Central Venous Catheter CVC Overview of how to
- Slides: 25
Central Venous Catheter (CVC) Overview of how to access/care for Patients with Central Venous Access Devices (CVAD)
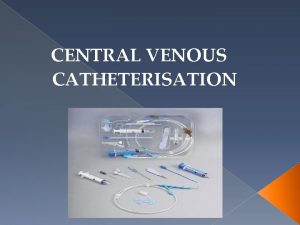
Central Venous Catheter (CVC) CVC- An indwelling catheter used where the need for Central Venous access is prolonged or essential to administer drugs A CVC terminates at or close to the heart or in one of the great vessels leading to the heart – SVC/ IVC
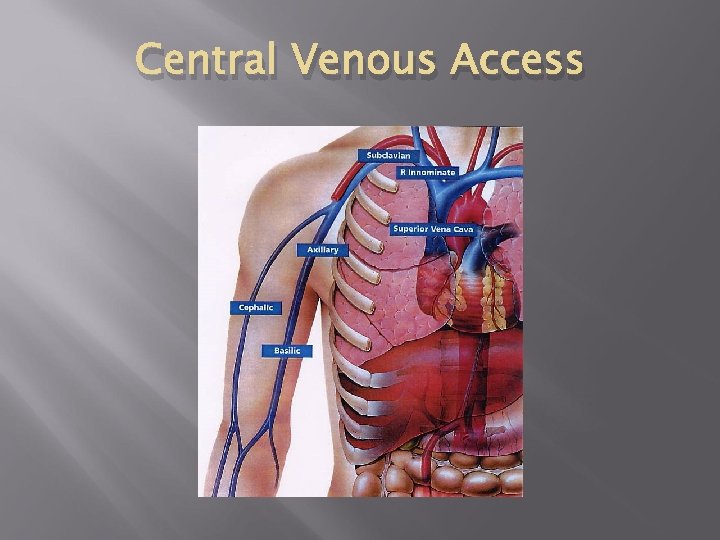
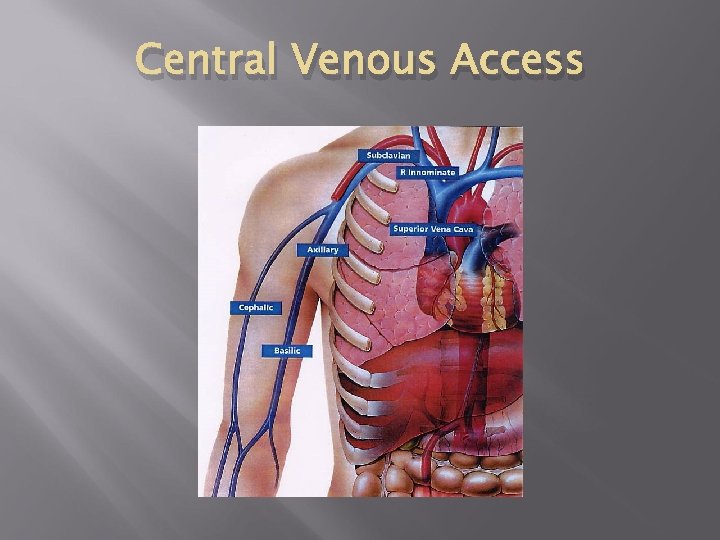
Central Venous Access
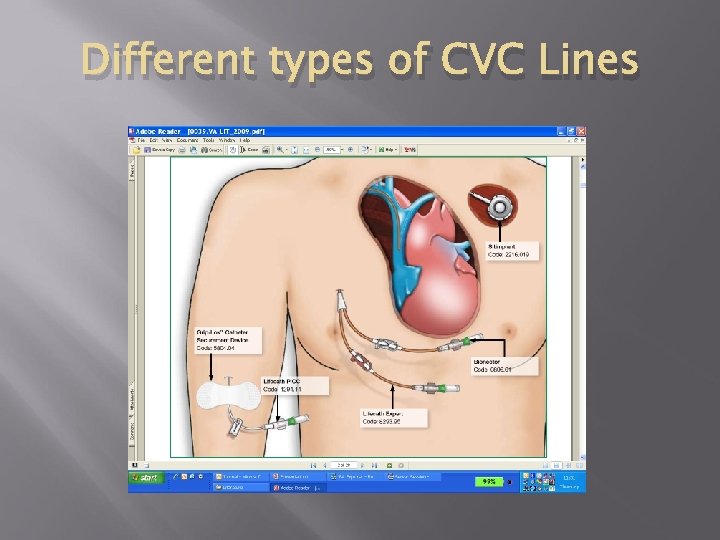
Types of CVC, S Hickman line Peripherally inserted central catheter PICC Midline Portacath
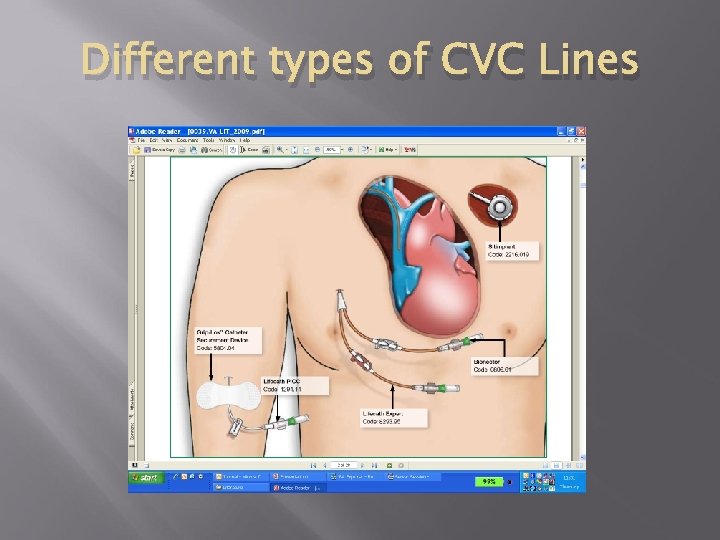
Different types of CVC Lines
Criteria for competence flushing and dressing a CVAD Practitioners must : have undertaken training including theory and simulated practice must have passed a practical assessment demonstrate knowledge of the trust Blood transfusion policy Be accountable for their own practice and ensure their practice remains up to date in line with local policy (NMC 2008). Take part in appropriate learning and practice activities that maintain and develop your competence and performance
Indications for CVC Used frequently in Haematology/Oncology for Drug and fluid administration: Infusional chemotherapy pumps Long chemotherapy regimens Bone Marrow Transplant Intermediate-long term Intravenous antibiotics Poor venous access Breast cancer patients - Axillary node clearance The patient can remain at home for part/all of their treatment Nutritional support (TPN) Assessment by (TPN) Nutrition Specialist Team ) Blood samples Patient choice
Contraindications Administration of drugs via a CVAD will not take place if: The Patient refuses treatment There is any concern over patency i. e the device is not flushing or aspirating as it should be There is any concern re the position of the device i. e the exit length has moved (picc) or signs of displacement.
Limitations to practice Oncology Nurses Radiographic evidence of catheter position is not documented (Important if administering vesicant drugs) Length of line inserted (cm) not documented to compare with exit length prior to use. Suspected line infection or thombosis
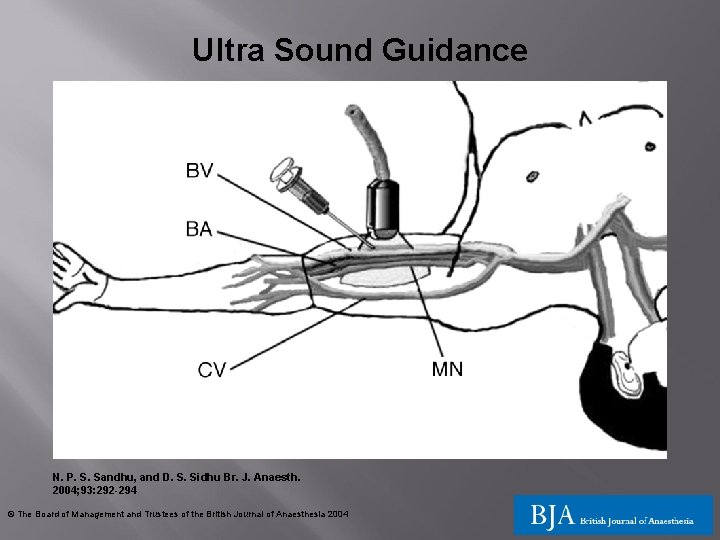
Placement of CVAD’s Hickman lines are inserted under radiological guidance in x-ray Directly into one of the central veins, the superior or inferior vena cava, both of which return blood into the right atrium and have the largest blood flow of any veins in the body PICC lines are generally inserted by specialist nurses via the cephalic/median/basilic veins and the tip is in the superior vena cava under ultra sound guidance X-ray following insertion to confirm correct placement
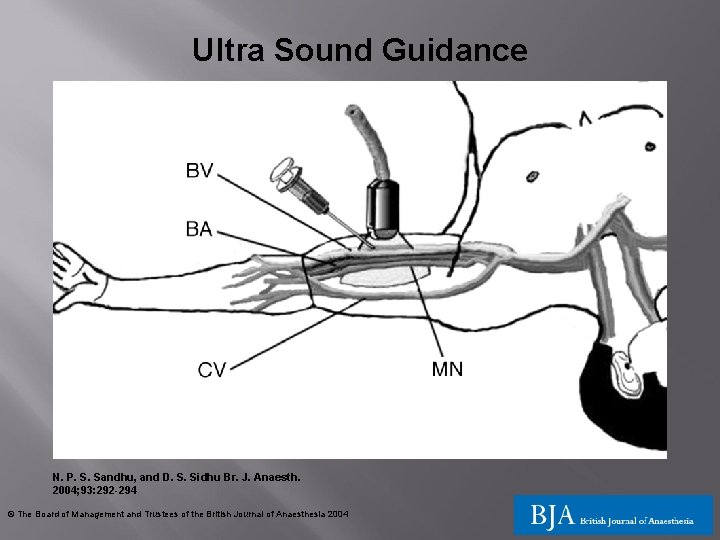
Ultra Sound Guidance N. P. S. Sandhu, and D. S. Sidhu Br. J. Anaesth. 2004; 93: 292 -294 © The Board of Management and Trustees of the British Journal of Anaesthesia 2004
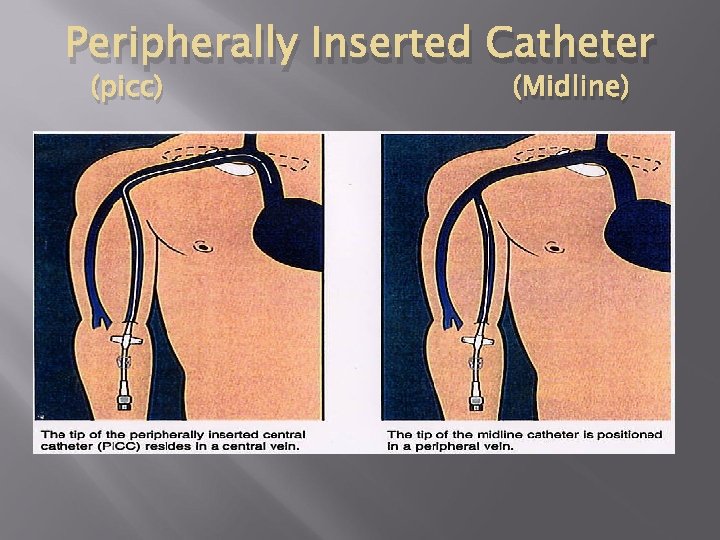
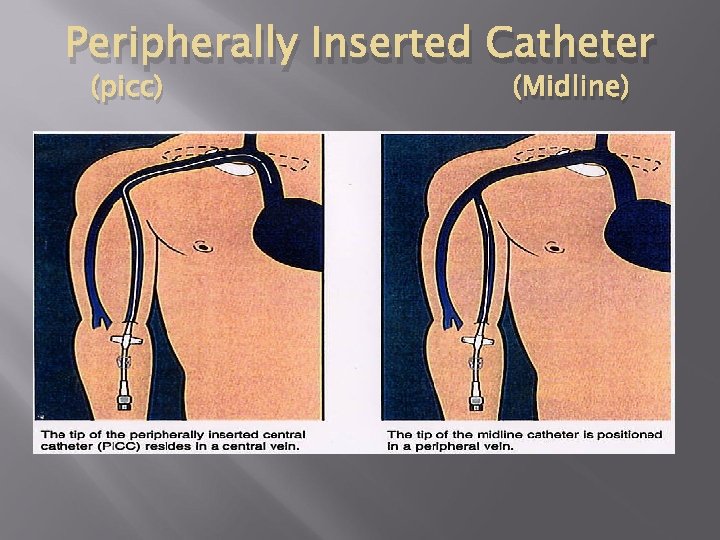
Peripherally Inserted Catheter (picc) (Midline)
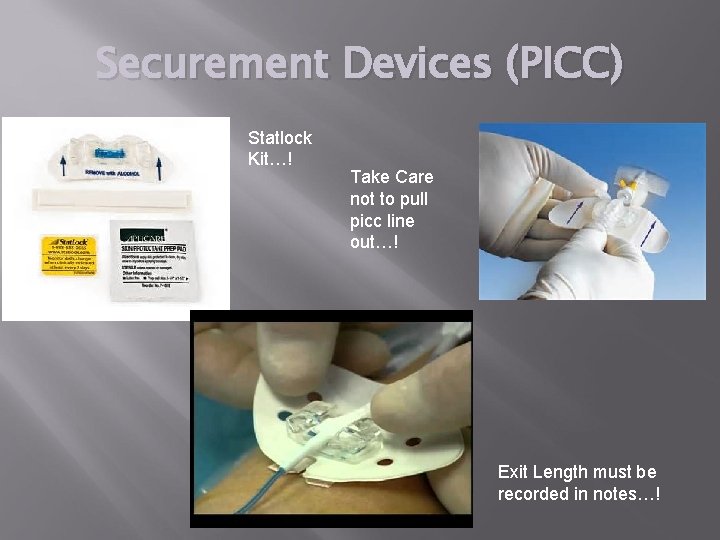
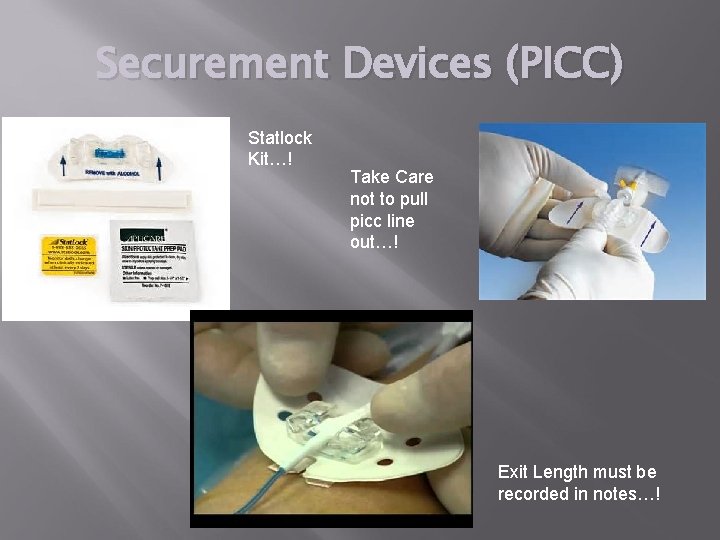
Securement Devices (PICC) Statlock Kit…! Take Care not to pull picc line out…! Exit Length must be recorded in notes…!
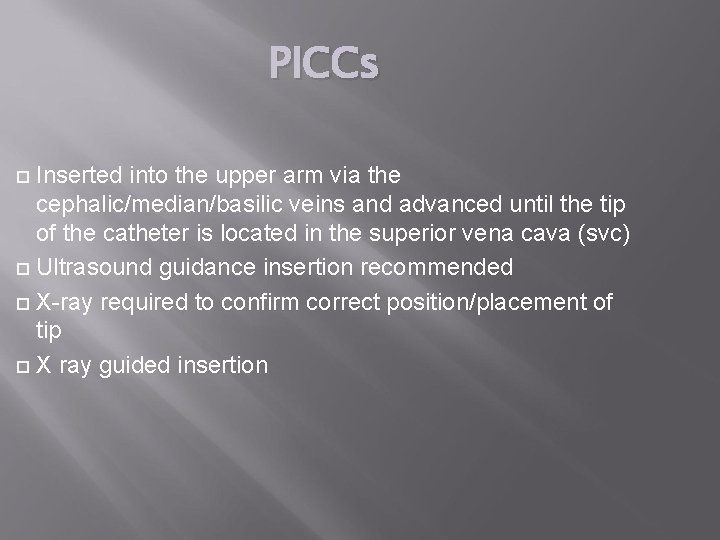
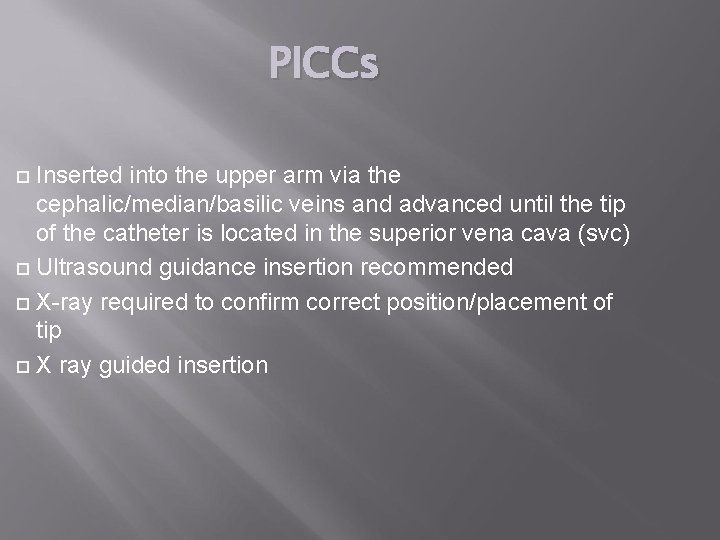
PICCs Inserted into the upper arm via the cephalic/median/basilic veins and advanced until the tip of the catheter is located in the superior vena cava (svc) Ultrasound guidance insertion recommended X-ray required to confirm correct position/placement of tip X ray guided insertion
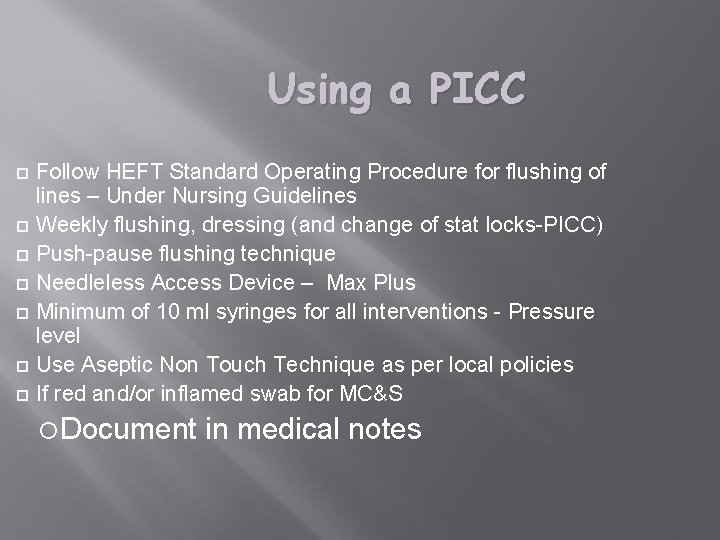
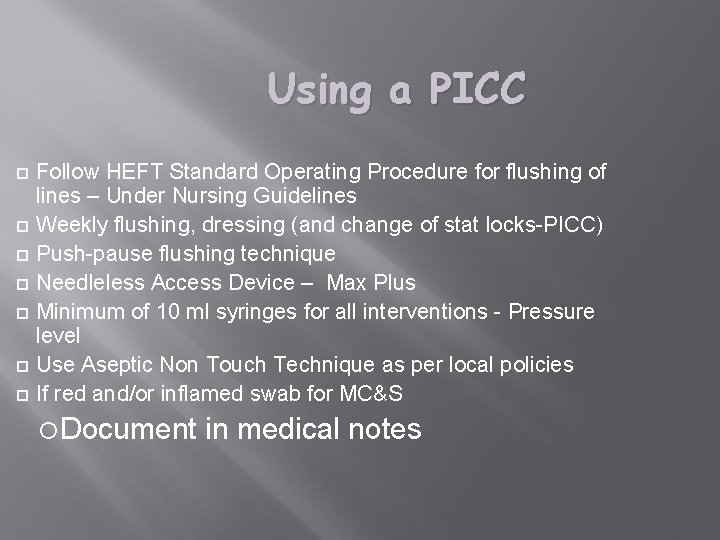
Using a PICC Follow HEFT Standard Operating Procedure for flushing of lines – Under Nursing Guidelines Weekly flushing, dressing (and change of stat locks-PICC) Push-pause flushing technique Needleless Access Device – Max Plus Minimum of 10 ml syringes for all interventions - Pressure level Use Aseptic Non Touch Technique as per local policies If red and/or inflamed swab for MC&S Document in medical notes
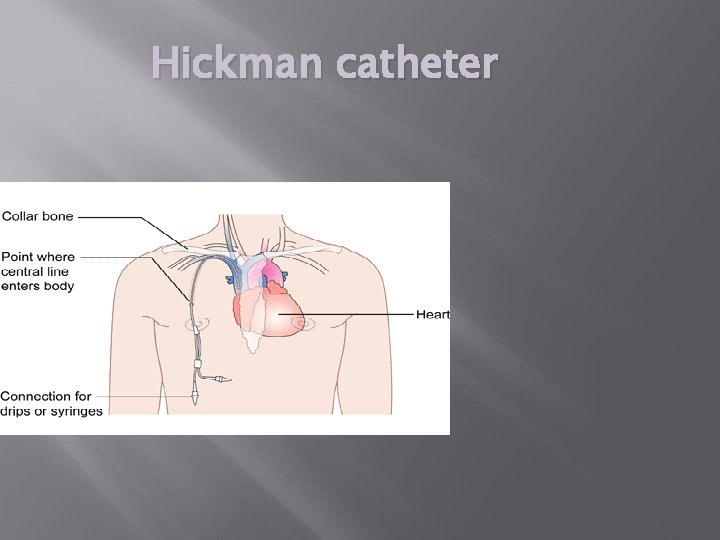
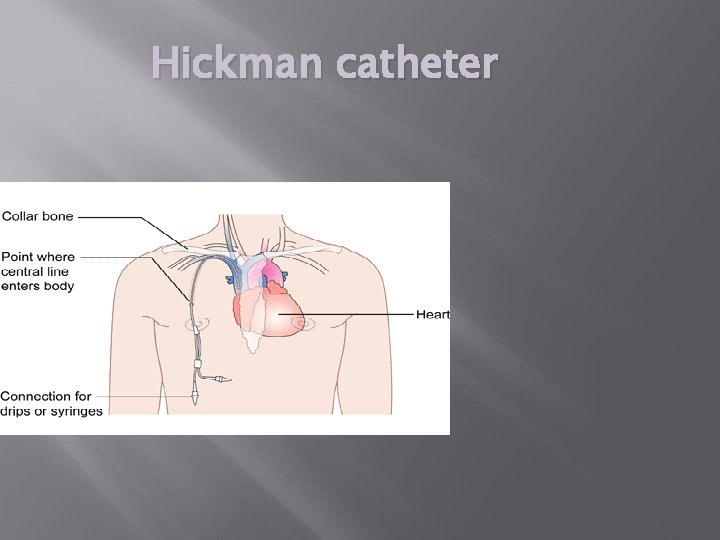
Hickman catheter
Hickman lines A tunnelled line made of soft silicone Single, double, triple lumen lines available Has cuff which is buried under the skin. This cuff acts as a barrier to infection, the line is sutured in place whilst tissue grows/forms around the cuff to secure it, reducing the risk of accidental displacement-(R. O. S exit site = 14 days) R. O. S at clavicle entry = 7 days Weekly Bio patch Change or When Soiled – ie Chlorhexidine Impregnated sponge which covers exit site
Using a Hickman catheter Follow the same principles for using a PICC Education of patients and relatives imperative Things to report - redness/swelling, pain, (line is longer PICC) Teaching the patient/relative to flush/dress lines Advice re showering Written information to consolidate all verbal information Documentation of care in medical notes and Nursing Care Plan
Routine care Always use an Aseptic Non Touch Technique Remove first 5 mls of blood - important when checking for asperate pre vesicant drugs or pre taking Bloods. Ensure a Flush after each use is used with 10 mls sterile Sodium Chloride 0. 9 % (or manufacturer’s recommended flush solution if not compatible) Needleless Access device – ie max plus connector Site care -assess daily for signs of infection & record assessment i. e exit length, dressing intact, Dressing changes- change weekly transparent dressing for visibility opsite 3000 , clean exit site with Alcoholic 2% chlorhexidine solution e. g. Chlora. Prep Solution 3 ml Discharge plan & Patient Education
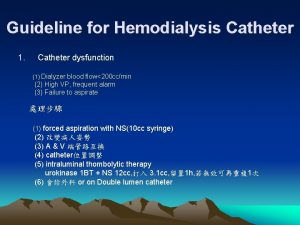
Problems which you could encounter Unable to with draw blood from line Unable to flush line Consider the following: Check clamp is off Check line not kinked Positional Clot in line fibrin sheath Line is not inside the vein Never apply force this can rupture/split line or dislodge a clot –Seek advice
Complications-CVAD Occlusion Phlebitis Infection Thrombosis Catheter embolus Venous damage Pneumothorax Cardiac arrhythmias Arterial puncture Nerve damage (particularly PICC’s) Cardiac tamponade
Blocked Hickman Line Administration of Syner-Kinase (Urokinase) Urokinase is a naturally occurring enzyme that converts plasminogen to plasmin, which is then able to degrade fibrin and cause the lysis of a clot. Syner-Kinase is used as a catheter “lock” Must be prescribed following Trust medicines policy Dissolve Urokinase 25, 000 U with 2 mls sterile saline Follow ALGORITHM FOR PARTIAL WITHDRAWAL OCCLUSION FOR A PICC – SOP You may need to refer patient to experienced practitioner. Install 1 ml =12, 500 U using a sterile technique lock in line for 1 -4 hours-label line DO NOT USE and inform patient that no one can use the line until urokinase is removed Document actions (Refer to SOP)
Who Removes the lines ? Hickman Lines Ideally should be removed by the practitioner who inserted the line but not always practical X-Ray department (planned procedure) Haematology Registrars/Consultants (e. g line needs to be removed due to infection) and have had training PICC- CNS who inserted/Nurse who has been trained
Document removal in medical notes including length of line removed Never attempt to push any line back in position seek advice
Questions? ? ? Contacts: Tanya Szczygielski Faculty Senior Educator ext 42043 Bleep: 3335 or Martina keane Clinical Nurse Educator Ext 415730
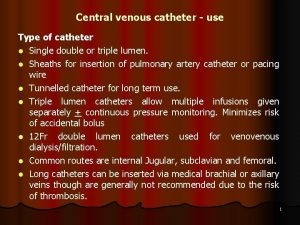
 Most common complication of central venous catheter
Most common complication of central venous catheter Most common complication of central venous catheter
Most common complication of central venous catheter Broviac vs hickman
Broviac vs hickman Central venous lines
Central venous lines Normal cvp
Normal cvp Cvp tracing
Cvp tracing 23110 cvc
23110 cvc Shirley cvc
Shirley cvc Tunneled cvc
Tunneled cvc Systur cvc com br
Systur cvc com br Cvc 22406
Cvc 22406 Cvc rule
Cvc rule Bundle of urinary catheter
Bundle of urinary catheter Phonology examples in english
Phonology examples in english Congestion hyperemia
Congestion hyperemia Universidade cvc
Universidade cvc Pinch off cvc
Pinch off cvc Scm 1
Scm 1 Finlandbased 108m
Finlandbased 108m Condom catheter
Condom catheter Pv loop catheter
Pv loop catheter A line nursing
A line nursing Yaunkauer
Yaunkauer Broviac catheter
Broviac catheter Cvvh kezelés
Cvvh kezelés Catheter
Catheter