EXPERIMENTAL STUDIES Epidemiological Studies Epidemiological studies are either
- Slides: 34
EXPERIMENTAL STUDIES
Epidemiological Studies • Epidemiological studies are either observational or experimental. • Observational studies are considered “natural” experiments • Experimental studies are considered true experiments
Assigning Exposure 1. Defining feature – Investigator assigns exposure to study subjects A. B. C. D. E. most closely resemble controlled laboratory experiments serve as models for the conduct of observational studies gold standard of epidemiological research have high status and validity can pick up small and modest effects
2. Overall Conduct A. B. C. D. Hypothesis formed Study subjects recruited based on specific criteria Informed consent Eligible and willing subjects randomly allocated to receive treatment arm(s) E. Study groups monitored for outcome A. recurrence of disease B. first occurrence of disease C. getting better, side effects F. Outcome rates compared across groups
3. Ways to Categorize Experimental Studies • Individual versus community – treatment allocated to individual OR entire community – Do women with stage I breast cancer given a lumpectomy alone survive as long without recurrence of disease as women given a lumpectomy plus radiation? – Does fluoride in the water supply decrease the frequency of dental caries in a community compared to a similar community without such water treatment?
3. Ways to Categorize Experimental Studies • Preventive versus therapeutic – prophylactic agent given to healthy or high-risk individual to prevent disease OR treatment given to diseased individual to reduce risk of recurrence, improve survival – Does tamoxifen lower the incidence of breast cancer in women with high risk profile compared to high risk women not given tamoxifen? – Do combinations of two or three antiretroviral drugs prolong survival of AIDS patients as well as regimens of single drugs? – Ethics – which study is easier to get approval for?
4. Selection of Study Population A) Reference population - general group to whom results of a trial should be applicable (all humans, or some restrictions may apply) B) Study or experimental population – people who are considered for enrollment in a trial, potential participants Is this important – does it really matter who participates?
5. Issues to be Considered A. Size, size - not just number of people in the trial, but how many endpoints (outcome under study) are expected B. Restrictions on who is eligible (eligibility criteria) 1. Substantive: What group are you interested in? 2. Logistics: What group is accessible? Who will comply with study protocol? How feasible is complete and accurate follow-up on the subjects? 3. Characteristics of volunteers: How does study population differ from total experimental population?
6. Allocation of Treatment A) Should be random assignment 1. DEFINITION: Each individual has the same chance of receiving each possible “treatment” B) Some examples of random allocation 1. Random number table: as each subject enrolled, assigned a number from the random number table; assign even numbers to treatment A and odd to treatment B. C) Toss a coin for each subject: heads=A, tails=B 1. Some examples of nonrandom allocation 1. Alternate assignment of treatments 2. Assignment by day of the week 3. Why are these not random?
Goal of Randomization • To achieve baseline comparability between compared groups on factors related to outcome • Known factors • Unknown factors • Essence of good comparison between “treatments” is that the compared groups are the same EXCEPT for the “treatment. ”
Goal of Randomization • • The compared groups should have the same distribution of all of these characteristics. Equal distribution of known and unknown factors that are relevant to response to the treatment (confounders) Larger study – improves randomization works Do you ever have to worry about confounders?
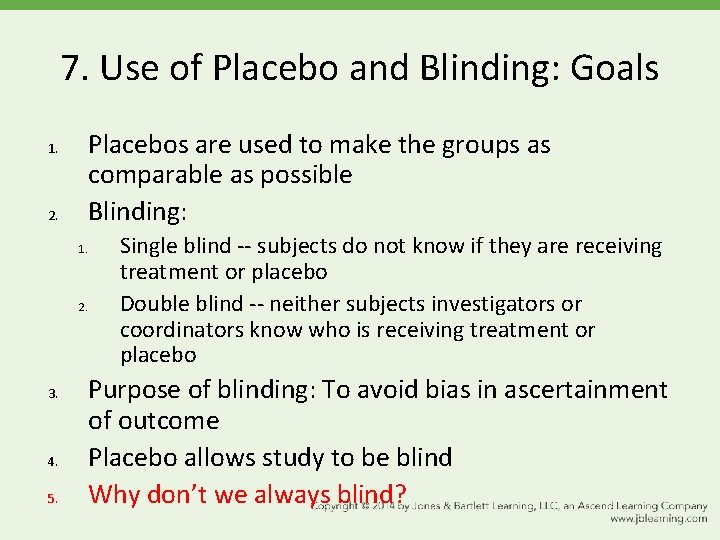
7. Use of Placebo and Blinding: Goals 1. 2. Placebos are used to make the groups as comparable as possible Blinding: 1. 2. 3. 4. 5. Single blind -- subjects do not know if they are receiving treatment or placebo Double blind -- neither subjects investigators or coordinators know who is receiving treatment or placebo Purpose of blinding: To avoid bias in ascertainment of outcome Placebo allows study to be blind Why don’t we always blind?
Maintenance/assessment of compliance A) Study requires active participation and cooperation of participants but deviations from the protocol will occur related to side effects, illness, level of interest, and length of follow-up B) Noncompliance makes the compared groups more alike – Why is this a problem? – Should you move a non-compliant person to the control arm? – Should you move someone who starts the intervention on their own in the control arm to the treatment arm? • Does this happen often?
Maintenance/assessment of compliance • Design phase strategy – Pick an interested group and design a simple protocol. – Problem with this? • Throughout study – frequent contact with subjects – incentives to continue • such as free check-ups • compensation for their time
9. Ascertaining the Outcome A) Goals 1. High follow-up rates: don’t lose people 1. Why? Uniform follow-up for compared groups: must be equally vigilant in follow-up in all compared groups 2. 1. Why?
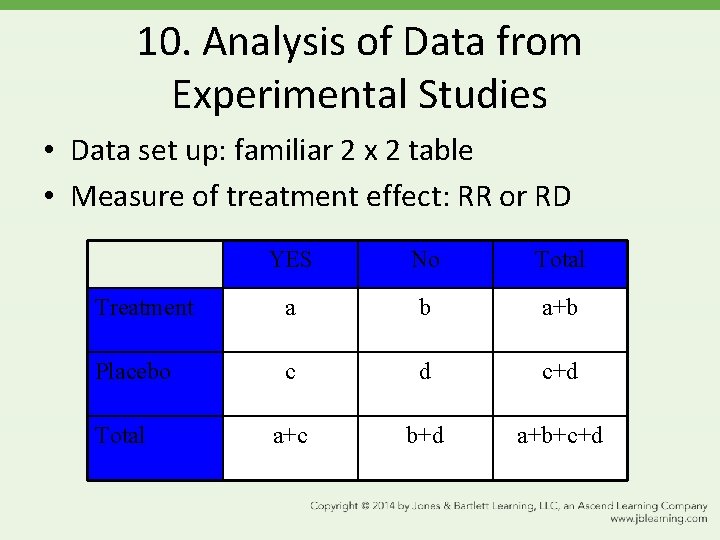
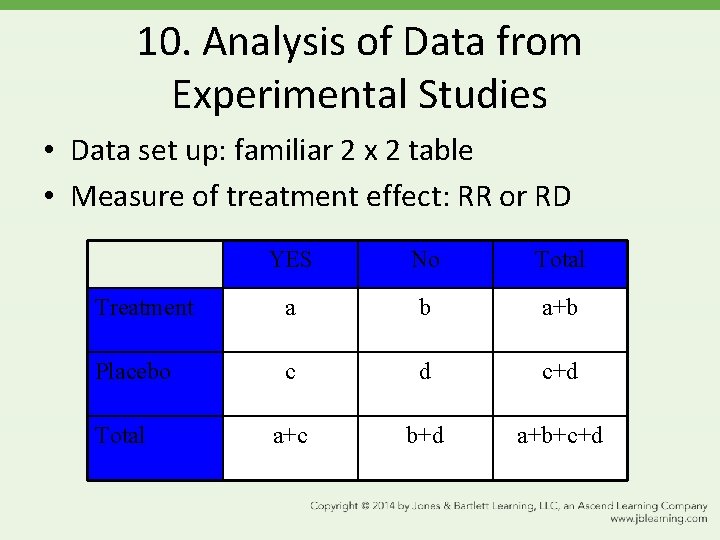
10. Analysis of Data from Experimental Studies • Data set up: familiar 2 x 2 table • Measure of treatment effect: RR or RD YES No Total Treatment a b a+b Placebo c d c+d a+c b+d a+b+c+d Total
11. Important Issues in Experimental Studies: Ethical Considerations • Equipoise • Must be genuine doubt about efficacy of treatment yet sufficient belief that it may work • Stopping rules • What if it becomes apparent, before the trial is over, that the new treatment is beneficial (and should not be withheld from the placebo group) or is toxic (and treatment should be withdrawn)?
11. Important Issues in Experimental Studies: Planning for an informative result • If the study finds no difference between compared treatments, do you believe it? • Or was there a difference but the study was not powerful enough to detect it? • Type II Error – failed to find a true difference • Initial consideration is study size.
11. Important Issues in Experimental Studies: Analyzing by intention to treat • As the saying goes… once randomized, always analyzed. • Why?
PRACTICE FOR THE EXAM
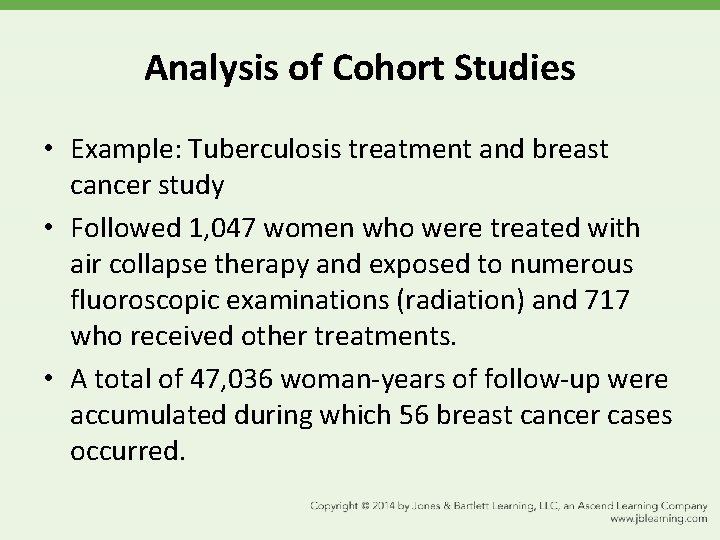
Analysis of Cohort Studies • Example: Tuberculosis treatment and breast cancer study • Followed 1, 047 women who were treated with air collapse therapy and exposed to numerous fluoroscopic examinations (radiation) and 717 who received other treatments. • A total of 47, 036 woman-years of follow-up were accumulated during which 56 breast cancer cases occurred.
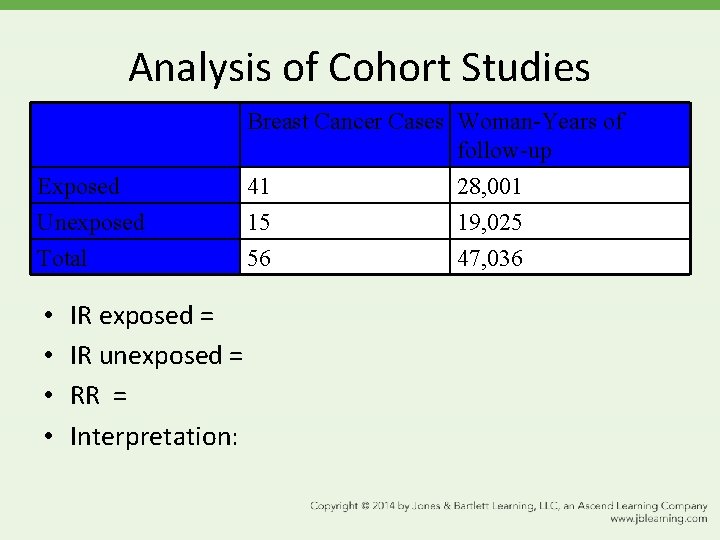
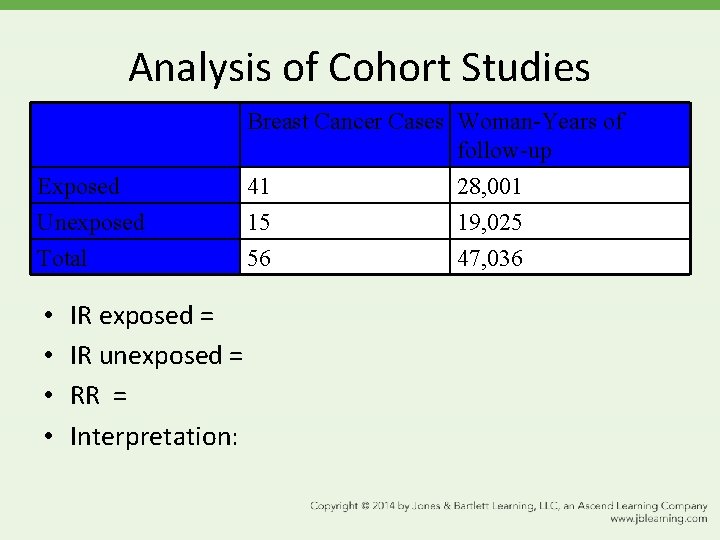
Analysis of Cohort Studies Exposed Unexposed Total • • IR exposed = IR unexposed = RR = Interpretation: Breast Cancer Cases Woman-Years of follow-up 41 28, 001 15 19, 025 56 47, 036
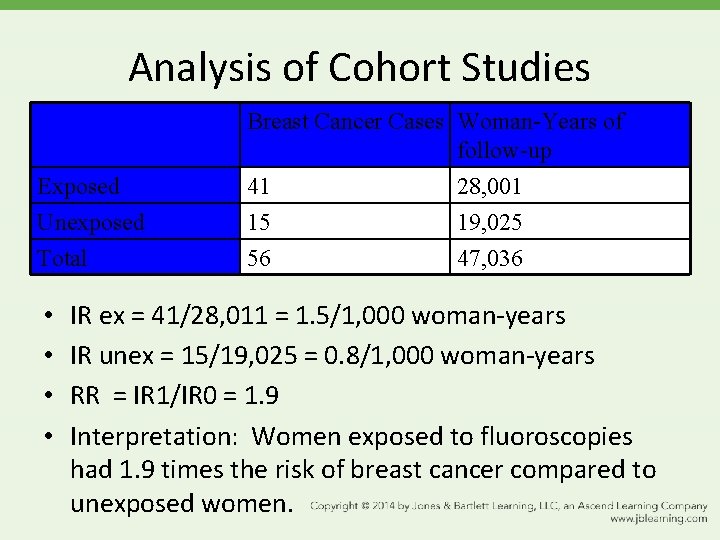
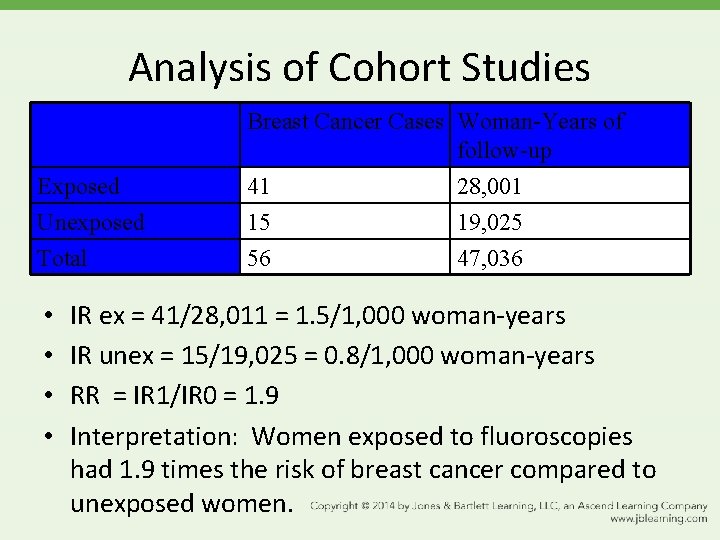
Analysis of Cohort Studies Exposed Unexposed Total • • Breast Cancer Cases Woman-Years of follow-up 41 28, 001 15 19, 025 56 47, 036 IR ex = 41/28, 011 = 1. 5/1, 000 woman-years IR unex = 15/19, 025 = 0. 8/1, 000 woman-years RR = IR 1/IR 0 = 1. 9 Interpretation: Women exposed to fluoroscopies had 1. 9 times the risk of breast cancer compared to unexposed women.
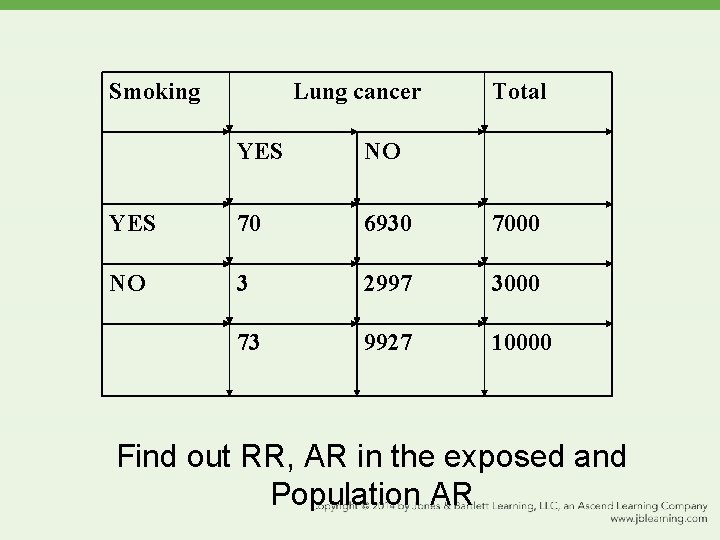
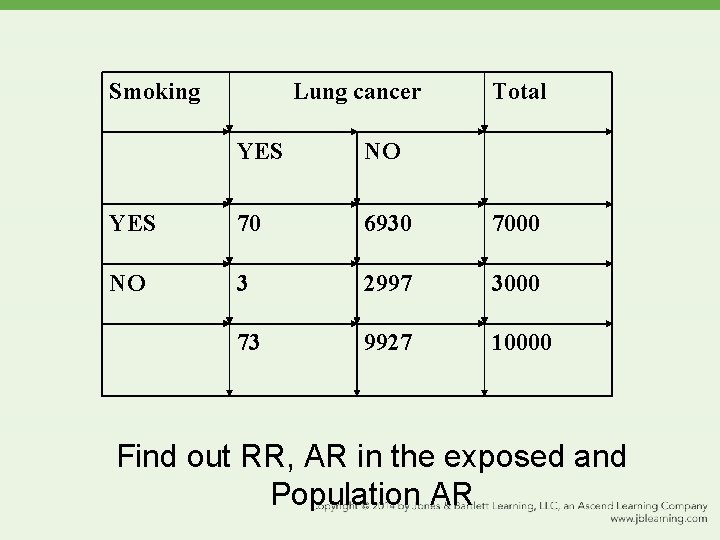
Smoking Lung cancer Total YES NO YES 70 6930 7000 NO 3 2997 3000 73 9927 10000 Find out RR, AR in the exposed and Population AR
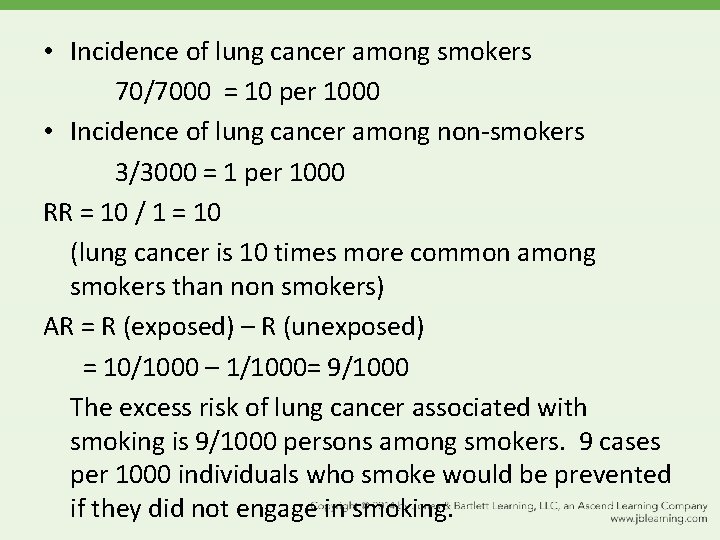
• Incidence of lung cancer among smokers 70/7000 = 10 per 1000 • Incidence of lung cancer among non-smokers 3/3000 = 1 per 1000 RR = 10 / 1 = 10 (lung cancer is 10 times more common among smokers than non smokers) AR = R (exposed) – R (unexposed) = 10/1000 – 1/1000= 9/1000 The excess risk of lung cancer associated with smoking is 9/1000 persons among smokers. 9 cases per 1000 individuals who smoke would be prevented if they did not engage in smoking.
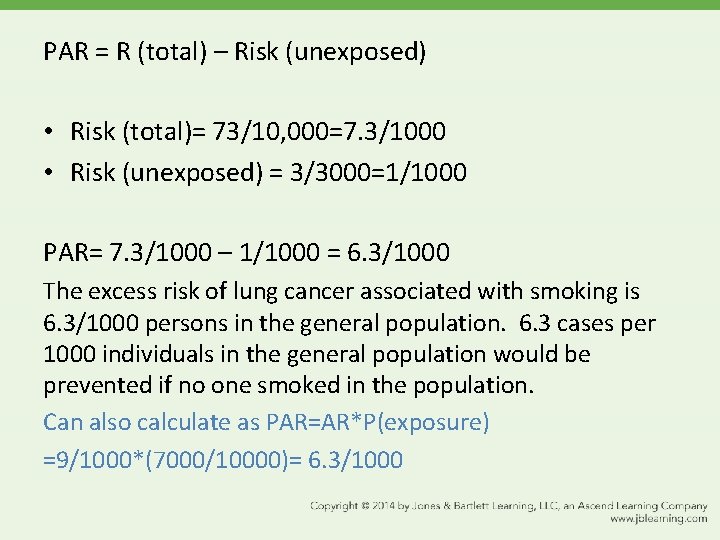
PAR = R (total) – Risk (unexposed) • Risk (total)= 73/10, 000=7. 3/1000 • Risk (unexposed) = 3/3000=1/1000 PAR= 7. 3/1000 – 1/1000 = 6. 3/1000 The excess risk of lung cancer associated with smoking is 6. 3/1000 persons in the general population. 6. 3 cases per 1000 individuals in the general population would be prevented if no one smoked in the population. Can also calculate as PAR=AR*P(exposure) =9/1000*(7000/10000)= 6. 3/1000
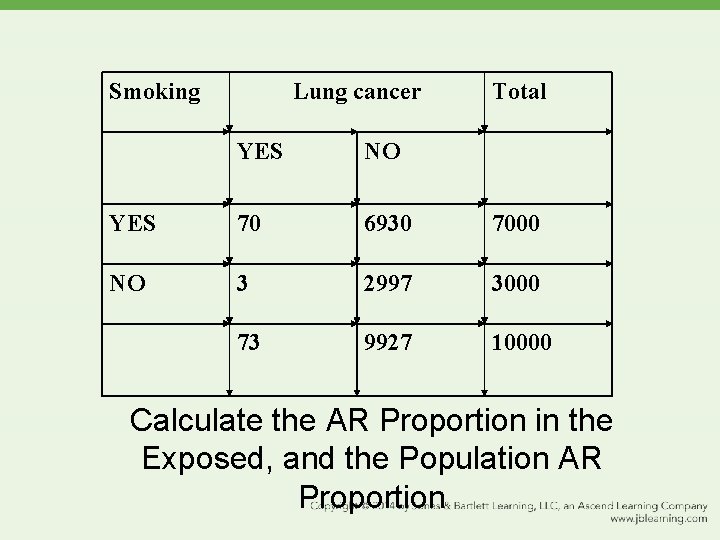
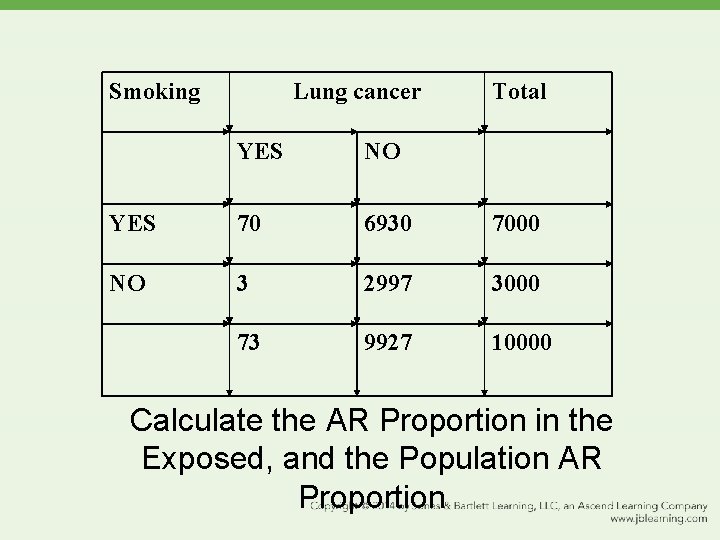
Smoking Lung cancer Total YES NO YES 70 6930 7000 NO 3 2997 3000 73 9927 10000 Calculate the AR Proportion in the Exposed, and the Population AR Proportion
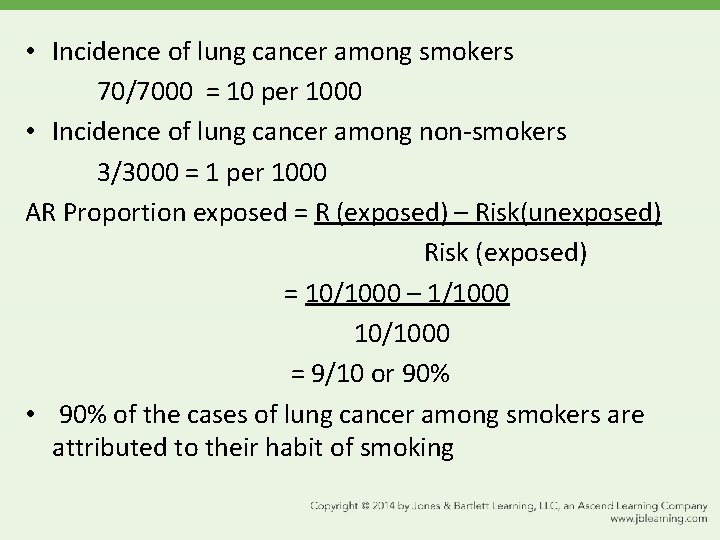
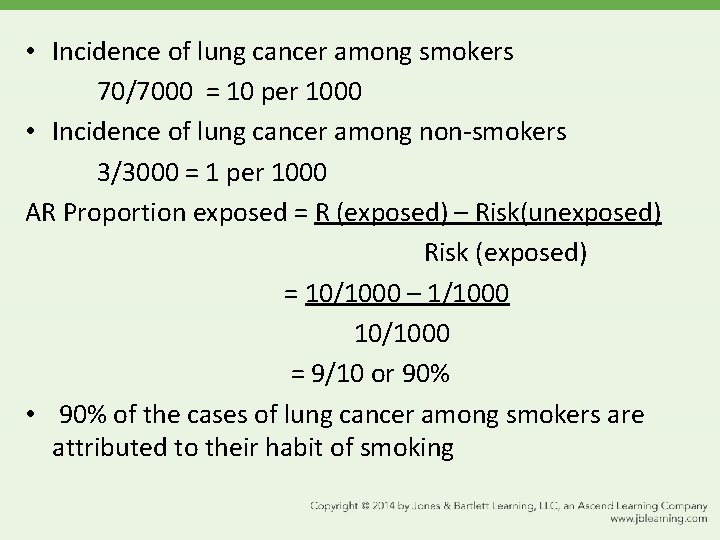
• Incidence of lung cancer among smokers 70/7000 = 10 per 1000 • Incidence of lung cancer among non-smokers 3/3000 = 1 per 1000 AR Proportion exposed = R (exposed) – Risk(unexposed) Risk (exposed) = 10/1000 – 1/1000 10/1000 = 9/10 or 90% • 90% of the cases of lung cancer among smokers are attributed to their habit of smoking
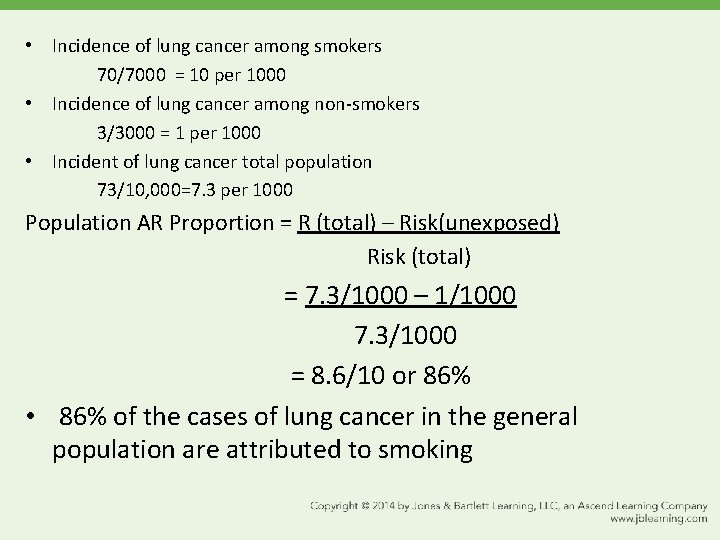
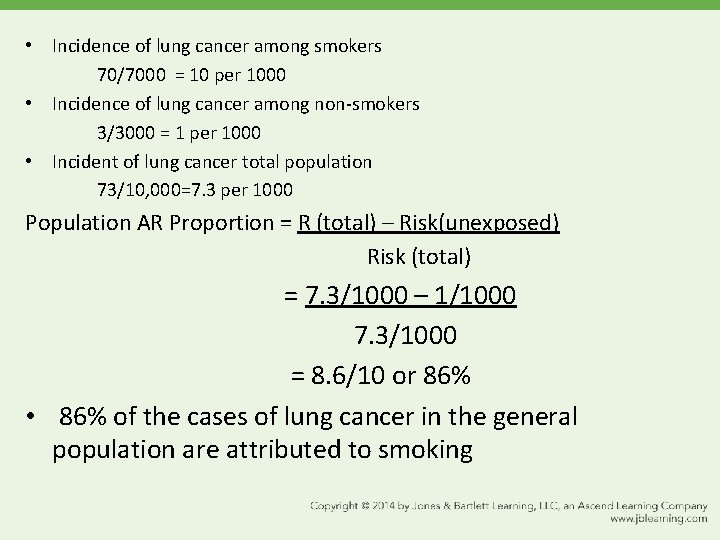
• Incidence of lung cancer among smokers 70/7000 = 10 per 1000 • Incidence of lung cancer among non-smokers 3/3000 = 1 per 1000 • Incident of lung cancer total population 73/10, 000=7. 3 per 1000 Population AR Proportion = R (total) – Risk(unexposed) Risk (total) = 7. 3/1000 – 1/1000 7. 3/1000 = 8. 6/10 or 86% • 86% of the cases of lung cancer in the general population are attributed to smoking
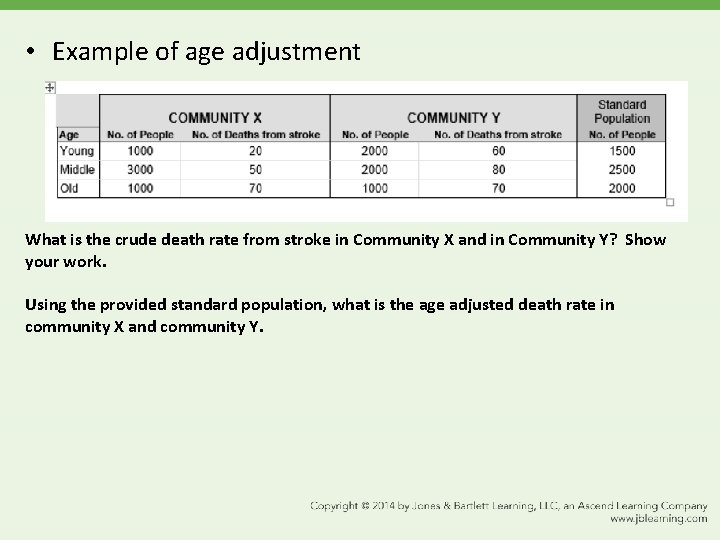
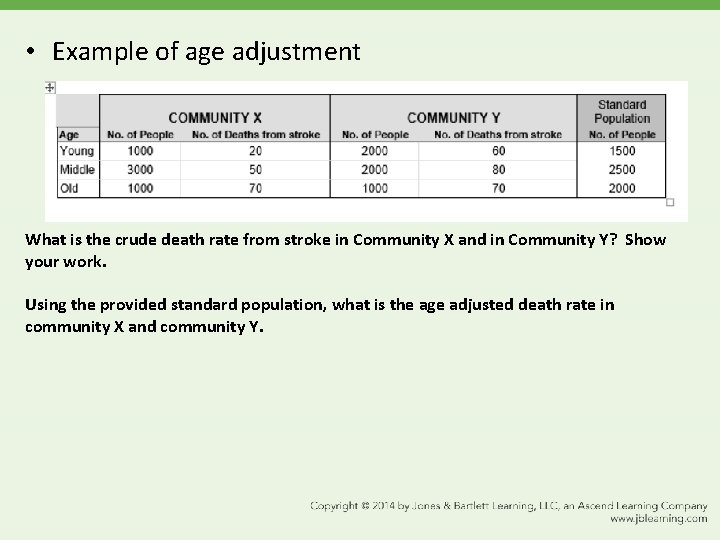
• Example of age adjustment What is the crude death rate from stroke in Community X and in Community Y? Show your work. Using the provided standard population, what is the age adjusted death rate in community X and community Y.
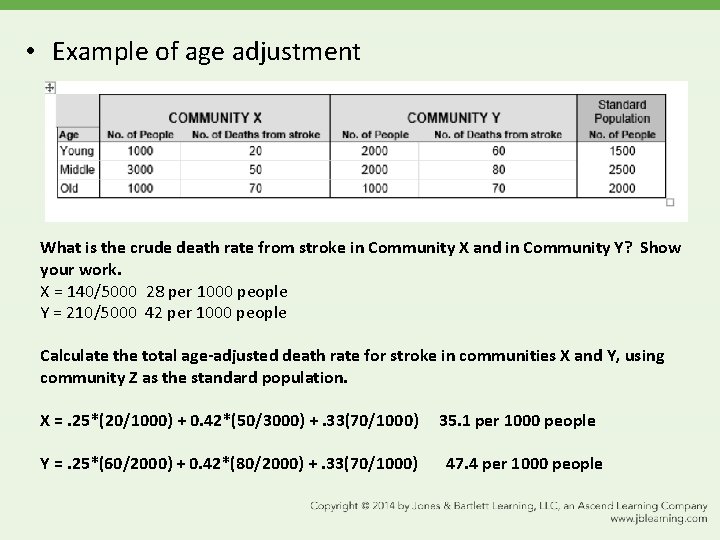
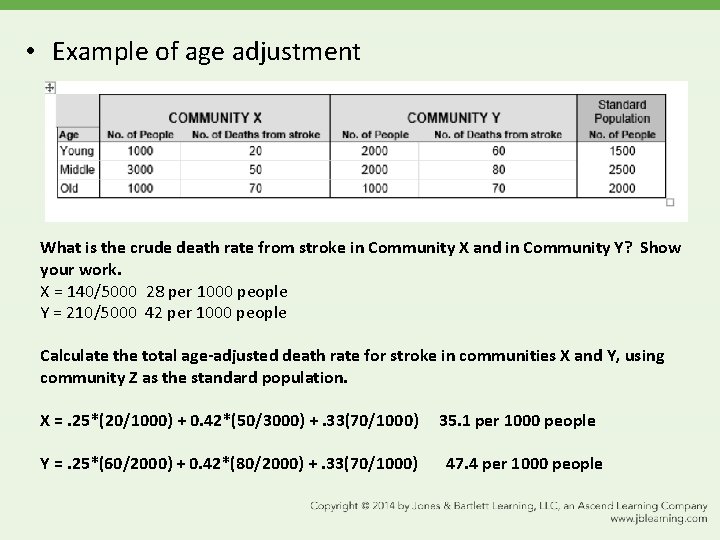
• Example of age adjustment What is the crude death rate from stroke in Community X and in Community Y? Show your work. X = 140/5000 28 per 1000 people Y = 210/5000 42 per 1000 people Calculate the total age-adjusted death rate for stroke in communities X and Y, using community Z as the standard population. X =. 25*(20/1000) + 0. 42*(50/3000) +. 33(70/1000) Y =. 25*(60/2000) + 0. 42*(80/2000) +. 33(70/1000) 35. 1 per 1000 people 47. 4 per 1000 people
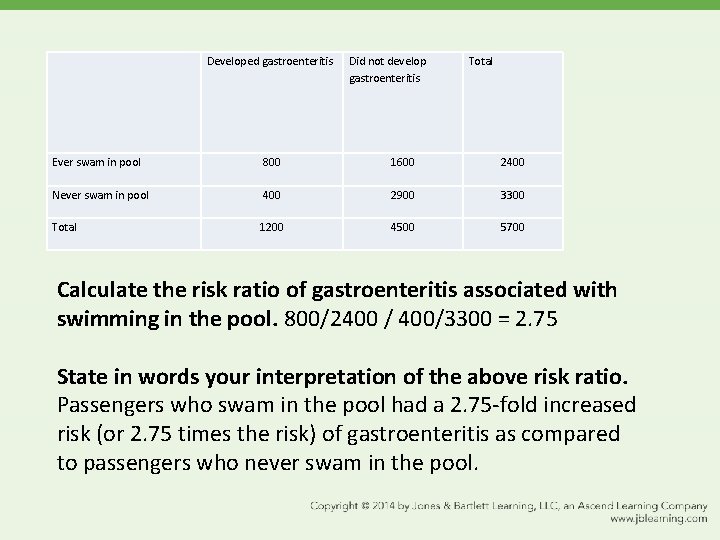
• Recently, there have been a number of norovirus outbreaks on cruise ships. The cruise ship owners contacted the CDC to conduct an in-depth analysis of the possible modes of transmission of norovirus in the cruise ship environment. CDC investigators interviewed all of the passengers on the last affected cruise (N=5700) and obtained information on the passenger’s recreational activities. They found the following results: 1, 200 passengers developed gastroenteritis during the cruise. 3300 passengers never swam in the pool during the cruise. 800 passengers swam in the pool and developed gastroenteritis during the cruise. FYI: The cruise lasted one week. Set up a two by two table and calculate the risk ratio.
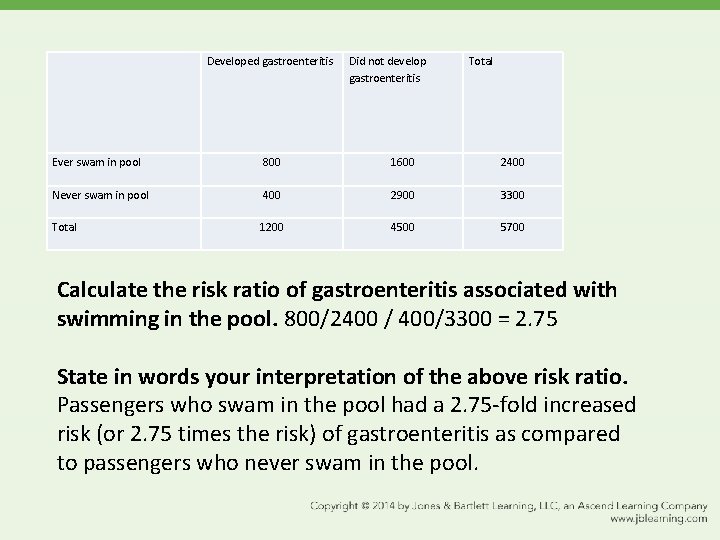
Developed gastroenteritis Did not develop gastroenteritis Total Ever swam in pool 800 1600 2400 Never swam in pool 400 2900 3300 Total 1200 4500 5700 Calculate the risk ratio of gastroenteritis associated with swimming in the pool. 800/2400 / 400/3300 = 2. 75 State in words your interpretation of the above risk ratio. Passengers who swam in the pool had a 2. 75 -fold increased risk (or 2. 75 times the risk) of gastroenteritis as compared to passengers who never swam in the pool.