Cervical Screening Programme March 2019 Why screening is





- Slides: 19

Cervical Screening Programme March 2019
Why screening is important? • There are 11 national screening programmes screening through the whole life course. • Screening is a way of finding out if people are at higher risk of a health problem so that early treatment can be offered or information given to help them make informed decisions. • Finding out about a problem early can mean that treatment is more effective. • The aim is to offer screening to the people who are most likely to benefit from it. For example, some screening tests are only offered to newborn babies, others such as breast screening and abdominal aortic aneurysm screening are only offered to older people.
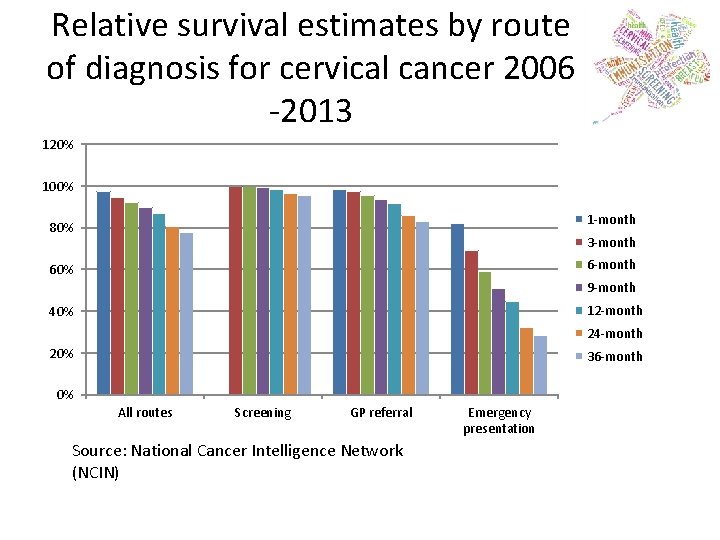
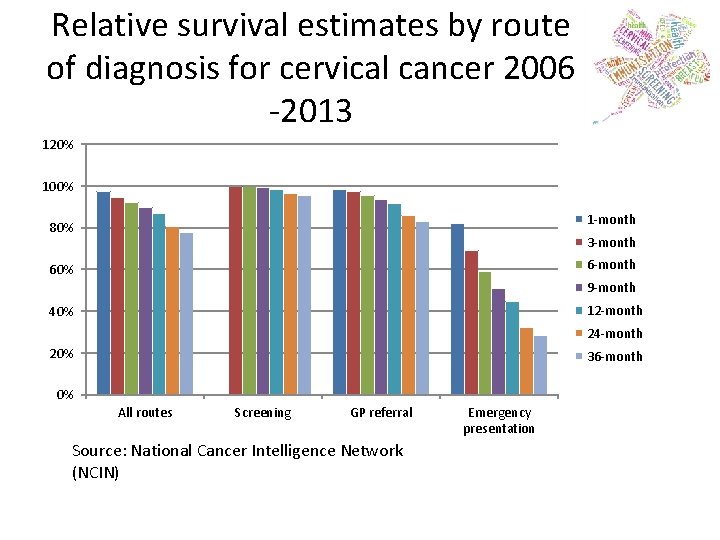
Relative survival estimates by route of diagnosis for cervical cancer 2006 -2013 120% 100% 1 -month 80% 3 -month 60% 9 -month 12 -month 40% 24 -month 20% 36 -month 0% All routes Screening GP referral Source: National Cancer Intelligence Network (NCIN) Emergency presentation

HPV • The Human Papilloma virus causes over 99% of cervical cancers of these 70% are caused by HPV types 16 and 18. • Since 2008 all girls have been offered the HPV vaccination in school. The vaccine protects against types 16 and 18 and types 6 and 11 which cause genital warts. • The HPV screening tests for all types of HPV that can cause cancer, which is why screening is still needed. It also can detect small cell cancers which are not HPV related. • Screening intervals may be extended in the future.
HPV • Understanding of HPV screening and what the results mean. The majority of women will come into contact with HPV during their lifetime and will clear the infection, however some women will have persistent infection and this is what causes abnormal cells. • Vaccinated women may think they do not need screening.
Key Messages The test doesn’t look for cancer. It looks for a virus/abnormal cells that if left could develop into cancer. Approximately 90% of women attending for screening have a normal result. More than ½ (52%) of cervical cancers in the UK are diagnosed in females under age 45. (2012 -2014). This will change as vaccinated women enter the programme. Women age 25 -35 are less likely to attend for screening, therefore having missed opportunities to have early abnormalities treated.


National Cervical Screening Campaign
Risks of cervical screening • The risks of cervical screening come from removing abnormal cells during a colposcopy and not from the screening test itself. • Removing abnormal cells can sometimes cause bleeding or an infection • It can also affect future pregnancies • Women who get pregnant after having abnormal cells removed are slightly more likely to have their baby 1 to 2 months early. NHS | Presentation to practice nurse forum 11
Symptoms • Symptoms of cervical cancer include: bleeding in between periods or after intercourse. Pain during intercourse. Postmenopausal bleeding, unusual vaginal discharge, lower back pain. • Anyone with symptoms should seek advice from their GP no matter what age they are. Screening is not appropriate for women with symptoms.
Reducing Risk • HPV vaccination for those eligible. • Attendance for screening when invited. • Higher incidence of cervical cancer in area’s of deprivation – women from lower socioeconomic groups are less likely to attend for screening. • Smoking is linked to a higher incidence of cervical cancer.
Issues in Practice Disabilities and special circumstances • Don’t assume women who are disabled or have learning disabilities are not sexually active. • Reasonable adjustments should be made to accommodate screening for these women. • Easy read literature is available for use. It is useful if practices know when a woman who may need literature in a different format is due to be invited – check the PNL.
Issues in Practice (con’t) • Female to male gender reassignment will fall outside normal call recall if they appear as a male on call/recall system. If they have a cervix the GP must act as call/recall. • Male to female gender reassignment will not require screening and will need to be ceased as no cervix.
Good Practice • If resources are short, concentrate efforts on those women who have never been screened. Regular screening is the best way to reduce risk of developing cervical cancer. • A lot of misconceptions exist regarding screening and these can be addressed by health professionals.
Useful Websites www. screening. nhs. uk www. cancerscreening. nhs. uk www. jostrust. org. uk www. gov. uk/government/organisations/publi c-health-england • https: //fingertips. phe. org. uk/profile/cancerse rvices • •
SIT Team england. lancashiresit@nhs. net
