City and Hackney Falls Pathway Manpreet Sahemey GP





- Slides: 21
City and Hackney Falls Pathway Manpreet Sahemey - GP Clinical Lead for Urgent Care Dr Deblina Dasgupta and Dr Carlo Prina Consultants in Acute and Geriatric Medicine
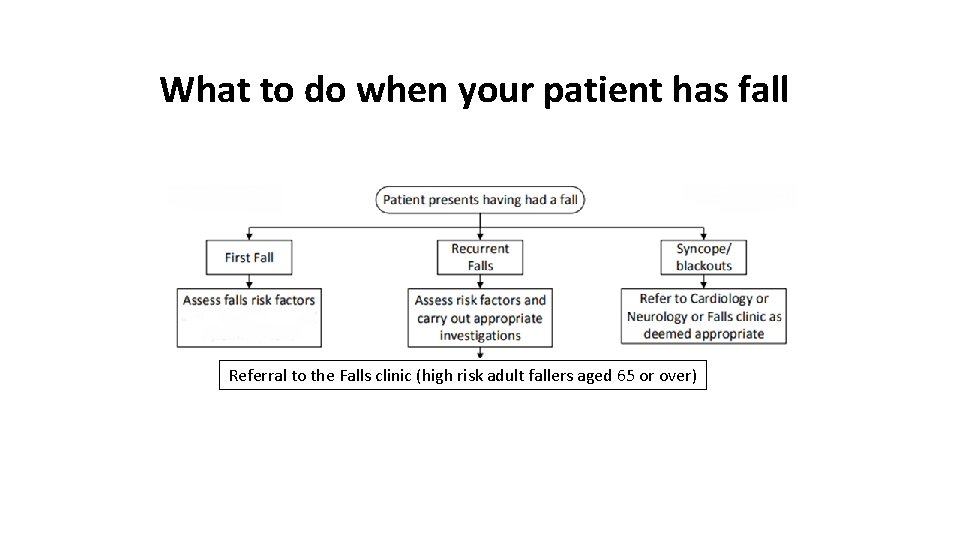
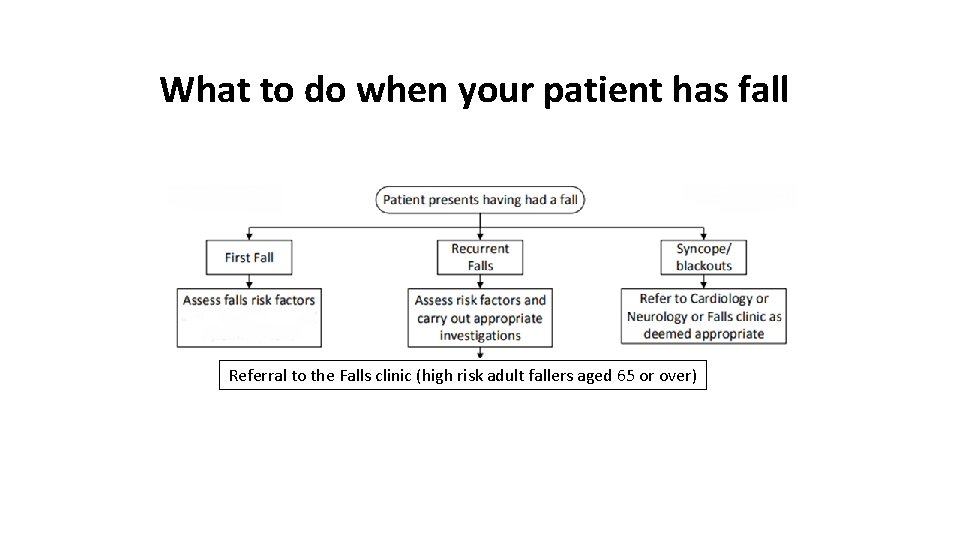
What to do when your patient has fall Referral to the Falls clinic (high risk adult fallers aged 65 or over)
Why refer to the Falls clinic? • For ‘high risk’ adult fallers aged 65 or over • For those with a high risk of falls or recurrent unexplained falls (2+ in one year) • Patient would benefit from an evidence-based strength and balance group (strong and steady exercise group) but needs a medical review first • Underlying the falls, the patient may have multiple medical problems which would benefit from a Geriatrician assessment
A falls risk assessment should be carried out in all adults aged over 65 who present with • • A fall in the community or recurrent falls Are at high risk of falls Report difficulties with gait or balance Are referred by other Health care providers e. g. London Ambulance Service or Paradoc.
Investigations that should be done by the GP where possible Lying and standing BP Urine dip (to exclude UTI) ECG Bloods including FBC, U&Es, LFTs, TFTs, glucose, B 12, folate • If there is a history of fragility fractures has a DEXA scan been carried out? Does the scan confirm osteoporosis? • Timed get up and go test • Address polypharmacy (4+ drugs) with a focus on benzodiazepines, hyponotics and other drugs which can increase falls risk • •
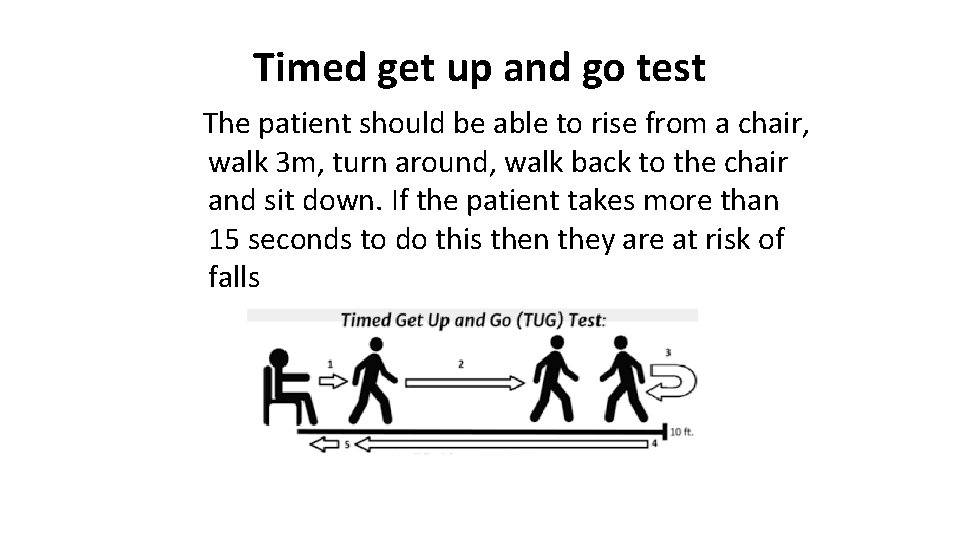
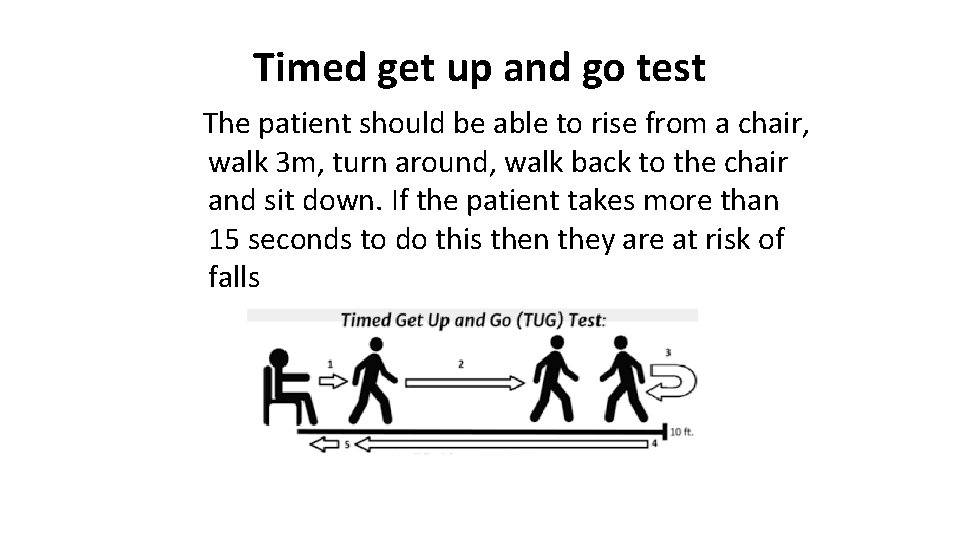
Timed get up and go test The patient should be able to rise from a chair, walk 3 m, turn around, walk back to the chair and sit down. If the patient takes more than 15 seconds to do this then they are at risk of falls
Risk factors for osteoporosis Previous fractures? Maternal history of #NOF? Family history of #NOF? Inflammatory bowel disease, chronic renal/liver disease, malabsorption? • On any of the following medication: Steroids, thyroid medication, anti-epileptics, aromatase inhibitors? • Post menopausal or early menopause? • •
A multi-factorial falls risk assessment includes the following: • • • An assessment of gait, balance, mobility and muscle strength An assessment of osteoporosis risk Perceived functional ability Vision assessment Cognitive assessment Urinary continence Hazards in the home Cardiovascular assessment Medication review
Referral options from Primary Care • Bryning Assessment and Rehabilitation Unit • Integrated Independence Team (Rapid Response Service) • Rapid Access Geriatrician • Adult Community Rehabilitation Team (ACRT) Session limited intervention • Integrated Independence Team (Home Treatment Team) • Therapy Led groups • Telecare • Social services • MRS Independent Living - Staying Steady programme
What Happens in the Falls Clinic • • Comprehensive Geriatric Assessment Geriatrician Nursing assessment Physiotherapy Assessment Occupational Therapy Assessment Focus on falls risk factors and bone health Investigations as needed

Further Care • • • Cardiac investigations Syncope clinic: head up tilt, CSM Vestibular Assessment Strong and Steady Group Home visits etc Links into IIT, ACRT, Memory clinic, continence clinic etc
Case: SR • • • 62 yr old bipolar 6 falls in six months- all sudden collapses Picked up on admission under surgeons Profound postural hypotension Full cardiac investigations Compression hoisery Also balance poor- Strong and Steady Fludrocortisone Falls less. More confidence
Case: LM • • • 92 retired Nurse Main carer for Husband with dementia He has worsening Behavioural Symptoms Some sudden collapses 1 x push from husband Cardiac Inv. Safeguarding IIT referral- urgent OT interventions Urgent social care referral Urgent respite referral
Falls: improving outcomes 23 rd March 2018 Anna Hanbury
Issue / opportunity • Right care have identified that C&H have an opportunity to improve falls related outcomes and spend. • There are 2, 624 admissions due to falls in the over 65 s per 100, 000 population (2015/16) in City and Hackney residents, significantly higher than 2, 253 in London and 2, 169 in England. • However, as a result of our young demographic, the actual number of admissions is much less. In 2016/17 there were 584 admissions due to falls in >65’s for City and Hackney residents (ICD 10 codes for injuries). • NHSE mandates the CCG to respond to this opportunity and the Unplanned Care Workstream has been given the responsibility for developing a programme of work to deliver this. • A target reduction of 3. 5% in number of admissions due to falls in >65’s has been proposed in the 2018/19 financial planning process.

The plan? 16 • Recognition of existing groups / work but none sufficient to deliver improvements required - Need to review / oversee outputs from existing work & develop a wider programme • Initial scoping discussions with key stakeholders to identify potential areas to focus - Primary care management – ensuring that those at risk are identified, assessed & appropriately referred (also acute management) - Acute response to falls – ensuring robust community response to mitigate unnecessary A&E / admissions - Falls interventions / prevention services - Availability and appropriate use of effective evidenced based interventions • Facilitated session(s) with wider stakeholders to identify opportunities - Review objective evidence – national guidance and current provision in C&H - Share opinions about what works well / doesn’t work - Select those likely to have significant improvement in outcomes that is readily achievable - Develop an outline of the work that is required with a suggestion of how it can be achieved

Key national policy • 2001: National Service Framework for Older People • 2004: NICE guideline CG 21 - Falls: the assessment and prevention of falls in older people • 2009: Do. H – Falls and Fractures. Effective interventions in health and social Care • 2013: NICE Guideline CG 161 - Falls in older people: assessing risk and prevention • 2017: NICE Quality Standard 86 – Falls in older people: Prevention • 2017: PHE Falls and Fracture consensus statement: supporting commissioning for prevention
2017: PHE Falls and Fracture consensus statement: supporting commissioning for prevention - promote healthy ageing across the different stages of the life course - optimise the reach of evidence based case finding and risk assessment - be able to demonstrate the commissioning of services that provide: • • an appropriate response attending people who have fallen multifactorial risk assessment and timely and evidence based tailored interventions for those at high risk of falls evidence based strength and balance programmes and opportunities for those at low to moderate risk of falls home hazard assessment and improvement programmes - ensure that local approaches to improve poor or inappropriate housing address falls prevention and promote healthy ageing - be able to demonstrate actions to reduce risk in high-risk health and residential care environments - provide fracture liaison services in line with clinical standards including access to effective falls interventions when necessary - provide evidence based collaborative, interdisciplinary care for falls-related serious injuries supported by clinical audit programmes - have a strategic lead and governance body with oversight and assurance of falls, bone health and related areas including frailty and multimorbidity
Primary Care • Existing work – Clinical leadership programme - Current management – objective measurement limited by EMIS coding - GP survey - varied awareness and use of the falls pathway - Acknowledged that existing pathway complex and potentially difficult to follow simplified guidance developed • Further opportunities (based on national guidance) - Ensuring those at risk are identified – MECC, Frailty index, ? Other register – FHV, Proactive care, LTC - Appropriate assessment of those at risk – Existing primary care assessment tool – is it for purpose? Are the right people getting one? Who needs more detailed (multifactorial) assessment of risk and who does this? - Referral to appropriate interventions - evidence based dependent on risk - Measurement & audit – EMIS codes and templates; • Number of patients identified at risk & risk assessed • Number referred to strength and balance - Role in acute response – Duty doctor & link with LAS / Paradoc / IIT

Paradoc extension • Para. Doc (ongoing) - From 12 midday to 12 midnight, 7 days a week. - The Para. Doc service provides an urgent call out to patients from a GP and a Paramedic/EMT, avoiding a call to the LAS. Aimed at preventing emergency admissions for a range of acute and chronic medical conditions (including Falls) for vulnerable/elderly/complex patients. Referrals from all HCPs, including Care Homes, Care workers, IIT, nurses, LAS and GP practices. • Para. Doc Falls Service (starting 9 th April, same telephone number) - From 8 am to 12 midday, 7 days a week. - Paramedic and IIT therapist for Falls on the floor; Critical assessment; Falls assessment and mobility issues. - Urgent referrals especially from Care homes, Nursing homes, Supported living schemes, Telecare, Homecare Providers and Care workers, LAS , Community nurses etc. This service will link back to the GP and manage onward IIT support as necessary.

How you can help? • We need your input/views on primary care proposals & opportunities • Attendance at the facilitated session • Small group to focus on developing primary care initiatives