Cardiovascular Epidemiology and Epidemiological Modelling KEY FACTS REGARDING

- Slides: 21

Cardiovascular Epidemiology and Epidemiological Modelling KEY FACTS REGARDING CVD TREATMENTS: USING THE EVIDENCE BASE IN MODELLING Martin O’Flaherty Simon Capewell Division of Public Health University of Liverpool
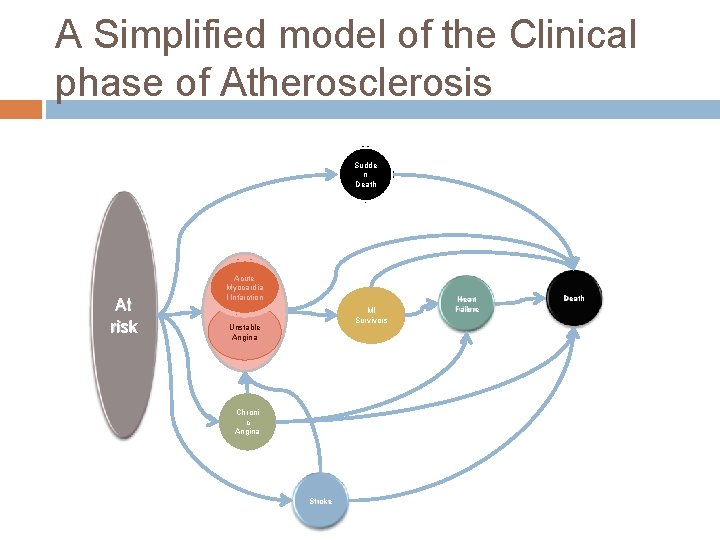
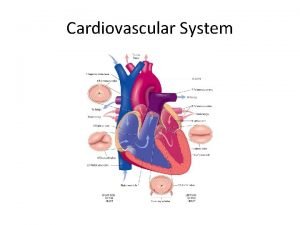
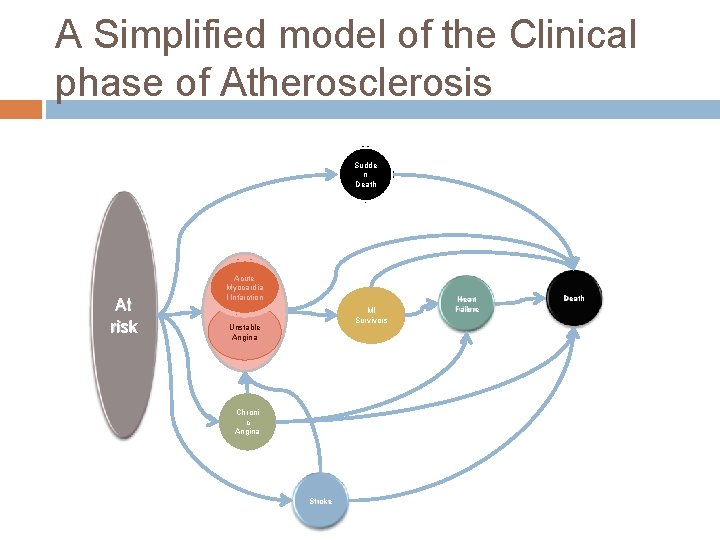
A Simplified model of the Clinical phase of Atherosclerosis Sudde n Death At risk Acute Myocardia l Infarction MI Survivors Unstable Angina Chroni c Angina Stroke Heart Failure Death
Key patients groups Acute Coronary Syndromes Stable Angina Heart Failure Stroke Peripheral Arterial disease
Strategies to Manage CVD Disease Aims: Prevent clinical disease Postpone disease progression Decrease mortality Increase Quality of Life
Acute Coronary Syndromes Complex situation: Definitions keep changing for clinical purposes. Epidemiological definitions: Circulation. 2003 Nov 18; 108(20): 2543 -9 Euro. CISS: http: //www. cuore. iss. it/eurociss Groups (Clinical) Acute Myocardial infarction STEMI (ST elevation Myocardial Infarction) NSTEMI (Non ST elevation Myocardial infarction Unstable angina
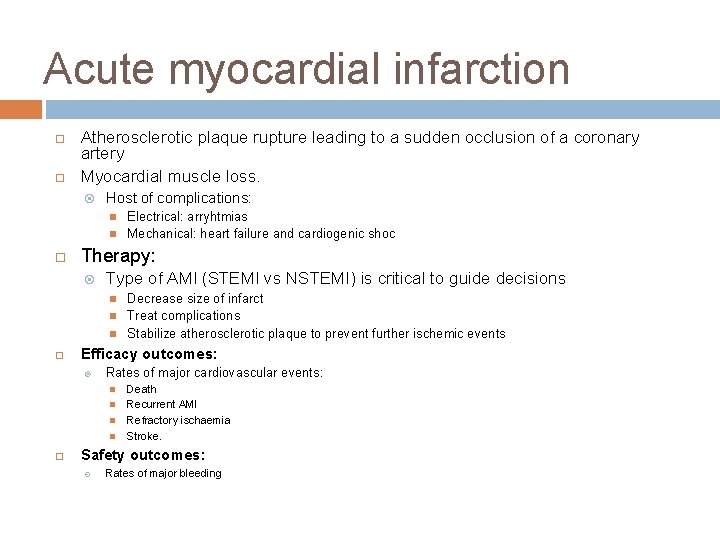
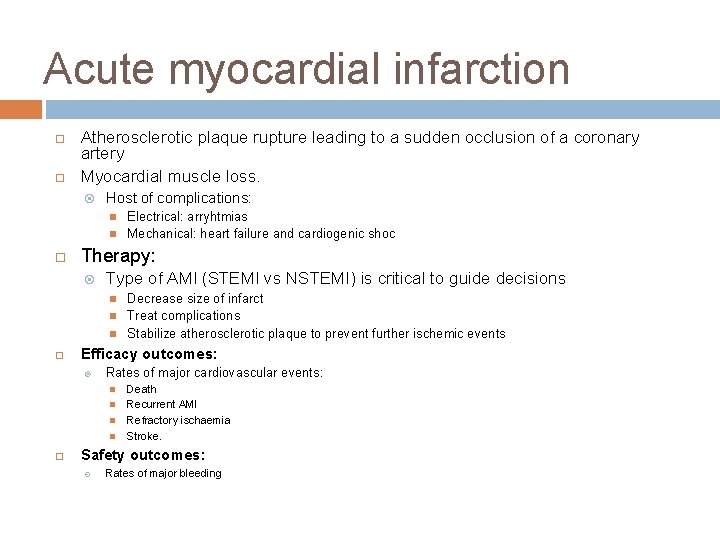
Acute myocardial infarction Atherosclerotic plaque rupture leading to a sudden occlusion of a coronary artery Myocardial muscle loss. Host of complications: Therapy: Type of AMI (STEMI vs NSTEMI) is critical to guide decisions Decrease size of infarct Treat complications Stabilize atherosclerotic plaque to prevent further ischemic events Efficacy outcomes: Rates of major cardiovascular events: Electrical: arryhtmias Mechanical: heart failure and cardiogenic shoc Death Recurrent AMI Refractory ischaemia Stroke. Safety outcomes: Rates of major bleeding
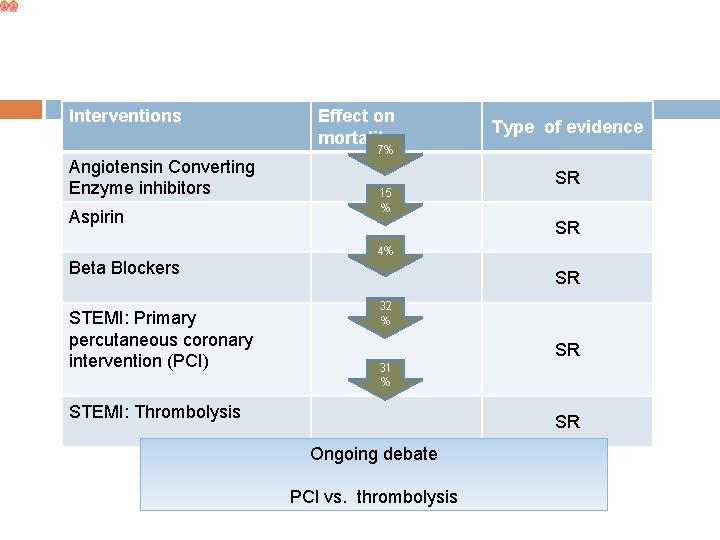
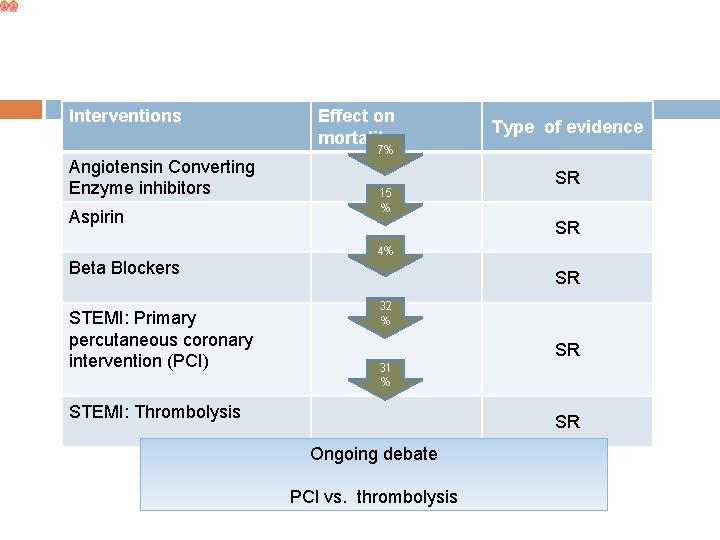
Interventions Angiotensin Converting Enzyme inhibitors Aspirin Beta Blockers STEMI: Primary percutaneous coronary intervention (PCI) Effect on mortality Type of evidence 7% 15 % SR SR 4% SR 32 % SR 31 % STEMI: Thrombolysis SR Ongoing debate PCI vs. thrombolysis
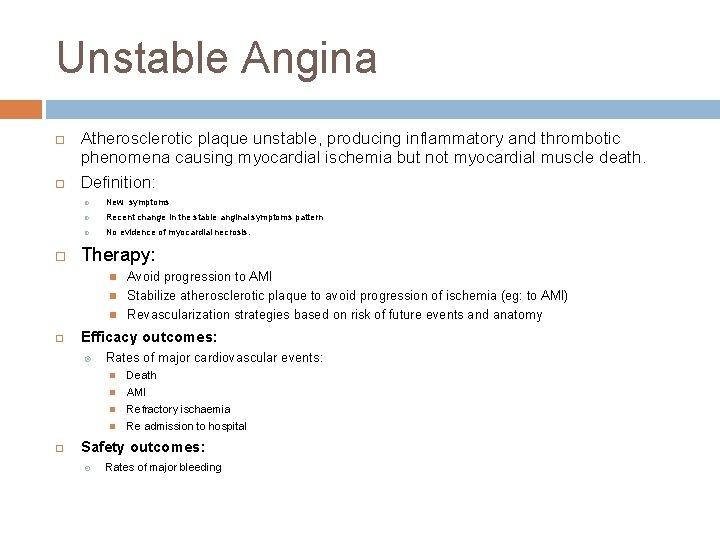
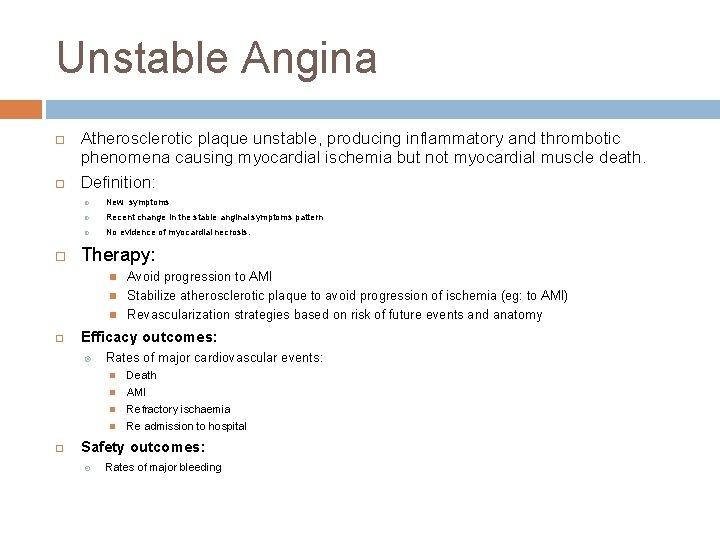
Unstable Angina Atherosclerotic plaque unstable, producing inflammatory and thrombotic phenomena causing myocardial ischemia but not myocardial muscle death. Definition: New symptoms Recent change in the stable anginal symptoms pattern No evidence of myocardial necrosis. Therapy: Efficacy outcomes: Avoid progression to AMI Stabilize atherosclerotic plaque to avoid progression of ischemia (eg: to AMI) Revascularization strategies based on risk of future events and anatomy Rates of major cardiovascular events: Death AMI Refractory ischaemia Re admission to hospital Safety outcomes: Rates of major bleeding
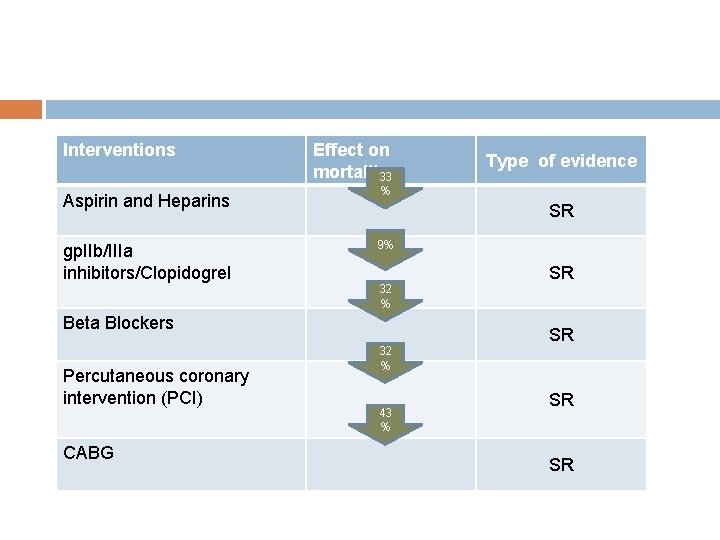
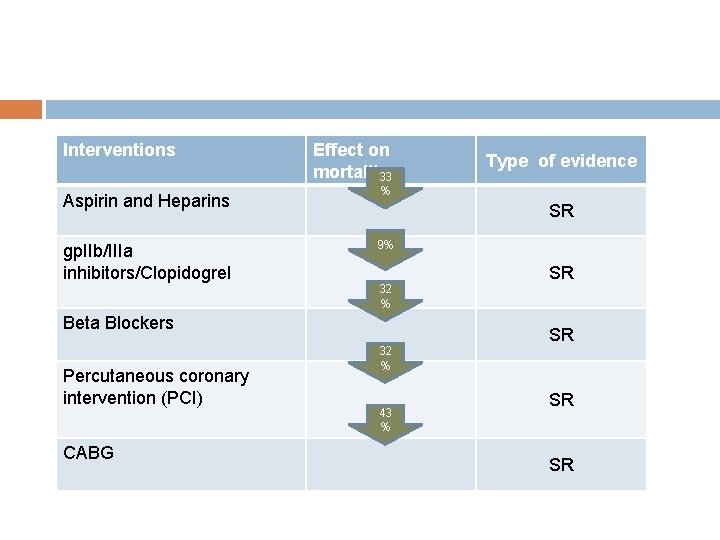
Interventions Effect on mortality 33 Aspirin and Heparins % gp. IIb/IIIa inhibitors/Clopidogrel 9% Type of evidence SR SR 32 % Beta Blockers Percutaneous coronary intervention (PCI) CABG 32 % 43 % SR SR SR
Chronic Angina Progressive occlusion by an atherosclerotic plaque, causing myocardial ischemia. Definition: Clinical definition based on anginal symptoms, pattern and duration Several validated questionnaires (Rose questionnaire) Therapy: Avoid ischemic events (secondary prevention) Symptom relief Efficacy outcomes: Rates of major cardiovascular events: Death AMI/UA Symptoms and Quality of Life Safety outcomes: Rates of major bleeding
Secondary Prevention in CVD patients Who: Every patient with Clinical CHD (Survivors of ACS, Chronic Angina, CHD related heart failure and) and Stroke Aspirin/Clopidogrel Anticoagulants ACEI/ARIIB Beta blockers (stroke: may not be indicated) Statins BP reduction Smoking cessation Rehabilitation
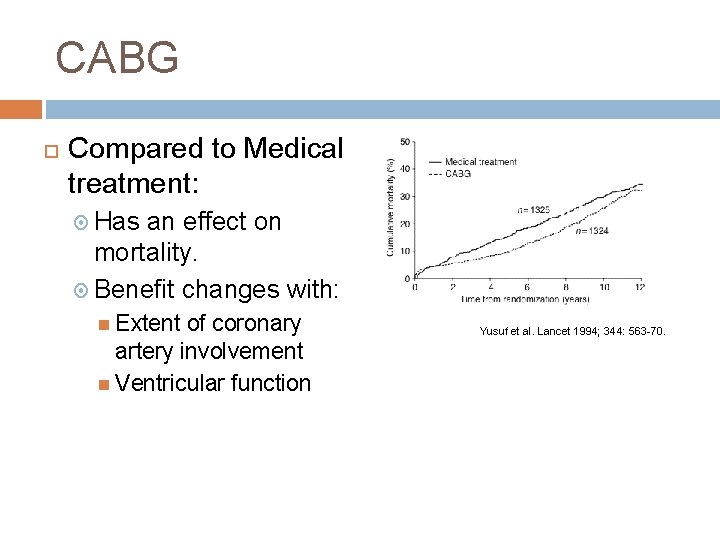
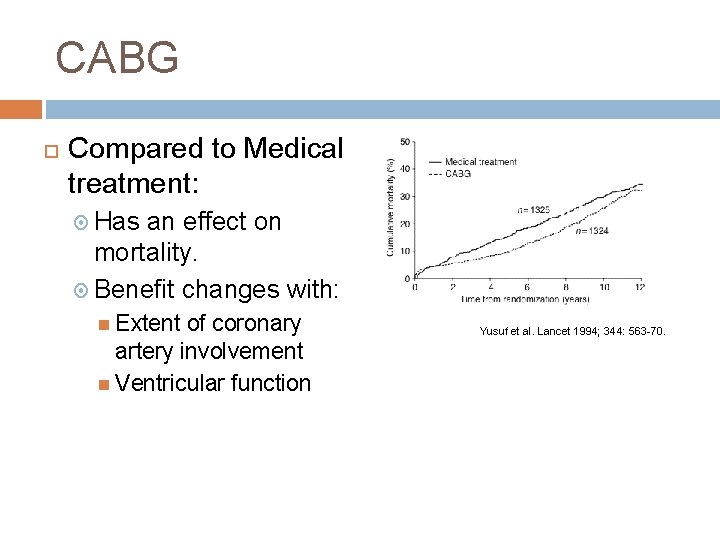
CABG Compared to Medical treatment: Has an effect on mortality. Benefit changes with: Extent of coronary artery involvement Ventricular function Yusuf et al. Lancet 1994; 344: 563 -70.
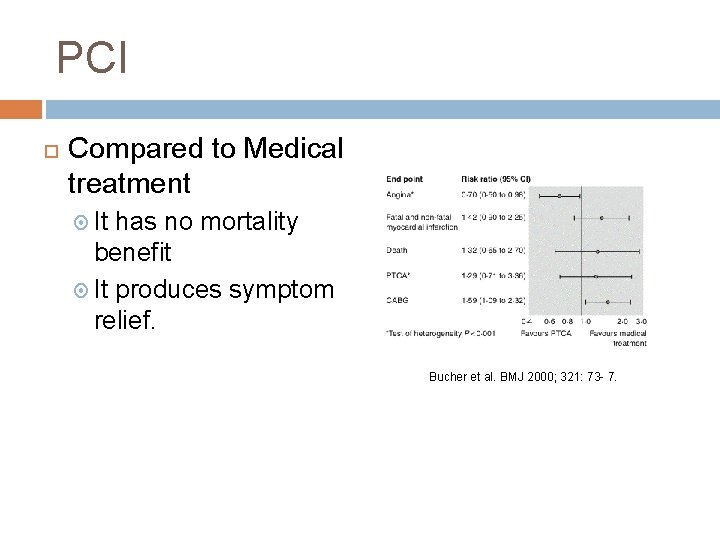
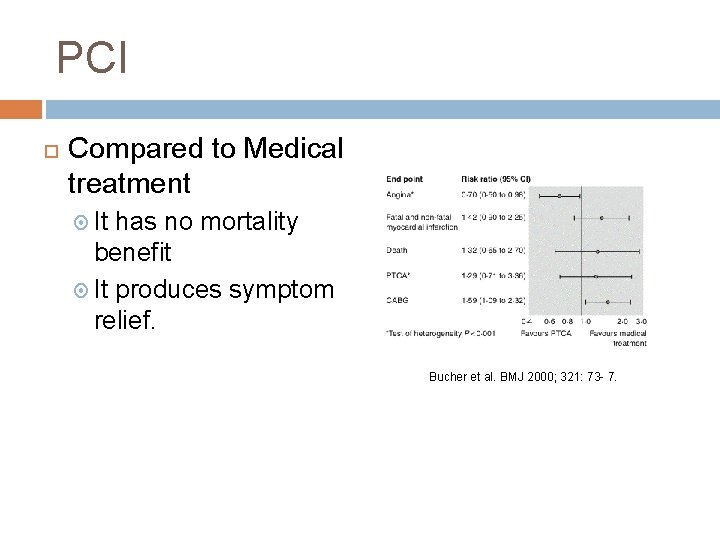
PCI Compared to Medical treatment It has no mortality benefit It produces symptom relief. Bucher et al. BMJ 2000; 321: 73 - 7.
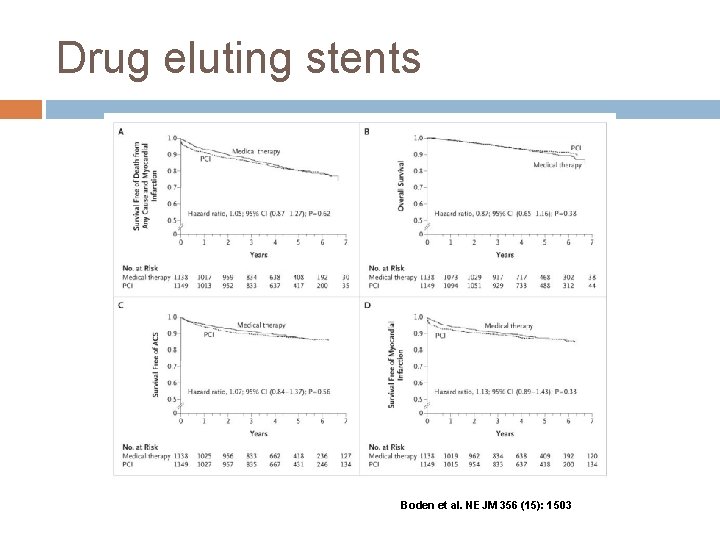
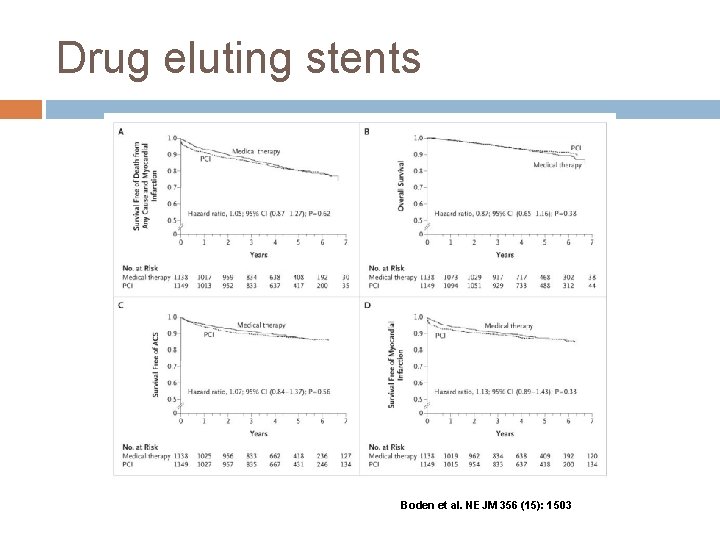
Drug eluting stents Boden et al. NEJM 356 (15): 1503
Heart Failure Progressive loss of the pump function of the heart Definition: Clinical syndrome + a measure of ventricular function. Some biomarkers are beeing increasingly used in clinical practice. Therapy: Decrease mortality from Progressive heart failure Sudden death Symptom relief Resource use control Efficacy outcomes: Rates of major cardiovascular events: Death Symptoms and Quality of Life Proxy measures of ventricular function
Available treatments for Heart Failure Rehab ACEI/ARII b Aspirin? Beta-blockers Implantable Cardio Defibrillators Spironolactone Anticoagulants ? Amiodarone? Statins?
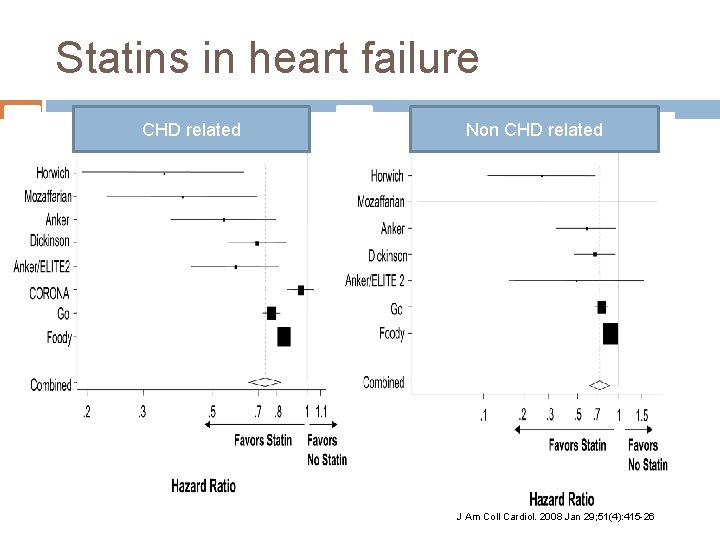
Statins in Heart Failure Current Debate: Physiopathological thinking suggests a role Role of statins in Post. MI and CA Observational evidence suggest an effect Clinical trials: CORONA : no effect GISSI: expecting results
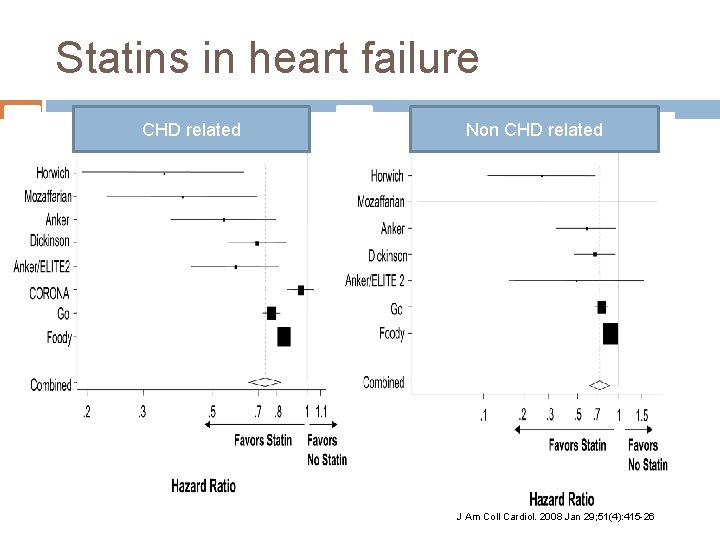
Statins in heart failure CHD related Non CHD related J Am Coll Cardiol. 2008 Jan 29; 51(4): 415 -26
Key issues when modelling interventions Mortality benefit or Quality of Life? Which patients are eligible? Current guidelines
Key issues when modelling interventions Efficacy vs effectiveness: RCT and SR usually better than real practice Uptake: those not receiving the drug do not benefit from it. Many interventions acting on the same individuals: Estimation of a common effect: The Mant-Hicks approach
Summary Patients groups Strategies High quality information on efficacy AMI Chronic Angina CABG vs PCI vs Medical Management Heart Failure PCI vs thrombolysis Statins Key facts in modelling interventions
 Epidemiological triad
Epidemiological triad Wheel causation model
Wheel causation model Stages of epidemiological transition
Stages of epidemiological transition Semashko model
Semashko model Epidemiologic transition
Epidemiologic transition Epidemiological triad
Epidemiological triad Theories of accident prevention
Theories of accident prevention What is epidemiological approach
What is epidemiological approach Epidemiological triad
Epidemiological triad What is epidemiological approach
What is epidemiological approach Diagnosis epidemiologi
Diagnosis epidemiologi Epidemiological transition model stage 2
Epidemiological transition model stage 2 Epidemiological transition model
Epidemiological transition model Neil mooser reaction positive in
Neil mooser reaction positive in Epidemiologic transition
Epidemiologic transition Epidemiological triad of typhoid fever
Epidemiological triad of typhoid fever Epidemiology triangle
Epidemiology triangle Descriptive vs analytic epidemiology examples
Descriptive vs analytic epidemiology examples Epidemiological transition
Epidemiological transition Difference between descriptive and analytical epidemiology
Difference between descriptive and analytical epidemiology Advantages and disadvantages of nutritional epidemiology
Advantages and disadvantages of nutritional epidemiology Difference between descriptive and analytical epidemiology
Difference between descriptive and analytical epidemiology