Integrating physical and mental health City and Hackney





- Slides: 26
Integrating physical and mental health City and Hackney Primary Care Education Session 30 th November 2018
SMI and Physical Health Drivers of Poor Health § In City and Hackney 40. 4% of people with SMI smoke compared to 16. 9% of general population. 62% of people with SMI offered smoking cessation. § City and Hackney SMI obesity rates are 31% of which 25% are offered a lifestyle intervention compared to 13. 5% general population § Alcohol misuse nationally in SMI is 50% higher than the general population. Reliable local data is not available. Health Outcomes § 14% of the City and Hackney SMI population have diabetes compared to 4. 6% of the general population § SMI life expectancy in London is 8 -14 years less for men and 10 -18 years less of women (SLAM, 2007 -09 study).

Smoking and BMI in City and Hackney SMI population compared to general population
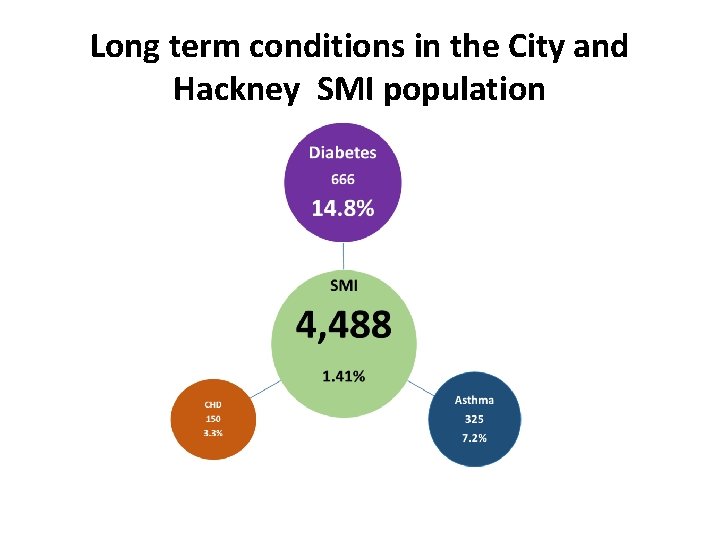
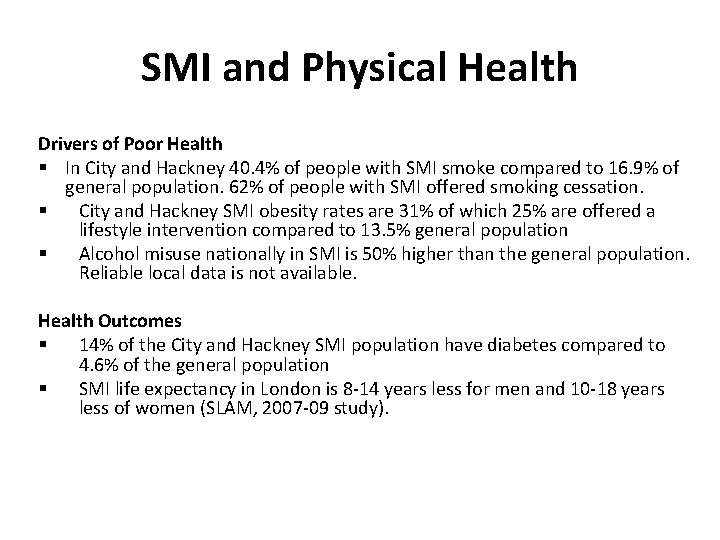
Long term conditions in the City and Hackney SMI population
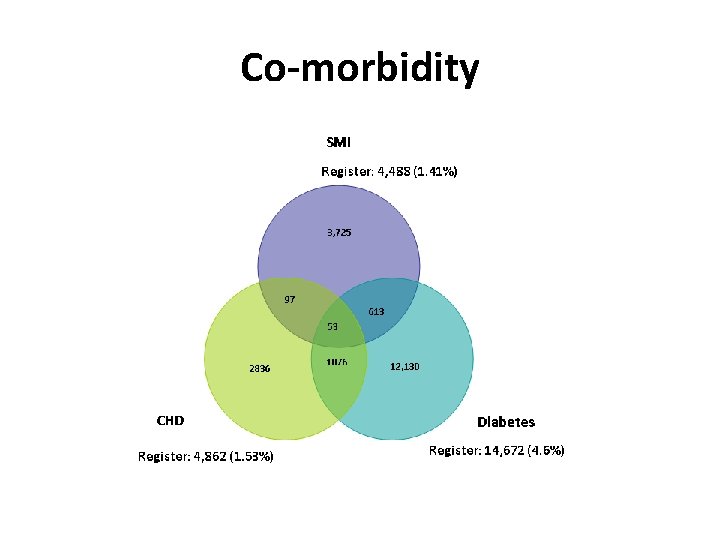
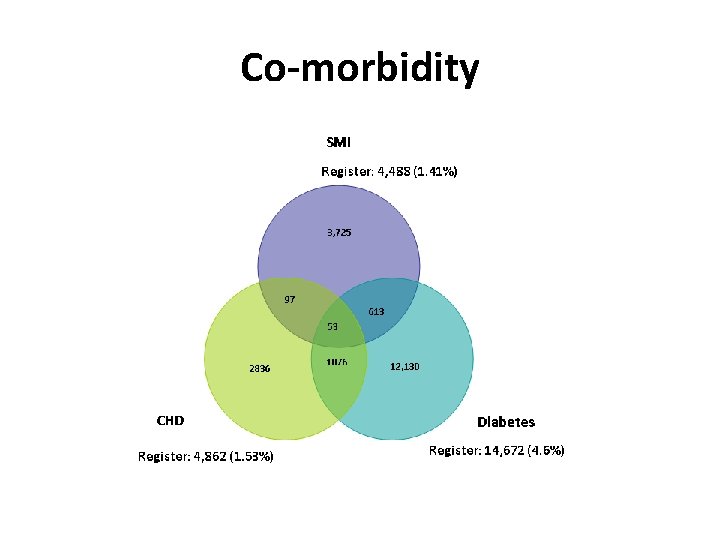
Co-morbidity

SMI contact with services 27 % 1, 200 3, 288 73 % 50% of people with SMI pass through secondary care per annum
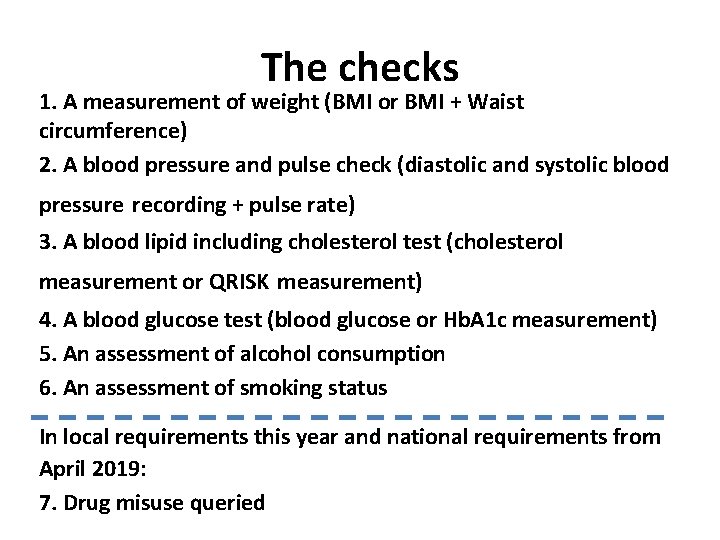
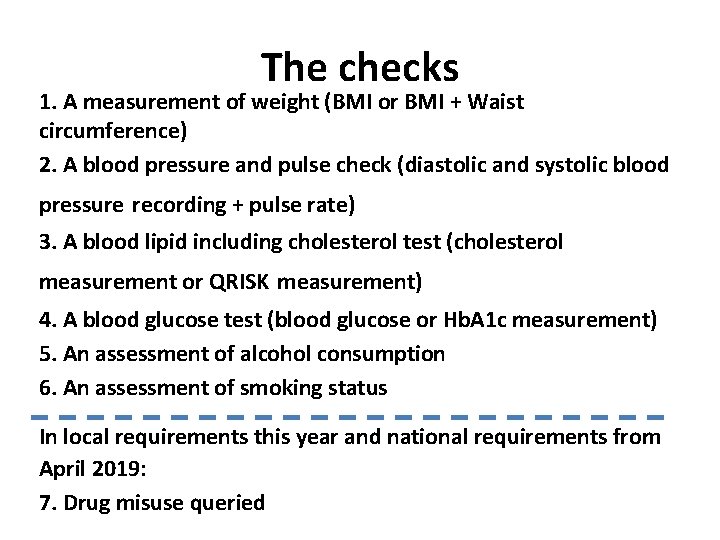
The checks 1. A measurement of weight (BMI or BMI + Waist circumference) 2. A blood pressure and pulse check (diastolic and systolic blood pressure recording + pulse rate) 3. A blood lipid including cholesterol test (cholesterol measurement or QRISK measurement) 4. A blood glucose test (blood glucose or Hb. A 1 c measurement) 5. An assessment of alcohol consumption 6. An assessment of smoking status In local requirements this year and national requirements from April 2019: 7. Drug misuse queried

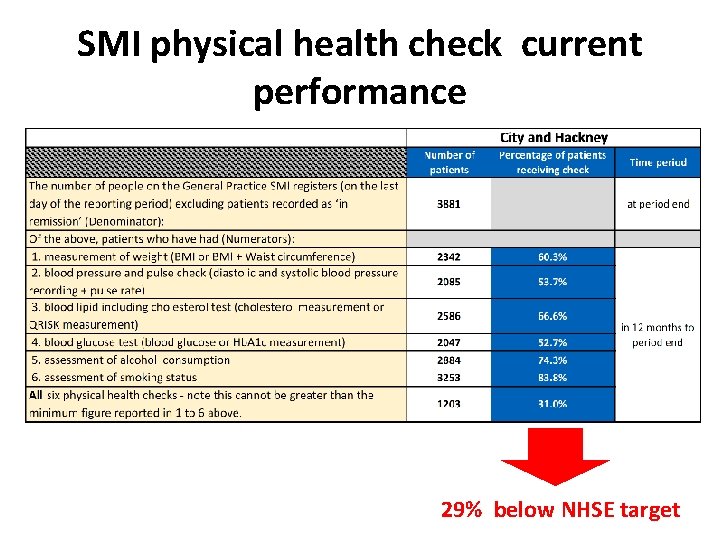
Targets • NHSE’s 2018 -19 target is 60% coverage of the SMI population with all 6 physical health checks. • City and Hackney GP practices receive £ 20, 000 collectively for 60% and £ 30, 000 for 70%+ for all six checks + drug misuse queried. • ELFT are will support these targets by completing physical health checks on EMIS for patients in secondary care. However ELFT need to match their patient lists with GP practices.
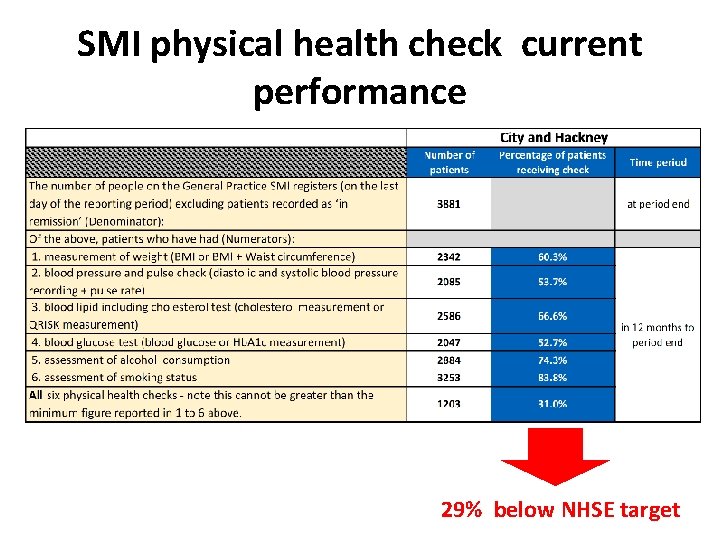
SMI physical health check current performance 29% below NHSE target
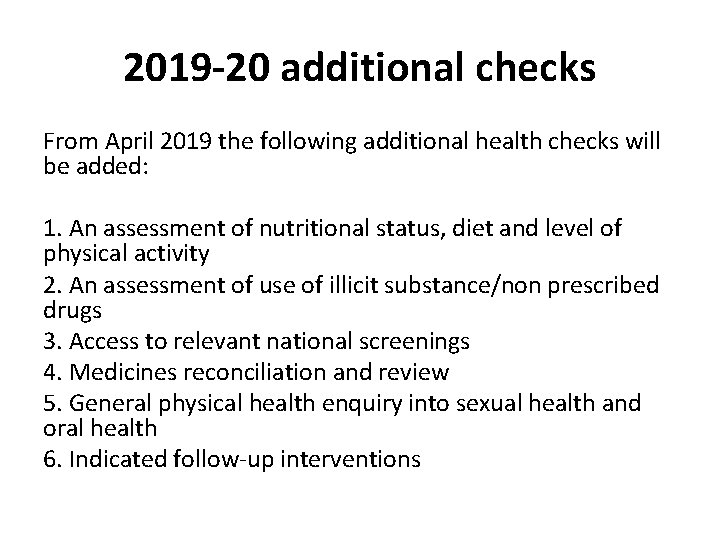
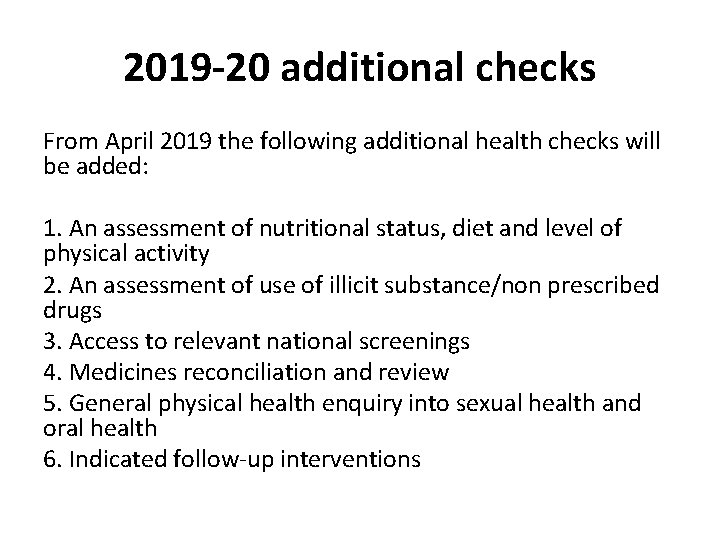
2019 -20 additional checks From April 2019 the following additional health checks will be added: 1. An assessment of nutritional status, diet and level of physical activity 2. An assessment of use of illicit substance/non prescribed drugs 3. Access to relevant national screenings 4. Medicines reconciliation and review 5. General physical health enquiry into sexual health and oral health 6. Indicated follow-up interventions
Discussion Points 1. What are the biggest challenges in reaching the physical health check targets? 2. Are some physical checks more challenging then others and if so why? 3. What are the challenges with ‘follow up interventions’?
Changing lifestyles • • Navigation Social prescribing Health coaching Working with low motivation
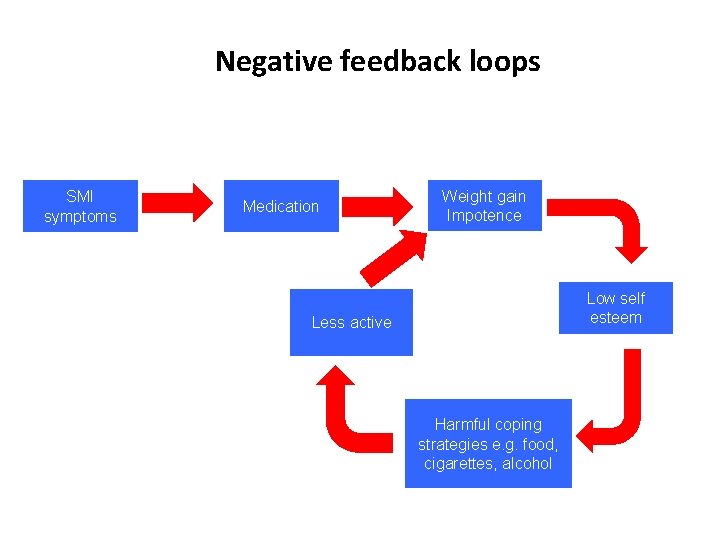
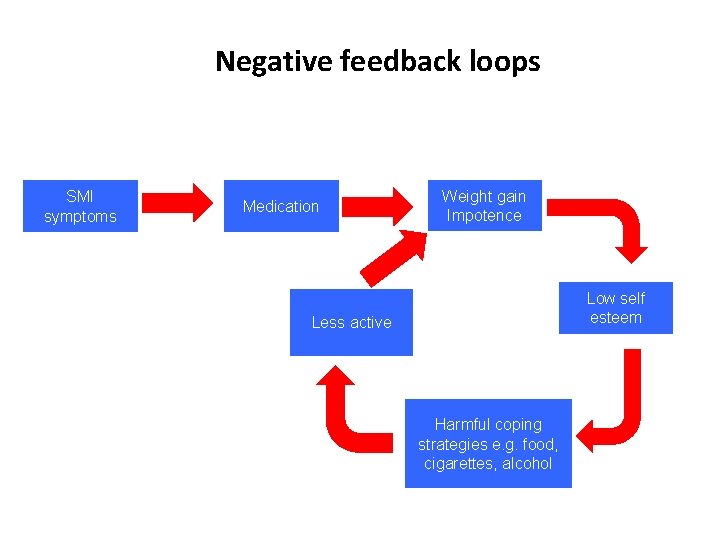
Negative feedback loops SMI symptoms Medication Weight gain Impotence Low self esteem Less active Harmful coping strategies e. g. food, cigarettes, alcohol
The Coachagator § § § Care navigation alone is not enough if people are poorly motivated Ideally we need a cross between a navigator and a health coach. A Coachagator – able motivate patients and link them with the right resources Patients can also learn to use self help tools e. g. online support

Integrated IAPT: Building specialised CBT pathways for patients with Long Term Conditions (LTCs)
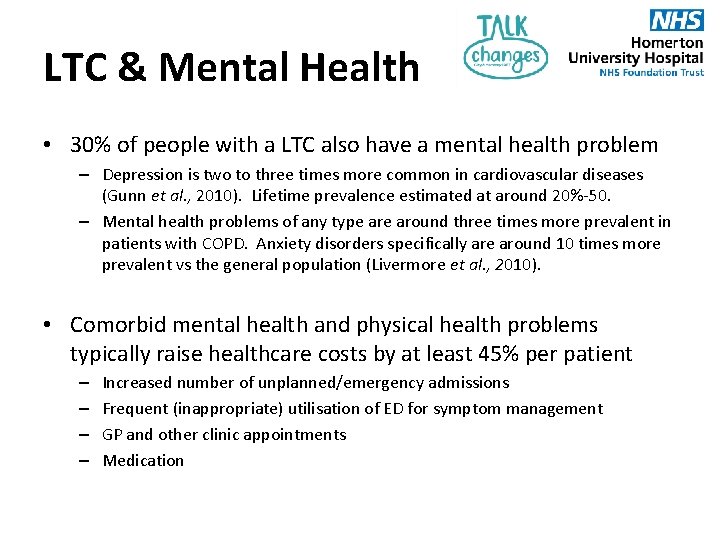
LTC & Mental Health • 30% of people with a LTC also have a mental health problem – Depression is two to three times more common in cardiovascular diseases (Gunn et al. , 2010). Lifetime prevalence estimated at around 20%-50. – Mental health problems of any type around three times more prevalent in patients with COPD. Anxiety disorders specifically are around 10 times more prevalent vs the general population (Livermore et al. , 2010). • Comorbid mental health and physical health problems typically raise healthcare costs by at least 45% per patient – – Increased number of unplanned/emergency admissions Frequent (inappropriate) utilisation of ED for symptom management GP and other clinic appointments Medication
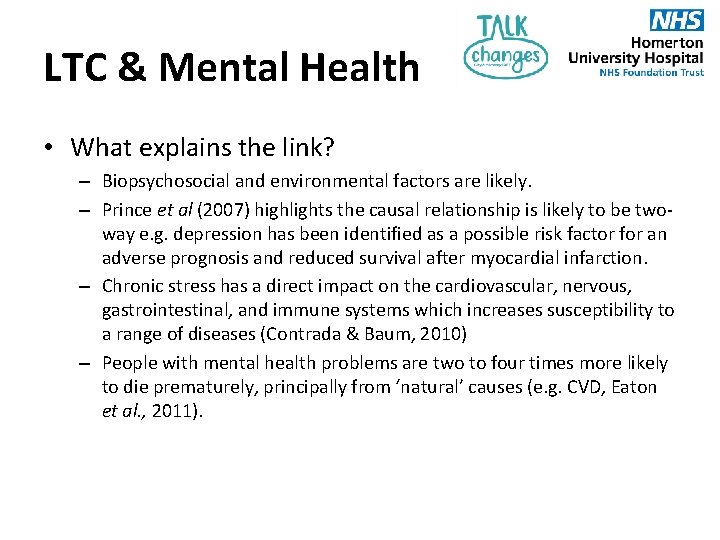
LTC & Mental Health • What explains the link? – Biopsychosocial and environmental factors are likely. – Prince et al (2007) highlights the causal relationship is likely to be twoway e. g. depression has been identified as a possible risk factor for an adverse prognosis and reduced survival after myocardial infarction. – Chronic stress has a direct impact on the cardiovascular, nervous, gastrointestinal, and immune systems which increases susceptibility to a range of diseases (Contrada & Baum, 2010) – People with mental health problems are two to four times more likely to die prematurely, principally from ‘natural’ causes (e. g. CVD, Eaton et al. , 2011).
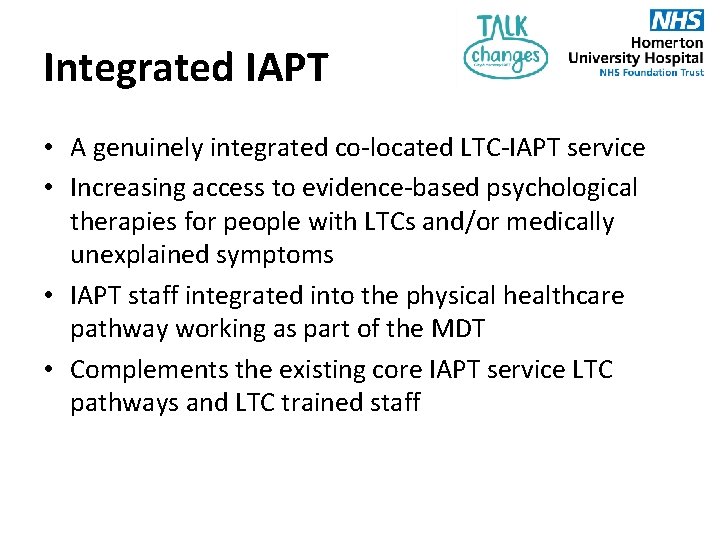
Integrated IAPT • A genuinely integrated co-located LTC-IAPT service • Increasing access to evidence-based psychological therapies for people with LTCs and/or medically unexplained symptoms • IAPT staff integrated into the physical healthcare pathway working as part of the MDT • Complements the existing core IAPT service LTC pathways and LTC trained staff
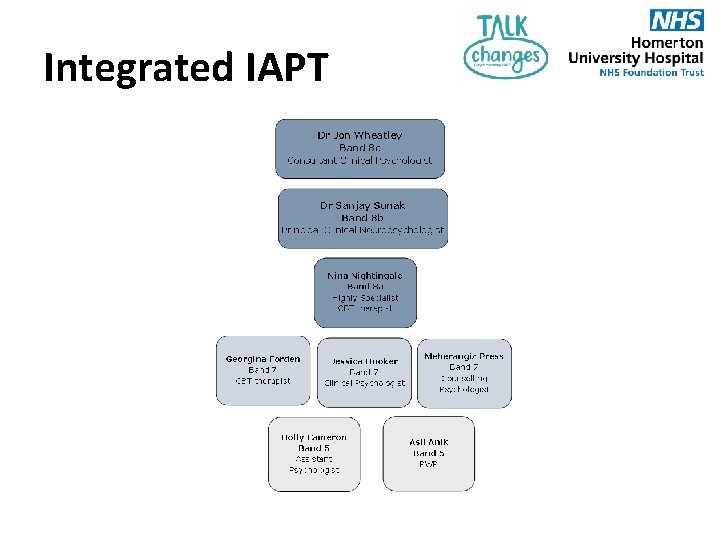
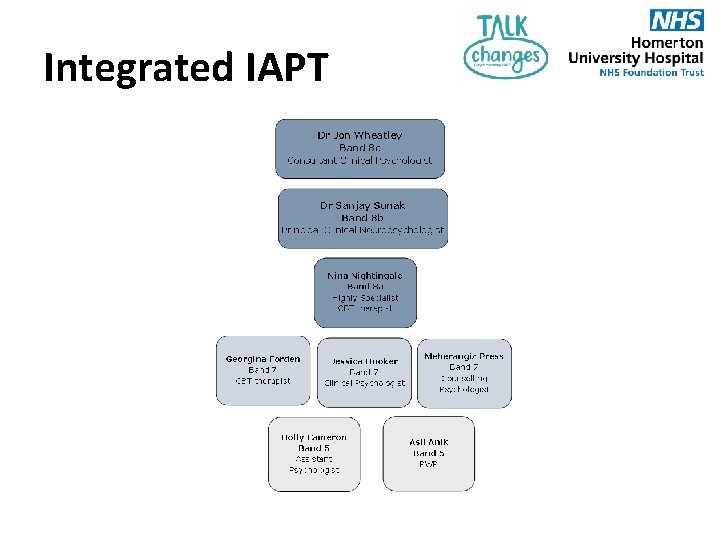
Integrated IAPT

Integrated IAPT Cardiac Diabetes COPD LTC IAPT IBS Pain
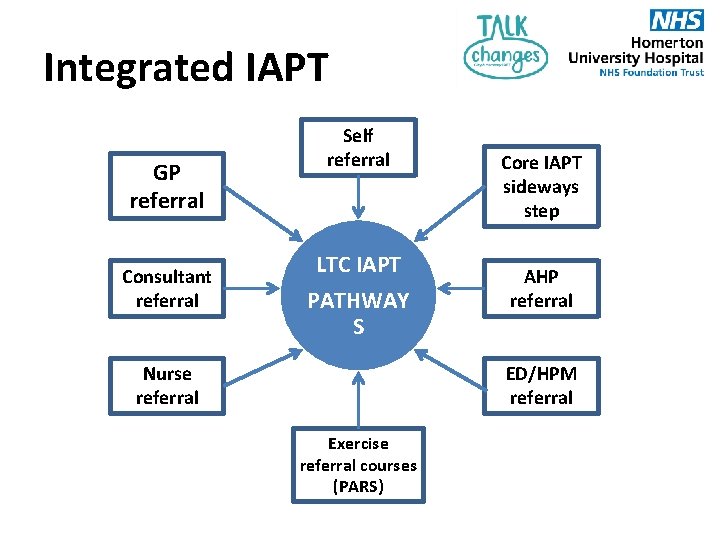
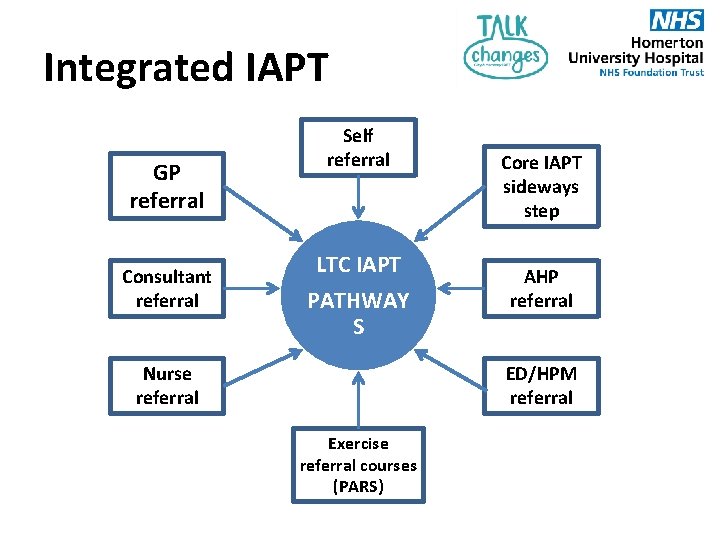
Integrated IAPT GP referral Consultant referral Self referral LTC IAPT PATHWAY S Nurse referral Core IAPT sideways step AHP referral ED/HPM referral Exercise referral courses (PARS)
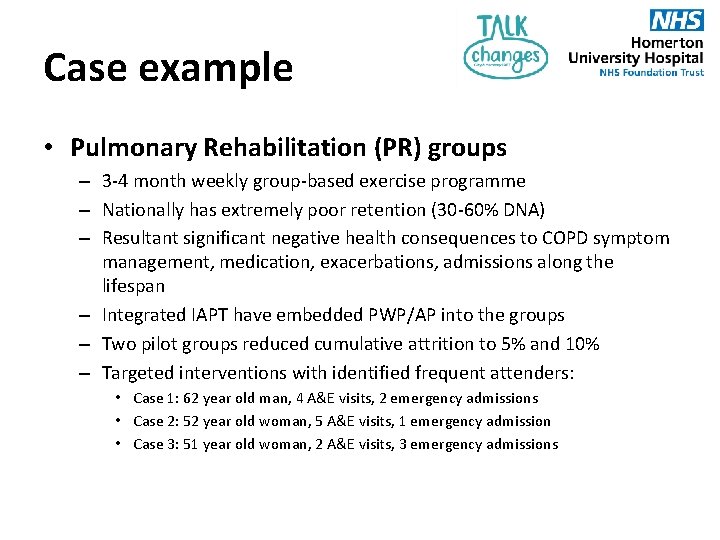
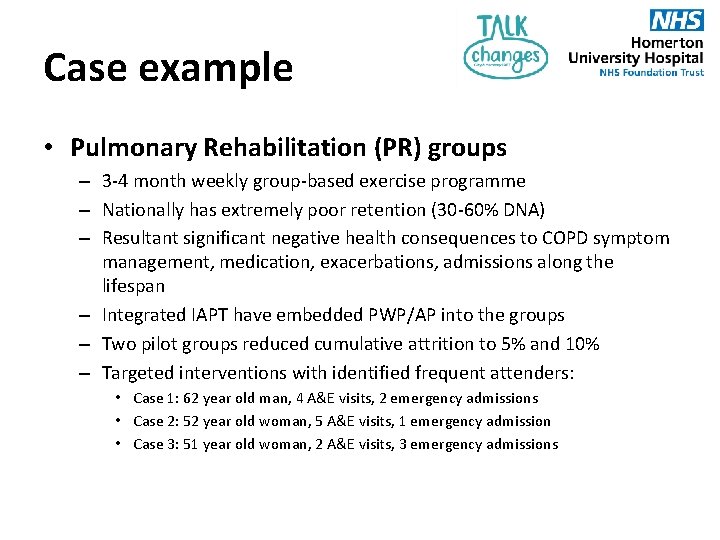
Case example • Pulmonary Rehabilitation (PR) groups – 3 -4 month weekly group-based exercise programme – Nationally has extremely poor retention (30 -60% DNA) – Resultant significant negative health consequences to COPD symptom management, medication, exacerbations, admissions along the lifespan – Integrated IAPT have embedded PWP/AP into the groups – Two pilot groups reduced cumulative attrition to 5% and 10% – Targeted interventions with identified frequent attenders: • Case 1: 62 year old man, 4 A&E visits, 2 emergency admissions • Case 2: 52 year old woman, 5 A&E visits, 1 emergency admission • Case 3: 51 year old woman, 2 A&E visits, 3 emergency admissions
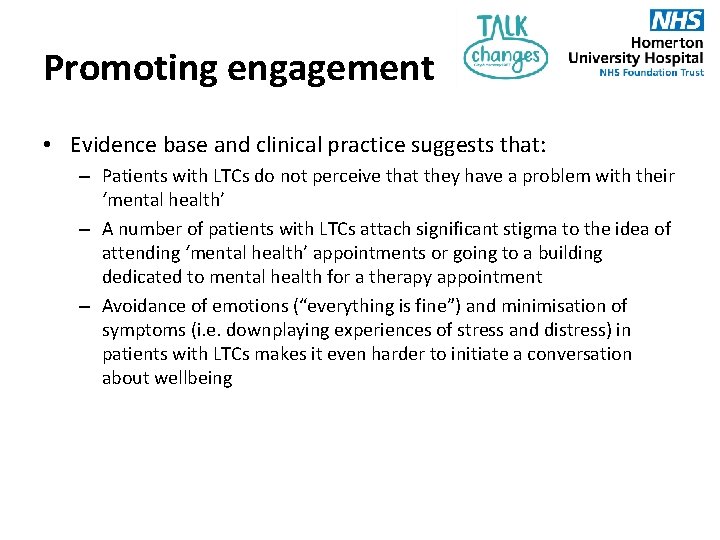
Promoting engagement • Evidence base and clinical practice suggests that: – Patients with LTCs do not perceive that they have a problem with their ‘mental health’ – A number of patients with LTCs attach significant stigma to the idea of attending ‘mental health’ appointments or going to a building dedicated to mental health for a therapy appointment – Avoidance of emotions (“everything is fine”) and minimisation of symptoms (i. e. downplaying experiences of stress and distress) in patients with LTCs makes it even harder to initiate a conversation about wellbeing
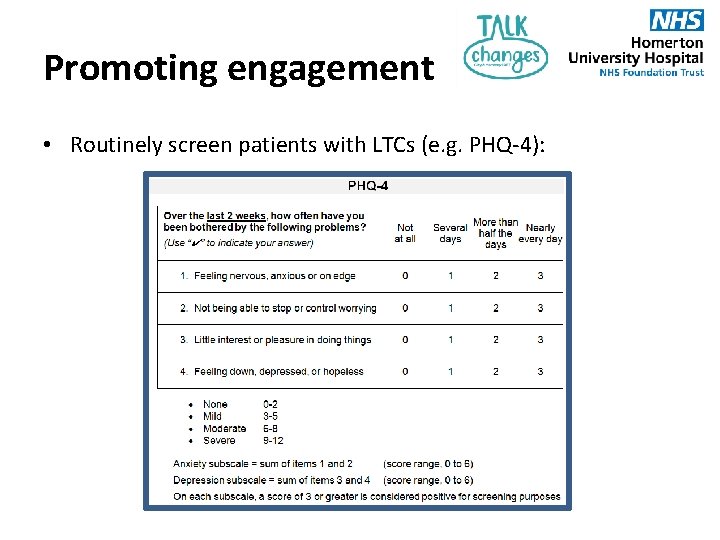
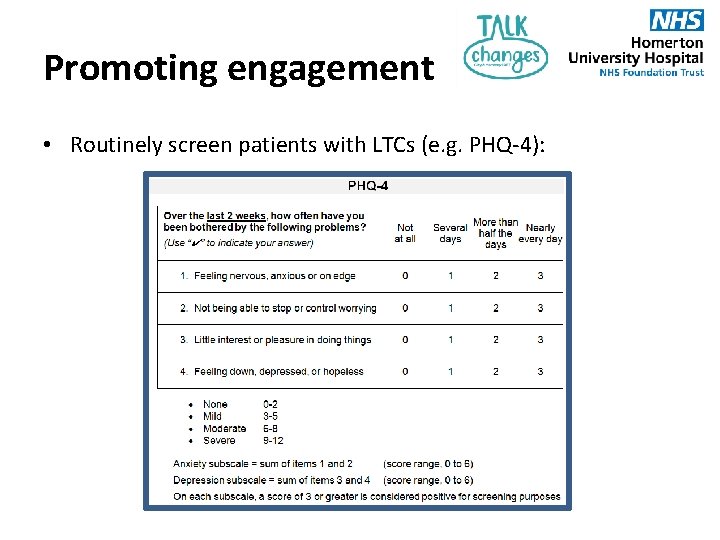
Promoting engagement • Routinely screen patients with LTCs (e. g. PHQ-4):
Promoting engagement • Tailoring language: • Avoid diagnostic/psychiatric language: stress, low mood, feeling scared, shock, ‘space to talk it through’, ‘feeling stuck’ • Focus the conversation on coping strategies (and where getting some support to learn or try out new coping strategies may make managing symptoms easier, or prevent another flare up in the future) • If time permits talk about the relationship between body and mind (“She [the GP] explained all about. . . the physiology of it. . . first time that I understood why my energy was so low; made a lot of sense”) • Offer the ‘salesperson pitches’: (i) what have you got to lose (e. g. only 45 minutes of your life etc); (ii) we’re trying everything that we can to help you manage your symptoms better, this referral may not change things overnight but if it helps by just 5% that feels…. – If you can get people to accept a telephone call just to explore their options, we will try and do the rest!
Discussion points from Dan 1. What are the challenges identifying psychological needs for people with LTCs? 2. What are the challenges referring on for help once a psychological need has been identified?
 City and hackney recovery college
City and hackney recovery college Mental health and mental illness chapter 20
Mental health and mental illness chapter 20 Mental health coping skills jeopardy
Mental health coping skills jeopardy Integrating public health and primary care
Integrating public health and primary care Cormier and hackney model
Cormier and hackney model Social prescribing hackney
Social prescribing hackney Hackney population density
Hackney population density Paradoc hackney
Paradoc hackney Hackney autism service
Hackney autism service Acrt hackney
Acrt hackney Hackney adhd clinic
Hackney adhd clinic North hackney cmht
North hackney cmht New jersey space grant consortium
New jersey space grant consortium Hackney community law centre
Hackney community law centre Integrating classification and association rule mining
Integrating classification and association rule mining Key internal forces
Key internal forces Integrating factor exact equations
Integrating factor exact equations Integrating science and social studies
Integrating science and social studies Integrating strategy and culture in internal assessment
Integrating strategy and culture in internal assessment Integrating qualitative and quantitative methods
Integrating qualitative and quantitative methods Integrating communications assessment and tactics
Integrating communications assessment and tactics Integrating sel and pbis
Integrating sel and pbis Is a combination of mental physical and social qualities
Is a combination of mental physical and social qualities The combination of physical, mental and social well-being.
The combination of physical, mental and social well-being. A state of complete physical mental and social well-being
A state of complete physical mental and social well-being Chapter 25 lesson 4 physical and mental challenges
Chapter 25 lesson 4 physical and mental challenges Health is a state of complete physical
Health is a state of complete physical