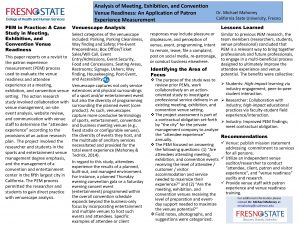
Venue Anita House North Hackney CMHT Duration 8



- Slides: 38
Venue: Anita House, North Hackney CMHT Duration : 8 sessions (24. 10. 08 – 12. 08) Duration : Group facilitators: Gulsen Huseyin, Clinical Psychologist Group facilitators: Martin Rodriguez-Tellez, Employment Coach Kerine Robertson, ST 4 Psychiatrist Michael Kabia, CPN

Who is the Group for? Those who have distressing psychotic experiences, particularly those who hear voices. A closed group comprised of service-users referred from the North and South Hackney Continuing Care CMHTs. Service-users who are not likely to feel too uncomfortable in a group setting, and feel able to actively contribute to group discussion. Service-users who are currently able to attend and listen to other group members, and think openly and flexibly about mental health issues.
What does Recovery mean? • The concept of recovery has been introduced primarily by people who have recovered from mental health experiences, rather than by mental health professionals. It means different things to different people and definitions of recovery are multiple. • Mental health recovery is a journey of healing and transformation enabling a person with a mental health problem to live a meaningful life in a community of his or her choice while striving to achieve his or her full potential. National consensus statement on mental health recovery, December 2004, US Dept of Health and Human Sciences • “…a personal process or tackling the adverse impacts of experiencing mental health problems, despite their continuing or long-term presence. It involves personal development and change. ” Leading mental health charity Rethink (Frak, 2005)
In line with; • Recommendations from the Alternative Pathways project, where service users emphasised the importance of recovery (Sandhu, 2007). • The Do. H (2008) asks services and practitioners to work according to the values and principles of a recovery approach. Numerous other policy statements and documents across the disciplines also call for mental health practitioners to promote recovery in all aspects of mental health care. • NHS mental health Trust and NICE Guideline targets to promote recovery, empowerment, social inclusion and a user-centred service (NIMHE guiding statement on recovery, 2005)
10 Fundamental Components of Recovery: • Self-direction • Individualised and Person-Centred • Empowerment • Holistic • Non-linear • Strengths-based • Peer support • Respect • Responsibility • Hope
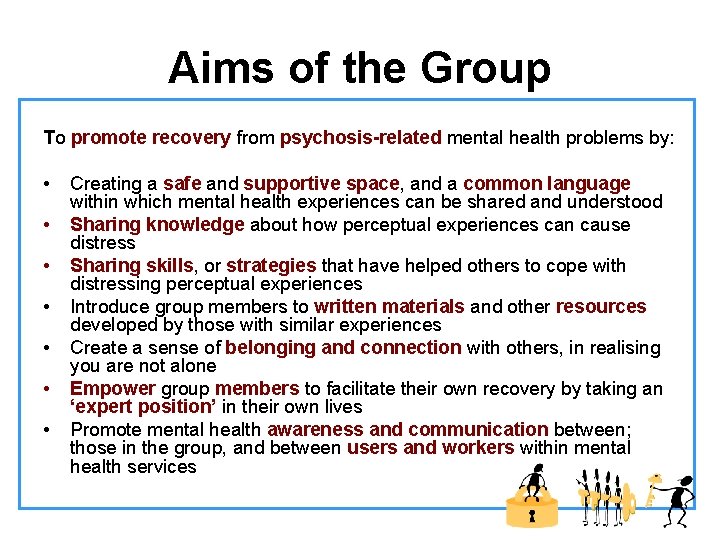
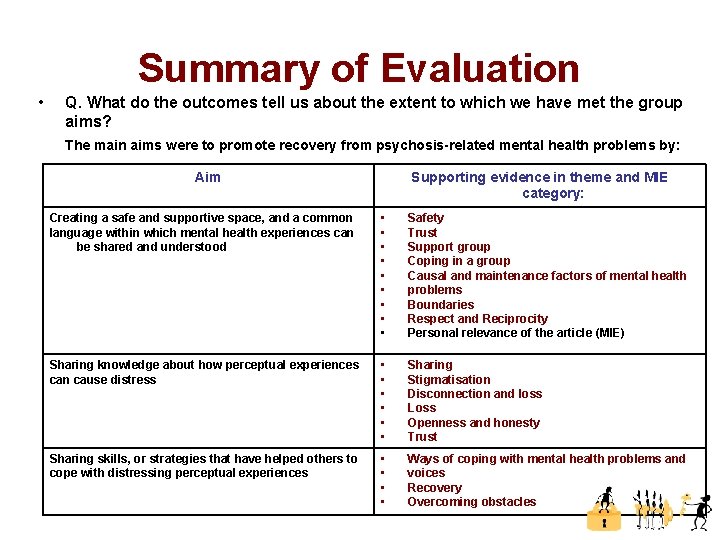
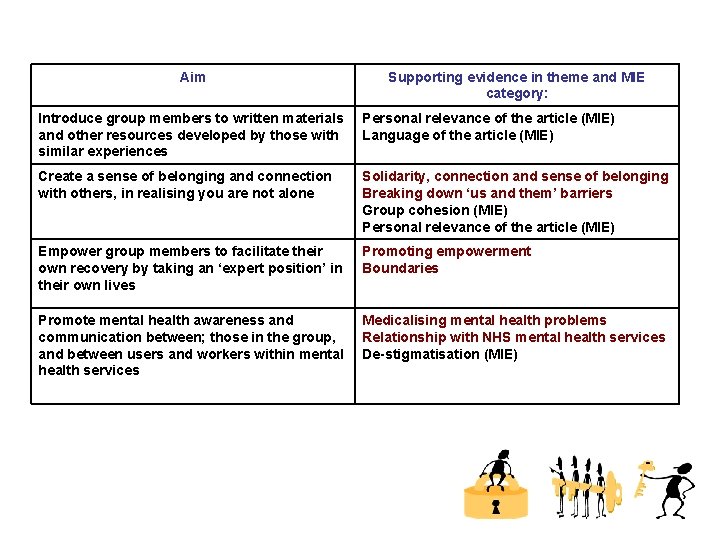
Aims of the Group To promote recovery from psychosis-related mental health problems by: • Creating a safe and supportive space, and a common language within which mental health experiences can be shared and understood • Sharing knowledge about how perceptual experiences can cause distress • Sharing skills, or strategies that have helped others to cope with distressing perceptual experiences • Introduce group members to written materials and other resources developed by those with similar experiences • Create a sense of belonging and connection with others, in realising you are not alone • Empower group members to facilitate their own recovery by taking an ‘expert position’ in their own lives • Promote mental health awareness and communication between; those in the group, and between users and workers within mental health services

Narrative Therapy Ø Draws on aspects of Narrative Therapy (Michael White and David Epston, 1990 s) – Aims to be non or anti-pathologising. No position held on the causes of problems, instead the focus is on ‘unique outcomes’ and ‘what works’. – Options are made invisible by the ‘dominant narrative’, and therefore need to be made visible by developing and re-constructing a preferred, more freeing narrative. – Undermines sense of failure and paves the way for co-operation in struggle against an external problem (the problem, not the person is the problem). Ø Promoting recovery using Narrative Therapy “One aspect of facilitating recovery may involve hearing the stories people have to tell and accepting their own words and terminology, thus creating a space for dialogue and exploration that can further understanding”. (Dillon and May, 2002)
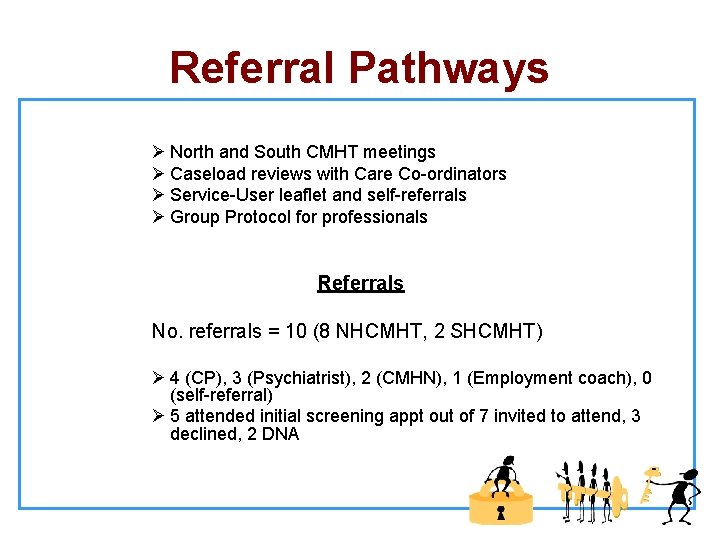
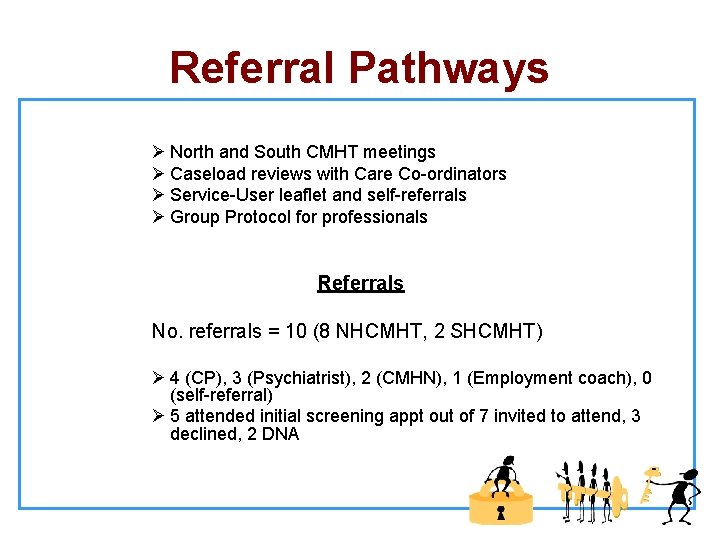
Referral Pathways Ø North and South CMHT meetings Ø Caseload reviews with Care Co-ordinators Ø Service-User leaflet and self-referrals Ø Group Protocol for professionals Referrals No. referrals = 10 (8 NHCMHT, 2 SHCMHT) Ø 4 (CP), 3 (Psychiatrist), 2 (CMHN), 1 (Employment coach), 0 (self-referral) Ø 5 attended initial screening appt out of 7 invited to attend, 3 declined, 2 DNA
Resources needed Ø Service User authored article – Power to Our Journeys. An Exploration of an alternative community mental health project. Dulwich Centre Newsletter, 1997 No. 1 Ø Flipchart board with A 1 poster paper and mixture of chunky and thin felt pens for group/poster exercises Ø Copies of Mindfulness of Breath exercise
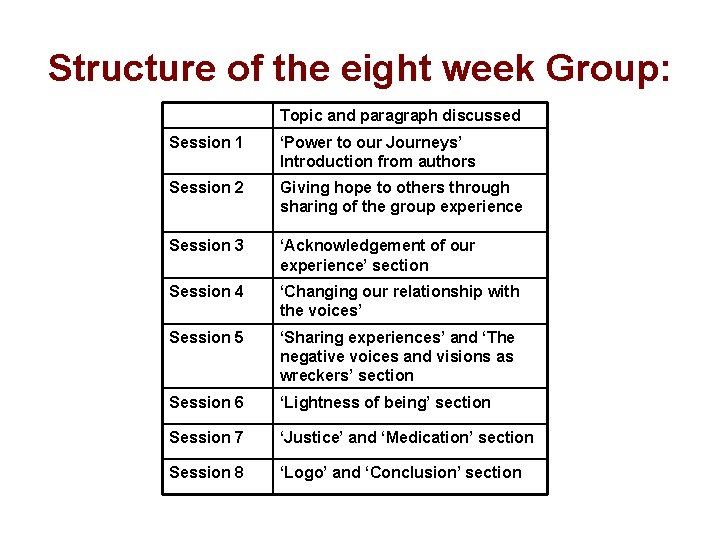
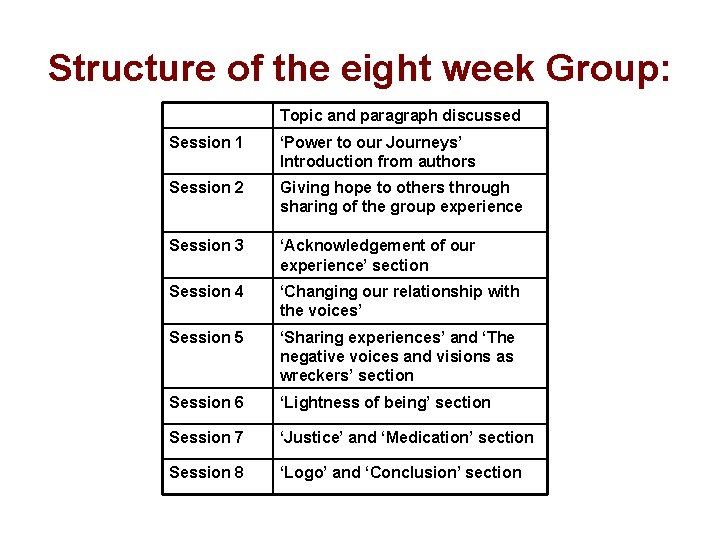
Structure of the eight week Group: Topic and paragraph discussed Session 1 ‘Power to our Journeys’ Introduction from authors Session 2 Giving hope to others through sharing of the group experience Session 3 ‘Acknowledgement of our experience’ section Session 4 ‘Changing our relationship with the voices’ Session 5 ‘Sharing experiences’ and ‘The negative voices and visions as wreckers’ section Session 6 ‘Lightness of being’ section Session 7 ‘Justice’ and ‘Medication’ section Session 8 ‘Logo’ and ‘Conclusion’ section
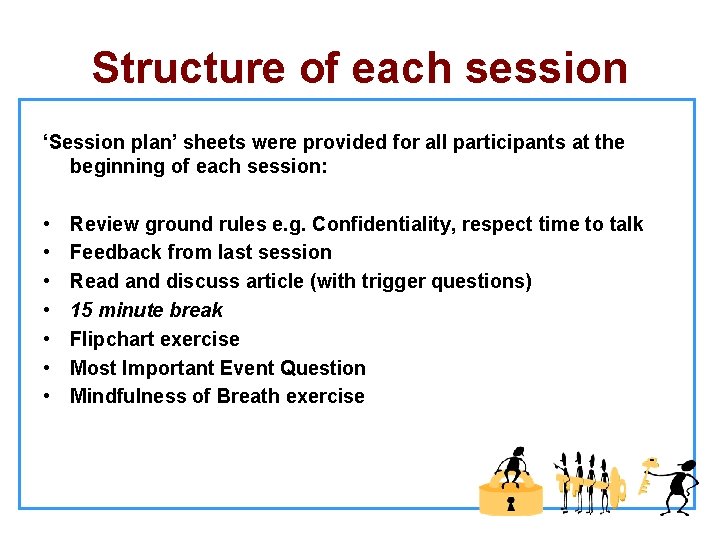
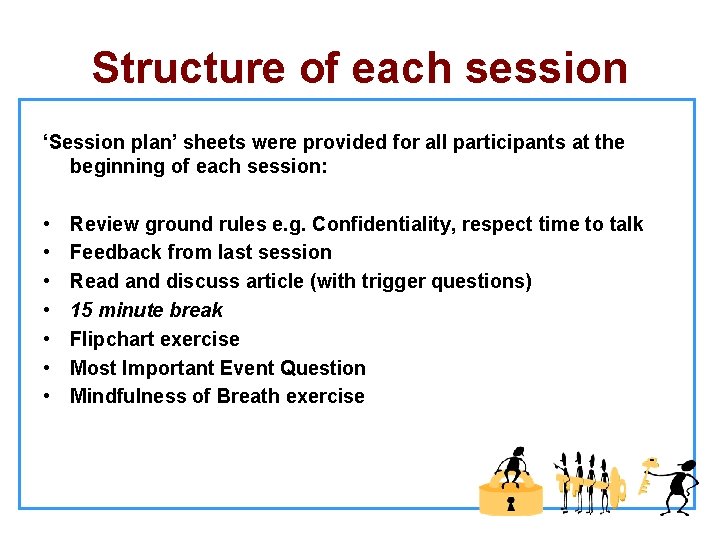
Structure of each session ‘Session plan’ sheets were provided for all participants at the beginning of each session: • Review ground rules e. g. Confidentiality, respect time to talk • Feedback from last session • Read and discuss article (with trigger questions) • 15 minute break • Flipchart exercise • Most Important Event Question • Mindfulness of Breath exercise
Flipchart Exercises Advantages and disadvantages of: • Sharing with others • Stepping outside of the expectations of others
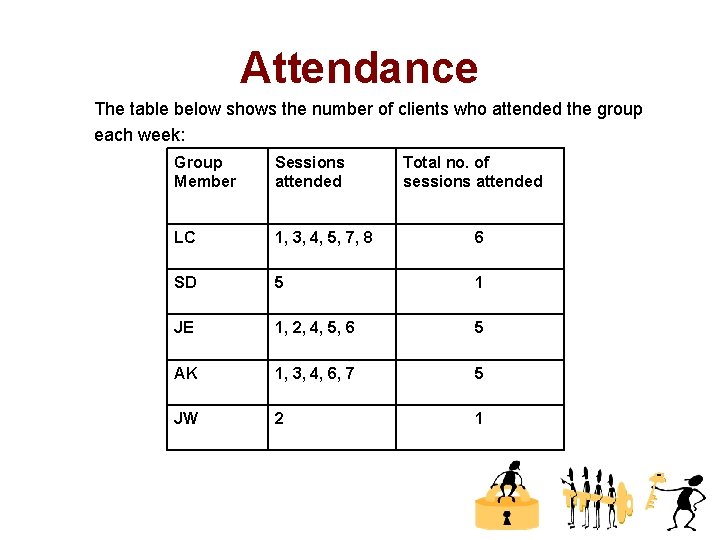
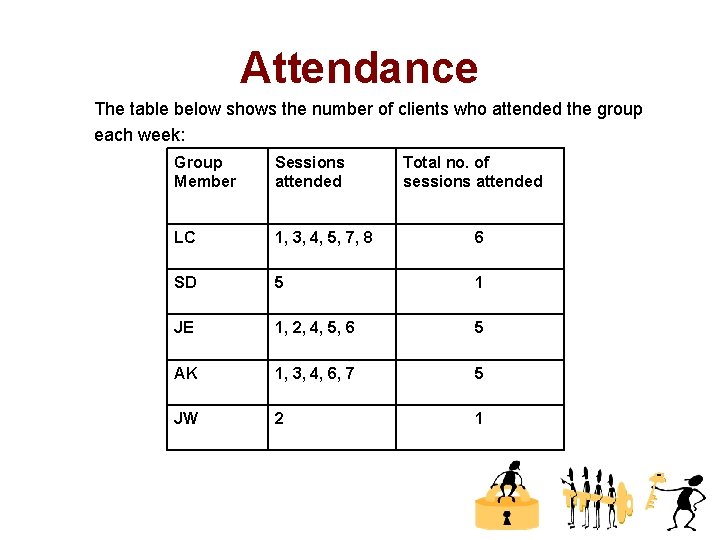
Attendance The table below shows the number of clients who attended the group each week: Group Member Sessions attended Total no. of sessions attended LC 1, 3, 4, 5, 7, 8 6 SD 5 1 JE 1, 2, 4, 5, 6 5 AK 1, 3, 4, 6, 7 5 JW 2 1
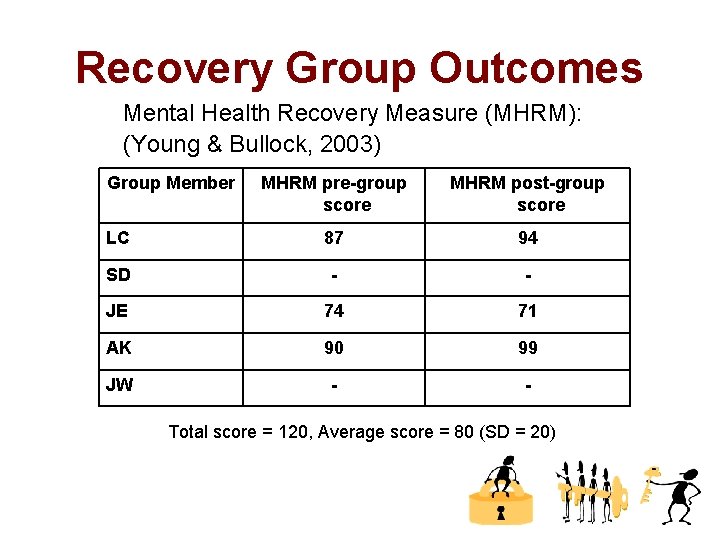
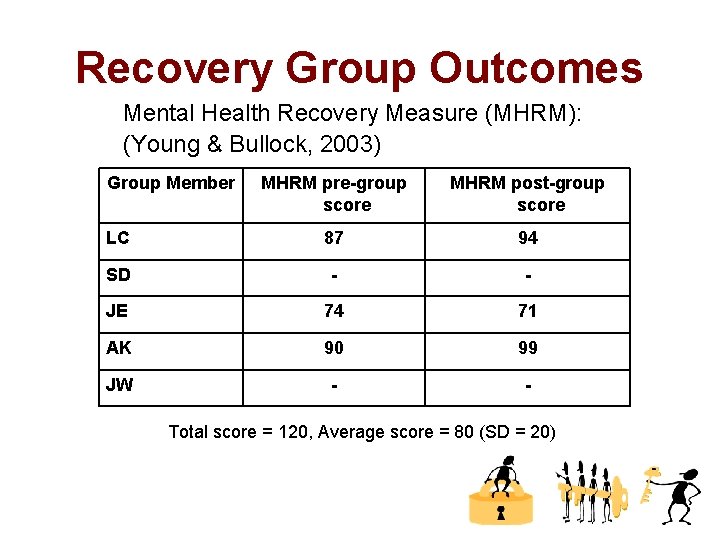
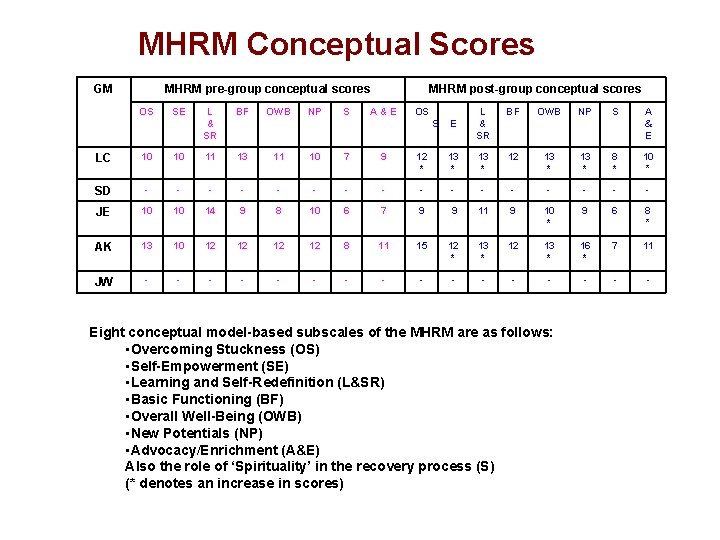
Recovery Group Outcomes Mental Health Recovery Measure (MHRM): (Young & Bullock, 2003) Group Member MHRM pre-group score MHRM post-group score LC 87 94 SD - - JE 74 71 AK 90 99 JW - - Total score = 120, Average score = 80 (SD = 20)
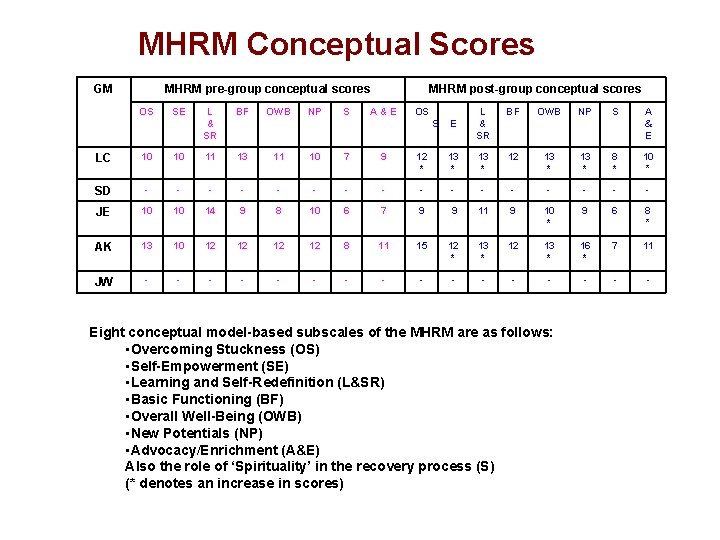
MHRM Conceptual Scores GM MHRM pre-group conceptual scores OS SE L & SR BF OWB NP S MHRM post-group conceptual scores A & E OS S L & SR BF OWB NP S E A & E LC 10 10 11 13 11 10 7 9 12 * 13 * 12 13 * 8 * 10 * SD - - - - JE 10 10 14 9 8 10 6 7 9 9 11 9 10 * 9 6 8 * AK 13 10 12 12 8 11 15 12 * 13 * 12 13 * 16 * 7 11 JW - - - - Eight conceptual model-based subscales of the MHRM are as follows: • Overcoming Stuckness (OS) • Self-Empowerment (SE) • Learning and Self-Redefinition (L&SR) • Basic Functioning (BF) • Overall Well-Being (OWB) • New Potentials (NP) • Advocacy/Enrichment (A&E) Also the role of ‘Spirituality’ in the recovery process (S) (* denotes an increase in scores)

Qualitative Outcome Data
Thematic Analysis of Post-group facilitator notes
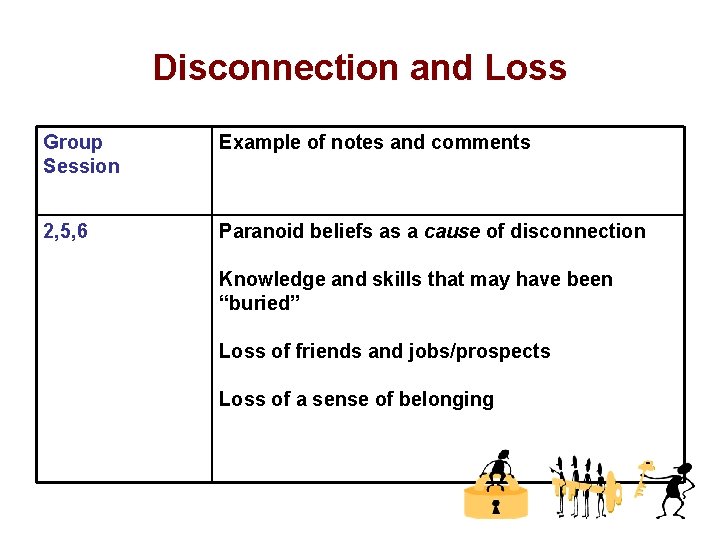
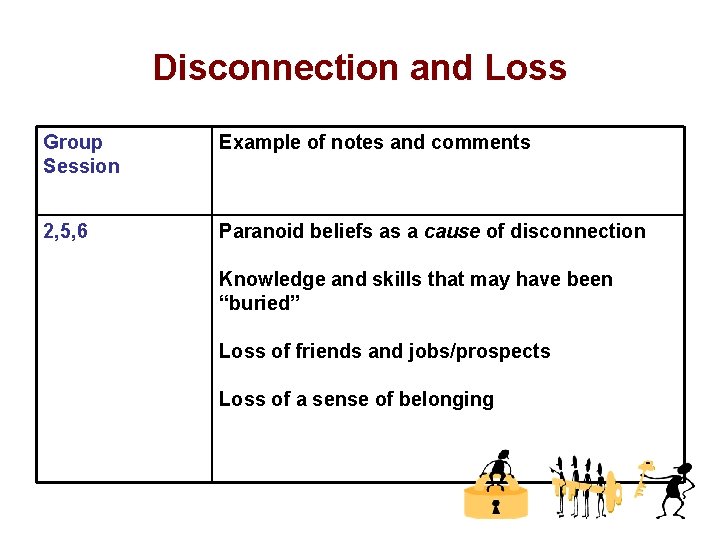
Disconnection and Loss Group Session Example of notes and comments 2, 5, 6 Paranoid beliefs as a cause of disconnection Knowledge and skills that may have been “buried” Loss of friends and jobs/prospects Loss of a sense of belonging
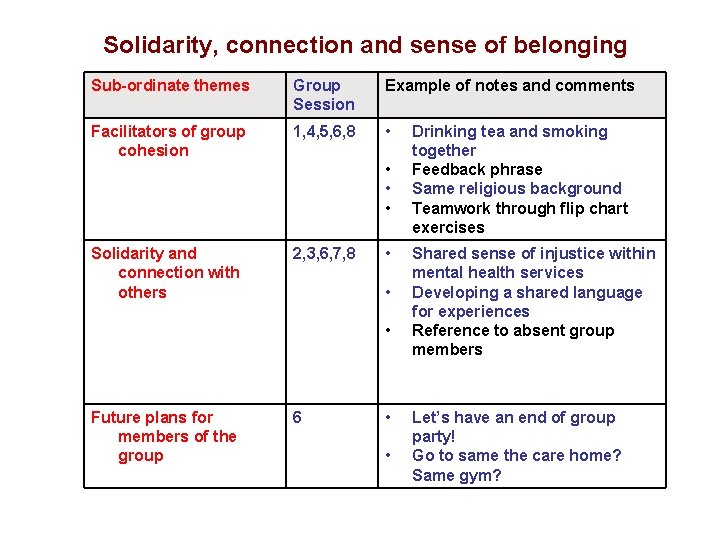
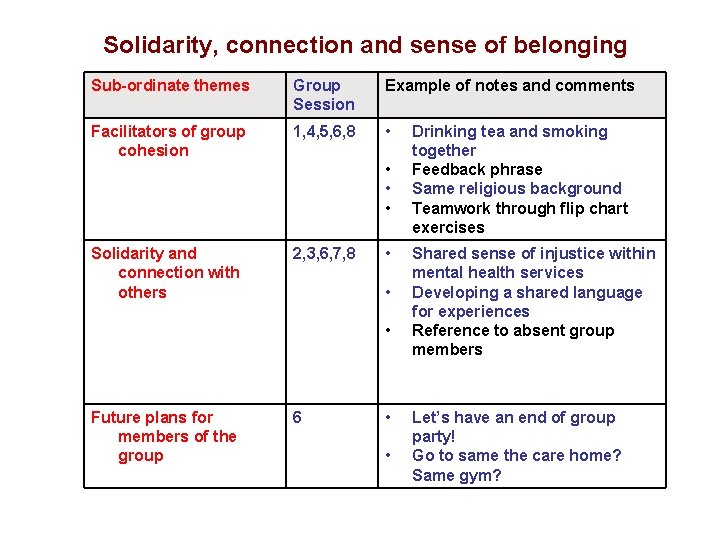
Solidarity, connection and sense of belonging Sub-ordinate themes Group Session Example of notes and comments Facilitators of group cohesion 1, 4, 5, 6, 8 • • Solidarity and connection with others 2, 3, 6, 7, 8 • • • Future plans for members of the group 6 • • Drinking tea and smoking together Feedback phrase Same religious background Teamwork through flip chart exercises Shared sense of injustice within mental health services Developing a shared language for experiences Reference to absent group members Let’s have an end of group party! Go to same the care home? Same gym?
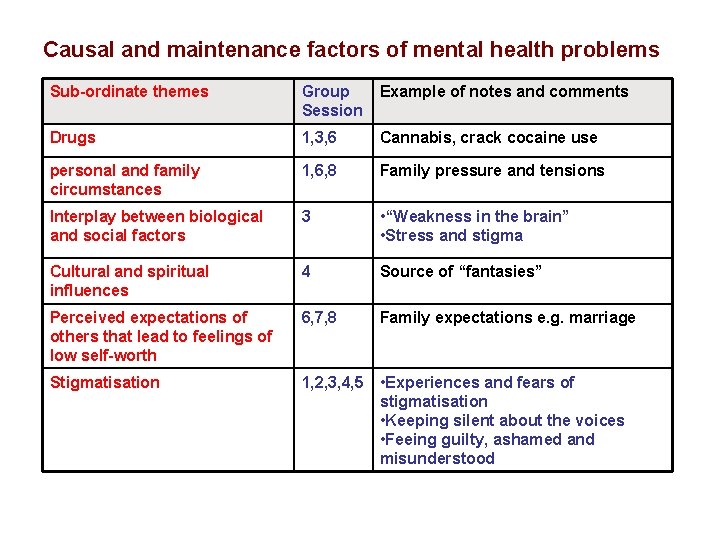
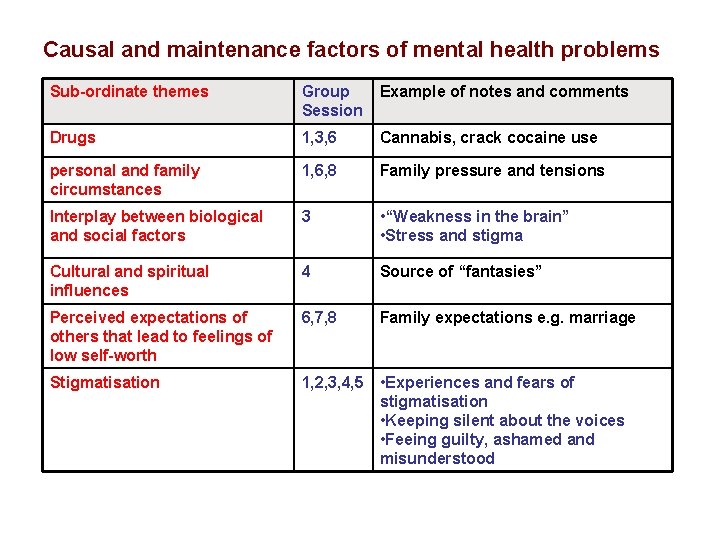
Causal and maintenance factors of mental health problems Sub-ordinate themes Group Session Example of notes and comments Drugs 1, 3, 6 Cannabis, crack cocaine use personal and family circumstances 1, 6, 8 Family pressure and tensions Interplay between biological and social factors 3 • “Weakness in the brain” • Stress and stigma Cultural and spiritual influences 4 Source of “fantasies” Perceived expectations of others that lead to feelings of low self-worth 6, 7, 8 Family expectations e. g. marriage Stigmatisation 1, 2, 3, 4, 5 • Experiences and fears of stigmatisation • Keeping silent about the voices • Feeing guilty, ashamed and misunderstood
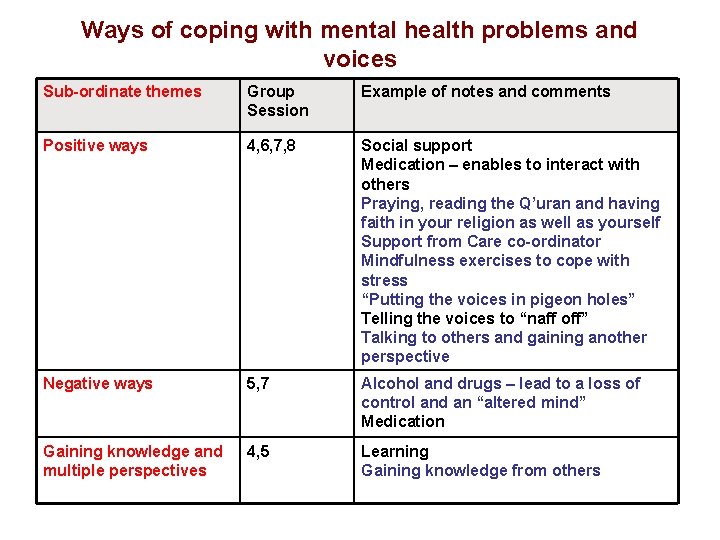
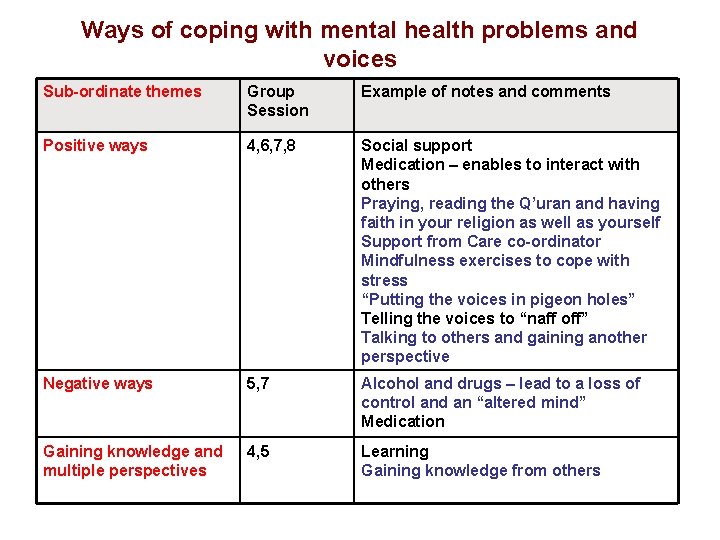
Ways of coping with mental health problems and voices Sub-ordinate themes Group Session Example of notes and comments Positive ways 4, 6, 7, 8 Social support Medication – enables to interact with others Praying, reading the Q’uran and having faith in your religion as well as yourself Support from Care co-ordinator Mindfulness exercises to cope with stress “Putting the voices in pigeon holes” Telling the voices to “naff off” Talking to others and gaining another perspective Negative ways 5, 7 Alcohol and drugs – lead to a loss of control and an “altered mind” Medication Gaining knowledge and multiple perspectives 4, 5 Learning Gaining knowledge from others
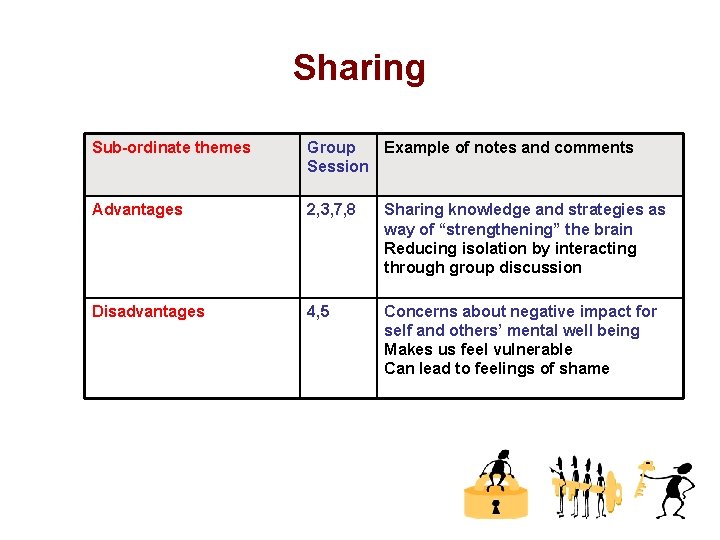
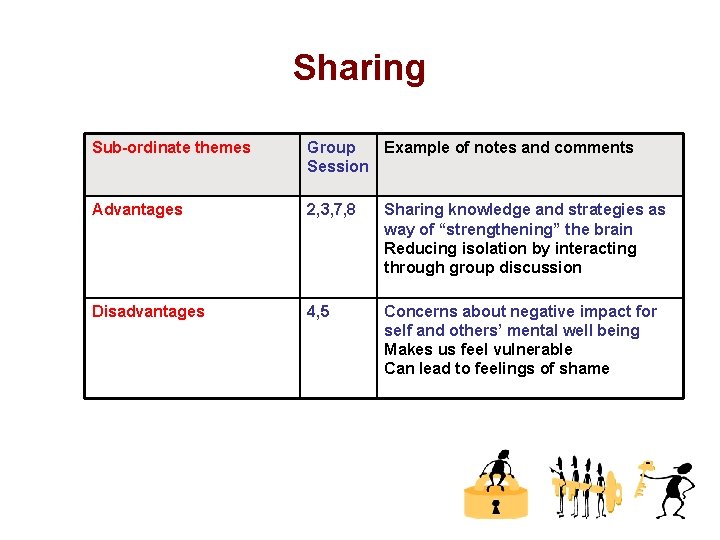
Sharing Sub-ordinate themes Group Example of notes and comments Session Advantages 2, 3, 7, 8 Sharing knowledge and strategies as way of “strengthening” the brain Reducing isolation by interacting through group discussion Disadvantages 4, 5 Concerns about negative impact for self and others’ mental well being Makes us feel vulnerable Can lead to feelings of shame
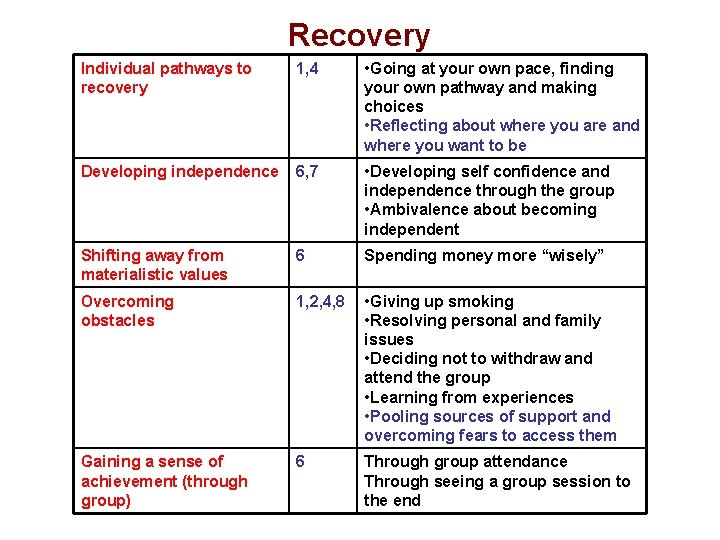
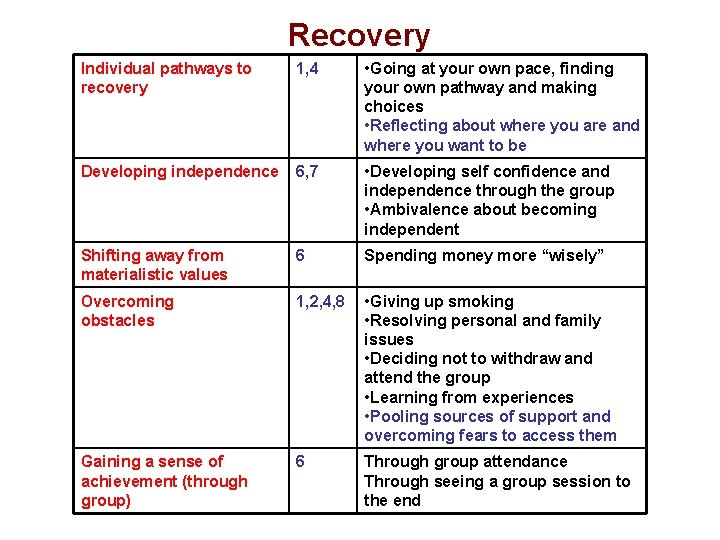
Recovery Individual pathways to recovery 1, 4 • Going at your own pace, finding your own pathway and making choices • Reflecting about where you are and where you want to be Developing independence 6, 7 • Developing self confidence and independence through the group • Ambivalence about becoming independent Shifting away from materialistic values 6 Spending money more “wisely” Overcoming obstacles 1, 2, 4, 8 • Giving up smoking • Resolving personal and family issues • Deciding not to withdraw and attend the group • Learning from experiences • Pooling sources of support and overcoming fears to access them Gaining a sense of achievement (through group) 6 Through group attendance Through seeing a group session to the end
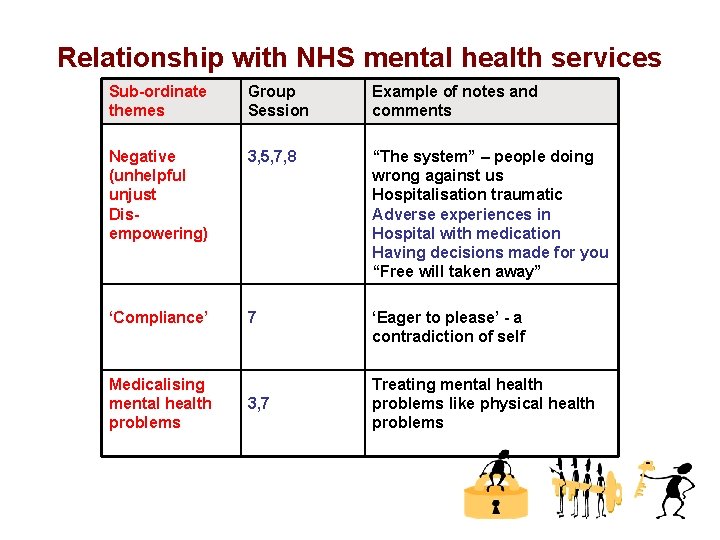
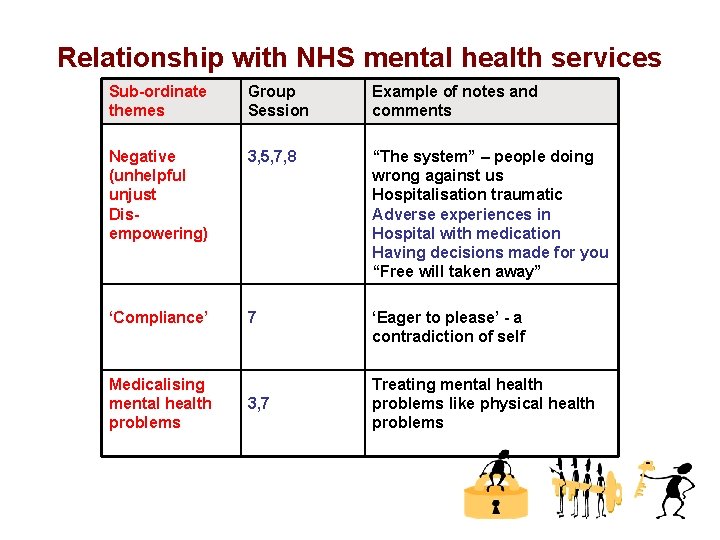
Relationship with NHS mental health services Sub-ordinate themes Group Session Example of notes and comments Negative (unhelpful unjust Disempowering) 3, 5, 7, 8 “The system” – people doing wrong against us Hospitalisation traumatic Adverse experiences in Hospital with medication Having decisions made for you “Free will taken away” ‘Compliance’ 7 ‘Eager to please’ - a contradiction of self Medicalising mental health problems 3, 7 Treating mental health problems like physical health problems
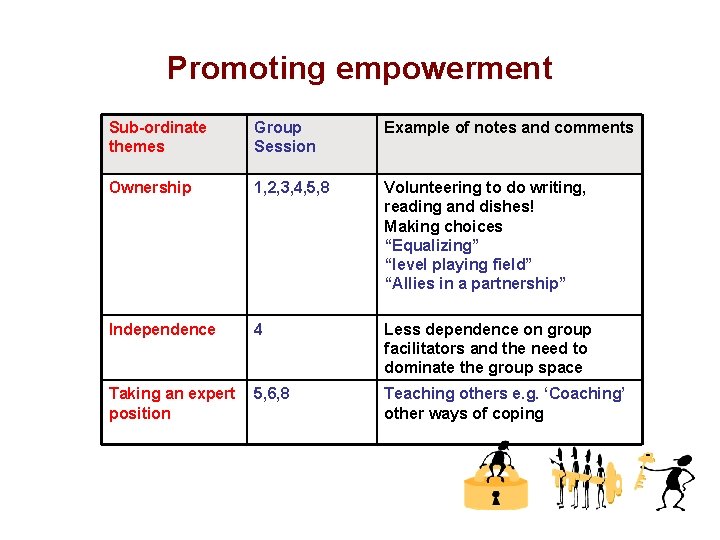
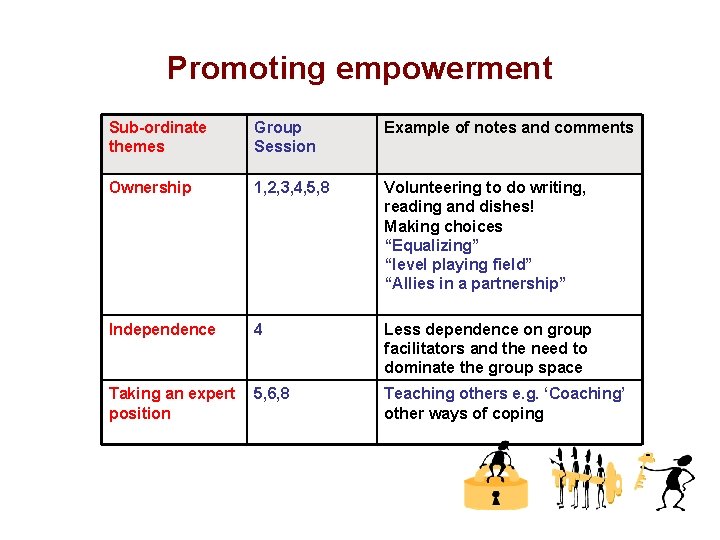
Promoting empowerment Sub-ordinate themes Group Session Example of notes and comments Ownership 1, 2, 3, 4, 5, 8 Volunteering to do writing, reading and dishes! Making choices “Equalizing” “level playing field” “Allies in a partnership” Independence 4 Less dependence on group facilitators and the need to dominate the group space Taking an expert 5, 6, 8 position Teaching others e. g. ‘Coaching’ other ways of coping
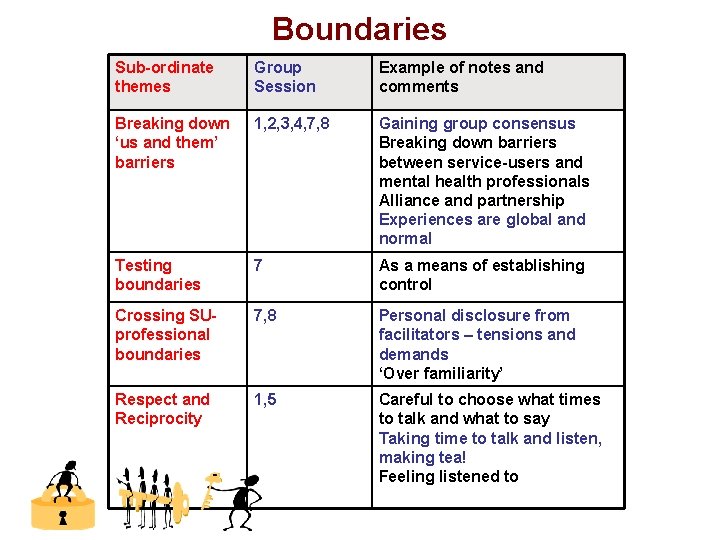
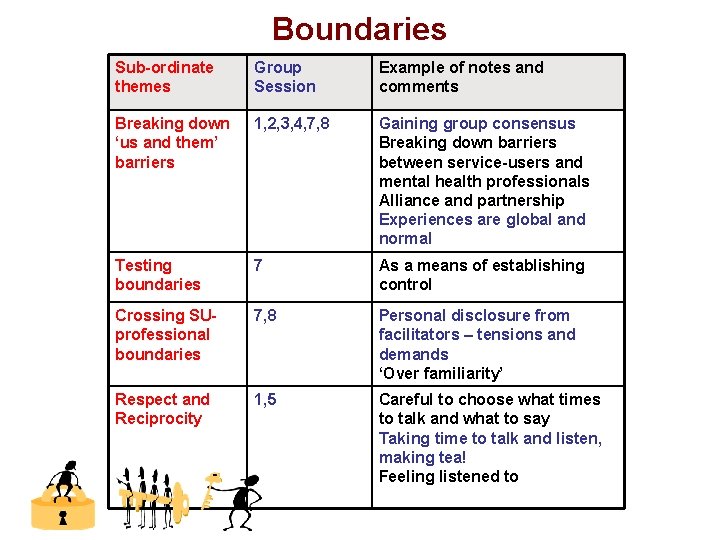
Boundaries Sub-ordinate themes Group Session Example of notes and comments Breaking down ‘us and them’ barriers 1, 2, 3, 4, 7, 8 Gaining group consensus Breaking down barriers between service-users and mental health professionals Alliance and partnership Experiences are global and normal Testing boundaries 7 As a means of establishing control Crossing SUprofessional boundaries 7, 8 Personal disclosure from facilitators – tensions and demands ‘Over familiarity’ Respect and Reciprocity 1, 5 Careful to choose what times to talk and what to say Taking time to talk and listen, making tea! Feeling listened to
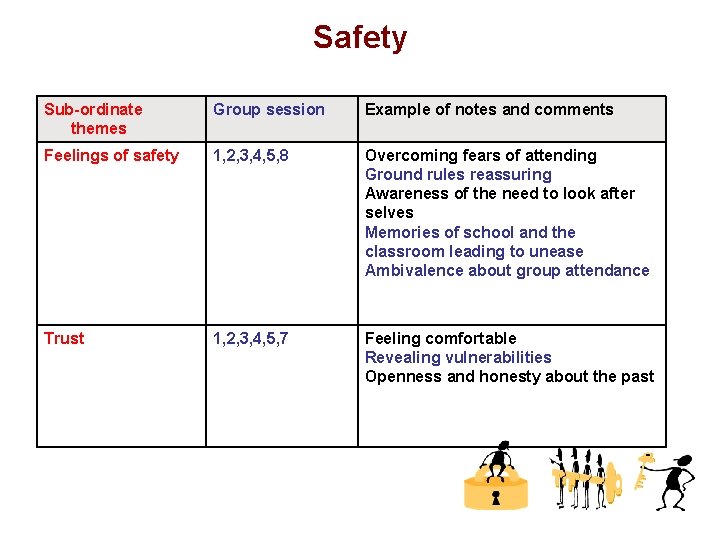
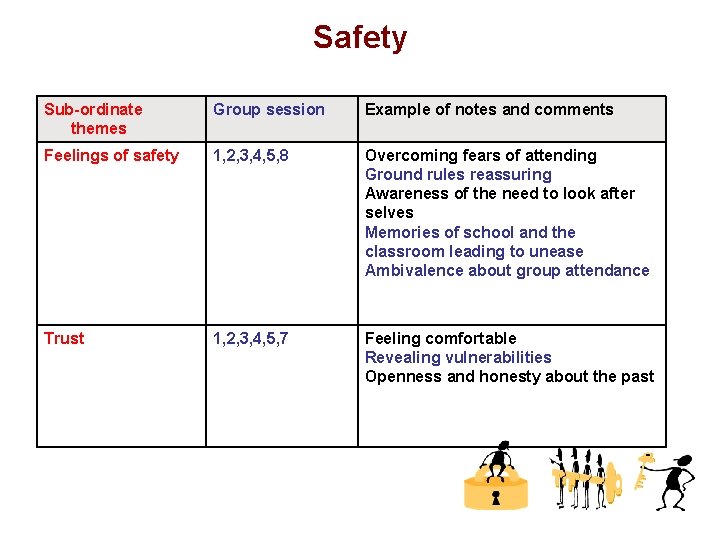
Safety Sub-ordinate themes Group session Example of notes and comments Feelings of safety 1, 2, 3, 4, 5, 8 Overcoming fears of attending Ground rules reassuring Awareness of the need to look after selves Memories of school and the classroom leading to unease Ambivalence about group attendance Trust 1, 2, 3, 4, 5, 7 Feeling comfortable Revealing vulnerabilities Openness and honesty about the past
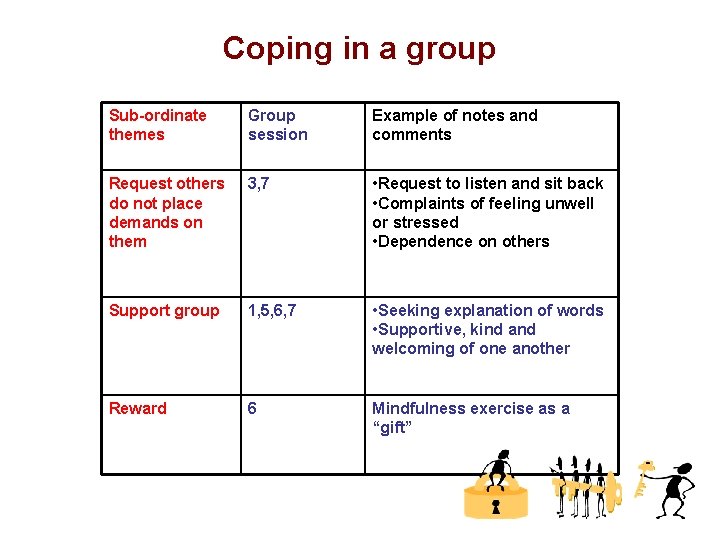
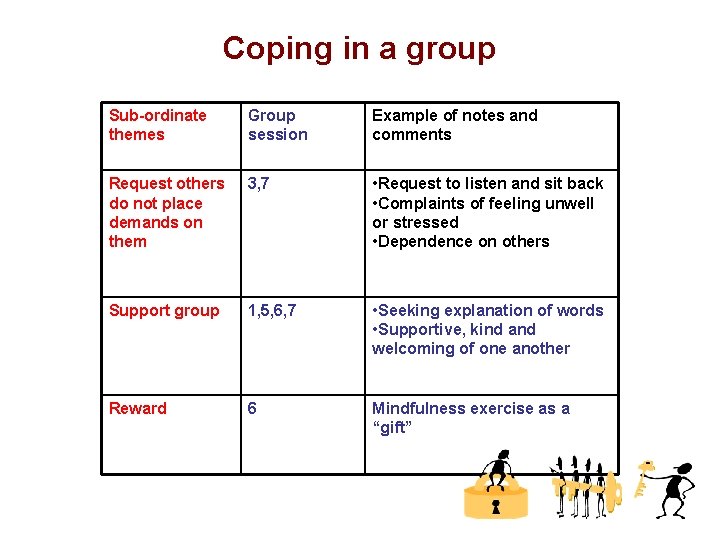
Coping in a group Sub-ordinate themes Group session Example of notes and comments Request others do not place demands on them 3, 7 • Request to listen and sit back • Complaints of feeling unwell or stressed • Dependence on others Support group 1, 5, 6, 7 • Seeking explanation of words • Supportive, kind and welcoming of one another Reward 6 Mindfulness exercise as a “gift”
Most Important Event Question: Of the events that occurred this session, which one do you think was the most important for you personally? Why was it so important for you?
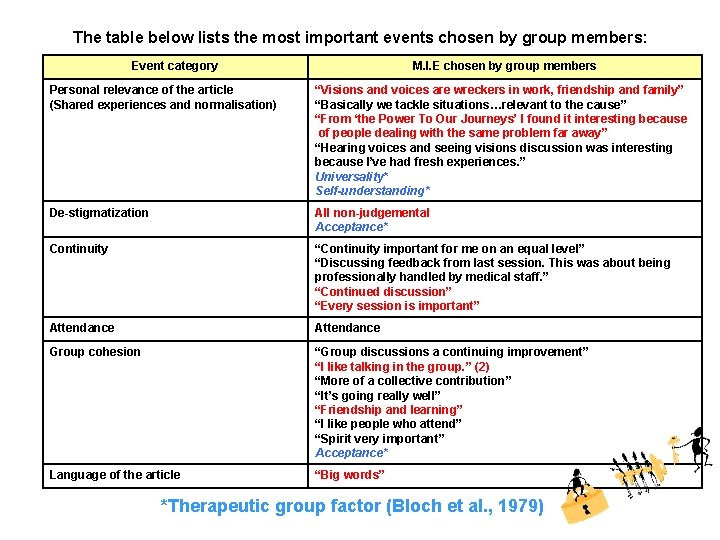
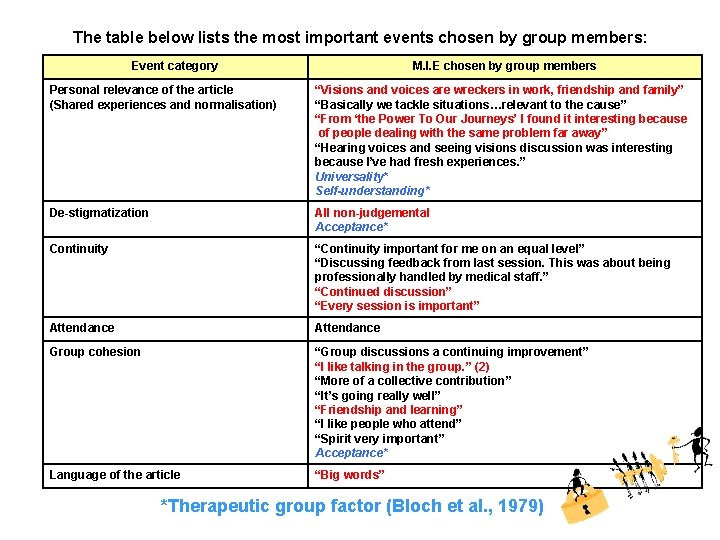
The table below lists the most important events chosen by group members: Event category M. I. E chosen by group members Personal relevance of the article (Shared experiences and normalisation) “Visions and voices are wreckers in work, friendship and family” “Basically we tackle situations…relevant to the cause” “From ‘the Power To Our Journeys’ I found it interesting because of people dealing with the same problem far away” “Hearing voices and seeing visions discussion was interesting because I’ve had fresh experiences. ” Universality* Self-understanding* De-stigmatization All non-judgemental Acceptance* Continuity “Continuity important for me on an equal level” “Discussing feedback from last session. This was about being professionally handled by medical staff. ” “Continued discussion” “Every session is important” Attendance Group cohesion “Group discussions a continuing improvement” “I like talking in the group. ” (2) “More of a collective contribution” “It’s going really well” “Friendship and learning” “I like people who attend” “Spirit very important” Acceptance* Language of the article “Big words” *Therapeutic group factor (Bloch et al. , 1979)
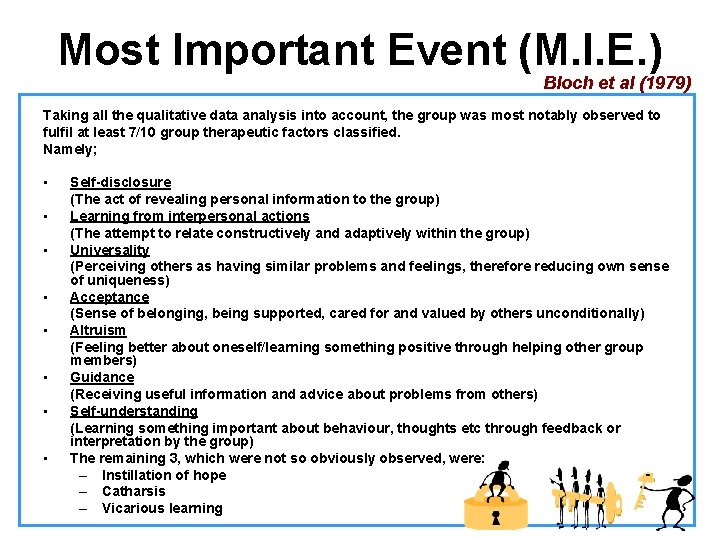
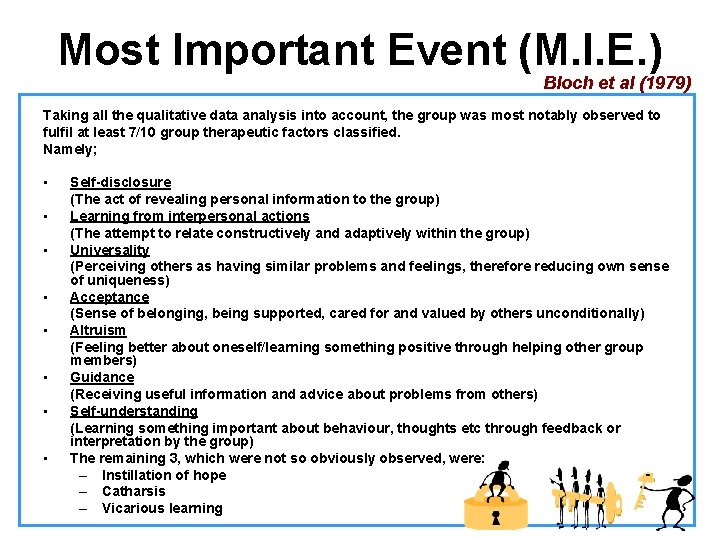
Most Important Event (M. I. E. ) Bloch et al (1979) Taking all the qualitative data analysis into account, the group was most notably observed to fulfil at least 7/10 group therapeutic factors classified. Namely; • Self-disclosure (The act of revealing personal information to the group) • Learning from interpersonal actions (The attempt to relate constructively and adaptively within the group) • Universality (Perceiving others as having similar problems and feelings, therefore reducing own sense of uniqueness) • Acceptance (Sense of belonging, being supported, cared for and valued by others unconditionally) • Altruism (Feeling better about oneself/learning something positive through helping other group members) • Guidance (Receiving useful information and advice about problems from others) • Self-understanding (Learning something important about behaviour, thoughts etc through feedback or interpretation by the group) • The remaining 3, which were not so obviously observed, were: – Instillation of hope – Catharsis – Vicarious learning
What came after… Ø Therapeutic letters (a therapeutic document) • A document of knowledge and affirmation • Helpful when people are in danger of losing their preferred identities (consolidating the subjugated narrative they have developed) • Useful in stressful situations when people are most likely to forget the knowledge and skills that they have acquired Ø Follow-up appointments to develop a recovery plan
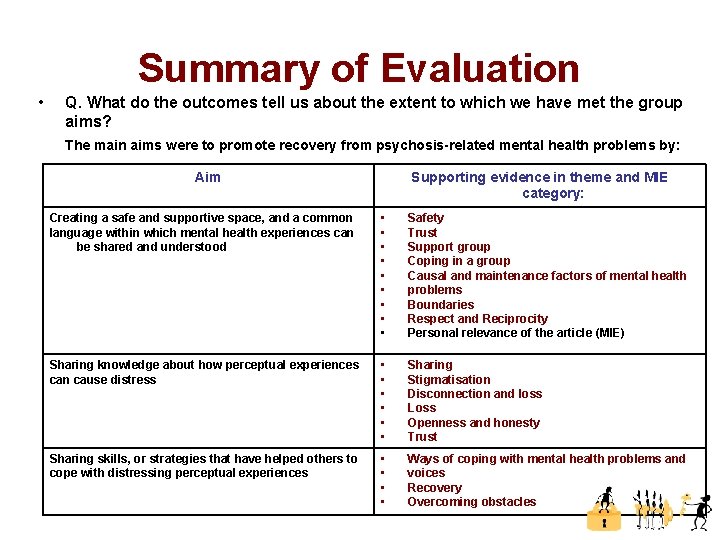
Summary of Evaluation • Q. What do the outcomes tell us about the extent to which we have met the group aims? The main aims were to promote recovery from psychosis-related mental health problems by: Aim Supporting evidence in theme and MIE category: Creating a safe and supportive space, and a common language within which mental health experiences can be shared and understood • • • Safety Trust Support group Coping in a group Causal and maintenance factors of mental health problems Boundaries Respect and Reciprocity Personal relevance of the article (MIE) Sharing knowledge about how perceptual experiences can cause distress • • • Sharing Stigmatisation Disconnection and loss Loss Openness and honesty Trust Sharing skills, or strategies that have helped others to cope with distressing perceptual experiences • • Ways of coping with mental health problems and voices Recovery Overcoming obstacles
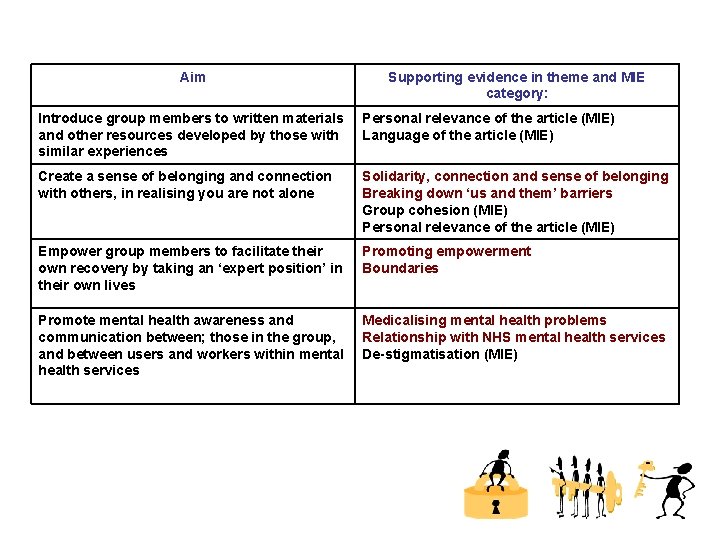
Aim Supporting evidence in theme and MIE category: Introduce group members to written materials and other resources developed by those with similar experiences Personal relevance of the article (MIE) Language of the article (MIE) Create a sense of belonging and connection with others, in realising you are not alone Solidarity, connection and sense of belonging Breaking down ‘us and them’ barriers Group cohesion (MIE) Personal relevance of the article (MIE) Empower group members to facilitate their own recovery by taking an ‘expert position’ in their own lives Promoting empowerment Boundaries Promote mental health awareness and communication between; those in the group, and between users and workers within mental health services Medicalising mental health problems Relationship with NHS mental health services De-stigmatisation (MIE)
Recommendations Ø More referrals for bigger groups Ø Use non-verbal materials produced by service-users e. g. DVDs. Art, photos to tap into peoples’ different strengths. Ø Ensure goodness of fit between materials and group members i. e. level of educational attainment, concentration and attention Ø Move beyond psychosis to include recovery from other severe and enduring mental health problems e. g. those diagnosed with BPAD Ø Promoting wider use of a ‘recovery-based’ approach by continually involving non-psychologists as co-facilitators. Ideally these should be permanent CMHT workers so that the skills and knowledge stay within the service.
Future Possibilities… Ø Recruit service-users as paid co-facilitators • Possible funding via the ‘Florid’ Organisation? Ø Increase access to the recovery group for others, including; • Non-English speaking service-users and other ethnic minority groups (in line with the Delivering Race Equality initiative in mental health care; DRE, Do. H, 2005). • Those in other Hackney mental health services e. g. AOS, Rehab & Recovery Team? Voluntary Sector services? • Open up to other boroughs within the trust? February 2009
Members Said… • By sharing our experiences we gain knowledge of our • • conditions Contact with mental health staff is useful but it must be ‘professionally’ handled To understand make time to find out about a person’s background and history Team work, positive sharing, positive outcome Bridging the gap between mental health professionals and people’s understanding of mental health experiences and problems Being aware of sources of support, overcoming fear, and finding confidence to access support
Contact gulsen. huseyin@eastlondon. nhs. uk martin. rodriguez-tellez@eastlondon. nhs. uk
 South hackney cmht
South hackney cmht Organization building venue
Organization building venue Jurisdiction vs venue
Jurisdiction vs venue Event
Event Proposal venue
Proposal venue L'heure est venue ou les vrais adorateurs
L'heure est venue ou les vrais adorateurs Swot analysis event planning
Swot analysis event planning 5 importance of work immersion
5 importance of work immersion Awareness session invitation
Awareness session invitation Contoh layout usaha
Contoh layout usaha National gallery venue hire
National gallery venue hire Jurisdiction vs venue
Jurisdiction vs venue Parys conference venue
Parys conference venue Venue readiness
Venue readiness Stages of counseling
Stages of counseling City and hackney recovery college
City and hackney recovery college Hackney adhd clinic
Hackney adhd clinic Paradoc hackney
Paradoc hackney Richard hackney
Richard hackney Social prescribing hackney
Social prescribing hackney Hackney autism service
Hackney autism service Hackney community law centre
Hackney community law centre Hackney population density
Hackney population density Acrt hackney
Acrt hackney True north vs magnetic north
True north vs magnetic north Cumbria and north east ics
Cumbria and north east ics Lesson quiz 14-1 north and south
Lesson quiz 14-1 north and south The north pole ____ a latitude of 90 degrees north
The north pole ____ a latitude of 90 degrees north Elevation map mathematical literacy
Elevation map mathematical literacy Gad4d
Gad4d Banished boarding house
Banished boarding house Acceptance houses meaning
Acceptance houses meaning My house shall be called
My house shall be called They went house to house
They went house to house Snug bugs home
Snug bugs home Reducing project duration examples
Reducing project duration examples Glyxmbi
Glyxmbi Ieee membership duration
Ieee membership duration Project duration
Project duration