Transitional Care Management Complex Chronic Care Management Thomas
- Slides: 35
Transitional Care Management Complex Chronic Care Management Thomas Weida, M. D. Professor, Family and Community Medicine Penn State College of Medicine
Nothing to Disclose 4/5/2014 © 2014, Thomas J. Weida, M. D. 2
Objectives • Implement proper use of Transitional Care Management Codes in the office • Prepare practice for upcoming Complex Care Coordination Codes and Advanced Directive Codes
Transitional Care Management (TCM) Services • Services required during transition to the community following certain discharges • No gap in care provided during transition • Medical or psychosocial problems of moderate or high complexity decision making • Takes responsibility for patient’s care • Can be used for new or established patients 4/5/2014 © 2014, Thomas J. Weida, M. D. 4
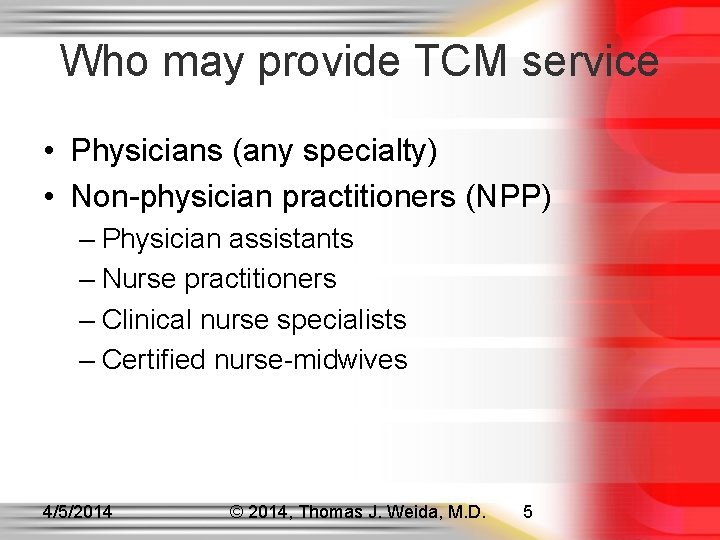
Who may provide TCM service • Physicians (any specialty) • Non-physician practitioners (NPP) – Physician assistants – Nurse practitioners – Clinical nurse specialists – Certified nurse-midwives 4/5/2014 © 2014, Thomas J. Weida, M. D. 5
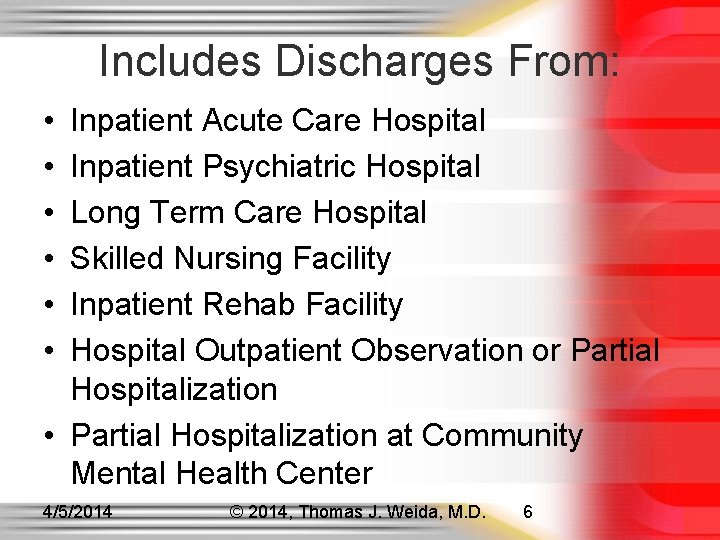
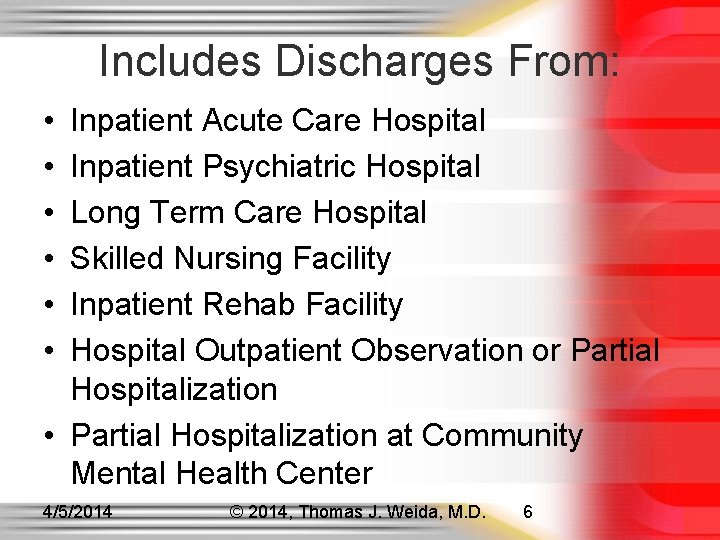
Includes Discharges From: • • • Inpatient Acute Care Hospital Inpatient Psychiatric Hospital Long Term Care Hospital Skilled Nursing Facility Inpatient Rehab Facility Hospital Outpatient Observation or Partial Hospitalization • Partial Hospitalization at Community Mental Health Center 4/5/2014 © 2014, Thomas J. Weida, M. D. 6
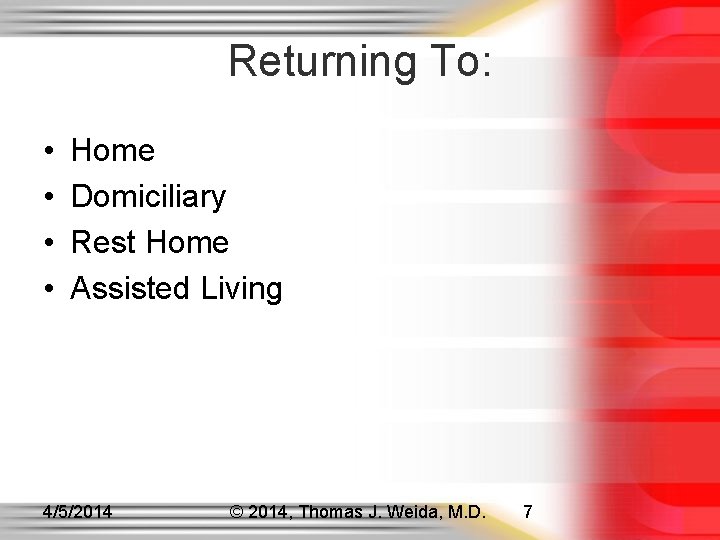
Returning To: • • Home Domiciliary Rest Home Assisted Living 4/5/2014 © 2014, Thomas J. Weida, M. D. 7
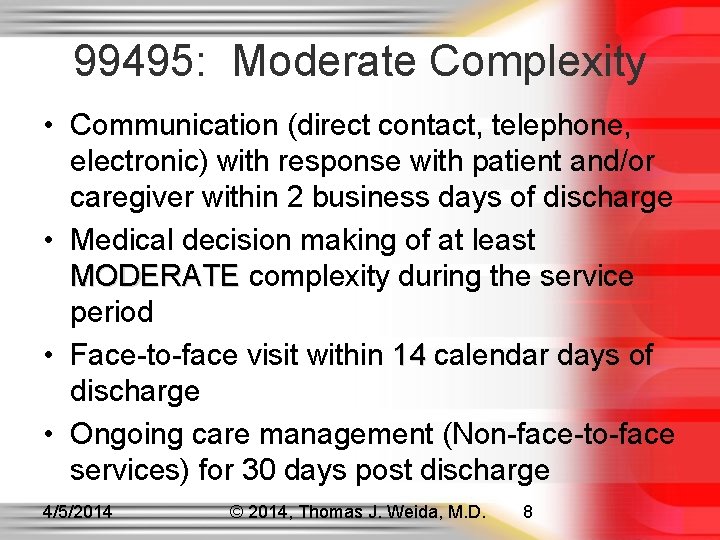
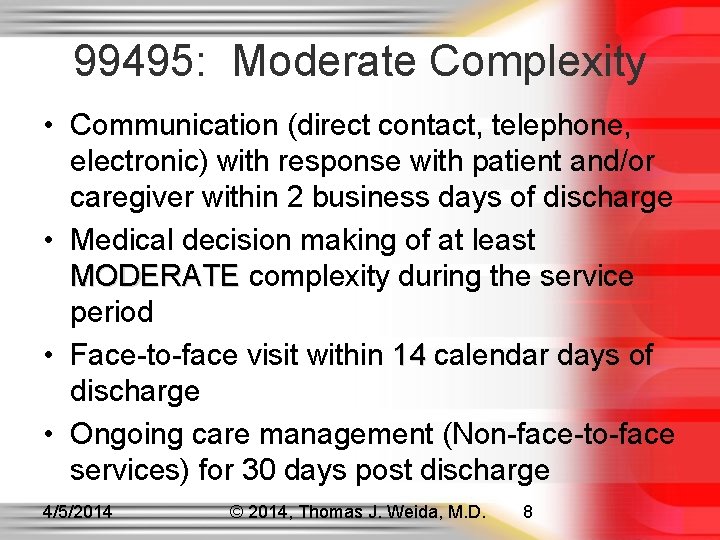
99495: Moderate Complexity • Communication (direct contact, telephone, electronic) with response with patient and/or caregiver within 2 business days of discharge • Medical decision making of at least MODERATE complexity during the service MODERATE period • Face-to-face visit within 14 calendar days of 14 discharge • Ongoing care management (Non-face-to-face services) for 30 days post discharge 4/5/2014 © 2014, Thomas J. Weida, M. D. 8
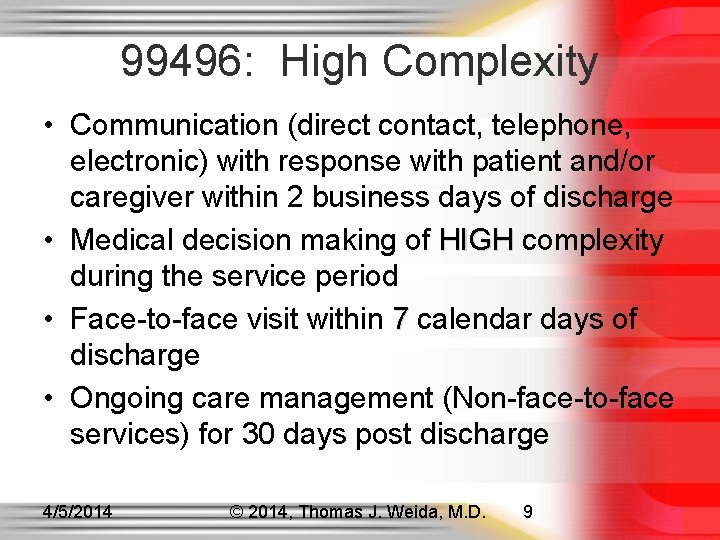
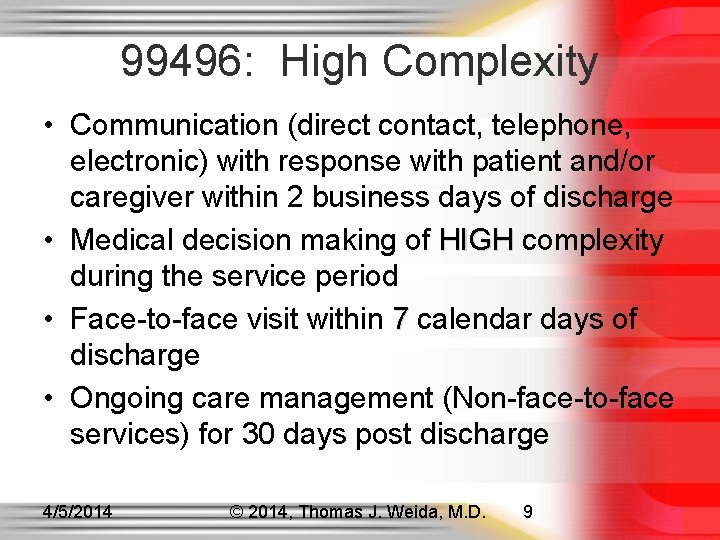
99496: High Complexity • Communication (direct contact, telephone, electronic) with response with patient and/or caregiver within 2 business days of discharge • Medical decision making of HIGH complexity HIGH during the service period • Face-to-face visit within 7 calendar days of discharge • Ongoing care management (Non-face-to-face services) for 30 days post discharge 4/5/2014 © 2014, Thomas J. Weida, M. D. 9
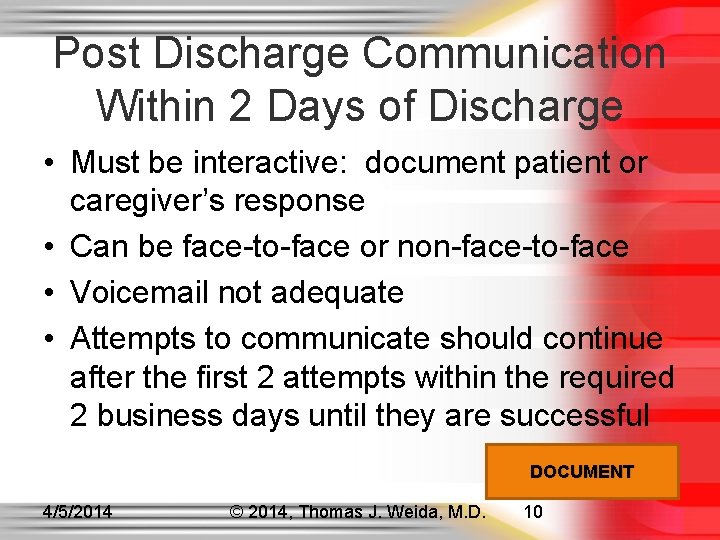
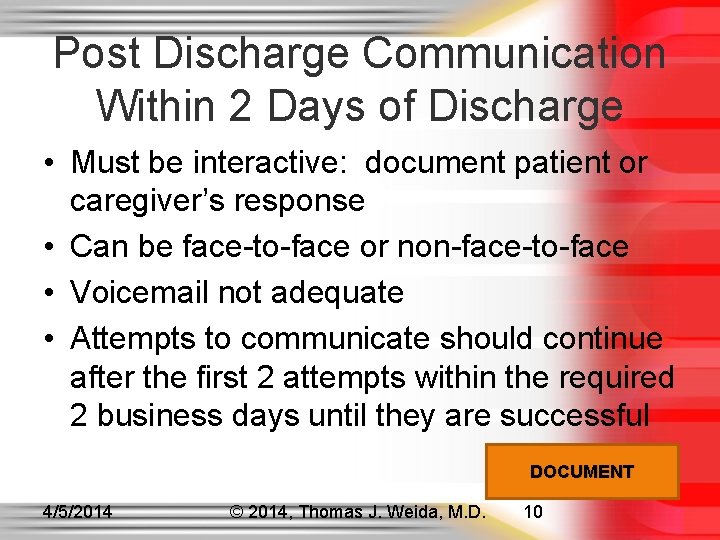
Post Discharge Communication Within 2 Days of Discharge • Must be interactive: document patient or caregiver’s response • Can be face-to-face or non-face-to-face • Voicemail not adequate • Attempts to communicate should continue after the first 2 attempts within the required 2 business days until they are successful DOCUMENT 4/5/2014 © 2014, Thomas J. Weida, M. D. 10
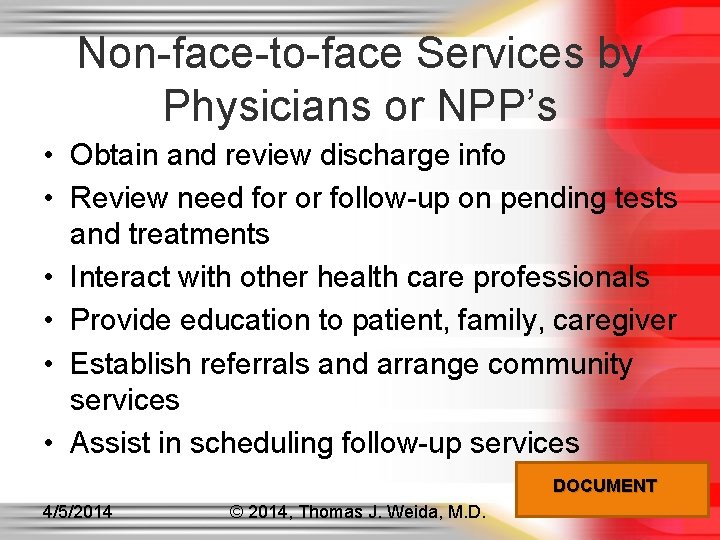
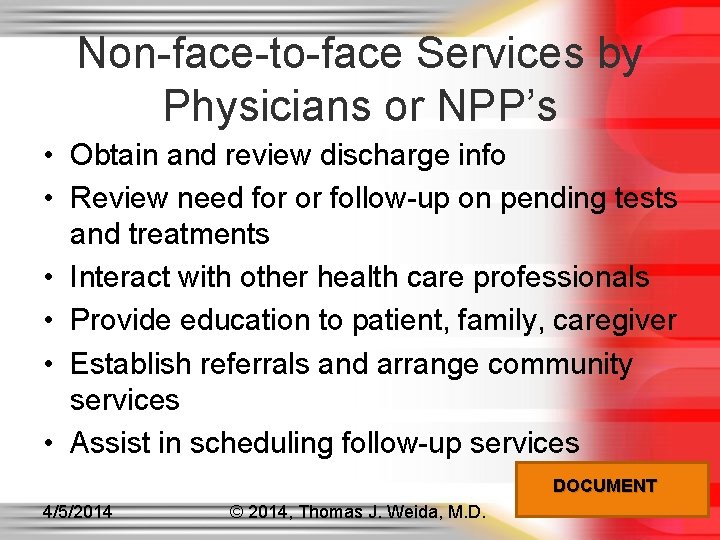
Non-face-to-face Services by Physicians or NPP’s • Obtain and review discharge info • Review need for or follow-up on pending tests and treatments • Interact with other health care professionals • Provide education to patient, family, caregiver • Establish referrals and arrange community services • Assist in scheduling follow-up services DOCUMENT 4/5/2014 © 2014, Thomas J. Weida, M. D. 11
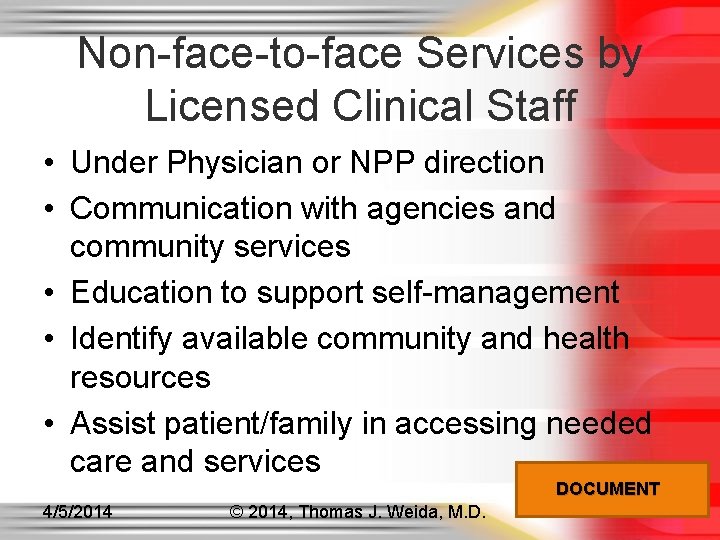
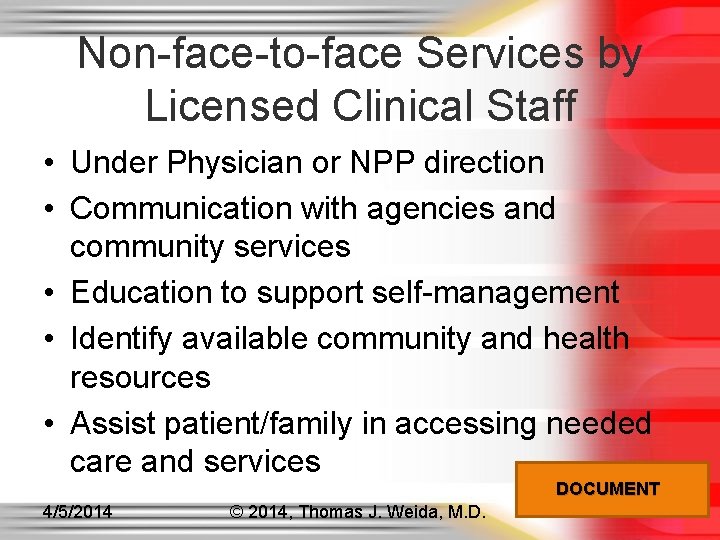
Non-face-to-face Services by Licensed Clinical Staff • Under Physician or NPP direction • Communication with agencies and community services • Education to support self-management • Identify available community and health resources • Assist patient/family in accessing needed care and services DOCUMENT 4/5/2014 © 2014, Thomas J. Weida, M. D. 12
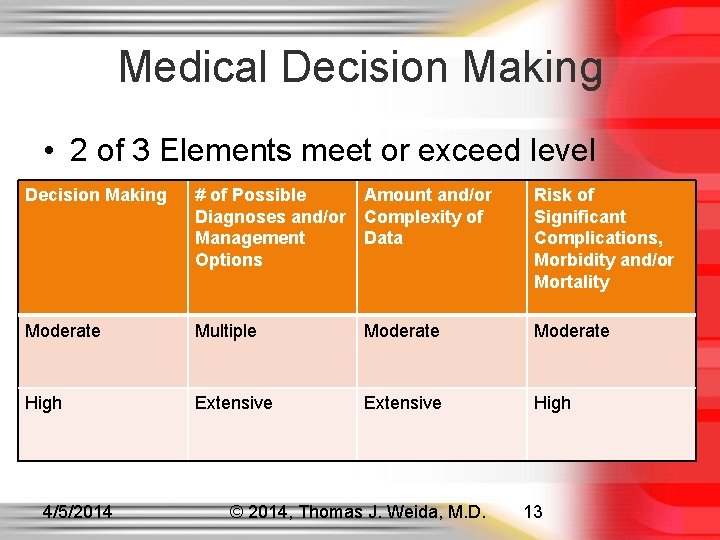
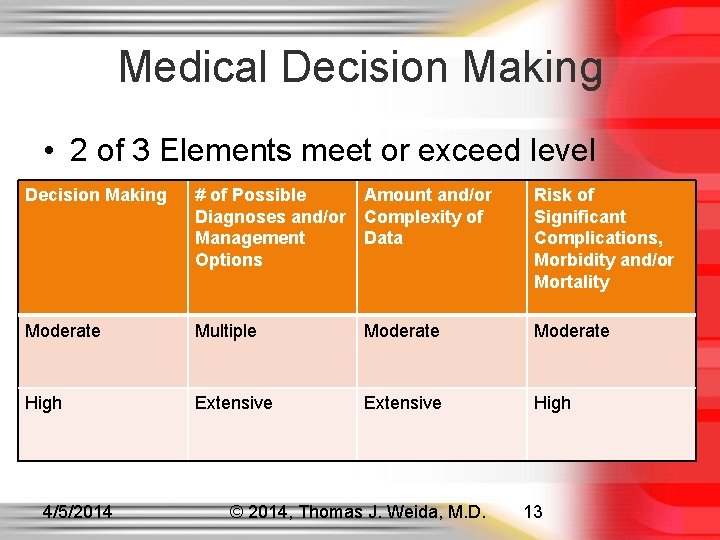
Medical Decision Making • 2 of 3 Elements meet or exceed level Decision Making # of Possible Diagnoses and/or Management Options Amount and/or Complexity of Data Risk of Significant Complications, Morbidity and/or Mortality Moderate Multiple Moderate High Extensive High 4/5/2014 © 2014, Thomas J. Weida, M. D. 13
Medication Reconciliation and Management • Furnished no later than the date of the Face-to-Face Visit DOCUMENT 4/5/2014 © 2014, Thomas J. Weida, M. D. 14
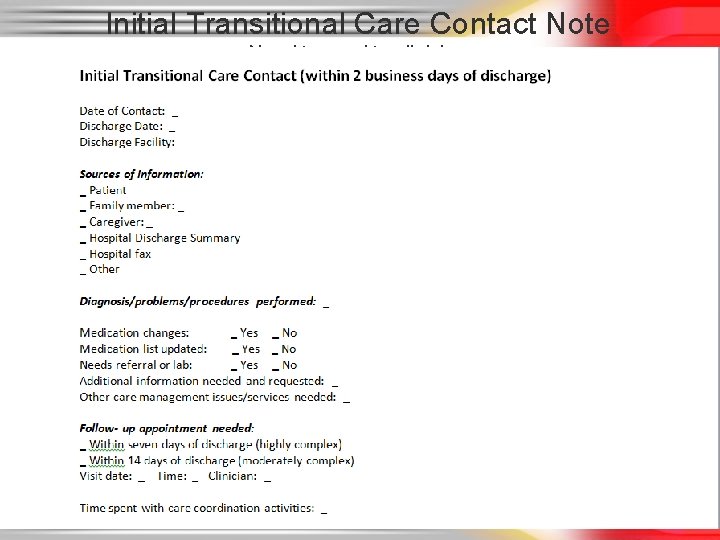
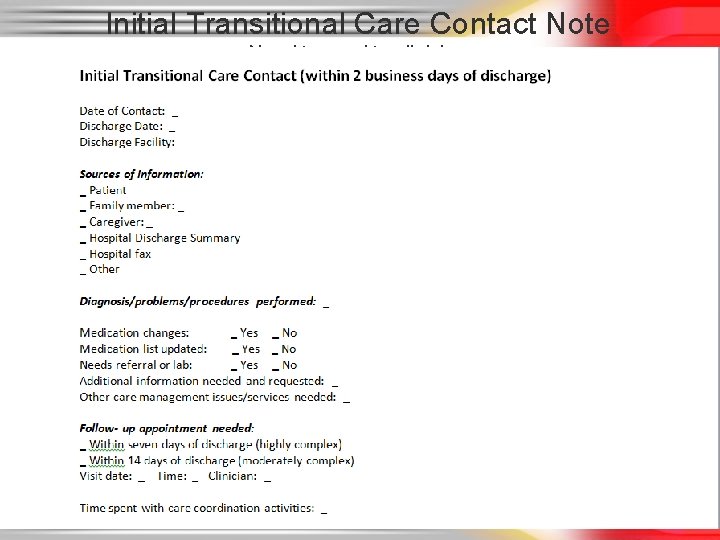
Initial Transitional Care Contact Note Need to send to clinician 4/5/2014 © 2014, Thomas J. Weida, M. D. 15
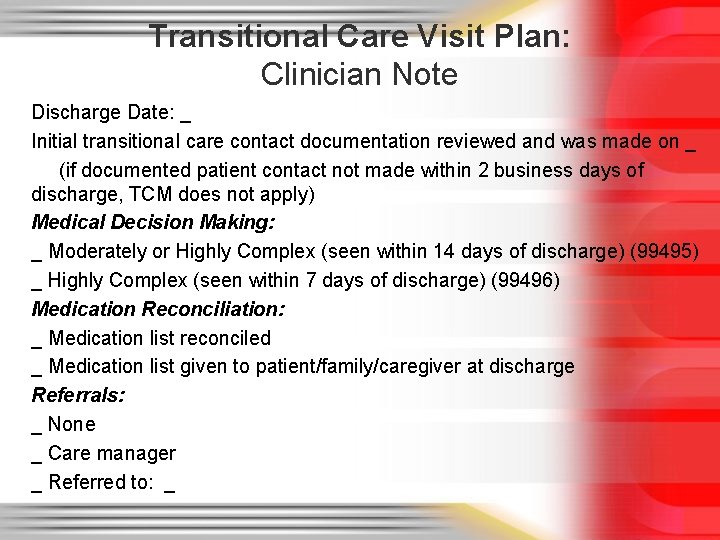
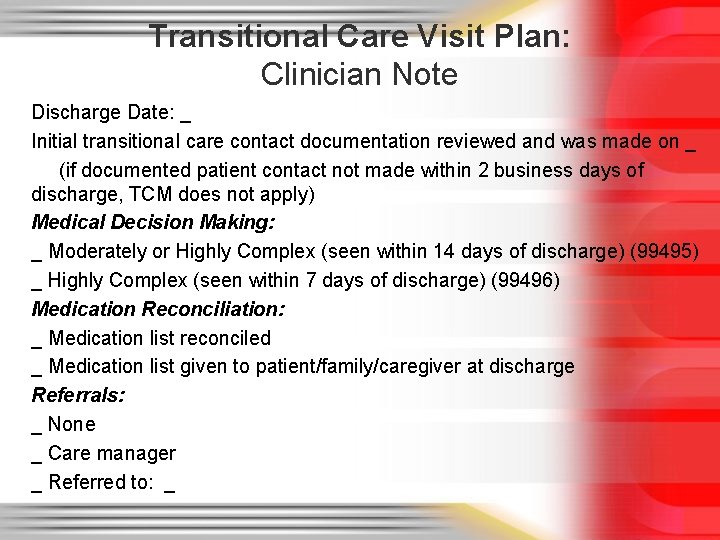
Transitional Care Visit Plan: Clinician Note Discharge Date: _ Initial transitional care contact documentation reviewed and was made on _ (if documented patient contact not made within 2 business days of discharge, TCM does not apply) Medical Decision Making: _ Moderately or Highly Complex (seen within 14 days of discharge) (99495) _ Highly Complex (seen within 7 days of discharge) (99496) Medication Reconciliation: _ Medication list reconciled _ Medication list given to patient/family/caregiver at discharge Referrals: _ None _ Care manager _ Referred to: _
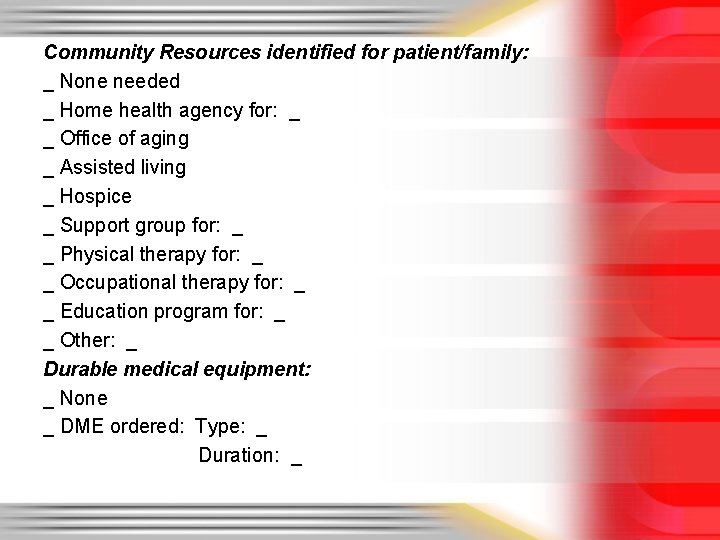
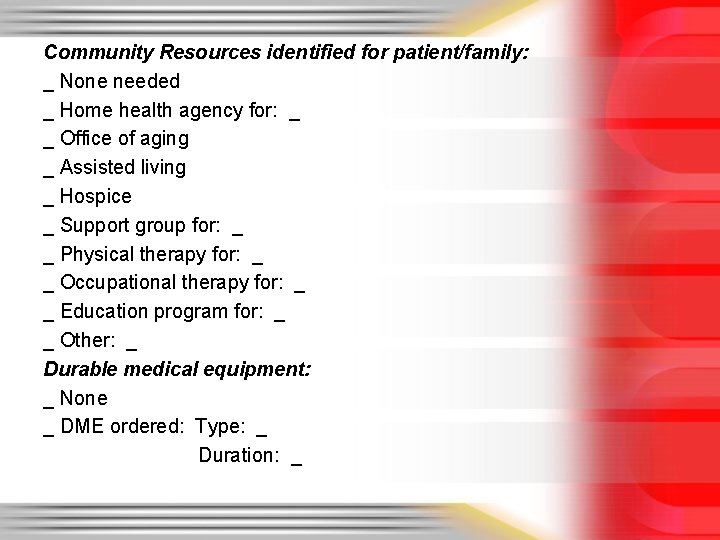
Community Resources identified for patient/family: _ None needed _ Home health agency for: _ _ Office of aging _ Assisted living _ Hospice _ Support group for: _ _ Physical therapy for: _ _ Occupational therapy for: _ _ Education program for: _ _ Other: _ Durable medical equipment: _ None _ DME ordered: Type: _ Duration: _
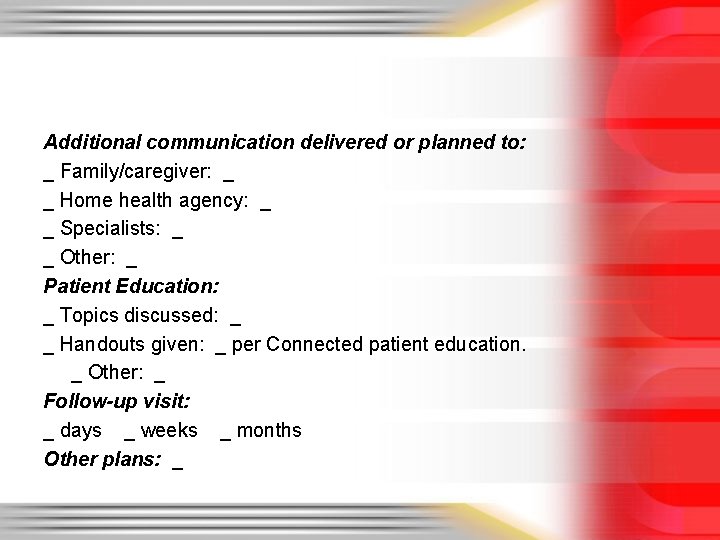
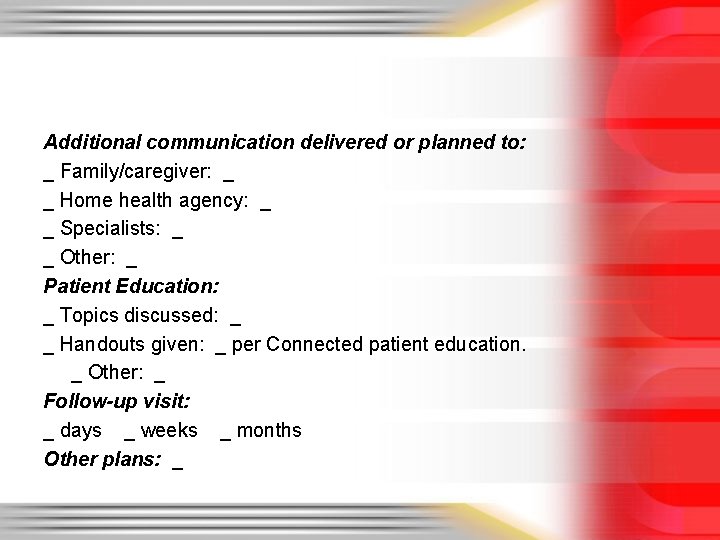
Additional communication delivered or planned to: _ Family/caregiver: _ _ Home health agency: _ _ Specialists: _ _ Other: _ Patient Education: _ Topics discussed: _ _ Handouts given: _ per Connected patient education. _ Other: _ Follow-up visit: _ days _ weeks _ months Other plans: _
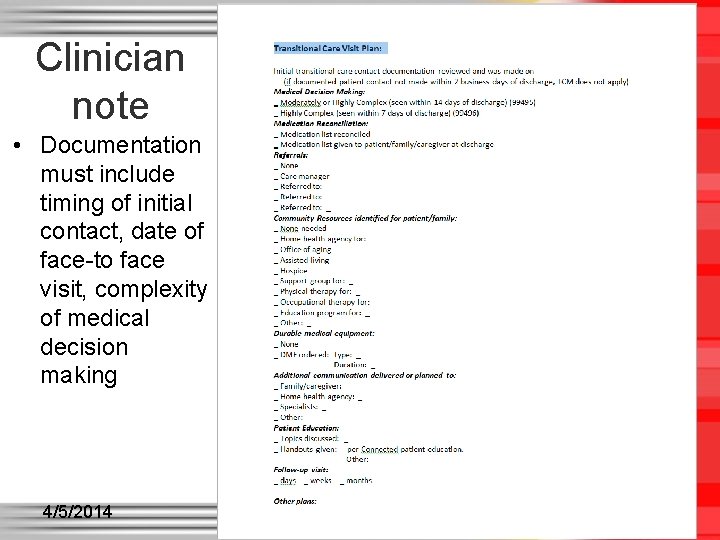
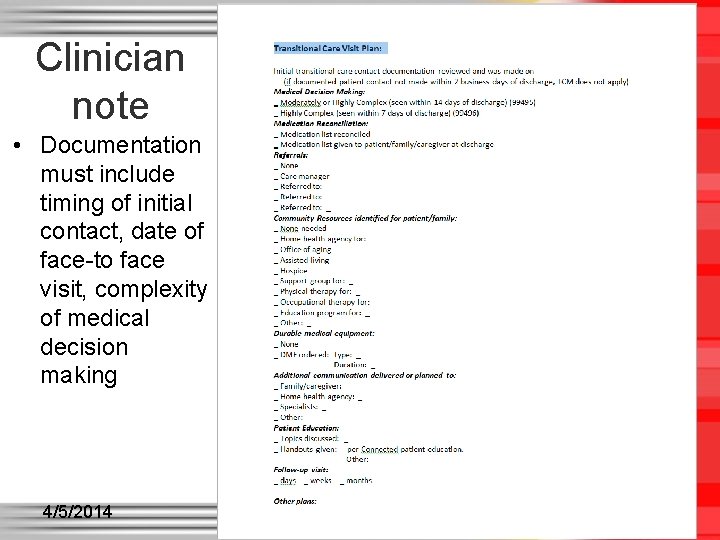
Clinician note • Documentation must include timing of initial contact, date of face-to face visit, complexity of medical decision making 4/5/2014 © 2014, Thomas J. Weida, M. D. 19
After face to face visit • Nurse care manager needs to document ongoing care management activities and ideally time spent doing care coordination/managing activities. • Note needs to be sent to clinician to review 4/5/2014 © 2014, Thomas J. Weida, M. D. 20
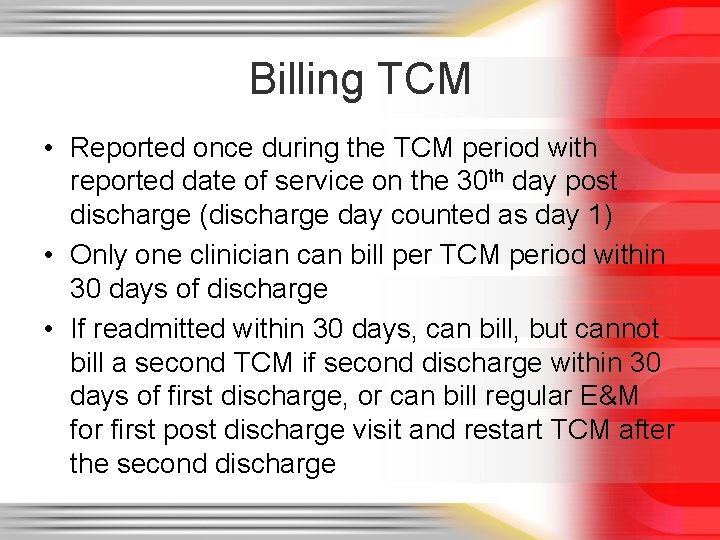
Billing TCM • Reported once during the TCM period with reported date of service on the 30 th day post discharge (discharge day counted as day 1) • Only one clinician can bill per TCM period within 30 days of discharge • If readmitted within 30 days, can bill, but cannot bill a second TCM if second discharge within 30 days of first discharge, or can bill regular E&M for first post discharge visit and restart TCM after the second discharge
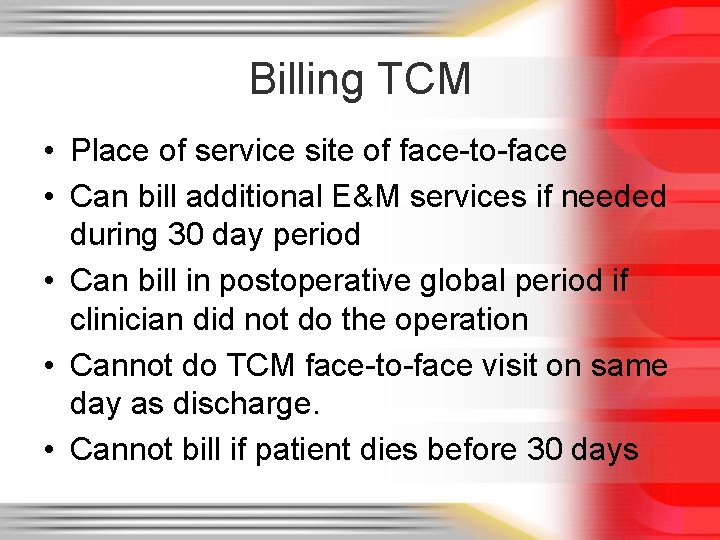
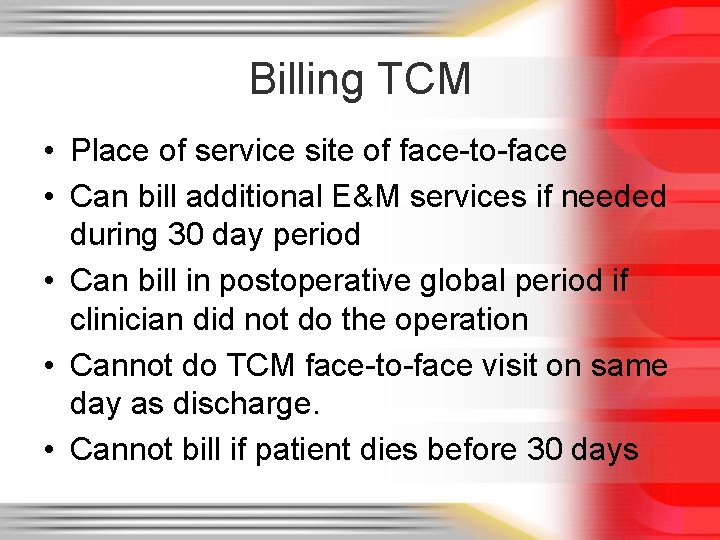
Billing TCM • Place of service site of face-to-face • Can bill additional E&M services if needed during 30 day period • Can bill in postoperative global period if clinician did not do the operation • Cannot do TCM face-to-face visit on same day as discharge. • Cannot bill if patient dies before 30 days
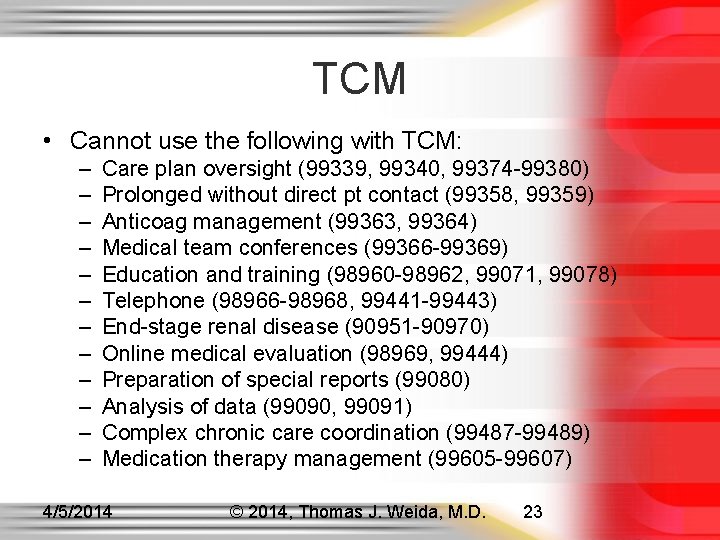
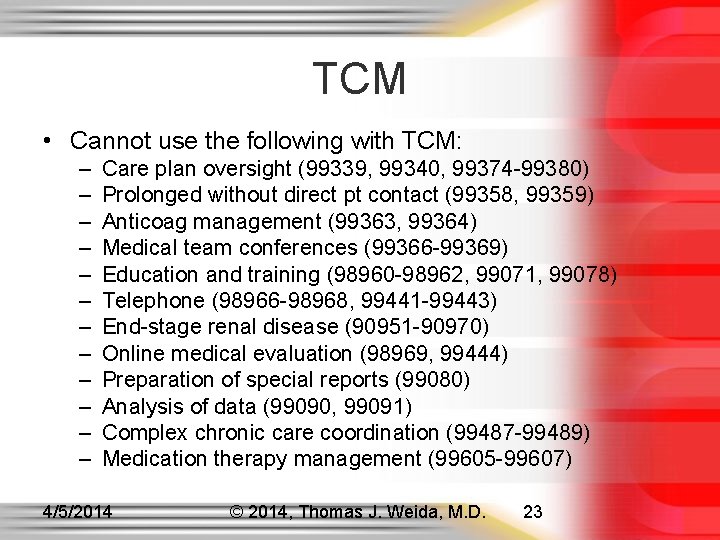
TCM • Cannot use the following with TCM: – – – Care plan oversight (99339, 99340, 99374 -99380) Prolonged without direct pt contact (99358, 99359) Anticoag management (99363, 99364) Medical team conferences (99366 -99369) Education and training (98960 -98962, 99071, 99078) Telephone (98966 -98968, 99441 -99443) End-stage renal disease (90951 -90970) Online medical evaluation (98969, 99444) Preparation of special reports (99080) Analysis of data (99090, 99091) Complex chronic care coordination (99487 -99489) Medication therapy management (99605 -99607) 4/5/2014 © 2014, Thomas J. Weida, M. D. 23
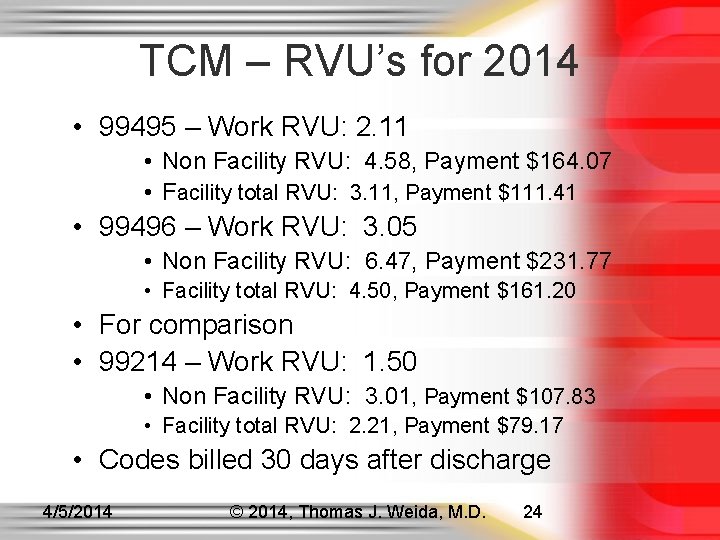
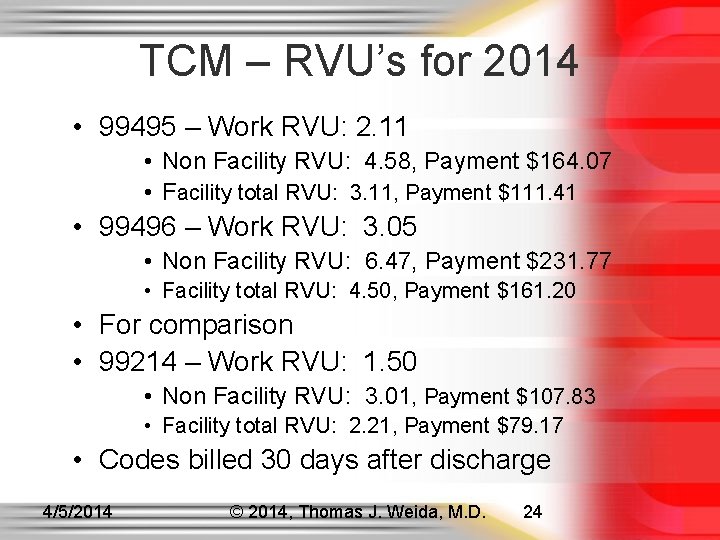
TCM – RVU’s for 2014 • 99495 – Work RVU: 2. 11 • Non Facility RVU: 4. 58, Payment $164. 07 • Facility total RVU: 3. 11, Payment $111. 41 • 99496 – Work RVU: 3. 05 • Non Facility RVU: 6. 47, Payment $231. 77 • Facility total RVU: 4. 50, Payment $161. 20 • For comparison • 99214 – Work RVU: 1. 50 • Non Facility RVU: 3. 01, Payment $107. 83 • Facility total RVU: 2. 21, Payment $79. 17 • Codes billed 30 days after discharge 4/5/2014 © 2014, Thomas J. Weida, M. D. 24
References • http: //www. aafp. org/dam/AAFP/documents/practi ce_management/payment/TCM 30 day. pdf • http: //www. aafp. org/dam/AAFP/documents/practi ce_management/payment/TCMFAQ. pdf • http: //www. cms. gov/Outreach-and. Education/Medicare-Learning-Network. MLN/MLNProducts/Downloads/Transitional-Care -Management-Services-Fact-Sheet. ICN 908628. pdf
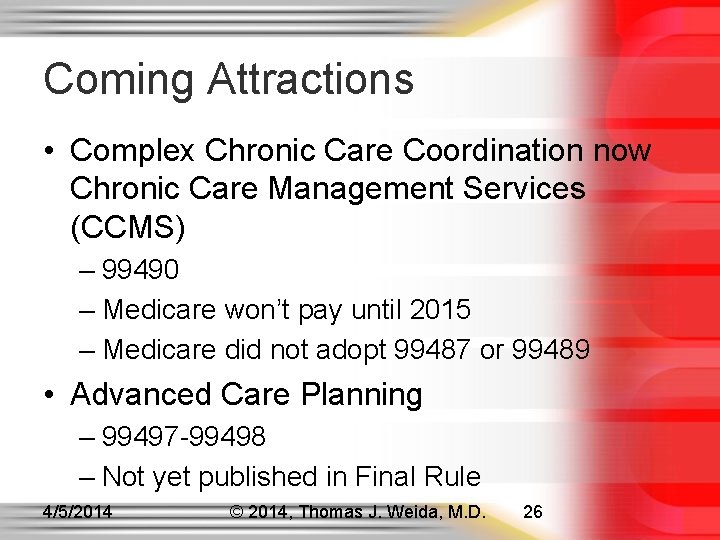
Coming Attractions • Complex Chronic Care Coordination now Chronic Care Management Services (CCMS) – 99490 – Medicare won’t pay until 2015 – Medicare did not adopt 99487 or 99489 • Advanced Care Planning – 99497 -99498 – Not yet published in Final Rule 4/5/2014 © 2014, Thomas J. Weida, M. D. 26
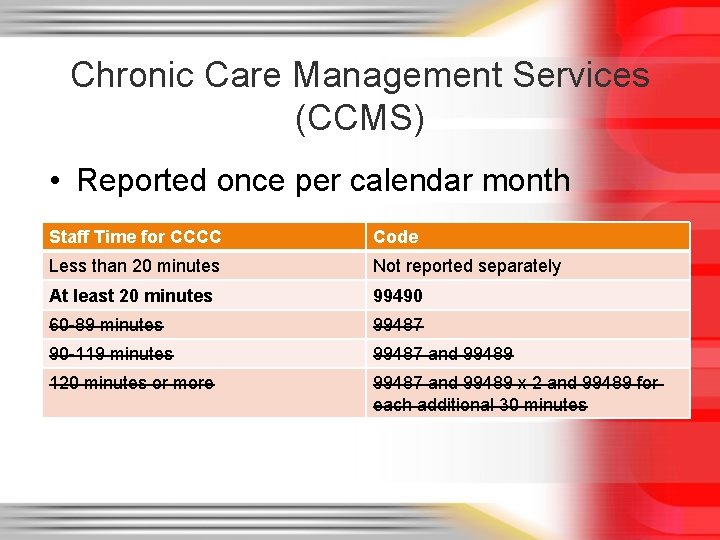
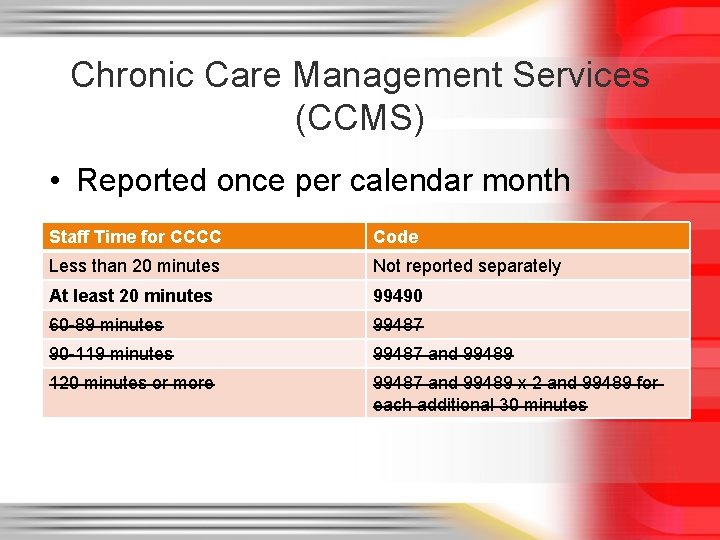
Chronic Care Management Services (CCMS) • Reported once per calendar month Staff Time for CCCC Code Less than 20 minutes Not reported separately At least 20 minutes 99490 60 -89 minutes 99487 90 -119 minutes 99487 and 99489 120 minutes or more 99487 and 99489 x 2 and 99489 for each additional 30 minutes
CMS CCMS Definition • “Furnishing care management to beneficiaries with multiple chronic conditions requires multidisciplinary care modalities that involve: regular physician development and/or revision of care plans; subsequent reports of patient status; review of laboratory and other studies; communication with other health professionals not employed in the same practice who are involved in the patient’s care; integration of new information into the care plan; and/or adjustment of medical therapy. ”
99490 • Multiple (2 or more) chronic conditions expected to last at least 12 months or until the death of the patient • Significant risk of death, acute exacerbation/decompensation or functional decline • Establishment or substantial revision of a comprehensive care plan • 20 minutes or more of clinical staff time directed by a physician or other qualified health care professional per calendar month • Cannot double count staff time (2 staff meeting) • Face-to-face visit not required
CCMS Office Requirements • 24/7 access/contact for acute chronic care needs • Continuity of care with a designated care team member with whom the patient can schedule successive routine appointments • Timely follow-up access and management after ER or discharge • EHR with timely access to clinical information • Standardized method to ID patients requiring CCM • Receives CCCC in a timely manner once identified • Standardized form and format for documentation • Educate patient & caregivers; coordinate care
CCMS Plan of Care • • • Problem list Expected outcome and progrnosis Measurable treatment goals Symptom management Planned interventions Medication management and reconciliation Community/social services ordered Communication with outside entities Written or electronic copy for patient
Typical Care Management • Communicate with patient, caregiver, professionals, home health agencies, community services • Collect health outcomes data and registry documentation • Self-management, independent living, and ADL support • Assessment and support for treatment and med manage • Identify available community and health resources • Facilitating access to care and services • Ongoing review of patient status, labs and studies • Development, communication, and maintenance of a comprehensive care plan based on a physical, mental, cognitive, psychosocial, functional and environmental assessment
99490 Billing • Can only bill once a month • Cannot be billed with CPT 99495 -99496, or CPT 90951 -90970 • Cannot be billed by multiple clinicians in same month • Patient must sign written agreement to have services provided, can withdraw at any time • Payment $42. 60
Advanced Care Planning • 99497 – Advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified healthcare professional; first 30 minutes, face-to-face with the patient, family member(s) and/or surrogate • 99498 – each additional 30 minutes
Advanced Care Planning • An advance directive is a document appointing an agent and/or recording the wishes of a patient pertaining to his/her medical treatment at a future time should he/she lack decisional capacity at that time. Examples of wri 1 tten advance directives include, but are not limited to, Health Care Proxy, Durable Power of Attorney for Health Care, Living Will and Medical Orders for Life-Sustaining Treatment (MOLST). • When using these codes, no active management of the problem(s) is undertaken during the time period reported. • Can be reported with another E&M code on the same day