Cost Repositioning an Institutional Case Study Kandice KottkeMarchant


- Slides: 33
Cost Repositioning – an Institutional Case Study Kandice Kottke-Marchant, MD, Ph. D Chair, Robert J. Tomsich Pathology & Laboratory Medicine Institute Cleveland Clinic
Cleveland Clinic’s Cost Repositioning Approach
Cost Repositioning Objectives • Provide value and ensure affordable care for patients • Leading innovation in changing industry • Transformational cost structure changes • Balancing the shift: volume to value

Cost Repositioning 2014 - 2016 Goals * Implemented Savings (in millions) $1 000 $800 TBD 140 75 $600 200 $400 560 270 $200 100 $0 l ff ca t a i t c n s i -S ire Cl sset n d A In No & s am gr o Pr 10 10 35 af t S f ar w te S ip h ds s Re rc a e h E c du on i t a % 20 p Ov la er al t To re lu Va a e. B se a d. C
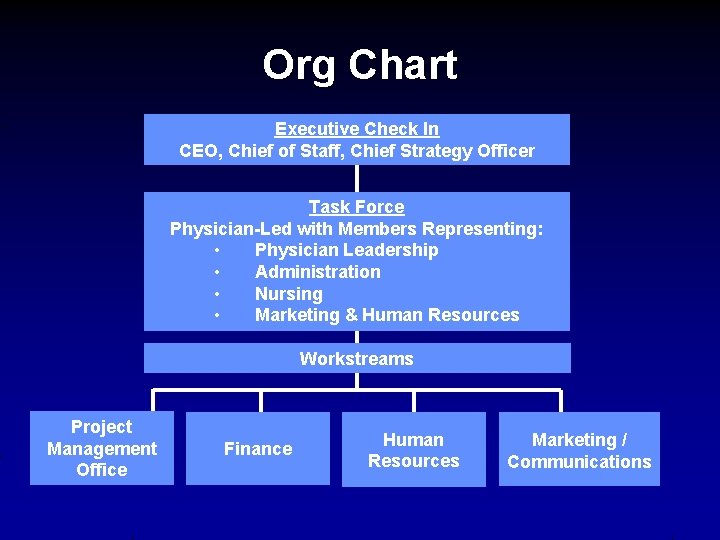
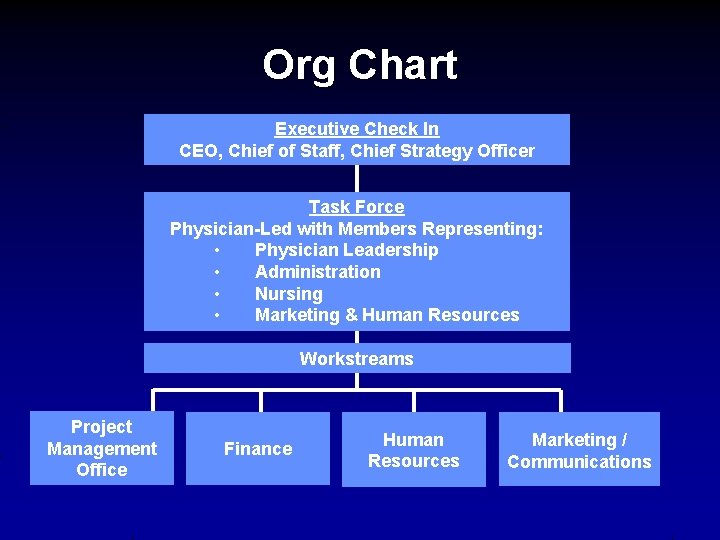
Org Chart Executive Check In CEO, Chief of Staff, Chief Strategy Officer Task Force Physician-Led with Members Representing: • Physician Leadership • Administration • Nursing • Marketing & Human Resources Workstreams Project Management Office Finance Human Resources Marketing / Communications
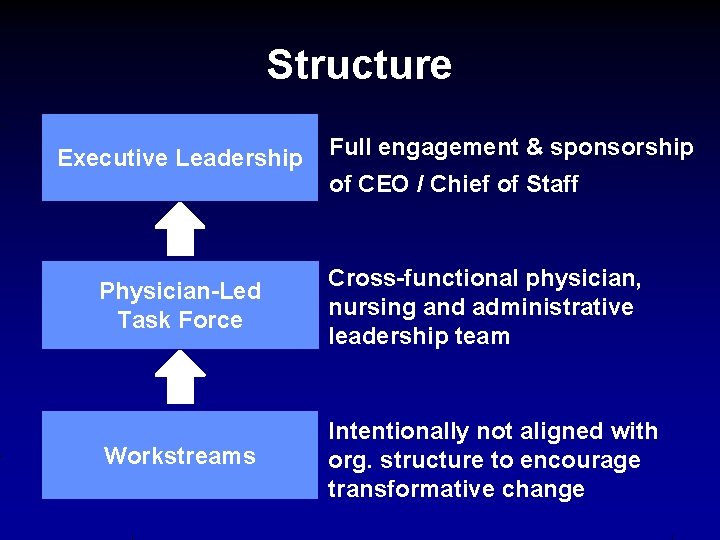
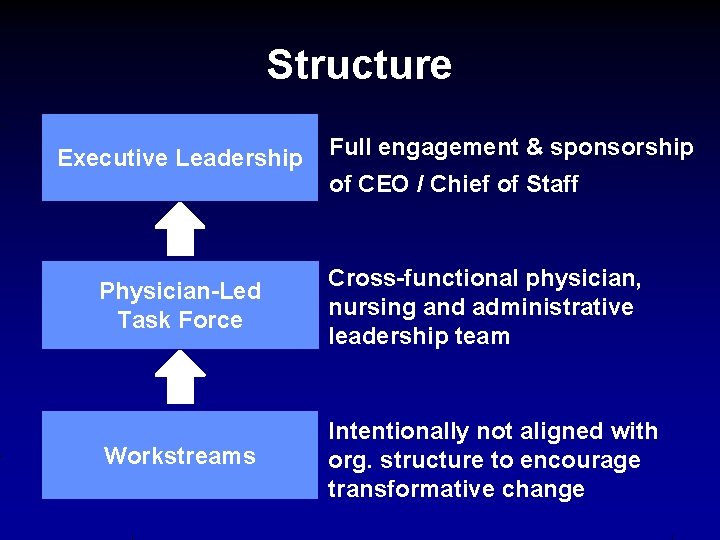
Structure Executive Leadership Full engagement & sponsorship of CEO / Chief of Staff Physician-Led Task Force Cross-functional physician, nursing and administrative leadership team Workstreams Intentionally not aligned with org. structure to encourage transformative change
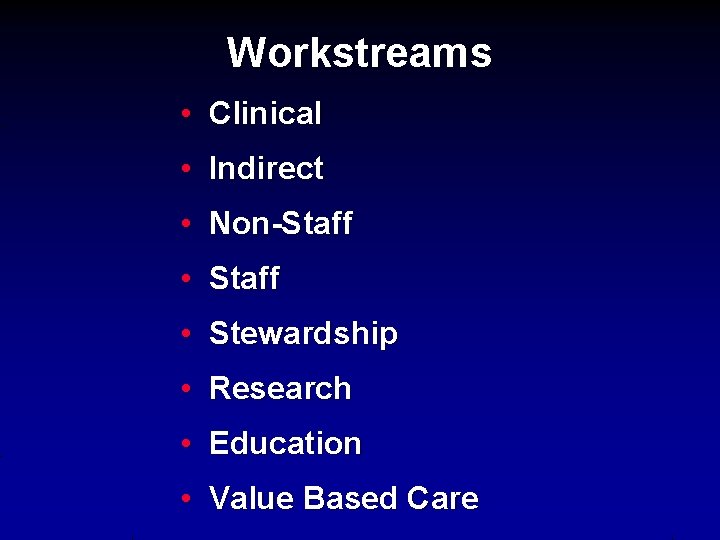
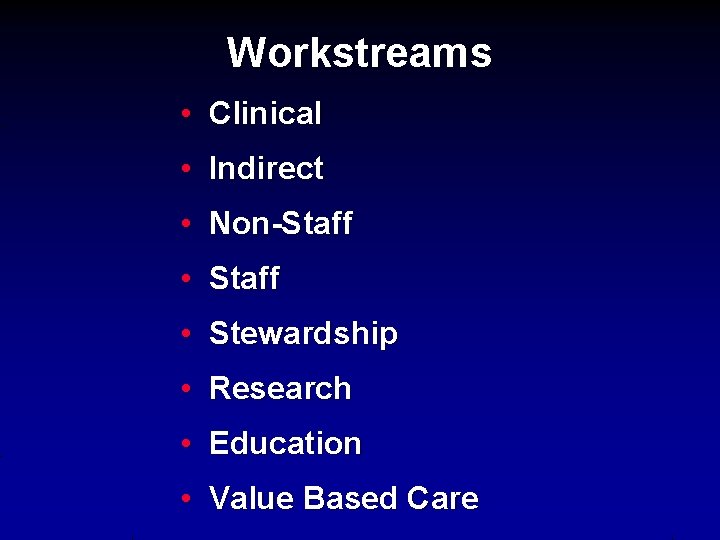
Workstreams • Clinical • Indirect • Non-Staff • Stewardship • Research • Education • Value Based Care
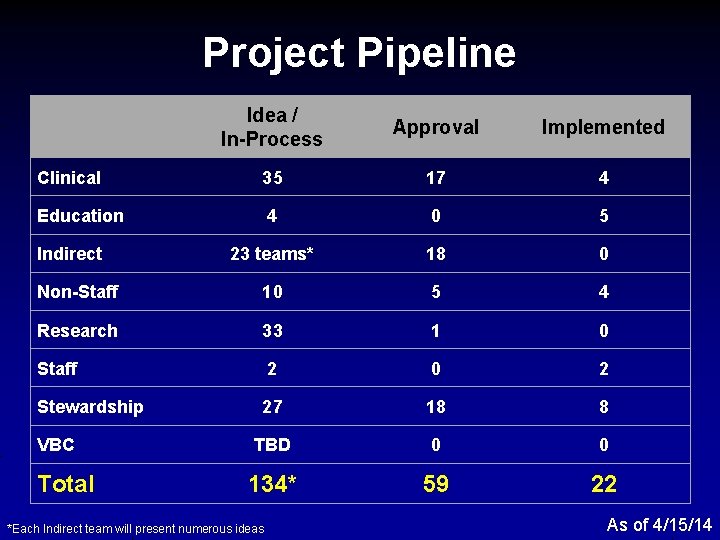
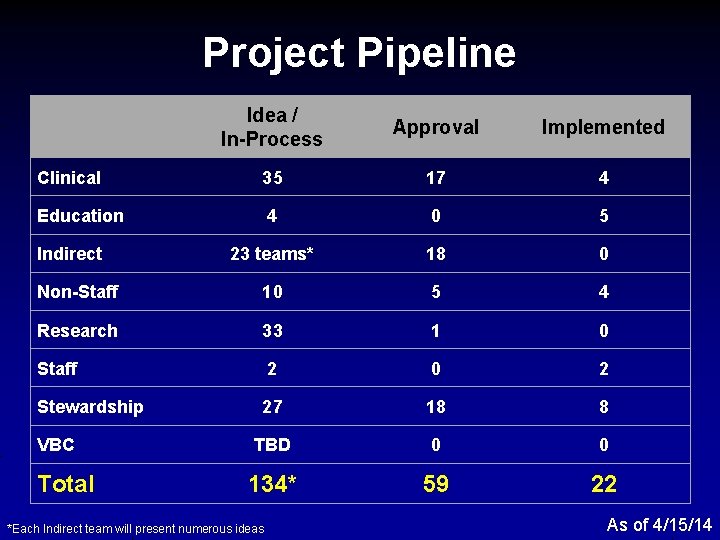
Project Pipeline Idea / In-Process Approval Implemented Clinical 35 17 4 Education 4 0 5 23 teams* 18 0 Non-Staff 10 5 4 Research 33 1 0 Staff 2 0 2 Stewardship 27 18 8 TBD 0 0 134* 59 22 Indirect VBC Total *Each Indirect team will present numerous ideas As of 4/15/14
Specific Pathology and Laboratory Medicine Drivers for Cost Reduction
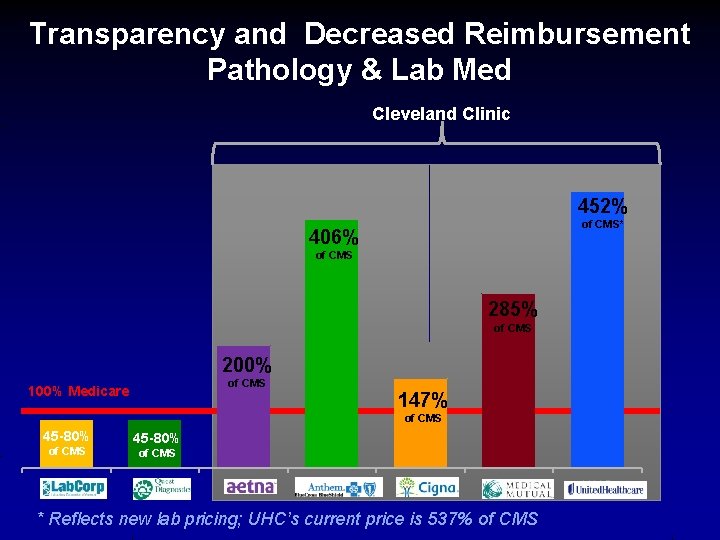
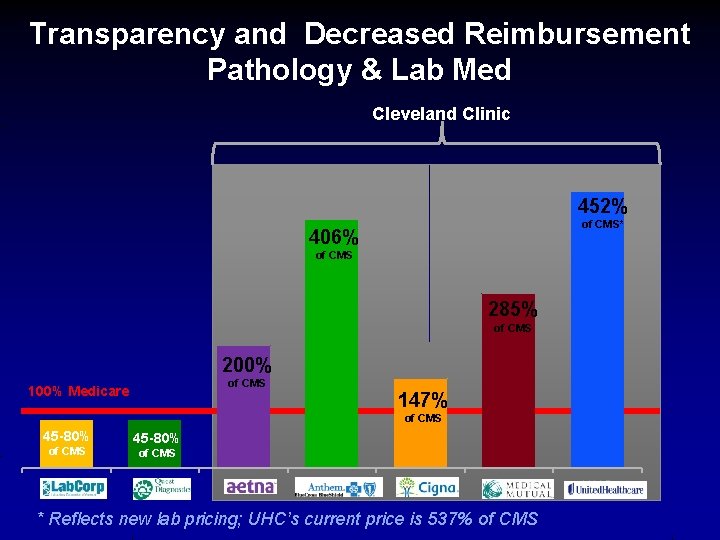
Transparency and Decreased Reimbursement Pathology & Lab Med Cleveland Clinic 452% of CMS* 406% of CMS 285% of CMS 200% of CMS 100% Medicare 147% of CMS 45 -80% of CMS Lab. Corp 45 -80% of CMS Quest Aetna Anthem Cigna MMO * Reflects new lab pricing; UHC’s current price is 537% of CMS UHC
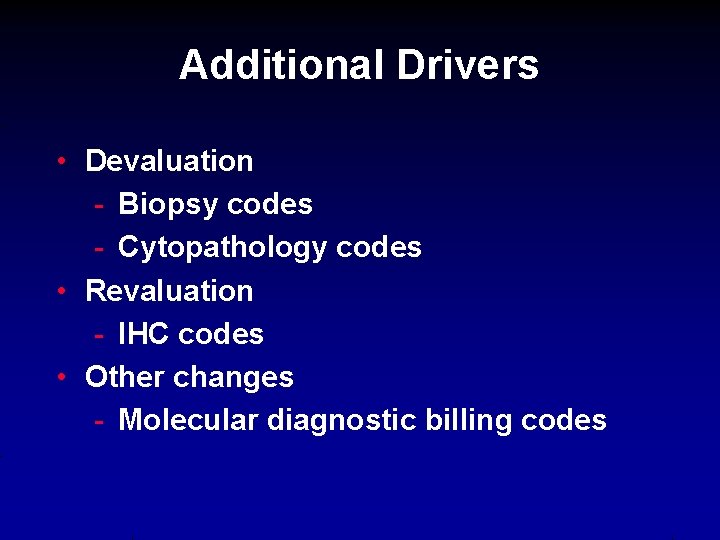
Additional Drivers • Devaluation - Biopsy codes - Cytopathology codes • Revaluation - IHC codes • Other changes - Molecular diagnostic billing codes
Robert J. Tomsich Pathology & Laboratory Medicine Institute Approach
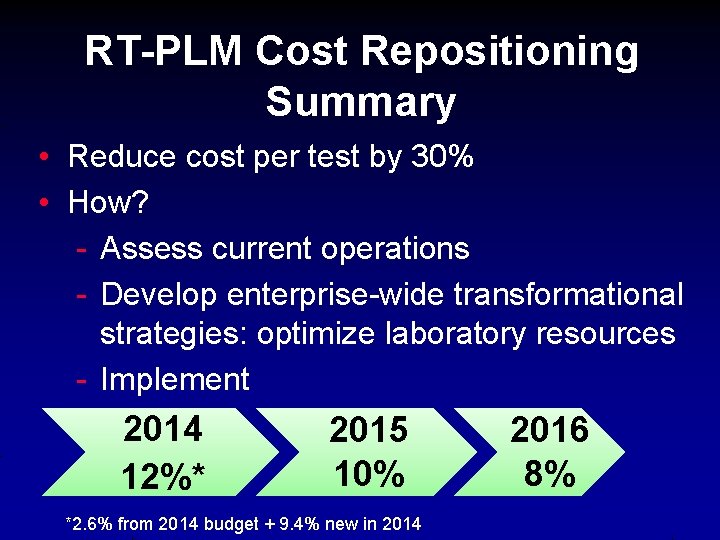
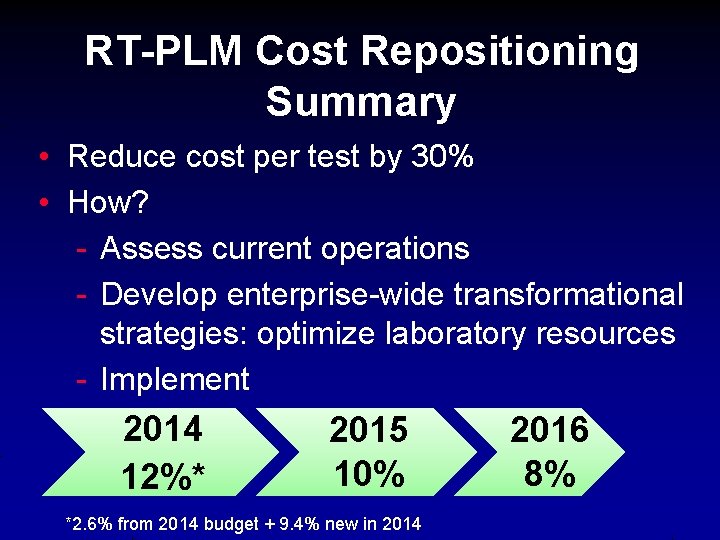
RT-PLM Cost Repositioning Summary • Reduce cost per test by 30% • How? - Assess current operations - Develop enterprise-wide transformational strategies: optimize laboratory resources - Implement 2014 12%* 2015 10% *2. 6% from 2014 budget + 9. 4% new in 2014 2016 8%
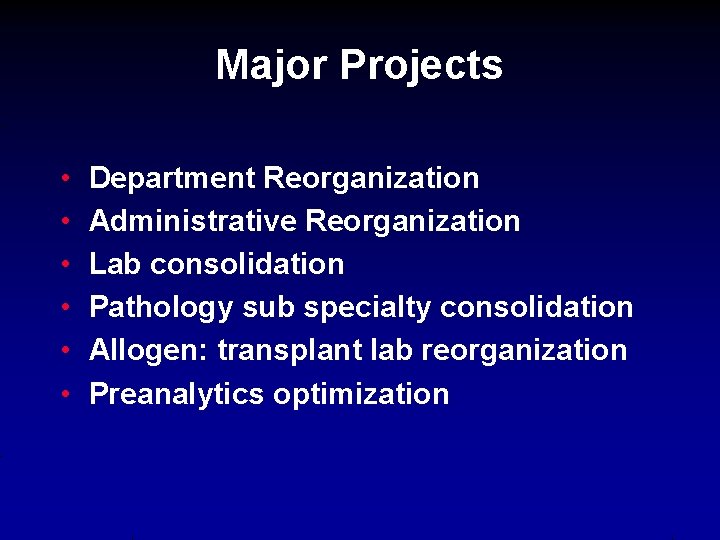
Major Projects • • • Department Reorganization Administrative Reorganization Lab consolidation Pathology sub specialty consolidation Allogen: transplant lab reorganization Preanalytics optimization
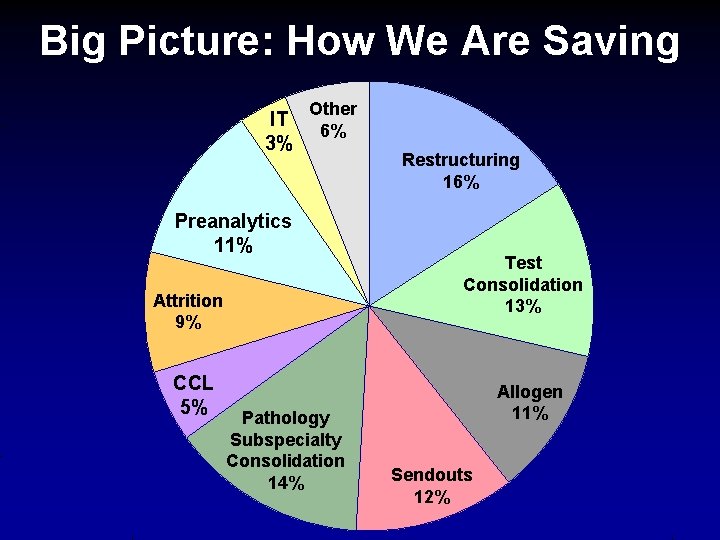
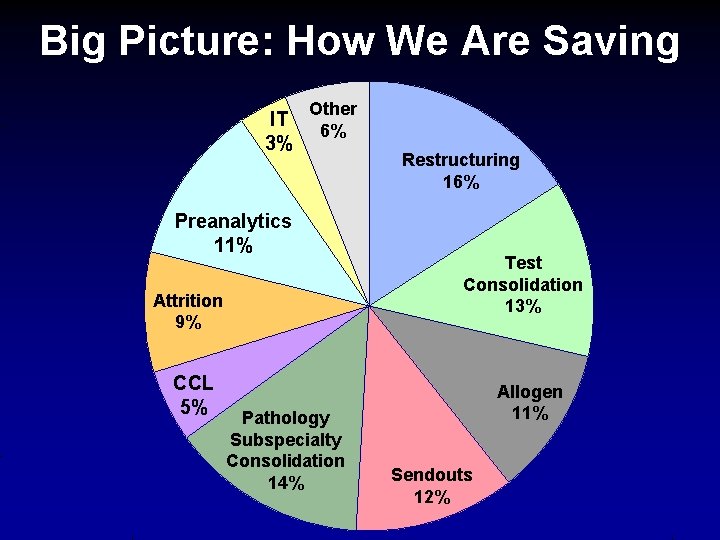
Big Picture: How We Are Saving IT 3% Other 6% Preanalytics 11% Attrition 9% CCL 5% Pathology Subspecialty Consolidation 14% Restructuring 16% Test Consolidation 13% Allogen 11% Sendouts 12%
Department and Administrative Reorganization
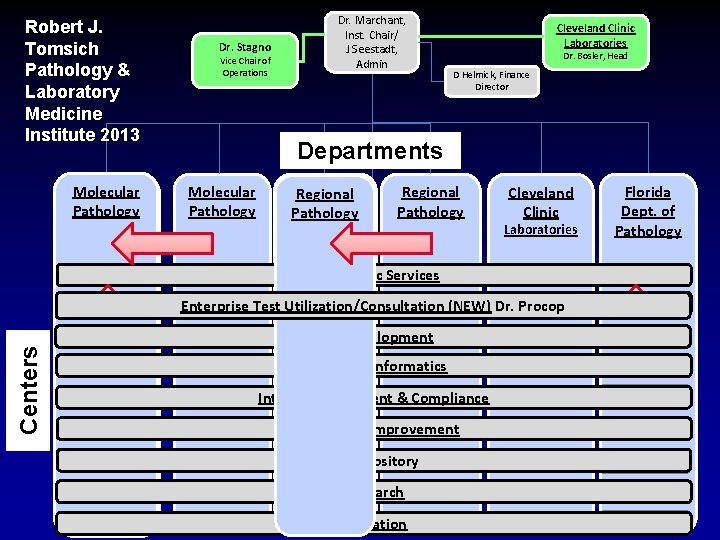
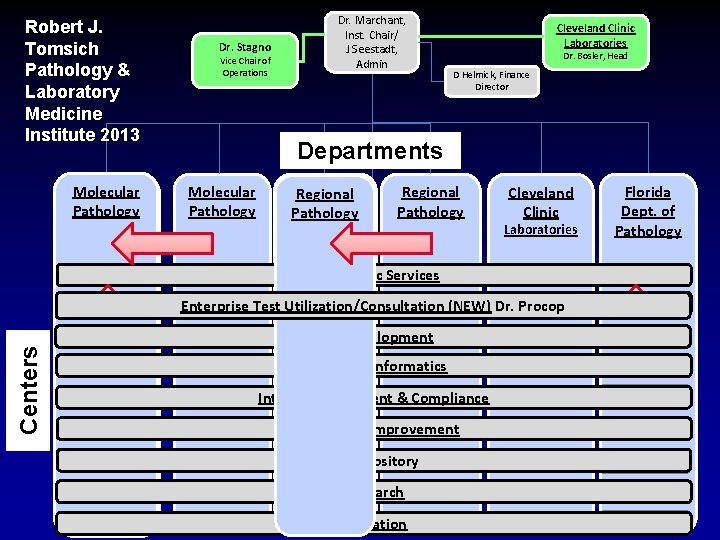
Robert J. Tomsich Pathology & Laboratory Medicine Institute 2013 Molecular Clinical Laboratory Pathology Medicine Dr. Hsi Dr. Stagno Vice Chair of Operations Dr. Marchant, Inst. Chair/ J Seestadt, Admin Cleveland Clinic Laboratories Dr. Bosler, Head D Helmick, Finance Director Departments Molecular Pathology Anatomic Regional Dr. Goldblum Pathology Dr. Goldblum Regional Pathology Cleveland Clinic Laboratories Preanalytic Services Centers Family Health Centers (NEW) Dr. Procop Enterprise Test Utilization/Consultation Test Development Pathology Informatics Internal Assessment & Compliance Continuous Improvement Biorepository Research Education Florida Dept. of Pathology
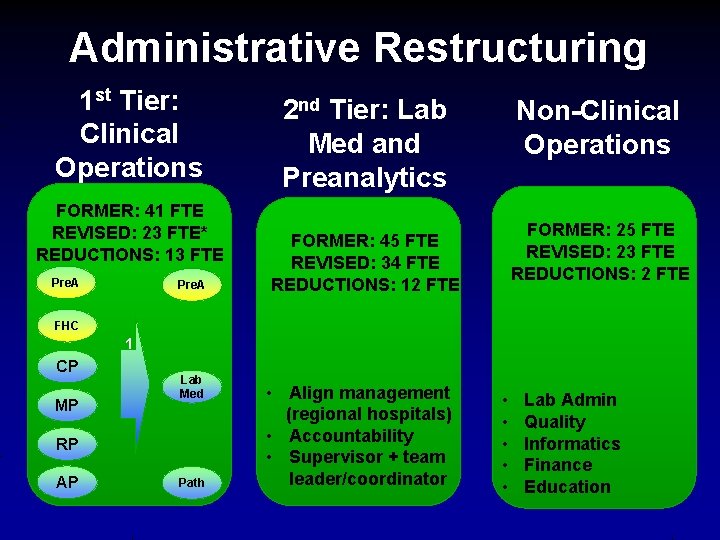
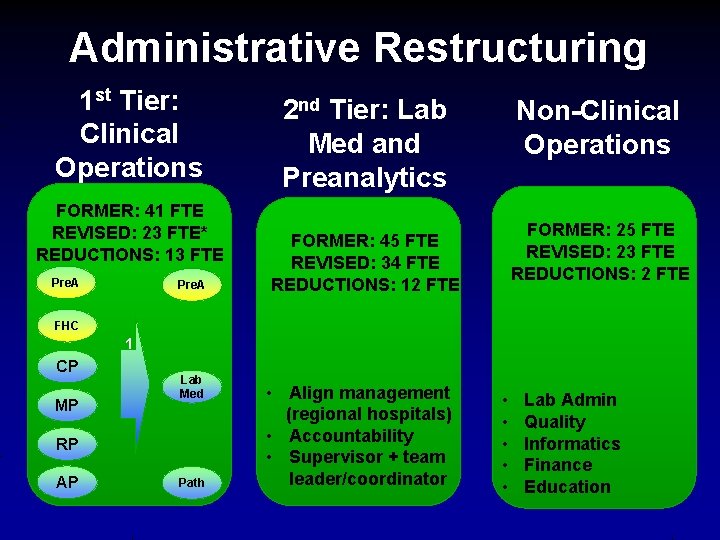
Administrative Restructuring 1 st Tier: Clinical Operations FORMER: 41 FTE REVISED: 23 FTE* REDUCTIONS: 13 FTE Pre. A 2 nd Tier: Lab Med and Preanalytics Non-Clinical Operations FORMER: 25 FTE REVISED: 23 FTE REDUCTIONS: 2 FTE FORMER: 45 FTE REVISED: 34 FTE REDUCTIONS: 12 FTE FHC 1 CP MP Lab Med RP AP Path • Align management (regional hospitals) • Accountability • Supervisor + team leader/coordinator • • • Lab Admin Quality Informatics Finance Education
Lab Consolidation
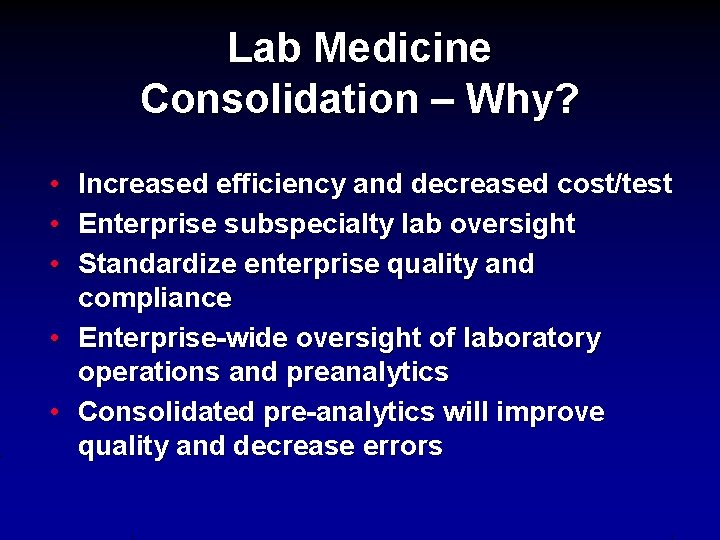
Lab Medicine Consolidation – Why? • Increased efficiency and decreased cost/test • Enterprise subspecialty lab oversight • Standardize enterprise quality and compliance • Enterprise-wide oversight of laboratory operations and preanalytics • Consolidated pre-analytics will improve quality and decrease errors
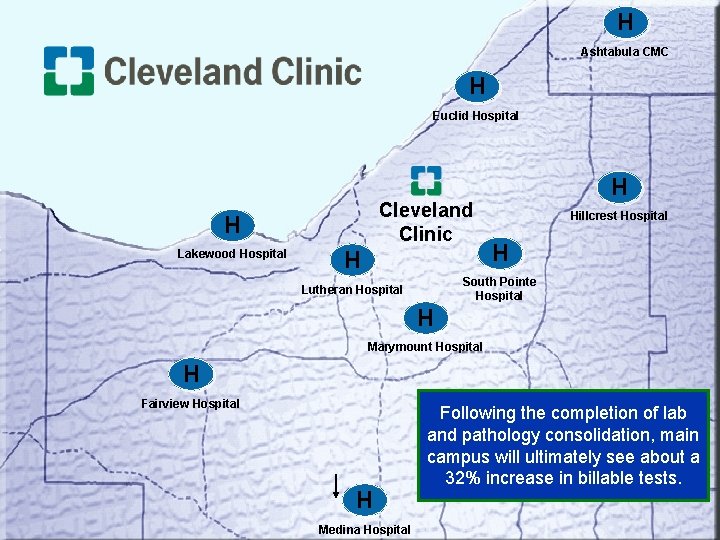
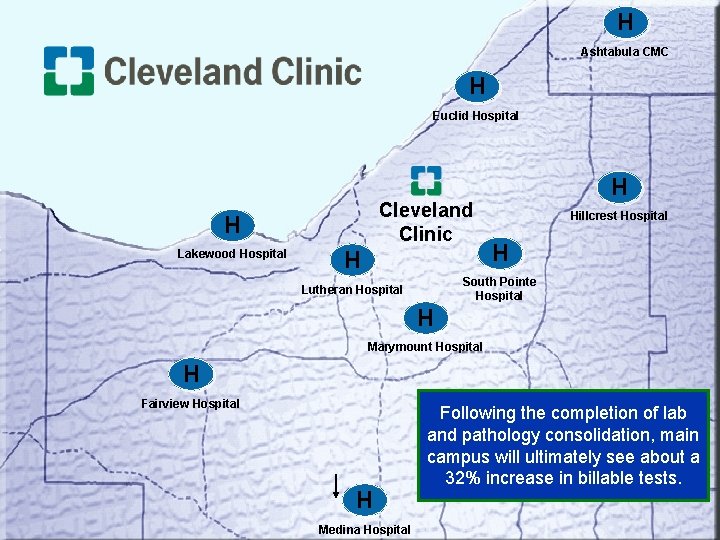
H Ashtabula CMC H Euclid Hospital Cleveland Clinic H Lakewood Hospital H H Hillcrest Hospital H South Pointe Hospital Lutheran Hospital H Marymount Hospital H Fairview Hospital H Medina Hospital Following the completion of lab and pathology consolidation, main campus will ultimately see about a 32% increase in billable tests.
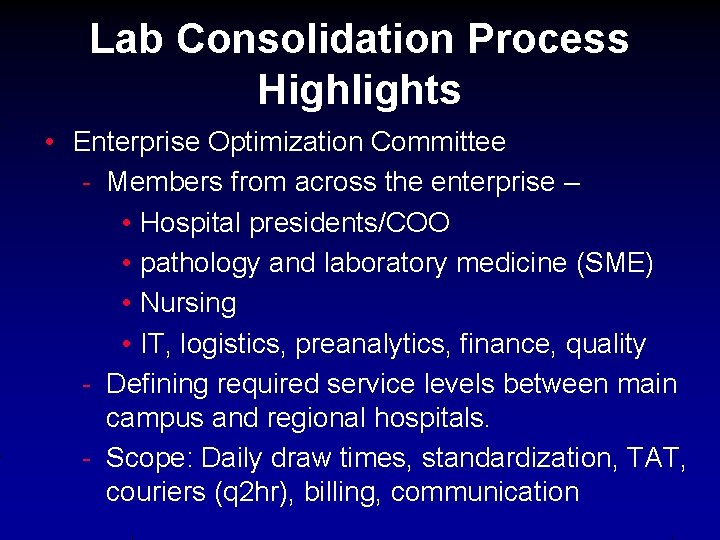
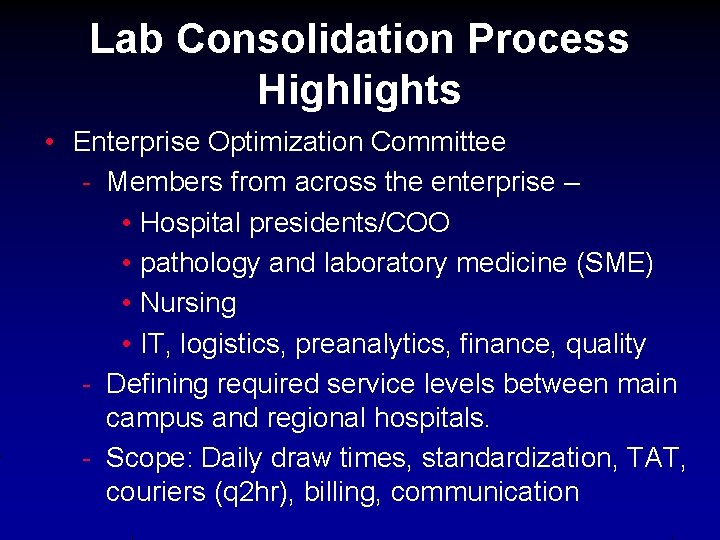
Lab Consolidation Process Highlights • Enterprise Optimization Committee - Members from across the enterprise – • Hospital presidents/COO • pathology and laboratory medicine (SME) • Nursing • IT, logistics, preanalytics, finance, quality - Defining required service levels between main campus and regional hospitals. - Scope: Daily draw times, standardization, TAT, couriers (q 2 hr), billing, communication
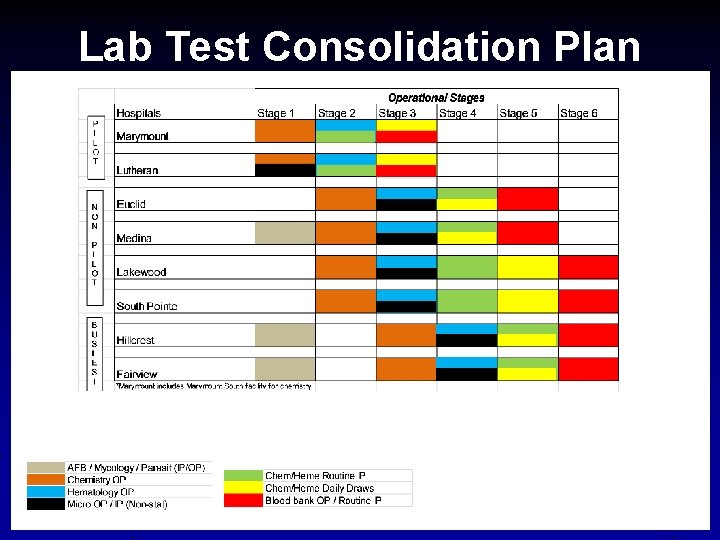
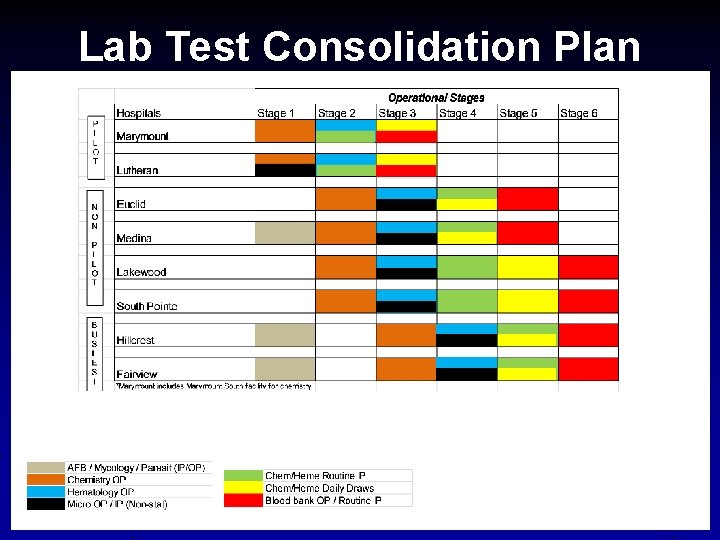
Lab Test Consolidation Plan
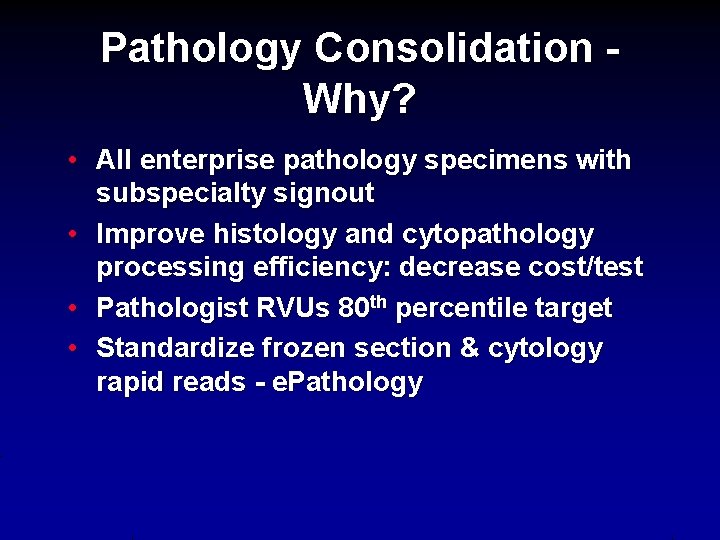
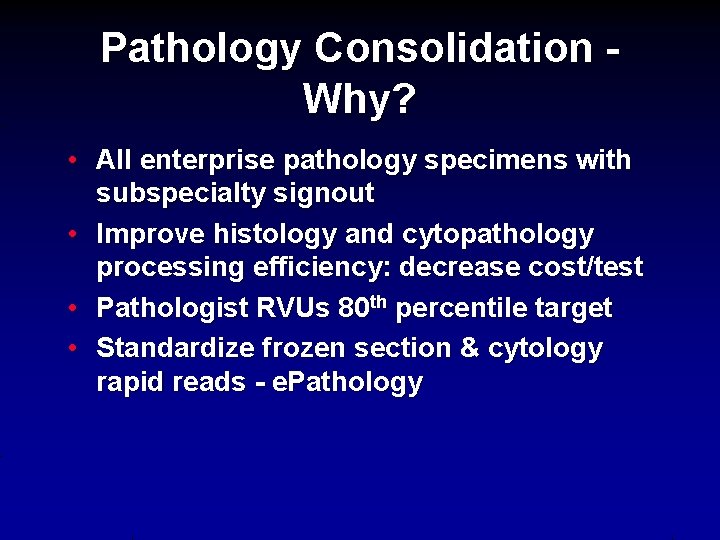
Pathology Consolidation Why? • All enterprise pathology specimens with subspecialty signout • Improve histology and cytopathology processing efficiency: decrease cost/test • Pathologist RVUs 80 th percentile target • Standardize frozen section & cytology rapid reads - e. Pathology
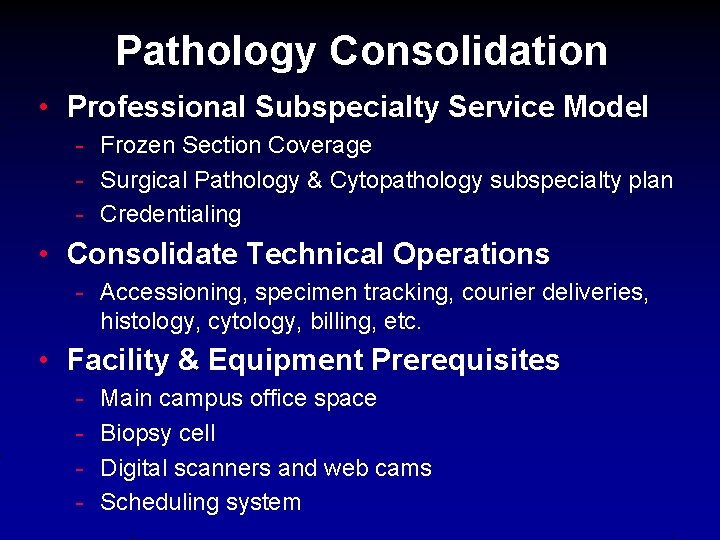
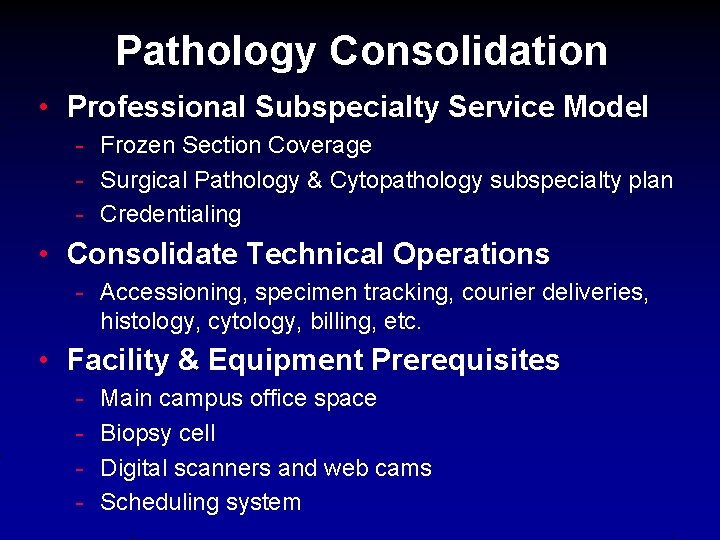
Pathology Consolidation • Professional Subspecialty Service Model - Frozen Section Coverage - Surgical Pathology & Cytopathology subspecialty plan - Credentialing • Consolidate Technical Operations - Accessioning, specimen tracking, courier deliveries, histology, cytology, billing, etc. • Facility & Equipment Prerequisites - Main campus office space Biopsy cell Digital scanners and web cams Scheduling system
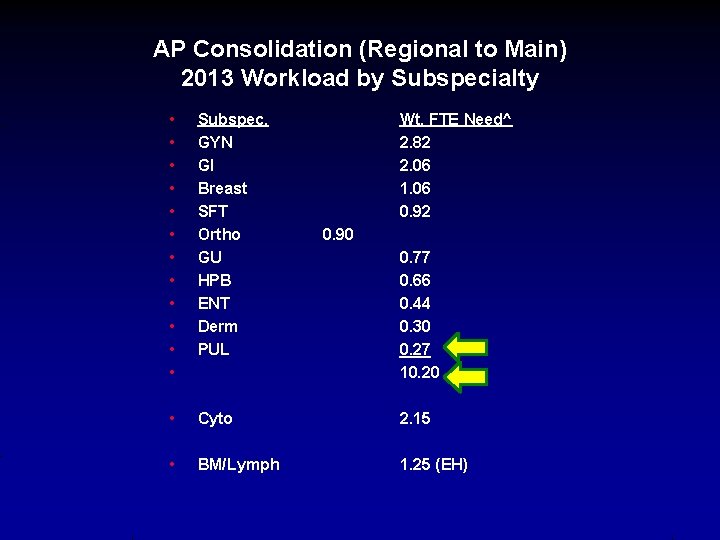
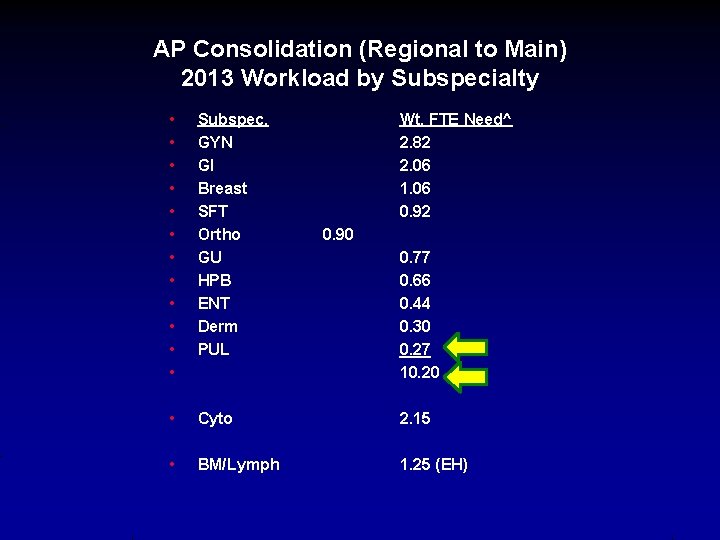
AP Consolidation (Regional to Main) 2013 Workload by Subspecialty • • • Subspec. GYN GI Breast SFT Ortho GU HPB ENT Derm PUL • Cyto 2. 15 • BM/Lymph 1. 25 (EH) Wt. FTE Need^ 2. 82 2. 06 1. 06 0. 92 0. 90 0. 77 0. 66 0. 44 0. 30 0. 27 10. 20
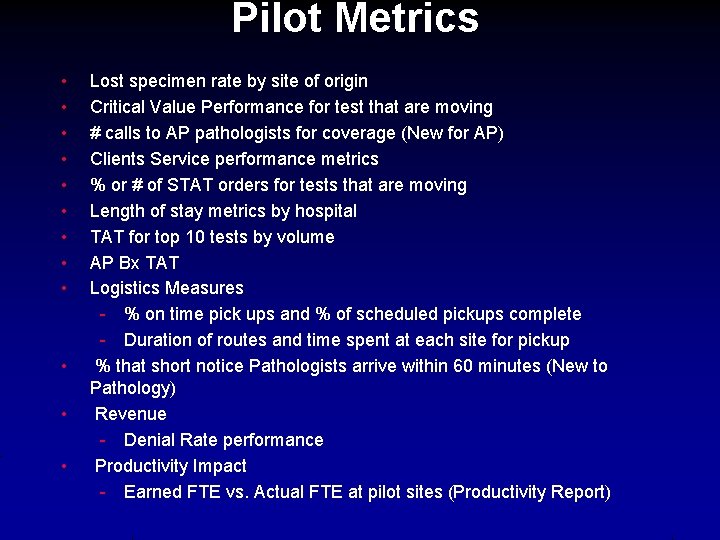
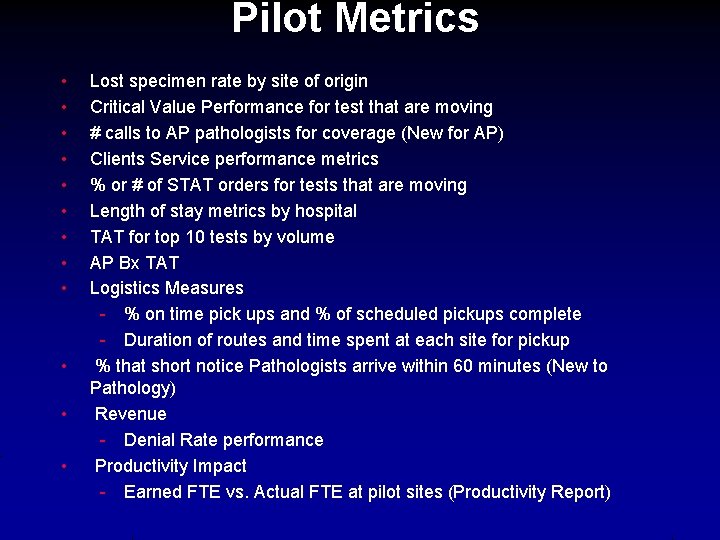
Pilot Metrics • • • Lost specimen rate by site of origin Critical Value Performance for test that are moving # calls to AP pathologists for coverage (New for AP) Clients Service performance metrics % or # of STAT orders for tests that are moving Length of stay metrics by hospital TAT for top 10 tests by volume AP Bx TAT Logistics Measures - % on time pick ups and % of scheduled pickups complete - Duration of routes and time spent at each site for pickup % that short notice Pathologists arrive within 60 minutes (New to Pathology) Revenue - Denial Rate performance Productivity Impact - Earned FTE vs. Actual FTE at pilot sites (Productivity Report)
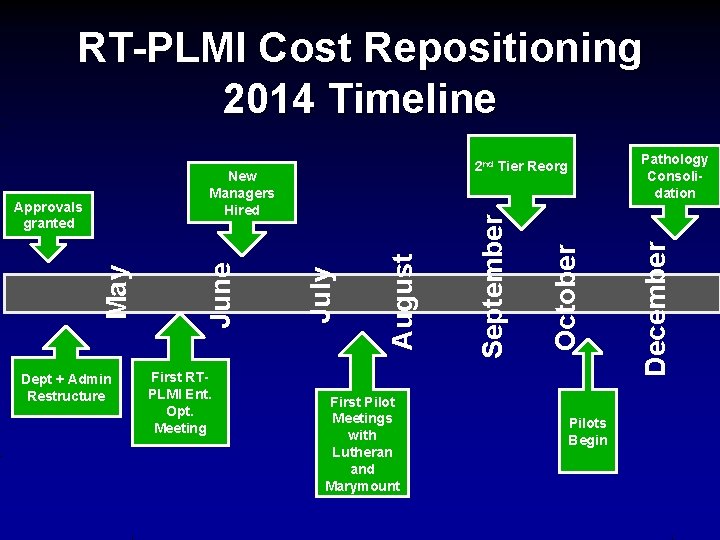
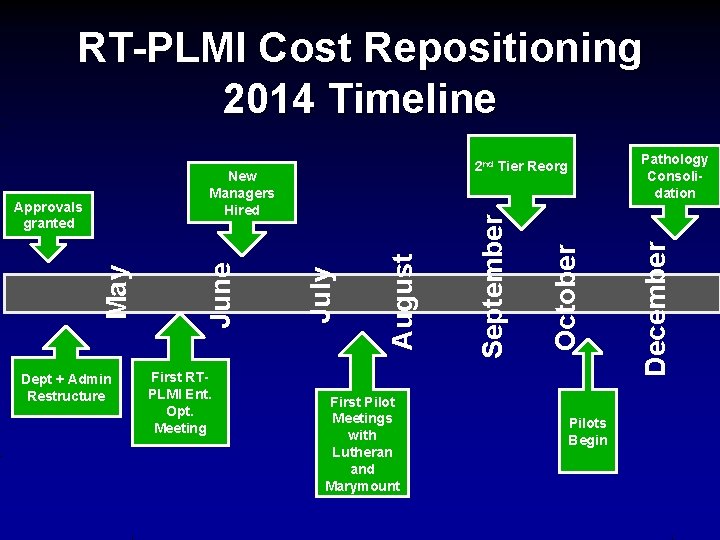
RT-PLMI Cost Repositioning 2014 Timeline October September August First Pilot Meetings with Lutheran and Marymount Pilots Begin December First RTPLMI Ent. Opt. Meeting July May Dept + Admin Restructure June New Managers Hired Approvals granted Pathology Consolidation 2 nd Tier Reorg
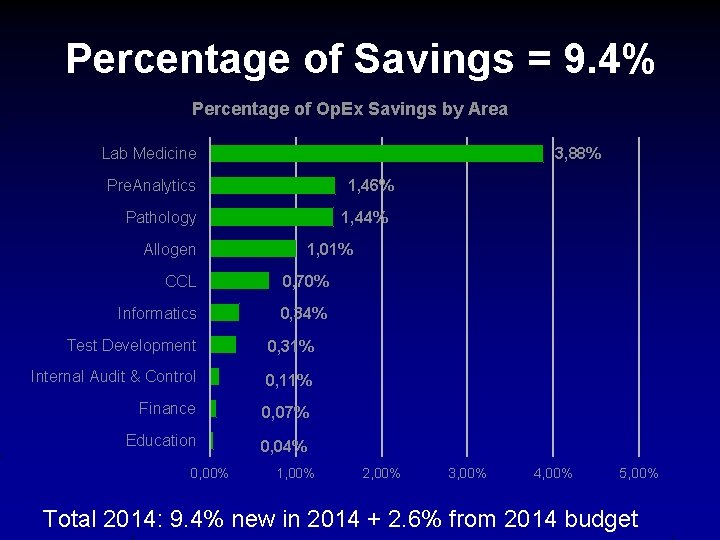
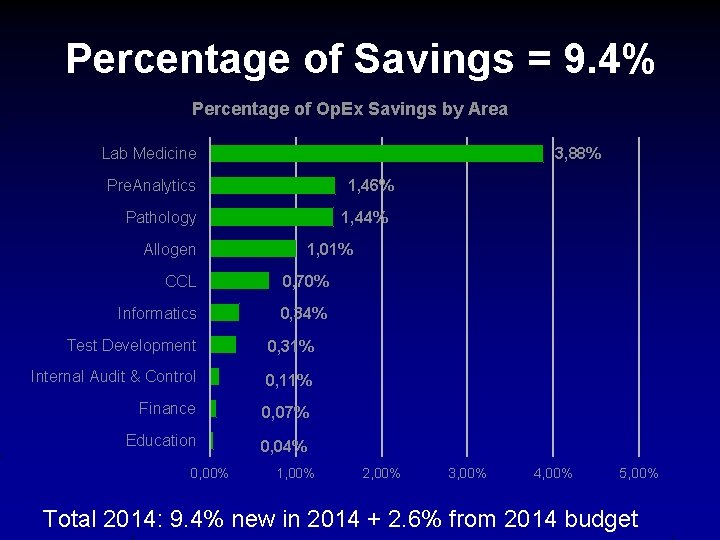
Percentage of Savings = 9. 4% Percentage of Op. Ex Savings by Area Lab Medicine 3, 88% Pre. Analytics 1, 46% Pathology 1, 44% Allogen 1, 01% CCL 0, 70% Informatics 0, 34% Test Development 0, 31% Internal Audit & Control 0, 11% Finance 0, 07% Education 0, 04% 0, 00% 1, 00% 2, 00% 3, 00% 4, 00% 5, 00% Total 2014: 9. 4% new in 2014 + 2. 6% from 2014 budget
Challenges • Long-term, multi-year transformation • Change throughout organization • Aligning annual planning timeline / process • Organizational engagement • Communication to all stakeholders • Setting service level expectations
“…. the pathway to improving quality and safety is the same pathway to lowering cost, and that involves relentlessly taking waste and unnecessary variability out of our processes. ”

Questions?