National Cervical Screening Programme Smear taker update Ministry

- Slides: 31
National Cervical Screening Programme Smear taker update Ministry of Health, October 2015
Presentation overview • NCSP key messages • Coverage • History of the NCSP • Quality in the NCSP • HPV immunisation • Changing the primary laboratory test - future directions
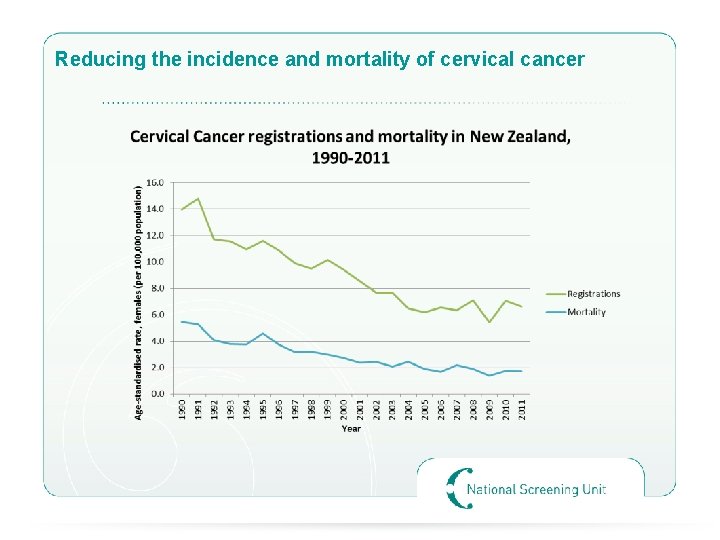
NCSP Key Messages • The NCSP is one of the most successful cervical screening programmes in the world. • We are reducing the incidence and mortality rate of cervical cancer by the detection and treatment of pre-cancerous squamous cell changes. • Cervical cancer is one of the most preventable of all cancers and screening every three years can reduce the risk of developing it by up to 90 percent.
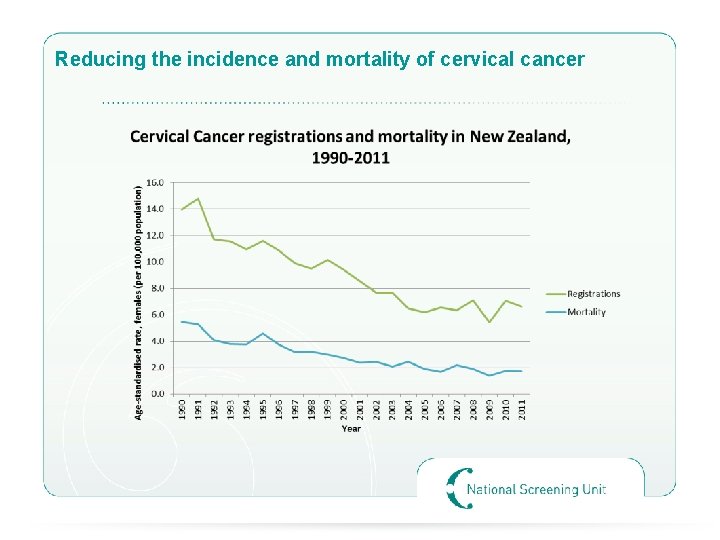
Reducing the incidence and mortality of cervical cancer
Key messages continued • Virtually all cervical cancers are caused by the human papillomavirus (HPV), which most people come into contact with at some stage in their life. • Regular cervical smear tests detects early cell changes that could lead to cervical cancer. Cervical screening every three years is recommended for women aged 20 to 70 years who have ever been sexually active. • Women who have had the HPV vaccine should also have regular cervical smears. • Having a smear test doesn’t take long and is a simple procedure that is proven to save lives.
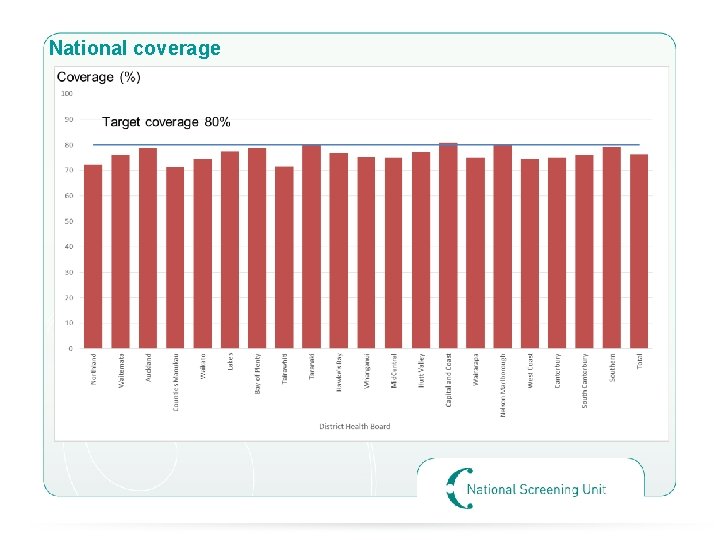
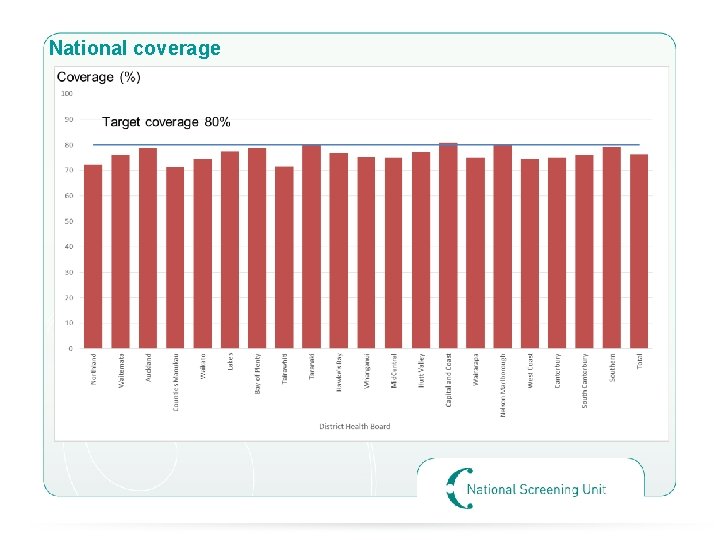
National coverage
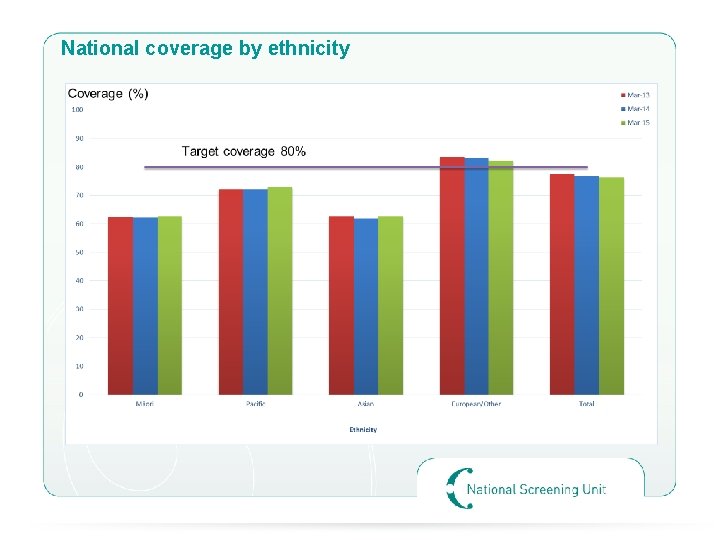
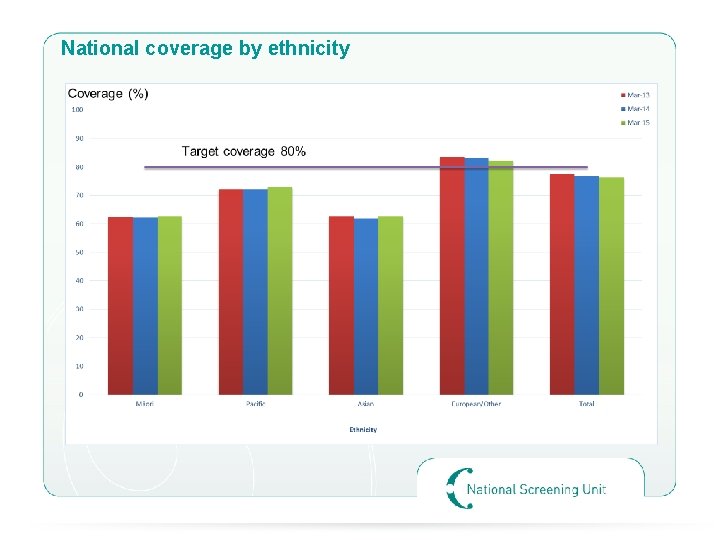
National coverage by ethnicity
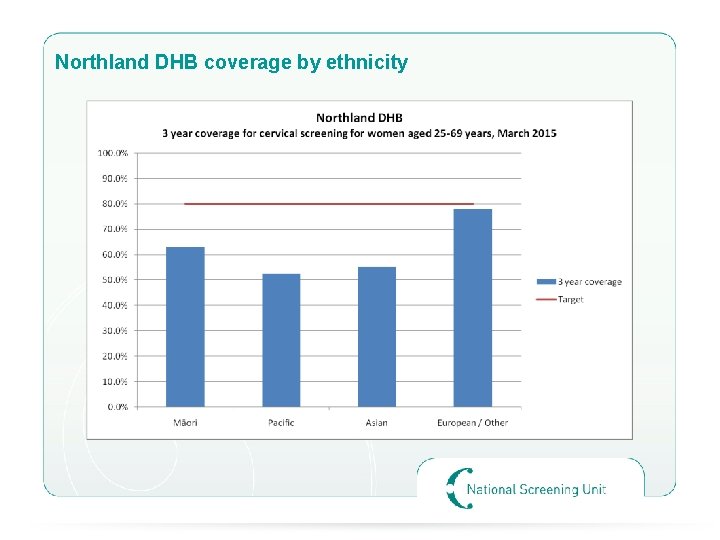
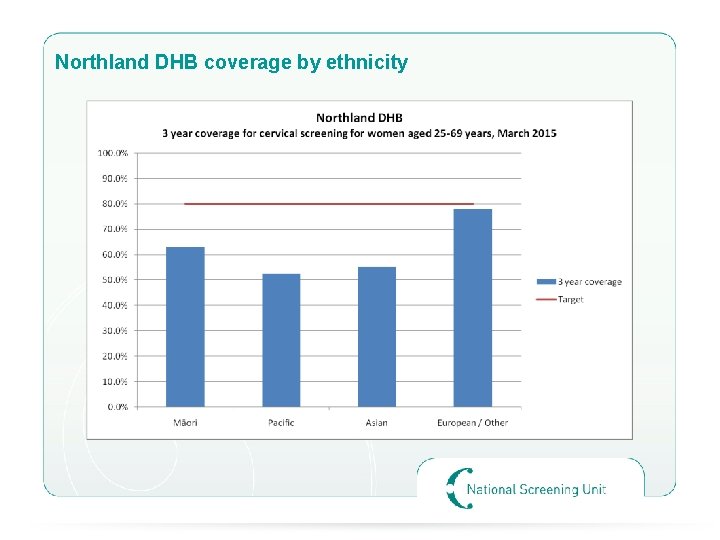
Northland DHB coverage by ethnicity
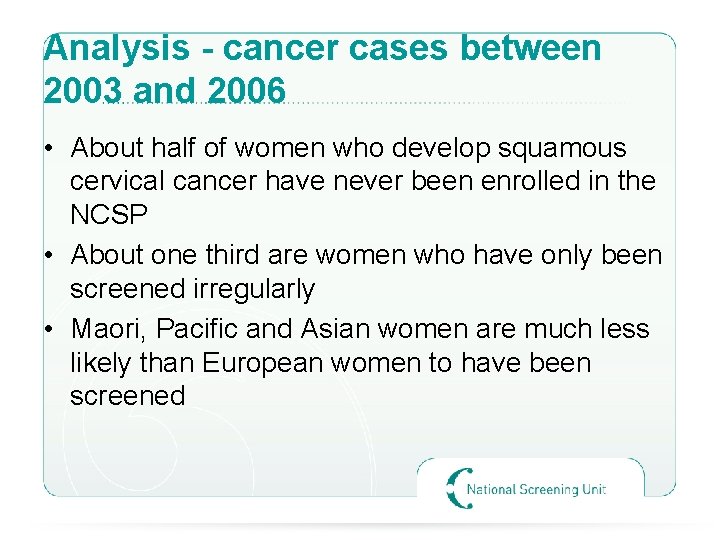
Analysis - cancer cases between 2003 and 2006 • About half of women who develop squamous cervical cancer have never been enrolled in the NCSP • About one third are women who have only been screened irregularly • Maori, Pacific and Asian women are much less likely than European women to have been screened
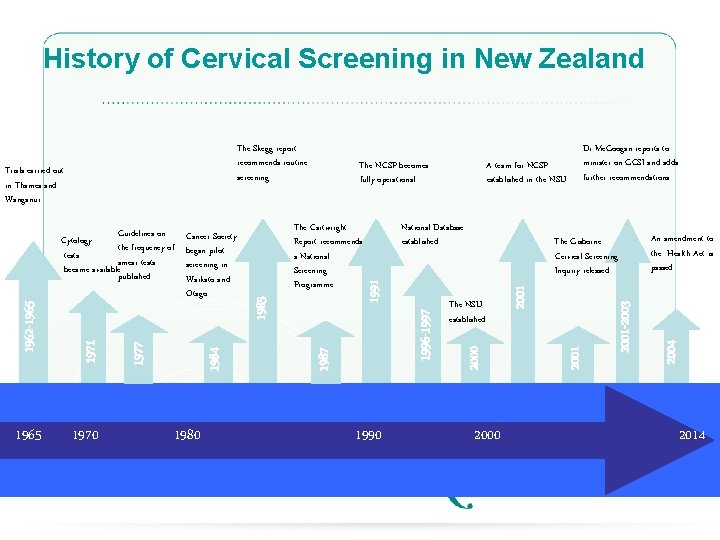
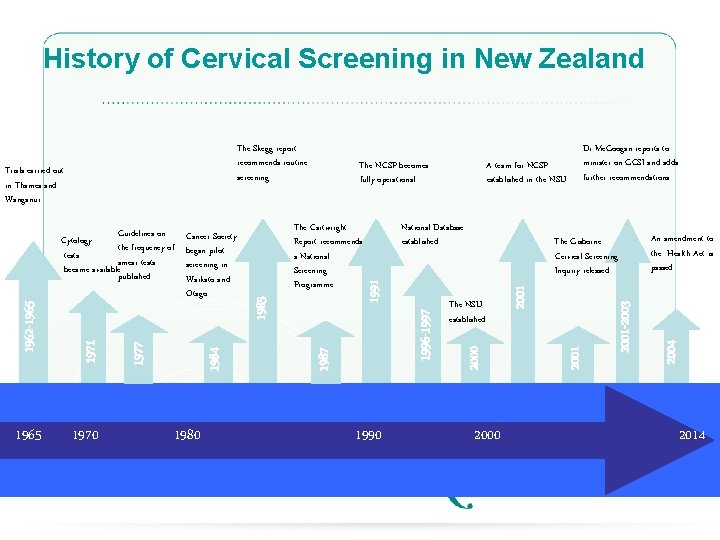
History of Cervical Screening in New Zealand 1965 1970 1980 National Database established 1990 2001 The NSU established 2001 -2003 The Gisborne Cervical Screening Inquiry released 2000 1996 -1997 1991 1985 The Cartwright Report recommends a National Screening Programme An amendment to the Health Act is passed 2004 A team for NCSP established in the NSU The NCSP becomes fully operational 1987 1984 1977 Guidelines on Cancer Society Cytology the frequency of began pilot tests smear tests screening in became available published Waikato and Otago 1971 1962 -1965 Trials carried out in Thames and Wanganui Dr Mc. Googan reports to minister on GCSI and adds further recommendations 2001 The Skegg report recommends routine screening 2014
The NCSP today • Health Act 1956 • NCSP Policies and Standards • Guidelines for Cervical Screening in NZ • The Ministry’s NCSP team and what we do: • National team of six people (supported by other teams) • Contract and relationship management – DHB regional services, colposcopy, labs, audit and monitoring providers, NCSP-Register • Social Marketing • Working with the Ministry’s Immunisation team re HPV vaccination • Regional NCSP teams in DHBs, primary care, labs, colposcopy services
NCSP Policies and Standards • NCSP Policies and Standards cover all parts of the programme (colposcopy, laboratories, Register, smear taking, regional services) • Section 4 covers responsibilities for smear takers • Training • Quality • Improving women’s participation • Providing information • Infection control • Taking a smear • Communication • Information required by the laboratory • Referral and follow up
Guidelines for cervical screening in NZ • Incorporate key NCSP policies such as recommendations as to the age to start screening, how often to screen and when to stop. • Based on extensive review of evidence together with expert advice from a wide range of medical practitioners, epidemiologists and consumer representatives. • Set the screening pathway – what do with women who have had normal or abnormal smears and when to request an HPV test
HPV e-learning – free to complete –http: //learnonline. health. nz/ • Information about HPV testing in the NCSP, designed for smear takers
NCSP Quality initiatives • Achieving equity - Maori Health Plans - Free smears - Support to screening services • Monitoring the performance of the programme • NCSP-Register management • Laboratories and colposcopy monitoring and audit • Working with regional services to improve programme delivery
Informing women of abnormal results • The smear taker has primary responsibility for informing women of their results. The NCSP-Register letters provide a back up. • There are sometimes complaints where smear takers have not informed women of their abnormal smear result • With abnormal results, it’s important for women to understand the results, be able to ask questions, and get further information or support if they need it.
Correct labelling of smears • If you don’t label the smear vial correctly, the lab may have to discard the specimen, and the woman may need to return for another smear. • Details on the form and the specimen need to match –family or surname and given names –NHI number –Ethnicity (measures coverage) –postal address (so Register letters can be sent) . Ideally, date of birth will be included too.
Engaging women to have smears • Low knowledge of cervical screening – younger women don’t know anyone who has had cervical cancer. “Lack of importance” of cervical cancer. • “abnormal cells/ precancerous cells” are confused with cancer • Promotion of “wellness” is powerful – a call to action. We are preventing cancer. • Need cultural sensitivity in communicating about female body parts • Personal engagement is better than compliance brought by nagging. • Women had a smear when they wanted the pill. Not prepared for having a smear; don’t understood why they need to have routine smears.
Women’s experiences. . . (Phoenix Research Report) • Women interviewed pulled back in their chairs, held themselves rigid, screwed up their faces, clenched their fists and gritted their teeth when they recalled their screening experiences. • The test procedure is a “big deal” and they need a “big reason” to come back. Women felt violated, trust was broken. • A women’s equilibrium is shaken and not re-established before they leave – “a cup of tea would have been nice!” • Poor previous experience (eg unexpected pain) prevents ongoing participation. Warn women there may be discomfort, and don’t minimise it. • Game of “cat and mouse” with primary care re having smears. The importance of screening to primary care is out of line with the importance women place on it. The “health system’s” test, not “my” test.
It can be a good experience! • • • “Very easy person to talk to. Different position was nice. Great manner. Love your nursing philosophy. ” “Appreciated being given options. Enjoyed L) lateral position (for first time). ” “You are wonderful – the best nurse I’ve ever met! Felt so comfortable and safe” “It’s been lovely coming here” “Most painless experience. Didn’t even know it was being done” “Fantastic. Easiest smear ever!” ”Painless and comfortable (after past experiences). Felt safe and relaxed”. “So glad I did it and got you. Much easier and nicer than I expected” (first smear) “Fantastic – You were wonderful. Best smear ever (usually very painful)” “What a relief after last traumatic experience! So relieved it was so easy”. “Best smear ever; awesome; easy”. “Relaxed and enjoyable”.
Champions • Be a cervical screening champion in your practice! • Work with your PHO to get electronic data matching information and have completely up to date recall lists • Try innovative and personalised methods to engage women • Refer women to alternative screening locations as appropriate • The DHB regions with the best coverage have great regional coordination and leadership to engage primary care and support them to reach the women.
HPV immunisation • Together, immunisation and screening will offer the most effective protection against cervical cancer. • HPV immunisation coverage 61% for all ethnicities – better for Pacific, Asian and Māori • Protects against high-risk HPV (16 and 18) that cause up to 70% of cervical cancer. Also protects against genital warts (HPV 6 and 11) • Free for girls and young women up to their 20 th birthday. • Available through participating schools, family doctors, local health centres and some Family Planning clinics. Primary care can follow up girls who were not vaccinated in the school based programme • Immunised or not, women still need to participate in regular cervical screening. The vaccine does not protect against all hr. HPV types.
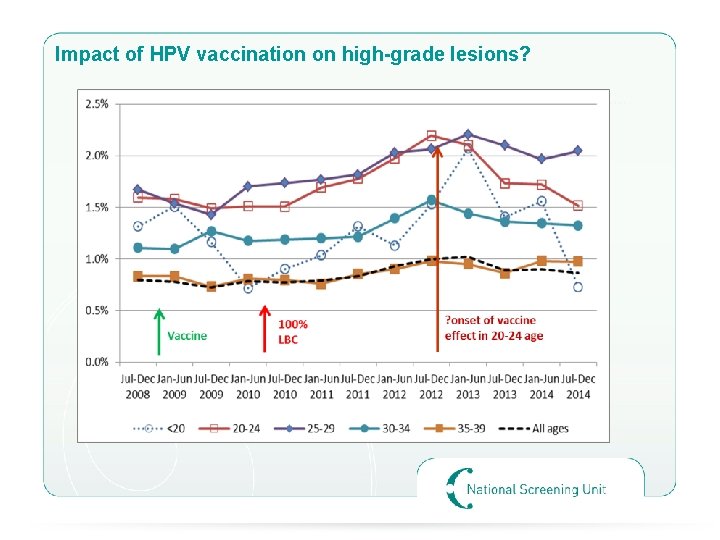
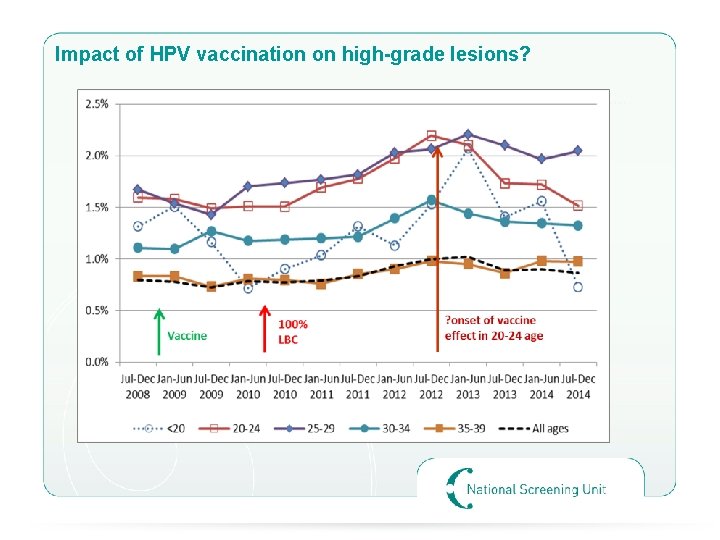
Impact of HPV vaccination on high-grade lesions?
Future direction - Changing the primary laboratory test
Primary HPV Screening • Plan to change from cytology as the primary test, to HPV screening as the primary test by 2018.
Guiding principles: • deliver a best practice national cervical screening programme • improve equitable access to screening for women in all population groups • be acceptable to women • maintain and improve safety and quality of screening for enrolled women • maintain a skilled and competent workforce to deliver the programme • consultation with a wide range of stakeholders to ensuring a smooth transition to the new primary screening pathway • maintain and improve the NCSP-Register’s capability required to support the programme.

Key points and questions • A woman still needs to have a smear • 5 yearly screening interval with primary HPV testing? • Screening age range 25 – 69? • Same pathway for unvaccinated and vaccinated women • Consideration of self-sampling? • Fewer cervical cancer cases and deaths • Fewer smears throughout a woman’s life • Potentially more cost effective than the current programme • The Register would need significant change
Next steps • • Public consultation has started and closes on 23 October What do you think? • Business as usual until 2018!
www. nsu. govt. nz
Questions?