CDI Module 6 Applying CDI to Home Management

- Slides: 39

CDI Module 6: Applying CDI to Home Management of Malaria ©Jhpiego Corporation The Johns Hopkins University A Training Program on Community. Directed Intervention (CDI) to Improve Access to Essential Health Services
Module 6 Objectives By the end of this module, learners will: § Outline three components of malaria case management § Describe the processes of case management with § Children § Pregnant women 2
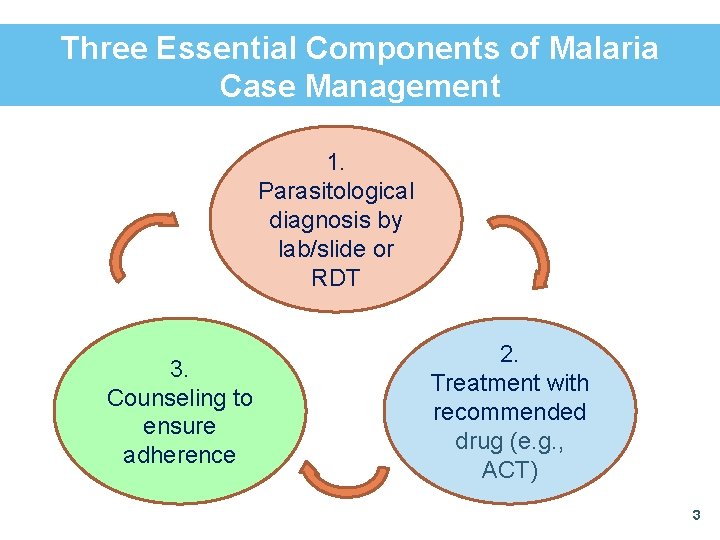
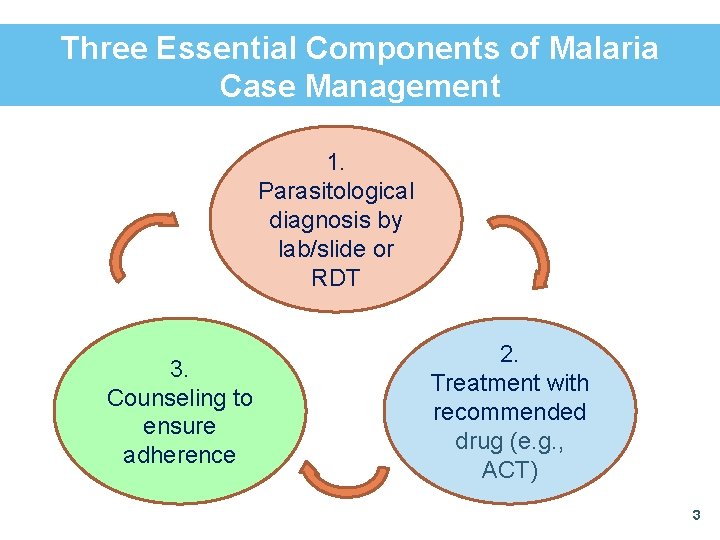
Three Essential Components of Malaria Case Management 1. Parasitological diagnosis by lab/slide or RDT 3. Counseling to ensure adherence 2. Treatment with recommended drug (e. g. , ACT) 3
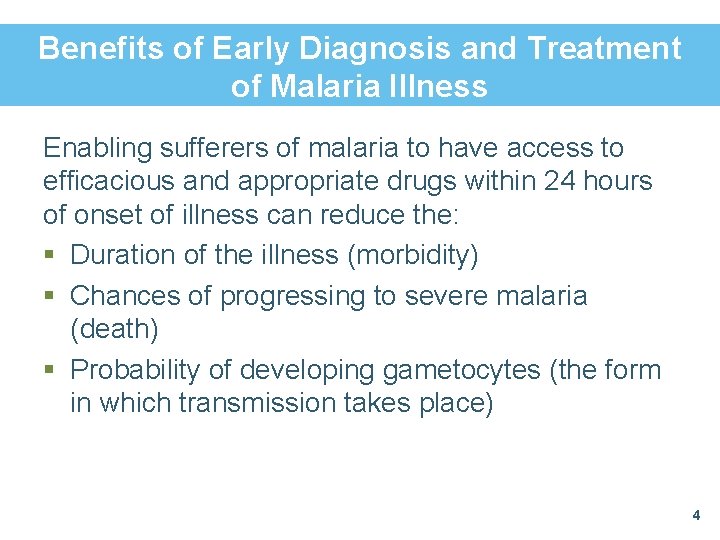
Benefits of Early Diagnosis and Treatment of Malaria Illness Enabling sufferers of malaria to have access to efficacious and appropriate drugs within 24 hours of onset of illness can reduce the: § Duration of the illness (morbidity) § Chances of progressing to severe malaria (death) § Probability of developing gametocytes (the form in which transmission takes place) 4
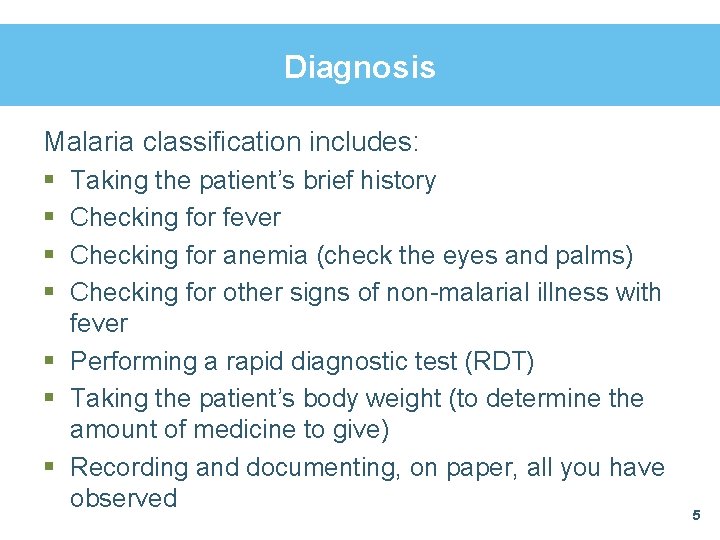
Diagnosis Malaria classification includes: § § Taking the patient’s brief history Checking for fever Checking for anemia (check the eyes and palms) Checking for other signs of non-malarial illness with fever § Performing a rapid diagnostic test (RDT) § Taking the patient’s body weight (to determine the amount of medicine to give) § Recording and documenting, on paper, all you have observed 5
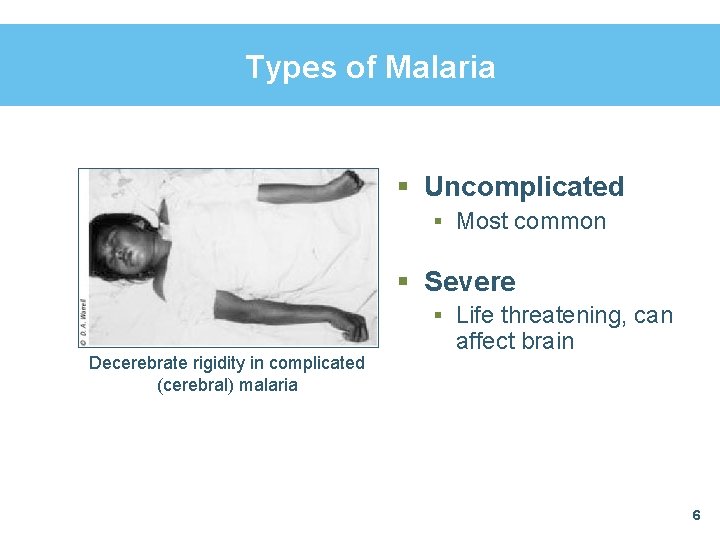
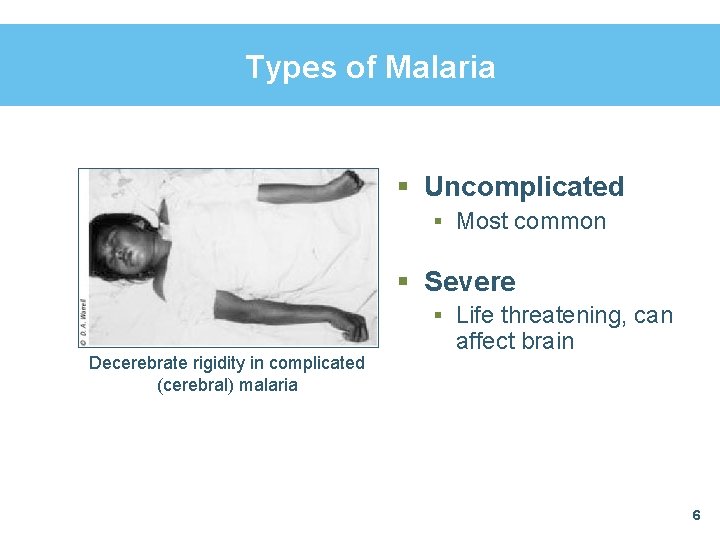
Types of Malaria § Uncomplicated § Most common § Severe § Life threatening, can Decerebrate rigidity in complicated (cerebral) malaria affect brain 6
Treating Malaria in Children 7
Recognizing Malaria How do you recognize malaria? § A child with malaria will have fever—fever simply means hotness of the body § You can recognize a child with fever: § By touching the chest/body with the back of your hand § If the child’s caregiver says the child had fever before coming, or § If the axillary (armpit) body temperature is 37. 5° C or higher 8
Other Symptoms § In addition to fever, other manifestations of malaria may include: § § § § Refusal to feed Generalized body weakness Not playing actively as usual/feeling unwell Excessive sweating Shivering and cold Vomiting Aches and body pains Bitterness in the mouth § NOTE: In the absence of an RDT or a lab test, a child who has fever—but none of the other symptoms—has malaria 9
Steps to Take When a Child Comes with Fever Step 1 § Assess fever § A patient has fever if he or she has: – History of fever – Feels hot or – Has axillary temperature of 37. 5° C and above § Then ask how long he or she has had fever 10
Recognizing Severe Malaria § Malaria can be serious—severe malaria can lead to disability or even death § A patient with severe malaria presents with general danger signs, in addition to fever 11
Danger Signs The following are the general danger signs: § Convulsions § Loss of consciousness/coma § Vomiting everything/severe vomiting § Child not able to drink or breastfeed § Very sick child (unable to sit or stand) § Difficulty in breathing or fast breathing 12
Steps to Take When a Child Comes with Fever (continued) Step 2 § Check for general danger signs § Ask: § Has the patient had convulsions? § Is the patient able to drink or eat—or breastfeed (if a child)? 13
What Can We Observe? Look to see if the patient: § § § § Is lethargic or unconscious Is convulsing now Has severe paleness/pallor (e. g. , very pale palms) Has difficulty in breathing (fast breathing) Is passing dark or little urine Has jaundice (yellowing of eyes) Has abnormal bleeding 14
How Can We Be Sure? Microscopy and RDTs § Unless we test for actual malaria parasites, we cannot be sure the person has malaria § We will address how to perform RDTs in a later module 15
Other Signs and Other Diseases § Look and feel for other signs that may indicate another disease that needs different treatment: § Stiff neck § Running nose § Signs of measles 16
Steps to Take When a Child Comes with Fever (continued) Step 3 § Classify fever § The two possible classifications for fever in a malarious area are: § Very severe febrile disease (febrile = with fever) § Malaria § Please give examples of other non-malarial febrile diseases 17
Classifying Malaria Look at the table in your job aid and classify the following case: § If a patient has a general danger sign, stiff neck, or symptoms or signs of severe malaria (passing dark or little urine, jaundice, severe dehydration or difficulty in breathing, abnormal bleeding), then the patient has: § Severe malaria—please refer immediately § If the patient has only fever without general danger signs, classify as: § Mild malaria—please treat 18
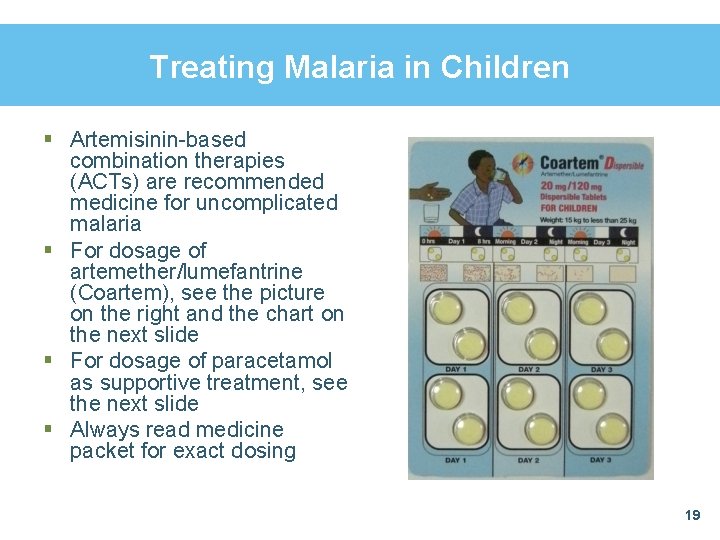
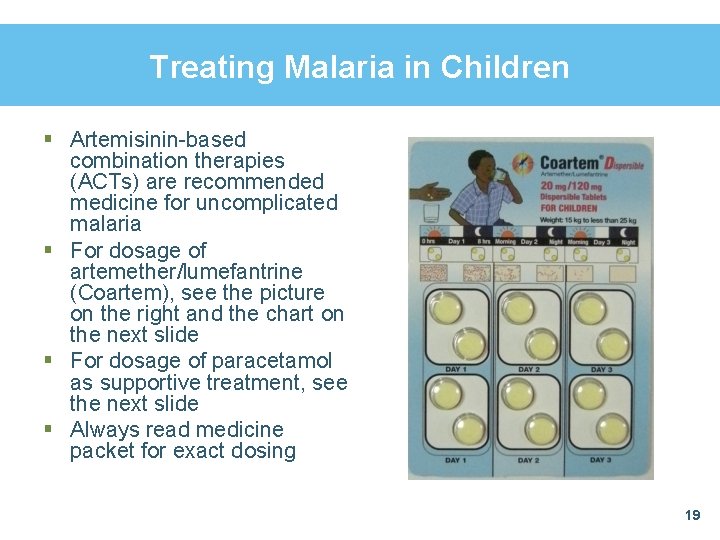
Treating Malaria in Children § Artemisinin-based combination therapies (ACTs) are recommended medicine for uncomplicated malaria § For dosage of artemether/lumefantrine (Coartem), see the picture on the right and the chart on the next slide § For dosage of paracetamol as supportive treatment, see the next slide § Always read medicine packet for exact dosing 19
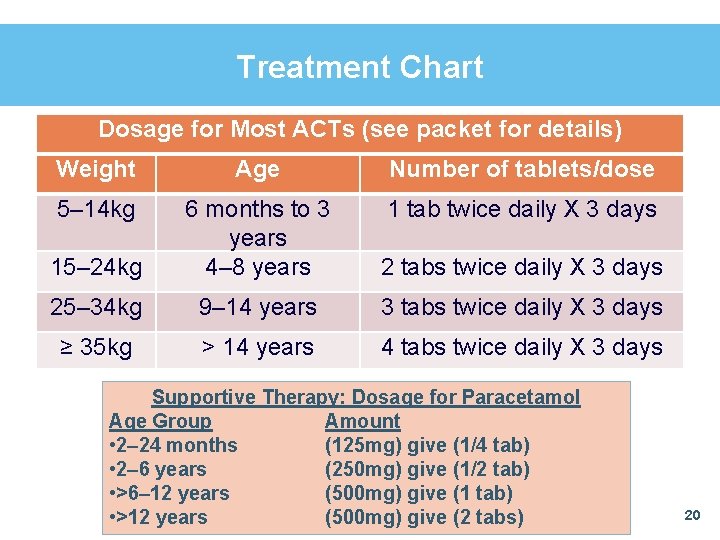
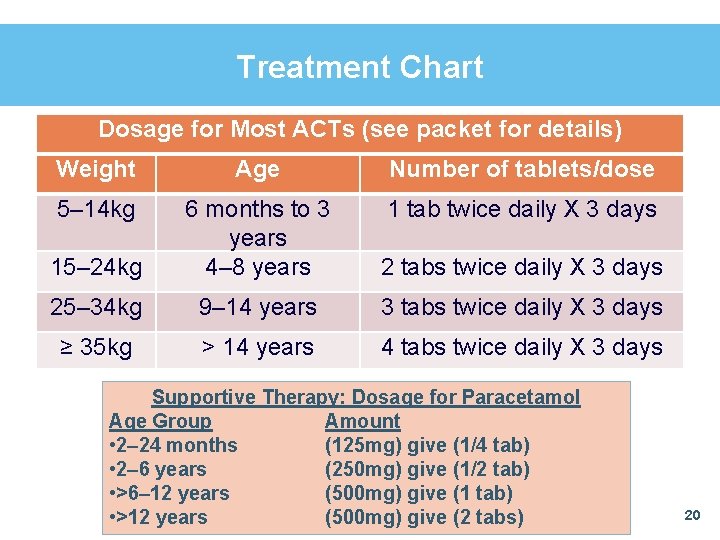
Treatment Chart Dosage for Most ACTs (see packet for details) Weight Age Number of tablets/dose 5– 14 kg 1 tab twice daily X 3 days 15– 24 kg 6 months to 3 years 4– 8 years 2 tabs twice daily X 3 days 25– 34 kg 9– 14 years 3 tabs twice daily X 3 days ≥ 35 kg > 14 years 4 tabs twice daily X 3 days Supportive Therapy: Dosage for Paracetamol Age Group Amount • 2‒ 24 months (125 mg) give (1/4 tab) • 2‒ 6 years (250 mg) give (1/2 tab) • >6‒ 12 years (500 mg) give (1 tab) • >12 years (500 mg) give (2 tabs) 20
Treating Malaria in Children— Dosing Caution Note: These drugs stay in the body for a long time So, to avoid overdosing: § A child—who had a complete course of appropriate ACT in the same month, and is now presenting again with fever, should be referred 21
TIPS on Counseling for Malaria Medicines § New Coartem will dissolve in water § If using artesunate-amodiaquine (AA) for children less than one year of age, you may need to crush the tablet § Mix banana or honey with the crushed medicine to sweeten it (discuss) § Make sure the child eats some food before taking medicine § Fatty foods help the body absorb medicine § If the child vomits within 30 minutes of swallowing the medicine, please repeat that vomited dose 22
More Tips If the child begins to react to the medicine, take him/her to the health facility immediately Reactions may include: § § Rashes and itching Difficulty breathing/cough Restlessness Other behavior or manifestation the caregiver considers unusual 23
How to Prevent Onset of Danger Signs at Home § Give the child correct treatment immediately when you notice illness and ensure that the child completes the full dose § Bring down fever immediately by: § Undressing the child and fanning him/her § Bathing the child with lukewarm or tepid water § Giving the appropriate dose of paracetamol § Giving the child enough fluid § If the child is not responding to treatment, take him/her to a health center immediately 24
Convulsions § What is convulsion? § When the whole or part of the child’s body begins to make repeated jerky movements § In small children, convulsion is usually caused by a sudden rise in body temperature § What to do? § See next slide 25
What to Do If Convulsion Occurs § Loosen all tight clothing, and leave only light clothing on the child § Disperse the crowd § Keep the child isolated § Lay the child flat on the floor § Remove any dangerous objects around the child § Take the child to a health center as soon as possible 26
Treatment Challenges— What If It Is Not Malaria? § When we involve the community in delivering integrated community case management (i. CCM), we are creating expectations that community-directed distributors (CDDs) and other volunteers will be able to address common illnesses § If our diagnosis using signs, symptoms and RDTs does not find that a fever is caused by malaria: § We have (it is hoped) included treatment of pneumonia in our i. CCM package § Fever could be caused by something other than malaria, and our CDDs will need to refer people when the cause of their fever is not clear 27
Treating Malaria in Pregnancy 28
Benefits of Treatment Treat malaria in pregnancy (MIP) quickly and correctly to prevent: § § § Anemia in pregnancy Miscarriage Fetal growth retardation Low birth weight Stillbirth Greater likelihood of death in the neonatal period 29
Recognizing Malaria in Pregnant Women Uncomplicated Malaria § Fever (hot body) § Shivering/chills/rigors § Weakness § Headaches § Muscle and/or joint pains § Nausea with or without vomiting § False labor pains § Mild anemia § Loss of appetite 30
Common Signs of Malaria Some common signs of malaria are: § Axillary temperature of 37. 5° C or higher § Anemia (pallor of the mucus membrane or palms) § Enlarged spleen and/or liver If any one or more of these symptoms and signs are found: § Malaria should be considered § Use RDT and follow the results 31
Malaria in Different Transmission Settings § In highly endemic, stable, year-round malaria transmission areas, a pregnant woman may not always exhibit the typical clinical signs due to some acquired immunity § RDTs are very helpful in this situation 32
Recognizing Severe Malaria § Pregnant women are more likely to get severe malaria than non-pregnant women § Signs of uncomplicated malaria plus one or more of the following indicate severe malaria: § § § § Dizziness Breathlessness/difficulty breathing Sleepiness/drowsiness Confusion Coma Sometimes fits, jaundice, severe dehydration Severe anemia Pulmonary edema § Again, always verify with an RDT 33
Treating Malaria: Uncomplicated or Severe § ACTs are the drug of choice for uncomplicated malaria § The most common ACTs are artemether-lumefantrine and artesunate-amodiaquine § ACTs are also recommended for the treatment of MIP in most countries, but guidelines vary § Quinine is also recommended for MIP and is usually the drug of choice for severe malaria § Facilitators will provide a handout for MIP treatment in your own country 34
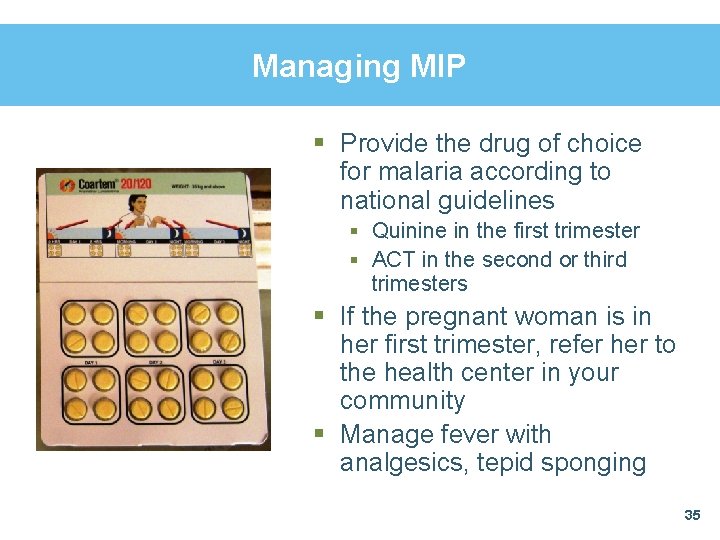
Managing MIP § Provide the drug of choice for malaria according to national guidelines § Quinine in the first trimester § ACT in the second or third trimesters § If the pregnant woman is in her first trimester, refer her to the health center in your community § Manage fever with analgesics, tepid sponging 35
Treating MIP § Observe the client taking the first dose of antimalarial drugs § Direct observation of treatment (DOT) strategy ensures that medicines are not wasted § Advise the client to: § Complete the course of drugs § Return if there is no improvement in 48 hours § Consume iron-rich food (e. g. , plantain, beans) § Use long-lasting insecticide-treated nets (LLINs)/insecticide-treated nets (ITNs) and other preventive measures 36
As Part of Treating MIP … § Arrange follow-up within 48 hours of DOT § Advise to return if condition worsens § Educate on danger signs § Reinforce use of LLINs/ITNs Most clients will respond to malaria treatment and begin to feel better within 48 hours; however: § If the woman’s condition does not improve—or worsens—within 48 hours of starting treatment, and/or other symptoms appear, refer immediately 37
Summary § Malaria case management has three essential components—diagnosis, treatment and counseling § We should differentiate malaria from other febrile illnesses and treat all illnesses correctly § Look for danger signs to prevent cerebral malaria (e. g. , convulsions) § Treat malaria in pregnant women to prevent stillbirth, miscarriage and low birth weight 38
In Conclusion § If the person who is ill does not have malaria, treat for appropriate illness or refer § We will address two other illnesses, pneumonia and diarrhea, in subsequent modules § Any comments or questions please? 39