Antiallergic drugs Lector prof Posokhova K A Types





- Slides: 31
Antiallergic drugs Lector prof. Posokhova K. A.
Types of allergic reactions (according to Gell and Cumbs): 1. I type reactions (anaphylactic) 2. II type reaction (humoral cytotoxic immune reactions) 3 III type reactions 4. IV type reactions 5. V type reactions (autosensibilization)
Classification of allergic reactions in clinic: 1. reactions of immediate type (I, III, V types after Cumbs) 2. reactions of delayed type (IV type after Cumbs)
General principles of prevention and treatment of allergic reactions 1) Avoiding contact with the allergen 2) Performing specific desensitization by repeated introduction of small doses of specific antigen 3) Performing nonspecific desensitization through administration of drugs which depress immune reactions (immune depressants) 4) Using antiallergic drugs which are able to prevent releasing the mediators of allergic reaction through stabilization of mast sells’ membranes or to block receptors with which these mediators interact in tissues 5) Symptomatic treatment of allergic reactions manifestations which have already developed
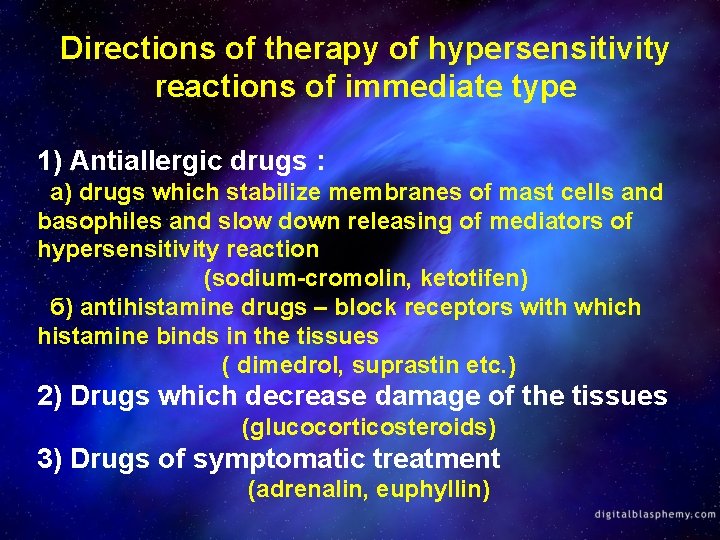
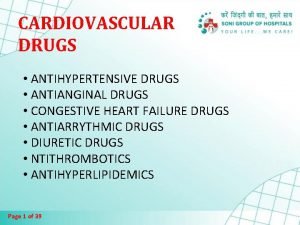
Directions of therapy of hypersensitivity reactions of immediate type 1) Antiallergic drugs : а) drugs which stabilize membranes of mast cells and basophiles and slow down releasing of mediators of hypersensitivity reaction (sodium-cromolin, ketotifen) б) antihistamine drugs – block receptors with which histamine binds in the tissues ( dimedrol, suprastin etc. ) 2) Drugs which decrease damage of the tissues (glucocorticosteroids) 3) Drugs of symptomatic treatment (adrenalin, euphyllin)
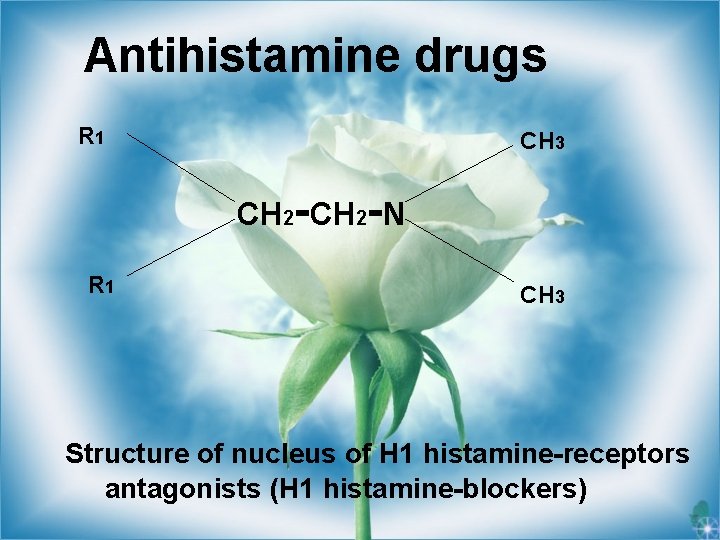
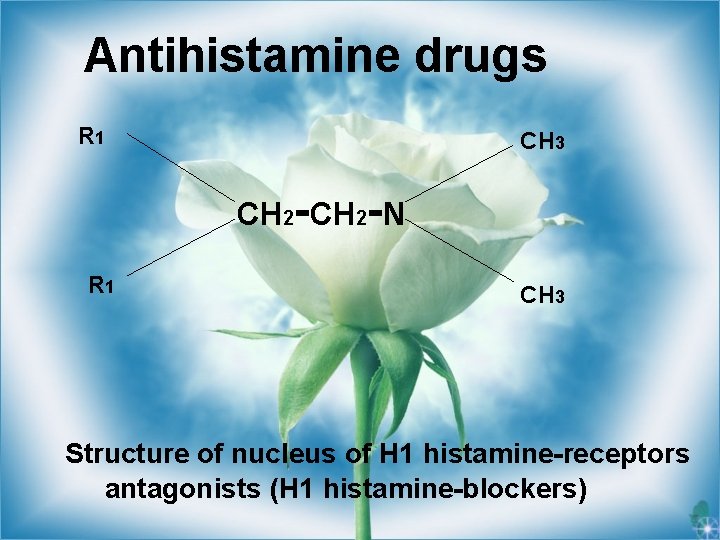
Antihistamine drugs R 1 CH 3 CH 2 -N R 1 CH 3 Structure of nucleus of Н 1 histamine-receptors antagonists (H 1 histamine-blockers)
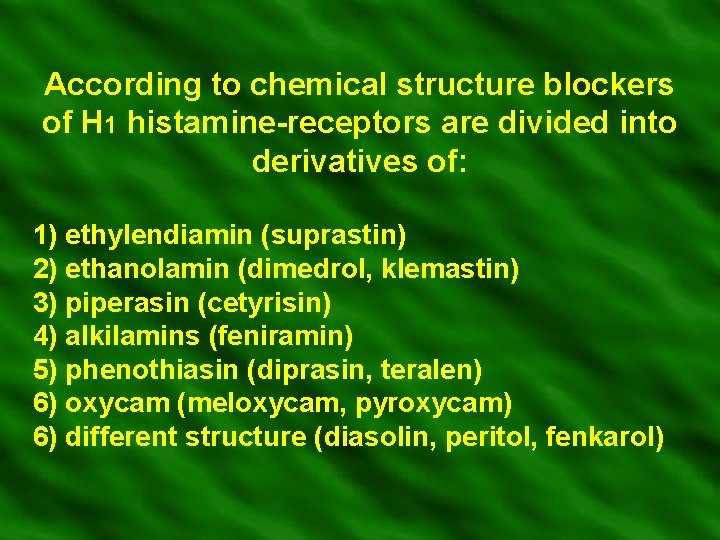
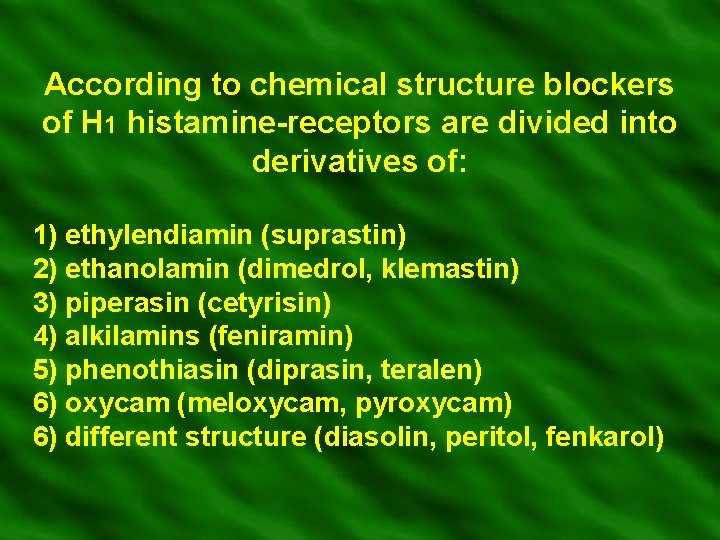
According to chemical structure blockers of Н 1 histamine-receptors are divided into derivatives of: 1) ethylendiamin (suprastin) 2) ethanolamin (dimedrol, klemastin) 3) piperasin (cetyrisin) 4) alkilamins (feniramin) 5) phenothiasin (diprasin, teralen) 6) oxycam (meloxycam, pyroxycam) 6) different structure (diasolin, peritol, fenkarol)
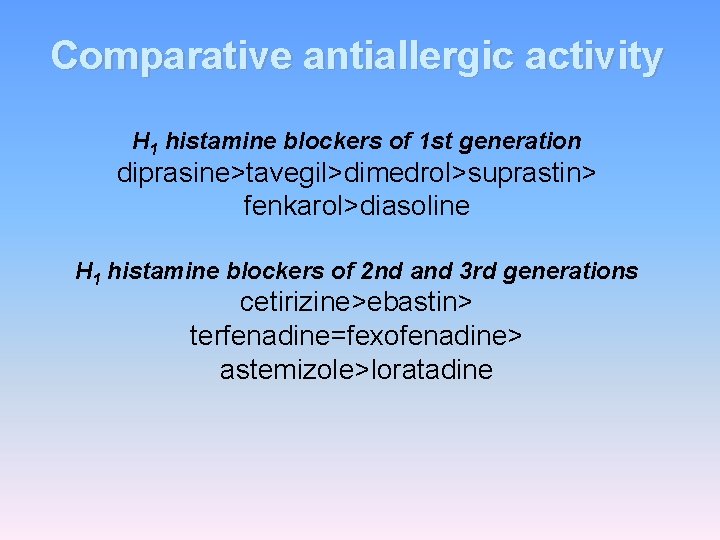
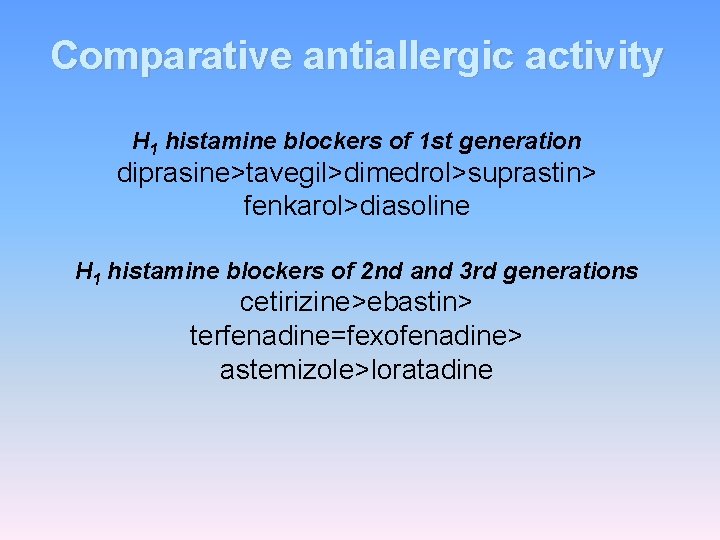
Comparative antiallergic activity Н 1 histamine blockers of 1 st generation diprasine>tavegil>dimedrol>suprastin> fenkarol>diasoline Н 1 histamine blockers of 2 nd and 3 rd generations cetirizine>ebastin> terfenadine=fexofenadine> astemizole>loratadine

Indications for administration of antihistamine drugs: 1. Nettle-rash 2. Hay fever 3. Vasomotor rhinitis 4. Contact dermatitis 5. Angionevrotic edema 6. Serum diseases 7. Anaphylactic shock 8. Others
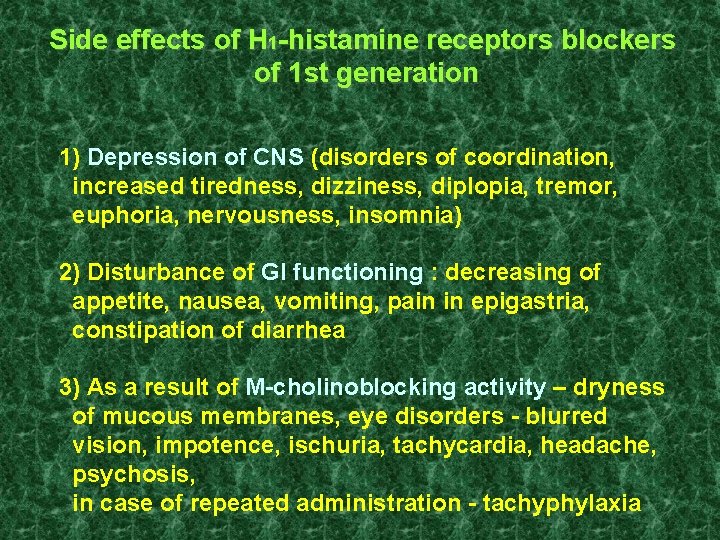
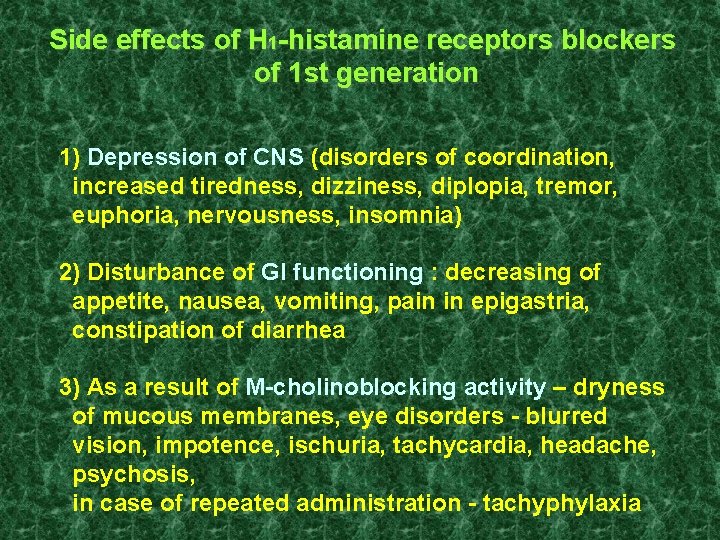
Side effects of Н 1 -histamine receptors blockers of 1 st generation 1) Depression of CNS (disorders of coordination, increased tiredness, dizziness, diplopia, tremor, euphoria, nervousness, insomnia) 2) Disturbance of GI functioning : decreasing of appetite, nausea, vomiting, pain in epigastria, constipation of diarrhea 3) As a result of M-cholinoblocking activity – dryness of mucous membranes, eye disorders - blurred vision, impotence, ischuria, tachycardia, headache, psychosis, in case of repeated administration - tachyphylaxia
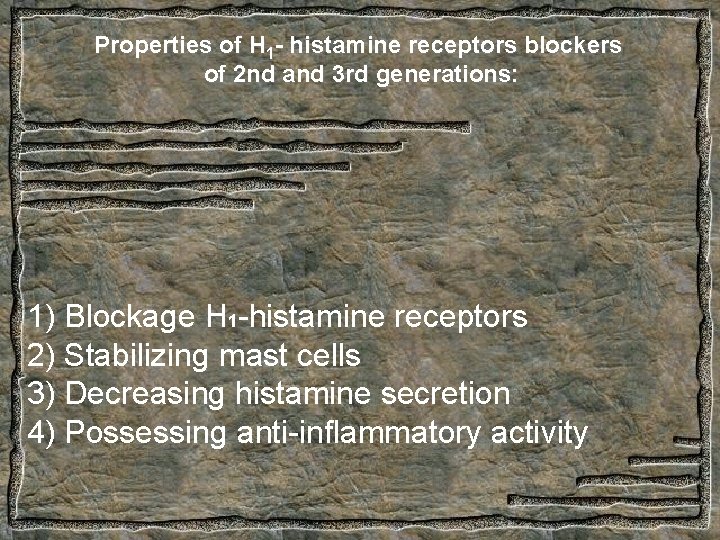
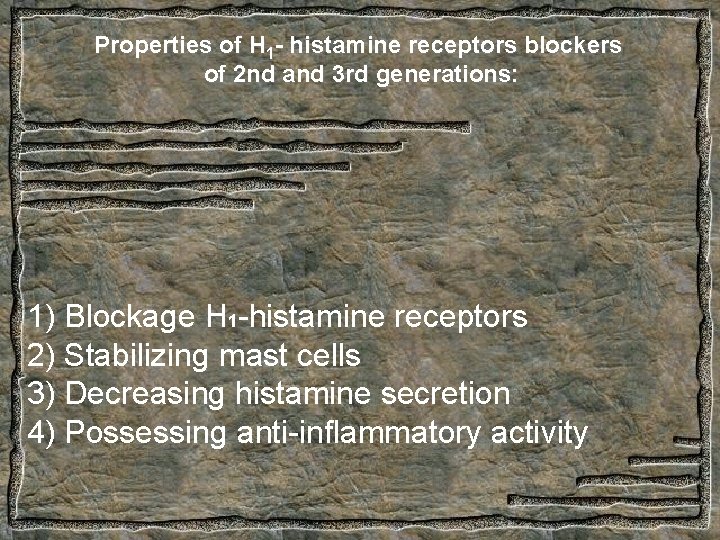
Properties of Н 1 - histamine receptors blockers of 2 nd and 3 rd generations: 1) Blockage Н 1 -histamine receptors 2) Stabilizing mast cells 3) Decreasing histamine secretion 4) Possessing anti-inflammatory activity
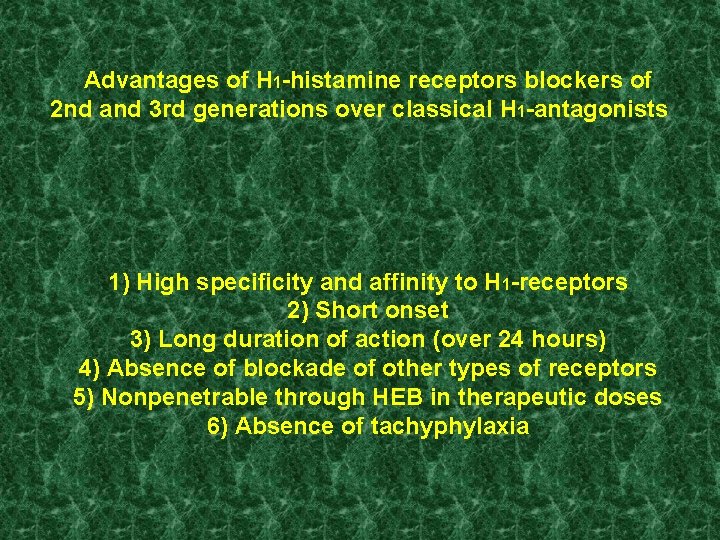
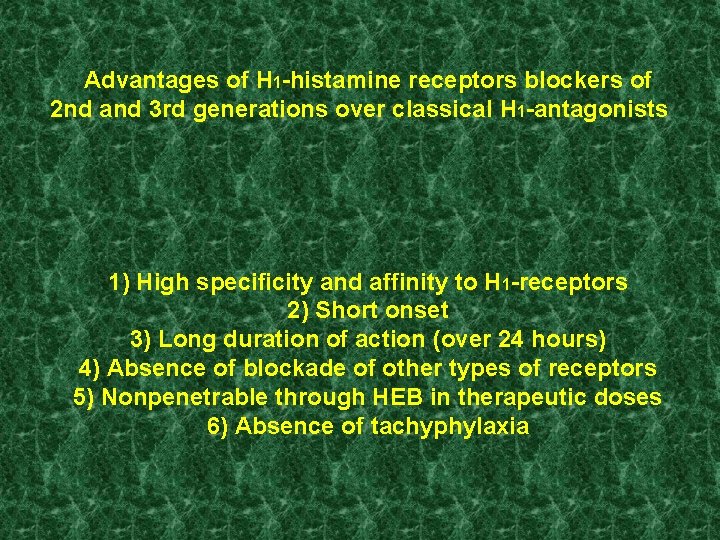
Advantages of Н 1 -histamine receptors blockers of 2 nd and 3 rd generations over classical Н 1 -antagonists 1) High specificity and affinity to Н 1 -receptors 2) Short onset 3) Long duration of action (over 24 hours) 4) Absence of blockade of other types of receptors 5) Nonpenetrable through HEB in therapeutic doses 6) Absence of tachyphylaxia

Anti-inflammatory drugs
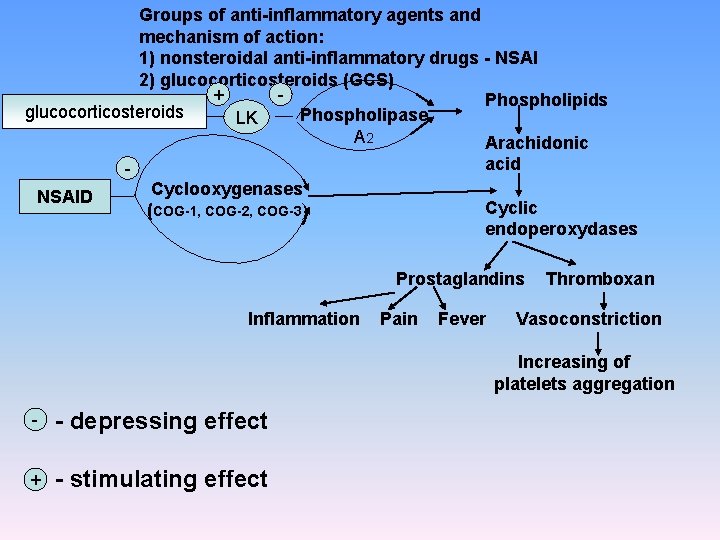
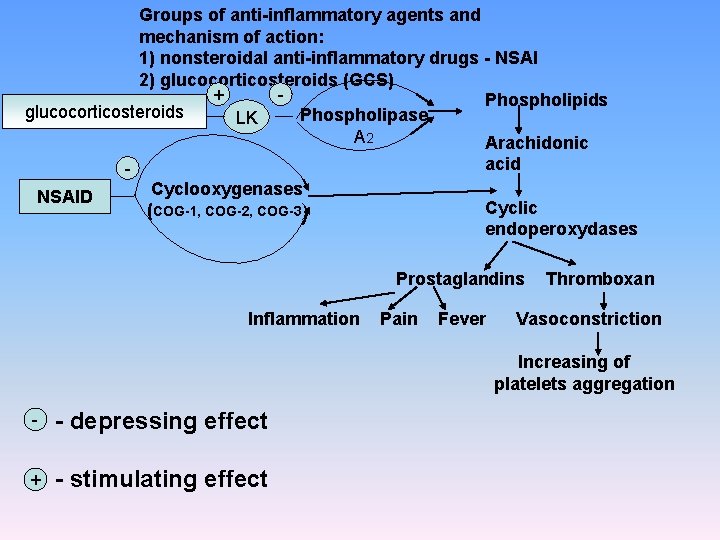
Groups of anti-inflammatory agents and mechanism of action: 1) nonsteroidal anti-inflammatory drugs - NSAI 2) glucocorticosteroids (GCS) + Phospholipids glucocorticosteroids Phospholipase LK А 2 Arachidonic NSAID acid Cyclooxygenases (COG-1, COG-2, COG-3) Cyclic endoperoxydases Prostaglandins Inflammation Pain Fever Thromboxan Vasoconstriction Increasing of platelets aggregation - - depressing effect + - stimulating effect
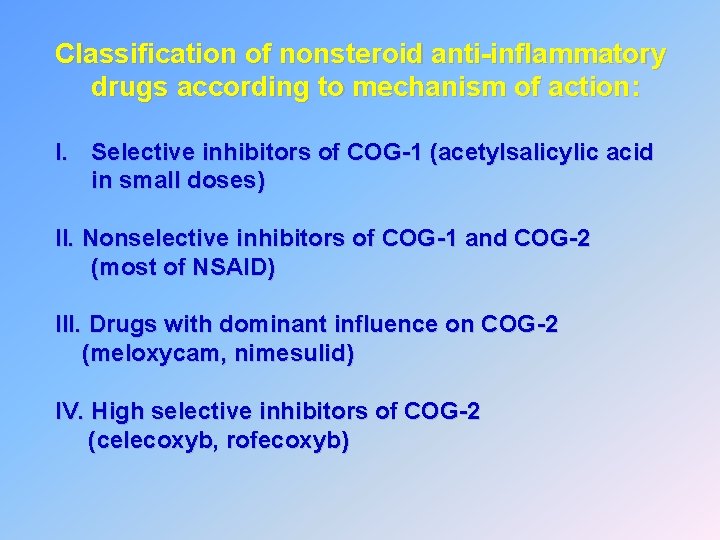
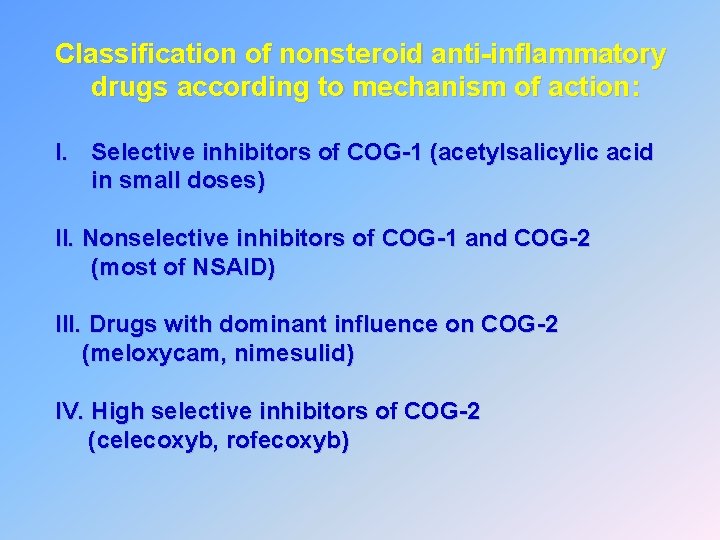
Classification of nonsteroid anti-inflammatory drugs according to mechanism of action: I. Selective inhibitors of COG-1 (acetylsalicylic acid in small doses) II. Nonselective inhibitors of COG-1 and COG-2 (most of NSAID) III. Drugs with dominant influence on COG-2 (meloxycam, nimesulid) IV. High selective inhibitors of COG-2 (celecoxyb, rofecoxyb)
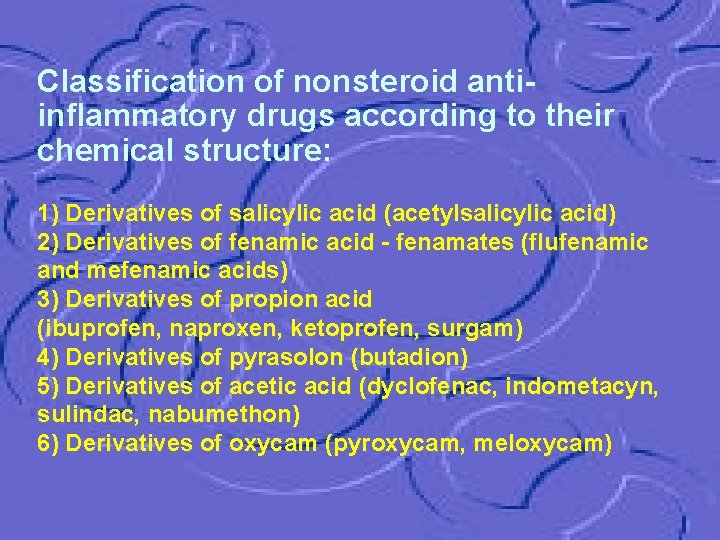
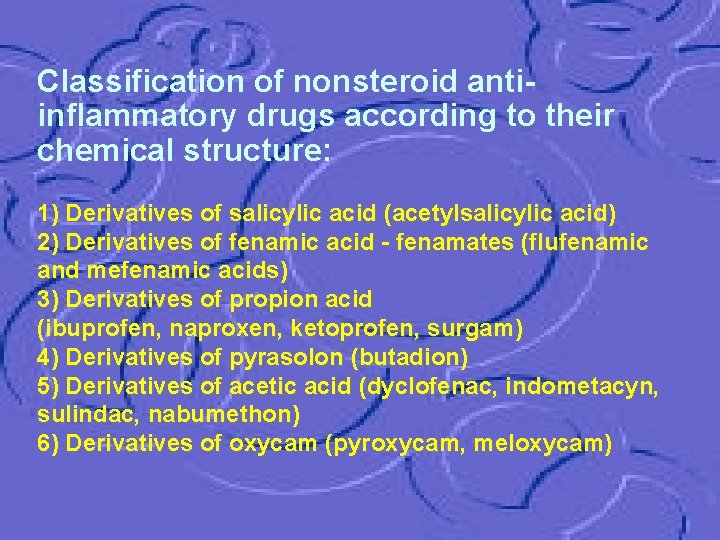
Classification of nonsteroid antiinflammatory drugs according to their chemical structure: 1) Derivatives of salicylic acid (acetylsalicylic acid) 2) Derivatives of fenamic acid - fenamates (flufenamic and mefenamic acids) 3) Derivatives of propion acid (ibuprofen, naproxen, ketoprofen, surgam) 4) Derivatives of pyrasolon (butadion) 5) Derivatives of acetic acid (dyclofenac, indometacyn, sulindac, nabumethon) 6) Derivatives of oxycam (pyroxycam, meloxycam)
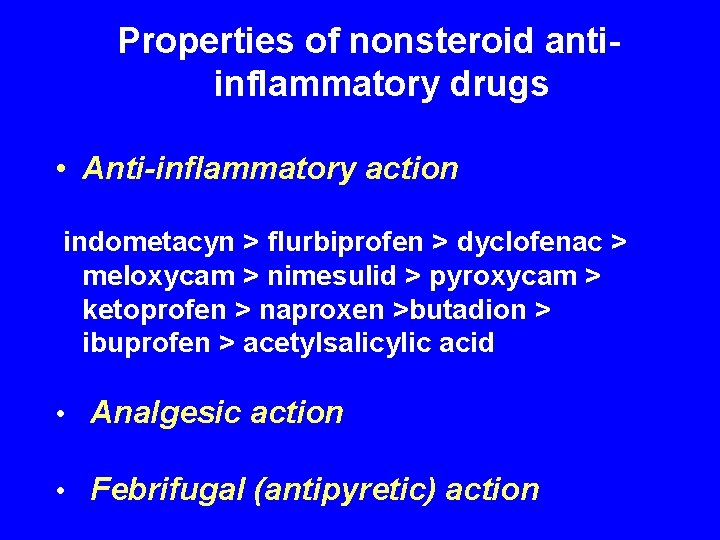
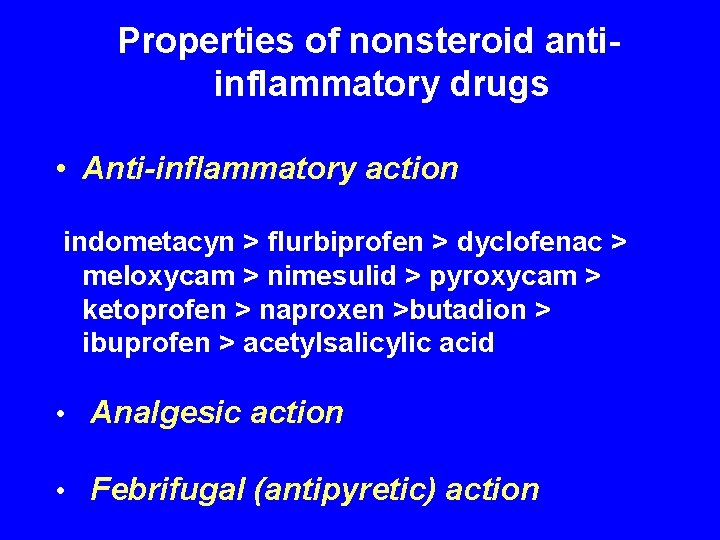
Properties of nonsteroid antiinflammatory drugs • Anti-inflammatory action indometacyn > flurbiprofen > dyclofenac > meloxycam > nimesulid > pyroxycam > ketoprofen > naproxen >butadion > ibuprofen > acetylsalicylic acid • Analgesic action • Febrifugal (antipyretic) action
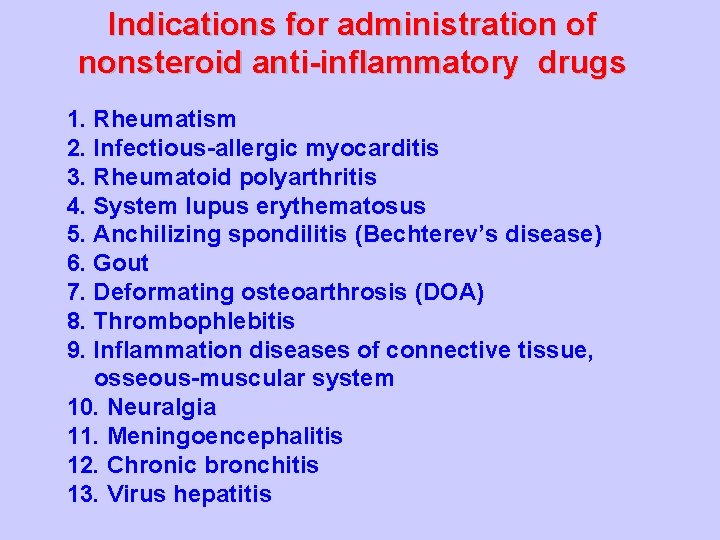
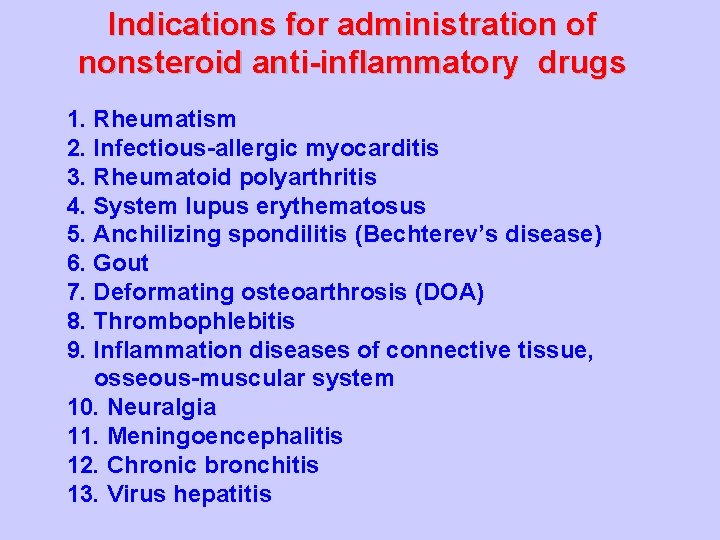
Indications for administration of nonsteroid anti-inflammatory drugs 1. Rheumatism 2. Infectious-allergic myocarditis 3. Rheumatoid polyarthritis 4. System lupus erythematosus 5. Anchilizing spondilitis (Bechterev’s disease) 6. Gout 7. Deformating osteoarthrosis (DOA) 8. Thrombophlebitis 9. Inflammation diseases of connective tissue, osseous-muscular system 10. Neuralgia 11. Meningoencephalitis 12. Chronic bronchitis 13. Virus hepatitis
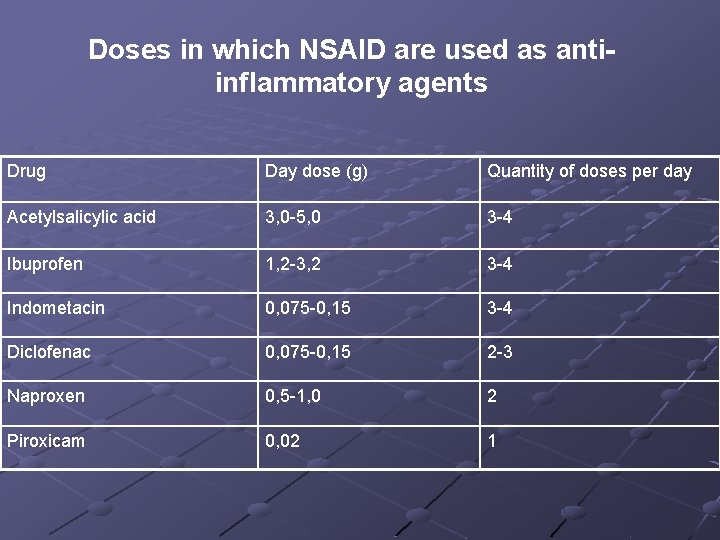
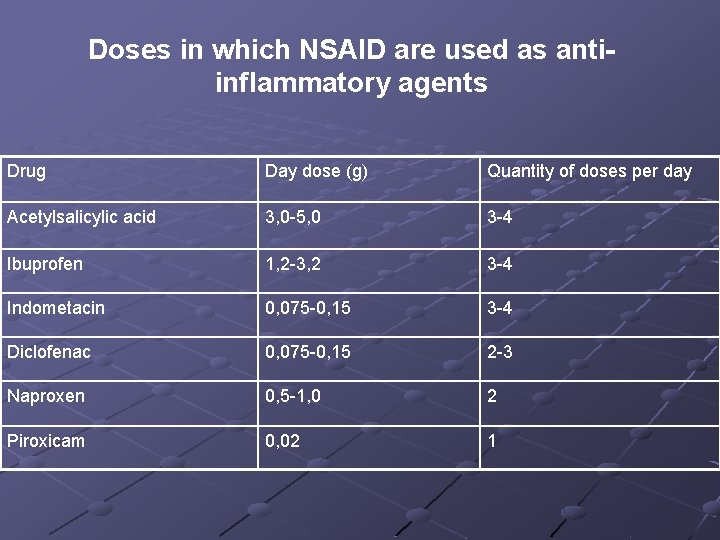
Doses in which NSAID are used as antiinflammatory agents Drug Day dose (g) Quantity of doses per day Acetylsalicylic acid 3, 0 -5, 0 3 -4 Ibuprofen 1, 2 -3, 2 3 -4 Indometacin 0, 075 -0, 15 3 -4 Diclofenac 0, 075 -0, 15 2 -3 Naproxen 0, 5 -1, 0 2 Piroxicam 0, 02 1
Acetylsalicylic acid
Aspirin С

Aspirin
Butadion

Indometacin (methyndol)
Ibuprofen (brufen)

Piroxicam
Sodium diclofenac
Voltaren
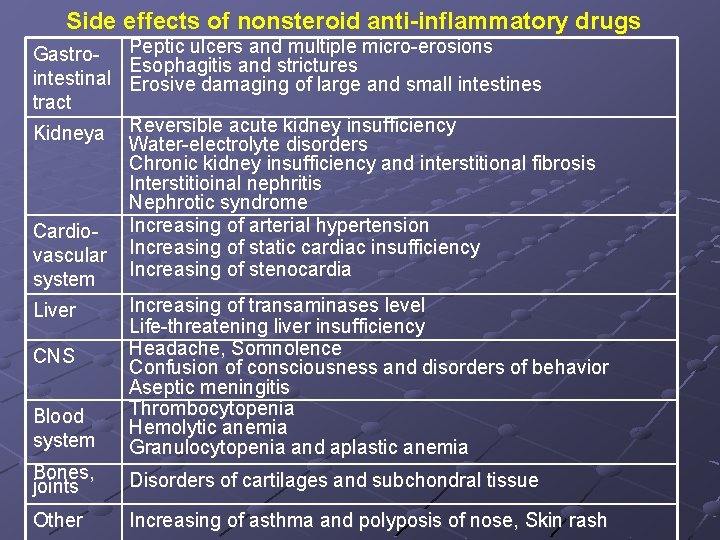
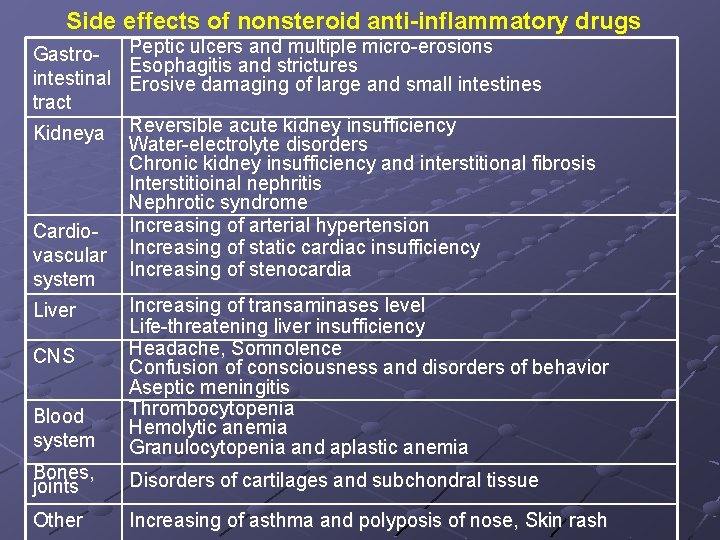
Side effects of nonsteroid anti-inflammatory drugs Gastrointestinal tract Peptic ulcers and multiple micro-erosions Esophagitis and strictures Erosive damaging of large and small intestines Kidneya Reversible acute kidney insufficiency Water-electrolyte disorders Chronic kidney insufficiency and interstitional fibrosis Interstitioinal nephritis Nephrotic syndrome Increasing of arterial hypertension Increasing of static cardiac insufficiency Increasing of stenocardia Cardiovascular system Blood system Increasing of transaminases level Life-threatening liver insufficiency Headache, Somnolence Confusion of consciousness and disorders of behavior Aseptic meningitis Thrombocytopenia Hemolytic anemia Granulocytopenia and aplastic anemia Bones, joints Disorders of cartilages and subchondral tissue Other Increasing of asthma and polyposis of nose, Skin rash Liver CNS
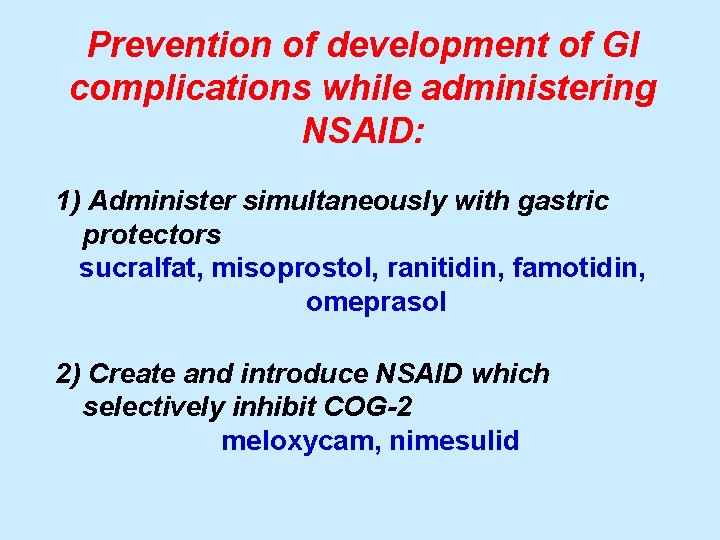
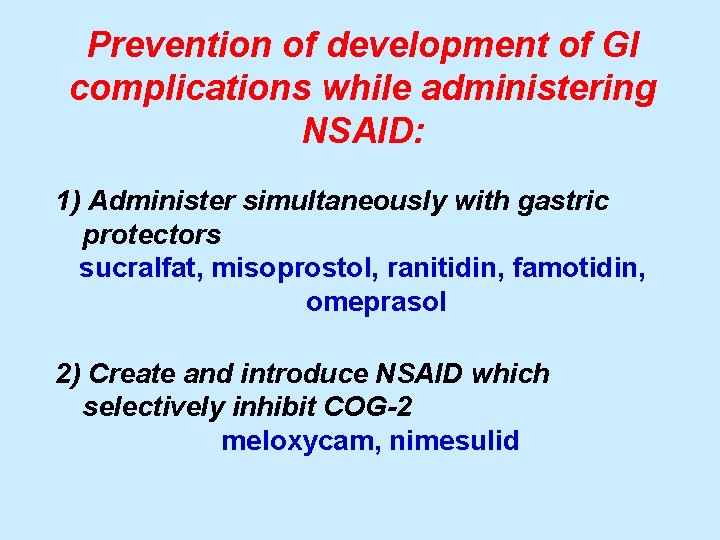
Prevention of development of GI complications while administering NSAID: 1) Administer simultaneously with gastric protectors sucralfat, misoprostol, ranitidin, famotidin, omeprasol 2) Create and introduce NSAID which selectively inhibit COG-2 meloxycam, nimesulid
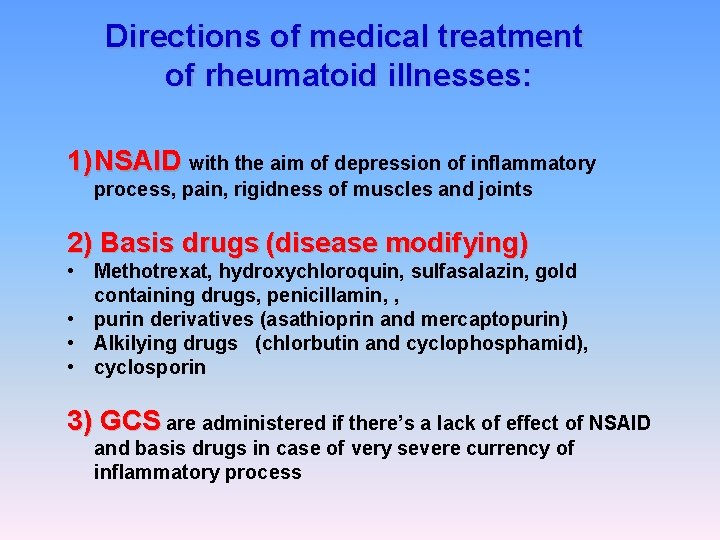
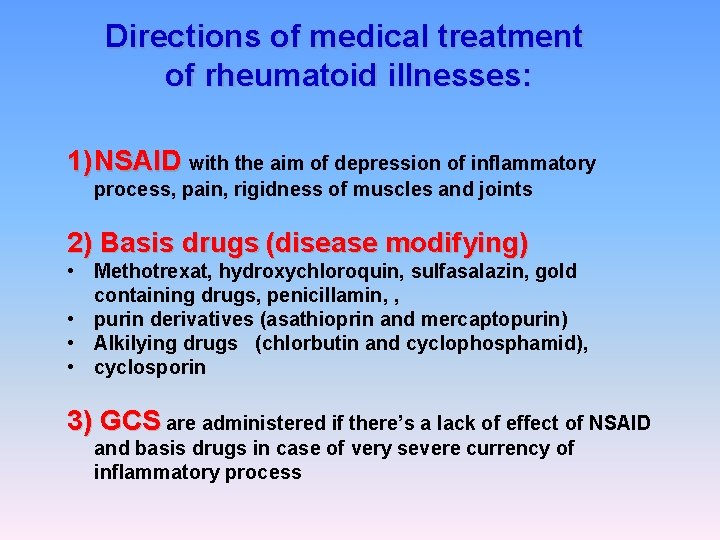
Directions of medical treatment of rheumatoid illnesses: 1) NSAID with the aim of depression of inflammatory process, pain, rigidness of muscles and joints 2) Basis drugs (disease modifying) • Methotrexat, hydroxychloroquin, sulfasalazin, gold containing drugs, penicillamin, , • purin derivatives (asathioprin and mercaptopurin) • Alkilying drugs (chlorbutin and cyclophosphamid), • cyclosporin 3) GCS are administered if there’s a lack of effect of NSAID and basis drugs in case of very severe currency of inflammatory process
 Lecturas para evaluar dominio lector
Lecturas para evaluar dominio lector Objetivos de un lector
Objetivos de un lector Intentio autoris
Intentio autoris Estructura no rígida en literatura
Estructura no rígida en literatura Que es el mlo
Que es el mlo Texte demi lune lector lectrix
Texte demi lune lector lectrix Lector de tarjetas
Lector de tarjetas Quehaceres del lector
Quehaceres del lector Proceso unificado de desarrollo de software ejemplo
Proceso unificado de desarrollo de software ejemplo Lector lectrix l'homme à l'oreille coupée
Lector lectrix l'homme à l'oreille coupée Conclusiones del plan lector
Conclusiones del plan lector Dominio
Dominio Aqu agregat
Aqu agregat Simicole
Simicole Dominio lector
Dominio lector Que es plan lector
Que es plan lector Lector vs lecturer
Lector vs lecturer Mechanism of action of antifungal drugs
Mechanism of action of antifungal drugs Types of drugs
Types of drugs Types of drugs
Types of drugs Deliberate adulteration definition
Deliberate adulteration definition Drug basket system
Drug basket system Types of drugs
Types of drugs Drug and alcohol jeopardy
Drug and alcohol jeopardy Schedule 1 drugs
Schedule 1 drugs Liothyronine
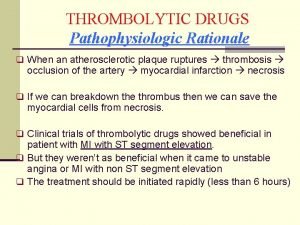
Liothyronine Thrombolytic drugs
Thrombolytic drugs Time goal for fibrinolytic checklist
Time goal for fibrinolytic checklist Thrombolytic drugs
Thrombolytic drugs Thrombolytic drugs mechanism of action
Thrombolytic drugs mechanism of action Mechanism of action of thrombolytic agents
Mechanism of action of thrombolytic agents British model involved with drugs
British model involved with drugs