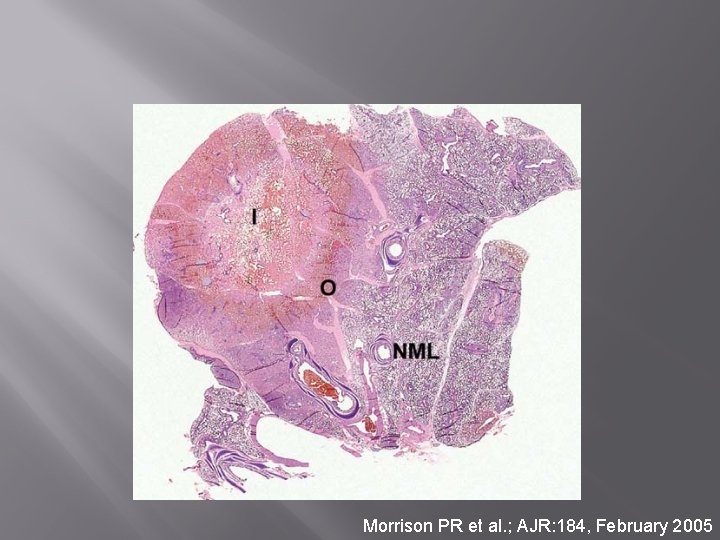
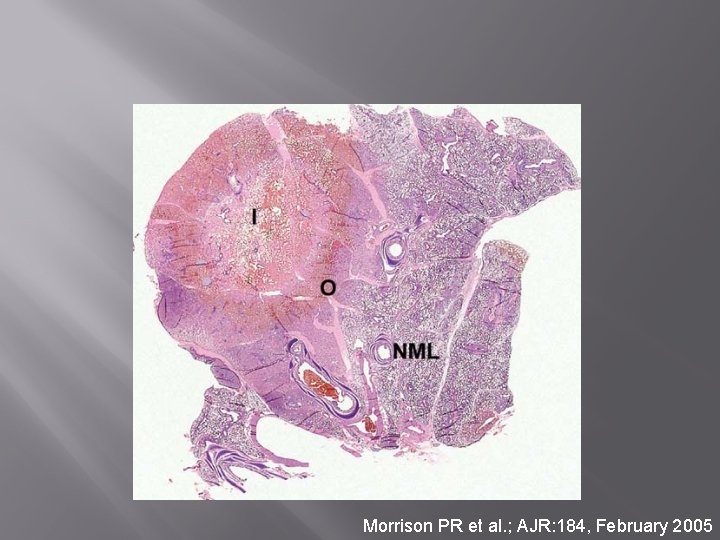
Morrison PR et al. ; AJR: 184, February 2005
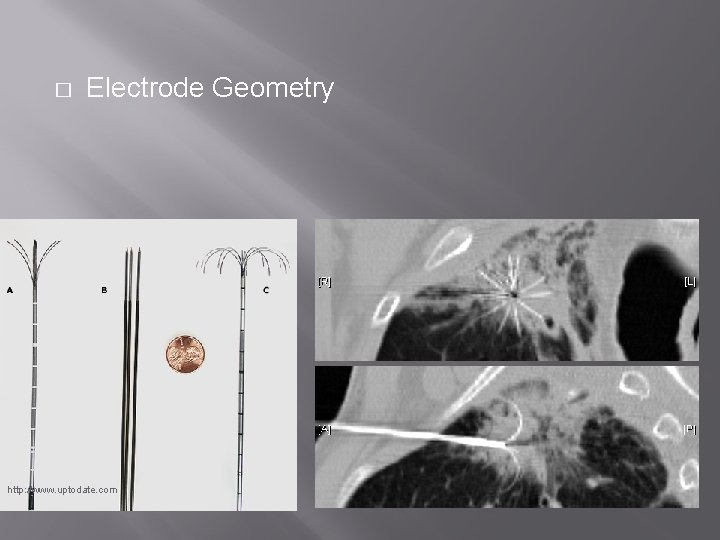
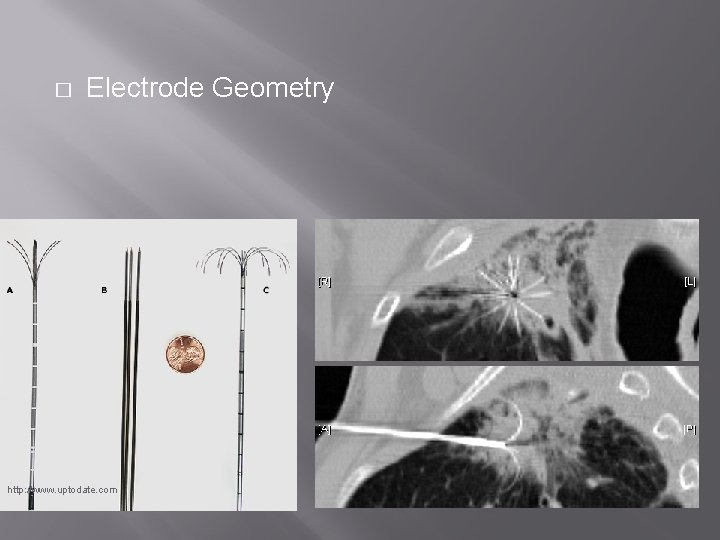
� Electrode Geometry http: //www. uptodate. com
Indications � Biologically favourable disease Best results with small slow growing tumours Modest number of lesions �Not a technical limitation but prognosis worse if >4 Long Disease free interval
Indications (Lung) � Definitive Therapy: Limited Number (centres vary - <5 per lung, preferably <3) of metastases � Palliation Rarely necessary with CRC Local Pain Control Recurrence in patients who have had XRT or surgery Control of haemoptysis
Indications (Liver) � � Up to 4 metastases (<4 cm) in suitable locations Downstaging for surgery
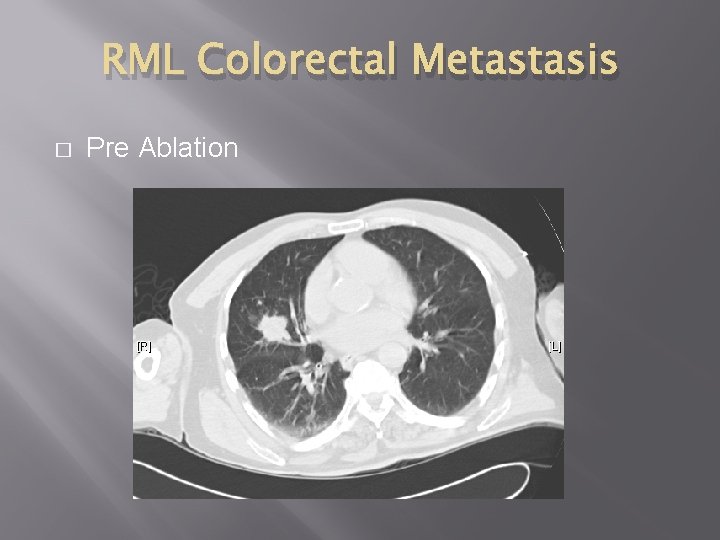
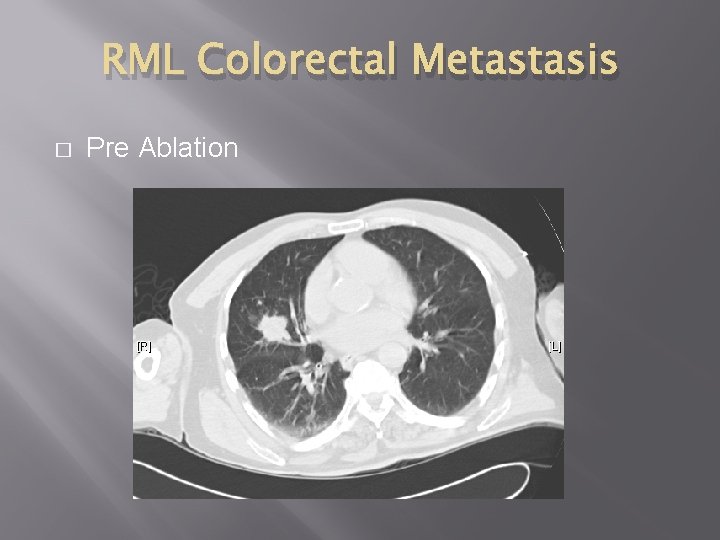
RML Colorectal Metastasis � Pre Ablation
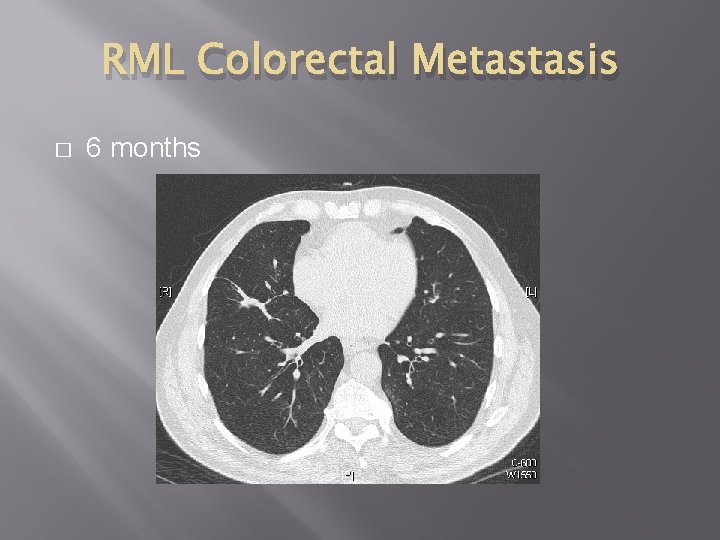
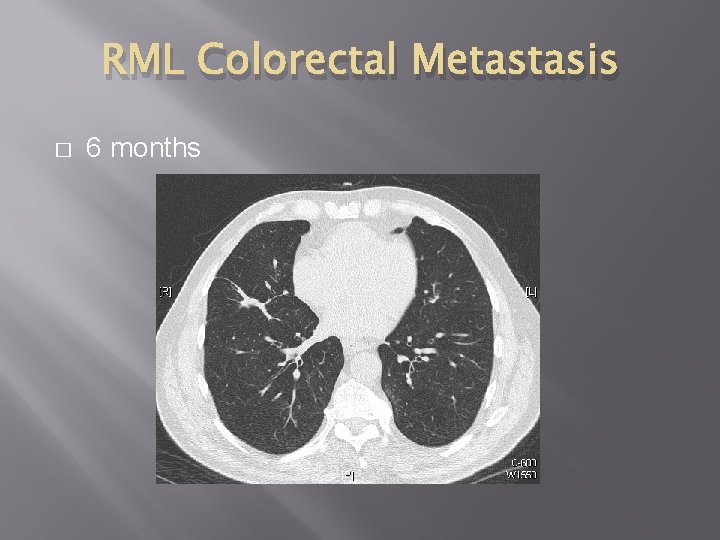
RML Colorectal Metastasis � 6 months
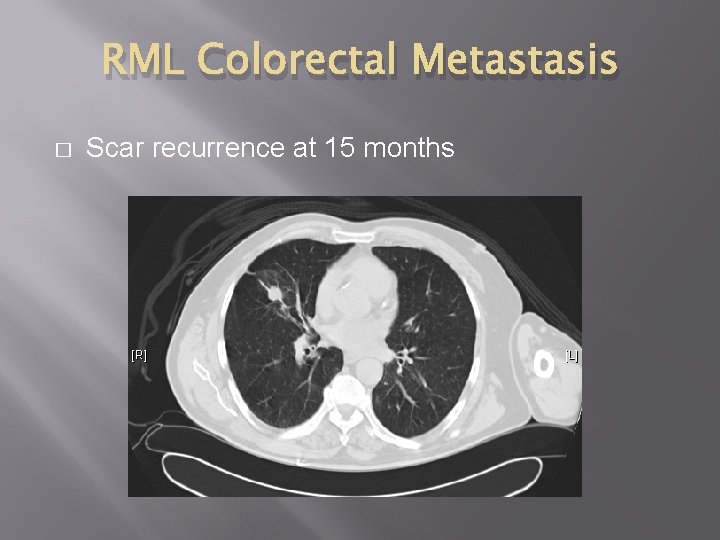
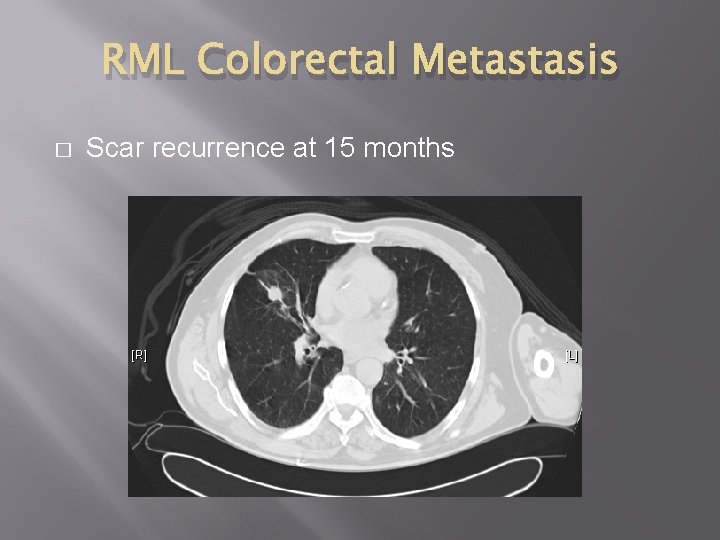
RML Colorectal Metastasis � Scar recurrence at 15 months
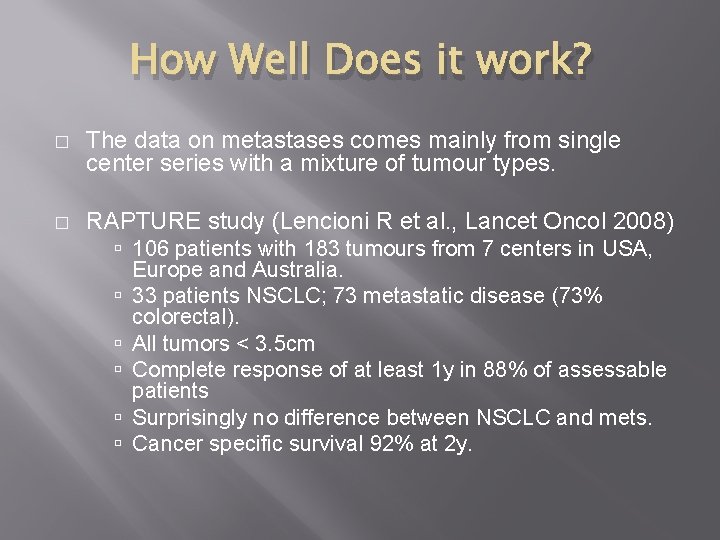
How Well Does it work? � The data on metastases comes mainly from single center series with a mixture of tumour types. � RAPTURE study (Lencioni R et al. , Lancet Oncol 2008) 106 patients with 183 tumours from 7 centers in USA, Europe and Australia. 33 patients NSCLC; 73 metastatic disease (73% colorectal). All tumors < 3. 5 cm Complete response of at least 1 y in 88% of assessable patients Surprisingly no difference between NSCLC and mets. Cancer specific survival 92% at 2 y.
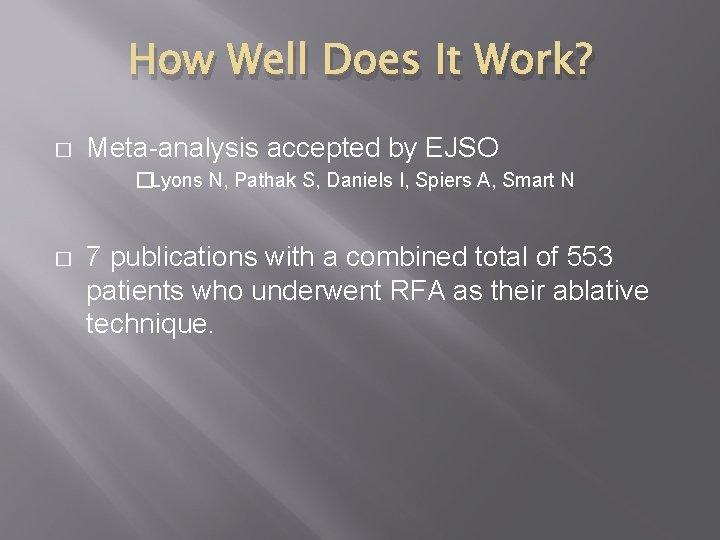
How Well Does It Work? � Meta-analysis accepted by EJSO �Lyons N, Pathak S, Daniels I, Spiers A, Smart N � 7 publications with a combined total of 553 patients who underwent RFA as their ablative technique.
How Well Does It Work? � The studies demonstrated a mortality rate of less than 1% and overall survival rates ranging from 31 -67 months with 1, 2 and 3 year survival ranges of 79 -91%, 56 -72% and 35 -65% respectively. � cf 36% 5 ys for complete resection; 13% 5 ys incomplete resection. These figures are comparable to Surgery � Local progression following ablation ranged from 9 -22%. � Major complication rates were noted in 1 -8% of patients with minor complications ranging between 7 -33%. � Overall 25% of patients required chest drain insertion post procedure. �
Lung RFA In Exeter � � First case October 2009 (still going strong) 168 procedures (93 for CRC) as of this morning 237 tumours ablated (141 for CRC) Audit shows ~15% local recurrence rate
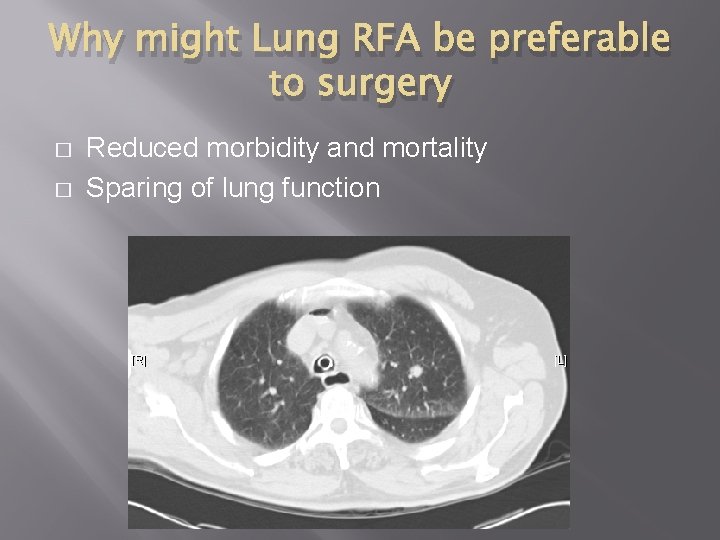
Why might Lung RFA be preferable to surgery � � Reduced morbidity and mortality Sparing of lung function
Comparison with othermal technologies � � Proper trials comparing different radiofrequency technologies have yet to be conducted, let alone comparisons with MWA, IRE and Cryo. Those who have switched to MWA are very enthusiastic about its advantages!
Liver RFA � � Much of what I have said about the lung applies to the liver Technique: Open>Laparoscopic>Percutaneous �Differences small � Data not of the highest quality �retrospective studies etc.
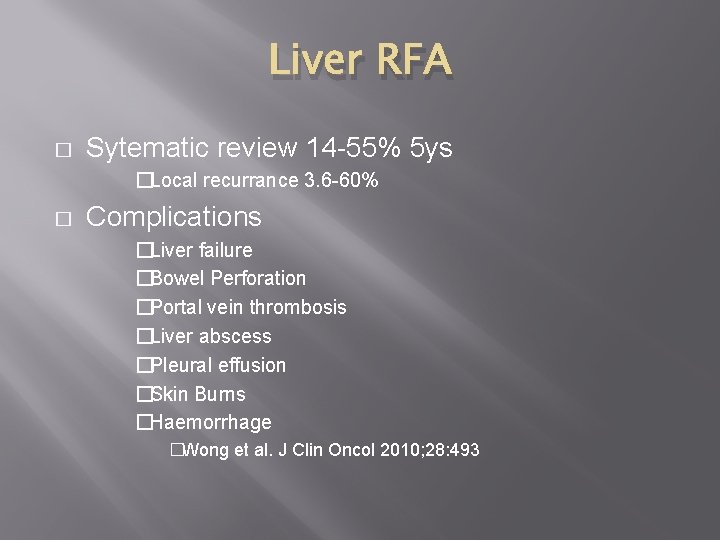
Liver RFA � Sytematic review 14 -55% 5 ys �Local recurrance 3. 6 -60% � Complications �Liver failure �Bowel Perforation �Portal vein thrombosis �Liver abscess �Pleural effusion �Skin Burns �Haemorrhage �Wong et al. J Clin Oncol 2010; 28: 493
Liver RFA � Current Status � Surgery treatment of choice � Possibly with initial chemotherapy to shrink metastases first � RFA if patient not surgical candidate Best results 3 lesions or less (<5 cm)
Limitations of RFA � � � � Limit to the size and number of lesions that can be treated. Some restriction in location of lesions Local recurrence/failure rate Complications Selection criteria remain rather vaguely defined Relationship to surgery , chemotherapy and radiotherapy remains undefined More promising technologies available

Under CT Scan Courtesy of L. Berard
Ablation vs Surgery � � Different patient populations Largely retrospective data with limited follow-up. Few randomized trials Systematic review (ASCO) 14 -55% 5 ys; 3. 6 -60% recurrence rate Not enough evidence t support RFA over surgery or where there is extrahepatic disease �Wong SL et al. J Clin Oncol. 2010; 28(3): 493. � No randomized trials comparing RFA with Surgery
Ablation with Chemotherapy � � Not much data Phase ll trial 119 randomised to FOLFOX +/- bevacizumab alone or combined with RFA(53%)/RFA+resection(47%) RFA group had longer median (45. 6 m vs 40. 5 m) and 8 year (36% vs 9%) Suggests RFA benefit but effect of surgery not subtracted �Ruers T et al. Ann Oncol 2012; 23 (10): 2619.
� Ablation does have the advantage that it can be repeated at the same site – often not the case with Surgery or SABR
Intra-arterial therapy � � � Metastases (>5 mm) derive 80% of supply from hepatic artery Arterial administration allows relatively lower systemic dose and avoids first pass metabolism in liver Trial of hepatic artery embolisation showed no benefit over controls Hunt TM Br J Surg 1990 Jul; 77(7): 779 -82. � Hepatic Intra-arterial chemotherapy (usually via implanted infusion pump). Results very drug dependent. No trials as yet with Irinotecan or Oxaliplatin � � Seems to produce better local response than systemic therapy but not a survival benefit Radioembolization (SIRT – Selective Internal Radiation Therapy) I 131 or Y 90 tagged glass or resin beads (20 -40 microns) � Small trials suggest some benefit when used on its own or in combination with systemic chemotherapy � Very expensive therapy probably best reserved for unresectable (liver predominant) metastatic disease (and life expectancy >15 m) �
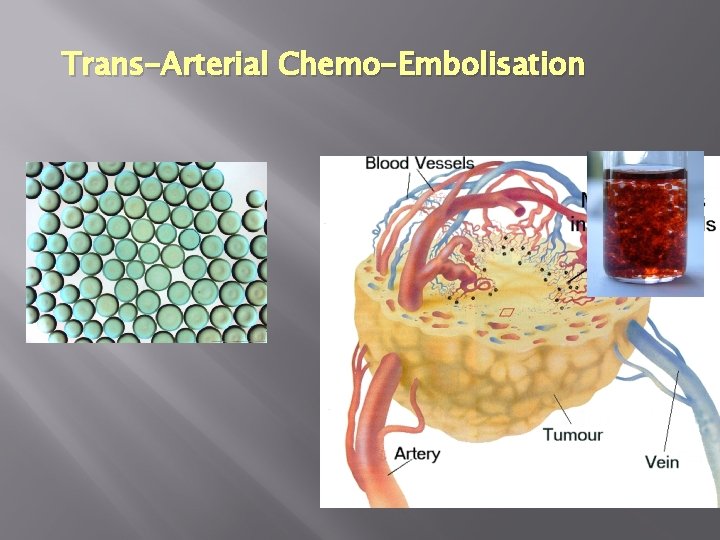
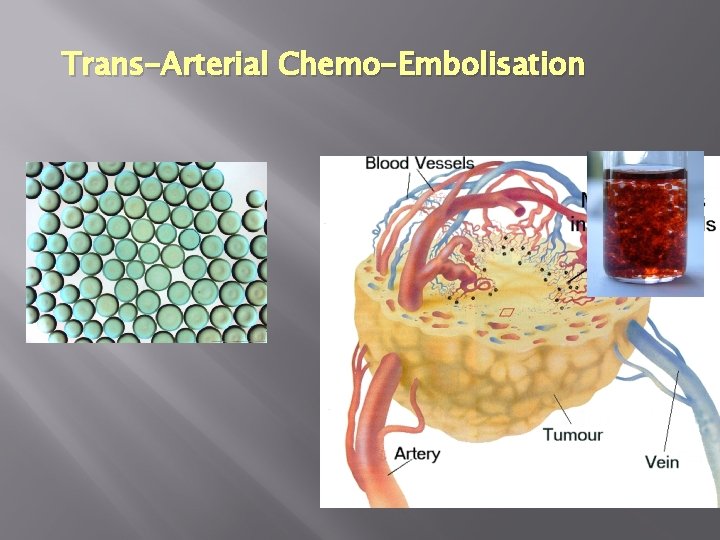
Trans-Arterial Chemo-Embolisation
Irinotecan-eluting Beads for TACE of CRC Mets Topoisomerase 1 inhibitor
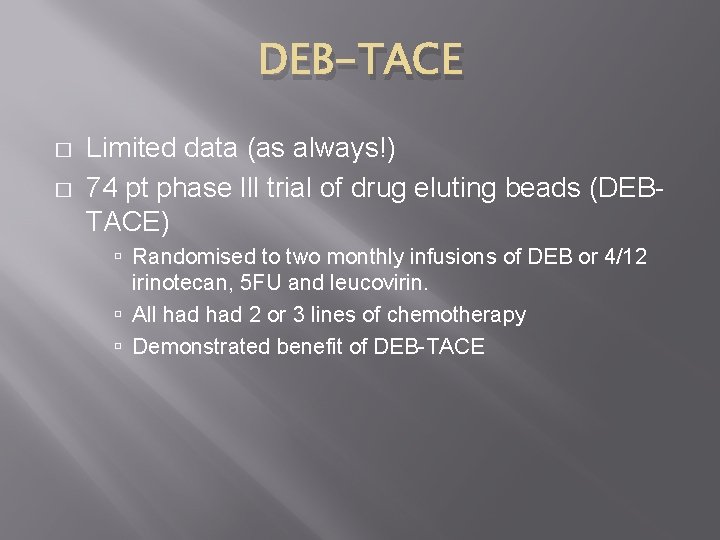
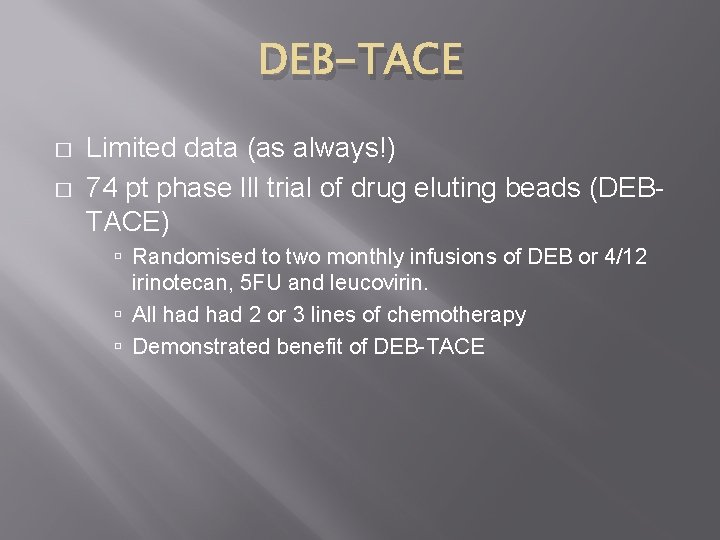
DEB-TACE � � Limited data (as always!) 74 pt phase lll trial of drug eluting beads (DEBTACE) Randomised to two monthly infusions of DEB or 4/12 irinotecan, 5 FU and leucovirin. All had 2 or 3 lines of chemotherapy Demonstrated benefit of DEB-TACE
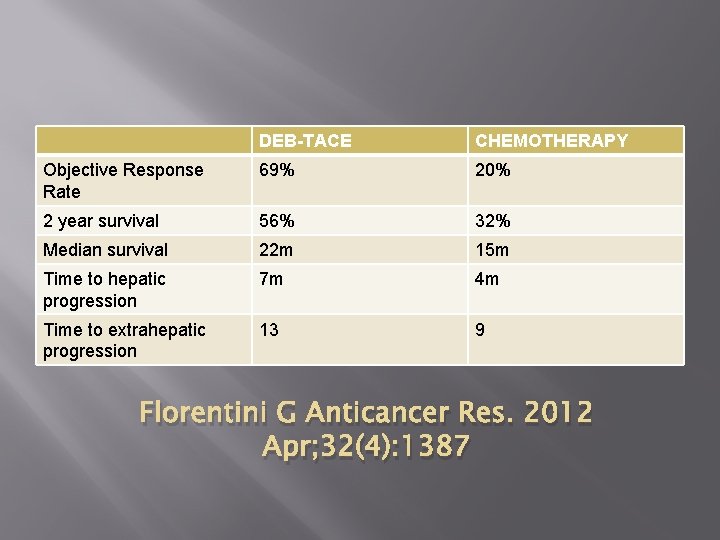
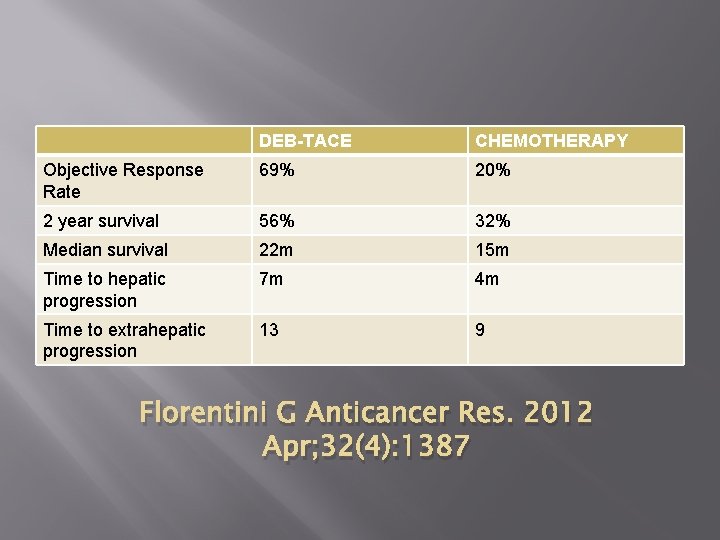
DEB-TACE CHEMOTHERAPY Objective Response Rate 69% 20% 2 year survival 56% 32% Median survival 22 m 15 m Time to hepatic progression 7 m 4 m Time to extrahepatic progression 13 9 Florentini G Anticancer Res. 2012 Apr; 32(4): 1387
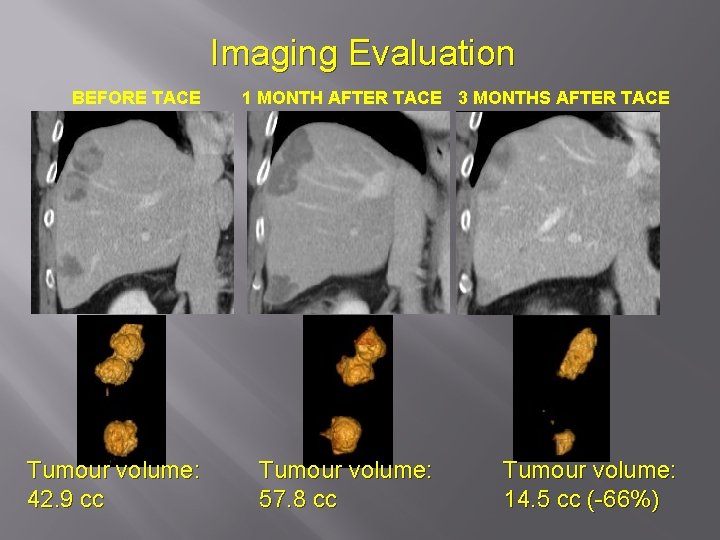
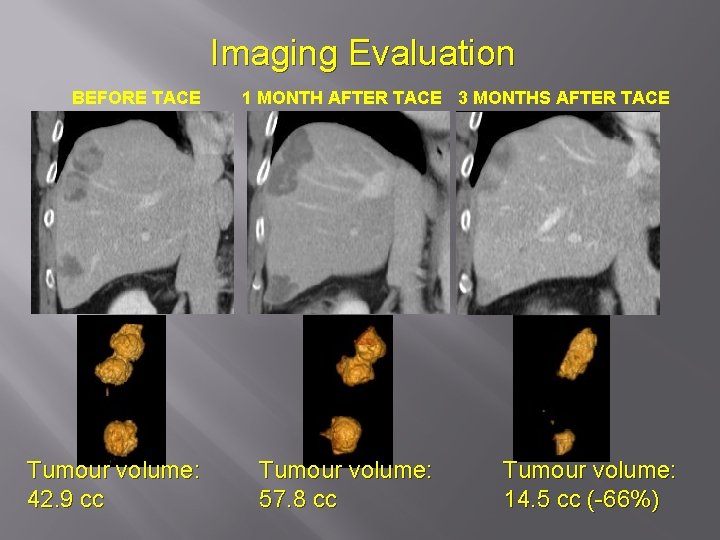
Imaging Evaluation BEFORE TACE Tumour volume: 42. 9 cc 1 MONTH AFTER TACE 3 MONTHS AFTER TACE Tumour volume: 57. 8 cc Tumour volume: 14. 5 cc (-66%)
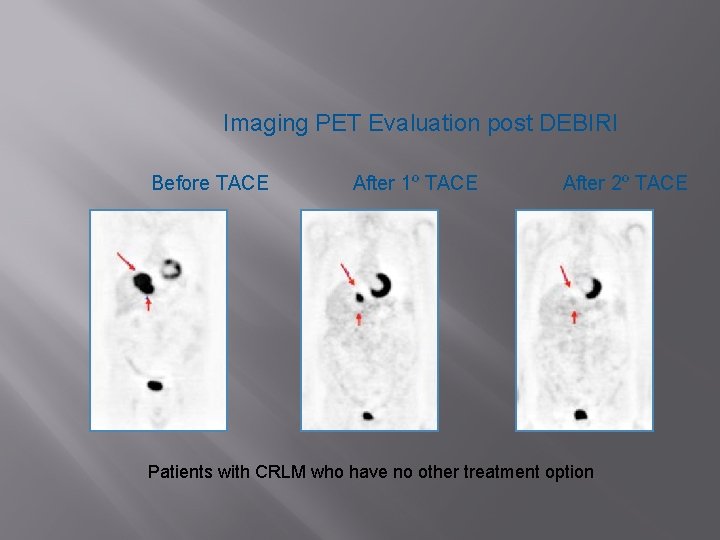
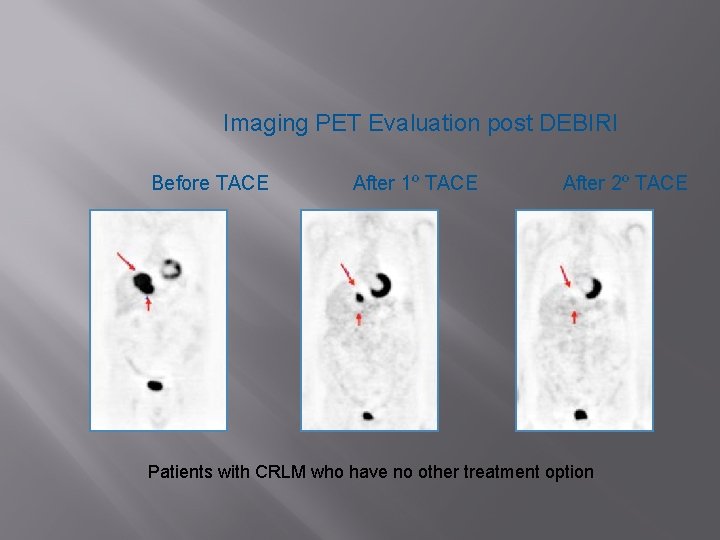
Imaging PET Evaluation post DEBIRI Before TACE After 1º TACE After 2º TACE Patients with CRLM who have no other treatment option
Should We Be Doing This? � � � I will illustrate this with the example of Lung metastasis ablation. The basis for treatment relies in part on belief in the concept of Oligometastatic disease … … and the belief that Surgical Metastasectomy confers survival benefit in selected patients.
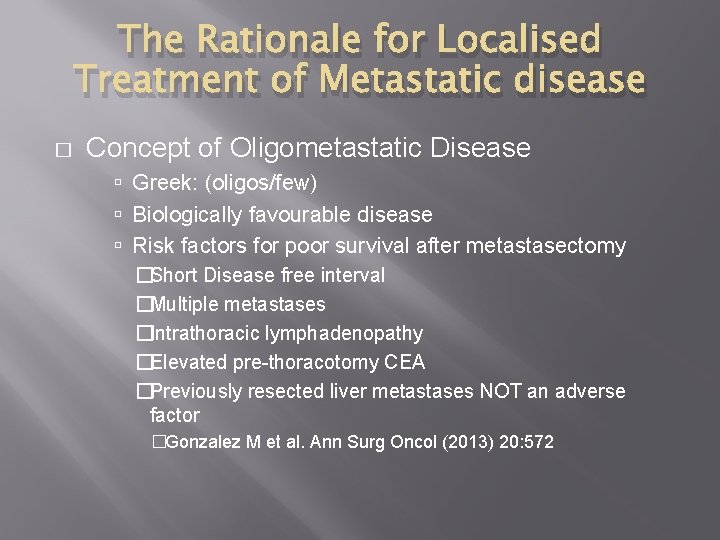
The Rationale for Localised Treatment of Metastatic disease � Concept of Oligometastatic Disease Greek: (oligos/few) Biologically favourable disease Risk factors for poor survival after metastasectomy �Short Disease free interval �Multiple metastases �Intrathoracic lymphadenopathy �Elevated pre-thoracotomy CEA �Previously resected liver metastases NOT an adverse factor �Gonzalez M et al. Ann Surg Oncol (2013) 20: 572
The Rationale for Localised Treatment of Metastatic disease � LONG-TERM RESULTS OF LUNG METASTASECTOMY: PROGNOSTIC ANALYSES BASED ON 5206 CASES. Pastorino U et al. J Thorac Cardiovasc Surg 1997; 113: 37 -49 � Results: The actuarial survival after complete metastasectomy was 36% at 5 years, 26% at 10 years, and 22% at 15 years (median 35 months) The corresponding values for incomplete resection were 13% at 5 years and 7% at 10 years (median 15 months). �
The Rationale for Localised Treatment of Metastatic disease � � � Among complete resections, the 5 -year survival was 33% for patients with a disease-free interval of 0 to 11 months and 45% for those with a diseasefree interval of more than 36 months 43% for single lesions and 27% for four or more lesions. Multivariate analysis showed a better prognosis for patients with germ cell tumors, disease-free intervals of 36 months or more, and single metastases.
The Rationale for Localised Treatment of Metastatic disease � Conclusions: These results confirm that lung metastasectomy is a safe and potentially curative procedure. Resectability, disease-free interval, and number of metastases enabled us to design a simple system of classification valid for different tumor types.
But … � � Lung disease is rarely the cause of death in CRC Local tumour ablation relies on the premise that surgical resection is effective European Society of Thoracic Surgeons Lung Metastasectomy Working Group: '…the level of evidence to support current practice is too low to set firm recommendations to the members of ESTS. In the absence of a randomized controlled trial looking at the effectiveness of pulmonary metastasectomy on survival and quality of life, it is unlikely that the current practice will ever be influenced. ‘ �Van Raemdonck D et al. J Thorac Oncol 2010; 5: S 127 -S 129. � � � Citation bias in published reviews A randomised trial is currently recruiting Pul. MICC One can make similar criticisms of the evidence for hepatic resections
Questioning the concept of Oligometastatic Disease � � � Clinical data indicate that the number of patients with oligometastatic disease receiving aggressive treatment is increasing rapidly. Numerous single-arm studies suggest that longterm survival is 'better-than-expected' after ablative treatment. The few studies with adequate controls raise the possibility that this long-term survival might not be due to the treatments themselves, but rather to the selection of patients based on favourable inclusion criteria.
Questioning the concept of Oligometastatic Disease � � � Ablative treatments carry a risk of harming healthy tissue, yet the risk–benefit ratio cannot be quantified if the benefits are unmeasured. If the strategy of treating oligometastases is to gain widespread acceptance as routine clinical practice, there should be stronger evidence supporting its efficacy. Palma A, Salama J, Lo S, Senan S, Treasure T, Govindan R, Weichselbaum R Nature Reviews Clinical Oncology 11, 549– 557
Questioning the concept of Oligometastatic Disease � � One could thus argue that we don’t know if we are actually helping our patients with Surgery/SABR or ablation If this is the case I would seem appropriate to offer therapy with the lowest morbidity – assuming it is effective.
The Future � � � Move to MWA? Combination therapies Role of SABR
Acknowledgements � � � Prof. Tony Watkinson Professor Tom Treasure The Nurses, Radiographers and Secretaries in the RD&E Xray Dept.

THANK YOU FOR YOUR ATTENTION – any questions?
 Colorectal cancer drug trial
Colorectal cancer drug trial Ann lyons colorectal surgeon
Ann lyons colorectal surgeon Sorunun cevabını bul
Sorunun cevabını bul Adenoma
Adenoma Colorectal cancer labs
Colorectal cancer labs Center for devices and radiological health
Center for devices and radiological health National radiological emergency preparedness conference
National radiological emergency preparedness conference Radiological dispersal device
Radiological dispersal device Tennessee division of radiological health
Tennessee division of radiological health Line current and phase current
Line current and phase current Line vs phase voltage
Line vs phase voltage Energy band diagram of pnp transistor
Energy band diagram of pnp transistor Line current and phase current
Line current and phase current Drift current
Drift current Drift current and diffusion current in semiconductor
Drift current and diffusion current in semiconductor A jfet always operates with
A jfet always operates with Balanced y-y connection
Balanced y-y connection Slideplayer
Slideplayer Drift current density unit
Drift current density unit Welding chapter 3 answers
Welding chapter 3 answers Touch current vs leakage current
Touch current vs leakage current Non planar circuit
Non planar circuit Primary settling
Primary settling Is current can be negative
Is current can be negative If you can imagine it you can achieve it
If you can imagine it you can achieve it You can tell harris about it just ____(easily) as i can.
You can tell harris about it just ____(easily) as i can. If you think you can you can poem
If you think you can you can poem If you can't measure it, you can't manage it
If you can't measure it, you can't manage it If you can't measure it you can't manage it
If you can't measure it you can't manage it Percussions corporelles
Percussions corporelles Curriculum design elements
Curriculum design elements You can tell harris about it just ____(easily) as i can.
You can tell harris about it just ____(easily) as i can. Comparative and superlative for less
Comparative and superlative for less I can could speak english
I can could speak english Look at the pictures and complete with can or can't
Look at the pictures and complete with can or can't The jean
The jean I know nothing is impossible
I know nothing is impossible If you can measure it you can manage it
If you can measure it you can manage it Talk en futuro
Talk en futuro Any fool can write code that a computer can understand
Any fool can write code that a computer can understand Literary devices in sonnet 18
Literary devices in sonnet 18 Was ist langfristiges fremdkapital
Was ist langfristiges fremdkapital Exº
Exº Water treatment fundamentals
Water treatment fundamentals Tertiary treatment of wastewater apes
Tertiary treatment of wastewater apes Purpose of wastewater treatment
Purpose of wastewater treatment Aquaculture water treataent factory
Aquaculture water treataent factory Design of grit chamber example
Design of grit chamber example Wast water treatment
Wast water treatment