Confusion Cause Dr Matthew Mc Namee Consultant Geriatrician









- Slides: 43
Confusion ? Cause Dr Matthew Mc. Namee Consultant Geriatrician IMT Regional Teaching 07/10/20
Case Outline Approach to older person with confusion ‘Agitated’ patient
Please come and see Mrs Smith IMT on Call Confused ? UTI Nurses are concerned as she keeps pulling at drip
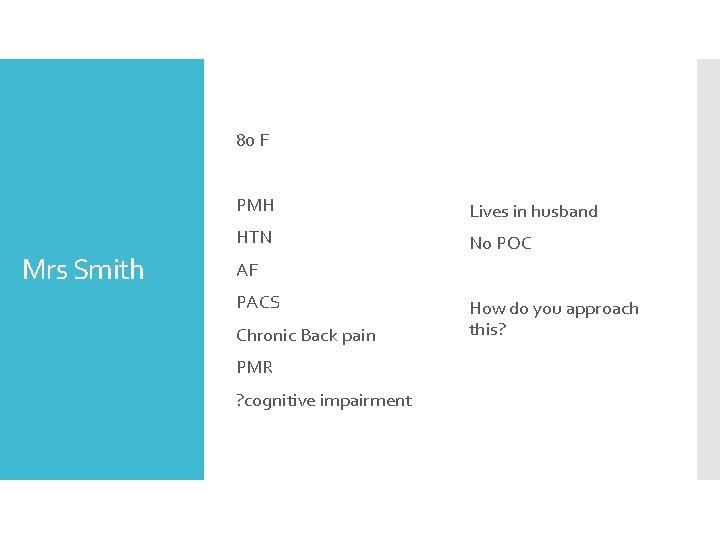
80 F Mrs Smith PMH Lives in husband HTN No POC AF PACS Chronic Back pain PMR ? cognitive impairment How do you approach this?
History is limited Rambling Mrs Smith Pulling at line/Catheter Trying to get out bed No results back
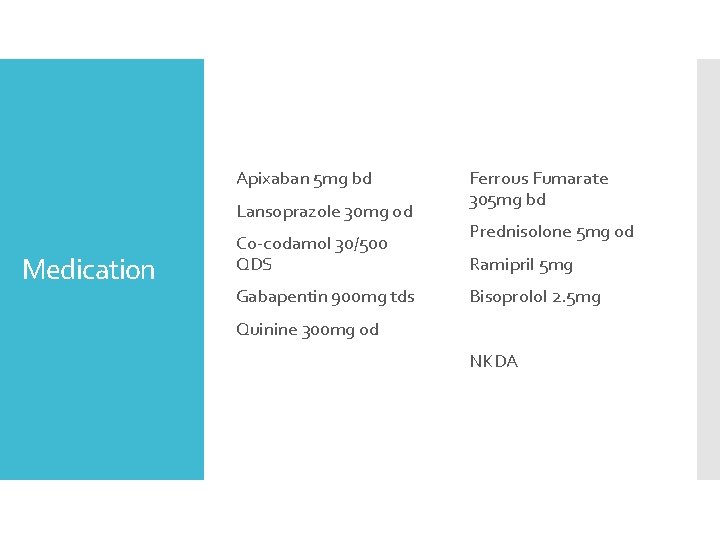
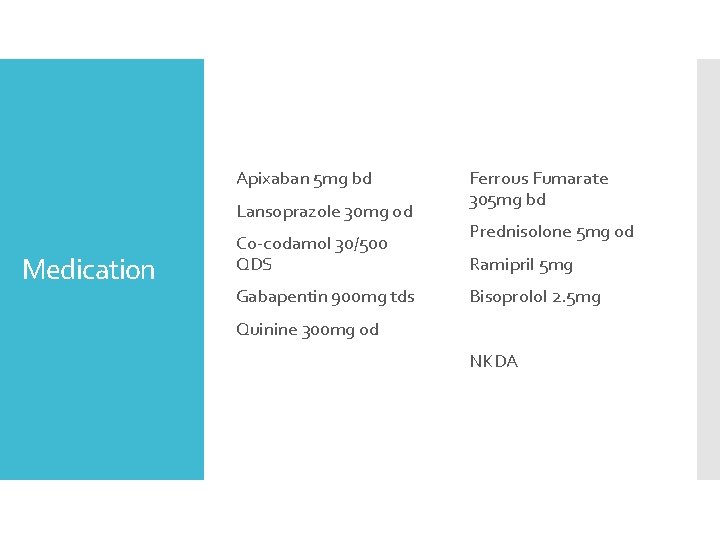
Apixaban 5 mg bd Lansoprazole 30 mg od Medication Co-codamol 30/500 QDS Gabapentin 900 mg tds Ferrous Fumarate 305 mg bd Prednisolone 5 mg od Ramipril 5 mg Bisoprolol 2. 5 mg Quinine 300 mg od NKDA
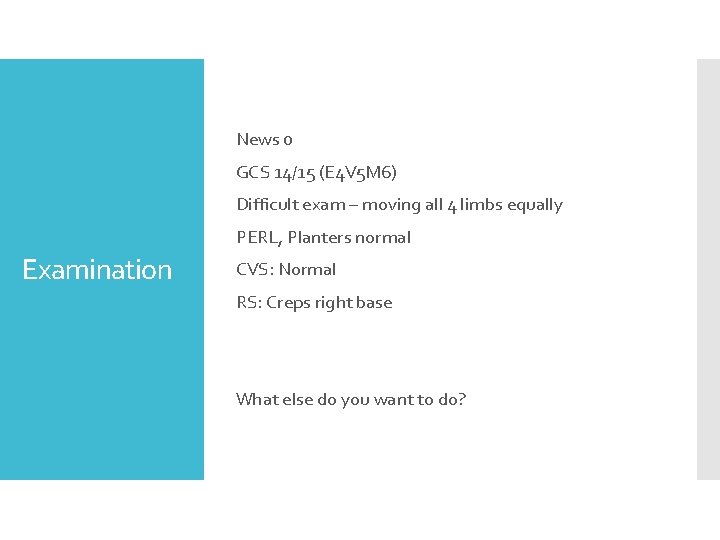
News 0 GCS 14/15 (E 4 V 5 M 6) Difficult exam – moving all 4 limbs equally PERL, Planters normal Examination CVS: Normal RS: Creps right base What else do you want to do?
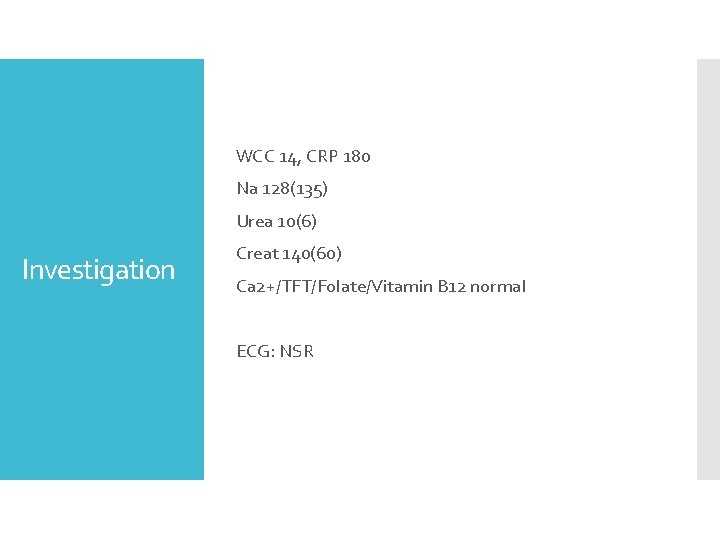
WCC 14, CRP 180 Na 128(135) Urea 10(6) Investigation Creat 140(60) Ca 2+/TFT/Folate/Vitamin B 12 normal ECG: NSR

Diagnosis
CAP – CURB 65 = 3 AKI Diagnosis Multifactorial Hyperactive delirium CAP AKI Drugs (Gabapentin/Co-codamol/Steroids) Change in environment
Doesn’t she have dementia? Mrs Smith Does she need a CT head? If she less agitated and ‘behaving well’ would that change the diagnosis?
Is Delirium a benign condition? Delirium How long can delirium last for? Where should Mrs Smith be managed?

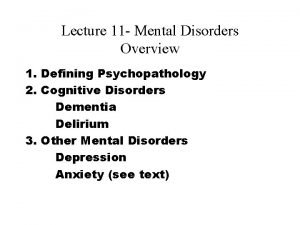
Delirium
‘Acute confusional state’ triggers by acute medical/physical health issue Key features Impaired cognition Acute onset – Hours to days Fluctuating in nature Impaired attention/concentration Hallucinations/delusions
Common – 20% of all adult medical patients ICU 75% Hip fracture 50% Underdiagnosed/Under appreciated Background Increase morbidity – Pressure sores/Dementia/Falls/Fractures Increase chance of institutionalisation Increase mortality – 10 -30%

Risk factors Advancing age Alcohol misue Pre existing dementia/Previous delirium Hospital admission Sensory impairment Frailty Polypharmacy Terminal illness Postoperative – 26% of patients > 65 had
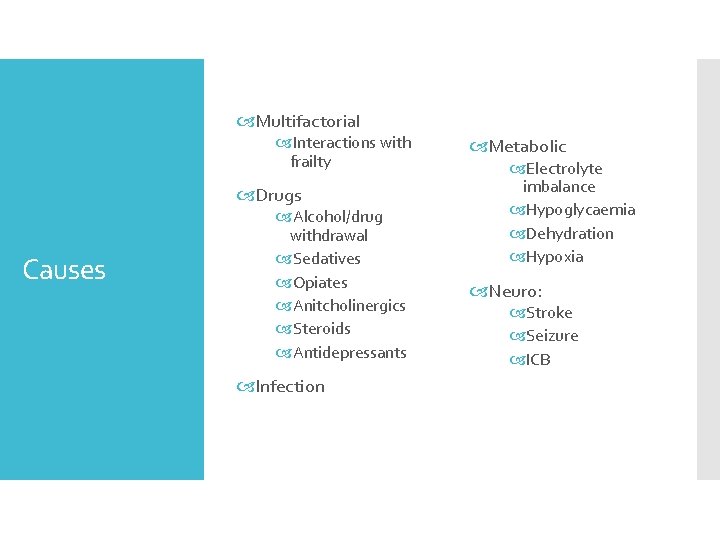
Causes
Multifactorial Interactions with frailty Drugs Causes Alcohol/drug withdrawal Sedatives Opiates Anitcholinergics Steroids Antidepressants Infection Metabolic Electrolyte imbalance Hypoglycaemia Dehydration Hypoxia Neuro: Stroke Seizure ICB

Other Causes Constipation Urinary retention IV lines/catheters Pain Unknown Environment Change of environment Bed moves Poor sleep Immobility Noise/lighting Sensory impairment
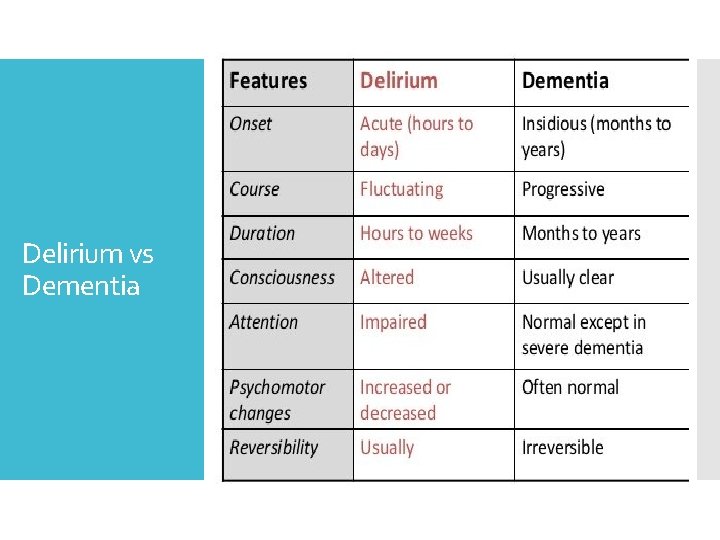
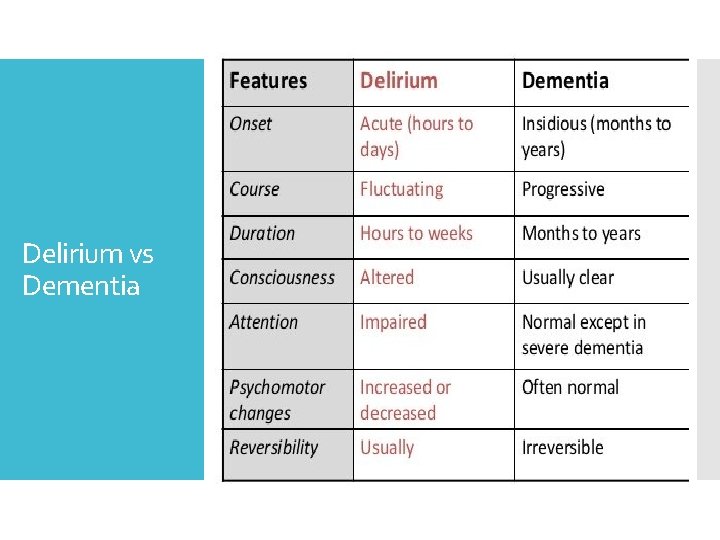
Delirium vs Dementia
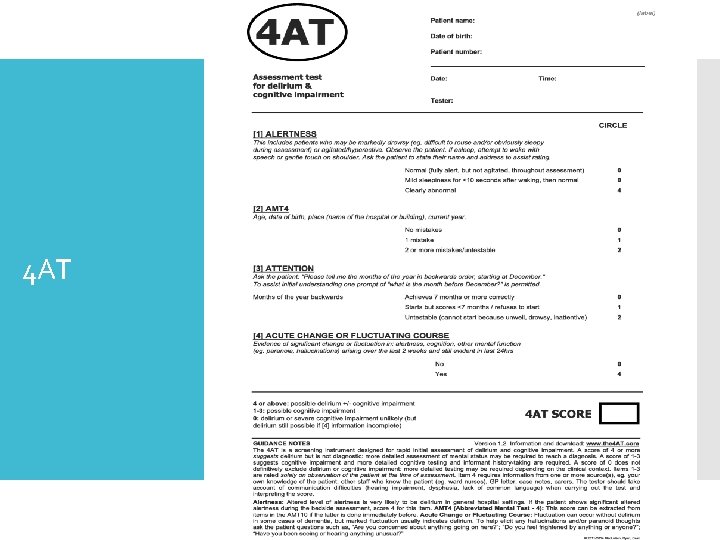
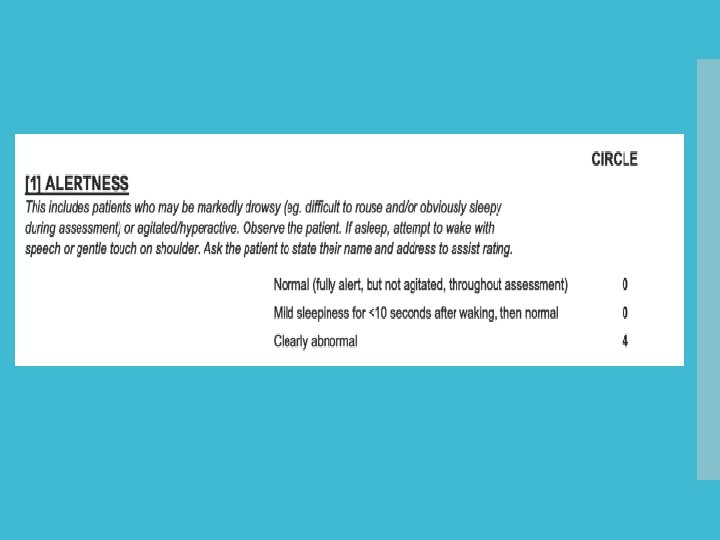
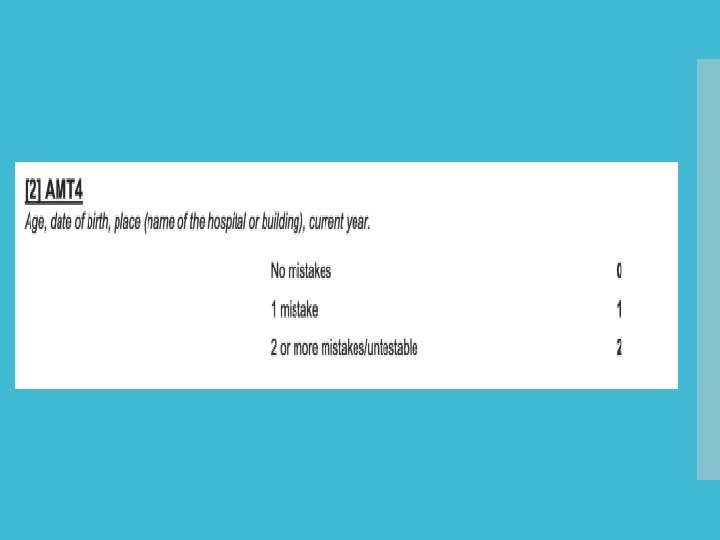
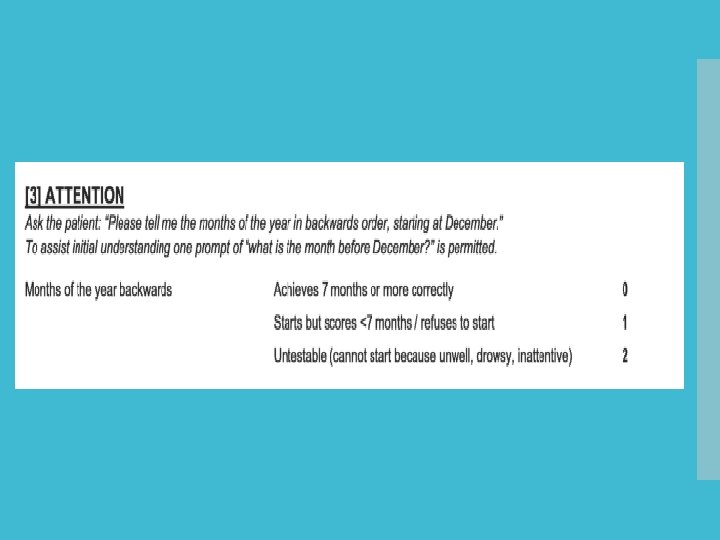
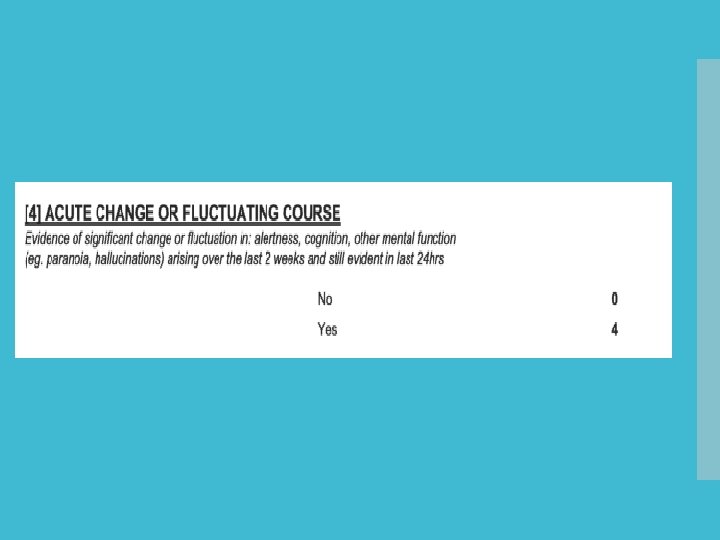
4 AT Diagnosis CAM
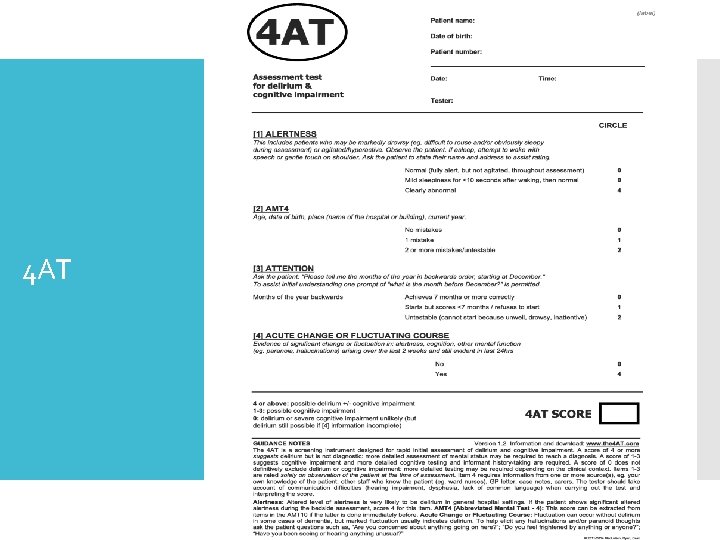
4 AT
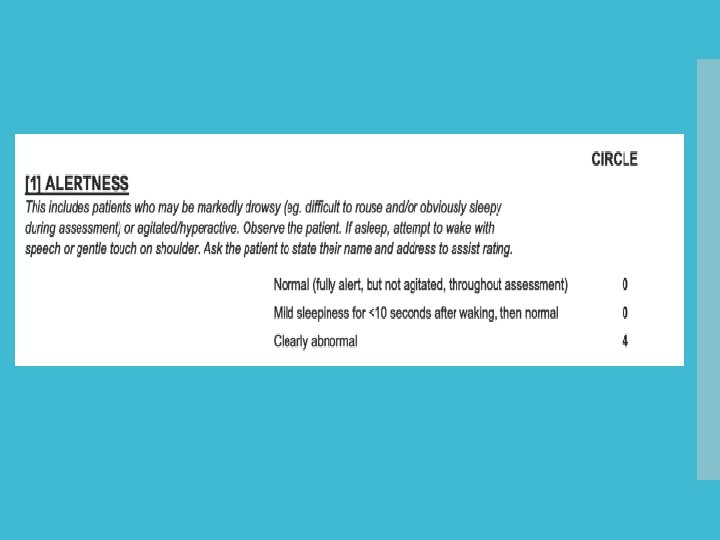
4 AT
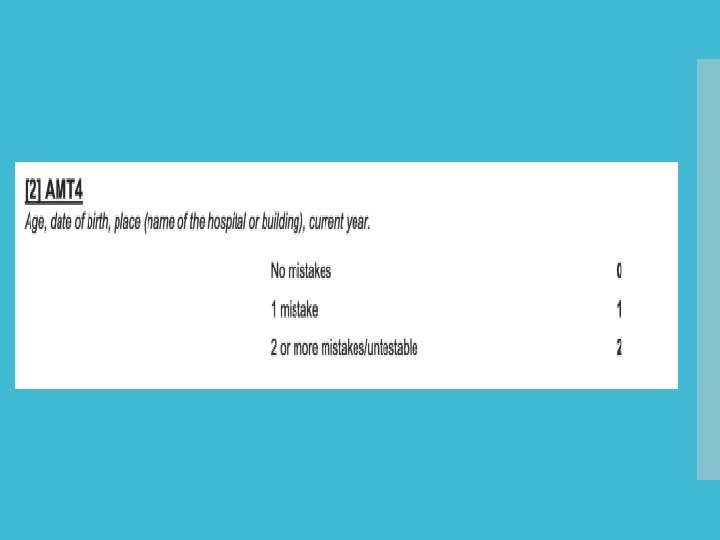
4 AT
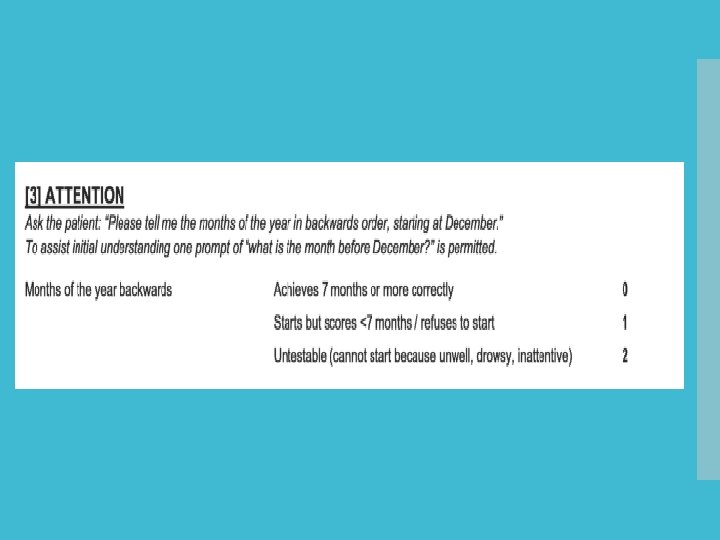
4 AT
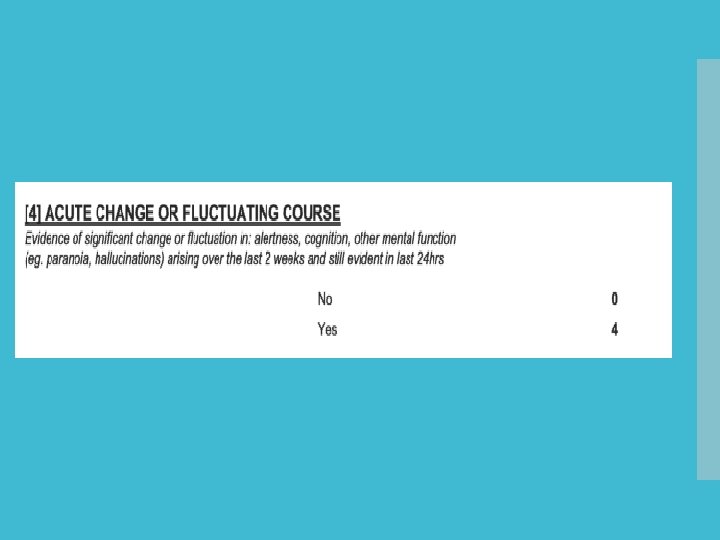
4 AT

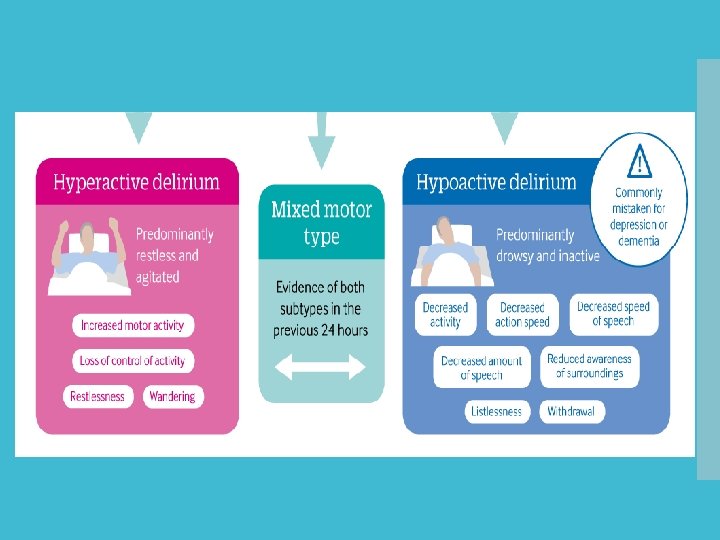
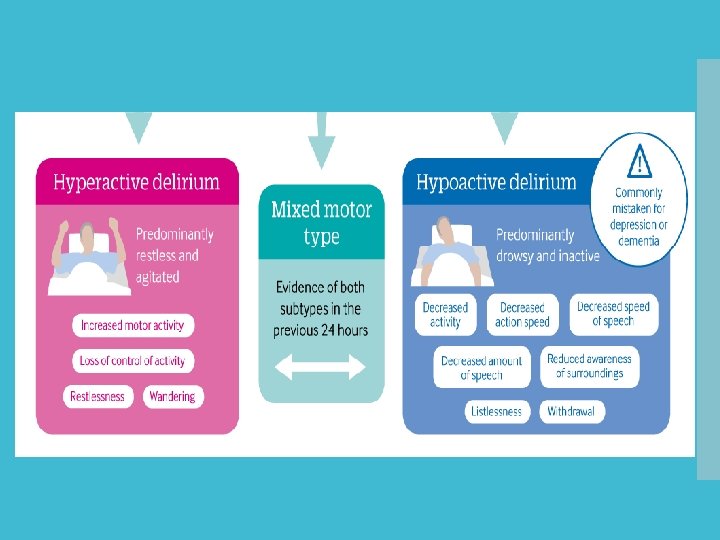
Hyperactive vs Hypoactive

Collateral history Acute, fluctuations, previous episodes of delirium Assessment Baseline Cognition Any previous concerns – any progressive symptoms Triggers: New medication, infection, Bowels
Consider triggers Blood tests – Vitamin b 12/folate/Ca 2+/TFTs Investigations Infection screen Consider Brain imaging
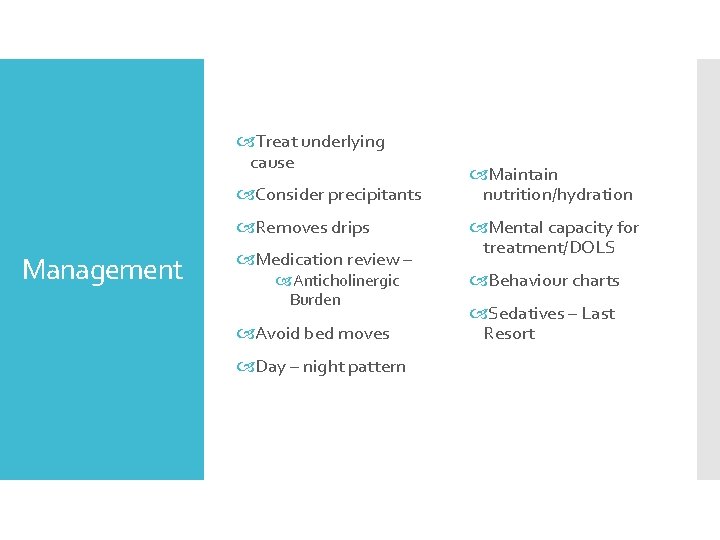
Treat underlying cause Consider precipitants Removes drips Management Medication review – Anticholinergic Burden Avoid bed moves Day – night pattern Maintain nutrition/hydration Mental capacity for treatment/DOLS Behaviour charts Sedatives – Last Resort

Environment Quiet, calm environment Family supportvisiting times Orientation – clocks/calenders Avoid ward moves Dangerous objects removed Encourage mobilisation Hearing aids/Glasses Education of staff, patients, relatives Consider dignity, not using bed rails (Mattress, lower bed) Supervision
Explore what there understanding of delirium Not back to ‘normal’ on discharge Can take day-weeks- 6 months to improve Discussion with relatives Best in own environment May need short term placement for assessment May not resolve Risk factor for developing dementia

Now on AMU IMT on call Mrs Smith Can you urgently come to see Mrs Smith as she has hit a member of staff Security are with patient at time
Non – pharmacological management preferred Drugs make delirium worse Symptom control Regularly rather than emergency Oral rather than IM Start low and go slow Covertly Support nursing and care staff
Oral medication Pharmacological management Haloperidol is first line – 0. 5 mg oral (Max 2 mg/24 hour) Risperidone – 0. 25 mg oral (Max 1 mg/24 hour) Contraindicated: QTC/PD/Lewy Body Dementia Lorazepam 0. 5 mg oral (Max 2 mg/24 hours)
Rapid sedation Last resort Discuss with NOK Deescalate Call family in DO NOT prescribe PRN This is me Check local guidelines Capacity assessment DOLS Support staff
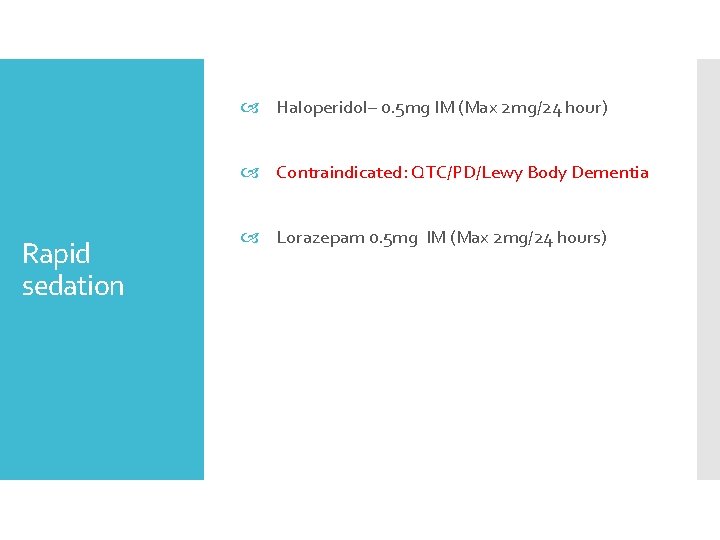
Haloperidol– 0. 5 mg IM (Max 2 mg/24 hour) Contraindicated: QTC/PD/Lewy Body Dementia Rapid sedation Lorazepam 0. 5 mg IM (Max 2 mg/24 hours)
Advice from Liaison Psychiatry Multidisciplinary working Medication advice Care needs Support family Follow up in community Neurology Physio and Occupational therapist
Thank you Questions
Mrs Andrew’s Story https: //www. youtube. com/watch? v=Fj_9 HG_TWE M

MDTea Podcasts https: //thehearingaidpodcasts. org. uk/ Useful links Geriatrics for juniors 2020 http: //aeme. org. uk/g 4 j 20/ Mini- Gems http: //aeme. org. uk/mini-gems/ Join BGS - https: //www. bgs. org. uk/
 Namee
Namee Compodit
Compodit Dr john ward geriatrician newcastle
Dr john ward geriatrician newcastle Geriatrics giants
Geriatrics giants Proximate cause and ultimate cause
Proximate cause and ultimate cause Proximate and ultimate causes of behaviour
Proximate and ultimate causes of behaviour Learned behavior biology
Learned behavior biology Ter death certificate
Ter death certificate Confusion matrix weka
Confusion matrix weka Avid tutorial process
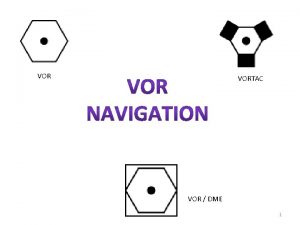
Avid tutorial process Vor dme symbol
Vor dme symbol Confusion is the first step toward clarity
Confusion is the first step toward clarity Confusion vs diffusion
Confusion vs diffusion Chapter 10:4 confusion and disorientation in the elderly
Chapter 10:4 confusion and disorientation in the elderly The melting point of naphthalene is 80
The melting point of naphthalene is 80 When confusion's my companion
When confusion's my companion Confusion dementia and alzheimer's disease
Confusion dementia and alzheimer's disease Confusion dementia and alzheimer disease chapter 19
Confusion dementia and alzheimer disease chapter 19 Constellation confusion worksheet
Constellation confusion worksheet Discalculia definicion
Discalculia definicion Maladaptation of identity vs role confusion
Maladaptation of identity vs role confusion Confusion matrix stata
Confusion matrix stata Confusion vs diffusion
Confusion vs diffusion ü
ü Melting confusion pmv
Melting confusion pmv Lesson 4.5 conditional probability and independence
Lesson 4.5 conditional probability and independence Diffusion and confusion in cryptography
Diffusion and confusion in cryptography Delirium definition
Delirium definition Trust vs mistrust example
Trust vs mistrust example Confusion and diffusion in block cipher
Confusion and diffusion in block cipher Identity vs confusion
Identity vs confusion Confusion dementia and alzheimer disease chapter 19
Confusion dementia and alzheimer disease chapter 19 What is identity vs role confusion
What is identity vs role confusion Post ictal
Post ictal Identity vs confusion
Identity vs confusion A helpful way for an na to respond to hallucinations is to
A helpful way for an na to respond to hallucinations is to Chapter 49 confusion and dementia
Chapter 49 confusion and dementia Identity foreclosure
Identity foreclosure Malfunction of communication
Malfunction of communication Alice in! 1 – the rabbit hole of confusion
Alice in! 1 – the rabbit hole of confusion Chapter 10:4 confusion and disorientation in the elderly
Chapter 10:4 confusion and disorientation in the elderly Chandelier electrical symbol
Chandelier electrical symbol Claudia norman a marketing consultant
Claudia norman a marketing consultant Stuart minty camden planning consultant
Stuart minty camden planning consultant