Chronic Disease Transitional Care Northridge Hospital Medical Center
- Slides: 14
Chronic Disease Transitional Care Northridge Hospital Medical Center Health Services Advisory Group 10/20/17 Dr. Jeremy Grosser Medical Director Transitional & Palliative Care
Disclosure • I have no financial relationships with commercial interests 2
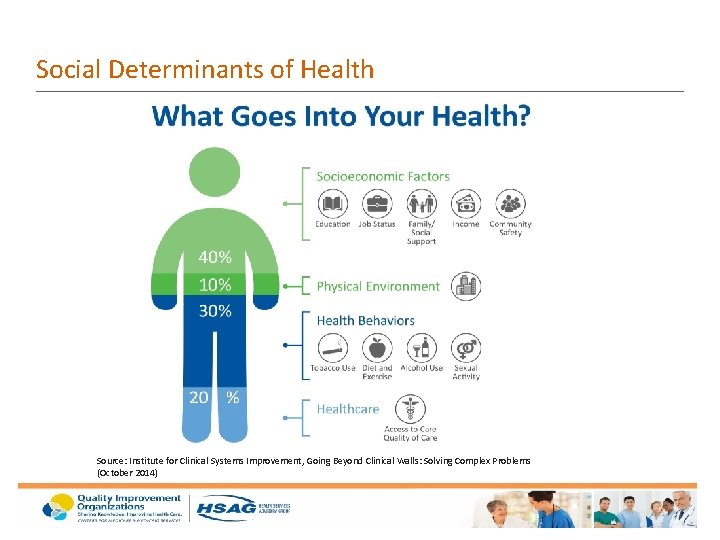
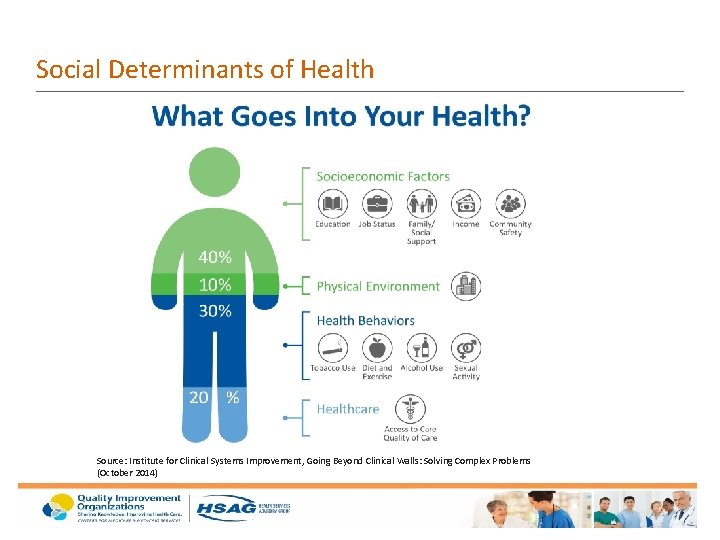
Social Determinants of Health Source: Institute for Clinical Systems Improvement, Going Beyond Clinical Walls: Solving Complex Problems (October 2014)
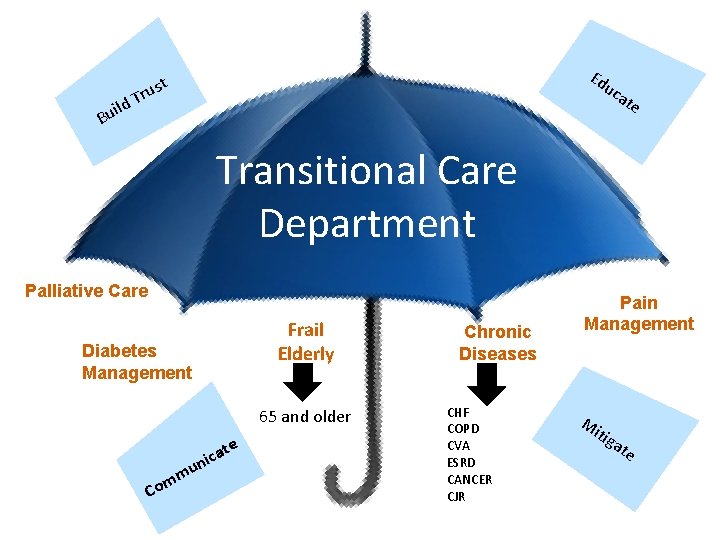
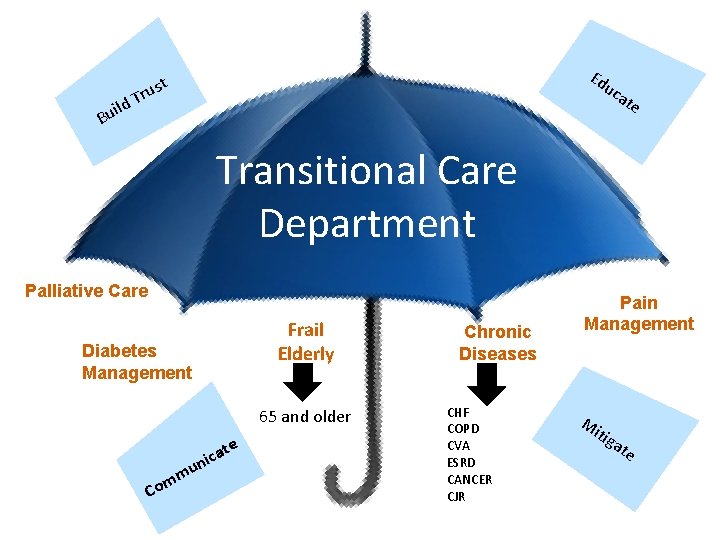
uild B Ed st u r T uc ate Transitional Care Department Palliative Care Frail Elderly Diabetes Management 65 and older te a c ni Co u m m Chronic Diseases CHF COPD CVA ESRD CANCER CJR Pain Management Mi tig ate
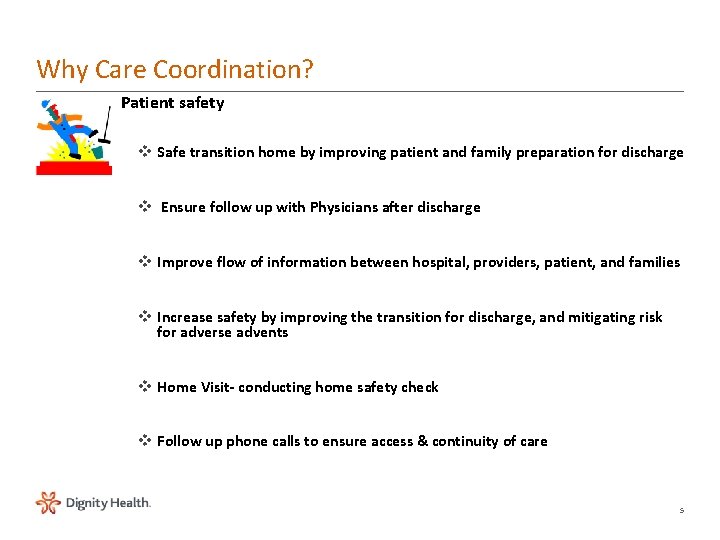
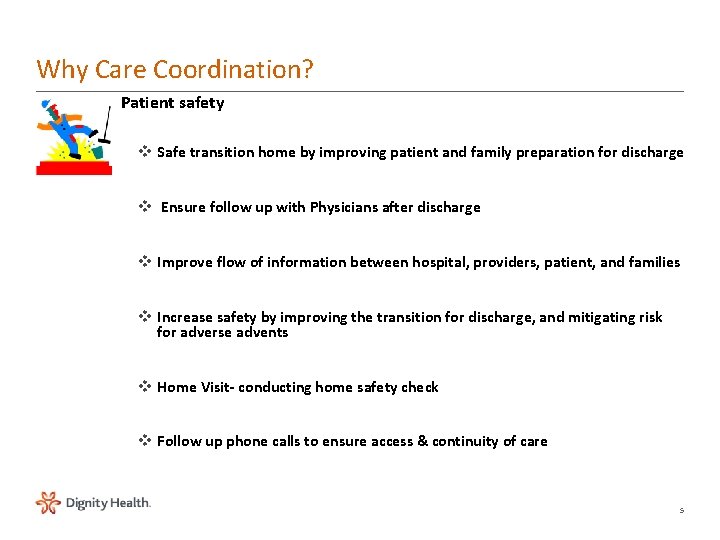
Why Care Coordination? Patient safety v Safe transition home by improving patient and family preparation for discharge v Ensure follow up with Physicians after discharge v Improve flow of information between hospital, providers, patient, and families v Increase safety by improving the transition for discharge, and mitigating risk for adverse advents v Home Visit- conducting home safety check v Follow up phone calls to ensure access & continuity of care 5
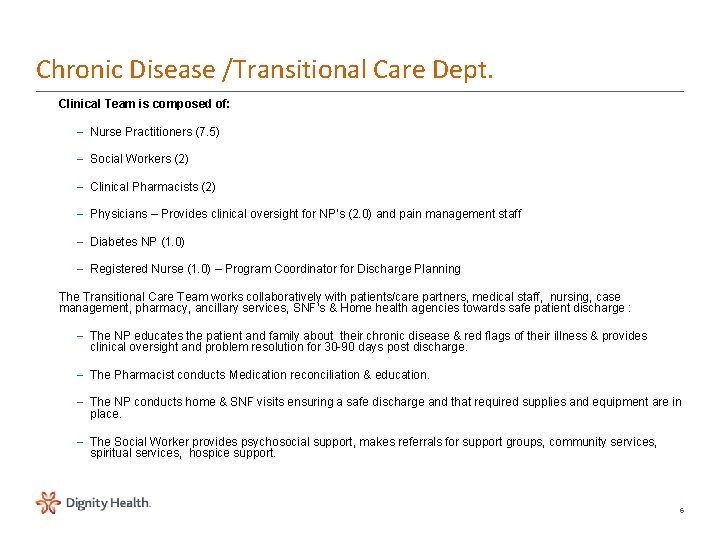
Chronic Disease /Transitional Care Dept. Clinical Team is composed of: – Nurse Practitioners (7. 5) – Social Workers (2) – Clinical Pharmacists (2) – Physicians – Provides clinical oversight for NP’s (2. 0) and pain management staff – Diabetes NP (1. 0) – Registered Nurse (1. 0) – Program Coordinator for Discharge Planning The Transitional Care Team works collaboratively with patients/care partners, medical staff, nursing, case management, pharmacy, ancillary services, SNF’s & Home health agencies towards safe patient discharge : – The NP educates the patient and family about their chronic disease & red flags of their illness & provides clinical oversight and problem resolution for 30 -90 days post discharge. – The Pharmacist conducts Medication reconciliation & education. – The NP conducts home & SNF visits ensuring a safe discharge and that required supplies and equipment are in place. – The Social Worker provides psychosocial support, makes referrals for support groups, community services, spiritual services, hospice support. 6
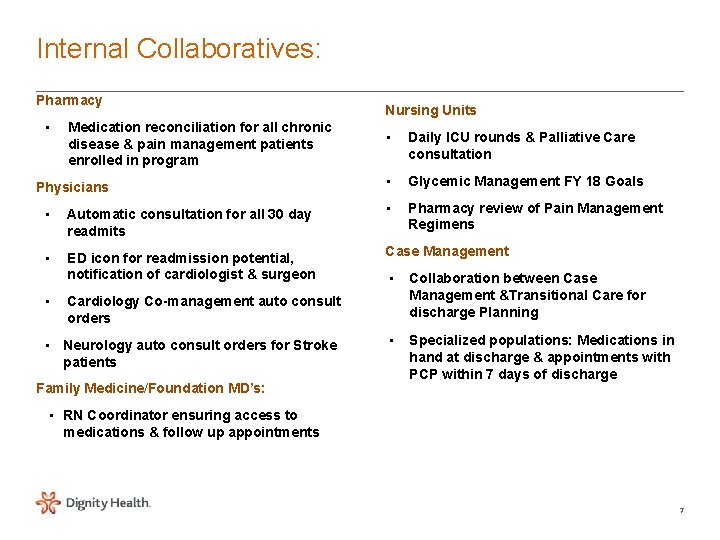
Internal Collaboratives: Pharmacy • Medication reconciliation for all chronic disease & pain management patients enrolled in program Physicians Nursing Units • Daily ICU rounds & Palliative Care consultation • Glycemic Management FY 18 Goals Pharmacy review of Pain Management Regimens • Automatic consultation for all 30 day readmits • • ED icon for readmission potential, notification of cardiologist & surgeon Case Management • • Collaboration between Case Management &Transitional Care for discharge Planning • Specialized populations: Medications in hand at discharge & appointments with PCP within 7 days of discharge Cardiology Co-management auto consult orders • Neurology auto consult orders for Stroke patients Family Medicine/Foundation MD’s: • RN Coordinator ensuring access to medications & follow up appointments 7
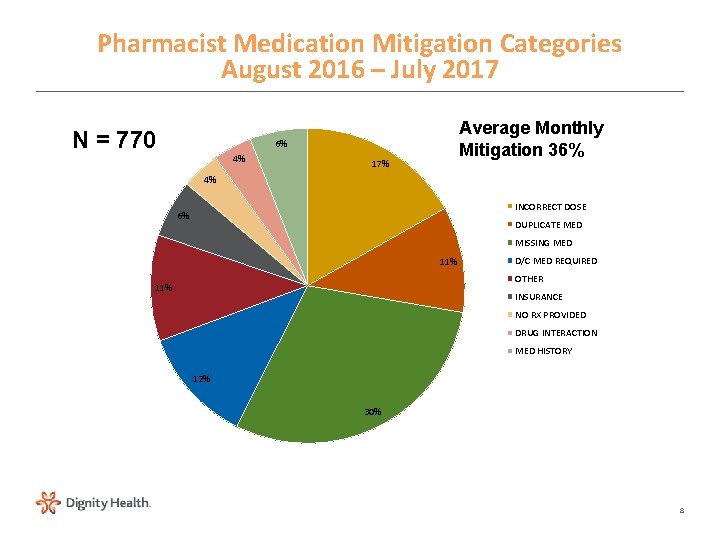
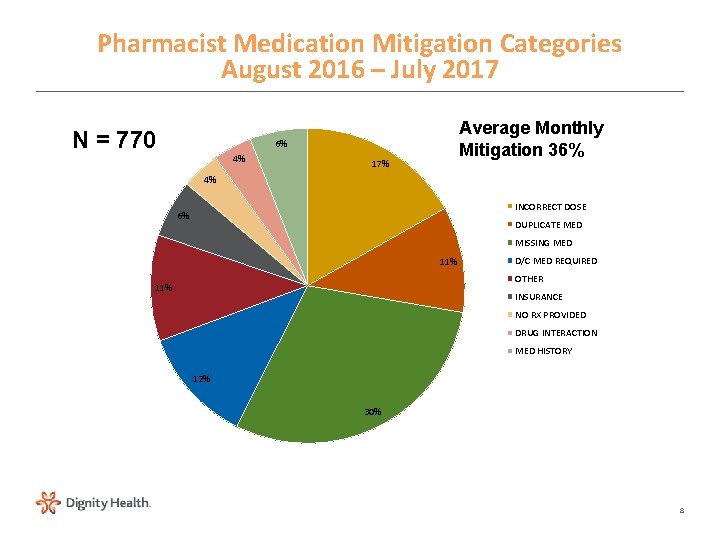
Pharmacist Medication Mitigation Categories August 2016 – July 2017 N = 770 Average Monthly Mitigation 36% 6% 4% 17% 4% INCORRECT DOSE 6% DUPLICATE MED MISSING MED 11% D/C MED REQUIRED OTHER 11% INSURANCE NO RX PROVIDED DRUG INTERACTION MED HISTORY 12% 30% 8
External Collaboratives Skilled nursing facilities (SNFs) • Must maintain Star rating at 3+ • Narrowed network of 8 facilities • Weekly NP driven patient rounds at the SNF’s • Weekly clinical calls with Medical Director & NP’s • Monthly collaborative meetings o Review of SNF readmission outcomes o Identify best performers o Adjustments to narrowed network as needed Home health • Narrowed network of 8 vendors • NP’s coordinate care with HHA • Weekly clinical calls with Medical Director & NP’s • Monthly collaborative meetings 9
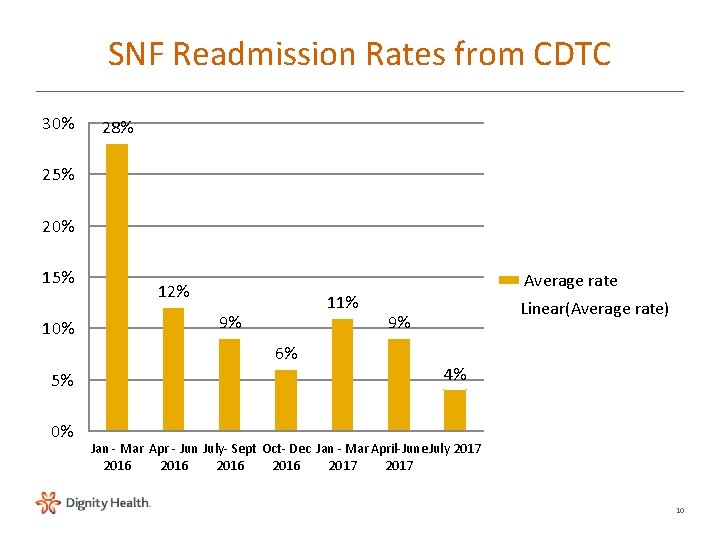
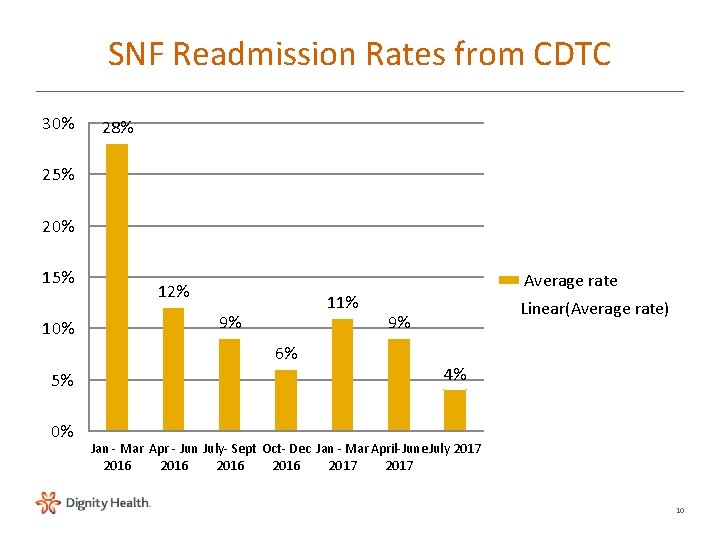
SNF Readmission Rates from CDTC 30% 28% 25% 20% 15% 10% 12% 11% 9% 6% 5% 0% Average rate Linear(Average rate) 9% 4% Jan - Mar Apr - Jun July- Sept Oct- Dec Jan - Mar April-June July 2017 2016 2017 10
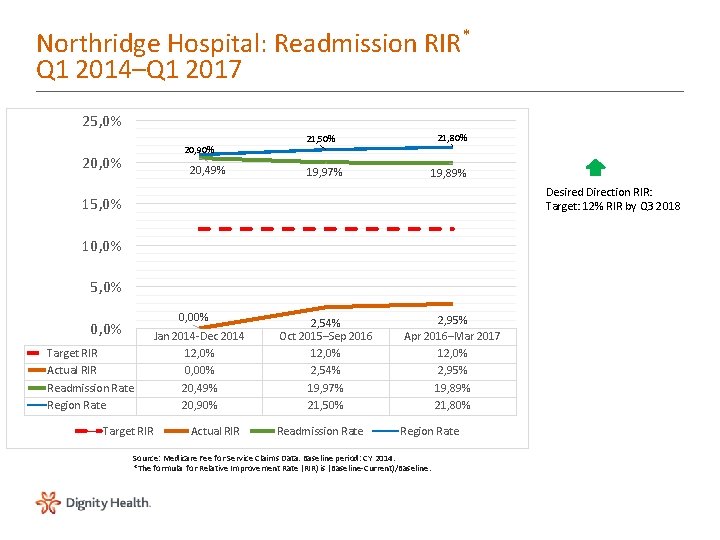
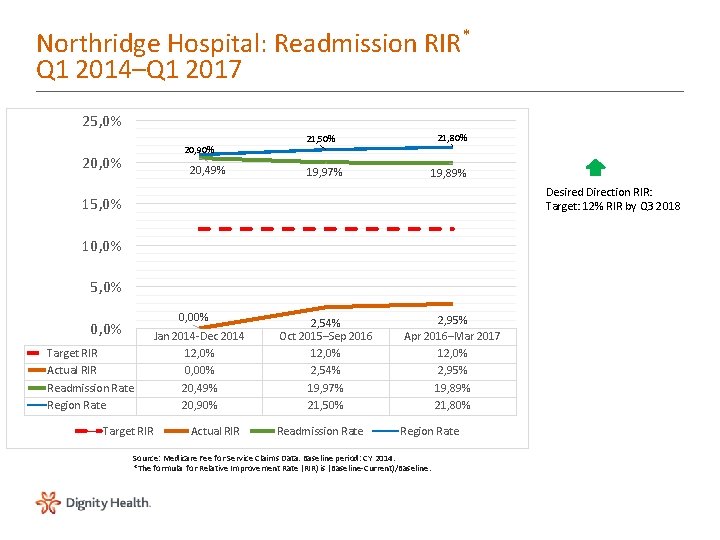
Northridge Hospital: Readmission RIR* Q 1 2014–Q 1 2017 25, 0% 20, 90% 20, 49% 21, 80% 21, 50% 19, 97% 19, 89% Desired Direction RIR: Target: 12% RIR by Q 3 2018 15, 0% 10, 0% 5, 0% 0, 0% Target RIR Actual RIR Readmission Rate Region Rate Target RIR Jan 2014 -Dec 2014 12, 0% 0, 00% 20, 49% 20, 90% Actual RIR 2, 54% Oct 2015–Sep 2016 12, 0% 2, 54% 19, 97% 21, 50% Readmission Rate 2, 95% Apr 2016–Mar 2017 12, 0% 2, 95% 19, 89% 21, 80% Region Rate Source: Medicare Fee for Service Claims Data. Baseline period: CY 2014. *The formula for Relative Improvement Rate (RIR) is (Baseline-Current)/Baseline.
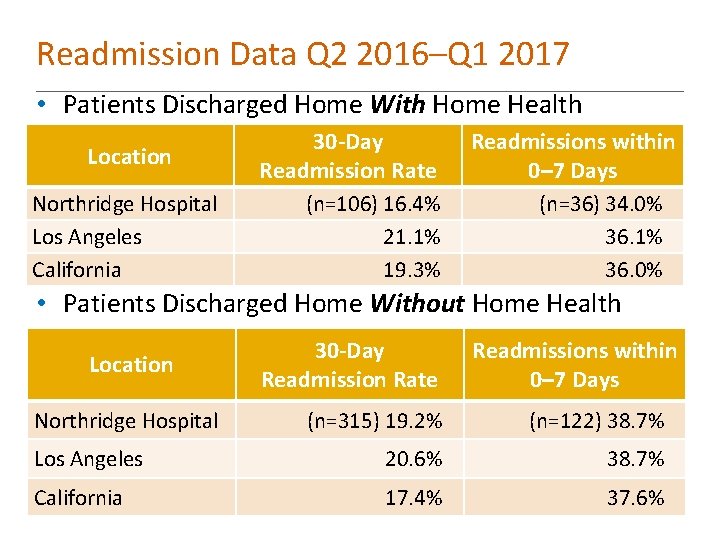
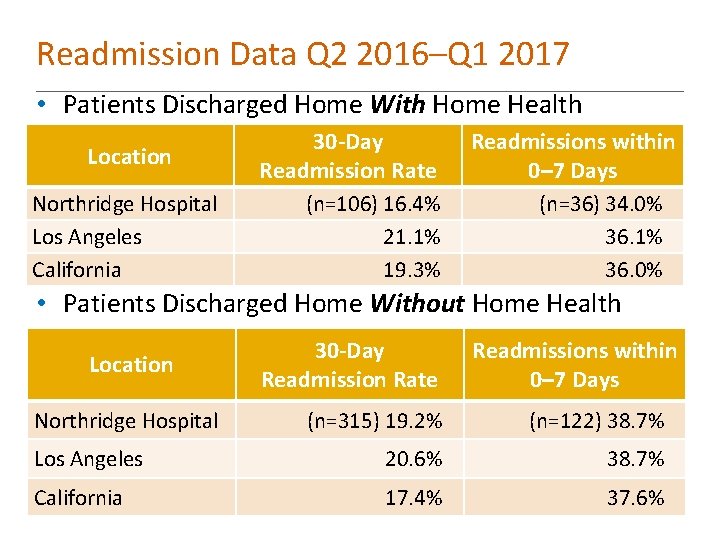
Readmission Data Q 2 2016–Q 1 2017 • Patients Discharged Home With Home Health Location Northridge Hospital Los Angeles California 30 -Day Readmission Rate (n=106) 16. 4% 21. 1% 19. 3% Readmissions within 0– 7 Days (n=36) 34. 0% 36. 1% 36. 0% • Patients Discharged Home Without Home Health Location Northridge Hospital 30 -Day Readmission Rate Readmissions within 0– 7 Days (n=315) 19. 2% (n=122) 38. 7% Los Angeles 20. 6% 38. 7% California 17. 4% 37. 6% 12
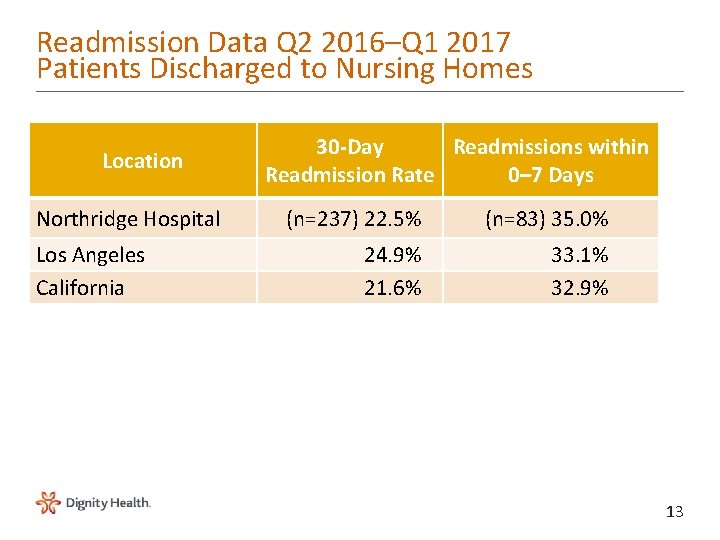
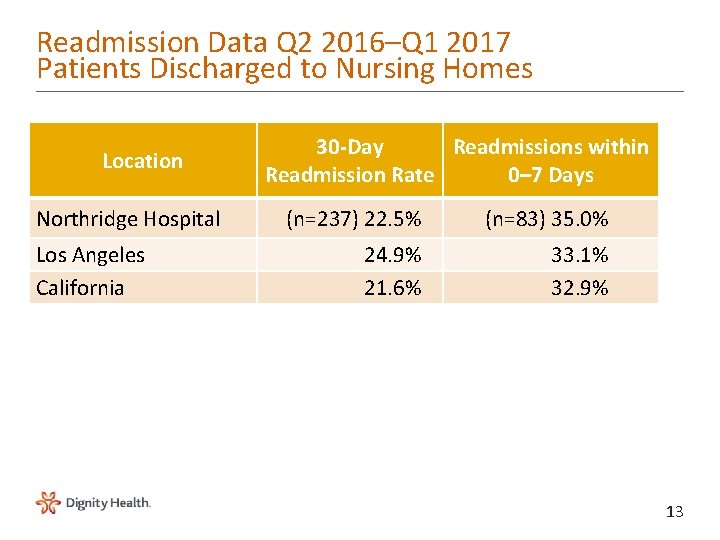
Readmission Data Q 2 2016–Q 1 2017 Patients Discharged to Nursing Homes Location Northridge Hospital Los Angeles California 30 -Day Readmissions within Readmission Rate 0– 7 Days (n=237) 22. 5% (n=83) 35. 0% 24. 9% 21. 6% 33. 1% 32. 9% 13
Thank You
 Jewish chronic disease hospital study
Jewish chronic disease hospital study Blind thrust fault animation
Blind thrust fault animation Cal state northridge psychology
Cal state northridge psychology Costco pharmacy northridge
Costco pharmacy northridge Transitional medical assistance ohio
Transitional medical assistance ohio Torrance memorial tcu
Torrance memorial tcu Chronic granulomatous disease
Chronic granulomatous disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Nephrology near atwater
Nephrology near atwater Chronic liver stigmata
Chronic liver stigmata Carlee oakley
Carlee oakley Peripheral stigmata of cld
Peripheral stigmata of cld Stigmata of chronic liver disease
Stigmata of chronic liver disease Kate lorig stanford
Kate lorig stanford Wagner's chronic care model
Wagner's chronic care model