City and Hackney Clinical Commissioning Forum Thursday 5
- Slides: 32
City and Hackney Clinical Commissioning Forum Thursday 5 th January 2017 St Joseph’s Hospice
Agenda 1. Welcome Haren Patel 2. Homerton update (verbal) Tracey Fletcher 3. Discovery update Kambiz Boomla 4. 111 service (for consultation ) May Cahill and Anna Hanbury The next Clinical Commissioning Forum will be held on Thursday 2 February 2017, 1. 00 pm in the 1 st Floor Education Centre, St Joseph’s Hospice, Mare Street, Hackney
Homerton update Tracey Fletcher HUH Chief Executive
Discovery update Kambiz Boomla
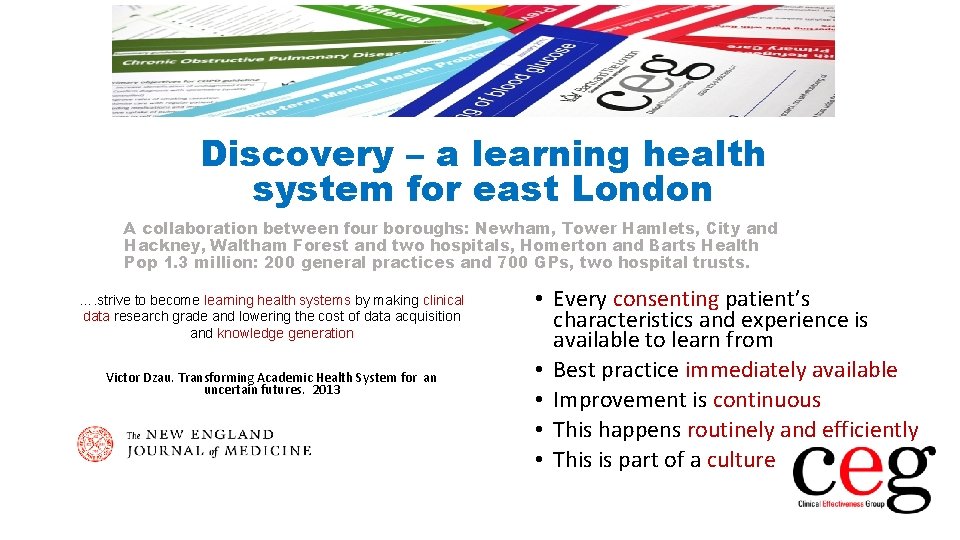
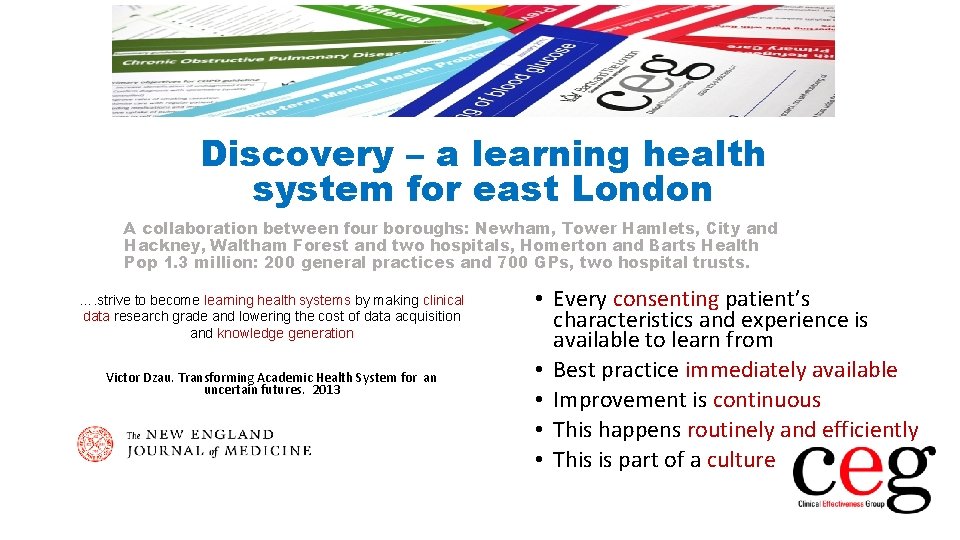
Discovery – a learning health system for east London A collaboration between four boroughs: Newham, Tower Hamlets, City and Hackney, Waltham Forest and two hospitals, Homerton and Barts Health Pop 1. 3 million: 200 general practices and 700 GPs, two hospital trusts. …. strive to become learning health systems by making clinical data research grade and lowering the cost of data acquisition and knowledge generation Victor Dzau. Transforming Academic Health System for an uncertain futures. 2013 • Every consenting patient’s characteristics and experience is available to learn from • Best practice immediately available • Improvement is continuous • This happens routinely and efficiently • This is part of a culture
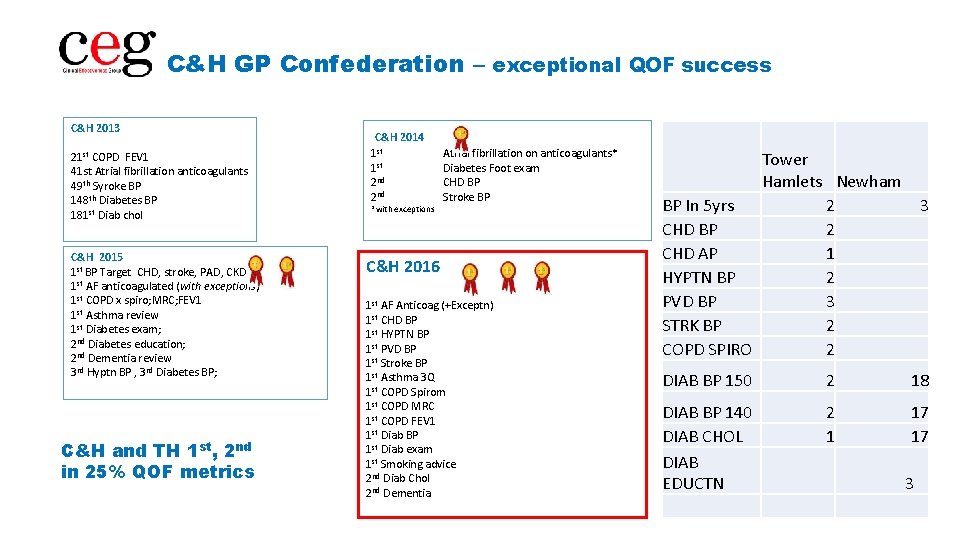
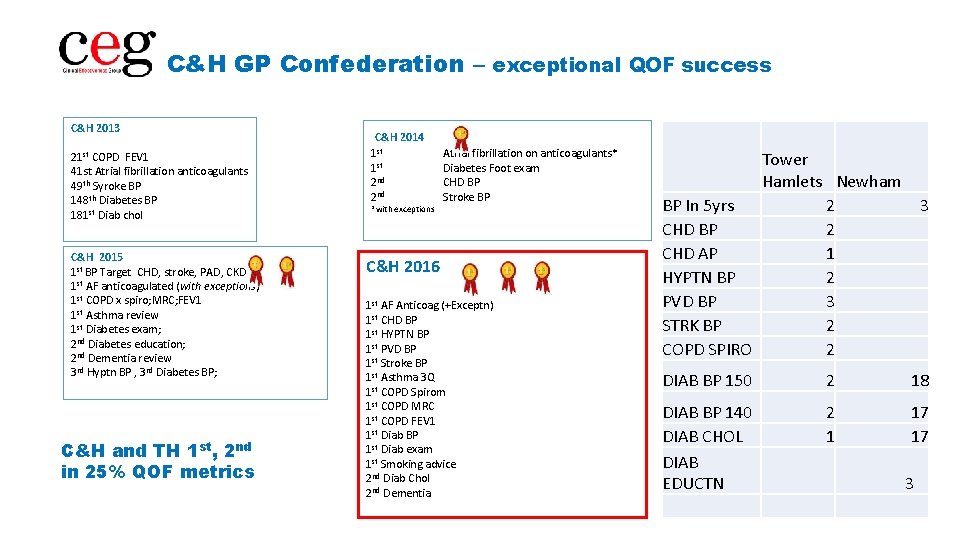
C&H GP Confederation – exceptional QOF success C&H 2013 21 st COPD FEV 1 41 st Atrial fibrillation anticoagulants 49 th Syroke BP 148 th Diabetes BP 181 st Diab chol C&H 2015 1 st BP Target CHD, stroke, PAD, CKD 1 st AF anticoagulated (with exceptions) 1 st COPD x spiro; MRC; FEV 1 1 st Asthma review 1 st Diabetes exam; 2 nd Diabetes education; 2 nd Dementia review 3 rd Hyptn BP , 3 rd Diabetes BP; C&H and TH 1 st, 2 nd in 25% QOF metrics C&H 2014 1 st 2 nd *with exceptions Atrial fibrillation on anticoagulants* Diabetes Foot exam CHD BP Stroke BP C&H 2016 1 st AF Anticoag (+Exceptn) 1 st CHD BP 1 st HYPTN BP 1 st PVD BP 1 st Stroke BP 1 st Asthma 3 Q 1 st COPD Spirom 1 st COPD MRC 1 st COPD FEV 1 1 st Diab BP 1 st Diab exam 1 st Smoking advice 2 nd Diab Chol 2 nd Dementia Tower Hamlets Newham BP In 5 yrs 2 CHD BP 2 CHD AP 1 HYPTN BP 2 PVD BP 3 STRK BP 2 COPD SPIRO 2 3 DIAB BP 150 2 18 DIAB BP 140 DIAB CHOL DIAB EDUCTN 2 1 17 17 3
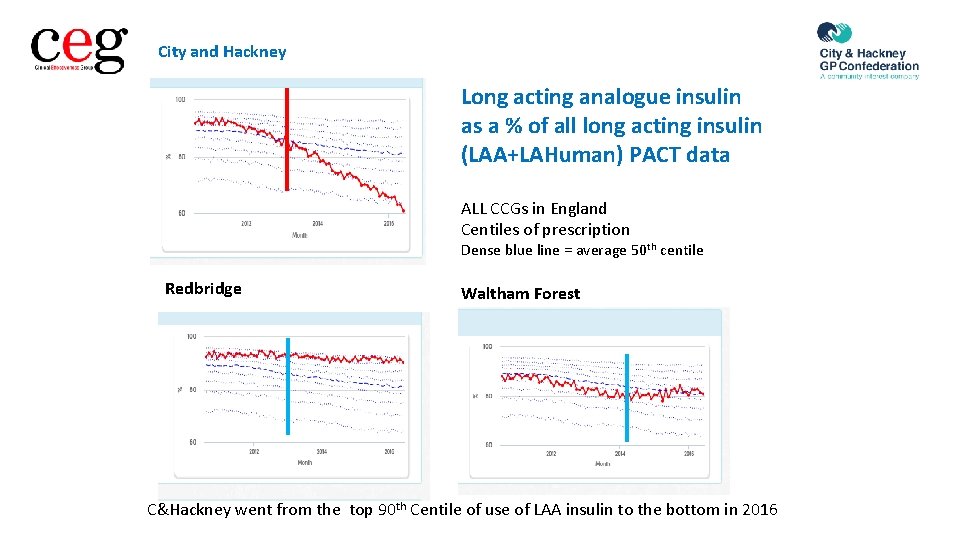
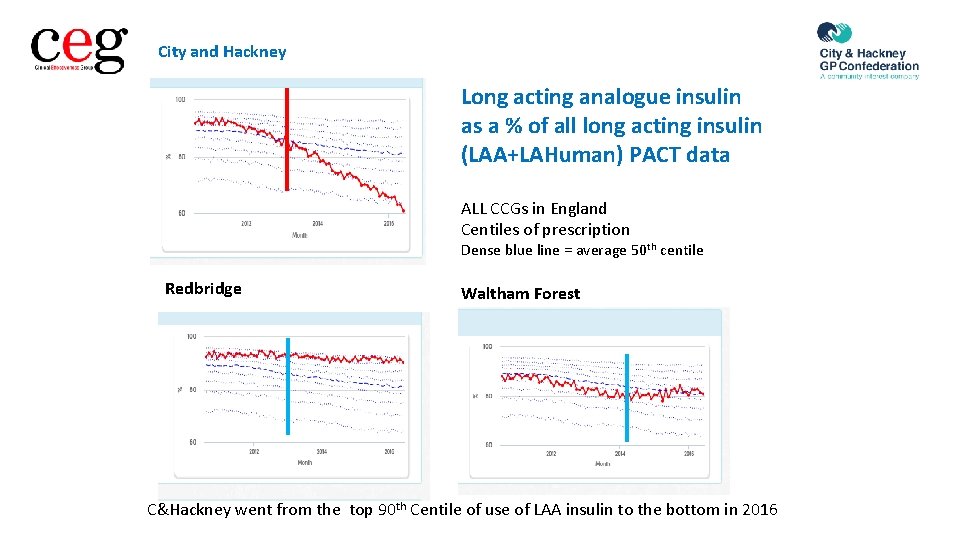
City and Hackney Long acting analogue insulin as a % of all long acting insulin (LAA+LAHuman) PACT data ALL CCGs in England Centiles of prescription Dense blue line = average 50 th centile Redbridge Waltham Forest C&Hackney went from the top 90 th Centile of use of LAA insulin to the bottom in 2016
EMIS CERNER Social Services HSCIC
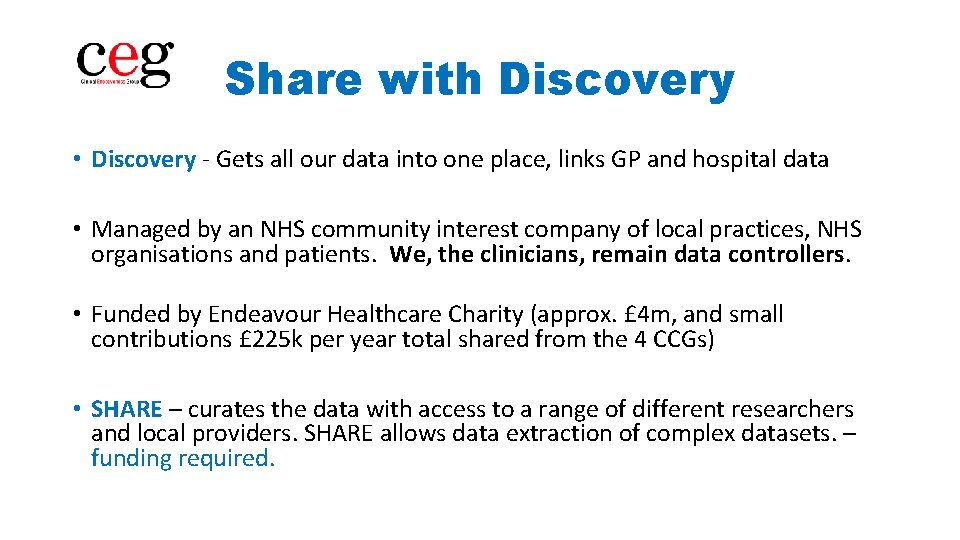
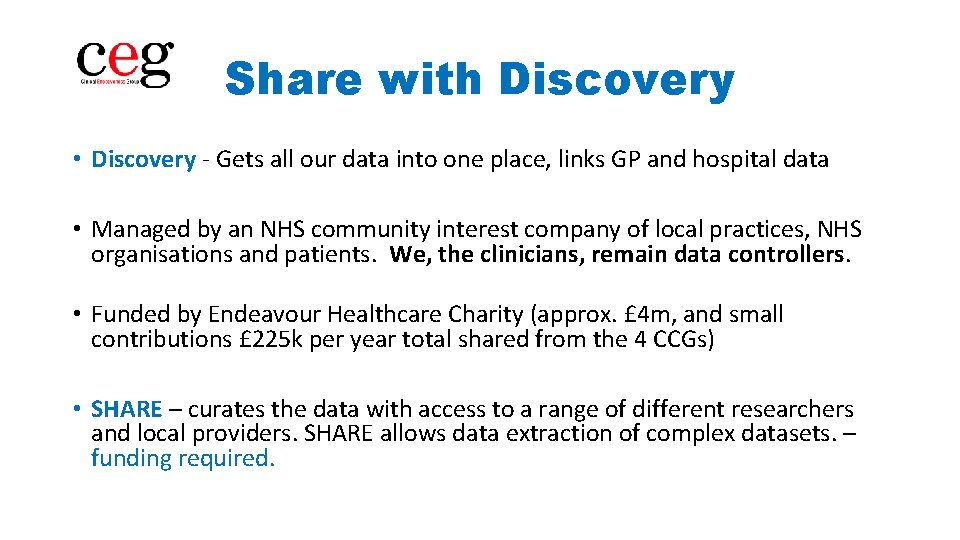
Share with Discovery • Discovery - Gets all our data into one place, links GP and hospital data • Managed by an NHS community interest company of local practices, NHS organisations and patients. We, the clinicians, remain data controllers. • Funded by Endeavour Healthcare Charity (approx. £ 4 m, and small contributions £ 225 k per year total shared from the 4 CCGs) • SHARE – curates the data with access to a range of different researchers and local providers. SHARE allows data extraction of complex datasets. – funding required.
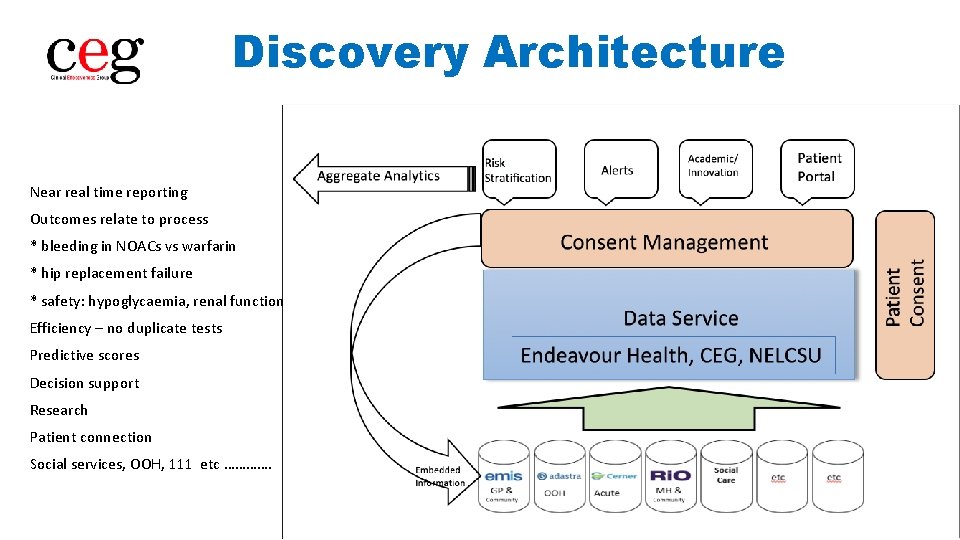
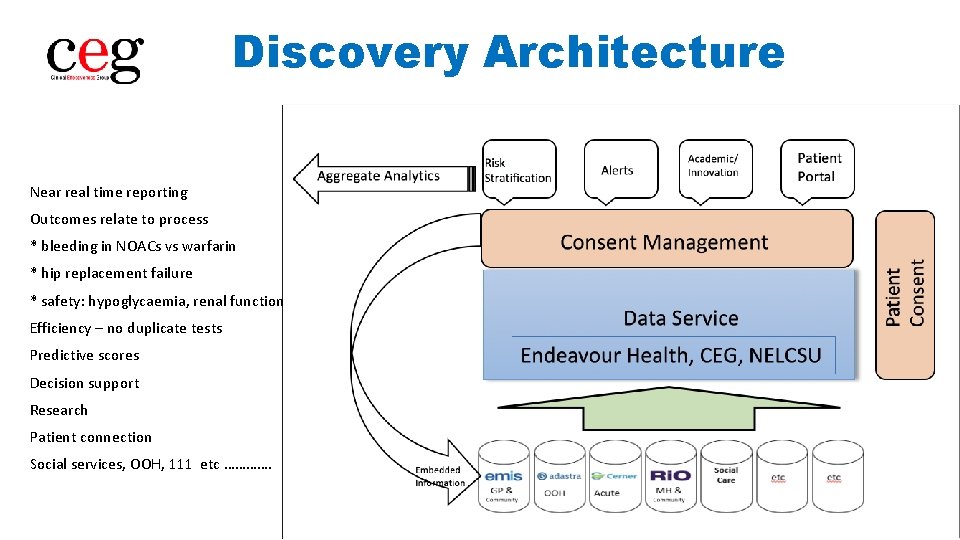
Discovery Architecture Near real time reporting Outcomes relate to process * bleeding in NOACs vs warfarin * hip replacement failure * safety: hypoglycaemia, renal function Efficiency – no duplicate tests Predictive scores Decision support Research Patient connection Social services, OOH, 111 etc ………….
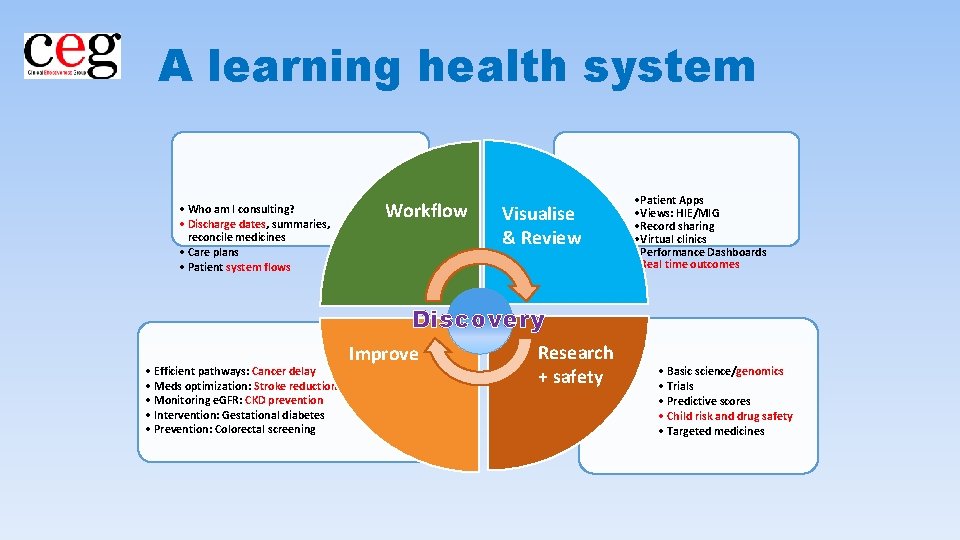
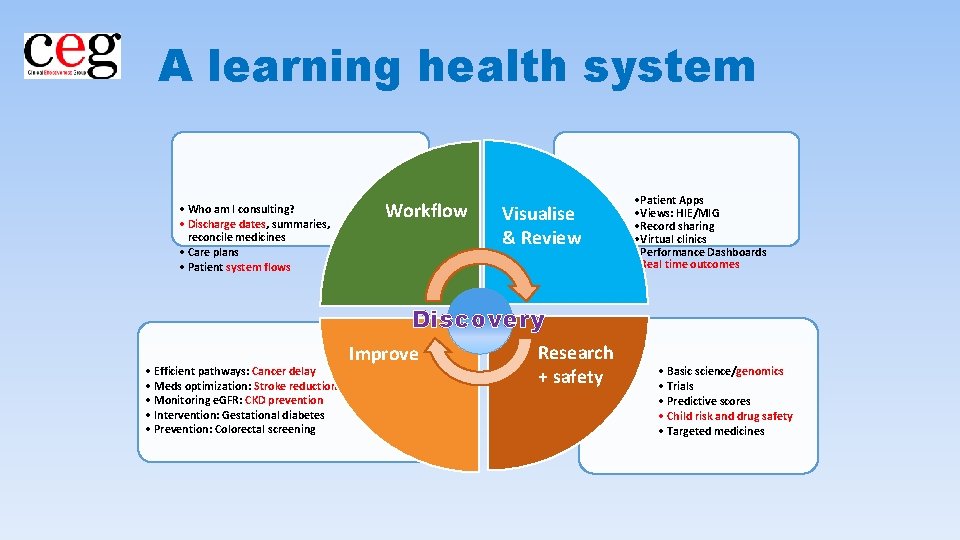
A learning health system • Who am I consulting? • Discharge dates, summaries, reconcile medicines • Care plans • Patient system flows Workflow Visualise & Review • Patient Apps • Views: HIE/MIG • Record sharing • Virtual clinics • Performance Dashboards • Real time outcomes Discovery • Efficient pathways: Cancer delay • Meds optimization: Stroke reduction • Monitoring e. GFR: CKD prevention • Intervention: Gestational diabetes • Prevention: Colorectal screening Improve Research + safety • Basic science/genomics • Trials • Predictive scores • Child risk and drug safety • Targeted medicines
Integrated Urgent Care / 111 5 th January 2017 Dr May Cahill
Integrated urgent care (IUC) – what and why? • UEC review and FYF view - Delivery requires closer integration of urgent care services • Integrated urgent care – the offer to the public - Single entry point (111) - Organisational collaboration - fully integrated services - High quality assessment, advice and treatment - Shared standards and processes - Clear leadership and accountability • The Clinical Advice Service (CAS) (aka ‘Clinical Hub’) - Central to the vision - Access to a wide range of clinicians (specialist and generalist) - Available for patients who need it - Also available to health care professionals (HCPs)
IUC – The vision • Access, Assessment, Advice, Treatment • The vision: If I have an urgent need, I can phone a single number (111) and they will, if necessary, arrange for me to see or speak to a GP, or other appropriate clinician / healthcare professional – any hour of the day and any day of the week.
The 8 Key Elements of IUC NHSE specification 1. A single call to get an appointment Out of Hours 2. Data can be sent between providers 3. The capacity for NHS 111 and OOHs is jointly planned 4. The Summary Care Record (SCR) is available in the hub and elsewhere 5. Care plans and patient notes are shared 6. Appointments can be made to in-hours GPs 7. There is Joint governance across urgent and Emergency Care providers 8. There is a Clinical Hub containing GPs and other health care professional
IUC from the patient’s perspective • A single number – NHS 111 – for all your urgent health needs • Be able to speak to a clinician if needed • Your health records available to clinicians treating you wherever you are (111, 999, community, hospital) • To be booked into the right service for you, when convenient to you • A clinically appropriate response to 999 which may be: treatment advice by phone, in person by ambulance staff, or taken to hospital • Care close to home (or at home) unless you need a specialist service • Access to specialist care services (e. g. major trauma/stroke) through a network that includes specialist hospitals in your wider area
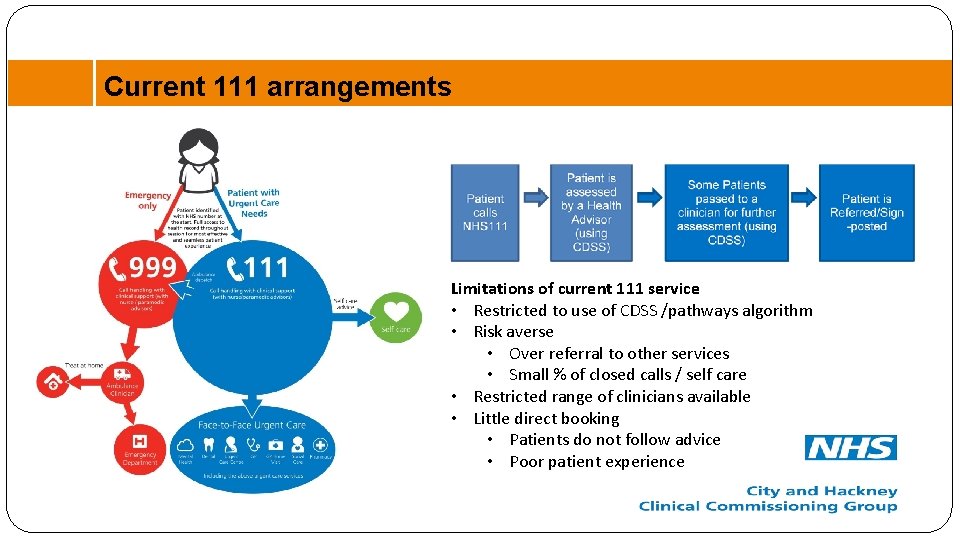
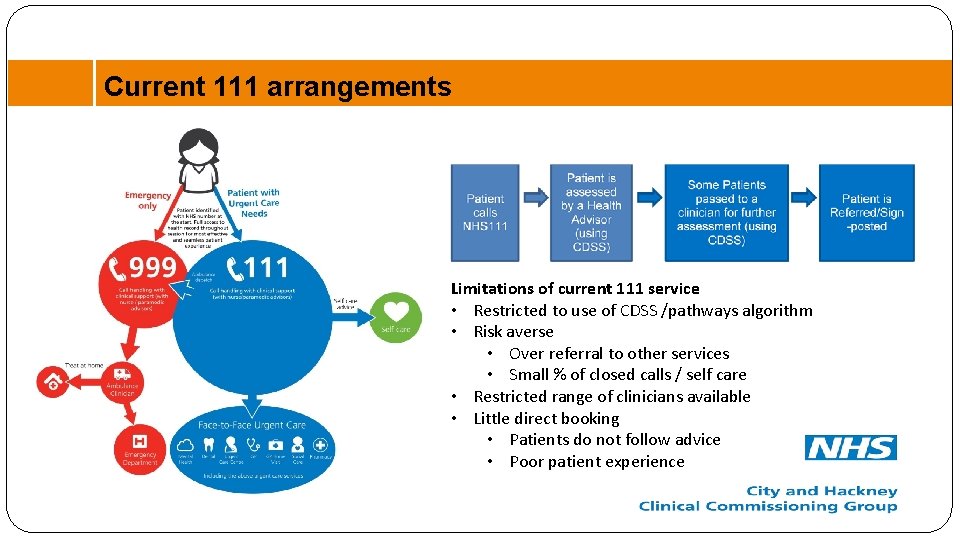
Current 111 arrangements Limitations of current 111 service • Restricted to use of CDSS /pathways algorithm • Risk averse • Over referral to other services • Small % of closed calls / self care • Restricted range of clinicians available • Little direct booking • Patients do not follow advice • Poor patient experience
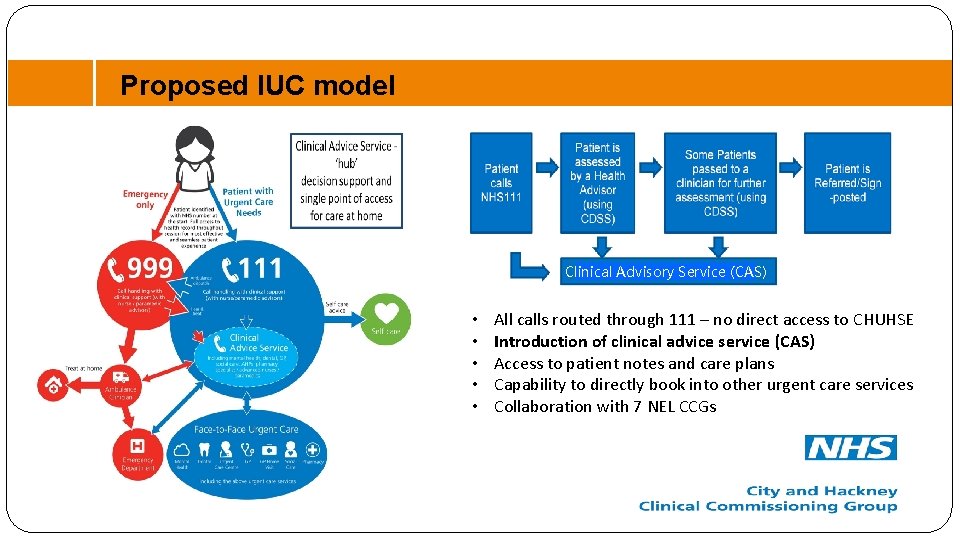
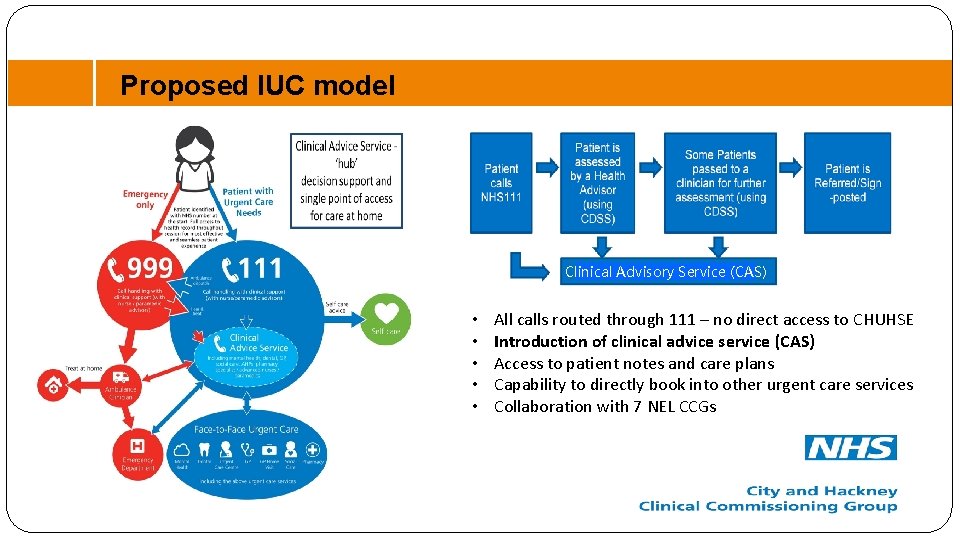
Proposed IUC model Clinical Advisory Service (CAS) • • • All calls routed through 111 – no direct access to CHUHSE Introduction of clinical advice service (CAS) Access to patient notes and care plans Capability to directly book into other urgent care services Collaboration with 7 NEL CCGs
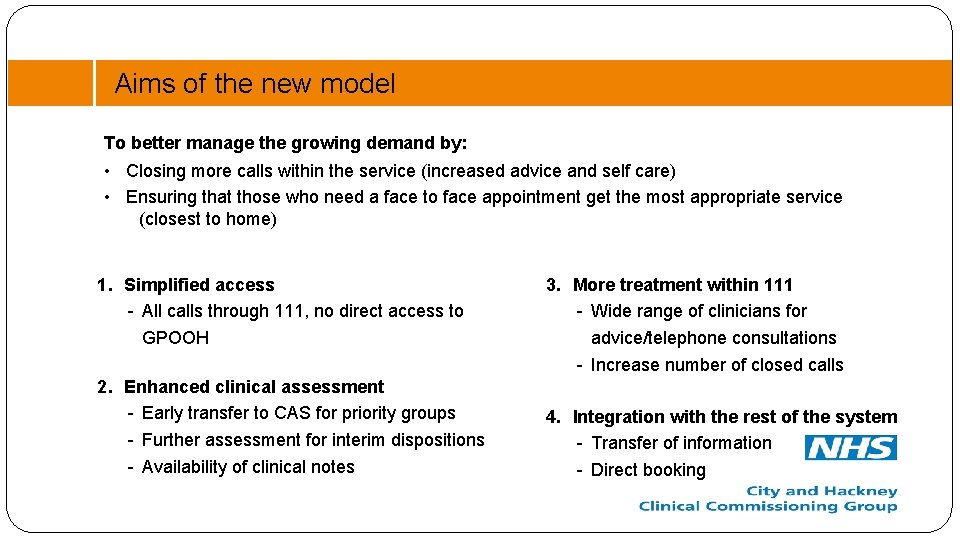
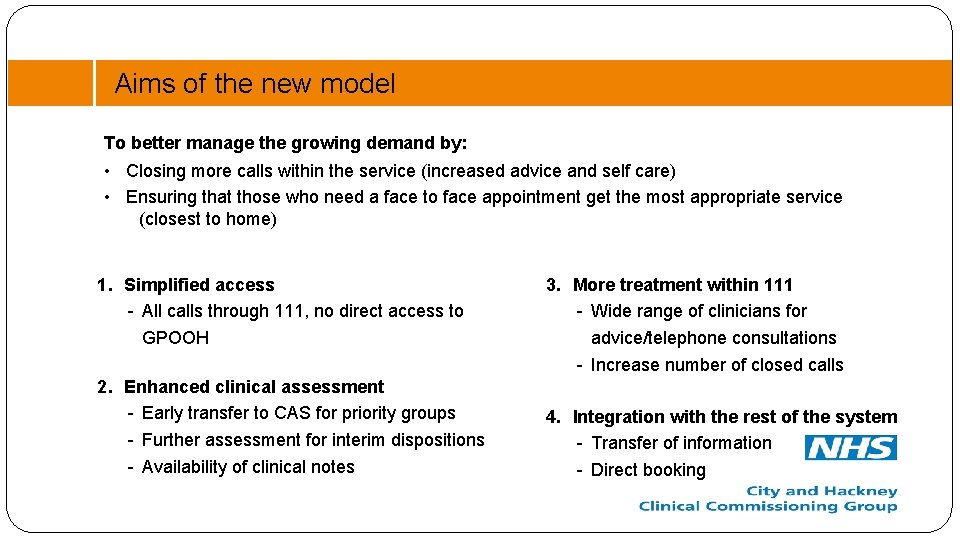
Aims of the new model To better manage the growing demand by: • Closing more calls within the service (increased advice and self care) • Ensuring that those who need a face to face appointment get the most appropriate service (closest to home) 1. Simplified access - All calls through 111, no direct access to GPOOH 2. Enhanced clinical assessment - Early transfer to CAS for priority groups - Further assessment for interim dispositions - Availability of clinical notes 3. More treatment within 111 - Wide range of clinicians for advice/telephone consultations - Increase number of closed calls 4. Integration with the rest of the system - Transfer of information - Direct booking
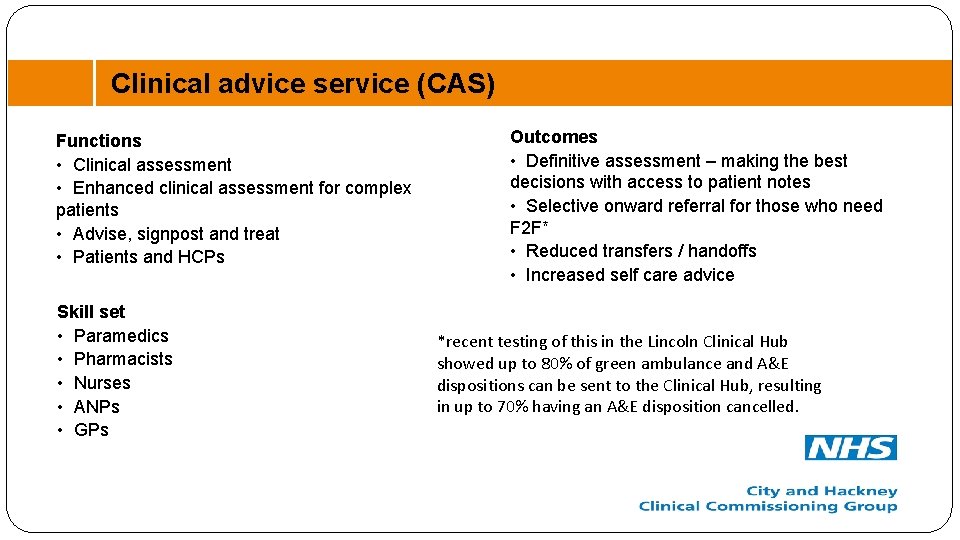
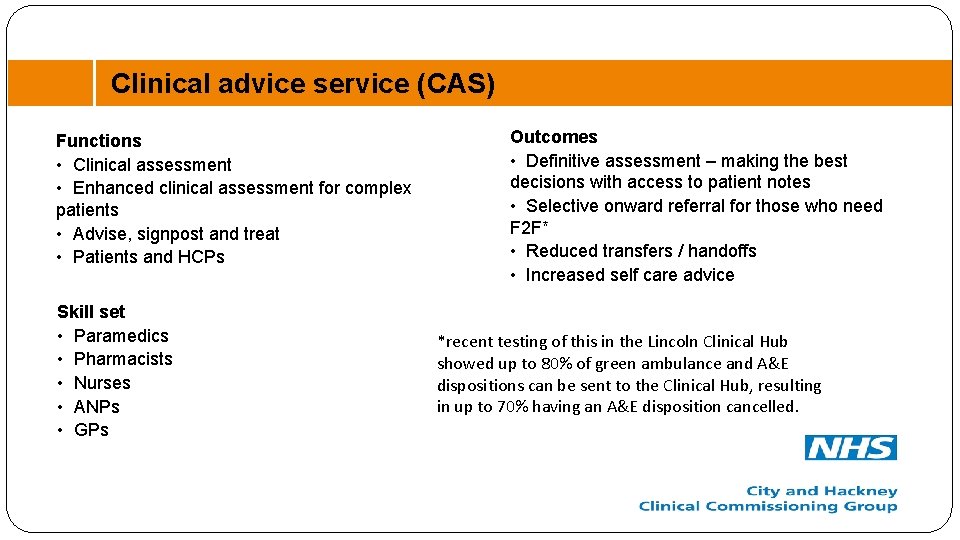
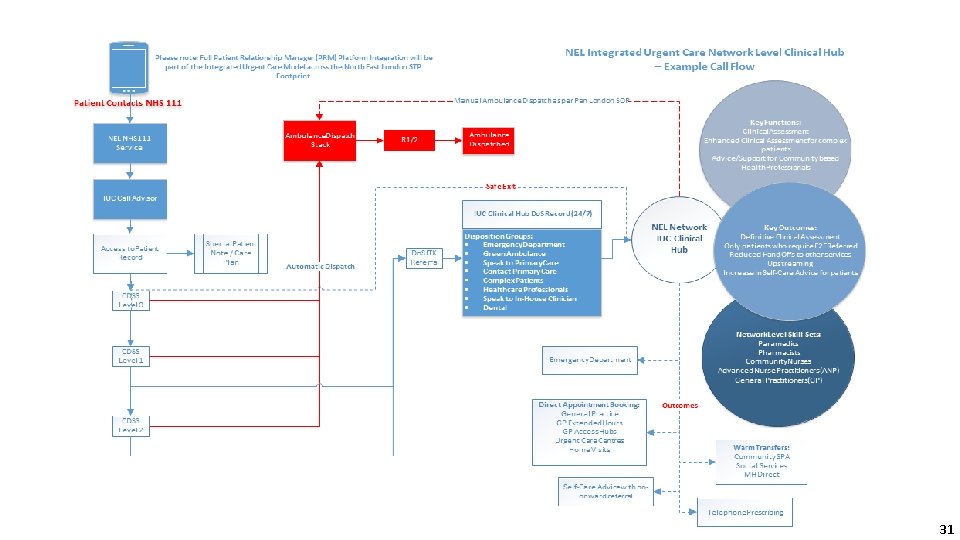
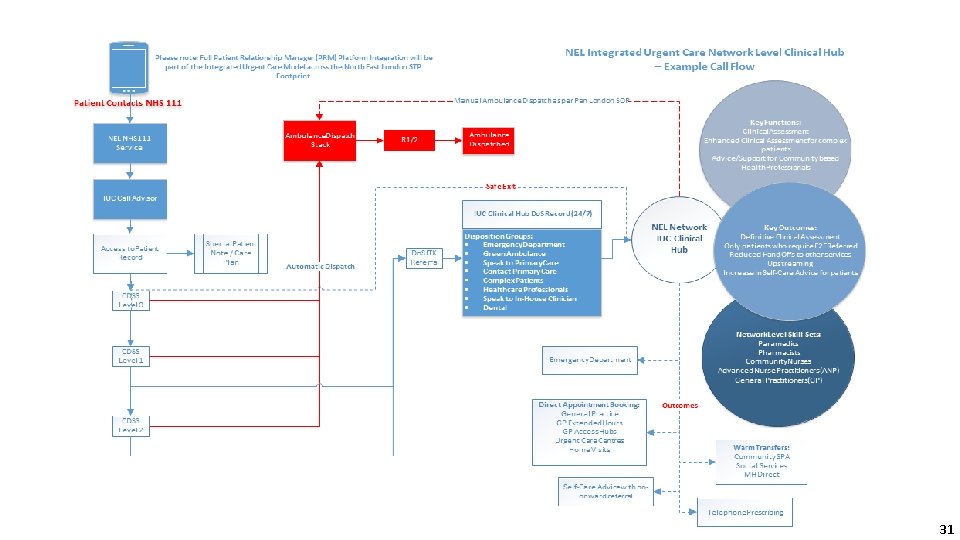
Clinical advice service (CAS) Functions • Clinical assessment • Enhanced clinical assessment for complex patients • Advise, signpost and treat • Patients and HCPs Skill set • Paramedics • Pharmacists • Nurses • ANPs • GPs Outcomes • Definitive assessment – making the best decisions with access to patient notes • Selective onward referral for those who need F 2 F* • Reduced transfers / handoffs • Increased self care advice *recent testing of this in the Lincoln Clinical Hub showed up to 80% of green ambulance and A&E dispositions can be sent to the Clinical Hub, resulting in up to 70% having an A&E disposition cancelled.
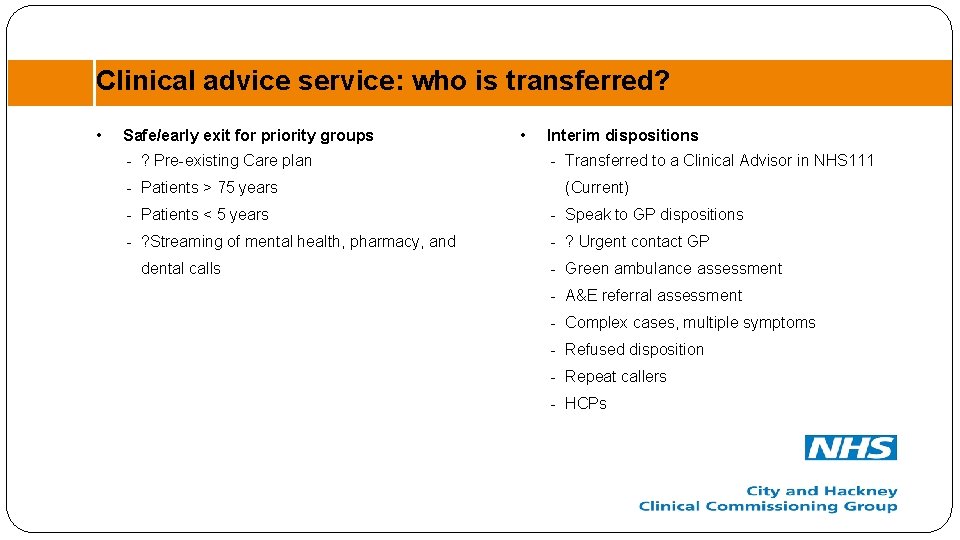
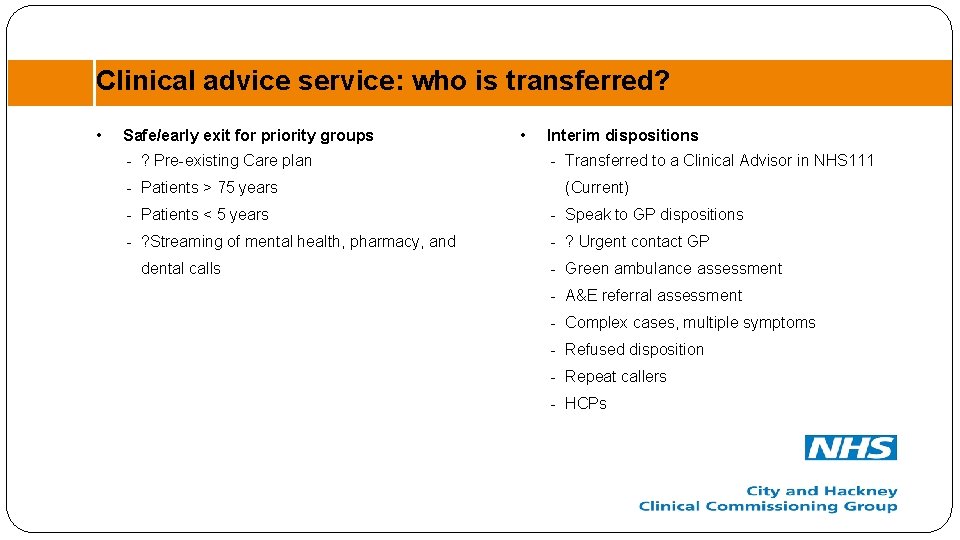
Clinical advice service: who is transferred? • Safe/early exit for priority groups - ? Pre-existing Care plan - Patients > 75 years • Interim dispositions - Transferred to a Clinical Advisor in NHS 111 (Current) - Patients < 5 years - Speak to GP dispositions - ? Streaming of mental health, pharmacy, and - ? Urgent contact GP dental calls - Green ambulance assessment - A&E referral assessment - Complex cases, multiple symptoms - Refused disposition - Repeat callers - HCPs
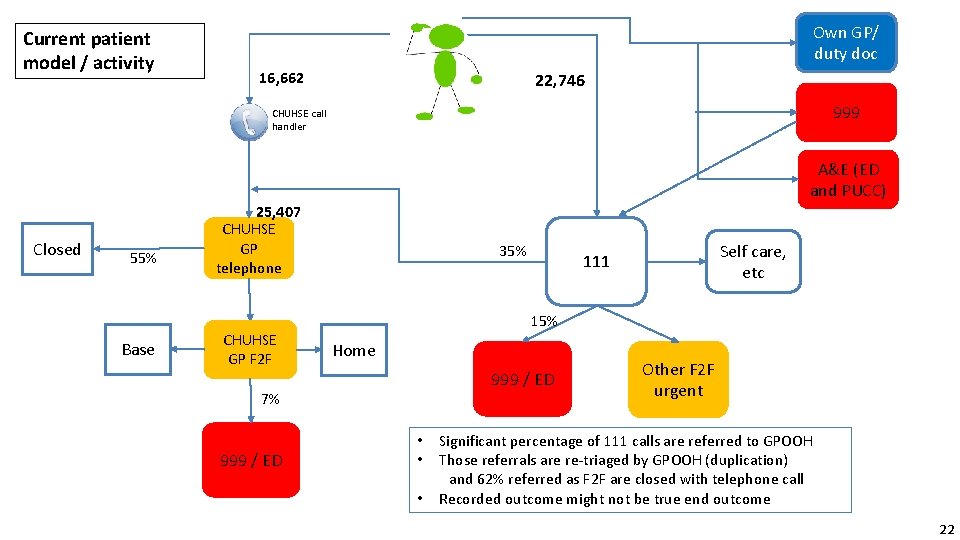
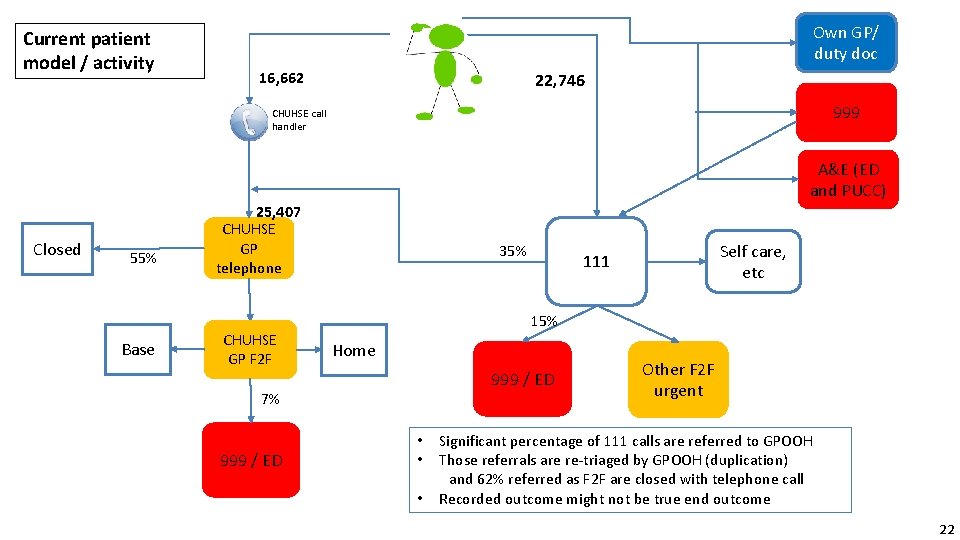
Current patient model / activity Own GP/ duty doc 16, 662 22, 746 999 CHUHSE call handler A&E (ED and PUCC) Closed 55% Base 25, 407 CHUHSE GP telephone CHUHSE GP F 2 F 35% 15% Home 999 / ED 7% 999 / ED Self care, etc 111 • • • Other F 2 F urgent Significant percentage of 111 calls are referred to GPOOH Those referrals are re-triaged by GPOOH (duplication) and 62% referred as F 2 F are closed with telephone call Recorded outcome might not be true end outcome 22
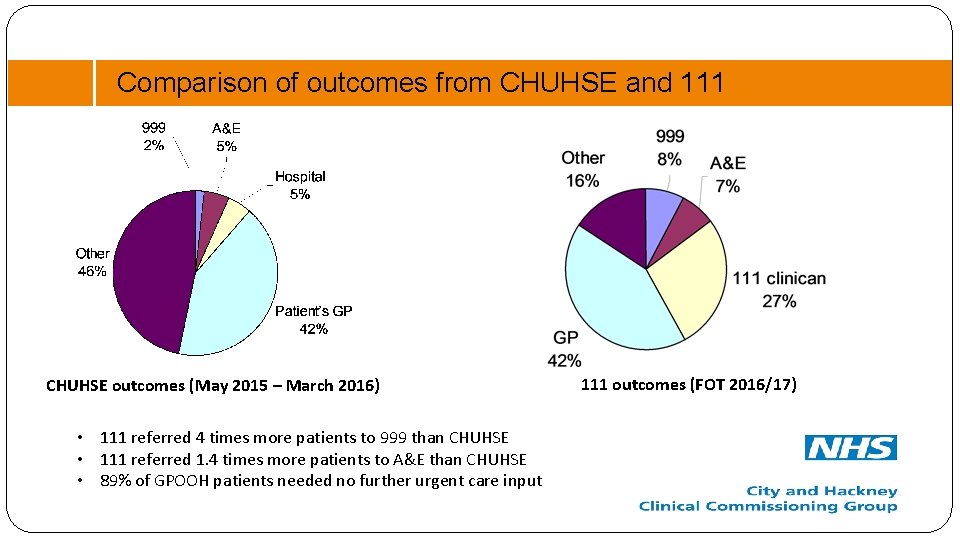
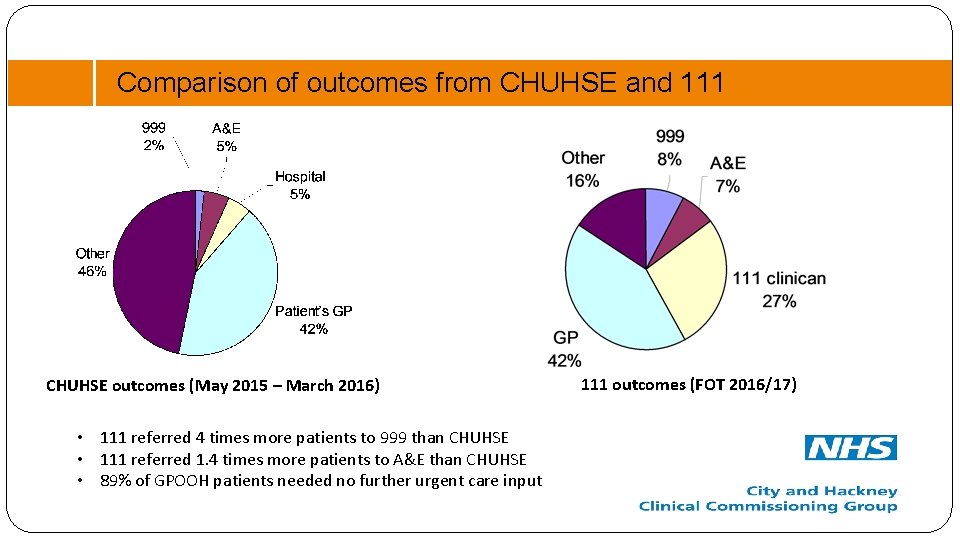
Comparison of outcomes from CHUHSE and 111 CHUHSE outcomes (May 2015 – March 2016) • 111 referred 4 times more patients to 999 than CHUHSE • 111 referred 1. 4 times more patients to A&E than CHUHSE • 89% of GPOOH patients needed no further urgent care input 111 outcomes (FOT 2016/17)
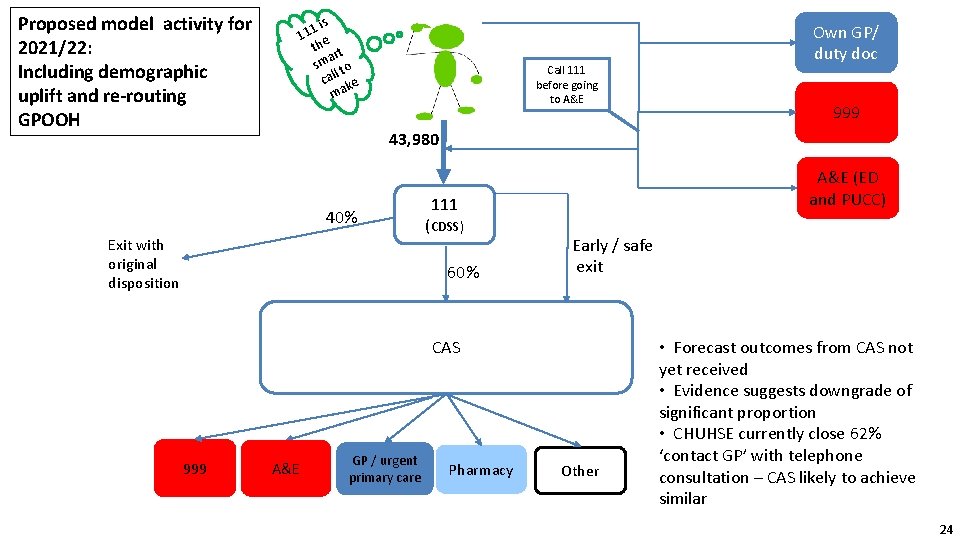
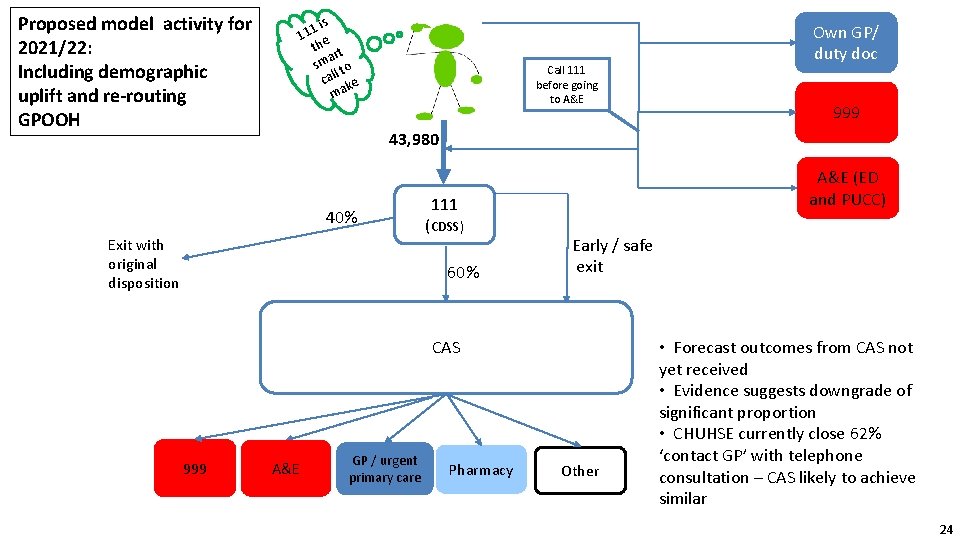
Proposed model activity for 2021/22: Including demographic uplift and re-routing GPOOH is 1 1 1 e th t ar sm to l cal ke ma Call 111 before going to A&E 999 43, 980 40% Exit with original disposition A&E (ED and PUCC) 111 (CDSS) 60% Early / safe exit CAS 999 Own GP/ duty doc A&E GP / urgent primary care Pharmacy Other • Forecast outcomes from CAS not yet received • Evidence suggests downgrade of significant proportion • CHUHSE currently close 62% ‘contact GP’ with telephone consultation – CAS likely to achieve similar 24
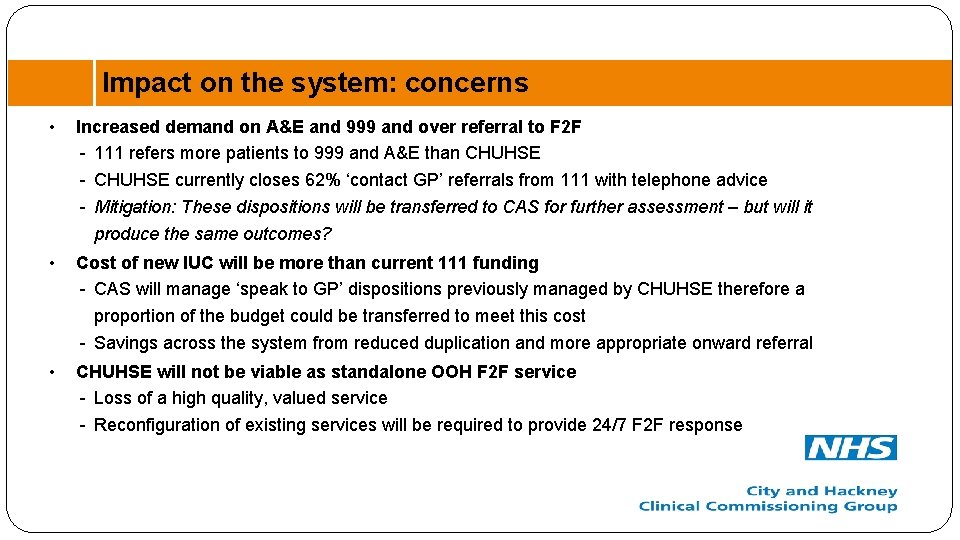
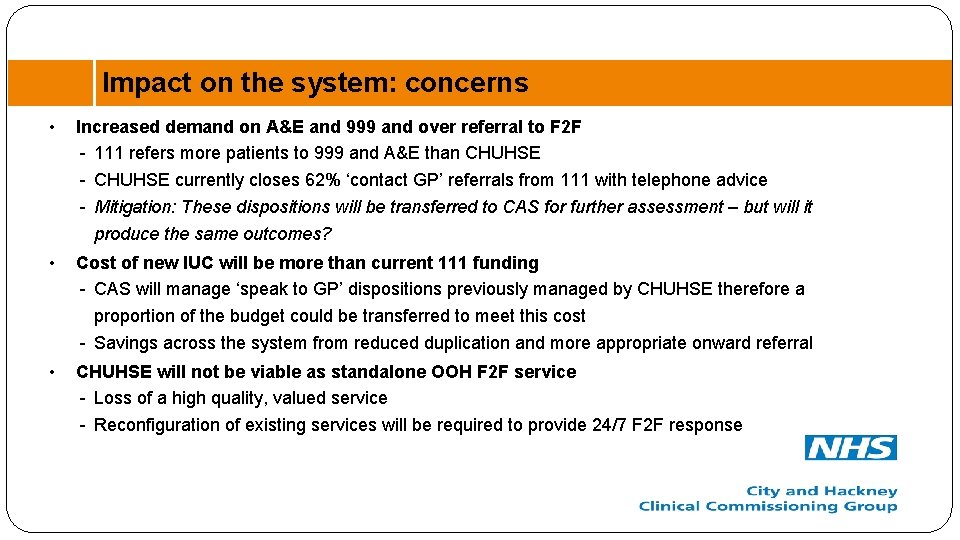
Impact on the system: concerns • Increased demand on A&E and 999 and over referral to F 2 F - 111 refers more patients to 999 and A&E than CHUHSE - CHUHSE currently closes 62% ‘contact GP’ referrals from 111 with telephone advice - Mitigation: These dispositions will be transferred to CAS for further assessment – but will it produce the same outcomes? • Cost of new IUC will be more than current 111 funding - CAS will manage ‘speak to GP’ dispositions previously managed by CHUHSE therefore a proportion of the budget could be transferred to meet this cost - Savings across the system from reduced duplication and more appropriate onward referral • CHUHSE will not be viable as standalone OOH F 2 F service - Loss of a high quality, valued service - Reconfiguration of existing services will be required to provide 24/7 F 2 F response
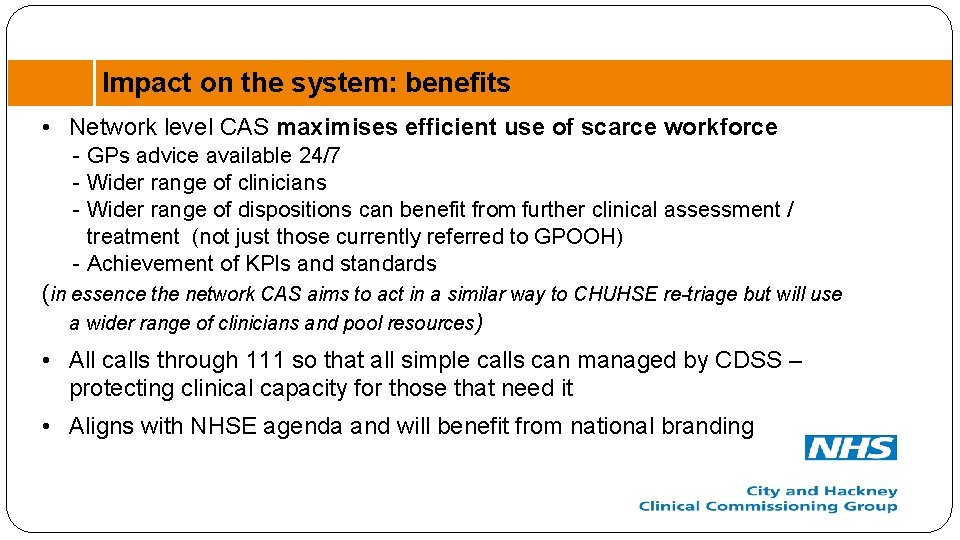
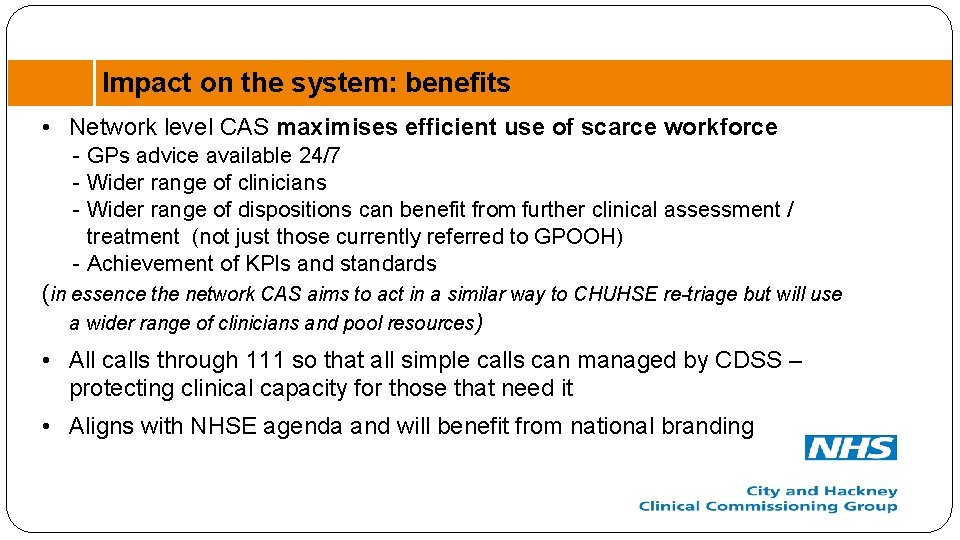
Impact on the system: benefits • Network level CAS maximises efficient use of scarce workforce - GPs advice available 24/7 - Wider range of clinicians - Wider range of dispositions can benefit from further clinical assessment / treatment (not just those currently referred to GPOOH) - Achievement of KPIs and standards (in essence the network CAS aims to act in a similar way to CHUHSE re-triage but will use a wider range of clinicians and pool resources) • All calls through 111 so that all simple calls can managed by CDSS – protecting clinical capacity for those that need it • Aligns with NHSE agenda and will benefit from national branding
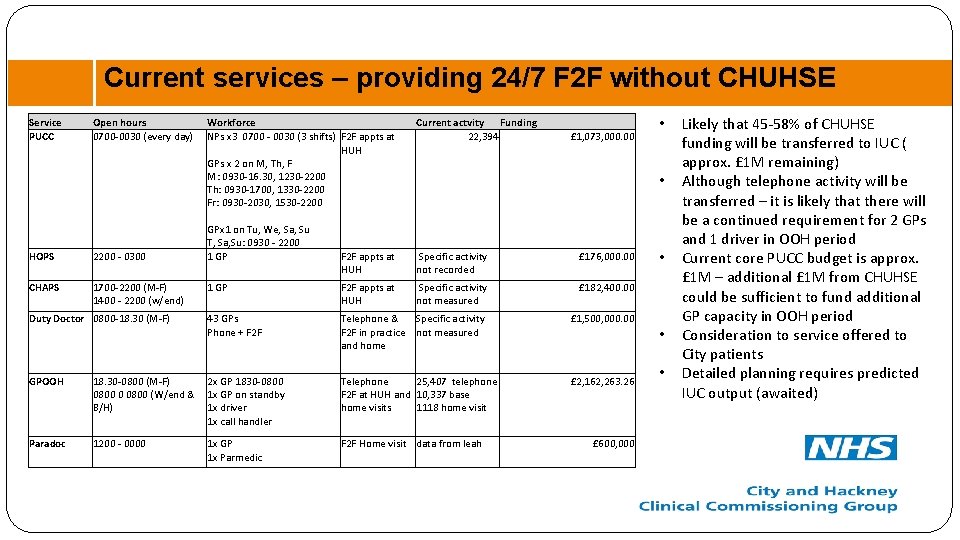
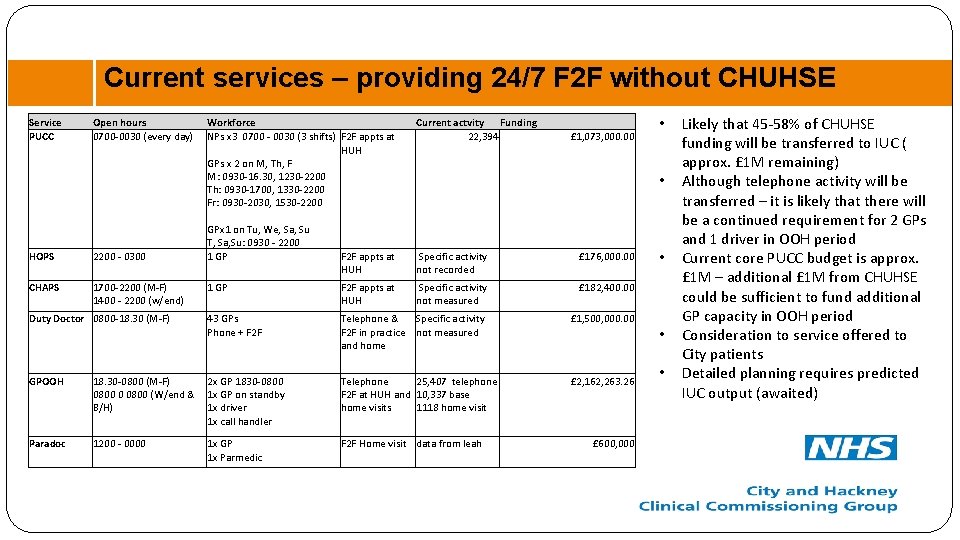
Current services – providing 24/7 F 2 F without CHUHSE Service PUCC Open hours 0700 -0030 (every day) HOPS 2200 - 0300 CHAPS 1700 -2200 (M-F) 1400 - 2200 (w/end) Workforce NPs x 3 0700 - 0030 (3 shifts) F 2 F appts at HUH GPs x 2 on M, Th, F M: 0930 -16. 30, 1230 -2200 Th: 0930 -1700, 1330 -2200 Fr: 0930 -2030, 1530 -2200 GPx 1 on Tu, We, Sa, Su T, Sa, Su: 0930 - 2200 1 GP Current actvity Funding 22, 394 £ 1, 073, 000. 00 • • F 2 F appts at HUH Specific activity not recorded £ 176, 000. 00 1 GP F 2 F appts at HUH Specific activity not measured £ 182, 400. 00 Duty Doctor 0800 -18. 30 (M-F) 43 GPs Phone + F 2 F Telephone & Specific activity F 2 F in practice not measured and home £ 1, 500, 000. 00 GPOOH 18. 30 -0800 (M-F) 0800 0 0800 (W/end & B/H) 2 x GP 1830 -0800 1 x GP on standby 1 x driver 1 x call handler Telephone 25, 407 telephone F 2 F at HUH and 10, 337 base home visits 1118 home visit £ 2, 162, 263. 26 Paradoc 1200 - 0000 1 x GP 1 x Parmedic F 2 F Home visit data from leah £ 600, 000 • • • Likely that 45 -58% of CHUHSE funding will be transferred to IUC ( approx. £ 1 M remaining) Although telephone activity will be transferred – it is likely that there will be a continued requirement for 2 GPs and 1 driver in OOH period Current core PUCC budget is approx. £ 1 M – additional £ 1 M from CHUHSE could be sufficient to fund additional GP capacity in OOH period Consideration to service offered to City patients Detailed planning requires predicted IUC output (awaited)
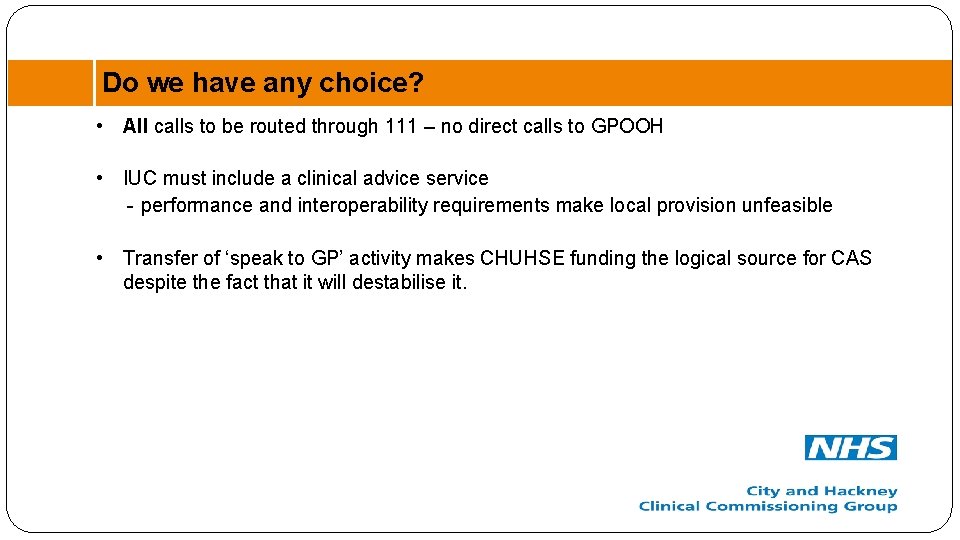
Do we have any choice? • All calls to be routed through 111 – no direct calls to GPOOH • IUC must include a clinical advice service - performance and interoperability requirements make local provision unfeasible • Transfer of ‘speak to GP’ activity makes CHUHSE funding the logical source for CAS despite the fact that it will destabilise it.
Questions ? • Do you see any other potential concerns or benefits? • Can you suggest any amendments to the proposed IUC model to minimise concerns? • Do you have any alternative proposals? - different model? - different funding? Could some funding be released from Duty Doctor as 111 will take calls in hours from Patients and HCPs? • What is your opinion on reconfiguration of existing services
Appendices
31
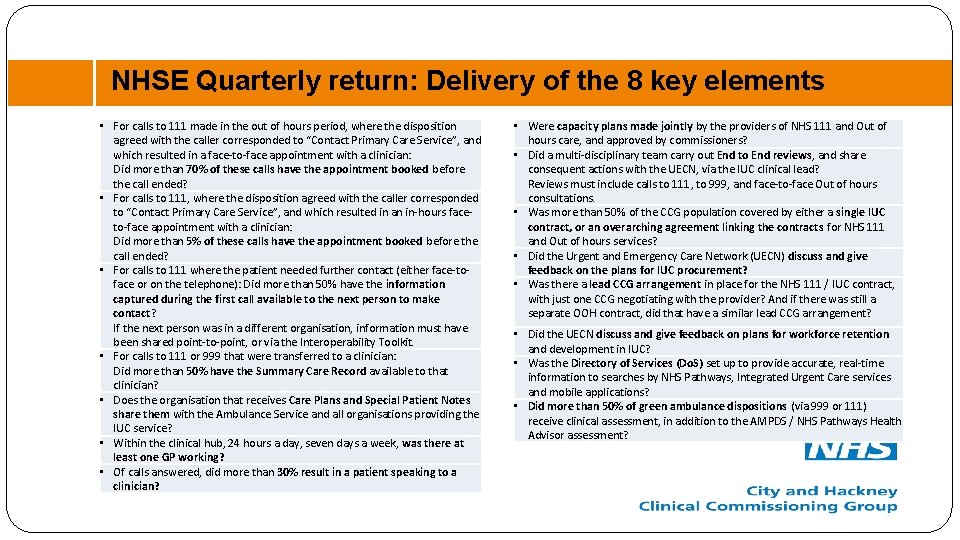
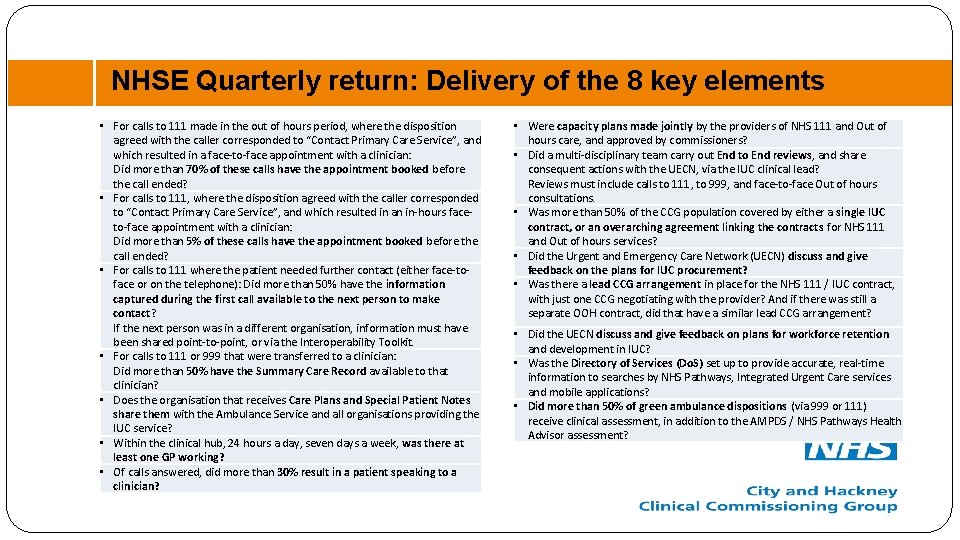
NHSE Quarterly return: Delivery of the 8 key elements • For calls to 111 made in the out of hours period, where the disposition agreed with the caller corresponded to “Contact Primary Care Service”, and which resulted in a face-to-face appointment with a clinician: Did more than 70% of these calls have the appointment booked before the call ended? • For calls to 111, where the disposition agreed with the caller corresponded to “Contact Primary Care Service”, and which resulted in an in-hours faceto-face appointment with a clinician: Did more than 5% of these calls have the appointment booked before the call ended? • For calls to 111 where the patient needed further contact (either face-toface or on the telephone): Did more than 50% have the information captured during the first call available to the next person to make contact? If the next person was in a different organisation, information must have been shared point-to-point, or via the Interoperability Toolkit. • For calls to 111 or 999 that were transferred to a clinician: Did more than 50% have the Summary Care Record available to that clinician? • Does the organisation that receives Care Plans and Special Patient Notes share them with the Ambulance Service and all organisations providing the IUC service? • Within the clinical hub, 24 hours a day, seven days a week, was there at least one GP working? • Of calls answered, did more than 30% result in a patient speaking to a clinician? • Were capacity plans made jointly by the providers of NHS 111 and Out of hours care, and approved by commissioners? • Did a multi-disciplinary team carry out End to End reviews, and share consequent actions with the UECN, via the IUC clinical lead? Reviews must include calls to 111, to 999, and face-to-face Out of hours consultations. • Was more than 50% of the CCG population covered by either a single IUC contract, or an overarching agreement linking the contracts for NHS 111 and Out of hours services? • Did the Urgent and Emergency Care Network (UECN) discuss and give feedback on the plans for IUC procurement? • Was there a lead CCG arrangement in place for the NHS 111 / IUC contract, with just one CCG negotiating with the provider? And if there was still a separate OOH contract, did that have a similar lead CCG arrangement? • Did the UECN discuss and give feedback on plans for workforce retention and development in IUC? • Was the Directory of Services (Do. S) set up to provide accurate, real-time information to searches by NHS Pathways, Integrated Urgent Care services and mobile applications? • Did more than 50% of green ambulance dispositions (via 999 or 111) receive clinical assessment, in addition to the AMPDS / NHS Pathways Health Advisor assessment?
 City and hackney recovery college
City and hackney recovery college Brent clinical commissioning group
Brent clinical commissioning group Croydon clinical commissioning group
Croydon clinical commissioning group Five stages of counseling process
Five stages of counseling process Social prescribing hackney
Social prescribing hackney Hackney population density
Hackney population density Paradoc hackney
Paradoc hackney Hackney autism service
Hackney autism service Acrt hackney
Acrt hackney Hackney adhd clinic
Hackney adhd clinic South hackney cmht
South hackney cmht New jersey space grant consortium
New jersey space grant consortium Hackney community law centre
Hackney community law centre Integrated commissioning and progress system
Integrated commissioning and progress system New york city technology forum
New york city technology forum Dementia care in bath
Dementia care in bath Commissioning cycle
Commissioning cycle Aecp army
Aecp army Commissioning cycle
Commissioning cycle Ecs commissioning
Ecs commissioning Fortis furnace commissioning sheet
Fortis furnace commissioning sheet Jwst timeline
Jwst timeline Completions commissioning management system
Completions commissioning management system C3sc
C3sc Value based commissioning
Value based commissioning Vacuum systems commissioning
Vacuum systems commissioning Power system commissioning
Power system commissioning Nihr ccf
Nihr ccf Commissioning
Commissioning Commissioning
Commissioning Aabc commissioning group
Aabc commissioning group Lidl charging points
Lidl charging points Tpc online tracking
Tpc online tracking