Community Geriatrics Dr Rhian Simpson Consultant Community Geriatrician










- Slides: 39
Community Geriatrics Dr Rhian Simpson Consultant Community Geriatrician Cambridgeshire Community Services
Summary • • Background Role of a Community Geriatrician Models for delivering community based care Evidence base
Background • • • Appointed in 2003 5 sessions Second Community Geriatrician locally No nationally accepted model Local recognition for more community based models of care


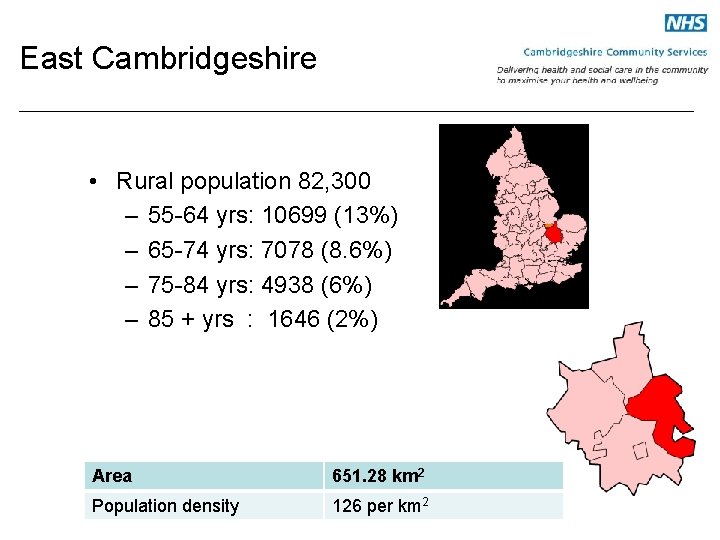
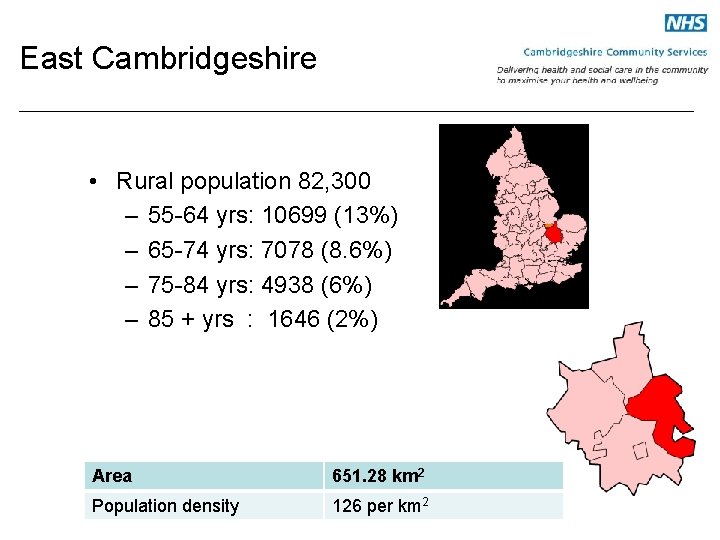
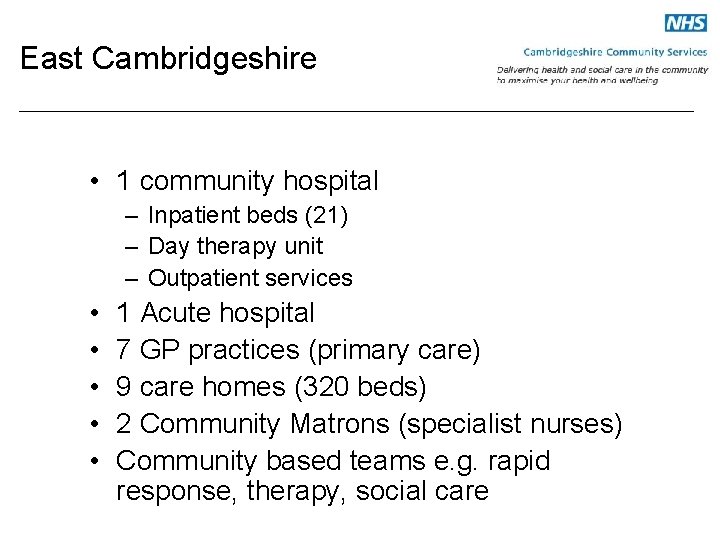
East Cambridgeshire • Rural population 82, 300 – 55 -64 yrs: 10699 (13%) – 65 -74 yrs: 7078 (8. 6%) – 75 -84 yrs: 4938 (6%) – 85 + yrs : 1646 (2%) Area 651. 28 km 2 Population density 126 per km 2
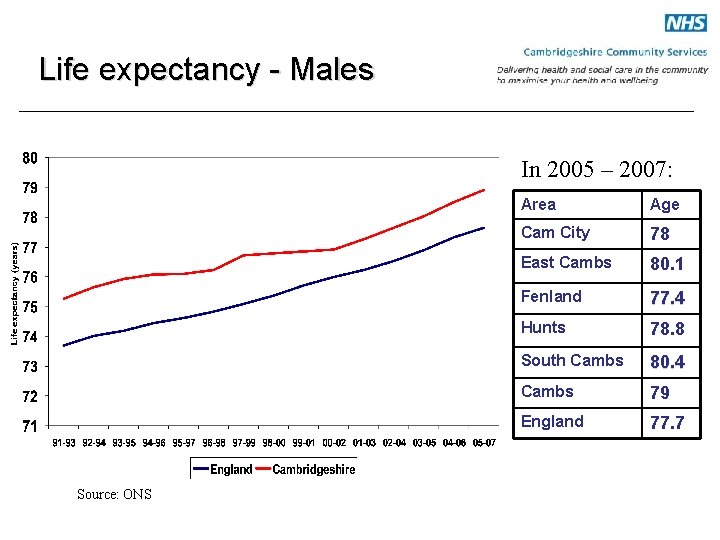
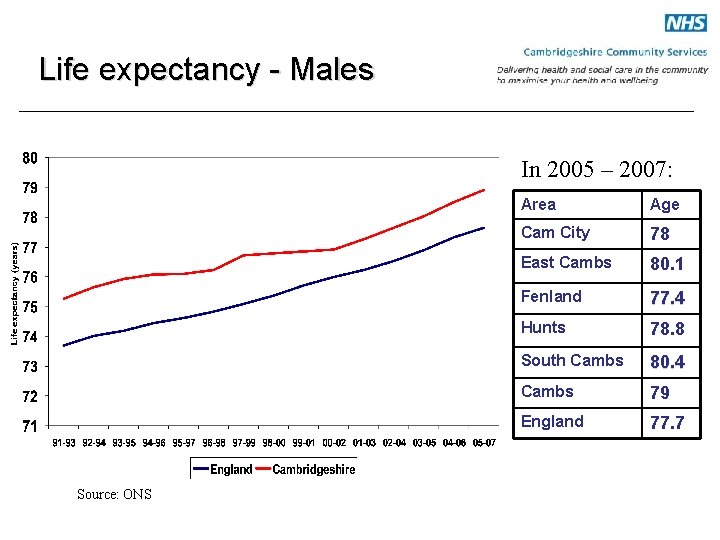
Life expectancy - Males In 2005 – 2007: Source: ONS Area Age Cam City 78 East Cambs 80. 1 Fenland 77. 4 Hunts 78. 8 South Cambs 80. 4 Cambs 79 England 77. 7
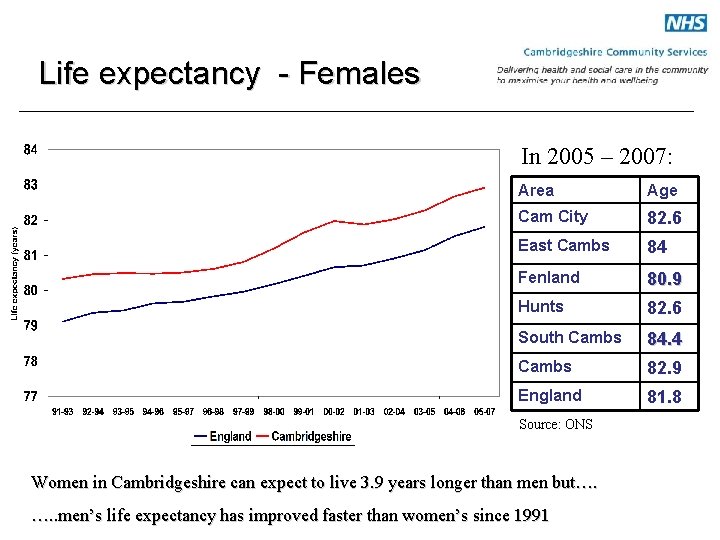
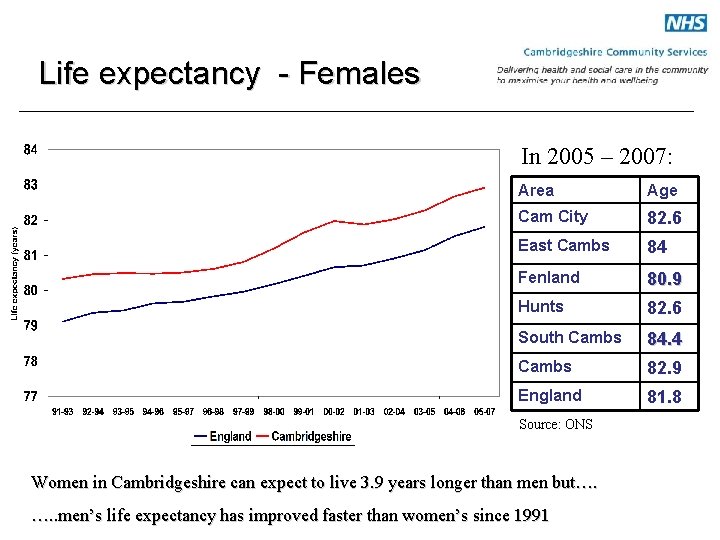
Life expectancy - Females In 2005 – 2007: Area Age Cam City 82. 6 East Cambs 84 Fenland 80. 9 Hunts 82. 6 South Cambs 84. 4 Cambs 82. 9 England 81. 8 Source: ONS Women in Cambridgeshire can expect to live 3. 9 years longer than men but…. …. . men’s life expectancy has improved faster than women’s since 1991
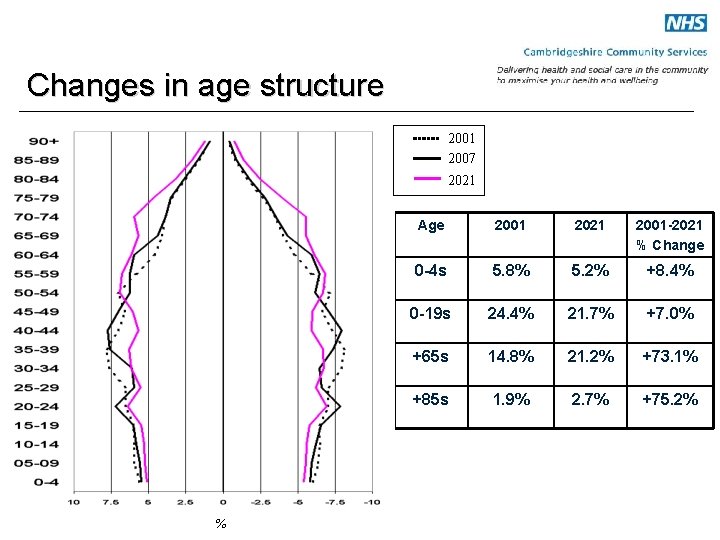
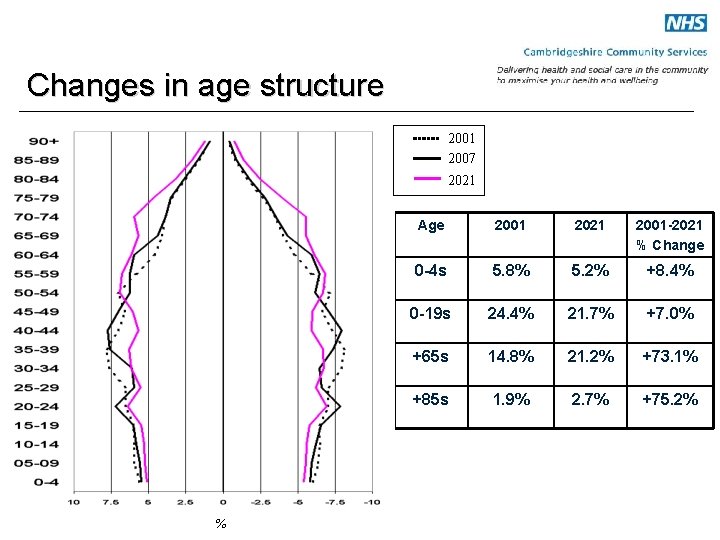
Changes in age structure 2001 2007 2021 % Age 2001 2021 2001 -2021 % Change 0 -4 s 5. 8% 5. 2% +8. 4% 0 -19 s 24. 4% 21. 7% +7. 0% +65 s 14. 8% 21. 2% +73. 1% +85 s 1. 9% 2. 7% +75. 2%
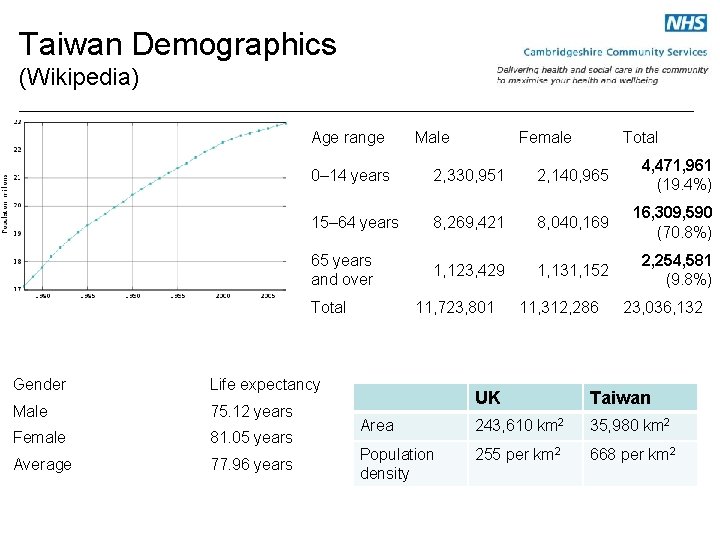
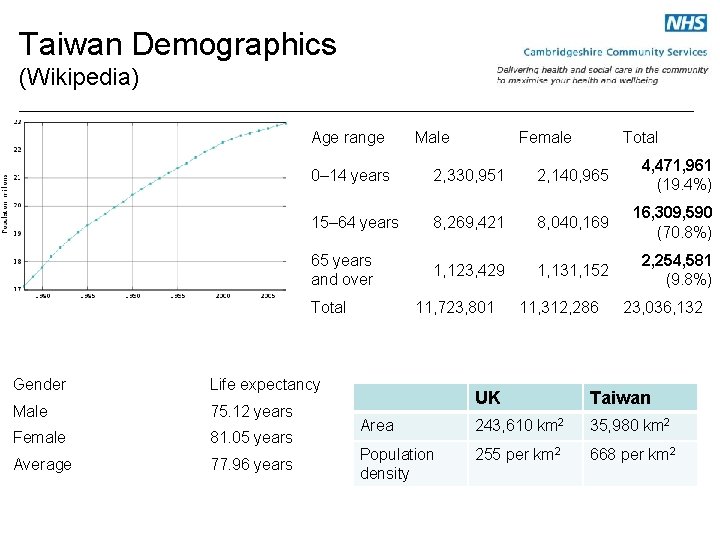
Taiwan Demographics (Wikipedia) Age range Male Female Total 0– 14 years 2, 330, 951 2, 140, 965 4, 471, 961 (19. 4%) 15– 64 years 8, 269, 421 8, 040, 169 16, 309, 590 (70. 8%) 65 years and over 1, 123, 429 1, 131, 152 2, 254, 581 (9. 8%) Total Gender Life expectancy Male 75. 12 years Female 81. 05 years Average 77. 96 years 11, 723, 801 11, 312, 286 23, 036, 132 UK Taiwan Area 243, 610 km 2 35, 980 km 2 Population density 255 per km 2 668 per km 2
East Cambridgeshire • 1 community hospital – Inpatient beds (21) – Day therapy unit – Outpatient services • • • 1 Acute hospital 7 GP practices (primary care) 9 care homes (320 beds) 2 Community Matrons (specialist nurses) Community based teams e. g. rapid response, therapy, social care
Community Services • Intermediate Care services – Community hospital – Day unit • Care Home reviews • Domiciliary Visits • Medical advice to local practitioners • End of life care

Marjorie Warren (1935) • West Middlesex Hospital London – 714 chronic sick “bedridden” “incurables” • Care process – Assessment – Team working – Environmental modifications • Outcome – 514 patients discharged home and ward shut
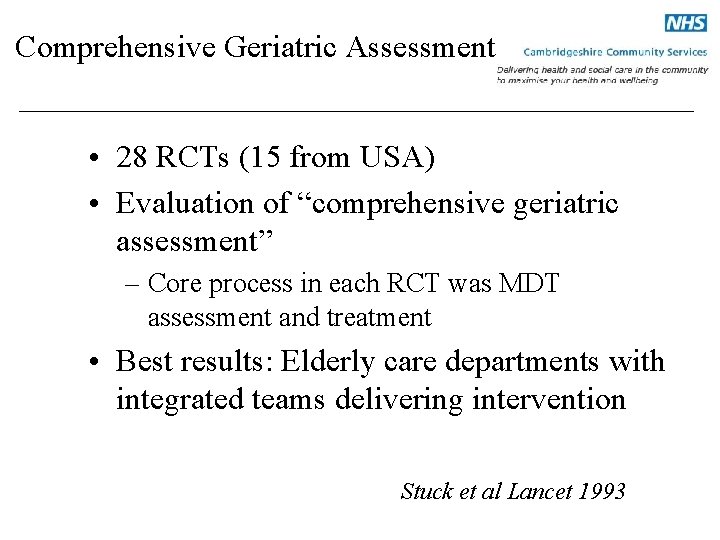
Comprehensive Geriatric Assessment • 28 RCTs (15 from USA) • Evaluation of “comprehensive geriatric assessment” – Core process in each RCT was MDT assessment and treatment • Best results: Elderly care departments with integrated teams delivering intervention Stuck et al Lancet 1993
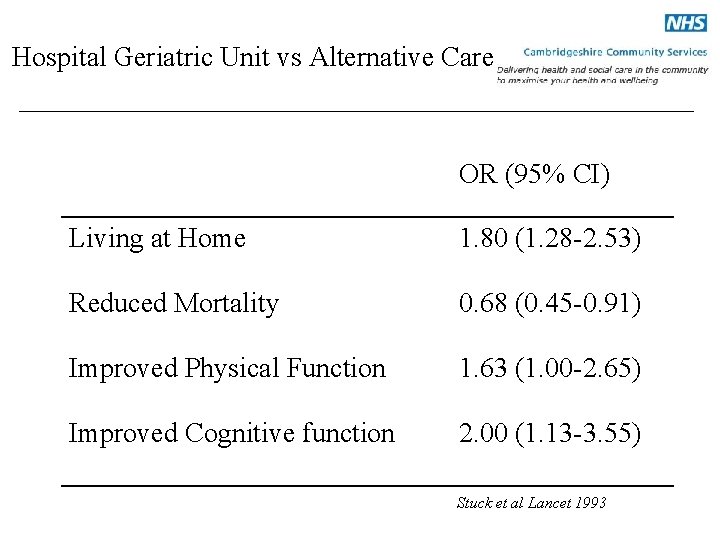
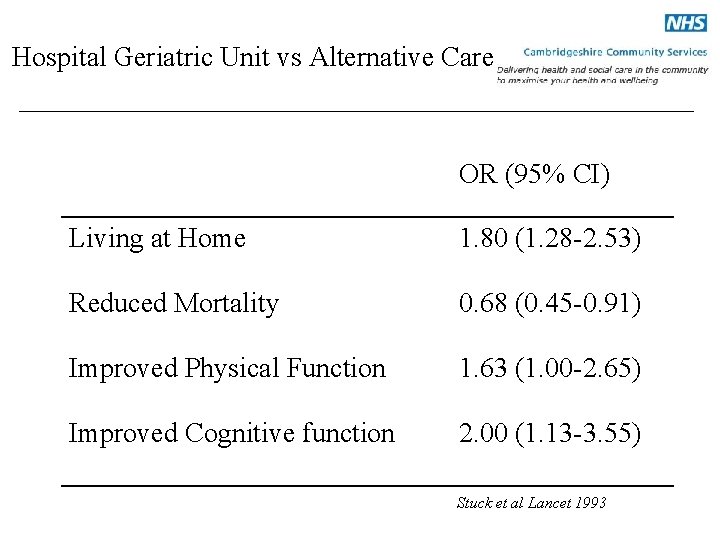
Hospital Geriatric Unit vs Alternative Care OR (95% CI) Living at Home 1. 80 (1. 28 -2. 53) Reduced Mortality 0. 68 (0. 45 -0. 91) Improved Physical Function 1. 63 (1. 00 -2. 65) Improved Cognitive function 2. 00 (1. 13 -3. 55) Stuck et al Lancet 1993
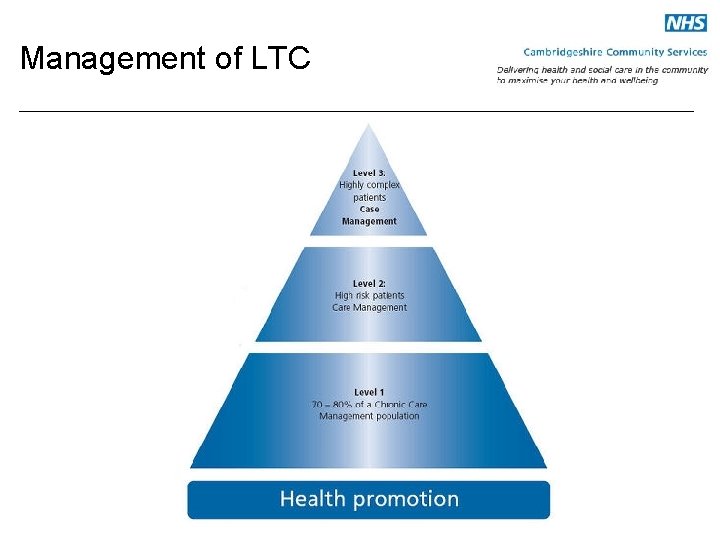
Long Term Conditions (LTC) (BGS 2005) • Geriatricians play key role • 3 level pyramid – Case management – Disease specific care management – Supported self care • Integrated model of care
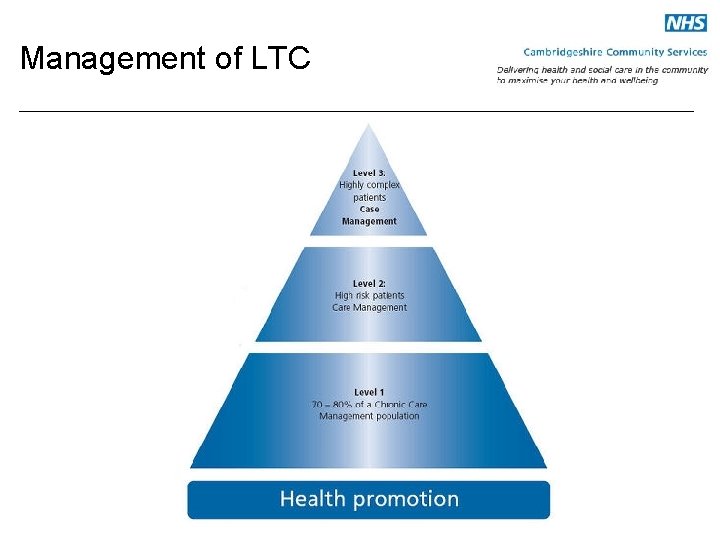
Management of LTC
Role of Community Geriatrician in management of LTC • • Complex multiple LTC Advice at times of transition Medical support for assessment process Leadership role in supporting community teams

Summary • CGA underpins community geriatric practice • Role will depend on local population • Core components – – Rehabilitation Care home medicine Supporting elderly in their own homes Palliative Care • Work at interface between primary and secondary care at times of transition • Integrated team working
Models of Care Intermediate Care (IC) • • • DH 2001 Integrated services Promote faster recovery from illness Prevent unnecessary hospital admissions Support timely discharge from hospital Maximise independent living

IC: Basic principles of service model • • Person centred care Robust assessment Partnership working Timely access to specialist services
Community Hospital IC Young et al JAGS 2007 • Design: RCT • Setting: 7 community and 5 general hospitals • Participants: 490 patients needing rehabilitation post acute admission • Intervention: MDT care in community hospital • Measurement: NEADL, BI, anxiety and depression score, mortality, discharge destination
Community Hospital IC (O’Reilly et al Age and Ageing 2008) • Results Primary outcome: CH group had significantly better NEADL score at 6/12 compared to general hospital group (p=0. 03) Secondary Outcome: No difference in mortality, patient and carer satisfaction, institutional rates, anxiety and depression scores Cost effectiveness similar in CH and GH
Community Hospital IC Garasen et al BMC Public Health 2007 • Design: RCT • Setting: Community hospital vs general hospital IC • Participants: 142 patients > 60 yrs • Intervention: MDT in community hospital setting • Measurements: hospital admission rates, ADL, mortality, institutional care
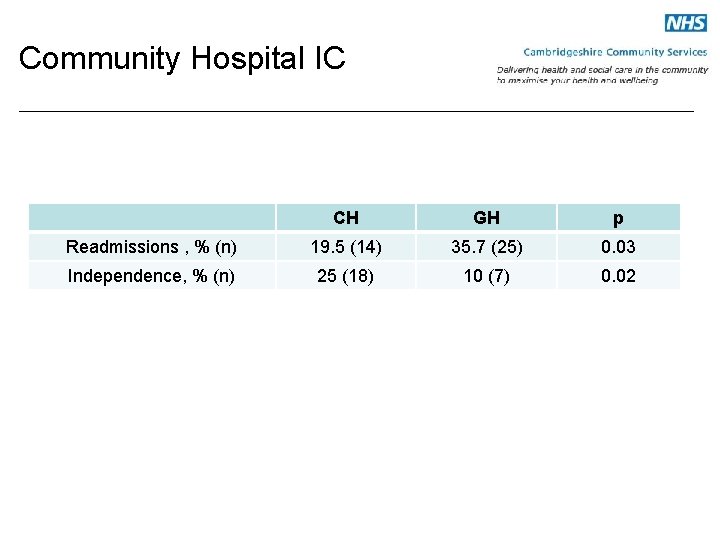
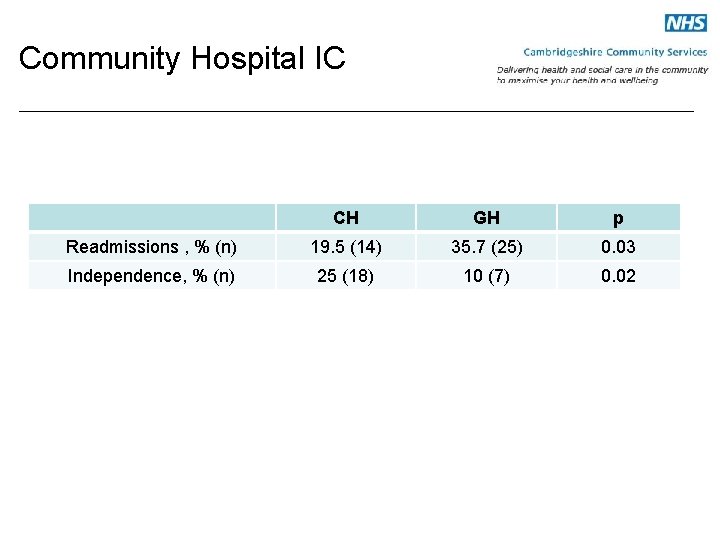
Community Hospital IC CH GH p Readmissions , % (n) 19. 5 (14) 35. 7 (25) 0. 03 Independence, % (n) 25 (18) 10 (7) 0. 02
Day Unit IC Cochrane review Foster et al 2008 • 13 RCTs with 3007 participants – 5 RCTs Day hospital vs elderly care – 5 RCTs Day hospital vs domiciliary care – 3 RCTs Day Hospital vs no elderly care • Conclusions – Day unit care more effective than no intervention – No clear advantage over other models of elderly care – No evidence to support admission avoidance

Hospital at Home IC Cochrane review Shepperd et al 2009 • 26 RCTs with n=3967 participants • Compared early discharge schemes at home with in patient hospital care – Readmission rates were significantly higher for elderly with multiple LTC (n=705) – Increased patient satisfaction for early discharge schemes – No evidence for cost savings – Elderly with LTC and stroke patients were less likely to be in residential care at 6/12 (7 trials)

Care Home IC Fleming et al Age and Ageing 2004 • RCT n= 165 frail hospitalised elderly • Intervention: IC in care home vs usual care • Outcome: institutionalisation, Barthel index, mortality. • Results: No significant differences between intervention and control group
IC Conclusions • No clear evidence base for IC service models based on current evidence • More research is needed • Best practice needs to be evaluated

Care Home Medicine • Care Home – 24 hour access to care – Spectrum of care • Residential care • Nursing home • Dementia units • Cost of care – 75% of places funded by government – Range of cost (£ 300 - £ 1000)
National census of care home residents in UK • N= 15, 483 (25% residential) in 244 care homes • 90% admitted due to medical morbidity or disability • > 50% had dementia, CVA or PD • 76% needed assistance with mobility • 71% were incontinent • 78% had mental impairment Bowman et al (2004) Age and Ageing 33: 561
The Health and Care of Older People in Care Homes • Interdisciplinary approach to assessment, care planning and care delivery • Development of the nurse as the lead practitioner • Service delivery needs to engage general and specialist aspects of medical practice • Practitioners should have appropriate education and training Report of a Joint Working Party. RCP, RCN, BGS (2000)
Resource Implications • • Gerontological nurse specialist Specialist GP service Specialist pharmacist Increase input from professions allied to medicine • Regular MDT consultant sessions and visits to homes • Improve care planning • Develop teaching nursing homes

Care home medicine in the UK in from the cold • Hallmark of caring society is how we care for weakest members • Complex patients • National guidelines (2000) • Finding local model that meets criteria Donald IP et al Age and Ageing, 2008.
Integrated primary and secondary care model in Manchester UK • 9 homes n=400 • Care home team – Advanced nurse practitioner – GP – Consultant community geriatrician • Anticipatory care • End of life planning • Audit (unpublished) – 35% decrease in emergency admissions – 68% reduction in emergency bed days – 56% decrease in hospital LOS for those admitted to hospital
Domiciliary Visit • 3 components – Advice on treatment and diagnosis – Patient unable to attend hospital – GP present • 60% of my outpatient work comprises DVs • (2/3 of these are in care homes) • Evidence base (Crome et al JRSoc Med 2000) – Valued by GPs – Variable practice – No evidence to show that it decreases hospital admission rates

Conclusions • Role of a Community Geriatrician – LTC in the community • Rehabilitation • End of life care • Team working and integration with other services essential • Local model will depend on population and links with acute units
Conclusions • Evidence base underpinning practice is the Comprehensive Geriatric Assessment • Evidence base for service models and best practice – Intermediate care
Conclusions • More research needed to evaluate best practice • Holisitic care and encompasses all aspects of geriatric medicine • Future of geriatric medicine is in the community
 Community geriatrics
Community geriatrics Giant of geriatric
Giant of geriatric Dr john ward geriatrician newcastle
Dr john ward geriatrician newcastle Simpson's diversity index equation
Simpson's diversity index equation Chapter 41 assisting in geriatrics
Chapter 41 assisting in geriatrics Pearson
Pearson Choosing wisely geriatrics
Choosing wisely geriatrics Einstein geriatrics
Einstein geriatrics California council on gerontology and geriatrics
California council on gerontology and geriatrics Einstein geriatrics
Einstein geriatrics A department store decides to use secret shoppers
A department store decides to use secret shoppers Internet marketing consultant job description
Internet marketing consultant job description New consultant in casualty
New consultant in casualty Nous hospital consultant
Nous hospital consultant Knowledge management consultant
Knowledge management consultant New consultant training
New consultant training Mrs rajlaxmi is working as the human resource consultant
Mrs rajlaxmi is working as the human resource consultant Stuart minty camden planning consultant
Stuart minty camden planning consultant Advanced nutraceuticals
Advanced nutraceuticals New consultant training
New consultant training Script for recruiter cold call
Script for recruiter cold call Sustainable tourism consultant jobs
Sustainable tourism consultant jobs Petrophysics
Petrophysics Threat modelling consultant
Threat modelling consultant Pearson vue pcnse
Pearson vue pcnse Engineers pi is 3
Engineers pi is 3 Judith james educational consultant
Judith james educational consultant Multiple consultant report
Multiple consultant report Psychiatrist leicester
Psychiatrist leicester Test consultant capgemini
Test consultant capgemini Dan rogers it consultant
Dan rogers it consultant Verizon business solutions consultant
Verizon business solutions consultant Associate consultant in capgemini
Associate consultant in capgemini Dr ian smith injury management consultant
Dr ian smith injury management consultant Family history consultant training
Family history consultant training Jojy mathew
Jojy mathew Expert in consultant liaison psychiatrist
Expert in consultant liaison psychiatrist Ellucian banner upgrade consultant
Ellucian banner upgrade consultant Stuart minty planning consultant
Stuart minty planning consultant Rcem consultant sign off
Rcem consultant sign off