CLINICAL AUDIT FOR AMS Husni Hussain FMS KK


- Slides: 33
CLINICAL AUDIT FOR AMS Husni Hussain FMS KK Salak
Elements of an effective AMS program Prescriber Clinical pharmacist with ID training Collaboration with other unit Clinical microbiology Infection control Epidemiologists Information system support Support from admin
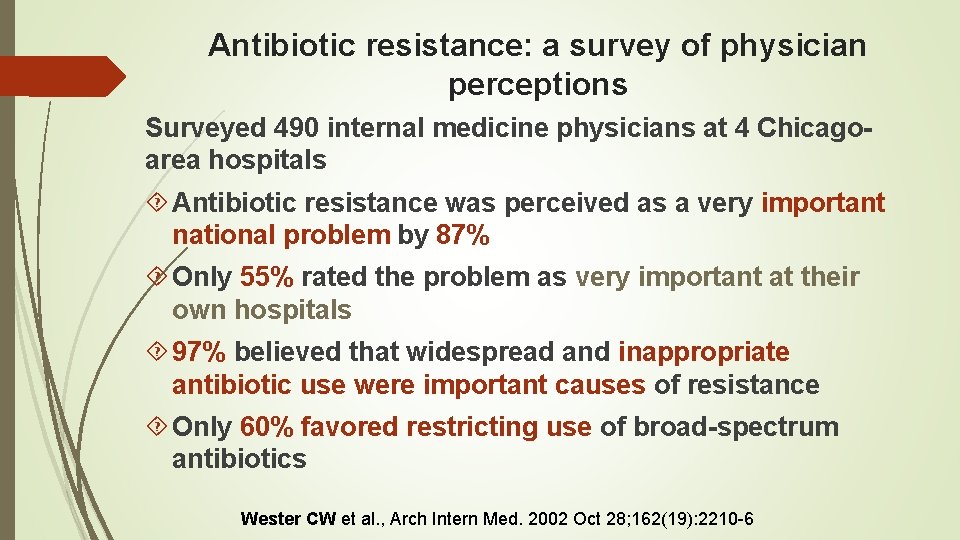
Antibiotic resistance: a survey of physician perceptions Surveyed 490 internal medicine physicians at 4 Chicagoarea hospitals Antibiotic resistance was perceived as a very important national problem by 87% Only 55% rated the problem as very important at their own hospitals 97% believed that widespread and inappropriate antibiotic use were important causes of resistance Only 60% favored restricting use of broad-spectrum antibiotics Wester CW et al. , Arch Intern Med. 2002 Oct 28; 162(19): 2210 -6
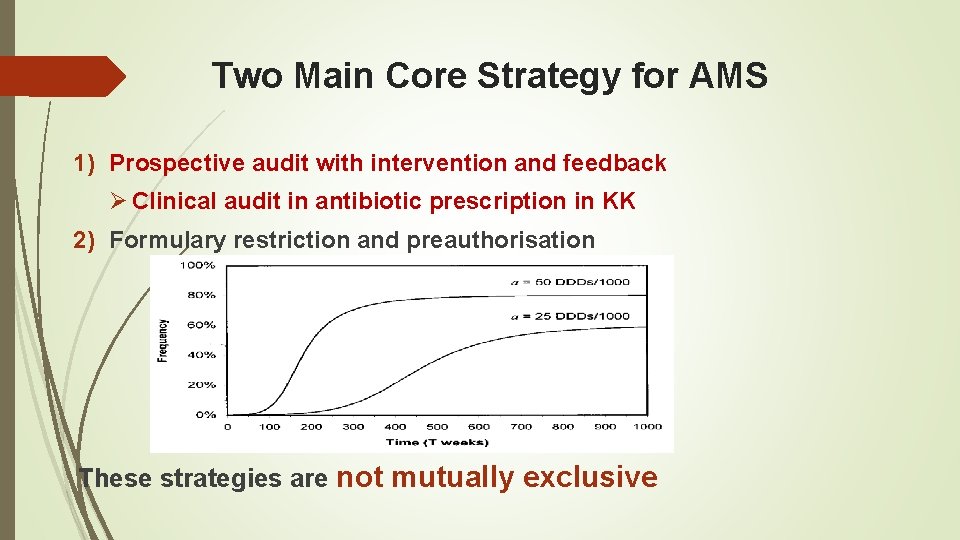
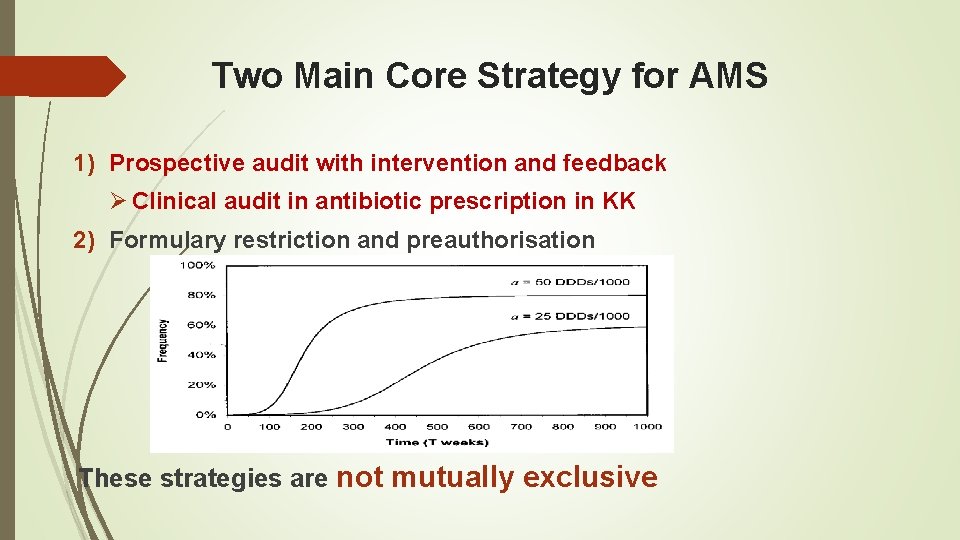
Two Main Core Strategy for AMS 1) Prospective audit with intervention and feedback Ø Clinical audit in antibiotic prescription in KK 2) Formulary restriction and preauthorisation These strategies are not mutually exclusive
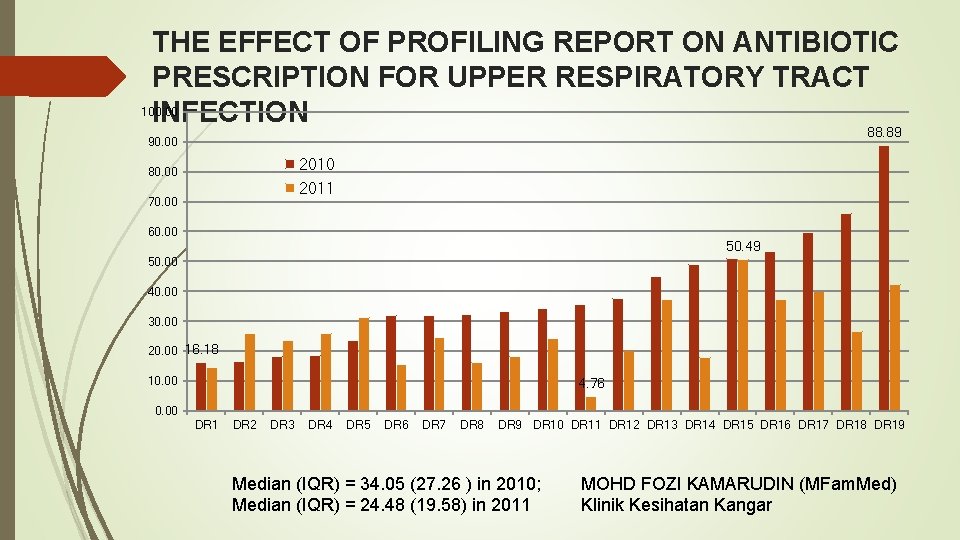
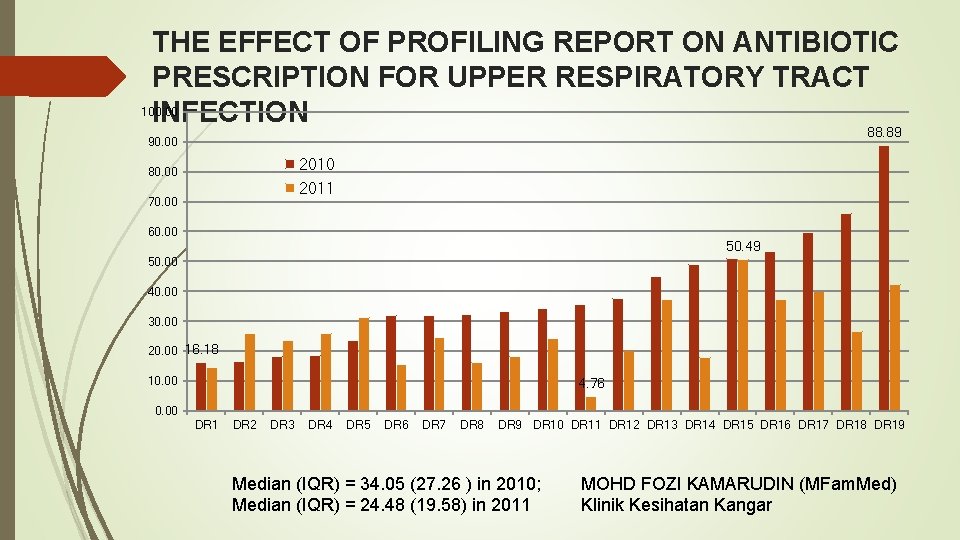
THE EFFECT OF PROFILING REPORT ON ANTIBIOTIC PRESCRIPTION FOR UPPER RESPIRATORY TRACT 100. 00 INFECTION 88. 89 90. 00 2010 80. 00 2011 70. 00 60. 00 50. 49 50. 00 40. 00 30. 00 20. 00 16. 18 10. 00 4. 76 0. 00 DR 1 DR 2 DR 3 DR 4 DR 5 DR 6 DR 7 DR 8 DR 9 DR 10 DR 11 DR 12 DR 13 DR 14 DR 15 DR 16 DR 17 DR 18 DR 19 Median (IQR) = 34. 05 (27. 26 ) in 2010; Median (IQR) = 24. 48 (19. 58) in 2011 MOHD FOZI KAMARUDIN (MFam. Med) Klinik Kesihatan Kangar
Other Strategies for AMS Guideline and clinical pathways Education Antimicrobial order forms Streaming / de-escalation therapy Dose optimisation Parenteral to oral conversion Profiling in antibiotic prescription eg; Point Prevalence survey
Outcome Measurement Cost of antimicrobial used Defined daily dose per patient-day Antimicrobial acquisition cost per patient-day Degree of AMR (antibiogram) Number of adverse drug effects Rate of C. difficile infection Performance with relation to guideline or clinical pathway Clinical audit scoring Can be individualised as per institutional needs
Introduction: AMS clinical audit Clinical audit; tool that looks into details in clinical practice by individual health care provider that prescribed antibiotic. This can be further used for quality improvement cycle that involves assessment of the effectiveness of clinical services against agreed standards of best practice.
Stage of implementation 1. Stage 1: Preparation 2. Done annually or as needed based on ØAlert by the pharmacist ØIncidental reporting etc 3. Identify available resources, e. g. audit team. 4. Existing guidelines defining desired standards as reference, such as NAG and clinical pathways.
Stage of implementation Stage 1 cont’d Define criteria: All antibiotic prescription by any particular health care providers for past 1 month will be randomly selected with minimum of 30 records. KK that interested to do profiling of individual prescriber may use the same audit format with minimum of 5 randomly selected records to justify interpretation.
Stage of implementation STAGE 2 - MEASURING LEVEL OF PERFORMANCE: Data collection maybe from computerised EMR or manual collection. Data entered in excel format with embedded formulas for auto calculations. Audited clinical record will be scored based on criteria of best practice with score of 80% and above would be consider as appropriate. Analyse the data collected: Compare actual performance with the set standard based on previous scoring. Discuss how well the standards were met. If the standards were not met, note the reasons for this.
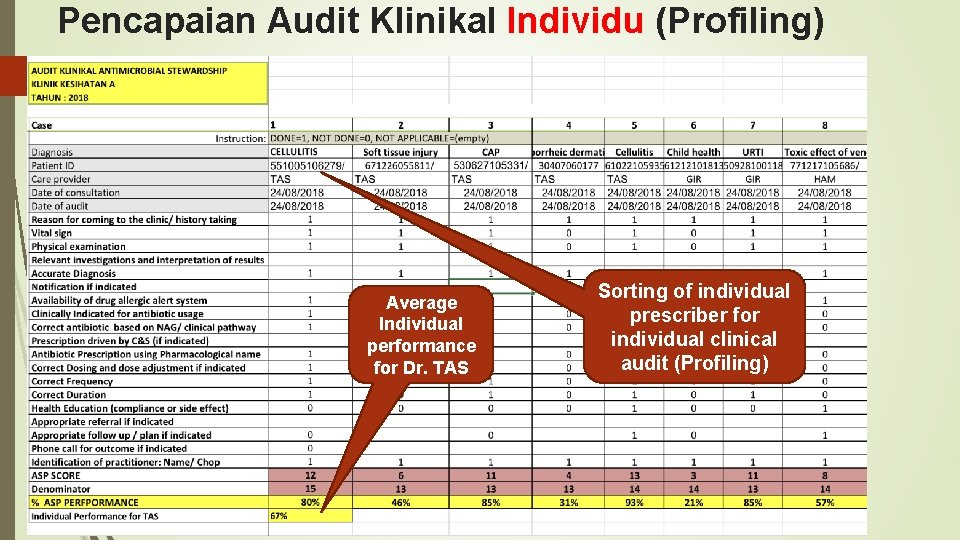
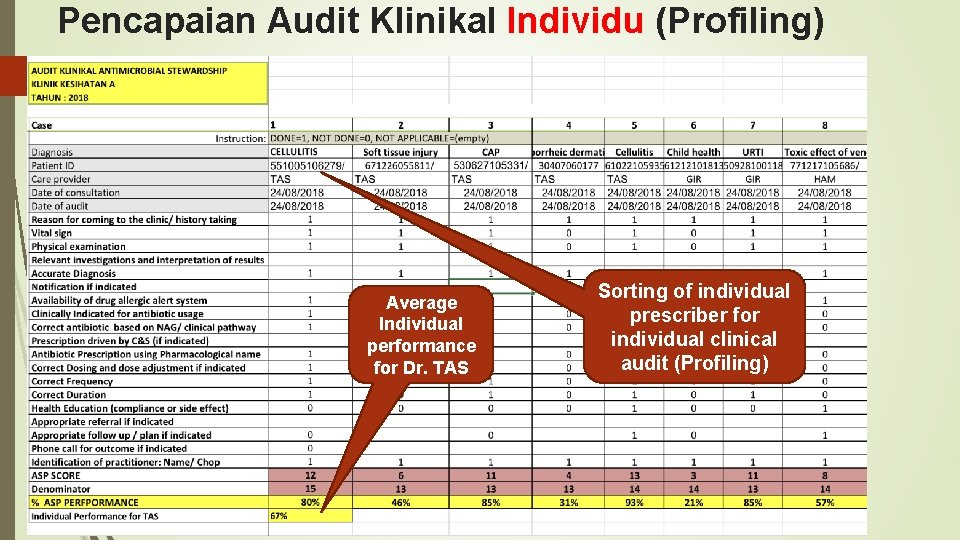
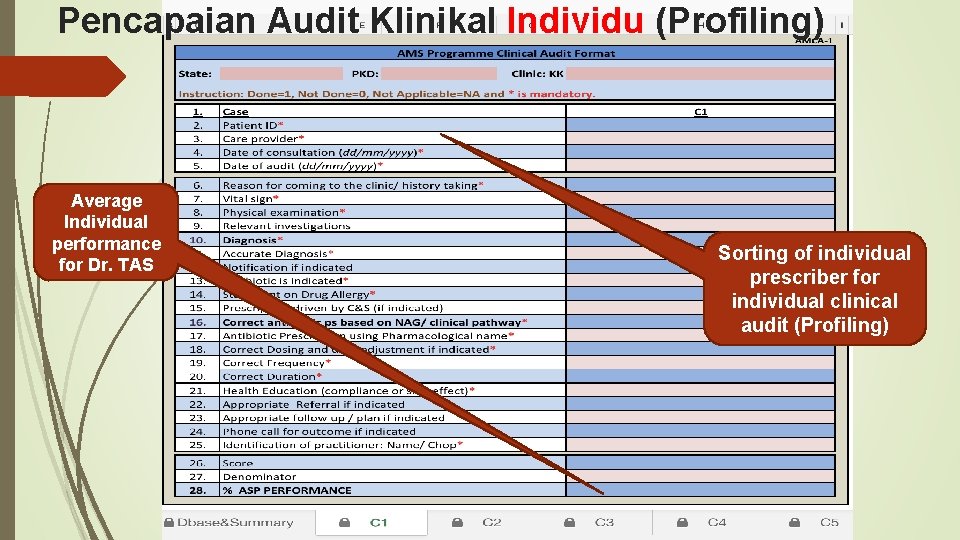
Pencapaian Audit Klinikal Individu (Profiling) Average Individual performance for Dr. TAS Sorting of individual prescriber for individual clinical audit (Profiling)
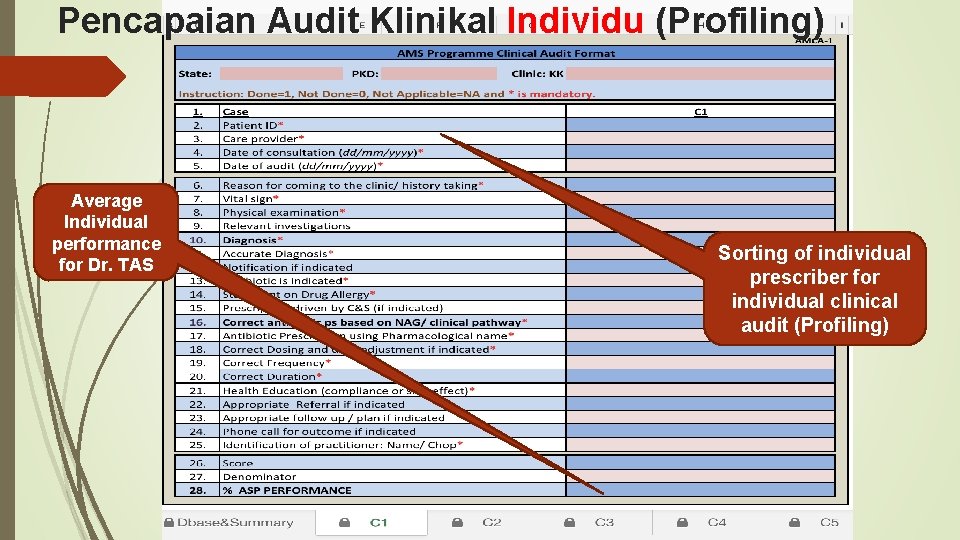
Pencapaian Audit Klinikal Individu (Profiling) Average Individual performance for Dr. TAS Sorting of individual prescriber for individual clinical audit (Profiling)
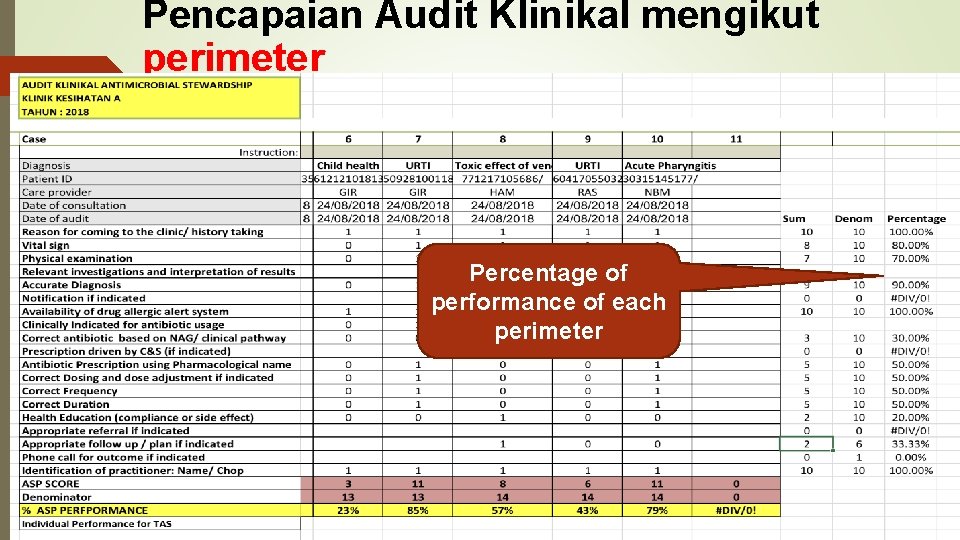
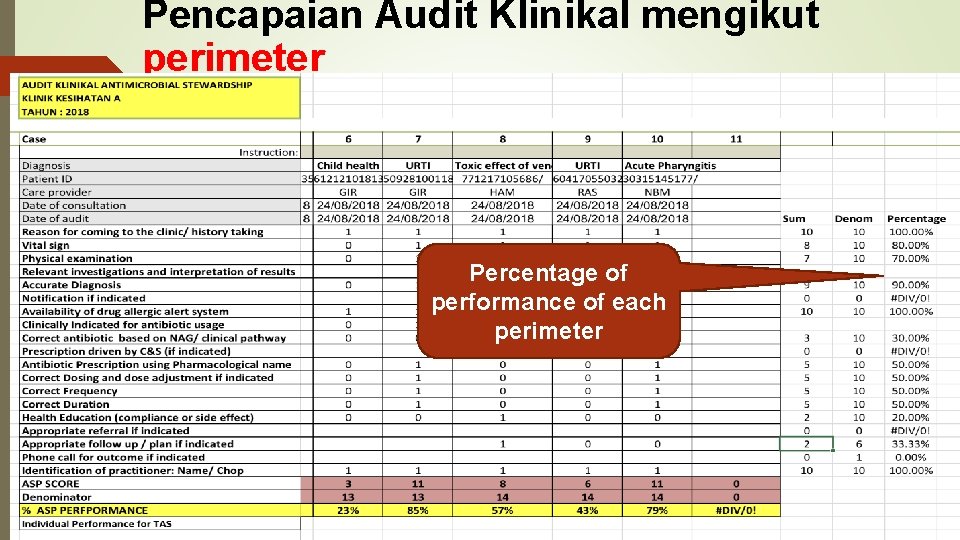
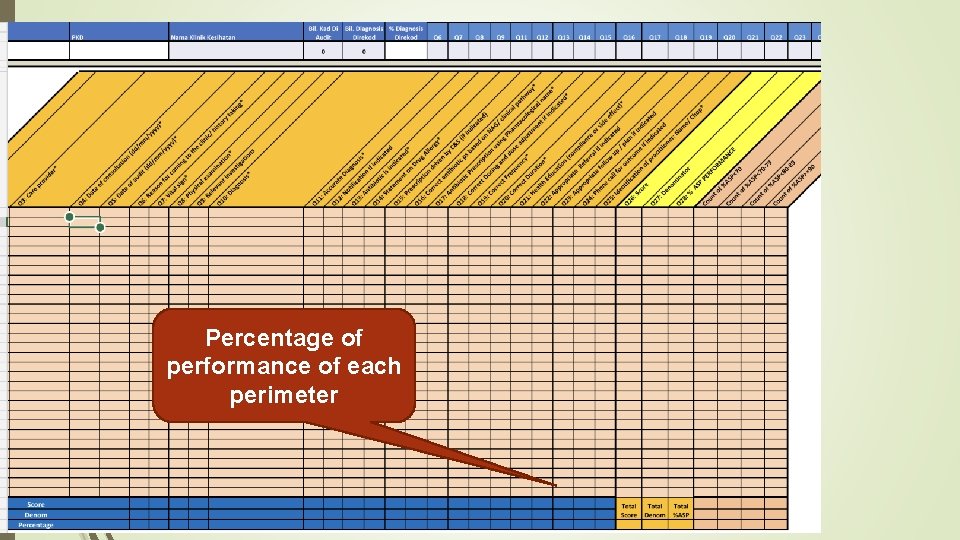
Pencapaian Audit Klinikal mengikut perimeter Percentage of performance of each perimeter
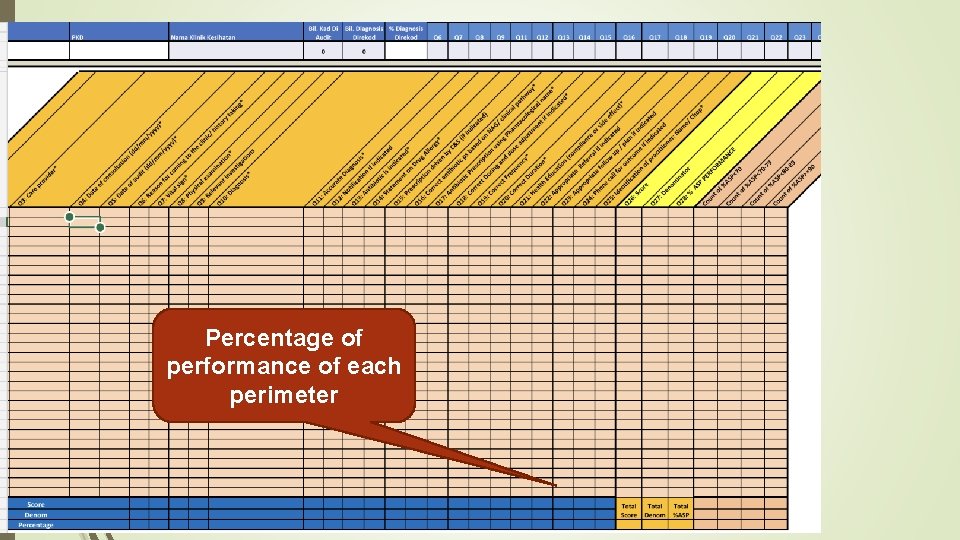
Percentage of performance of each perimeter
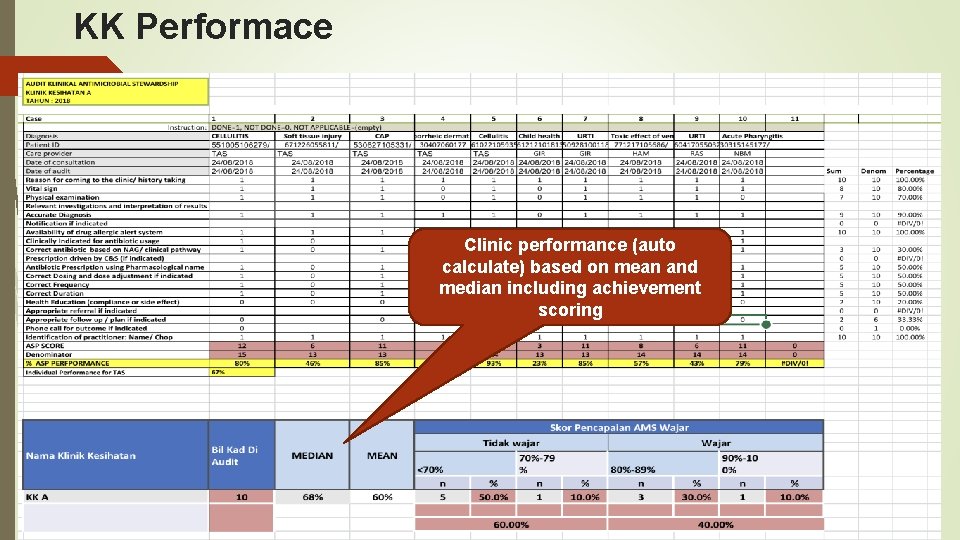
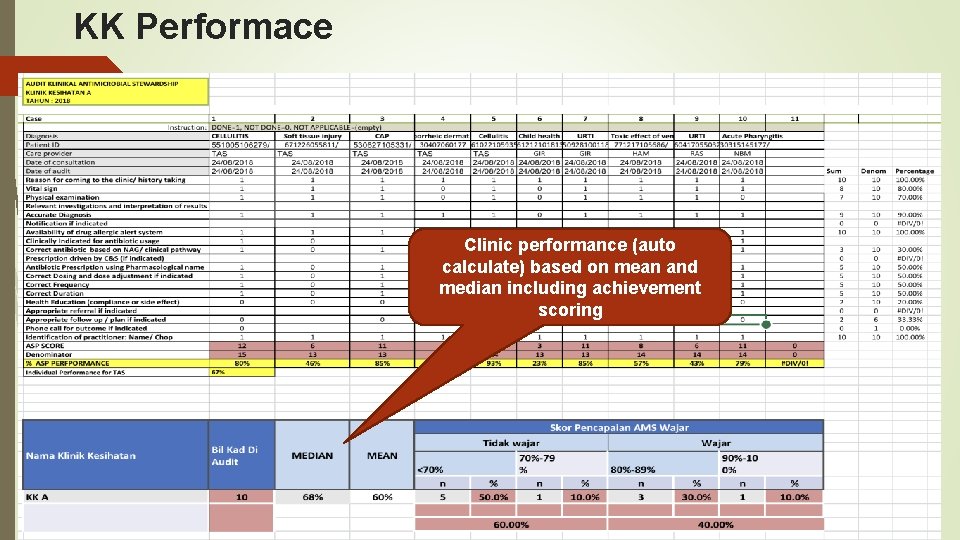
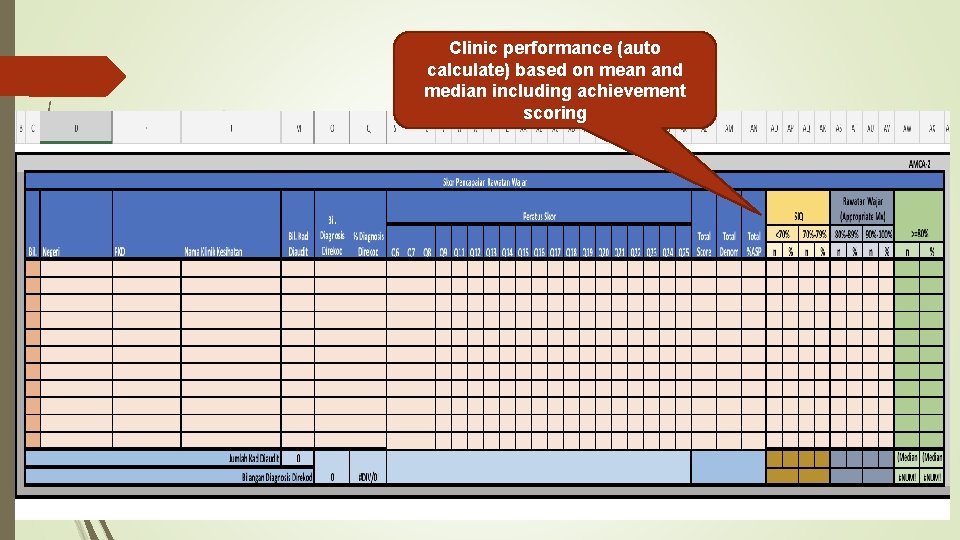
KK Performace Clinic performance (auto calculate) based on mean and median including achievement scoring
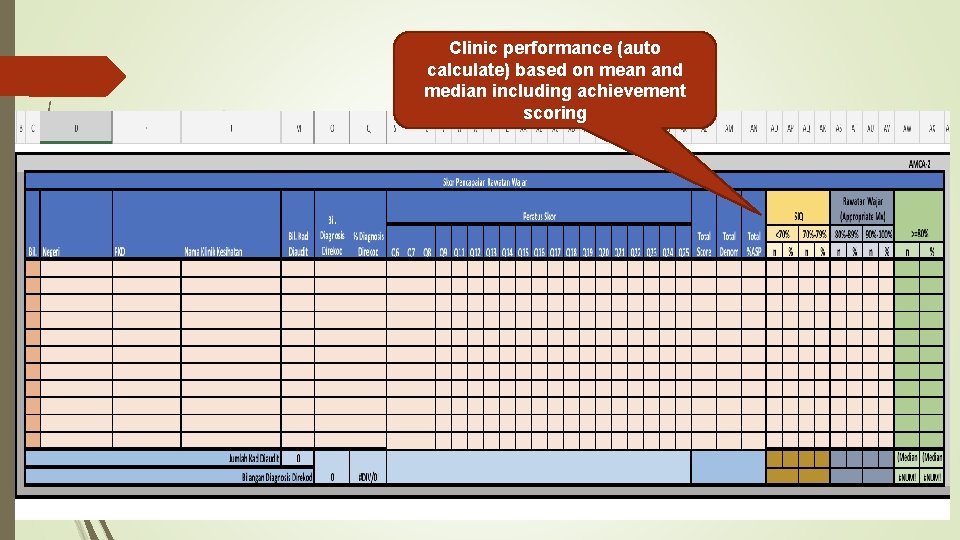
Clinic performance (auto calculate) based on mean and median including achievement scoring
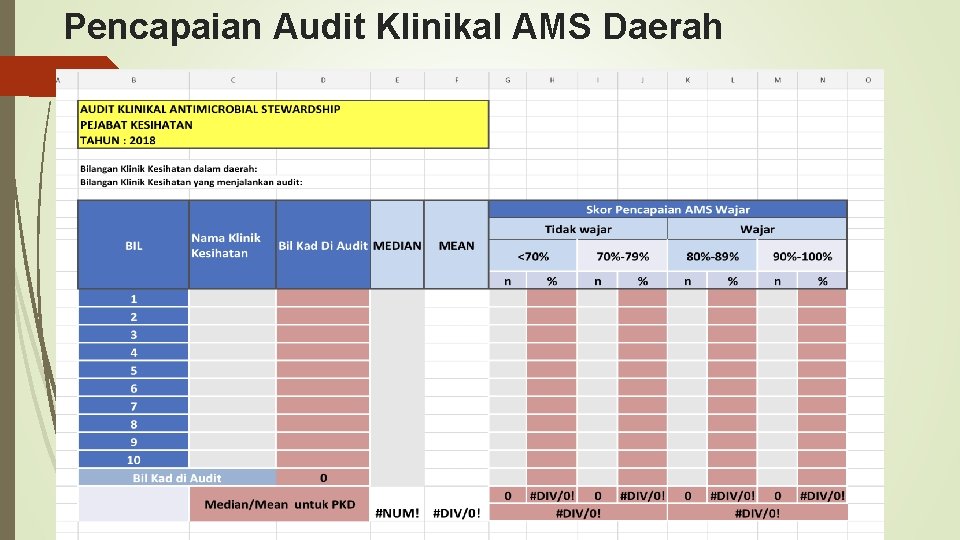
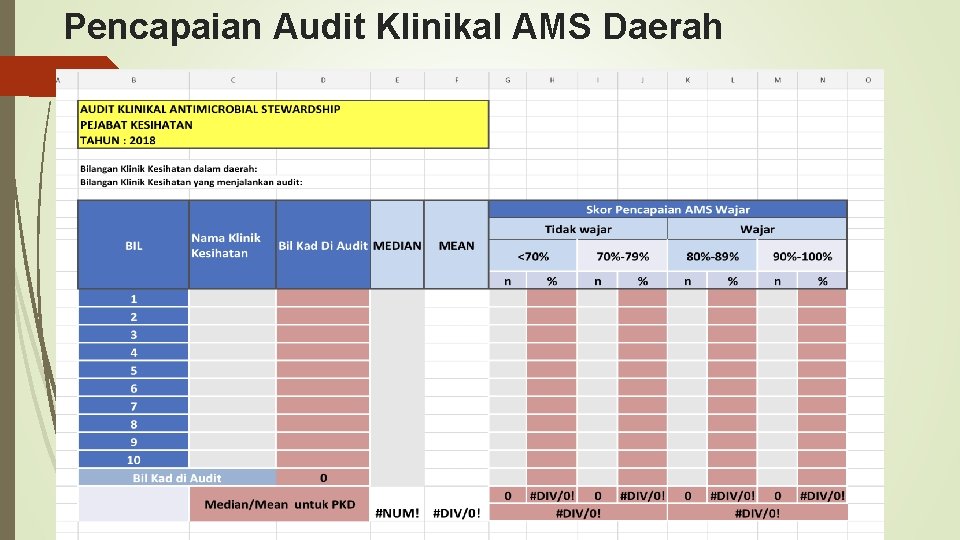
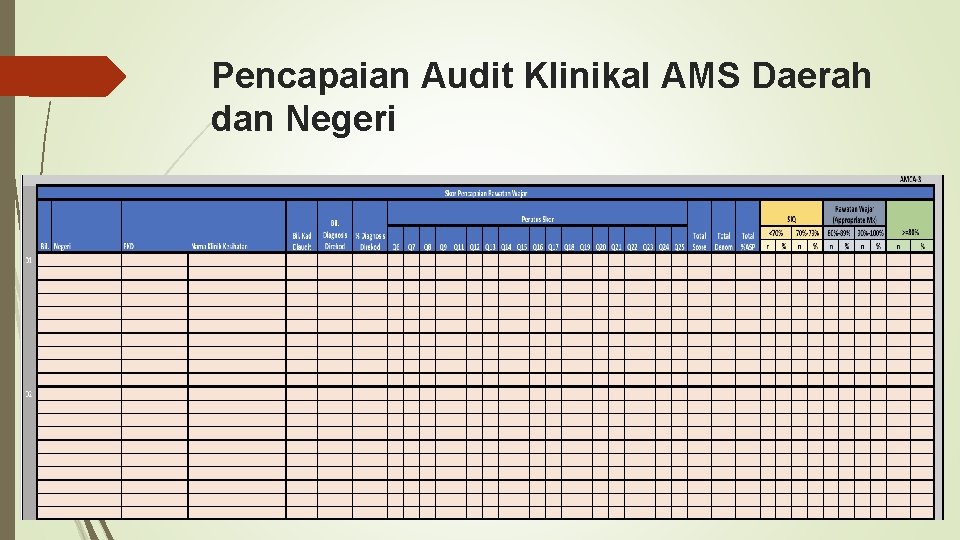
Pencapaian Audit Klinikal AMS Daerah
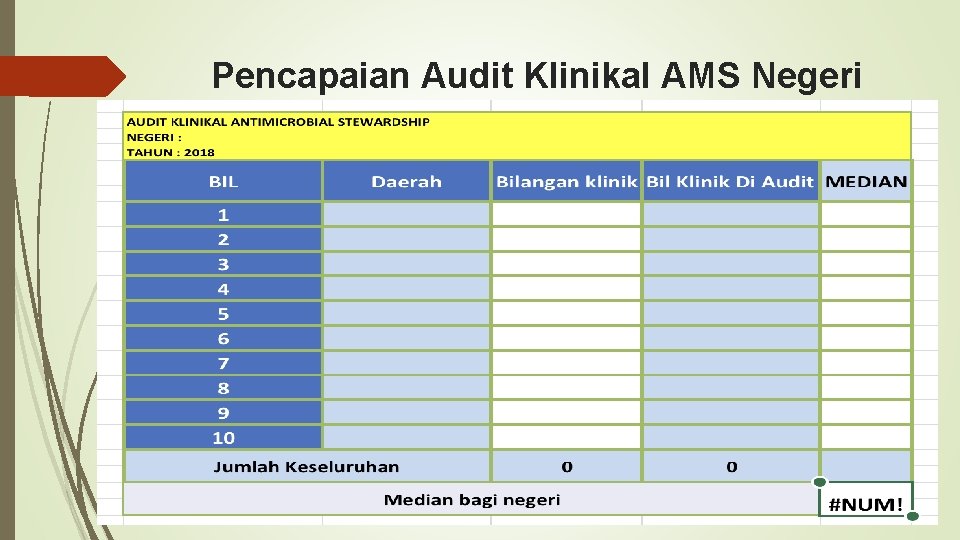
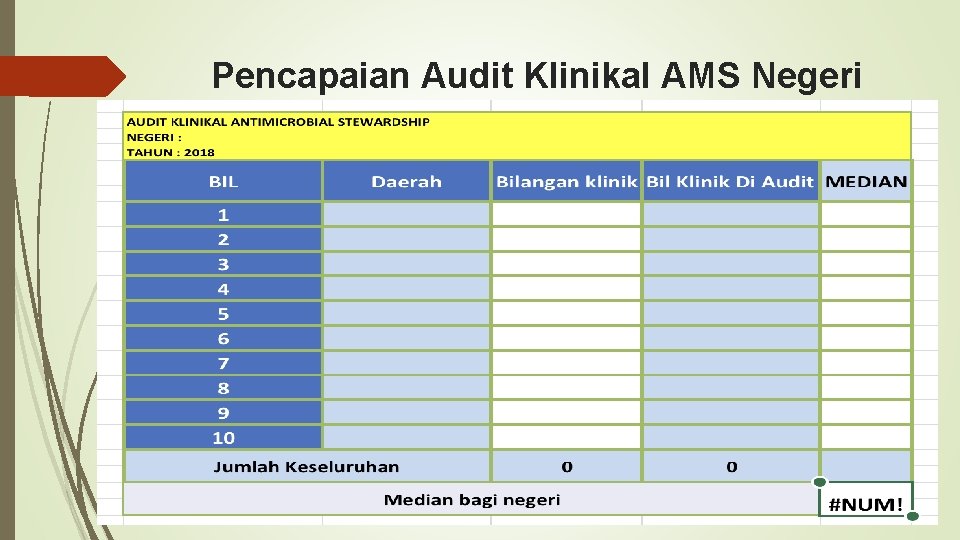
Pencapaian Audit Klinikal AMS Negeri
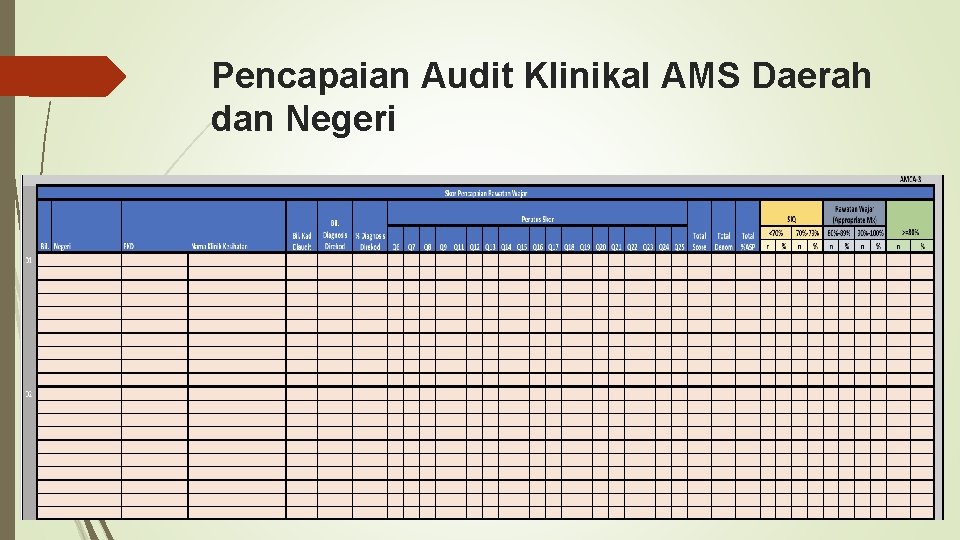
Pencapaian Audit Klinikal AMS Daerah dan Negeri
Stage of implementation STAGE 3 – MAKING IMPROVEMENTS: Present the results and discuss them with the relevant teams in the organisation. The results should be used to develop an action plan, specifying what needs to be done, how it will be done, who is going to do it and by when.
Stage of implementation STAGE 4 - MAINTAINING IMPROVEMENTS: This follows up the previous stages of the audit, to determine whether the actions taken have been effective, or whether further improvements are needed It involves repeating the audit (i. e. targets, results, discussion); hence the terms “audit cycle”.
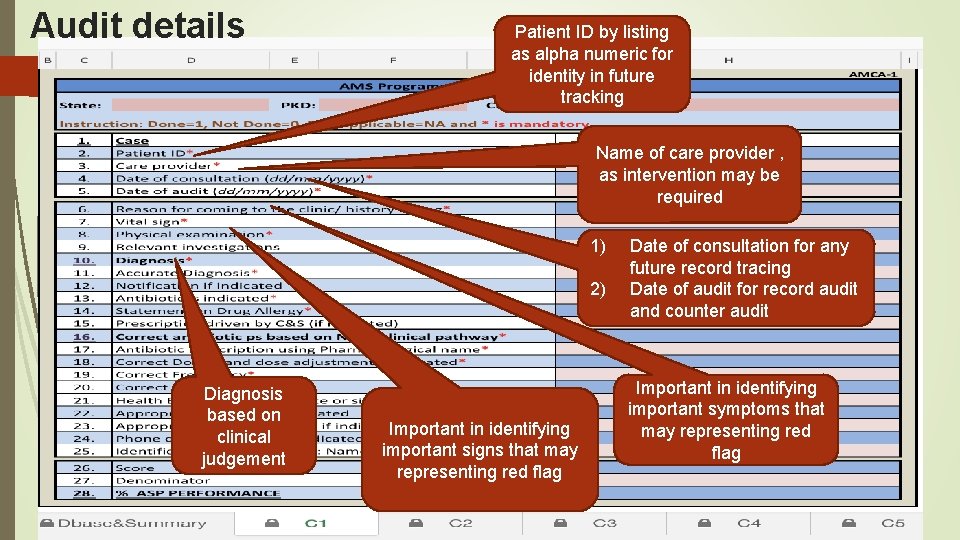
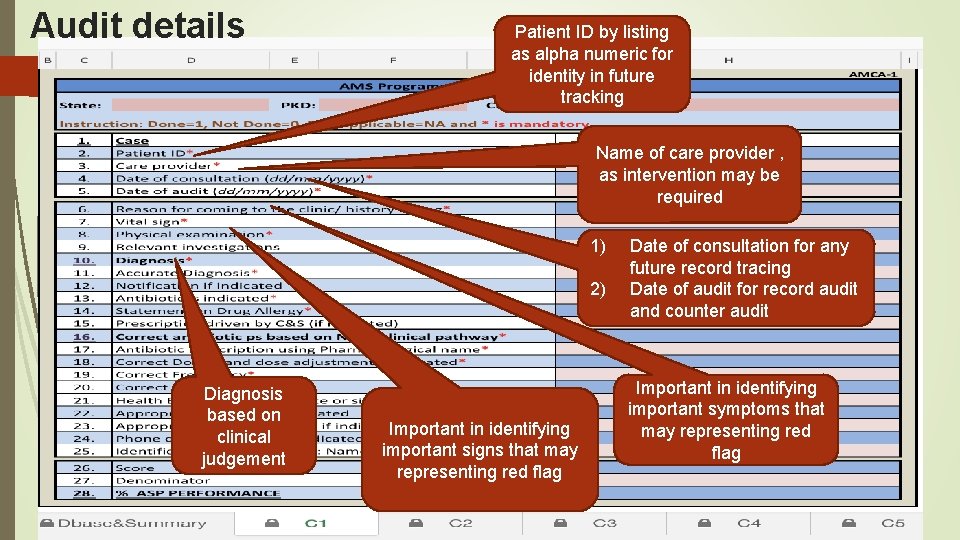
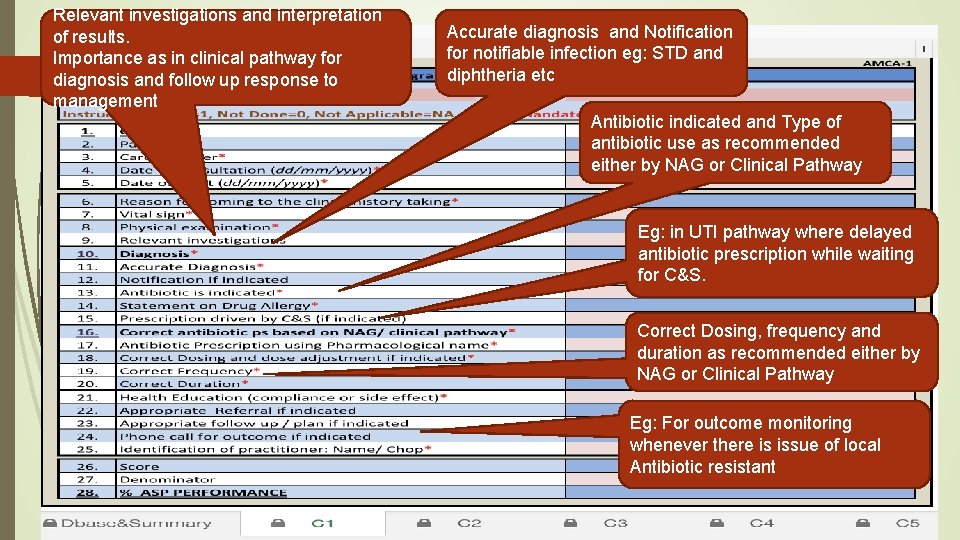
Audit details Patient ID by listing as alpha numeric for identity in future tracking Name of care provider , as intervention may be required 1) 2) Diagnosis based on clinical judgement Important in identifying important signs that may representing red flag Date of consultation for any future record tracing Date of audit for record audit and counter audit Important in identifying important symptoms that may representing red flag
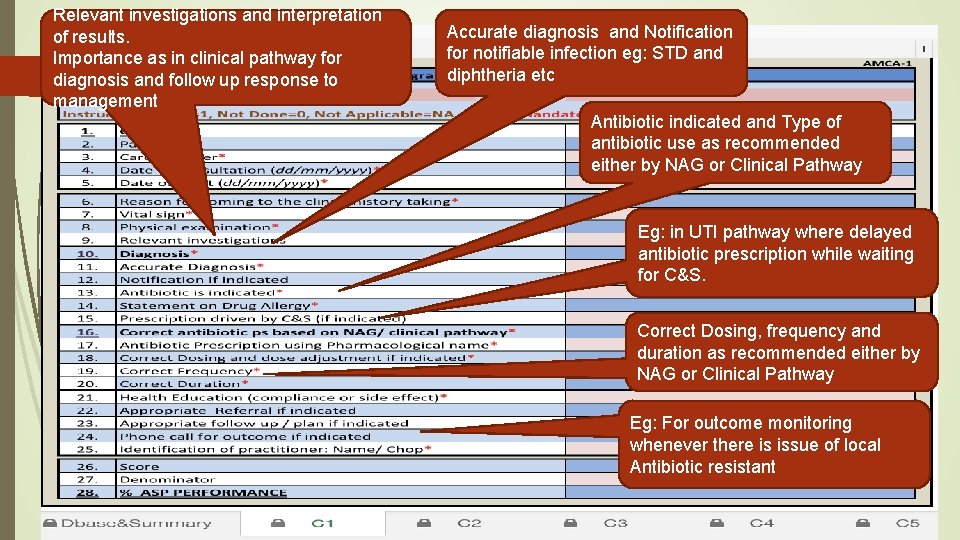
Relevant investigations and interpretation of results. Importance as in clinical pathway for diagnosis and follow up response to management Audit details Accurate diagnosis and Notification for notifiable infection eg: STD and diphtheria etc Antibiotic indicated and Type of antibiotic use as recommended either by NAG or Clinical Pathway Eg: in UTI pathway where delayed antibiotic prescription while waiting for C&S. Correct Dosing, frequency and duration as recommended either by NAG or Clinical Pathway Eg: For outcome monitoring whenever there is issue of local Antibiotic resistant
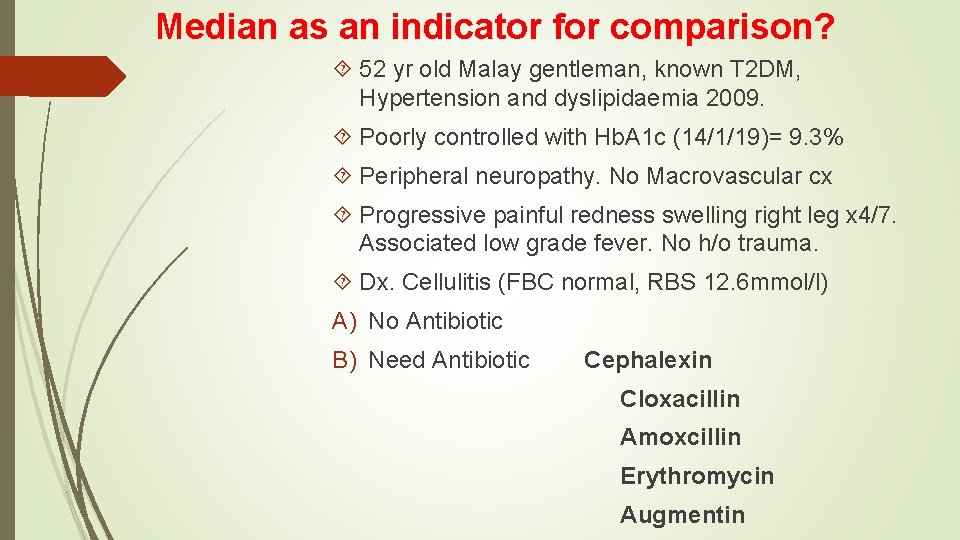
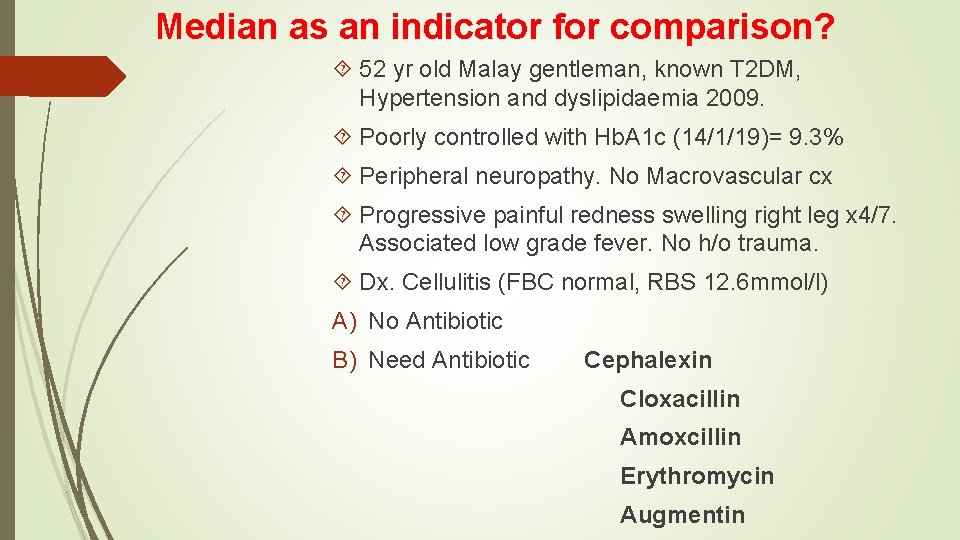
Median as an indicator for comparison? 52 yr old Malay gentleman, known T 2 DM, Hypertension and dyslipidaemia 2009. Poorly controlled with Hb. A 1 c (14/1/19)= 9. 3% Peripheral neuropathy. No Macrovascular cx Progressive painful redness swelling right leg x 4/7. Associated low grade fever. No h/o trauma. Dx. Cellulitis (FBC normal, RBS 12. 6 mmol/l) A) No Antibiotic B) Need Antibiotic Cephalexin Cloxacillin Amoxcillin Erythromycin Augmentin

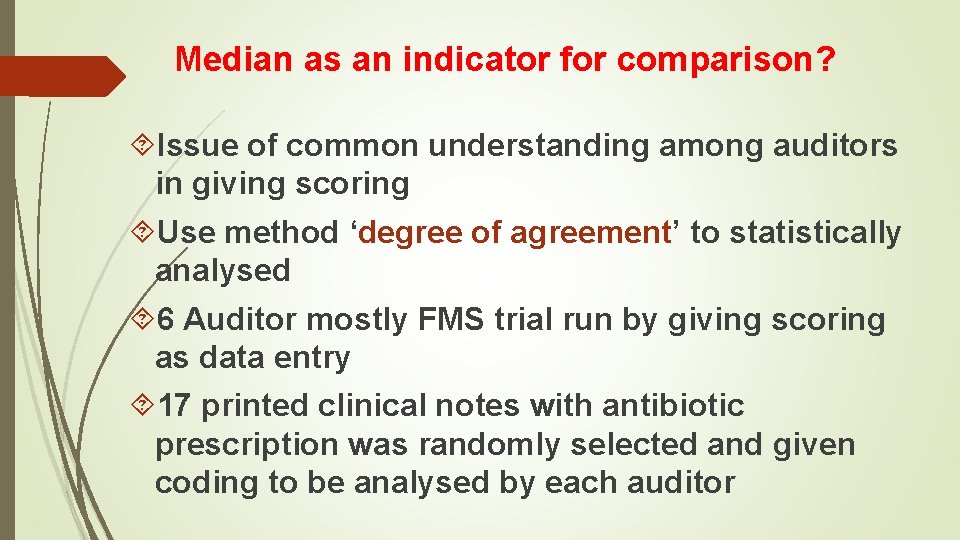
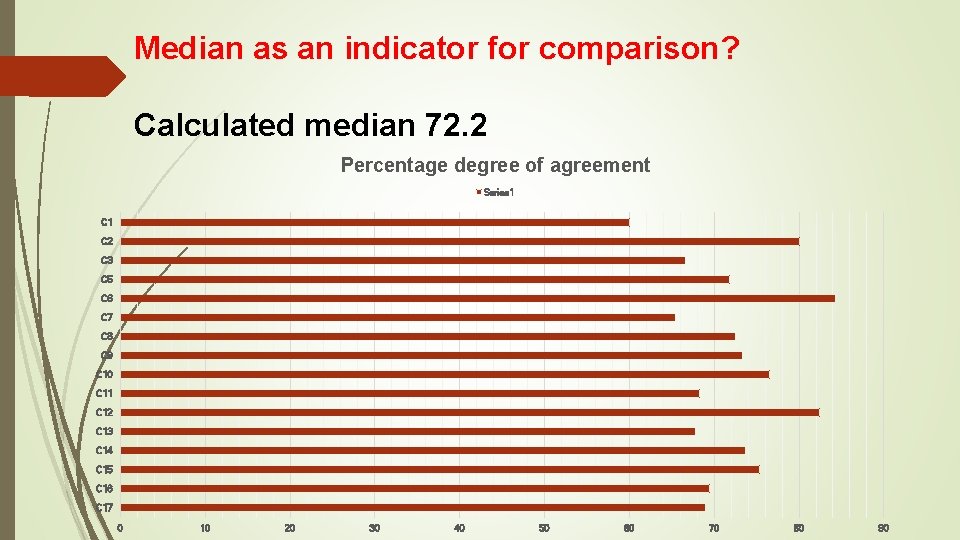
Median as an indicator for comparison? Issue of common understanding among auditors in giving scoring Use method ‘degree of agreement’ to statistically analysed 6 Auditor mostly FMS trial run by giving scoring as data entry 17 printed clinical notes with antibiotic prescription was randomly selected and given coding to be analysed by each auditor

Ujicuba audit klinikal AMS
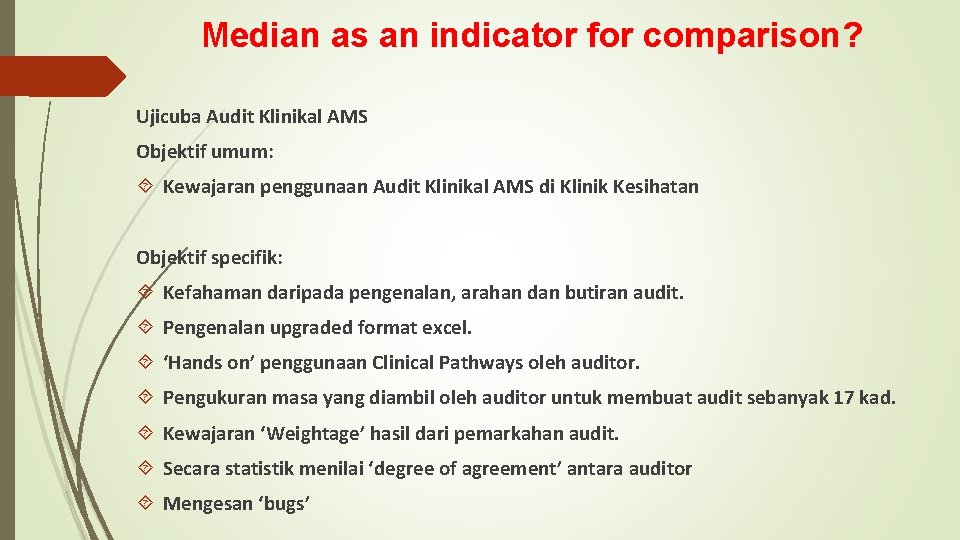
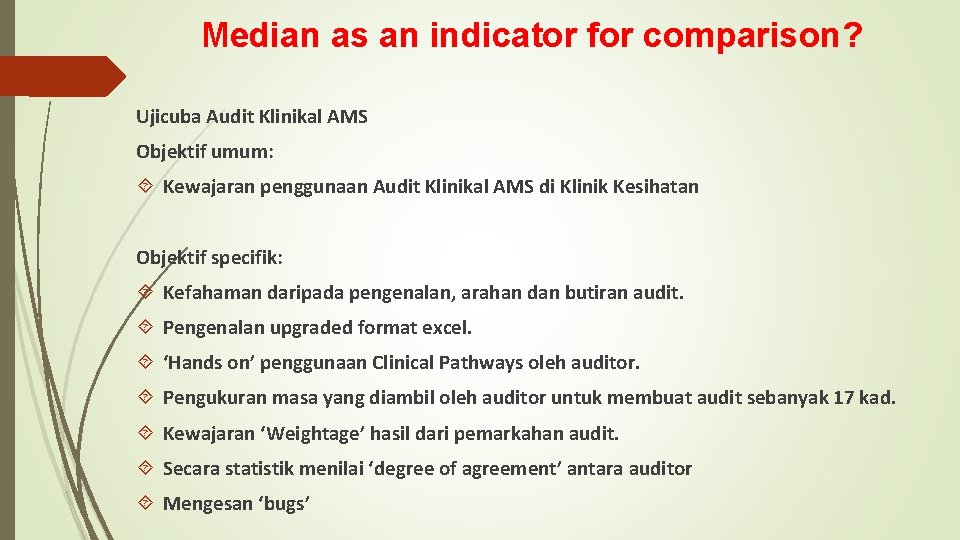
Median as an indicator for comparison? Ujicuba Audit Klinikal AMS Objektif umum: Kewajaran penggunaan Audit Klinikal AMS di Klinik Kesihatan Objektif specifik: Kefahaman daripada pengenalan, arahan dan butiran audit. Pengenalan upgraded format excel. ‘Hands on’ penggunaan Clinical Pathways oleh auditor. Pengukuran masa yang diambil oleh auditor untuk membuat audit sebanyak 17 kad. Kewajaran ‘Weightage’ hasil dari pemarkahan audit. Secara statistik menilai ‘degree of agreement’ antara auditor Mengesan ‘bugs’
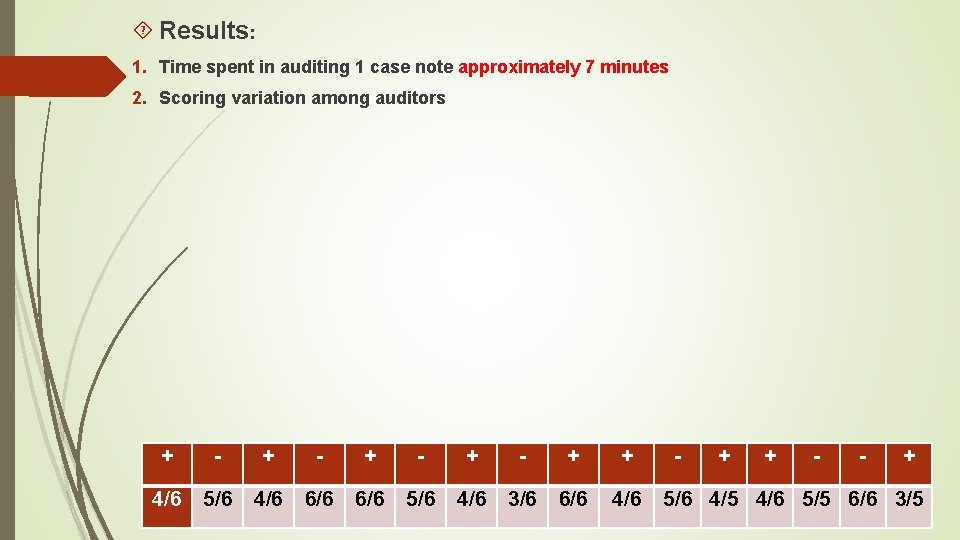
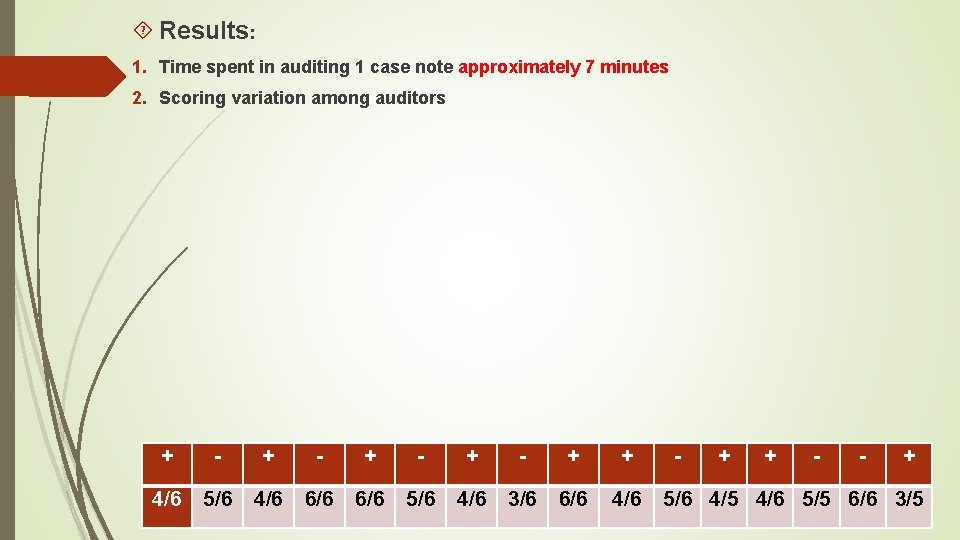
Results: 1. Time spent in auditing 1 case note approximately 7 minutes 2. Scoring variation among auditors + - + - + + 4/6 5/6 4/6 6/6 5/6 4/6 3/6 6/6 4/6 - + + - - + 5/6 4/5 4/6 5/5 6/6 3/5
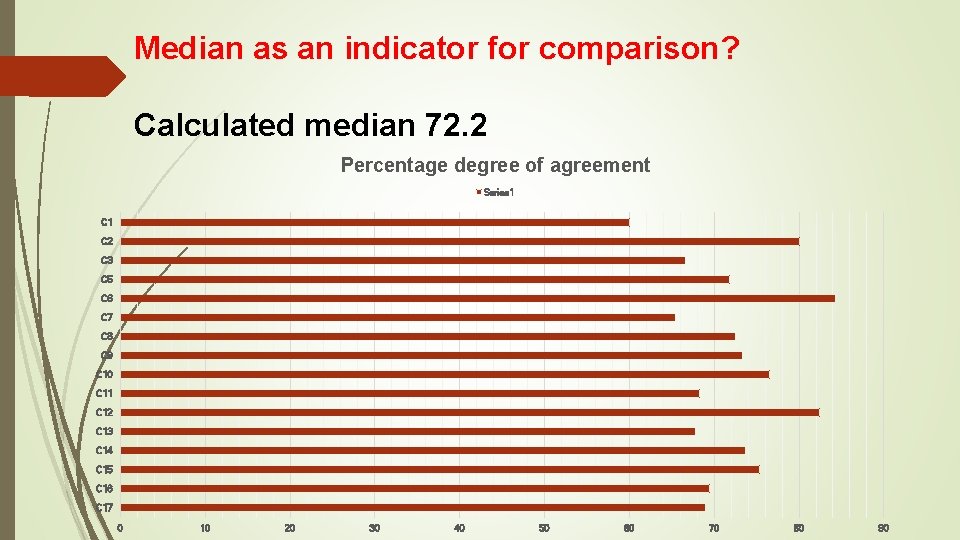
Median as an indicator for comparison? Calculated median 72. 2 Percentage degree of agreement Series 1 C 2 C 3 C 5 C 6 C 7 C 8 C 9 C 10 C 11 C 12 C 13 C 14 C 15 C 16 C 17 0 10 20 30 40 50 60 70 80 90
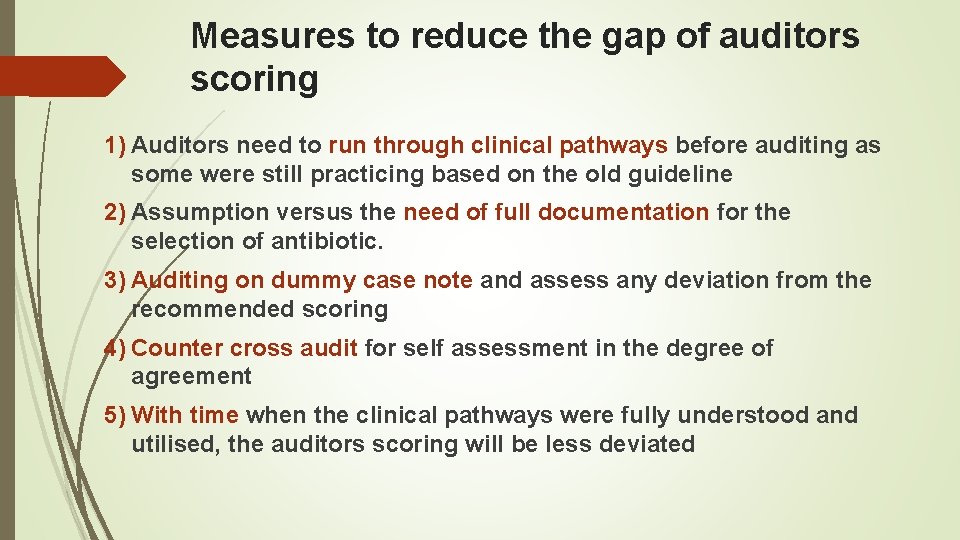
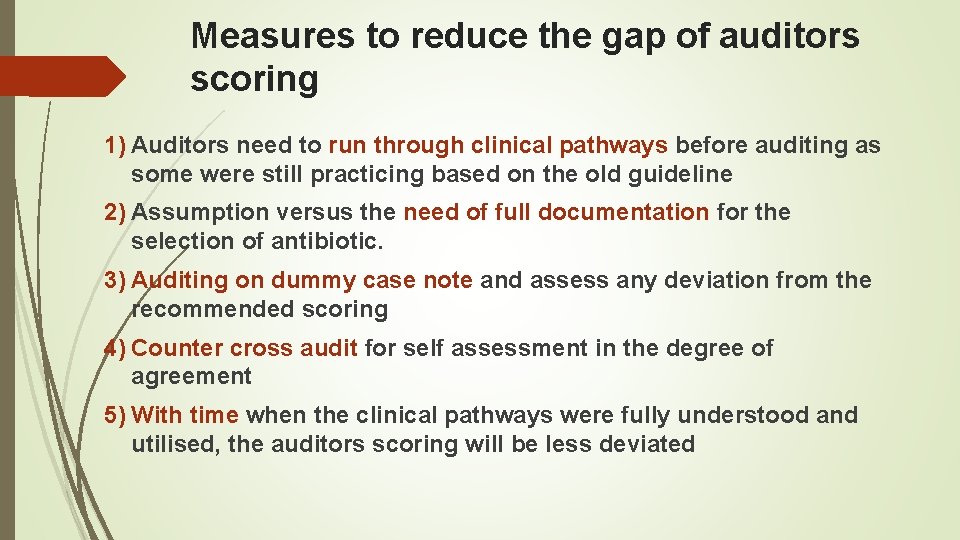
Measures to reduce the gap of auditors scoring 1) Auditors need to run through clinical pathways before auditing as some were still practicing based on the old guideline 2) Assumption versus the need of full documentation for the selection of antibiotic. 3) Auditing on dummy case note and assess any deviation from the recommended scoring 4) Counter cross audit for self assessment in the degree of agreement 5) With time when the clinical pathways were fully understood and utilised, the auditors scoring will be less deviated
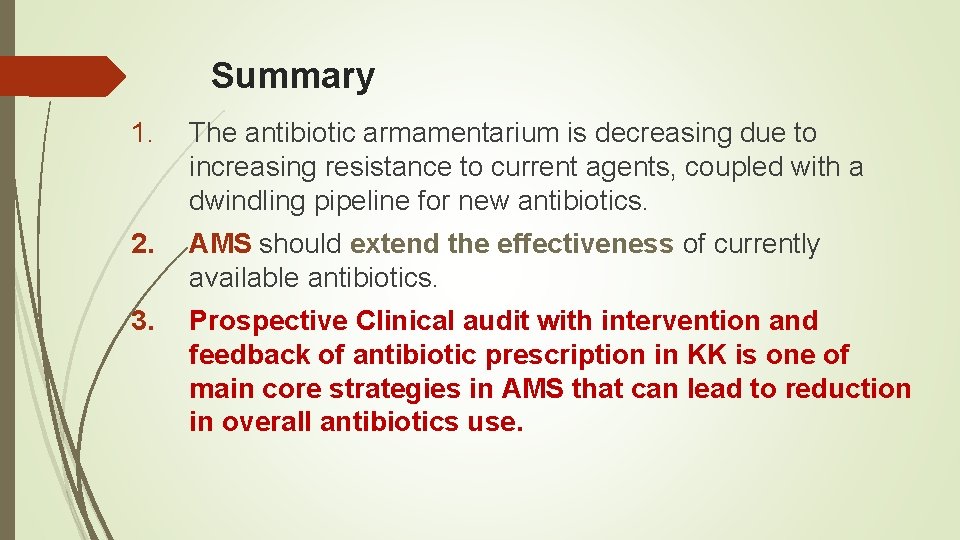
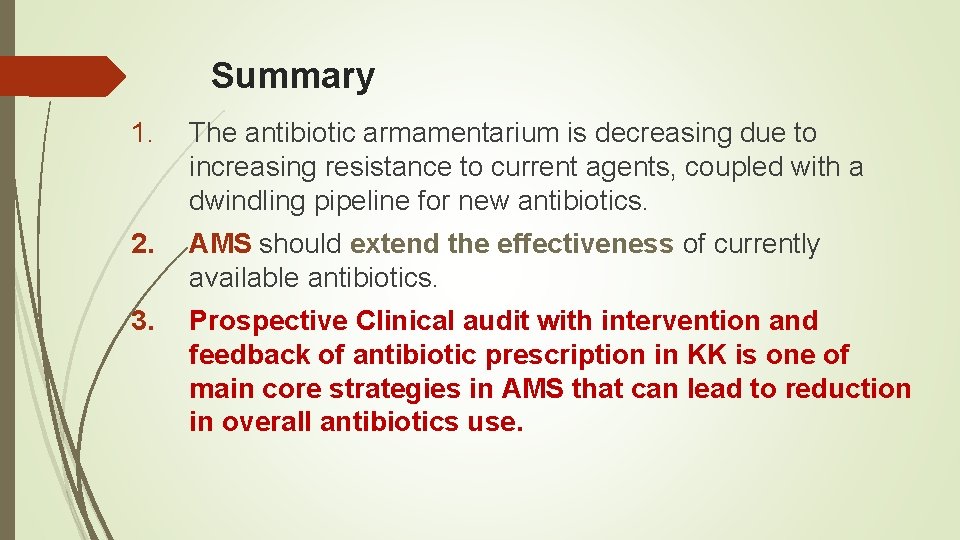
Summary 1. The antibiotic armamentarium is decreasing due to increasing resistance to current agents, coupled with a dwindling pipeline for new antibiotics. 2. AMS should extend the effectiveness of currently available antibiotics. 3. Prospective Clinical audit with intervention and feedback of antibiotic prescription in KK is one of main core strategies in AMS that can lead to reduction in overall antibiotics use.
 Audit ams
Audit ams Clinical audit example
Clinical audit example How to do clinical audit a brief guide
How to do clinical audit a brief guide Siq kkm
Siq kkm Akmol hussain
Akmol hussain Hanin hussain
Hanin hussain Gis
Gis Zahin hussain
Zahin hussain Mulazim hussain bukhari
Mulazim hussain bukhari Dr azhar hussain
Dr azhar hussain Maria hussain leeds
Maria hussain leeds Rosie hussain
Rosie hussain Dr insiya hussain
Dr insiya hussain Maria hussain leeds
Maria hussain leeds Cyrus vandrevala
Cyrus vandrevala Family tree of quraish tribe
Family tree of quraish tribe Stephanie husan
Stephanie husan Sehrish hussain
Sehrish hussain Iftikhar hussain md
Iftikhar hussain md Shahid hussain psychiatrist
Shahid hussain psychiatrist Journey of imam hussain
Journey of imam hussain Kabeer hussain
Kabeer hussain Hussain mujh ko maaf karna
Hussain mujh ko maaf karna Hussain
Hussain Waris husain
Waris husain Mulazim hussain bukhari
Mulazim hussain bukhari Hussain manawer does heaven have a balcony
Hussain manawer does heaven have a balcony Tarif-i-hussain shahi
Tarif-i-hussain shahi Beda audit medis dan audit klinis
Beda audit medis dan audit klinis Define auditing
Define auditing Overall audit plan
Overall audit plan Penyelesaian audit dan tanggung jawab pasca audit
Penyelesaian audit dan tanggung jawab pasca audit Perbedaan audit konvensional dengan audit berbasis risiko
Perbedaan audit konvensional dengan audit berbasis risiko Perbedaan audit konvensional dengan audit berbasis risiko
Perbedaan audit konvensional dengan audit berbasis risiko