Anticoagulacin en la Cirrosis e HTP no cirrtica
- Slides: 48
Anticoagulación en la Cirrosis e HTP no cirrótica Juan Carlos Garcia-Pagán Barcelona Hepatic Hemodynamic Laboratory. Liver Unit. IMDIM. Hospital Clinic. IDIBAPS. Ciberehd. Barcelona IV Curso para Residentes: “Diagnóstico y Tratamiento de las Enfermedades Hepáticas” Barcelona, 18 -19 Octubre 2013
• Coagulación y Cirrosis: Fundamentos del Tratamiento • Hay que anticoagular a los cirróticos: ¿Cuándo? ¿hay suficiente evidencia? • Trombosis portal aguda no cirrótica: anticoagulación y tratamientos locales intervencionistas
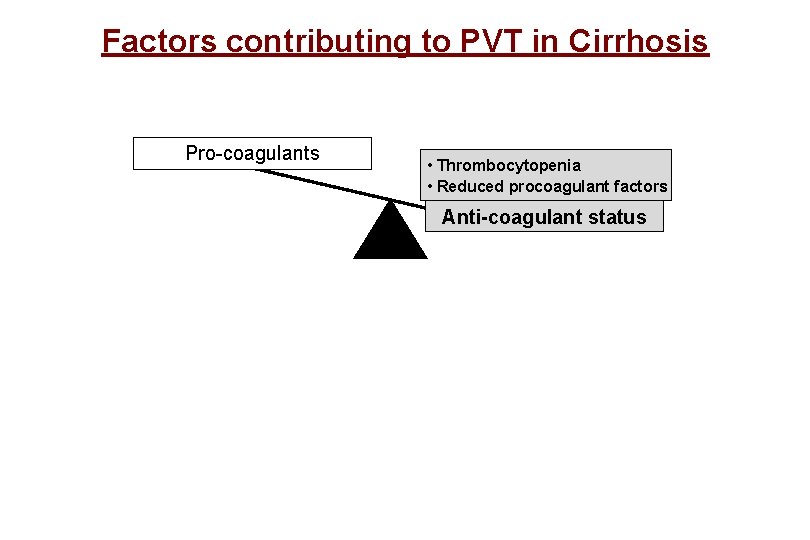
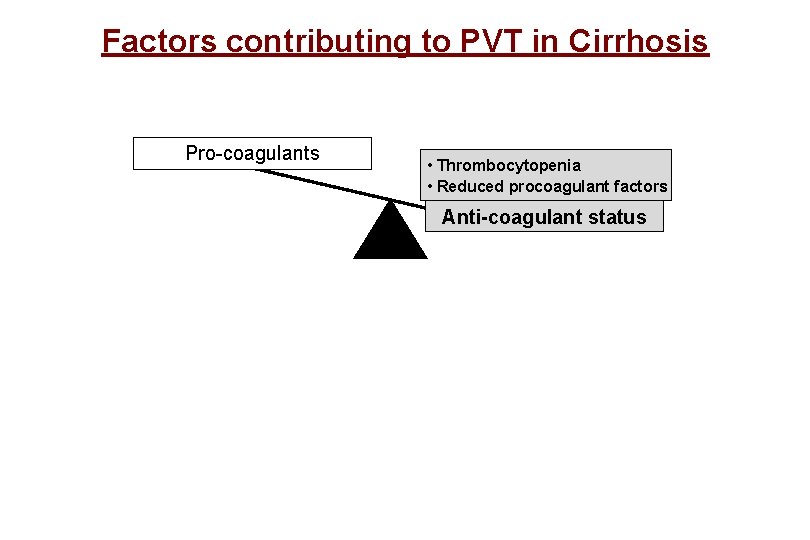
Factors contributing to PVT in Cirrhosis Pro-coagulants • Thrombocytopenia • Reduced procoagulant factors Anti-coagulant status
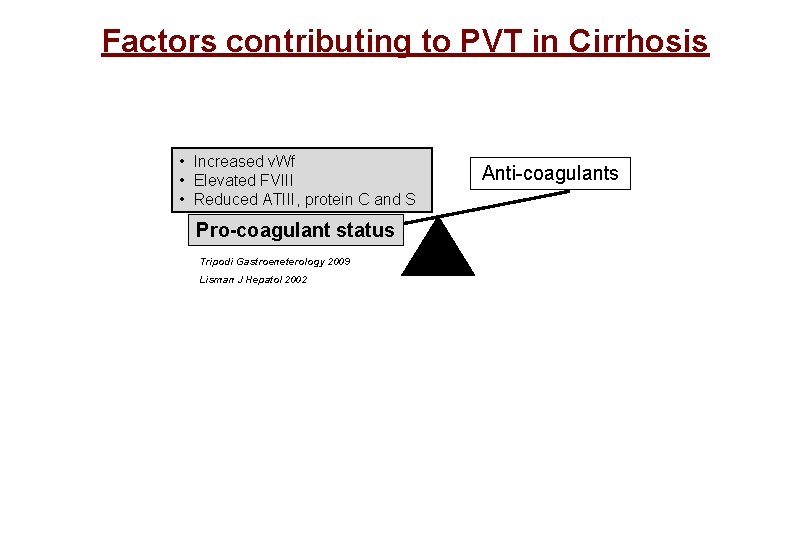
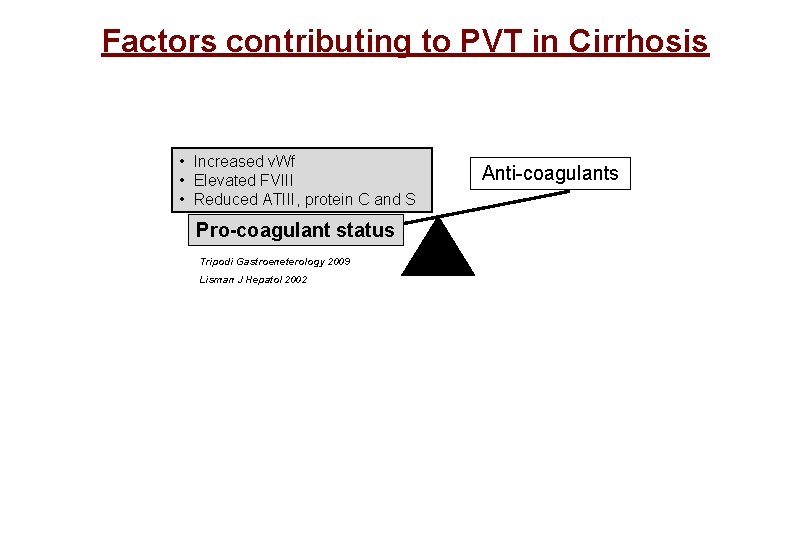
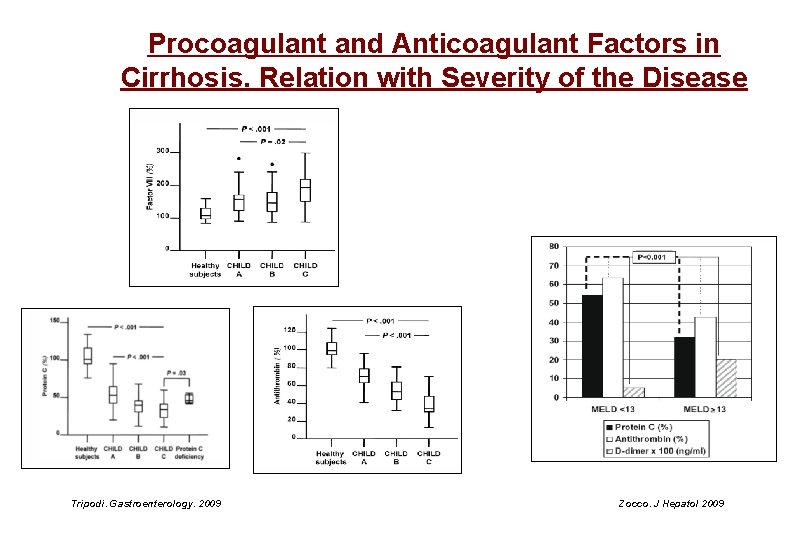
Factors contributing to PVT in Cirrhosis • Increased v. Wf • Elevated FVIII • Reduced ATIII, protein C and S Pro-coagulant status Tripodi Gastroeneterology 2009 Lisman J Hepatol 2002 Anti-coagulants
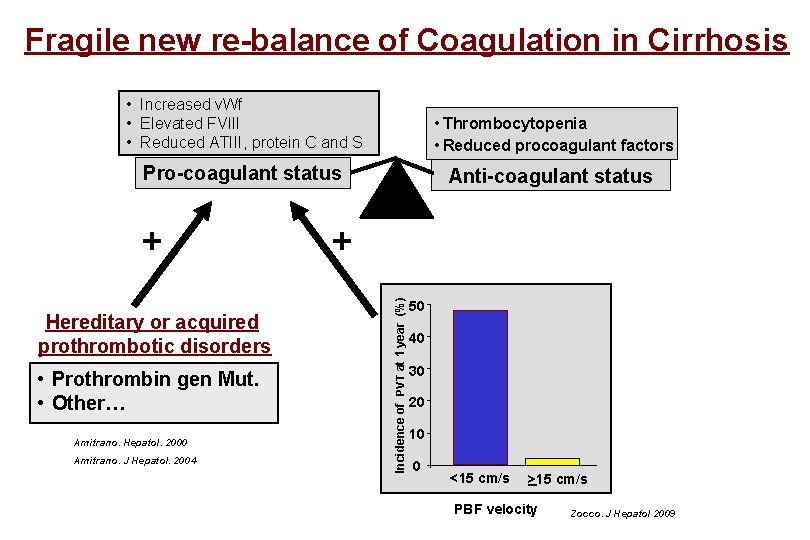
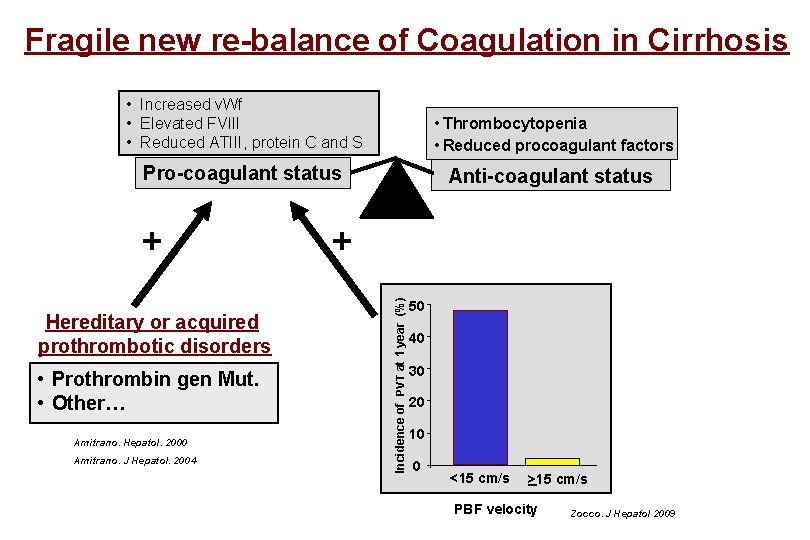
Fragile new re-balance of Coagulation in Cirrhosis • Increased v. Wf Pro-coagulants • Elevated FVIII • Reduced ATIII, protein C and S • Thrombocytopenia • Reduced procoagulant factors Pro-coagulant status Anti-coagulant status Hereditary or acquired prothrombotic disorders • Prothrombin gen Mut. • Other… Amitrano. Hepatol. 2000 Amitrano. J Hepatol. 2004 + Incidence of PVT at 1 year (%) + 50 40 30 20 10 0 <15 cm/s >15 cm/s PBF velocity Zocco. J Hepatol 2009
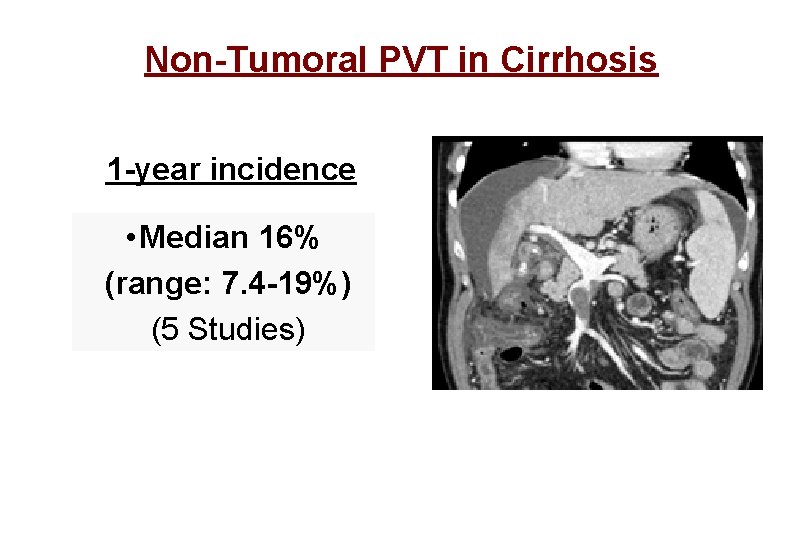
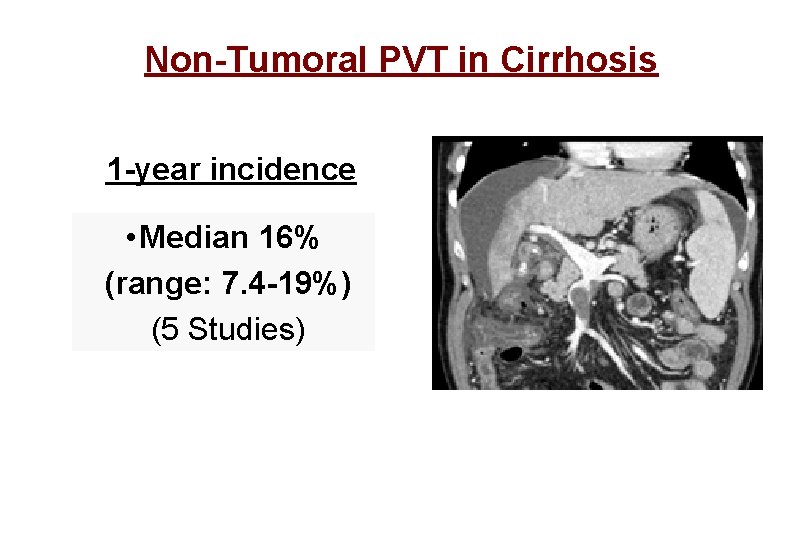
Non-Tumoral PVT in Cirrhosis 1 -year incidence • Median 16% (range: 7. 4 -19%) (5 Studies)
To treat or not to treat? • Whether PVT causes a further deterioration of the clinical condition (Variceal bleeding, ascites…) or actually appears when liver is already decompensated is not clear • More clear the impact on Liver Transplantation
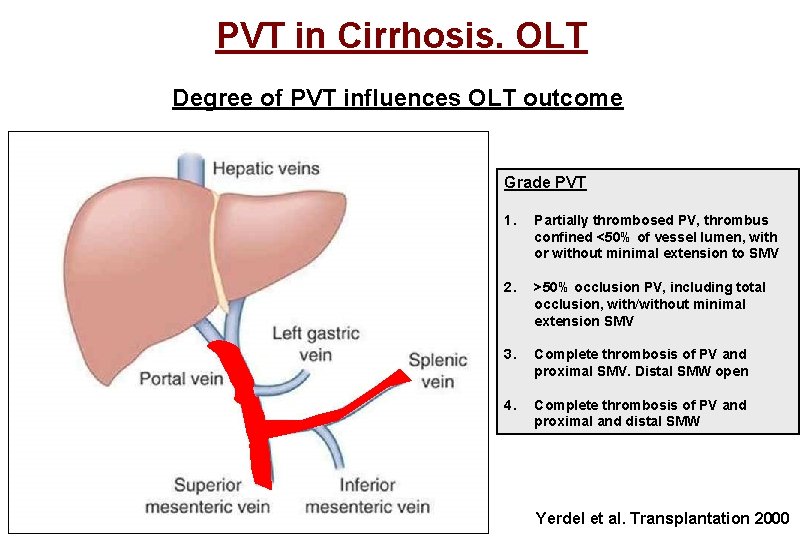
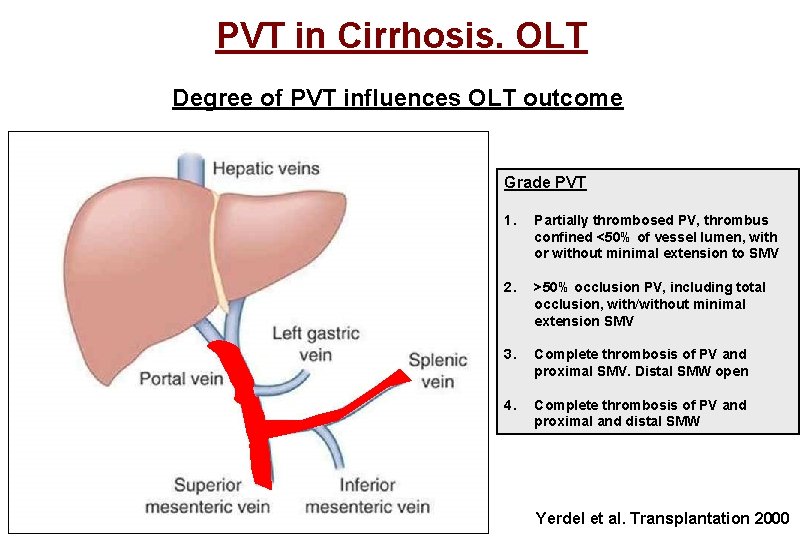
PVT in Cirrhosis. OLT Degree of PVT influences OLT outcome Grade PVT 1. Partially thrombosed PV, thrombus confined <50% of vessel lumen, with or without minimal extension to SMV 2. >50% occlusion PV, including total occlusion, with/without minimal extension SMV 3. Complete thrombosis of PV and proximal SMV. Distal SMW open 4. Complete thrombosis of PV and proximal and distal SMW Yerdel et al. Transplantation 2000
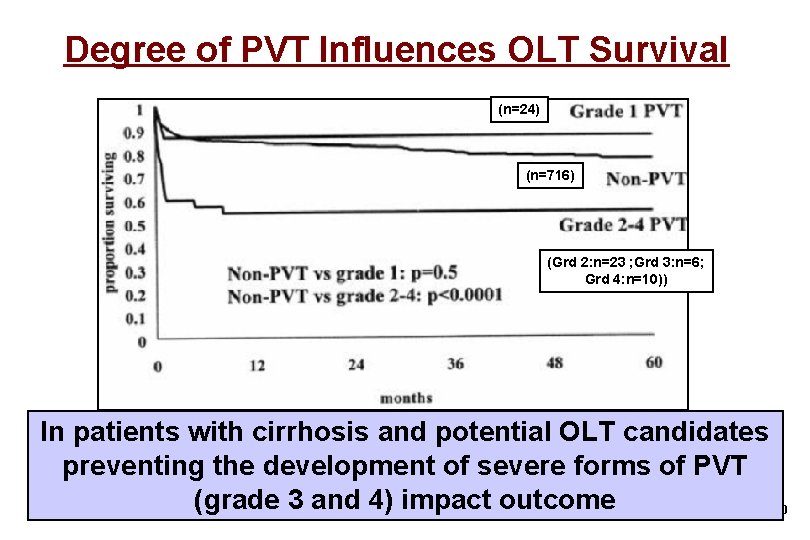
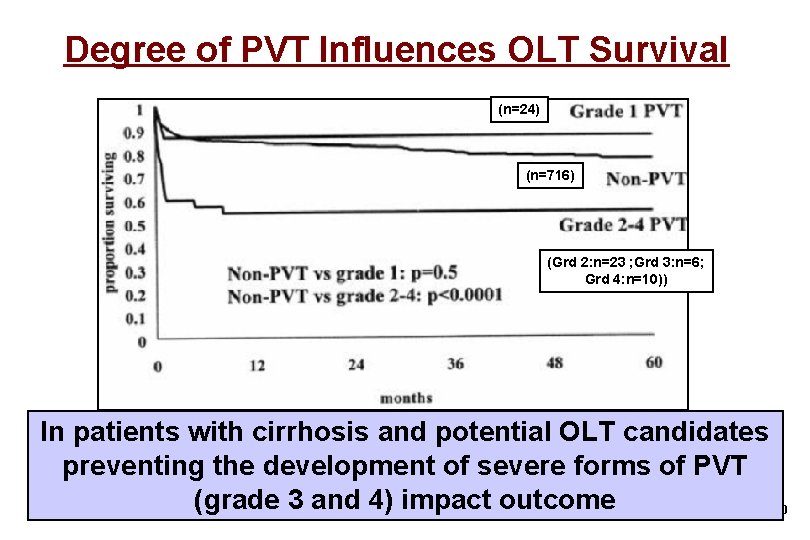
Degree of PVT Influences OLT Survival (n=24) (n=716) (Grd 2: n=23 ; Grd 3: n=6; Grd 4: n=10)) In patients with cirrhosis and potential OLT candidates preventing the development of severe forms of PVT (grade 3 and 4) impact outcome Yerdel et al. Transplantation 2000
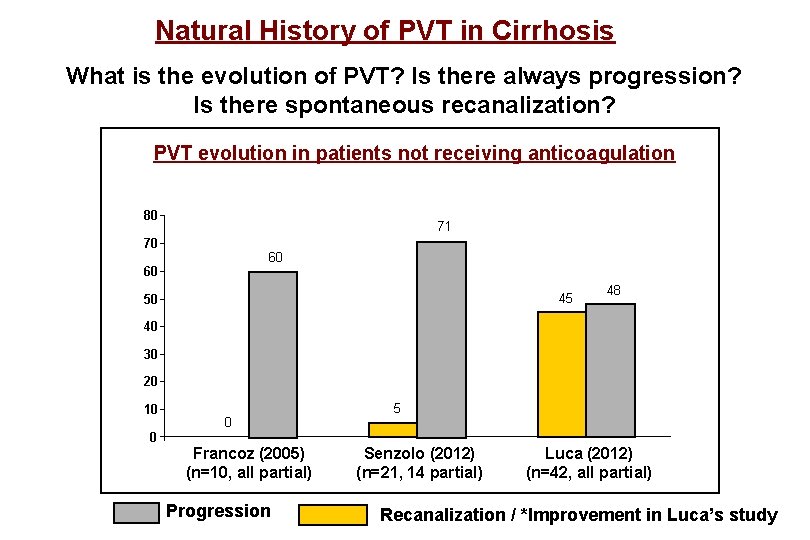
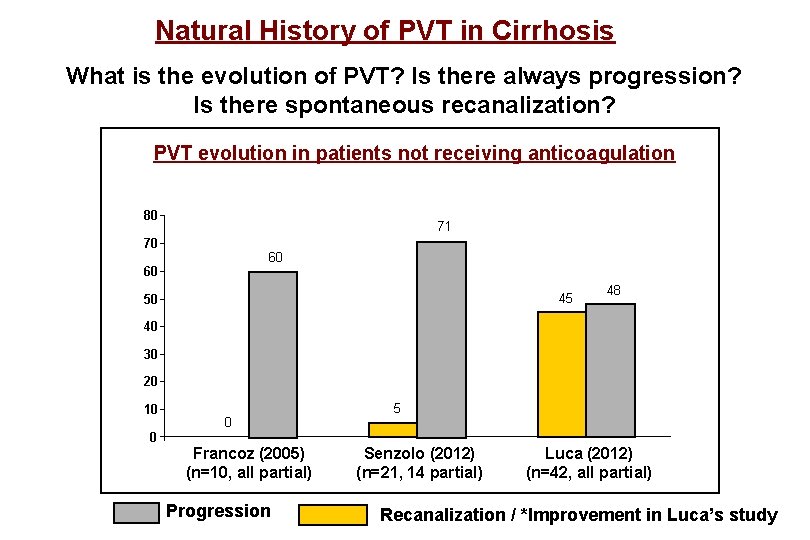
Natural History of PVT in Cirrhosis What is the evolution of PVT? Is there always progression? Is there spontaneous recanalization? PVT evolution in patients not receiving anticoagulation 80 71 70 60 60 45 50 48 40 30 20 10 0 0 Francoz (2005) (n=10, all partial) Progression 5 Senzolo (2012) (n=21, 14 partial) Luca (2012) (n=42, all partial) Recanalization / *Improvement in Luca’s study
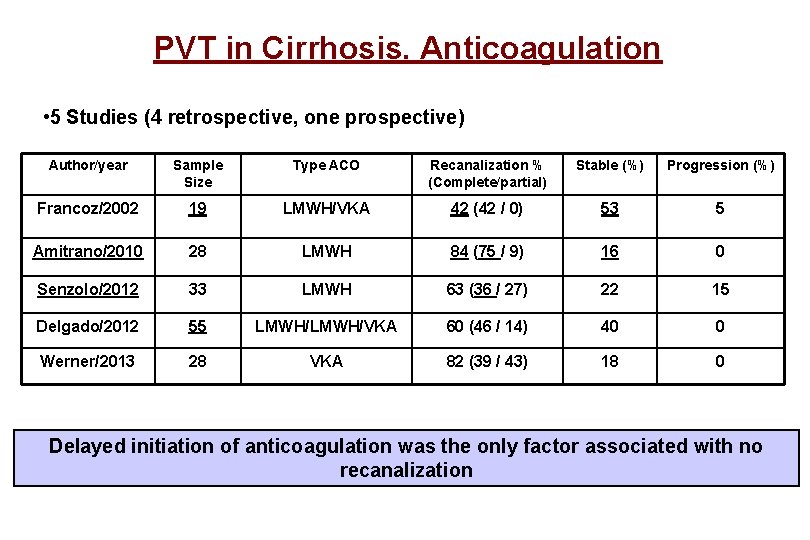
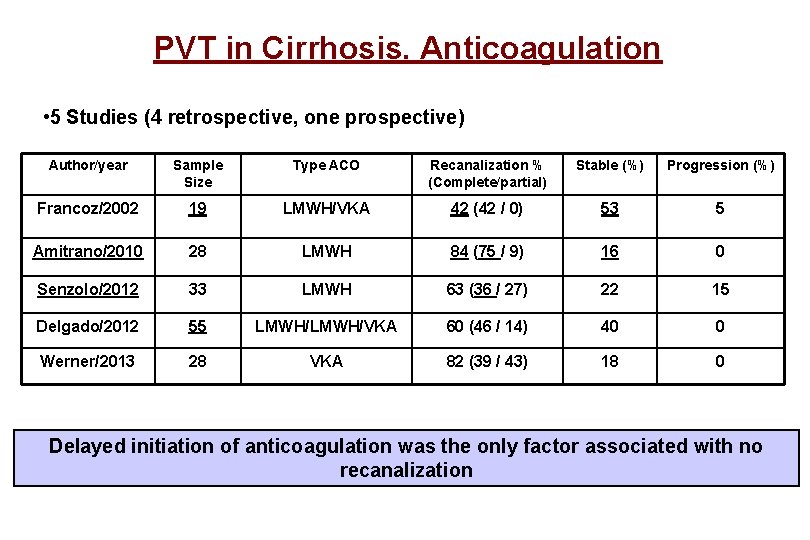
PVT in Cirrhosis. Anticoagulation • 5 Studies (4 retrospective, one prospective) Author/year Sample Size Type ACO Recanalization % (Complete/partial) Stable (%) Progression (%) Francoz/2002 19 LMWH/VKA 42 (42 / 0) 53 5 Amitrano/2010 28 LMWH 84 (75 / 9) 16 0 Senzolo/2012 33 LMWH 63 (36 / 27) 22 15 Delgado/2012 55 LMWH/VKA 60 (46 / 14) 40 0 Werner/2013 28 VKA 82 (39 / 43) 18 0 Delayed initiation of anticoagulation was the only factor associated with no recanalization
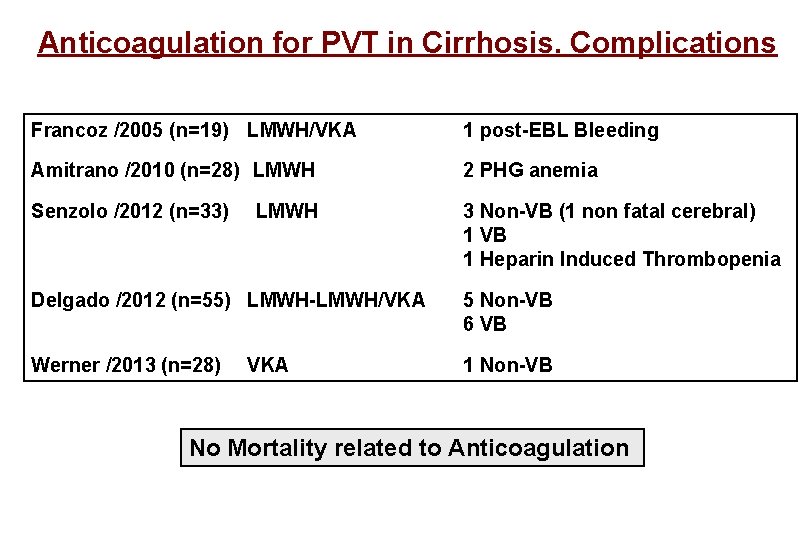
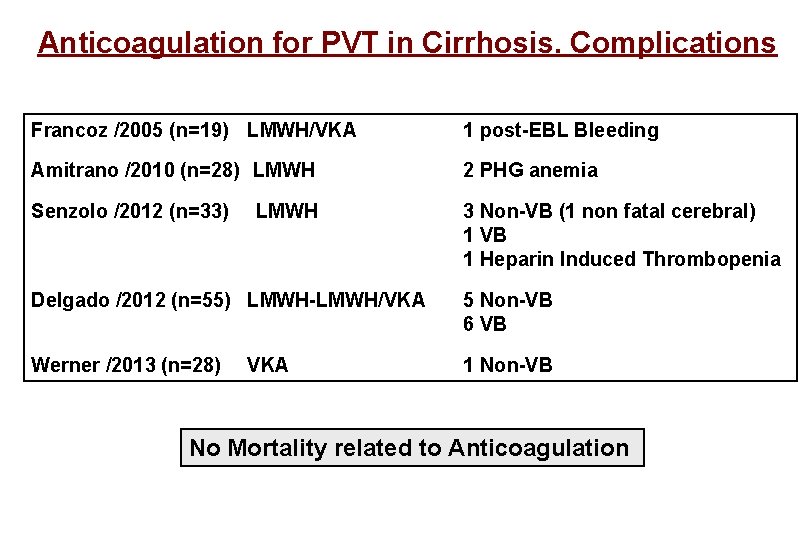
Anticoagulation for PVT in Cirrhosis. Complications Francoz /2005 (n=19) LMWH/VKA 1 post-EBL Bleeding Amitrano /2010 (n=28) LMWH 2 PHG anemia Senzolo /2012 (n=33) 3 Non-VB (1 non fatal cerebral) 1 VB 1 Heparin Induced Thrombopenia LMWH Delgado /2012 (n=55) LMWH-LMWH/VKA 5 Non-VB 6 VB Werner /2013 (n=28) 1 Non-VB VKA No Mortality related to Anticoagulation
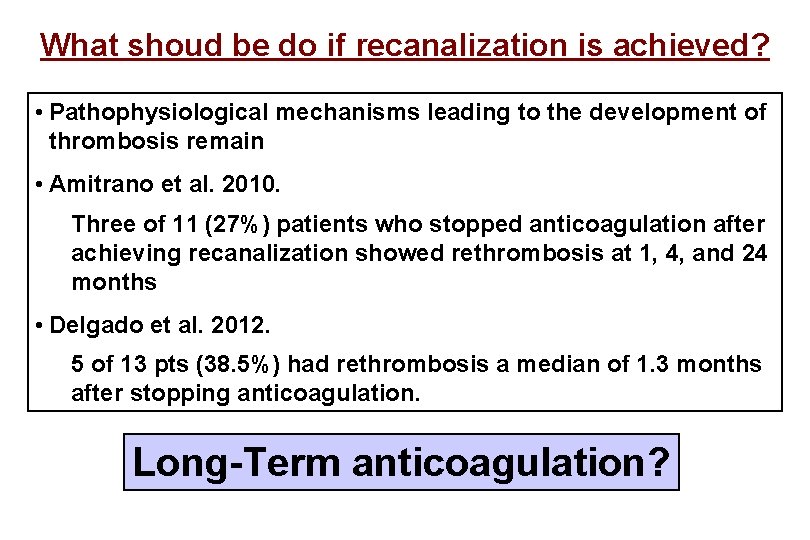
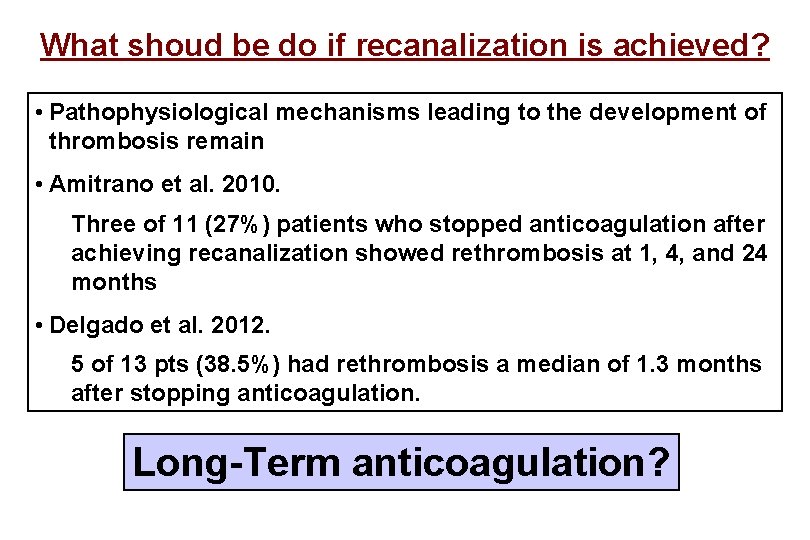
What shoud be do if recanalization is achieved? • Pathophysiological mechanisms leading to the development of thrombosis remain • Amitrano et al. 2010. Three of 11 (27%) patients who stopped anticoagulation after achieving recanalization showed rethrombosis at 1, 4, and 24 months • Delgado et al. 2012. 5 of 13 pts (38. 5%) had rethrombosis a median of 1. 3 months after stopping anticoagulation. Long-Term anticoagulation?
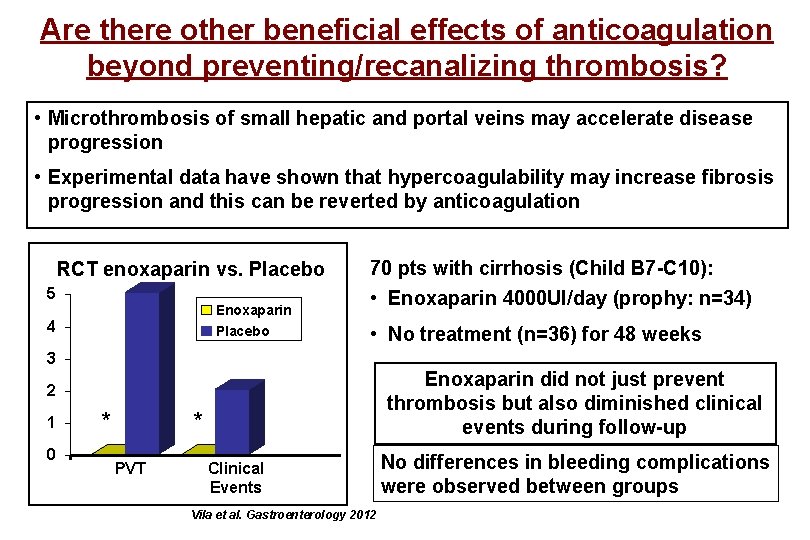
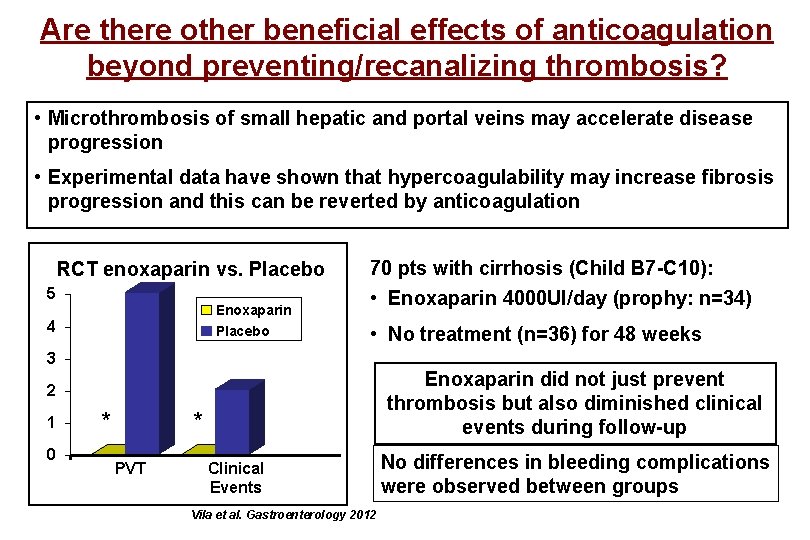
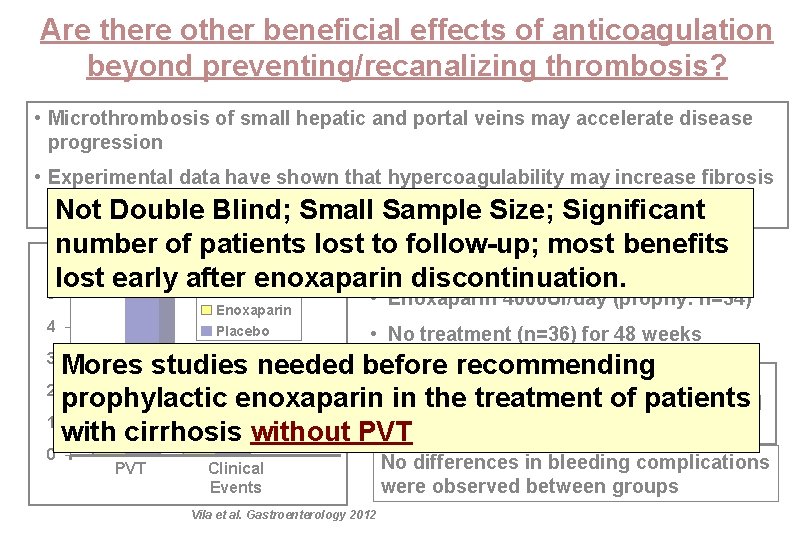
Are there other beneficial effects of anticoagulation beyond preventing/recanalizing thrombosis? • Microthrombosis of small hepatic and portal veins may accelerate disease progression • Experimental data have shown that hypercoagulability may increase fibrosis progression and this can be reverted by anticoagulation RCT enoxaparin vs. Placebo 5 Enoxaparin Placebo 4 70 pts with cirrhosis (Child B 7 -C 10): • Enoxaparin 4000 UI/day (prophy: n=34) • No treatment (n=36) for 48 weeks 3 Enoxaparin did not just prevent thrombosis but also diminished clinical events during follow-up 2 1 0 * * PVT Clinical Events Vila et al. Gastroenterology 2012 No differences in bleeding complications were observed between groups
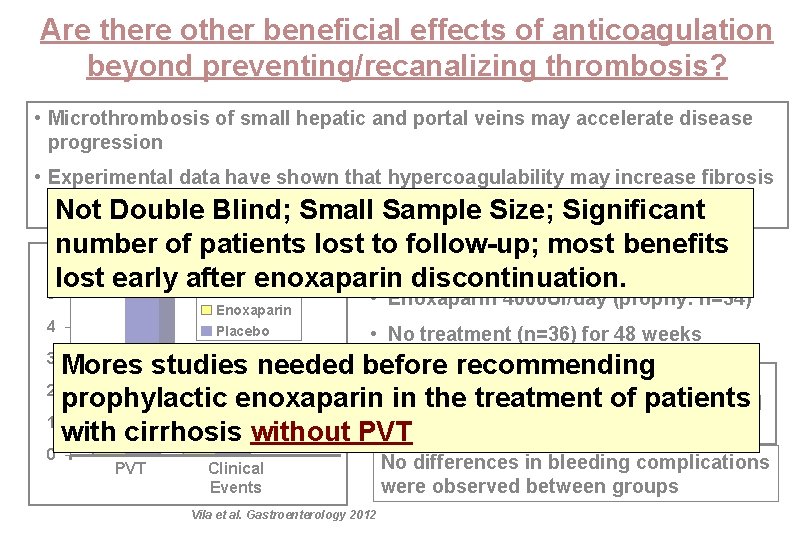
Are there other beneficial effects of anticoagulation beyond preventing/recanalizing thrombosis? • Microthrombosis of small hepatic and portal veins may accelerate disease progression • Experimental data have shown that hypercoagulability may increase fibrosis progression and this can be reverted by anticoagulation Not Double Blind; Small Sample Size; Significant number of patients lost to follow-up; most benefits 70 pts with cirrhosis (Child B 7 -C 10): RCT enoxaparin vs. Placebo lost early after enoxaparin discontinuation. 5 Enoxaparin Placebo 4 • Enoxaparin 4000 UI/day (prophy: n=34) • No treatment (n=36) for 48 weeks Mores studies needed before recommending Enoxaparin did not just prevent 2 prophylactic enoxaparin thrombosis in the treatment of patients but also diminished clinical * * 1 events during follow-up with cirrhosis without PVT 3 0 PVT Clinical Events Vila et al. Gastroenterology 2012 No differences in bleeding complications were observed between groups
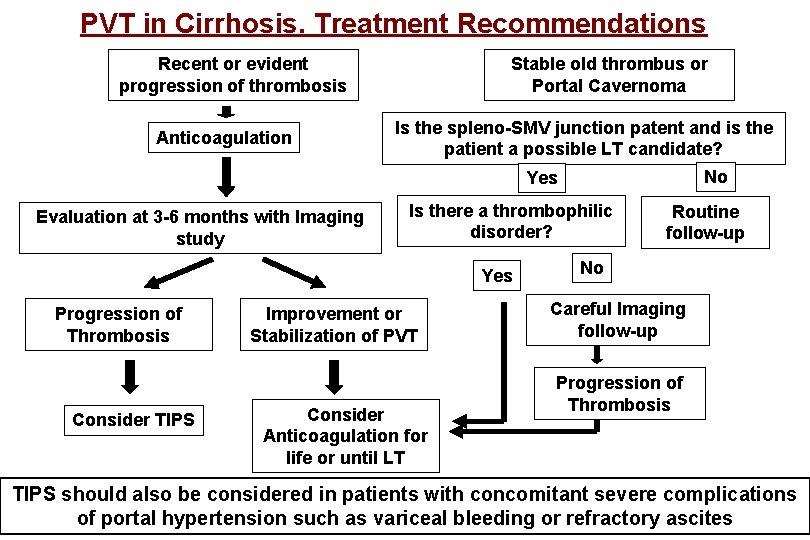
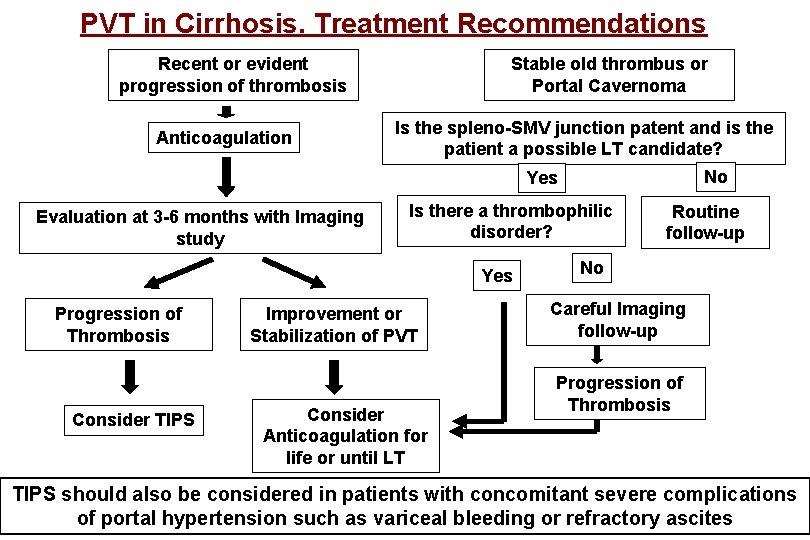
PVT in Cirrhosis. Treatment Recommendations Recent or evident progression of thrombosis Anticoagulation Stable old thrombus or Portal Cavernoma Is the spleno-SMV junction patent and is the patient a possible LT candidate? No Yes Evaluation at 3 -6 months with Imaging study Is there a thrombophilic disorder? Yes Progression of Thrombosis Consider TIPS Improvement or Stabilization of PVT Consider Anticoagulation for life or until LT Routine follow-up No Careful Imaging follow-up Progression of Thrombosis TIPS should also be considered in patients with concomitant severe complications of portal hypertension such as variceal bleeding or refractory ascites
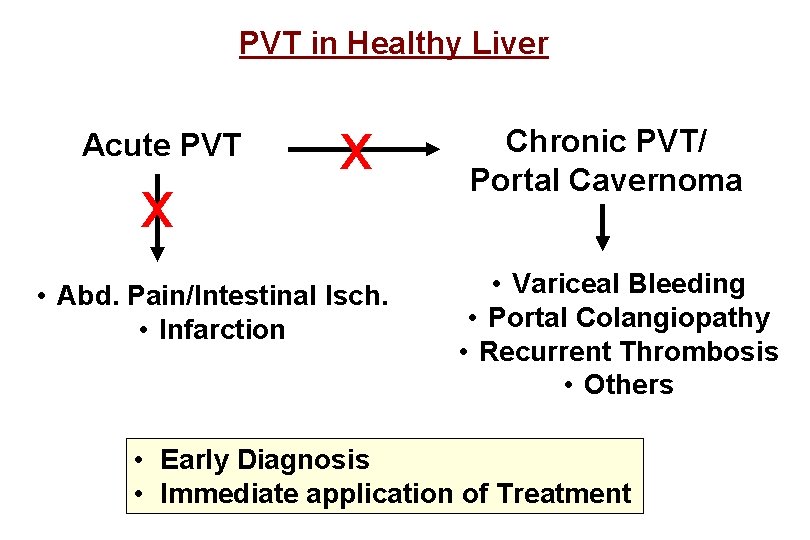
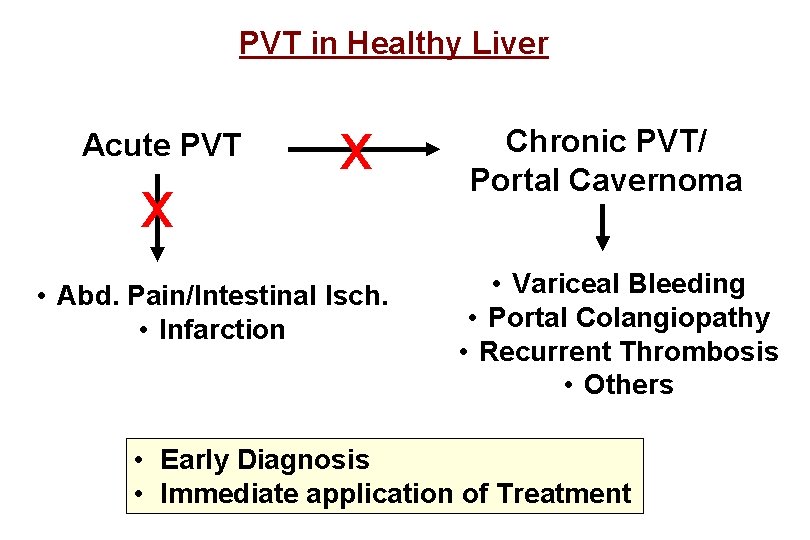
PVT in Healthy Liver Acute PVT x x • Abd. Pain/Intestinal Isch. • Infarction Chronic PVT/ Portal Cavernoma • Variceal Bleeding • Portal Colangiopathy • Recurrent Thrombosis • Others • Early Diagnosis • Immediate application of Treatment
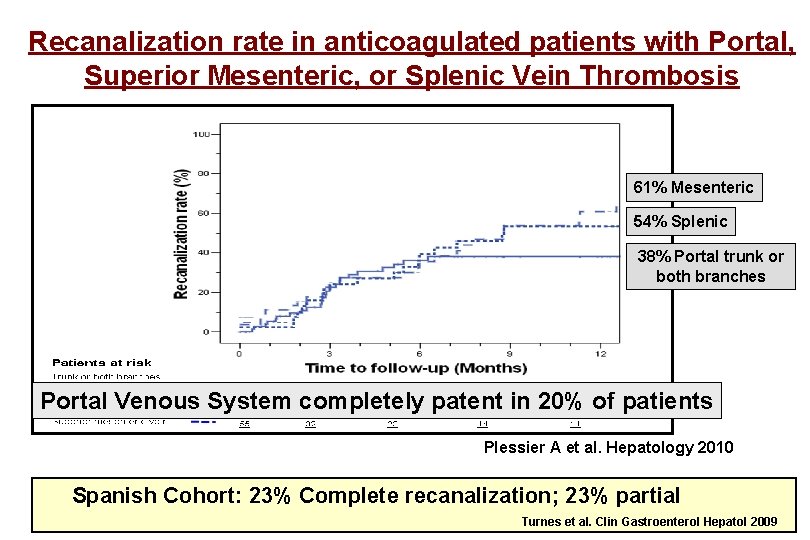
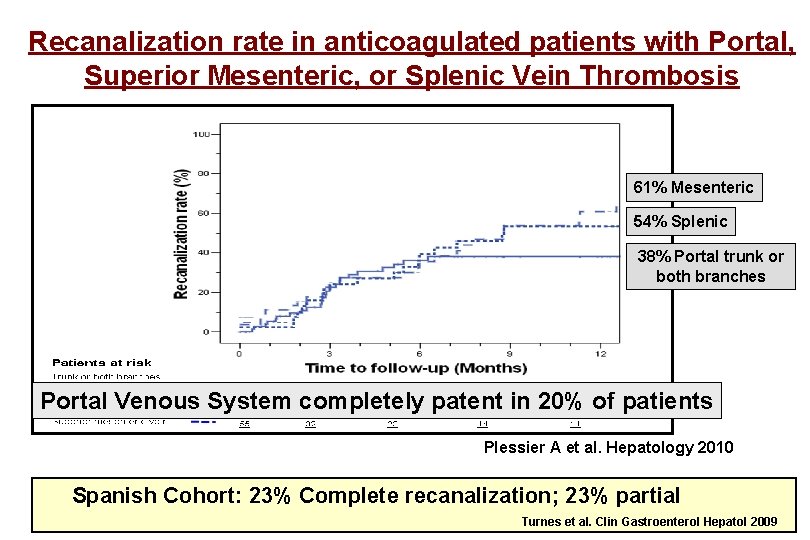
Recanalization rate in anticoagulated patients with Portal, Superior Mesenteric, or Splenic Vein Thrombosis 61% Mesenteric 54% Splenic 38% Portal trunk or both branches Portal Venous System completely patent in 20% of patients Plessier A et al. Hepatology 2010 Spanish Cohort: 23% Complete recanalization; 23% partial Turnes et al. Clin Gastroenterol Hepatol 2009
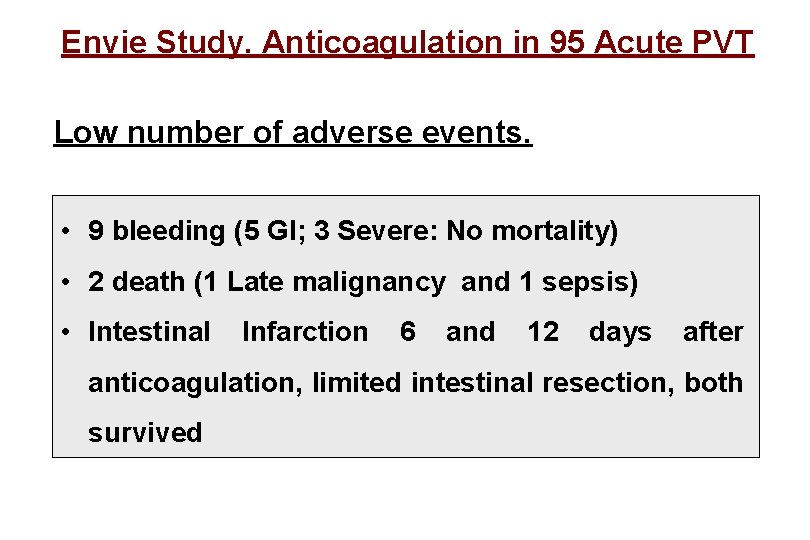
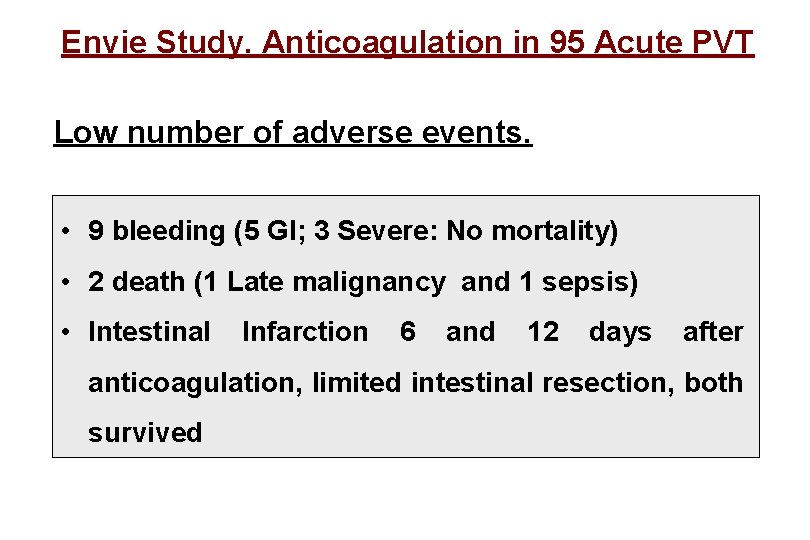
Envie Study. Anticoagulation in 95 Acute PVT Low number of adverse events. • 9 bleeding (5 GI; 3 Severe: No mortality) • 2 death (1 Late malignancy and 1 sepsis) • Intestinal Infarction 6 and 12 days after anticoagulation, limited intestinal resection, both survived
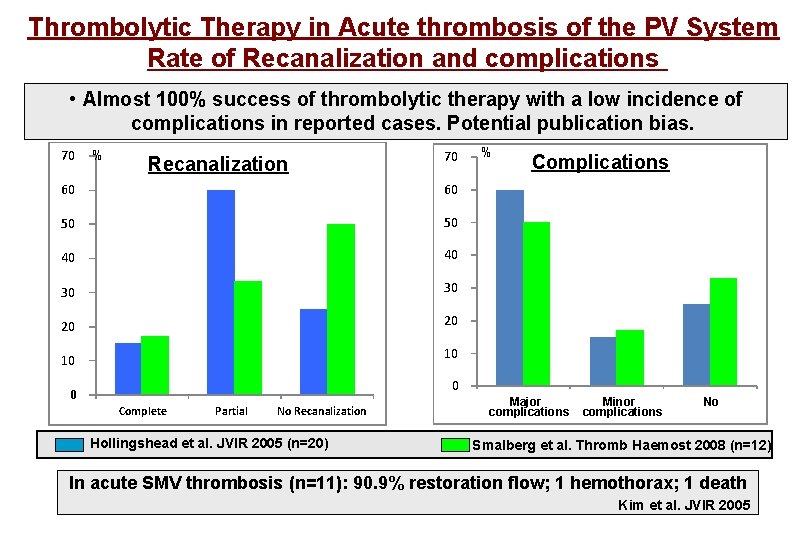
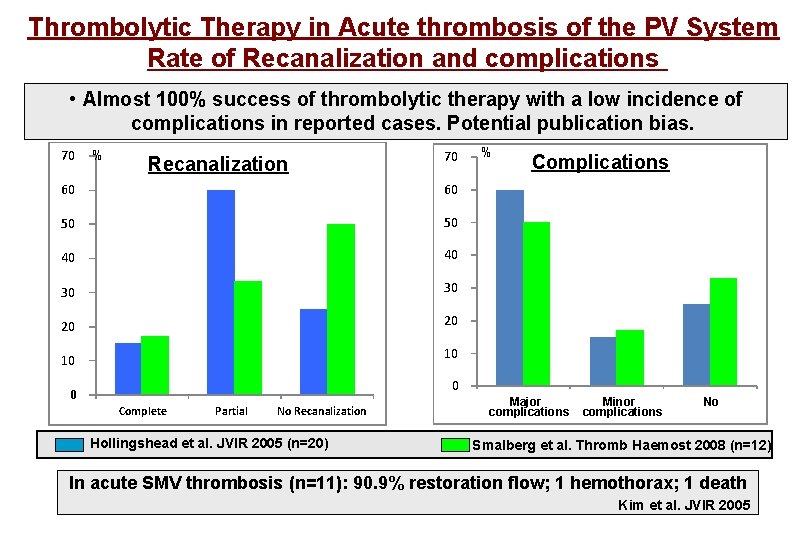
Thrombolytic Therapy in Acute thrombosis of the PV System Rate of Recanalization and complications • Almost 100% success of thrombolytic therapy with a low incidence of complications in reported cases. Potential publication bias. 70 % Recanalization 70 60 60 50 50 40 40 30 30 20 20 10 10 % Complications 0 0 Complete Partial No Recanalization Hollingshead et al. JVIR 2005 (n=20) Major complications Minor complications No Smalberg et al. Thromb Haemost 2008 (n=12) In acute SMV thrombosis (n=11): 90. 9% restoration flow; 1 hemothorax; 1 death Kim et al. JVIR 2005
Acute PVT. Recommendations for Treatment • Anticoagulation: First Choice Treatment • Thrombolysis/Thrombectomy if persistent or worsening symptoms despite anticoagulation (high risk of Intestinal Infarction!)
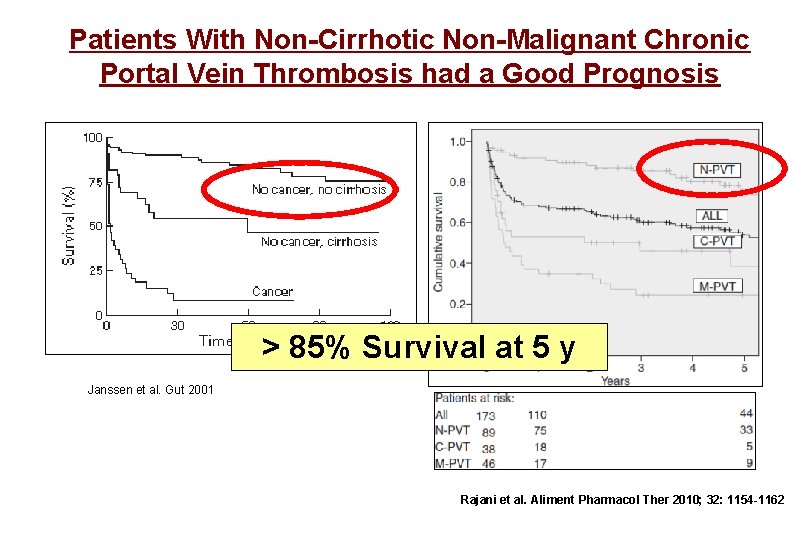
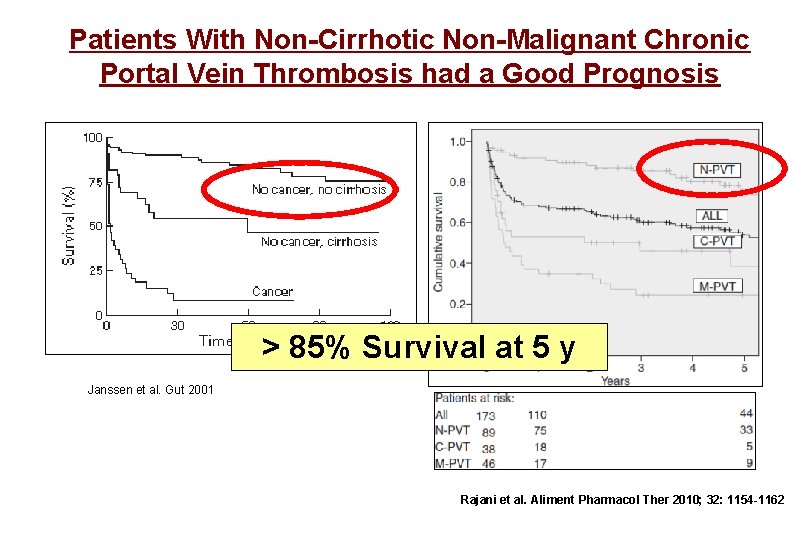
Patients With Non-Cirrhotic Non-Malignant Chronic Portal Vein Thrombosis had a Good Prognosis > 85% Survival at 5 y Janssen et al. Gut 2001 47 Rajani et al. Aliment Pharmacol Ther 2010; 32: 1154 -1162
Barcelona Portal Hypertension Team at Hospital Clinic in Barcelona Vascular liver diseases collaborative group Hepatic hemodynamics laboratory
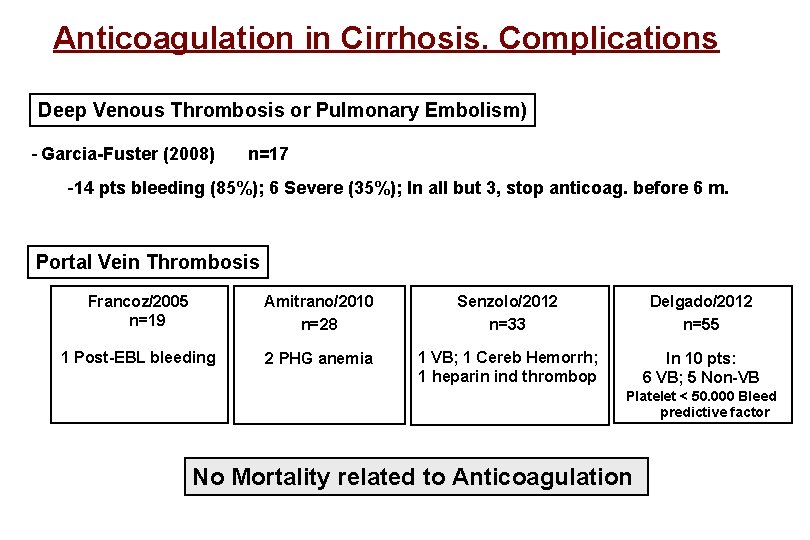
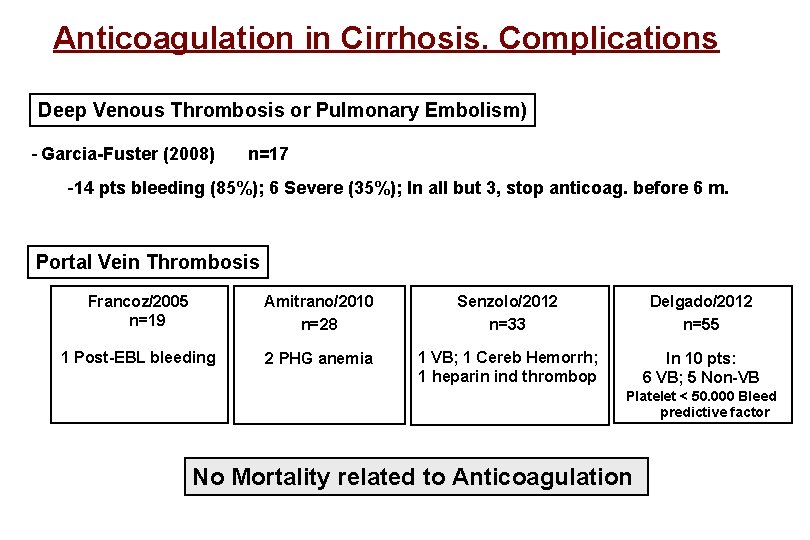
Anticoagulation in Cirrhosis. Complications Deep Venous Thrombosis or Pulmonary Embolism) - Garcia-Fuster (2008) n=17 -14 pts bleeding (85%); 6 Severe (35%); In all but 3, stop anticoag. before 6 m. Portal Vein Thrombosis Francoz/2005 n=19 Amitrano/2010 n=28 Senzolo/2012 n=33 Delgado/2012 n=55 1 Post-EBL bleeding 2 PHG anemia 1 VB; 1 Cereb Hemorrh; 1 heparin ind thrombop In 10 pts: 6 VB; 5 Non-VB Platelet < 50. 000 Bleed predictive factor No Mortality related to Anticoagulation
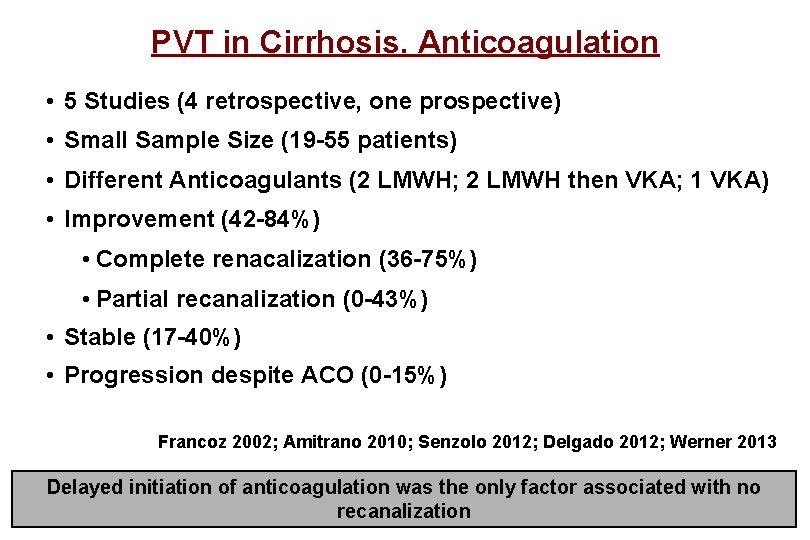
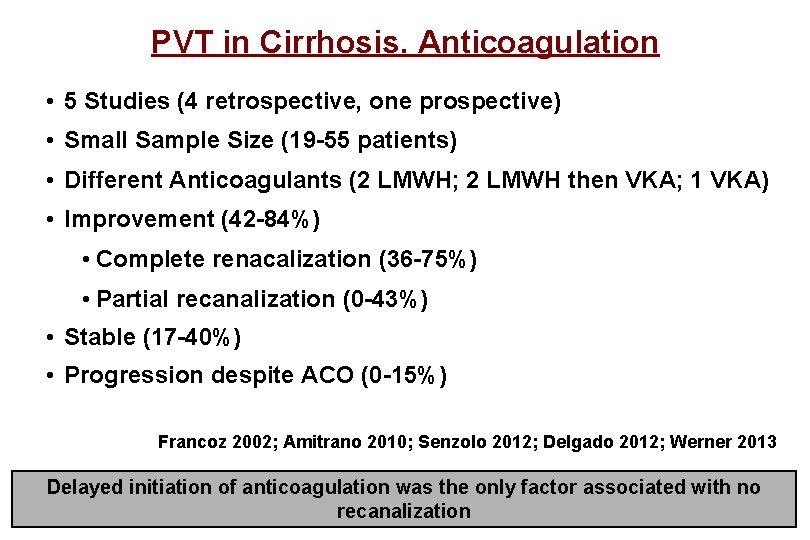
PVT in Cirrhosis. Anticoagulation • 5 Studies (4 retrospective, one prospective) • Small Sample Size (19 -55 patients) • Different Anticoagulants (2 LMWH; 2 LMWH then VKA; 1 VKA) • Improvement (42 -84%) • Complete renacalization (36 -75%) • Partial recanalization (0 -43%) • Stable (17 -40%) • Progression despite ACO (0 -15%) Francoz 2002; Amitrano 2010; Senzolo 2012; Delgado 2012; Werner 2013 Delayed initiation of anticoagulation was the only factor associated with no recanalization
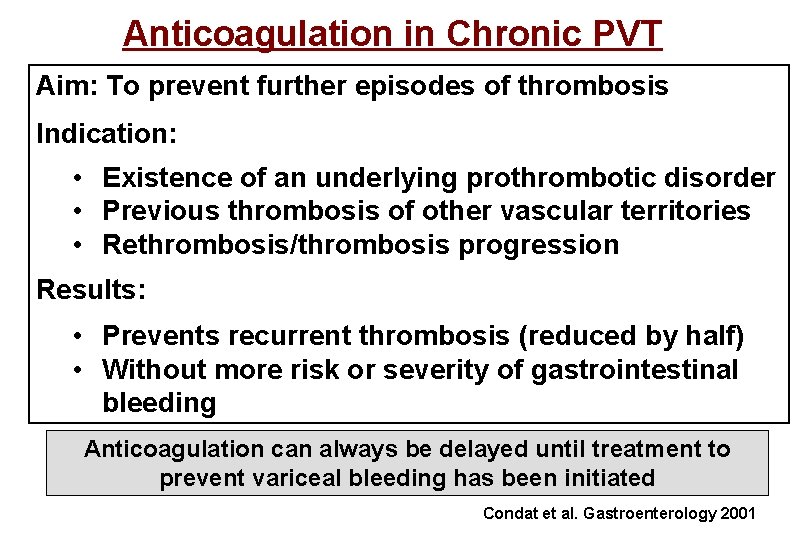
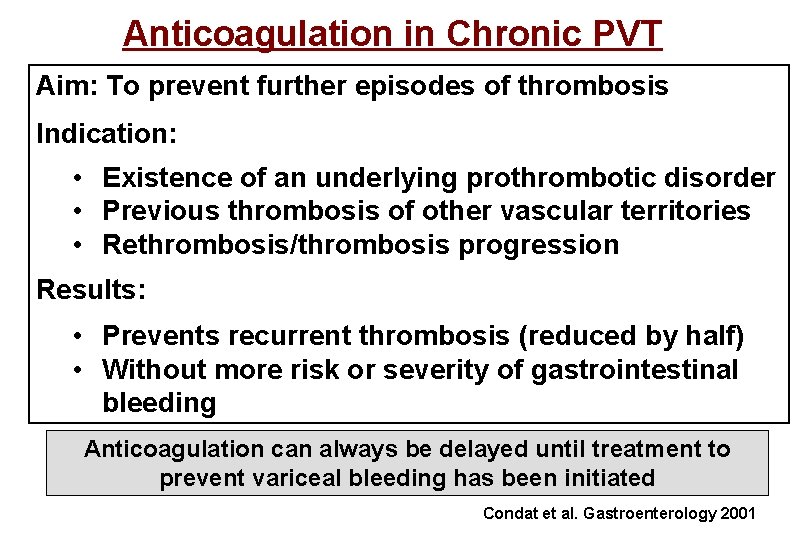
Anticoagulation in Chronic PVT Aim: To prevent further episodes of thrombosis Indication: • Existence of an underlying prothrombotic disorder • Previous thrombosis of other vascular territories • Rethrombosis/thrombosis progression Results: • Prevents recurrent thrombosis (reduced by half) • Without more risk or severity of gastrointestinal bleeding Anticoagulation can always be delayed until treatment to prevent variceal bleeding has been initiated Condat et al. Gastroenterology 2001
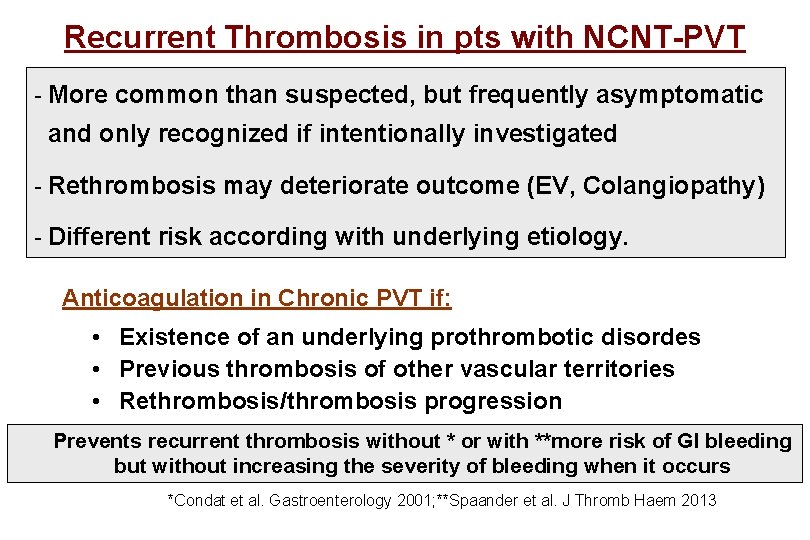
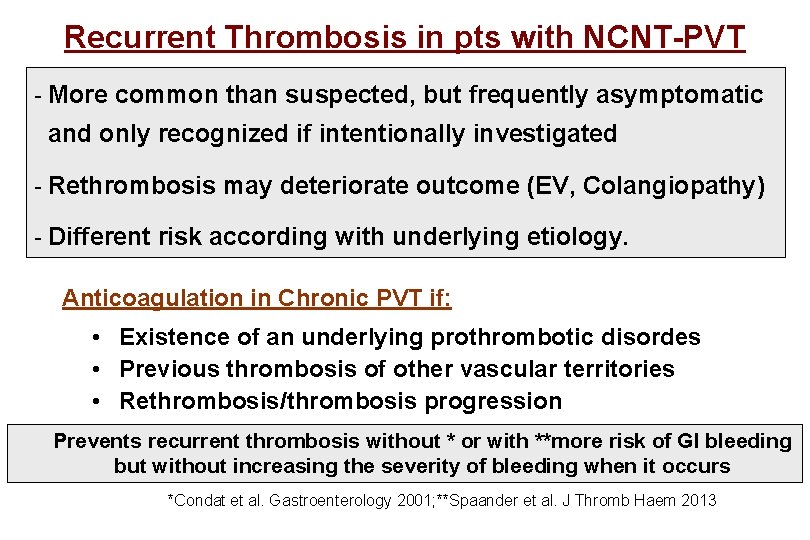
Recurrent Thrombosis in pts with NCNT-PVT - More common than suspected, but frequently asymptomatic and only recognized if intentionally investigated - Rethrombosis may deteriorate outcome (EV, Colangiopathy) - Different risk according with underlying etiology. Anticoagulation in Chronic PVT if: • Existence of an underlying prothrombotic disordes • Previous thrombosis of other vascular territories • Rethrombosis/thrombosis progression Prevents recurrent thrombosis without * or with **more risk of GI bleeding but without increasing the severity of bleeding when it occurs *Condat et al. Gastroenterology 2001; **Spaander et al. J Thromb Haem 2013
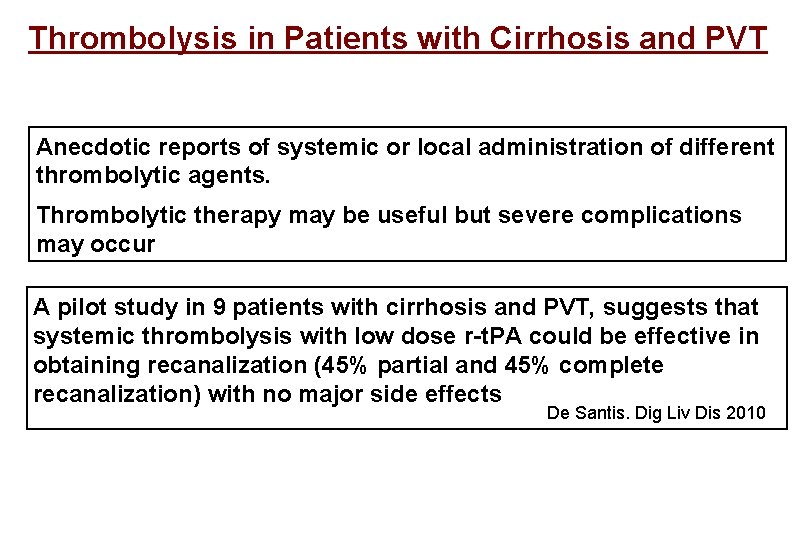
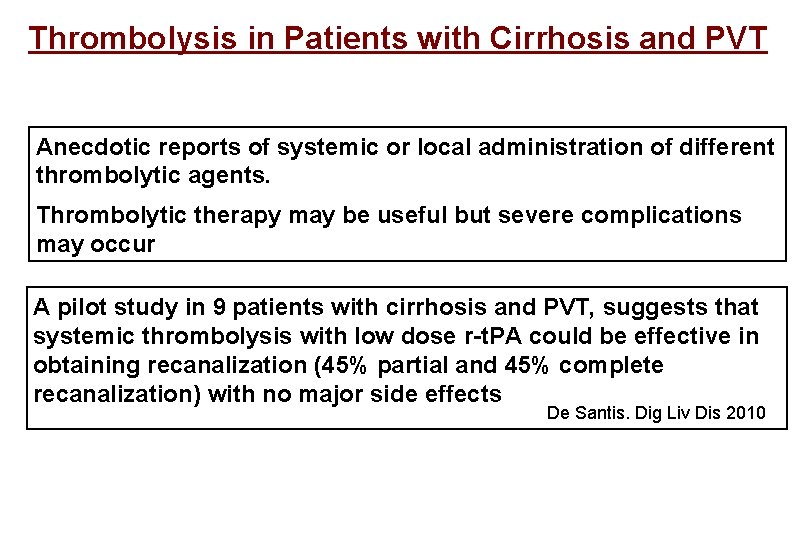
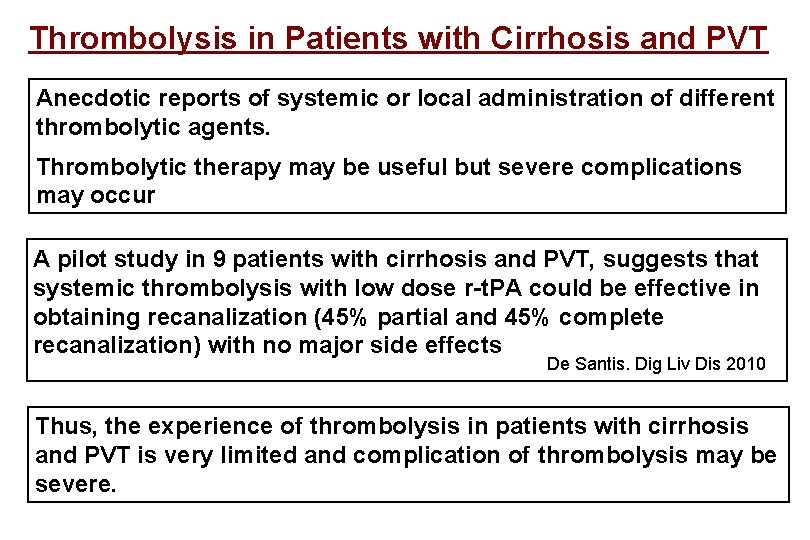
Thrombolysis in Patients with Cirrhosis and PVT Anecdotic reports of systemic or local administration of different thrombolytic agents. Thrombolytic therapy may be useful but severe complications may occur A pilot study in 9 patients with cirrhosis and PVT, suggests that systemic thrombolysis with low dose r-t. PA could be effective in obtaining recanalization (45% partial and 45% complete recanalization) with no major side effects De Santis. Dig Liv Dis 2010
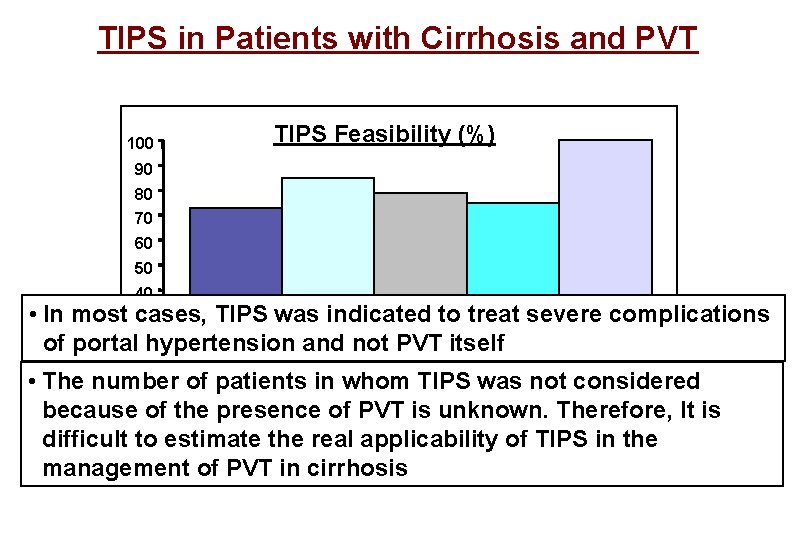
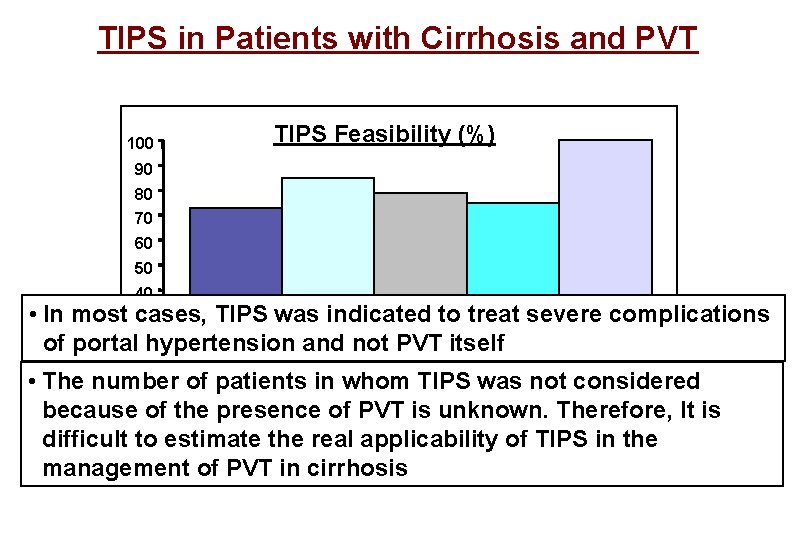
TIPS in Patients with Cirrhosis and PVT 100 TIPS Feasibility (%) 90 80 70 60 50 40 • In most cases, TIPS was indicated to treat severe complications 30 of portal 20 hypertension and not PVT itself 10 • The number of patients in whom TIPS was not considered 0 Senzolo 2006 Van Ha 2006 Perarnau 2010 Luca 2011 Han 2011 because of the presence isptsunknown. Therefore, It is 25 pts 15 of pts PVT 34 70 pts 57 pts difficult to estimate the real applicability of TIPS in the management of PVT in cirrhosis
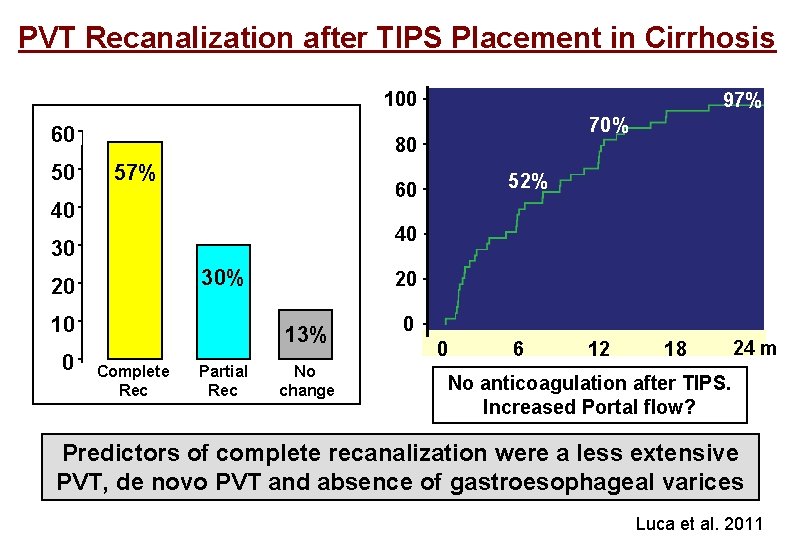
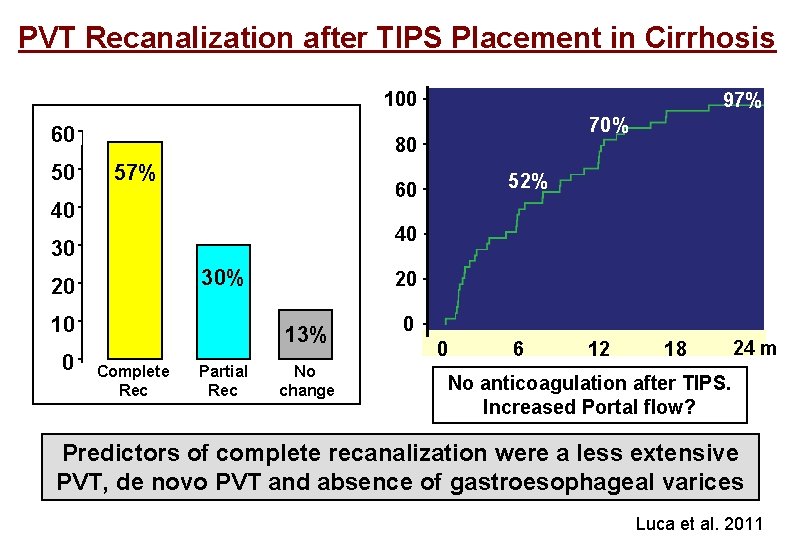
PVT Recanalization after TIPS Placement in Cirrhosis 100 60 50 70% 80 57% 52% 60 40 40 30 30% 20 10 0 97% 20 13% Complete Rec Partial Rec No change 0 0 6 12 18 24 m No anticoagulation after TIPS. Increased Portal flow? Predictors of complete recanalization were a less extensive PVT, de novo PVT and absence of gastroesophageal varices Luca et al. 2011
A Long Way to go…
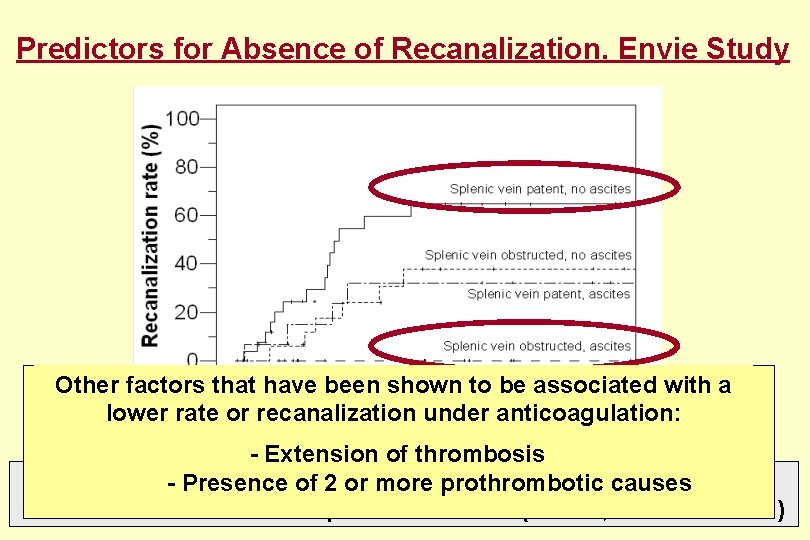
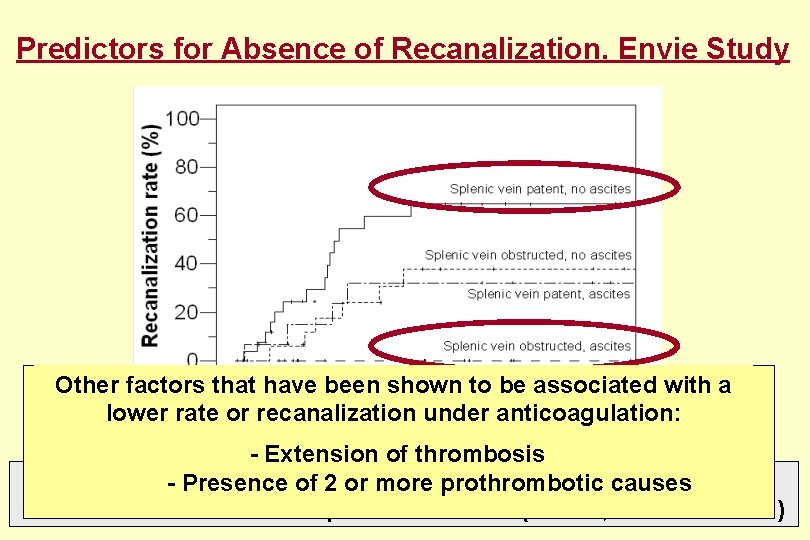
Predictors for Absence of Recanalization. Envie Study Other factors that have been shown to be associated with a lower rate or recanalization under anticoagulation: - Extension of thrombosis Multivariate analysis: Ascites (HR 3. 2, 95%causes CI 1. 3 -8) - Presence of 2 or more prothrombotic Splenic vein obst. (HR 3. 2, 95% CI 1. 3 -7. 6)
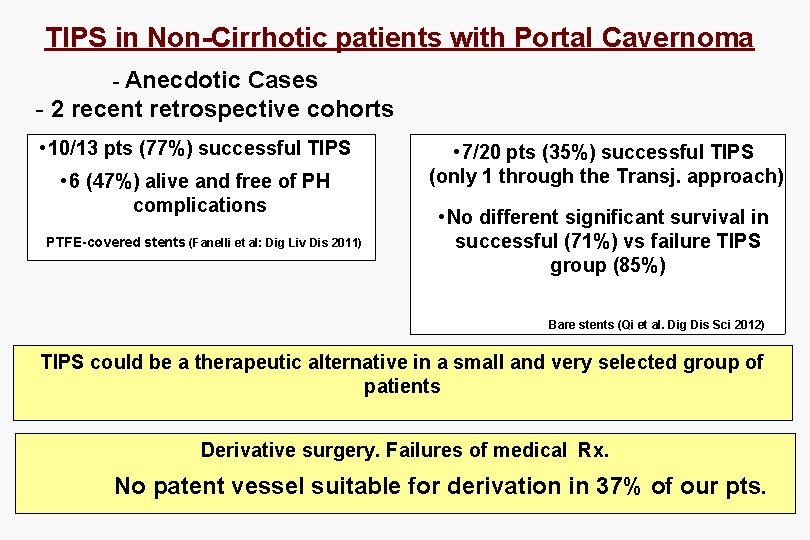
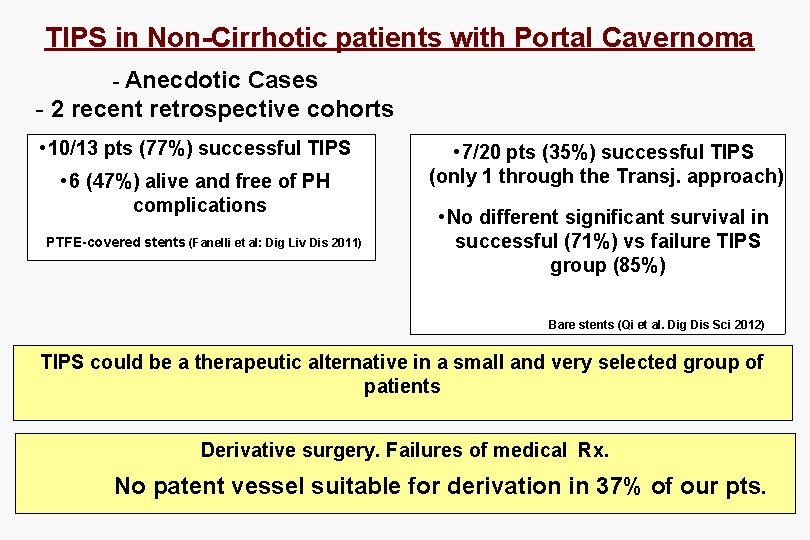
TIPS in Non-Cirrhotic patients with Portal Cavernoma - Anecdotic Cases - 2 recent retrospective cohorts • 10/13 pts (77%) successful TIPS • 6 (47%) alive and free of PH complications PTFE-covered stents (Fanelli et al: Dig Liv Dis 2011) • 7/20 pts (35%) successful TIPS (only 1 through the Transj. approach) • No different significant survival in successful (71%) vs failure TIPS group (85%) Bare stents (Qi et al. Dig Dis Sci 2012) TIPS could be a therapeutic alternative in a small and very selected group of patients Derivative surgery. Failures of medical Rx. No patent vessel suitable for derivation in 37% of our pts.
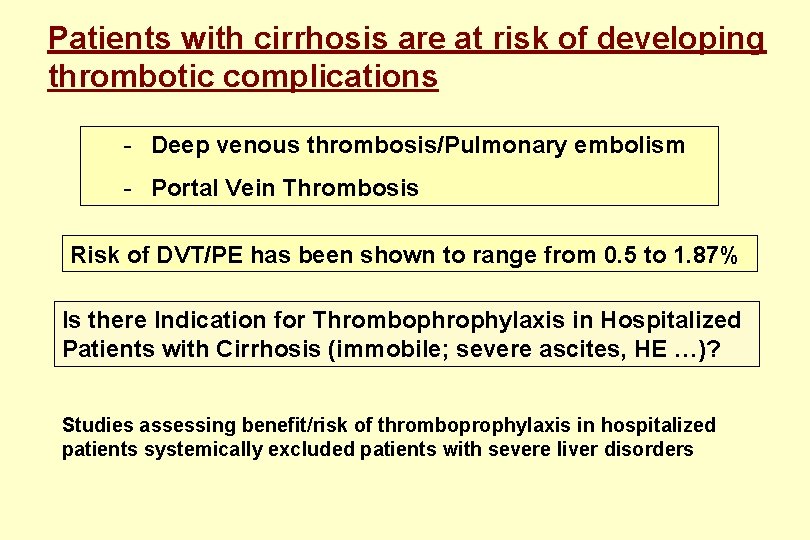
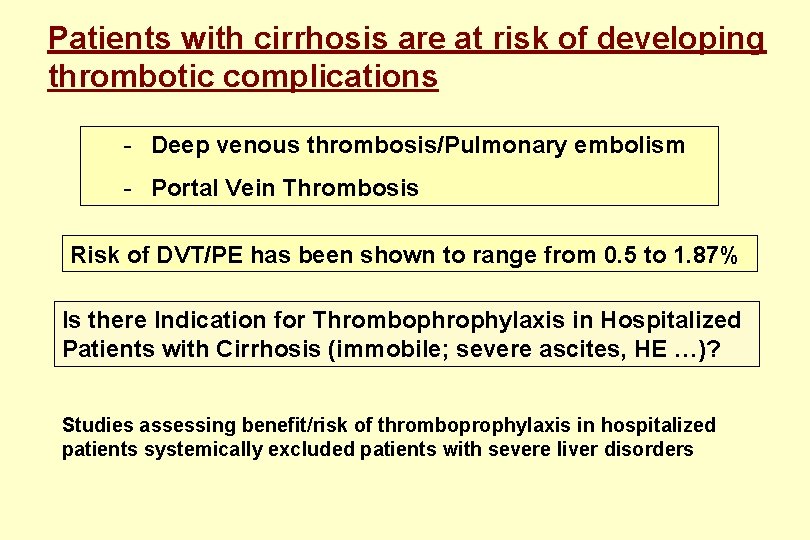
Patients with cirrhosis are at risk of developing thrombotic complications - Deep venous thrombosis/Pulmonary embolism - Portal Vein Thrombosis Risk of DVT/PE has been shown to range from 0. 5 to 1. 87% Is there Indication for Thrombophrophylaxis in Hospitalized Patients with Cirrhosis (immobile; severe ascites, HE …)? Studies assessing benefit/risk of thromboprophylaxis in hospitalized patients systemically excluded patients with severe liver disorders
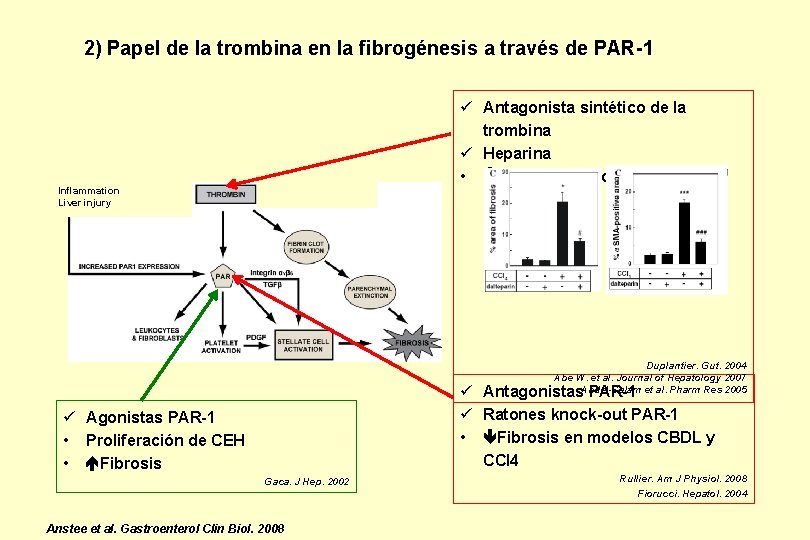
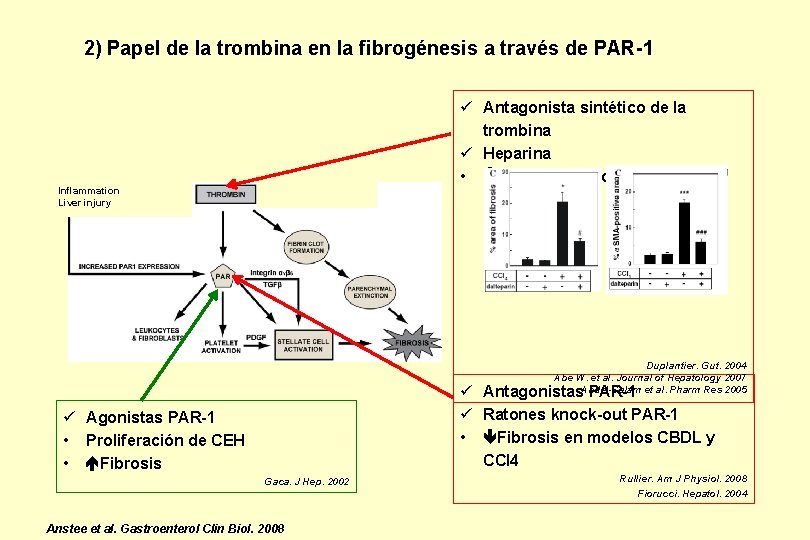
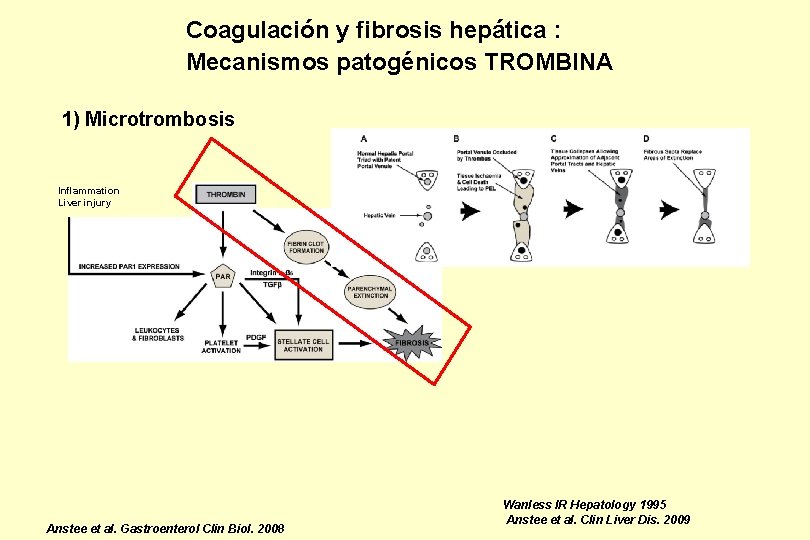
2) Papel de la trombina en la fibrogénesis a través de PAR-1 ü Antagonista sintético de la trombina ü Heparina • Fibrosis en modelos CBDL y CCl 4 Inflammation Liver injury Duplantier. Gut. 2004 Abe W. et al. Journal of Hepatology 2007 Abdel-Salam et al. Pharm Res 2005 ü Antagonistas PAR-1 ü Ratones knock-out PAR-1 • Fibrosis en modelos CBDL y CCl 4 ü Agonistas PAR-1 • Proliferación de CEH • Fibrosis Gaca. J Hep. 2002 Anstee et al. Gastroenterol Clin Biol. 2008 Rullier. Am J Physiol. 2008 Fiorucci. Hepatol. 2004
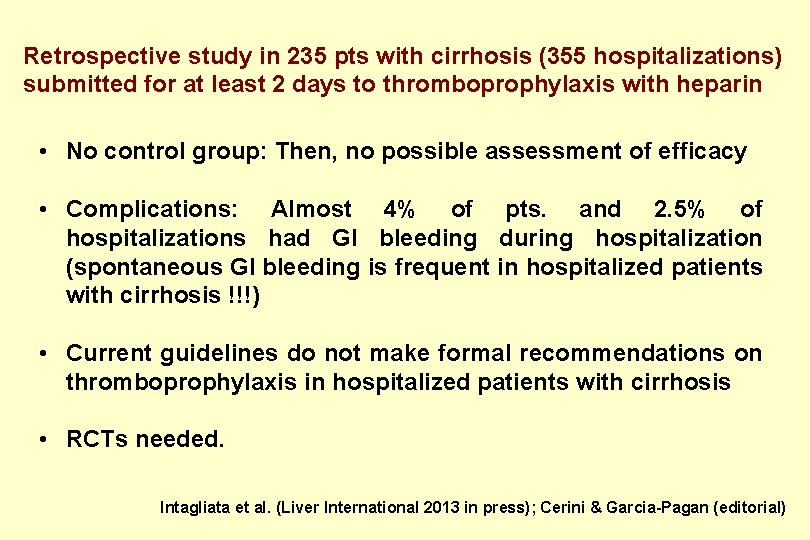
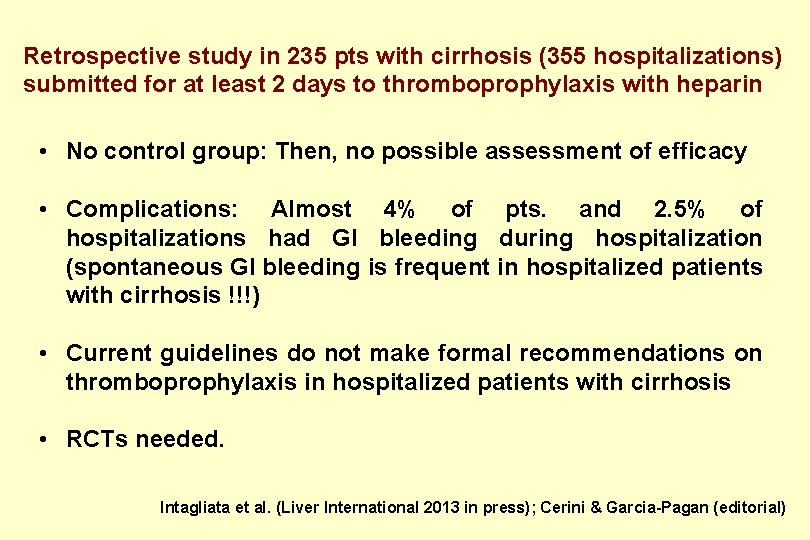
Retrospective study in 235 pts with cirrhosis (355 hospitalizations) submitted for at least 2 days to thromboprophylaxis with heparin • No control group: Then, no possible assessment of efficacy • Complications: Almost 4% of pts. and 2. 5% of hospitalizations had GI bleeding during hospitalization (spontaneous GI bleeding is frequent in hospitalized patients with cirrhosis !!!) • Current guidelines do not make formal recommendations on thromboprophylaxis in hospitalized patients with cirrhosis • RCTs needed. Intagliata et al. (Liver International 2013 in press); Cerini & Garcia-Pagan (editorial)
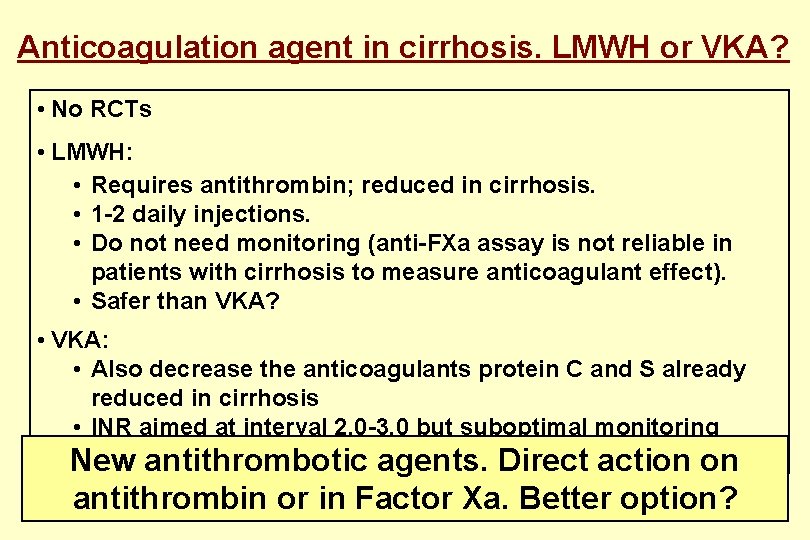
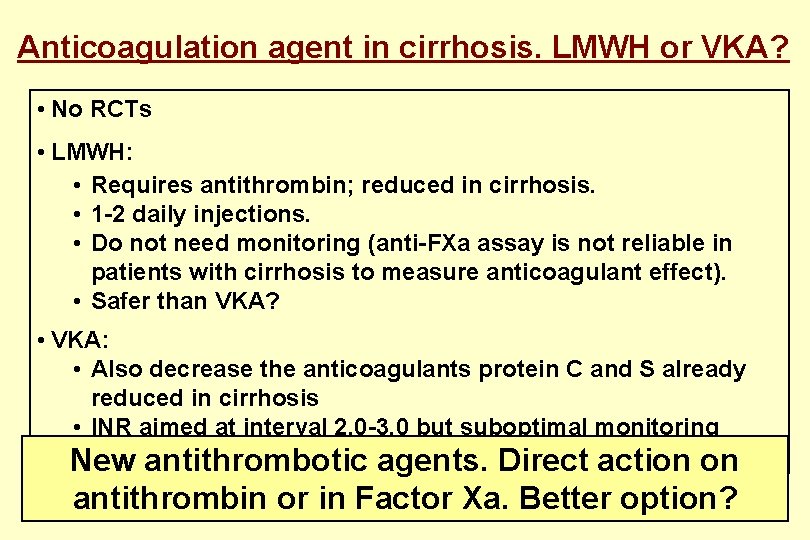
Anticoagulation agent in cirrhosis. LMWH or VKA? • No RCTs • LMWH: • Requires antithrombin; reduced in cirrhosis. • 1 -2 daily injections. • Do not need monitoring (anti-FXa assay is not reliable in patients with cirrhosis to measure anticoagulant effect). • Safer than VKA? • VKA: • Also decrease the anticoagulants protein C and S already reduced in cirrhosis • INR aimed at interval 2. 0 -3. 0 but suboptimal monitoring usingantithrombotic INR. Value of Modified INR (INR-Liver) unknown. on New agents. Direct action antithrombin or in Factor Xa. Better option?
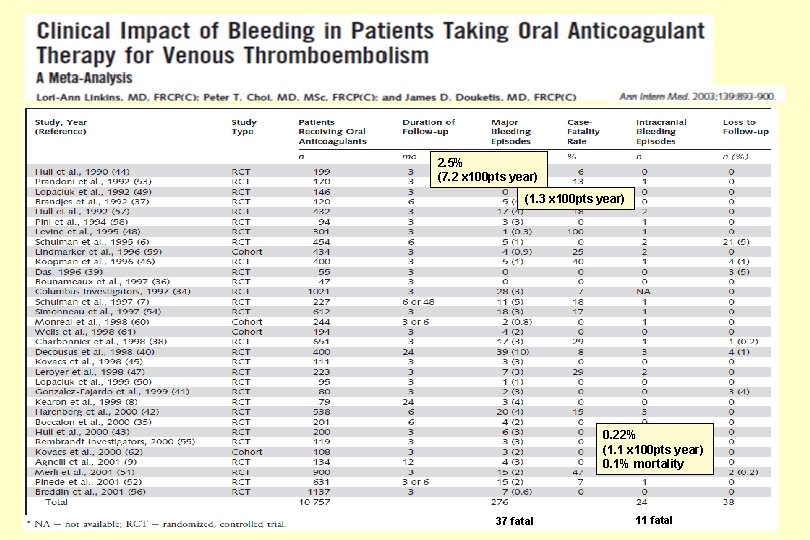
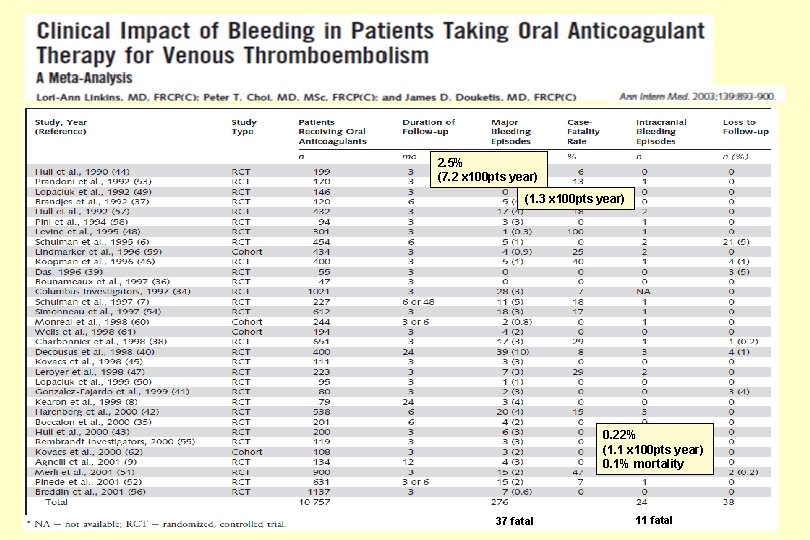
2. 5% (7. 2 x 100 pts year) (1. 3 x 100 pts year) 0. 22% (1. 1 x 100 pts year) 0. 1% mortality 37 fatal 11 fatal
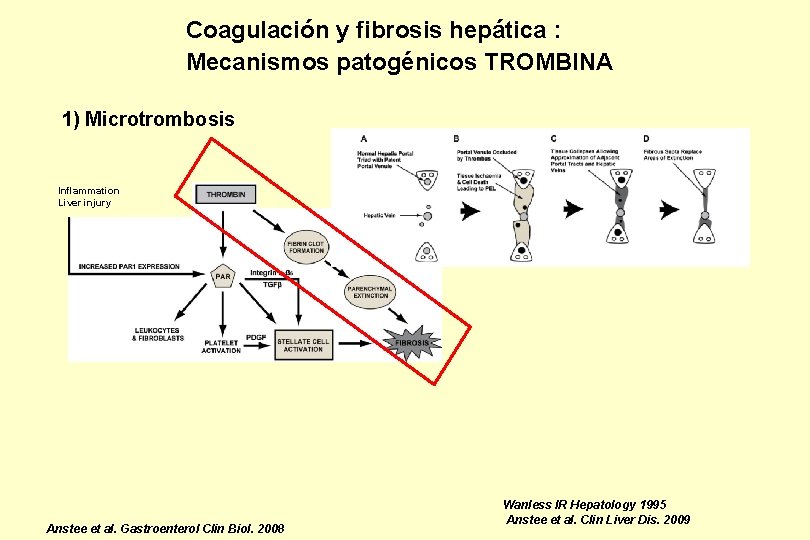
Coagulación y fibrosis hepática : Mecanismos patogénicos TROMBINA 1) Microtrombosis Inflammation Liver injury Anstee et al. Gastroenterol Clin Biol. 2008 Wanless IR Hepatology 1995 Anstee et al. Clin Liver Dis. 2009
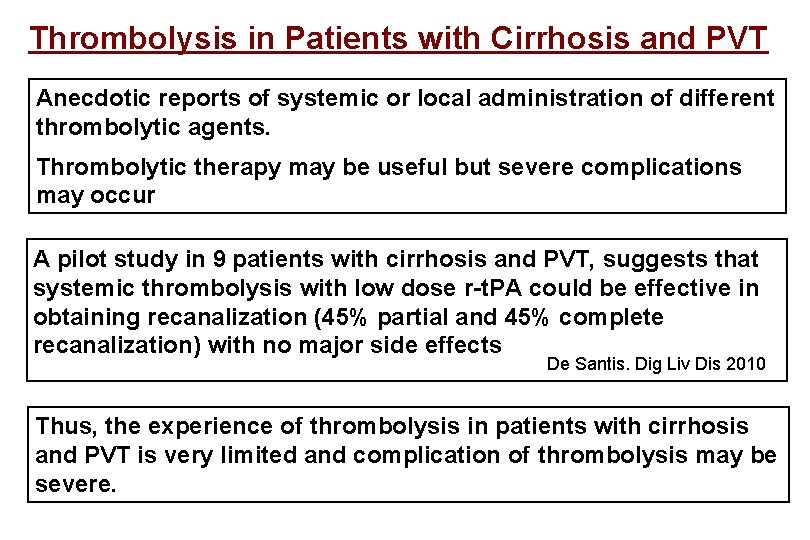
Thrombolysis in Patients with Cirrhosis and PVT Anecdotic reports of systemic or local administration of different thrombolytic agents. Thrombolytic therapy may be useful but severe complications may occur A pilot study in 9 patients with cirrhosis and PVT, suggests that systemic thrombolysis with low dose r-t. PA could be effective in obtaining recanalization (45% partial and 45% complete recanalization) with no major side effects De Santis. Dig Liv Dis 2010 Thus, the experience of thrombolysis in patients with cirrhosis and PVT is very limited and complication of thrombolysis may be severe.
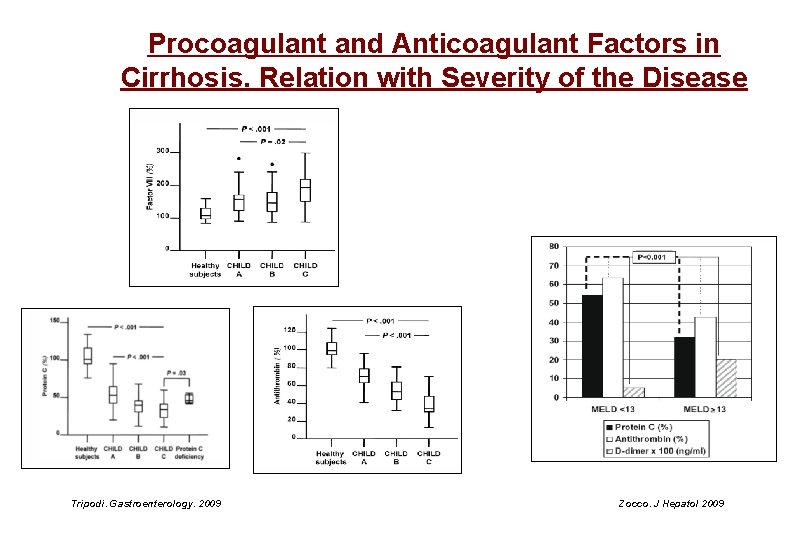
Procoagulant and Anticoagulant Factors in Cirrhosis. Relation with Severity of the Disease Tripodi. Gastroenterology. 2009 Zocco. J Hepatol 2009
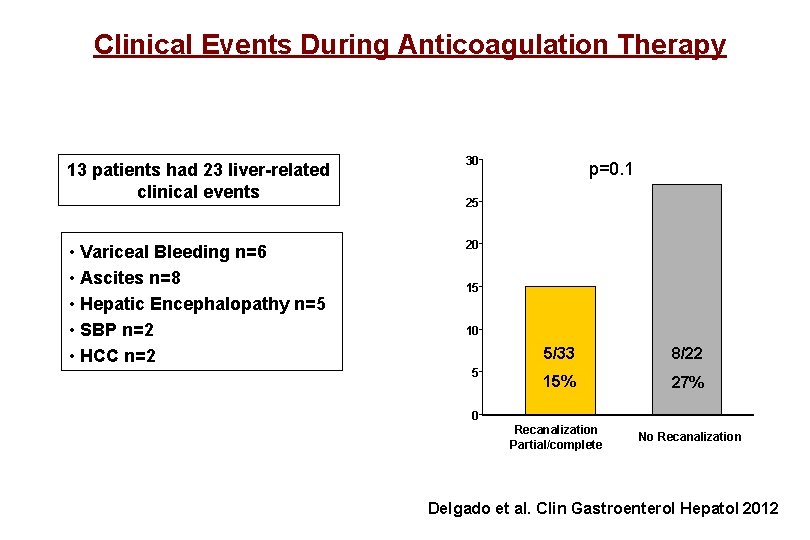
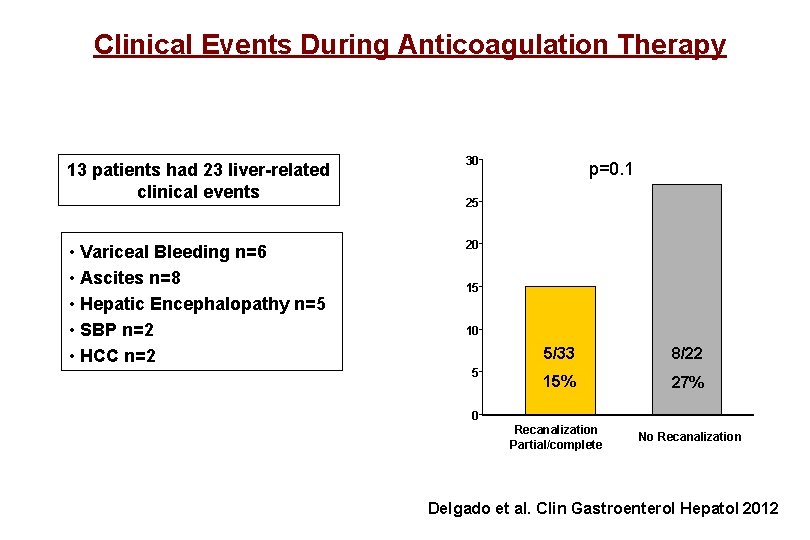
Clinical Events During Anticoagulation Therapy 13 patients had 23 liver-related clinical events 30 • Variceal Bleeding n=6 • Ascites n=8 • Hepatic Encephalopathy n=5 • SBP n=2 • HCC n=2 20 p=0. 1 25 15 10 5 5/33 8/22 15% 27% Recanalization Partial/complete No Recanalization 0 Delgado et al. Clin Gastroenterol Hepatol 2012
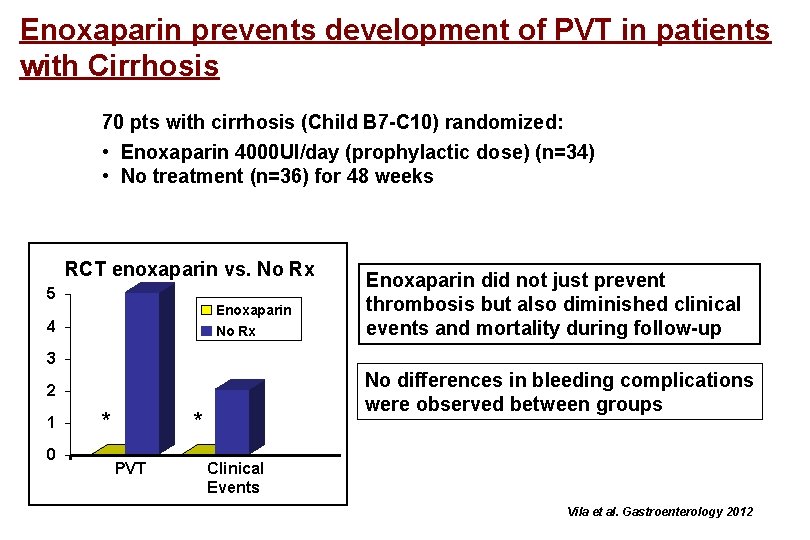
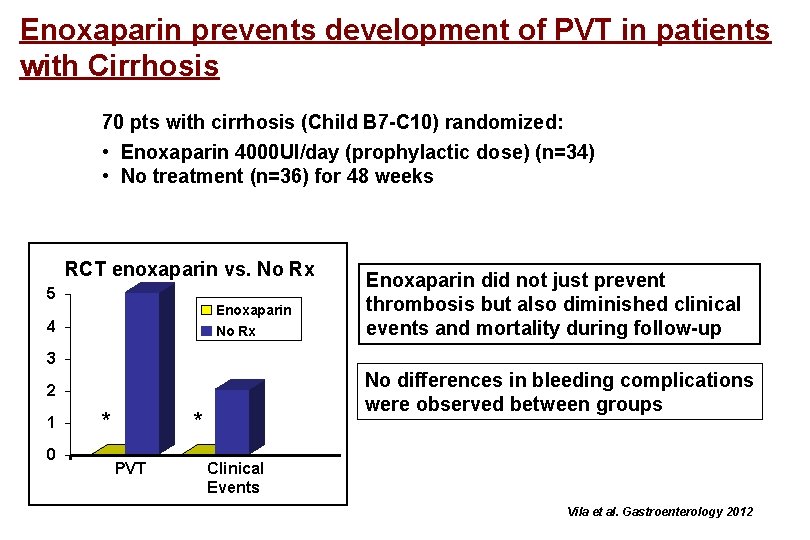
Enoxaparin prevents development of PVT in patients with Cirrhosis 70 pts with cirrhosis (Child B 7 -C 10) randomized: • Enoxaparin 4000 UI/day (prophylactic dose) (n=34) • No treatment (n=36) for 48 weeks RCT enoxaparin vs. No Rx 5 Enoxaparin No Rx 4 Enoxaparin did not just prevent thrombosis but also diminished clinical events and mortality during follow-up 3 No differences in bleeding complications were observed between groups 2 1 0 * * PVT Clinical Events Vila et al. Gastroenterology 2012
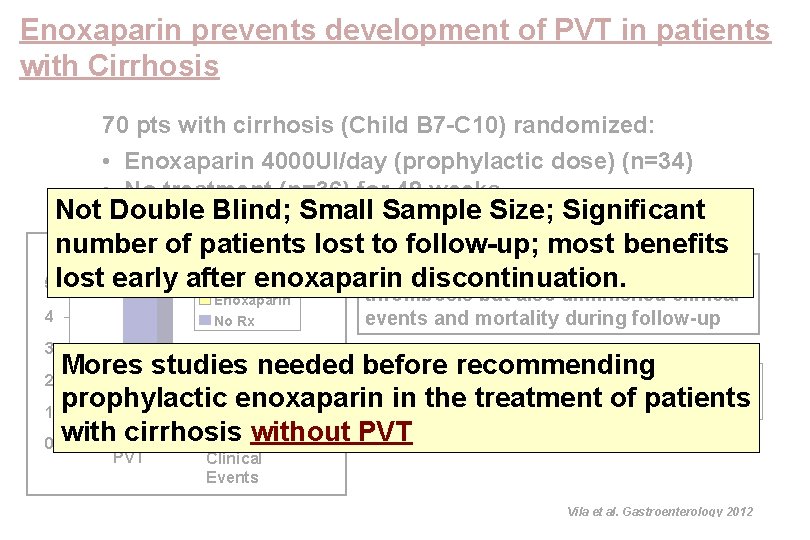
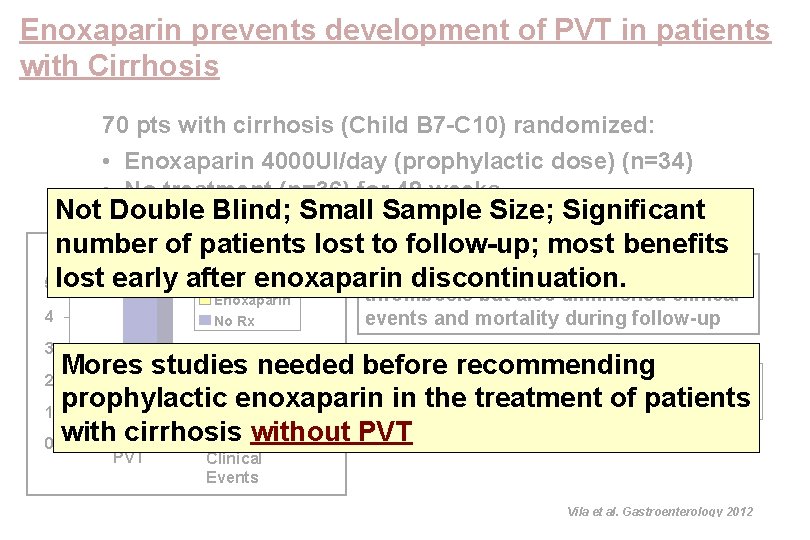
Enoxaparin prevents development of PVT in patients with Cirrhosis 70 pts with cirrhosis (Child B 7 -C 10) randomized: • Enoxaparin 4000 UI/day (prophylactic dose) (n=34) • No treatment (n=36) for 48 weeks Not Double Blind; Small Sample Size; Significant number of patients lost to follow-up; most benefits RCT enoxaparin vs. No Rx Enoxaparin did not just prevent 5 lost early after enoxaparin discontinuation. Enoxaparin No Rx 4 thrombosis but also diminished clinical events and mortality during follow-up 3 Mores studies needed before recommending No differences in bleeding complications prophylactic enoxaparin inobserved the treatment of patients were between groups * * 1 0 with cirrhosis without PVT 2 PVT Clinical Events Vila et al. Gastroenterology 2012
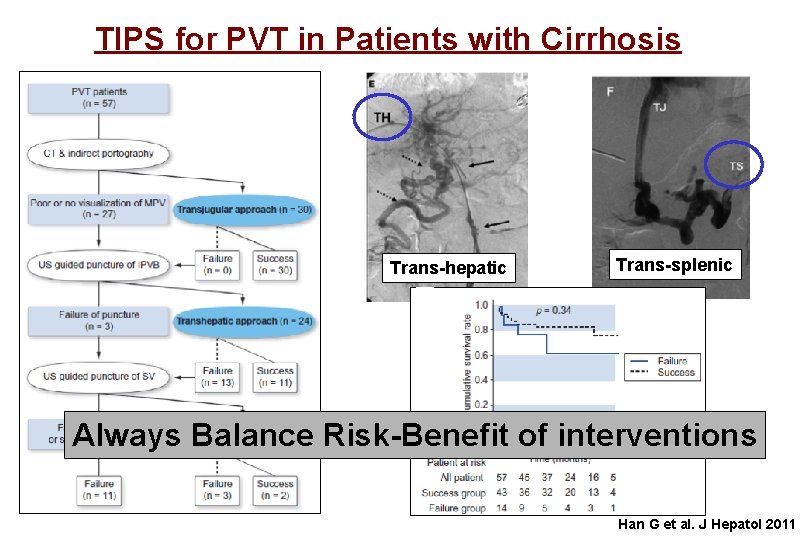
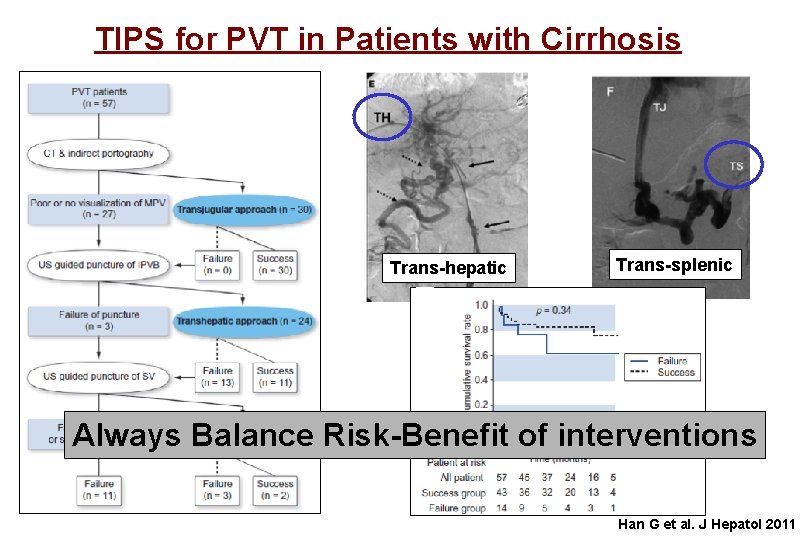
TIPS for PVT in Patients with Cirrhosis Trans-hepatic Trans-splenic Always Balance Risk-Benefit of interventions Han G et al. J Hepatol 2011
PVT in Cirrhosis Points to take into consideration • The natural history of PVT in cirrhosis (rate of progression, stability or possible regression, impact on the course of the disease) as well as the clinical impact of achieving recanalization is poorly known. • PVT could increase morbidity and mortality associated with OLT and it may even contraindicate it, especially if the thrombus extends to the splenic-SMV junction • Optimal Management unknown
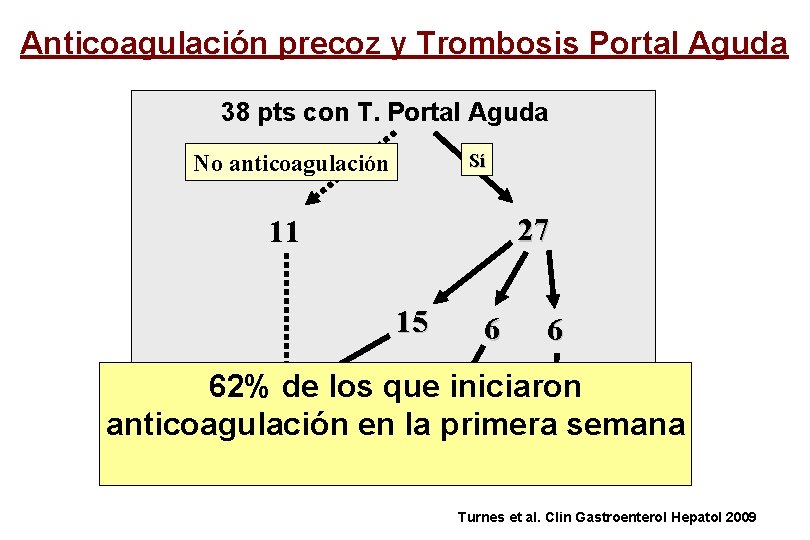
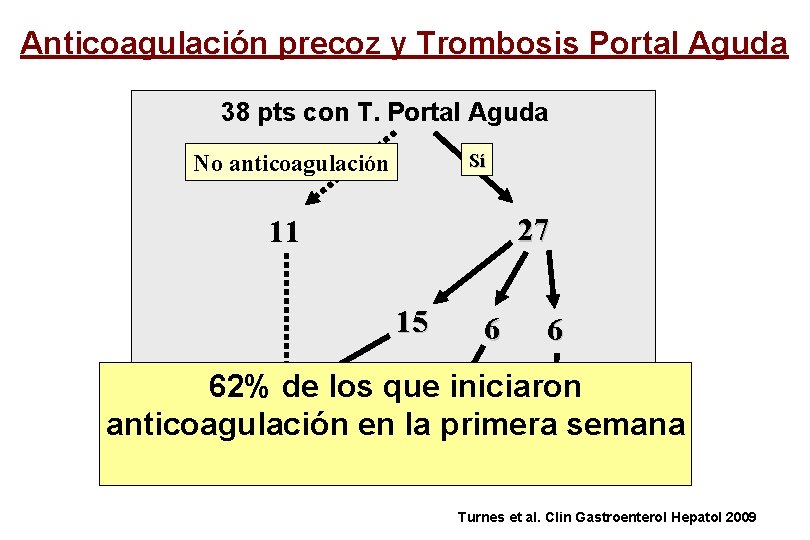
Anticoagulación precoz y Trombosis Portal Aguda 38 pts con T. Portal Aguda Sí No anticoagulación 27 11 15 6 6 62% de los que iniciaron No repermeab. en. Parcial Completa anticoagulación la primera semana (23% of Rx) Turnes et al. Clin Gastroenterol Hepatol 2009
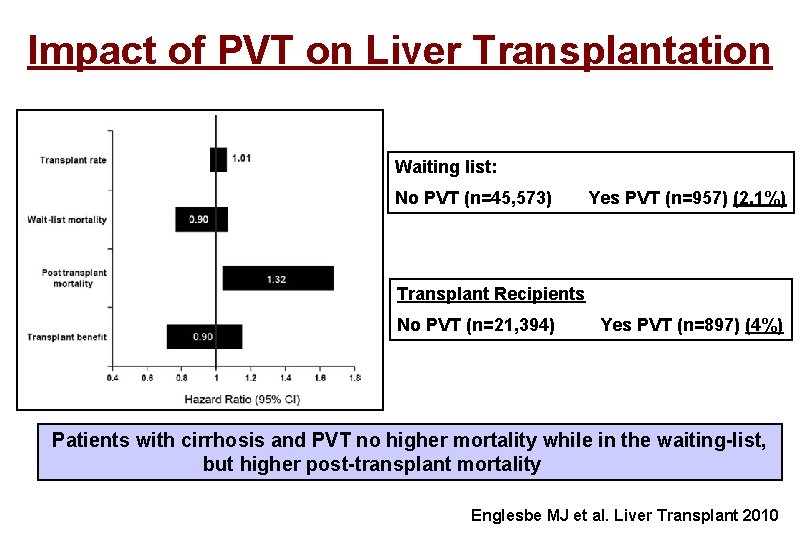
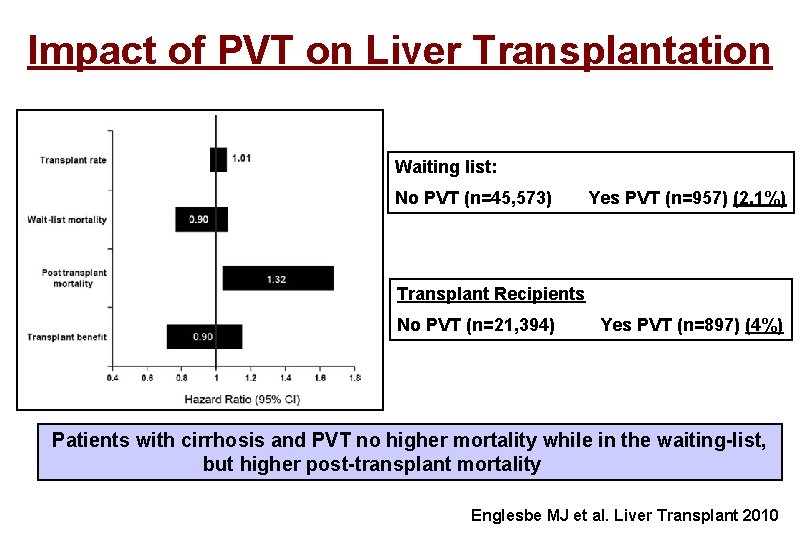
Impact of PVT on Liver Transplantation Waiting list: No PVT (n=45, 573) Yes PVT (n=957) (2, 1%) Transplant Recipients No PVT (n=21, 394) Yes PVT (n=897) (4%) Patients with cirrhosis and PVT no higher mortality while in the waiting-list, but higher post-transplant mortality Englesbe MJ et al. Liver Transplant 2010