A CostEffectiveness Analysis of Alternative Human papillomavirus HPV
- Slides: 33
A Cost-Effectiveness Analysis of Alternative Human papillomavirus (HPV) Vaccination Strategies Elamin H. Elbasha Merck Research Laboratories, USA
Presentation outline HPV infection and disease HPV vaccines Merck model Public health impact Economic impact Summary and conclusions 2
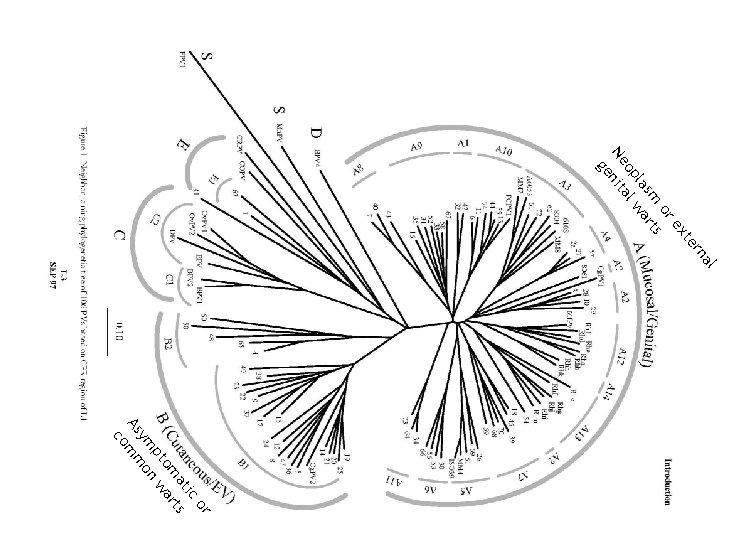
HPV infection HPV is small, non-enveloped, encapsulated, double-stranded DNA virus HPV encodes two structural proteins L 1 codes for major capsid protein L 2 codes for minor capsid proteins Enormous HPV diversity More than 100 HPV genotypes More than 40 types infect ano-genital tract At least 13 high-risk types cause cervical cancer Ubiquitous Lifetime Risk of HPV infection up to 70% among sexually active Major risk factor for HPV acquisition: number of sexual partners 3
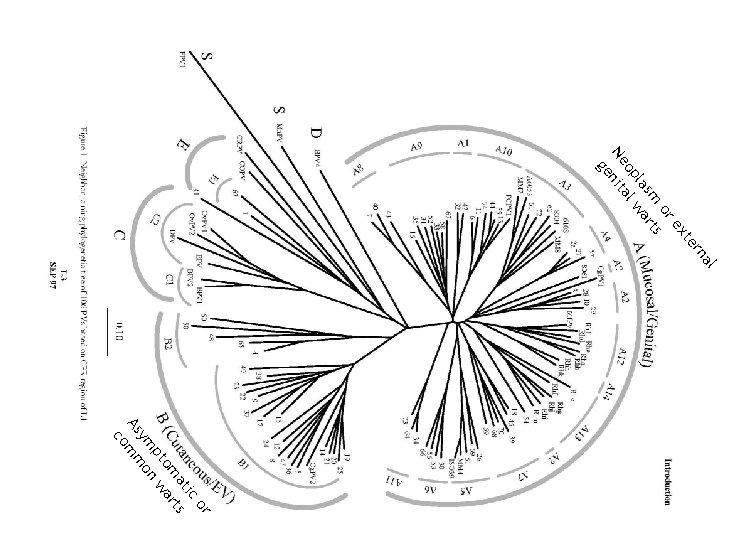
al rn te ex or s sm rt la wa op al Ne nit ge or ic at ts om ar pt n w ym o As mm co 4
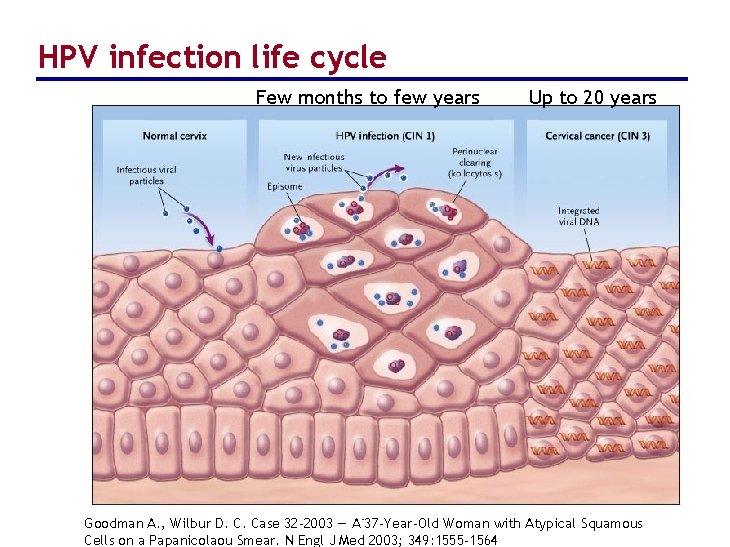
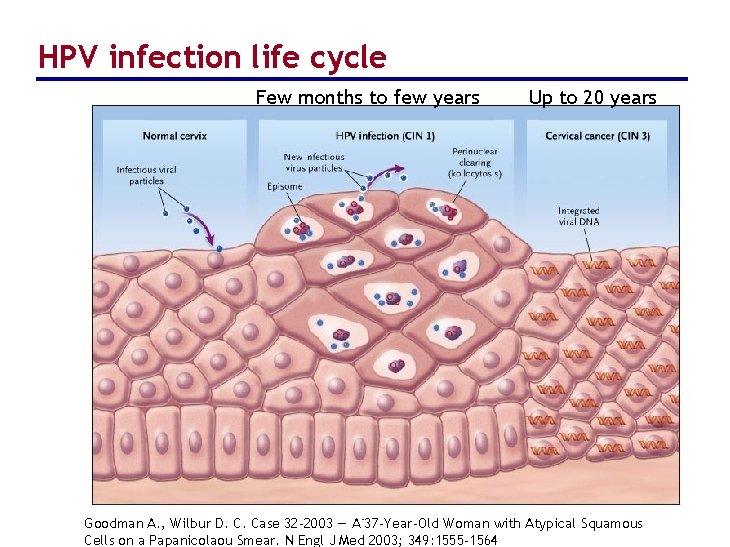
HPV infection life cycle Few months to few years 5 Up to 20 years Goodman A. , Wilbur D. C. Case 32 -2003 — A 37 -Year-Old Woman with Atypical Squamous Cells on a Papanicolaou Smear. N Engl J Med 2003; 349: 1555 -1564
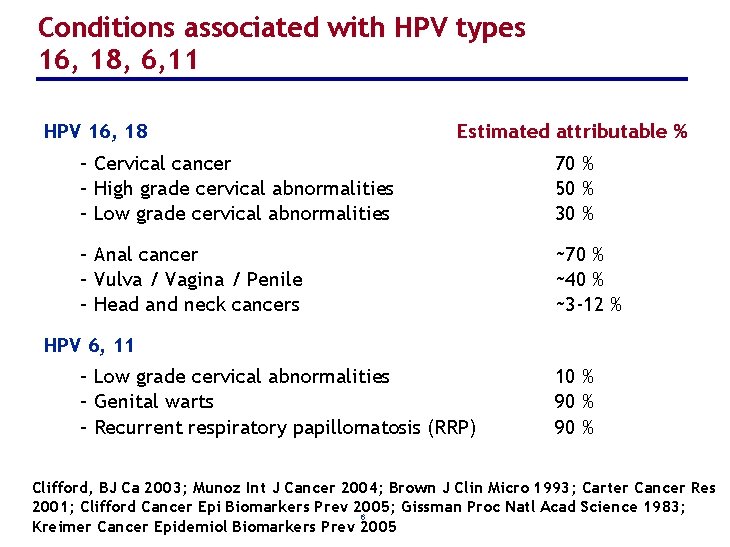
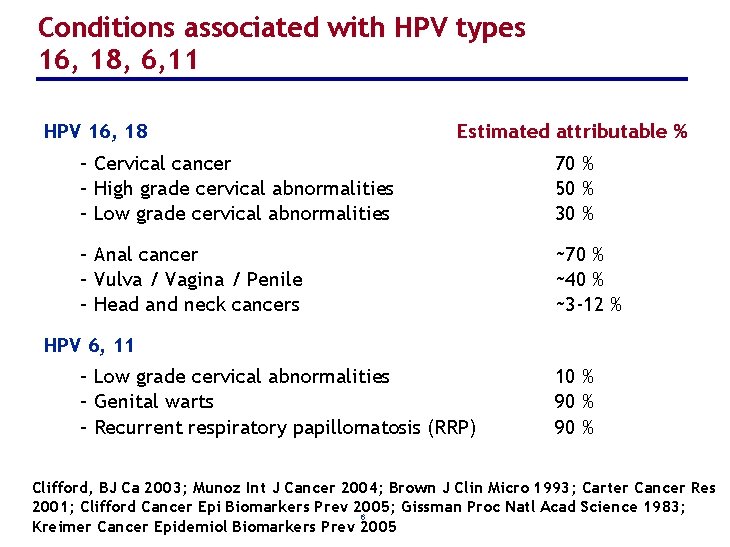
Conditions associated with HPV types 16, 18, 6, 11 HPV 16, 18 Estimated attributable % – Cervical cancer – High grade cervical abnormalities – Low grade cervical abnormalities 70 % 50 % 30 % – Anal cancer – Vulva / Vagina / Penile – Head and neck cancers ~70 % ~40 % ~3 -12 % HPV 6, 11 – Low grade cervical abnormalities – Genital warts – Recurrent respiratory papillomatosis (RRP) 10 % 90 % Clifford, BJ Ca 2003; Munoz Int J Cancer 2004; Brown J Clin Micro 1993; Carter Cancer Res 2001; Clifford Cancer Epi Biomarkers Prev 2005; Gissman Proc Natl Acad Science 1983; 6 Kreimer Cancer Epidemiol Biomarkers Prev 2005
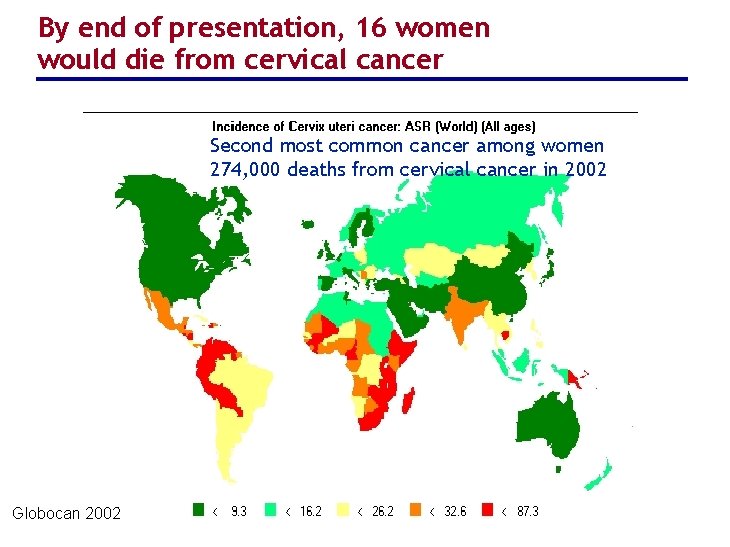
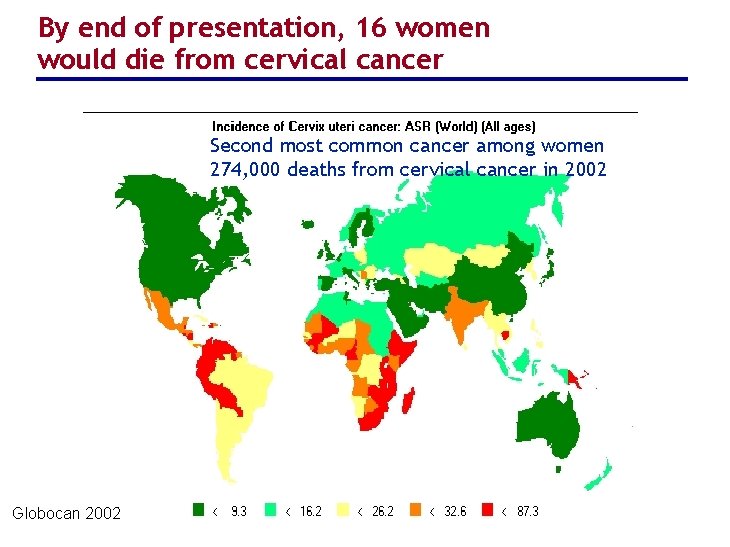
By end of presentation, 16 women would die from cervical cancer Second most common cancer among women 274, 000 deaths from cervical cancer in 2002 Globocan 2002 7
Immunologic Basis for HPV vaccines L 1 HPV major capsid protein self-assembles into empty virus-like particles (VLPs) In animal models of papillomavirus infection using species-specific VLPs Vaccination results in protection from infection and disease Efficacy associated with development of neutralizing antibodies Transfer of serum from vaccinated to unvaccinated animals transfers protective efficacy Protection is prophylactic, not likely to be therapeutic Protection is likely to be type-specific 8
HPV vaccines Prepared from virus-like particles (non-infectious) Produced by recombinant technology Do not contain any live biological product or DNA GARDASIL® [prophylactic quadrivalent HPV (6, 11, 16, 18) vaccine] licensed in U. S. & other countries First vaccine to prevent cervical cancer, precancerous genital lesions, and genital warts Series of three injections over a six-month period Safe and highly efficacious CERVARIX® [prophylactic bivalent HPV (16, 18) vaccine] in final stages of clinical testing 9
Research questions What are the epidemiologic consequences of HPV vaccination? What is the sensitivity of vaccine health impact (HPV, CIN, cervical cancer, genital warts) to: vaccine characteristics (e. g. , duration of protection)? vaccination strategies (females and males, females-only, catchup, etc. )? What is the cost-effectiveness of programs using a quadrivalent HPV (6/11/16/18) vaccine? 10
Methods Direct and indirect ‘herd immunity’ effects of vaccination Describe transmission of the virus and resulting disease in a population Assess impact of vaccine on vaccinees and their contacts An integrated disease transmission model and costutility analysis Demographic model Behavioral model HPV infection and disease models Economic model US healthcare system data and perspective Assumes existing screening practices 11
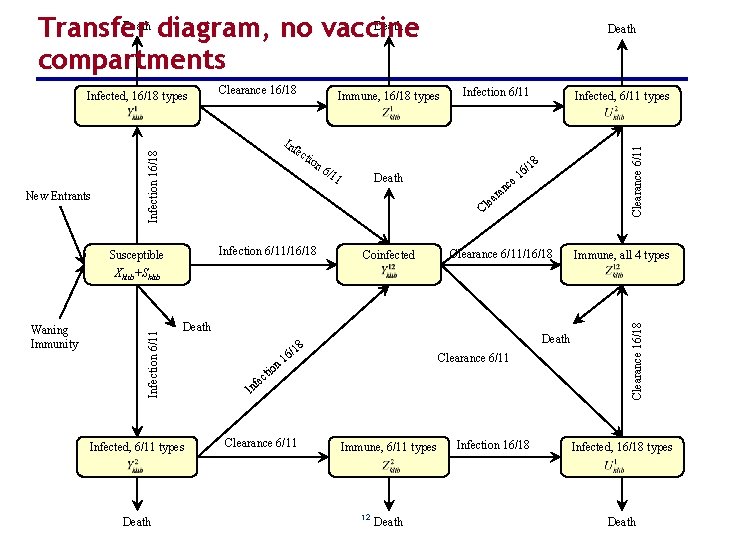
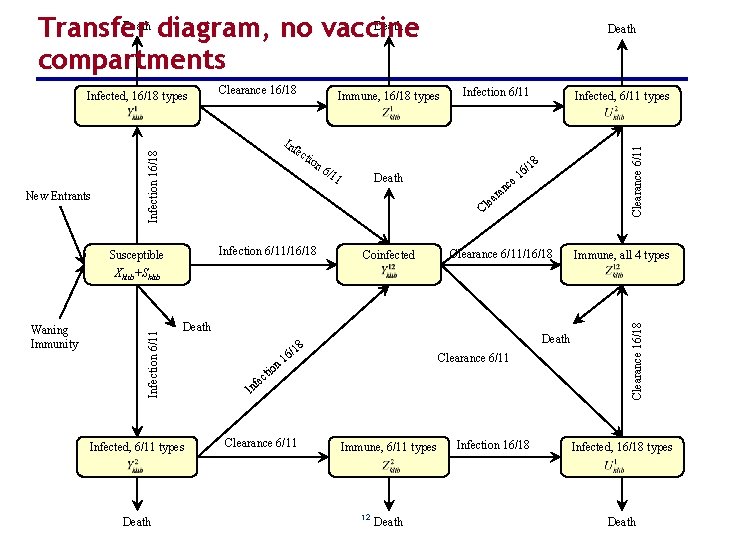
Death Transfer diagram, no vaccine compartments Immune, 16/18 types Inf ec Infection 16/18 New Entrants Clearance 16/18 tio n 6 /11 Infection 6/11 Infected, 6/11 types Clearance 6/11 Infected, 16/18 types Death 8 /1 Death c an r lea 6 e 1 C Infection 6/11/16/18 Susceptible Coinfected Clearance 6/11/16/18 Immune, all 4 types Death Infected, 6/11 types Death 8 n o cti 1 6/ Clearance 6/11 1 fe In Clearance 6/11 Immune, 6/11 types 12 Death Infection 16/18 Clearance 16/18 Waning Immunity Infection 6/11 Xklib+Sklib Infected, 16/18 types Death
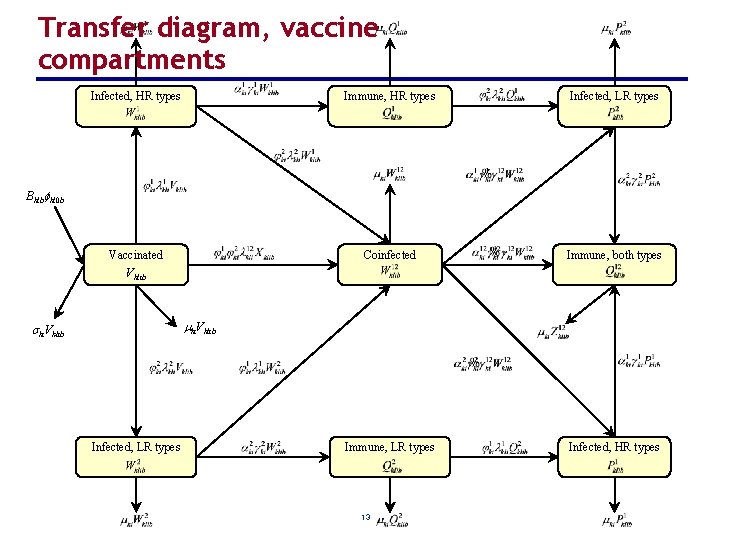
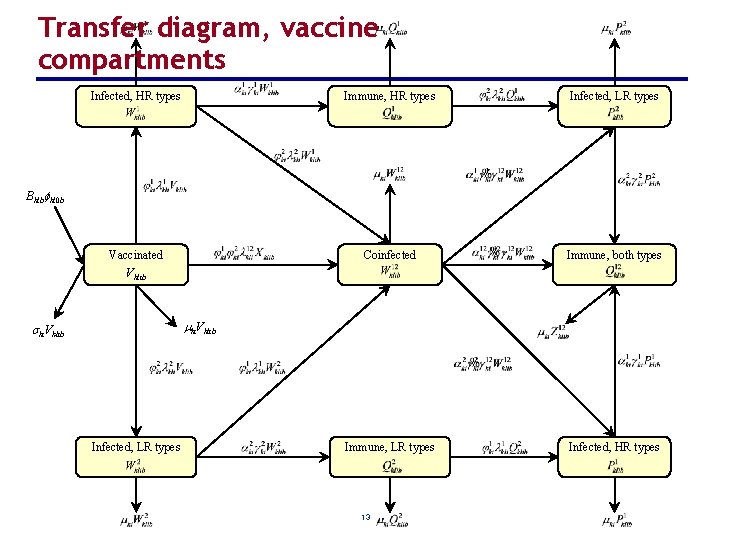
Transfer diagram, vaccine compartments Infected, HR types Immune, HR types Infected, LR types Vaccinated Coinfected Immune, both types Immune, LR types Infected, HR types Bklb kl 0 b Vklib ki. Vklib Infected, LR types 13
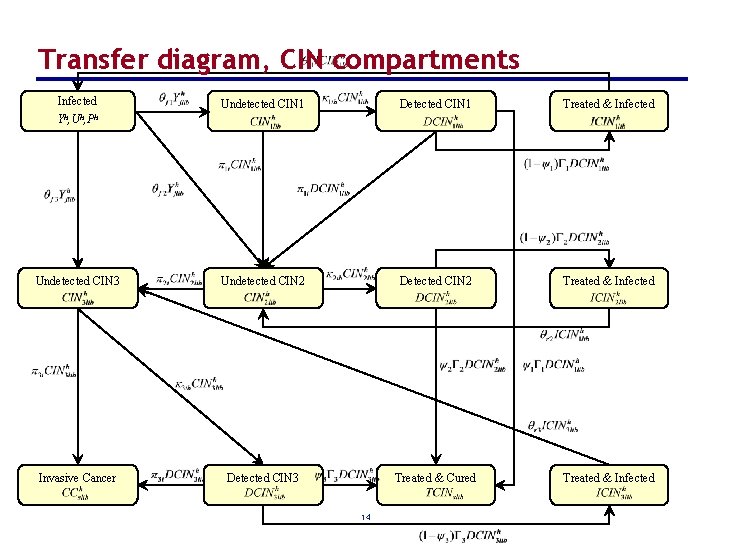
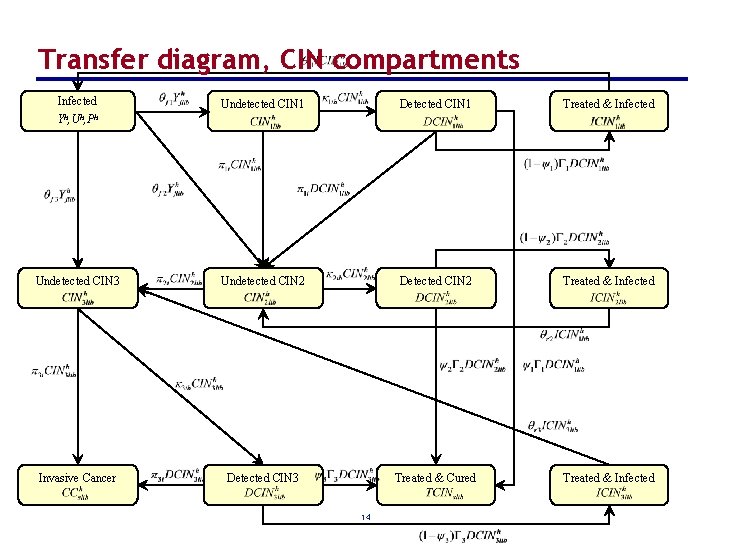
Transfer diagram, CIN compartments Infected Undetected CIN 1 Detected CIN 1 Treated & Infected Undetected CIN 3 Undetected CIN 2 Detected CIN 2 Treated & Infected Invasive Cancer Detected CIN 3 Treated & Cured Treated & Infected Yh, Uh, Ph 14
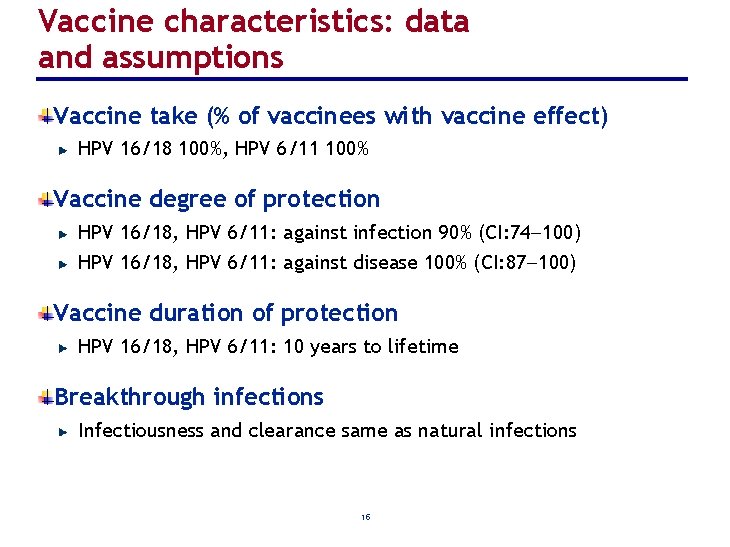
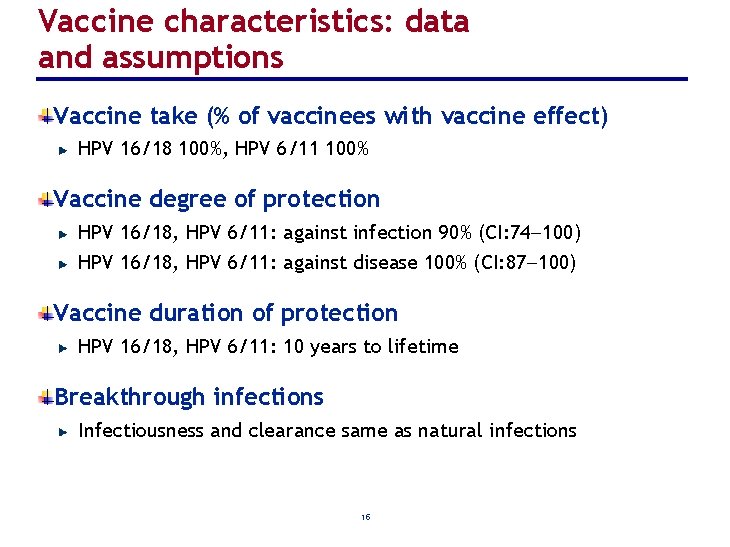
Vaccine characteristics: data and assumptions Vaccine take (% of vaccinees with vaccine effect) HPV 16/18 100%, HPV 6/11 100% Vaccine degree of protection HPV 16/18, HPV 6/11: against infection 90% (CI: 74 100) HPV 16/18, HPV 6/11: against disease 100% (CI: 87 100) Vaccine duration of protection HPV 16/18, HPV 6/11: 10 years to lifetime Breakthrough infections Infectiousness and clearance same as natural infections 15
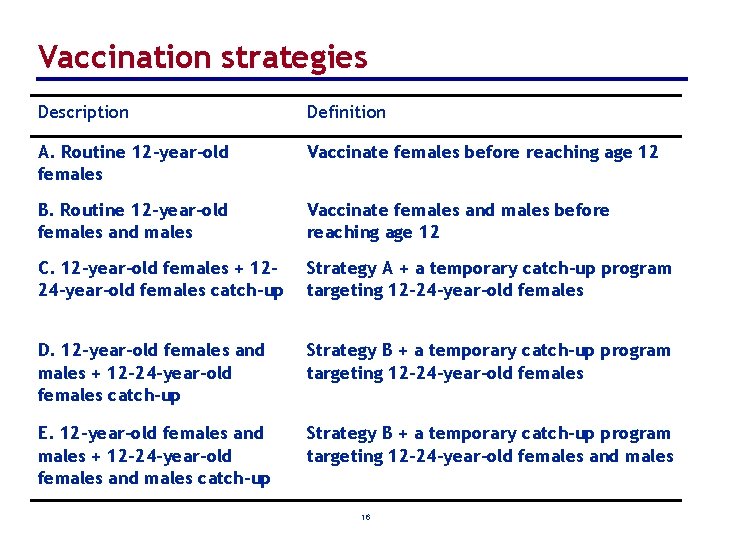
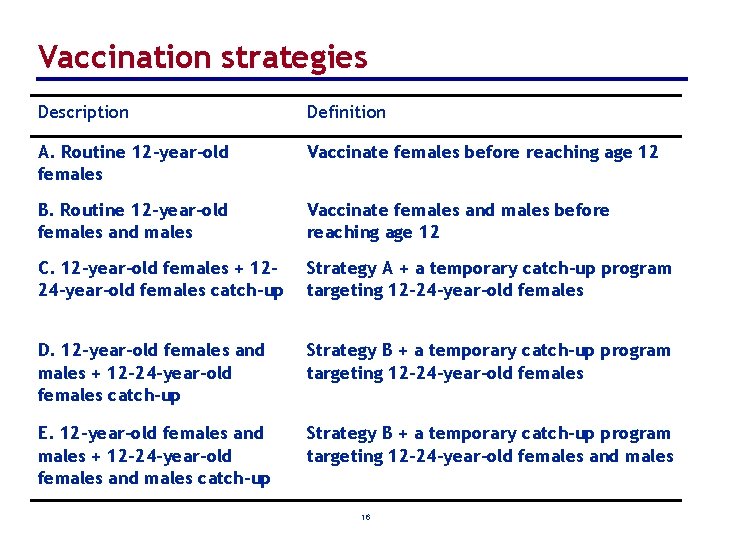
Vaccination strategies Description Definition A. Routine 12 -year-old females Vaccinate females before reaching age 12 B. Routine 12 -year-old females and males Vaccinate females and males before reaching age 12 C. 12 -year-old females + 12– 24 -year-old females catch-up Strategy A + a temporary catch-up program targeting 12– 24 -year-old females D. 12 -year-old females and males + 12– 24 -year-old females catch-up Strategy B + a temporary catch-up program targeting 12– 24 -year-old females E. 12 -year-old females and males + 12– 24 -year-old females and males catch-up Strategy B + a temporary catch-up program targeting 12– 24 -year-old females and males 16
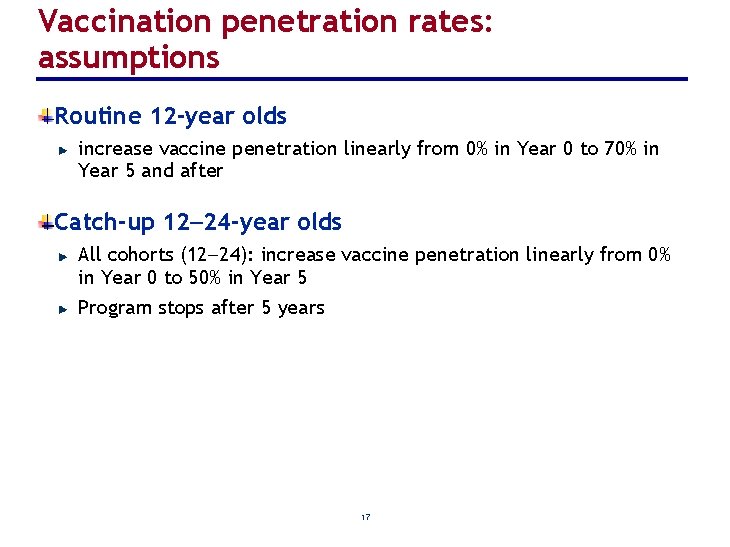
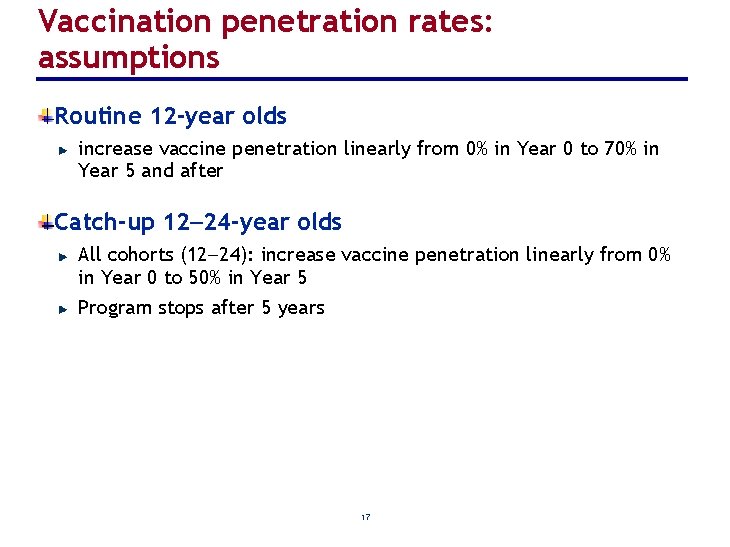
Vaccination penetration rates: assumptions Routine 12 -year olds increase vaccine penetration linearly from 0% in Year 0 to 70% in Year 5 and after Catch-up 12 24 -year olds All cohorts (12 24): increase vaccine penetration linearly from 0% in Year 0 to 50% in Year 5 Program stops after 5 years 17
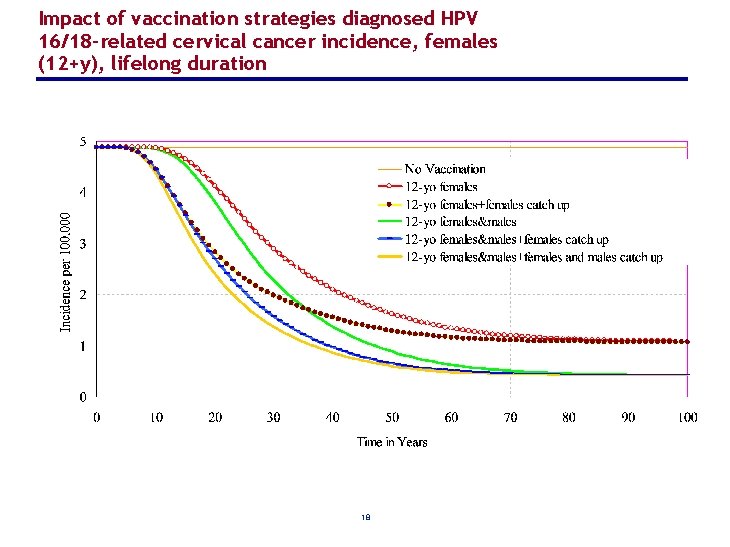
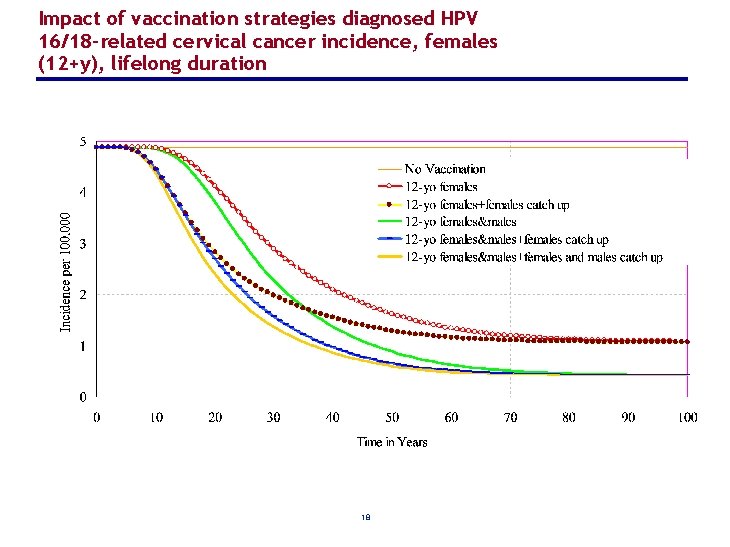
Impact of vaccination strategies diagnosed HPV 16/18 -related cervical cancer incidence, females (12+y), lifelong duration 18
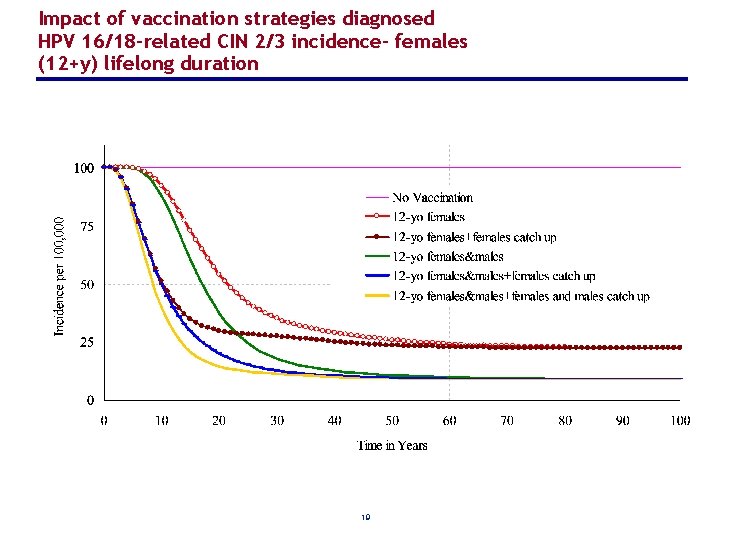
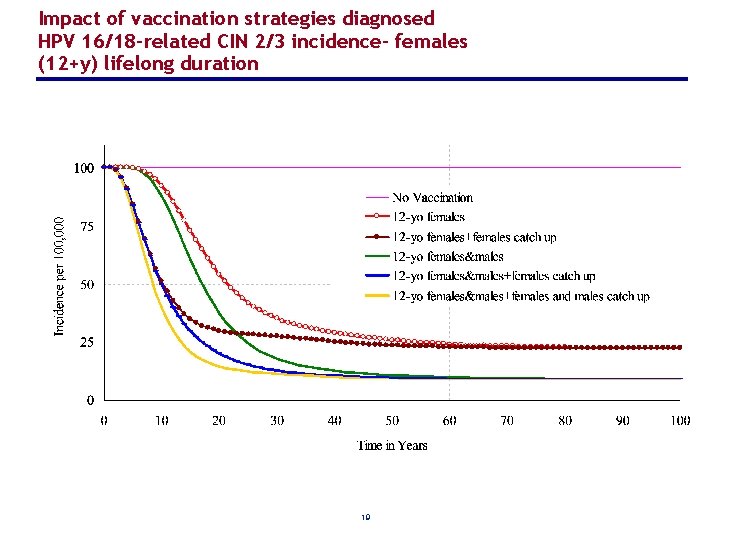
Impact of vaccination strategies diagnosed HPV 16/18 -related CIN 2/3 incidence- females (12+y) lifelong duration 19
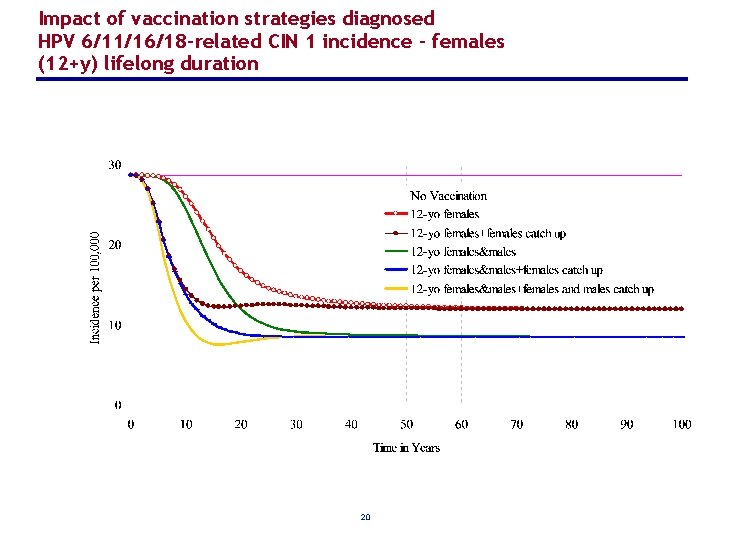
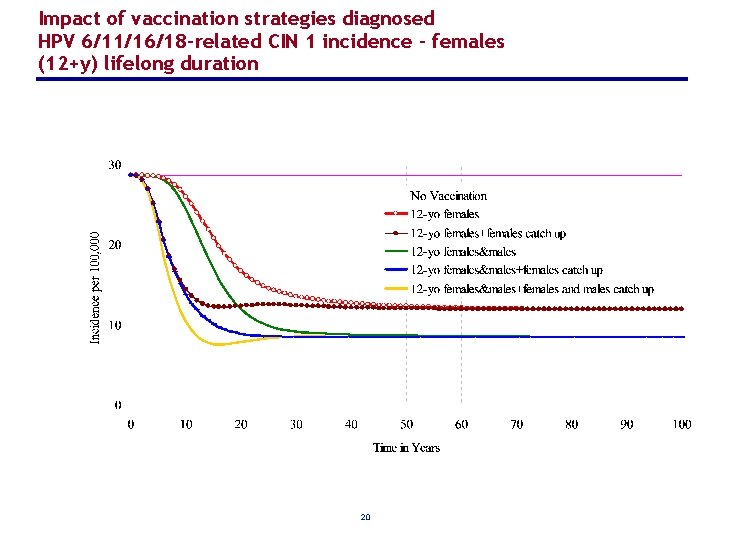
Impact of vaccination strategies diagnosed HPV 6/11/16/18 -related CIN 1 incidence - females (12+y) lifelong duration 20
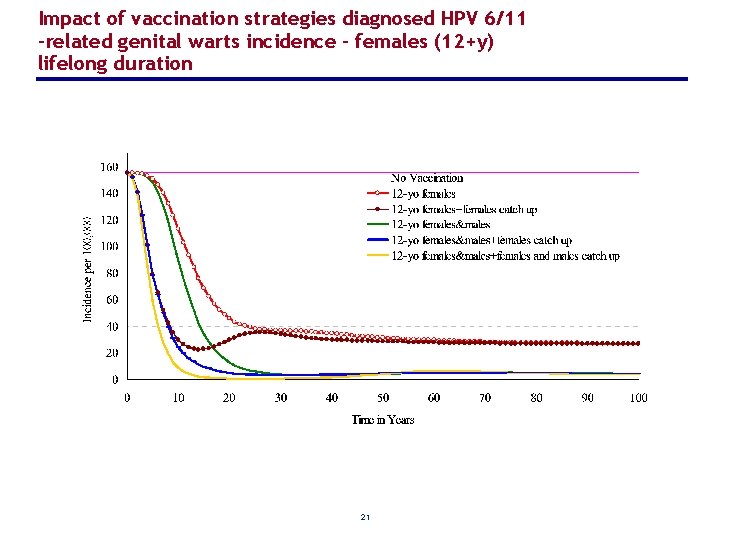
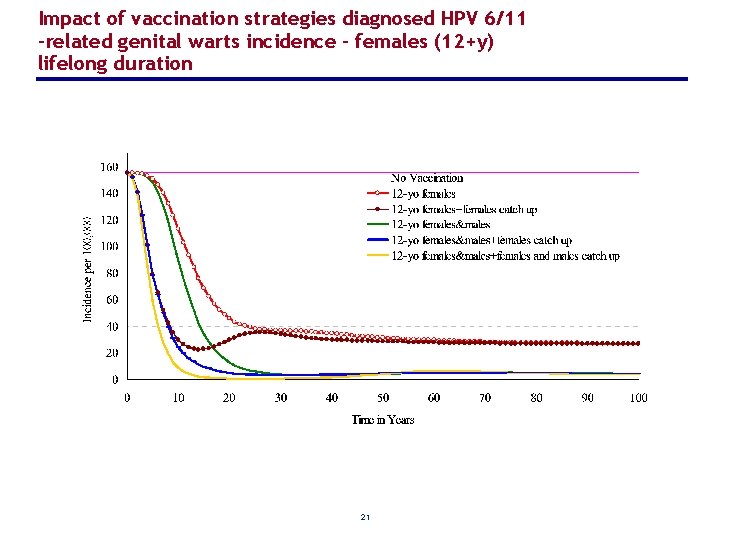
Impact of vaccination strategies diagnosed HPV 6/11 -related genital warts incidence - females (12+y) lifelong duration 21
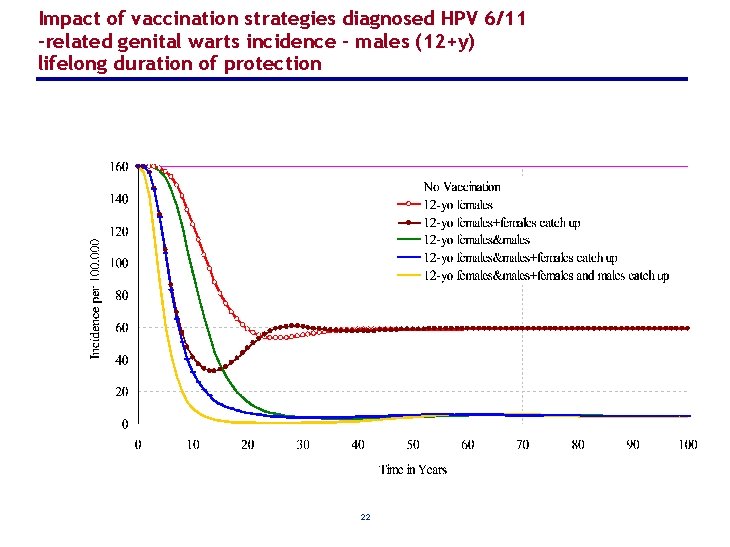
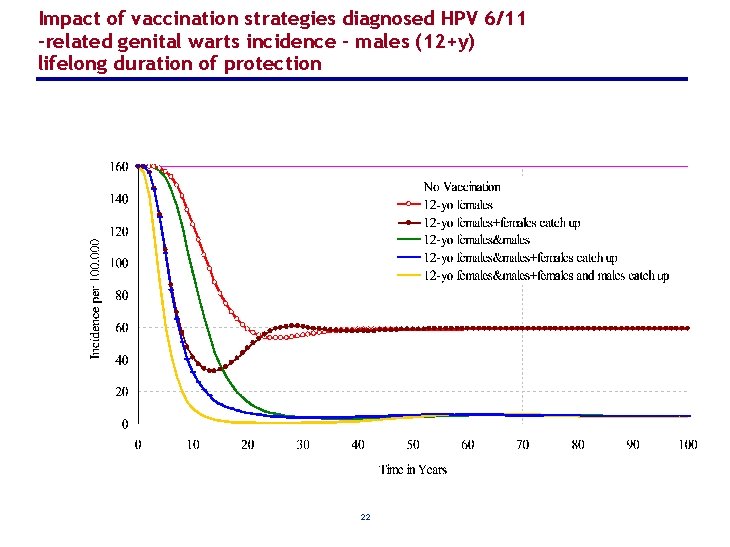
Impact of vaccination strategies diagnosed HPV 6/11 -related genital warts incidence - males (12+y) lifelong duration of protection 22
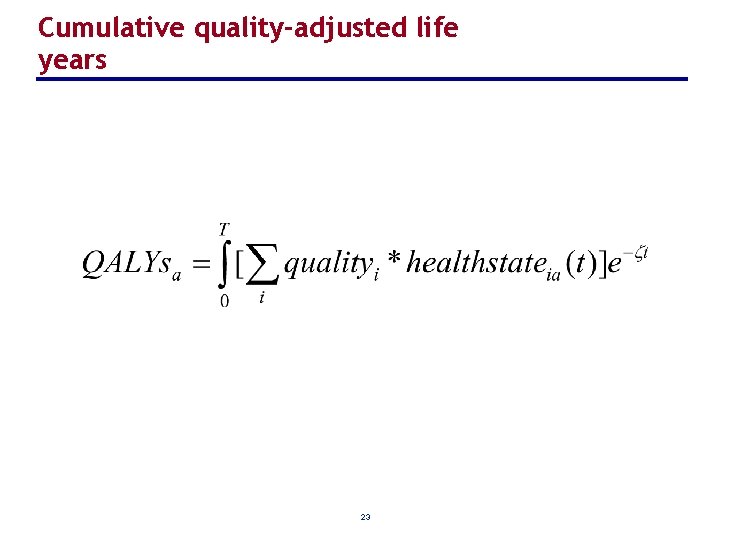
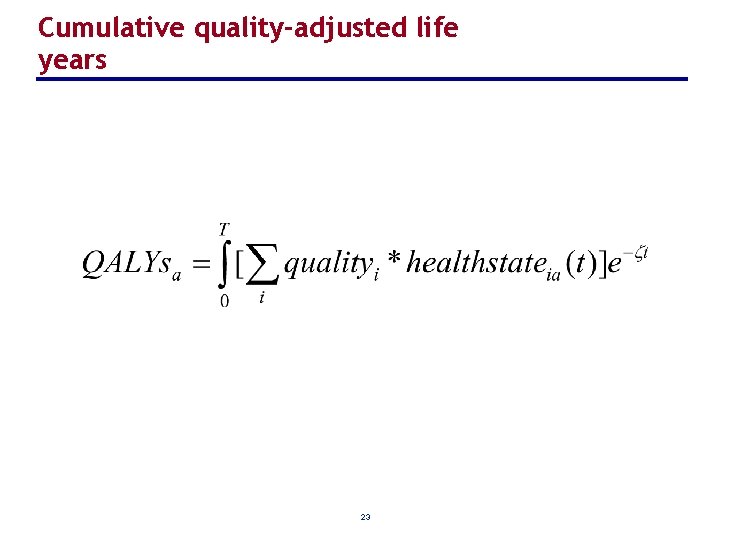
Cumulative quality-adjusted life years 23
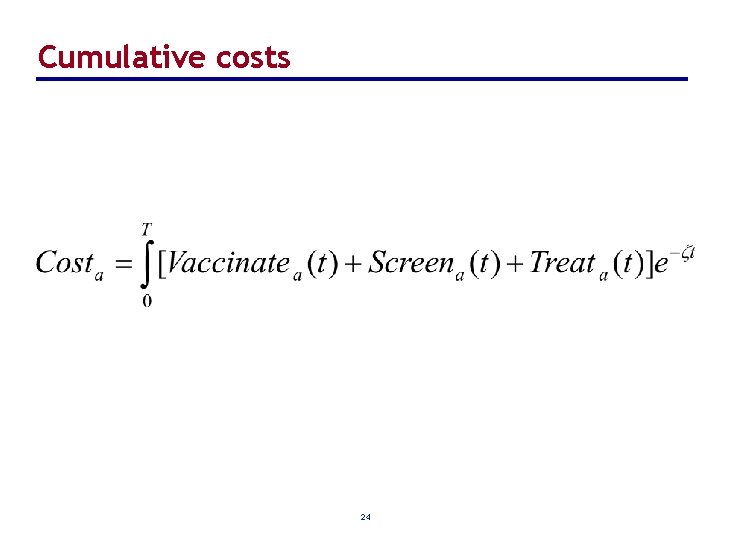
Cumulative costs 24
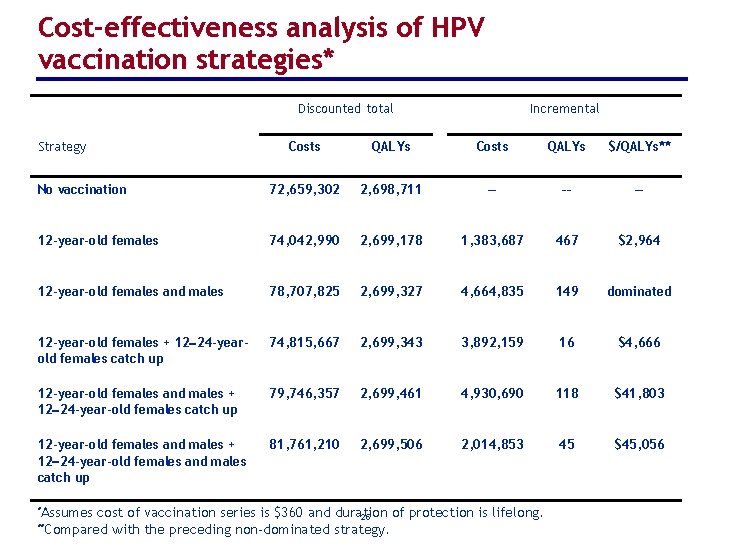
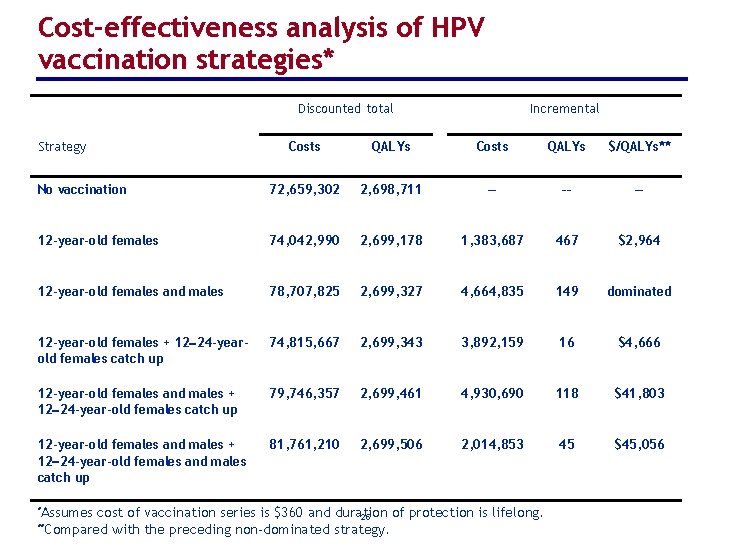
Cost-effectiveness analysis of HPV vaccination strategies* Discounted total Strategy Incremental Costs QALYs $/QALYs** No vaccination 72, 659, 302 2, 698, 711 –– –– –– 12 -year-old females 74, 042, 990 2, 699, 178 1, 383, 687 467 $2, 964 12 -year-old females and males 78, 707, 825 2, 699, 327 4, 664, 835 149 dominated 12 -year-old females + 12 24 -yearold females catch up 74, 815, 667 2, 699, 343 3, 892, 159 16 $4, 666 12 -year-old females and males + 12 24 -year-old females catch up 79, 746, 357 2, 699, 461 4, 930, 690 118 $41, 803 12 -year-old females and males + 12 24 -year-old females and males catch up 81, 761, 210 2, 699, 506 2, 014, 853 45 $45, 056 *Assumes cost of vaccination series is $360 and duration of protection is lifelong. 25 with the preceding non-dominated strategy. **Compared
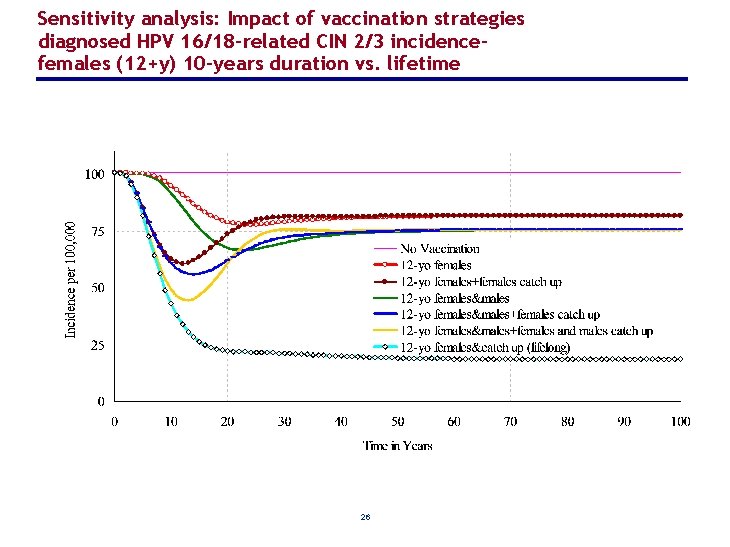
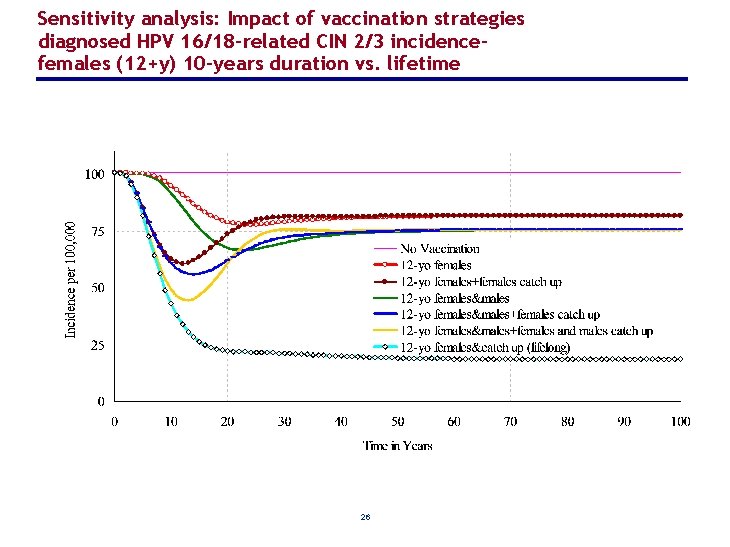
Sensitivity analysis: Impact of vaccination strategies diagnosed HPV 16/18 -related CIN 2/3 incidencefemales (12+y) 10 -years duration vs. lifetime 26
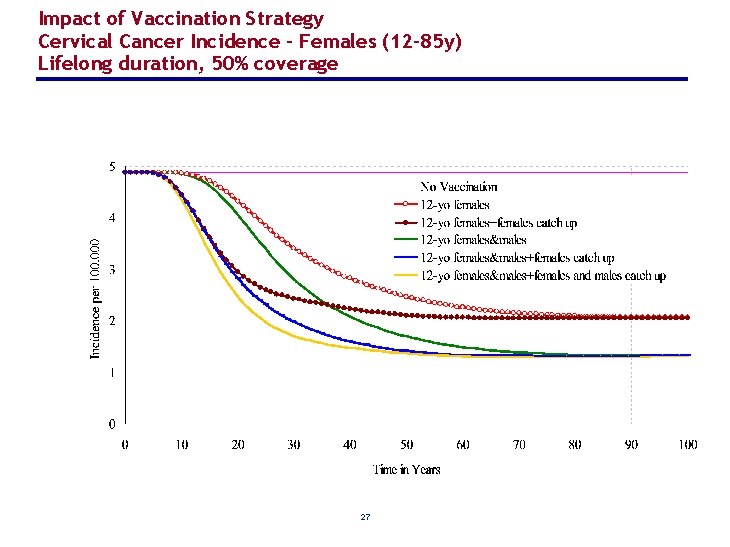
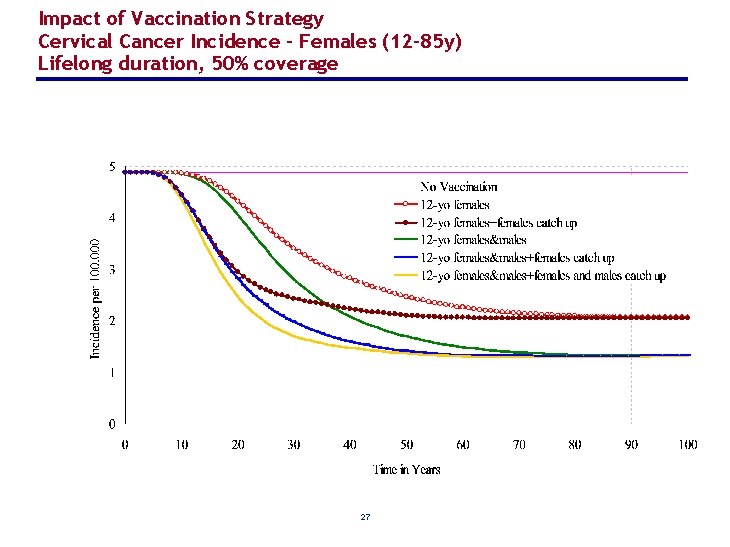
Impact of Vaccination Strategy Cervical Cancer Incidence - Females (12– 85 y) Lifelong duration, 50% coverage 27
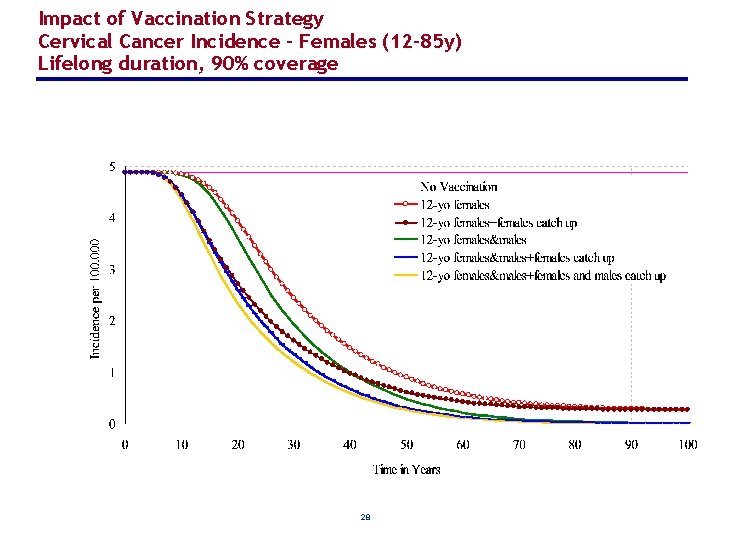
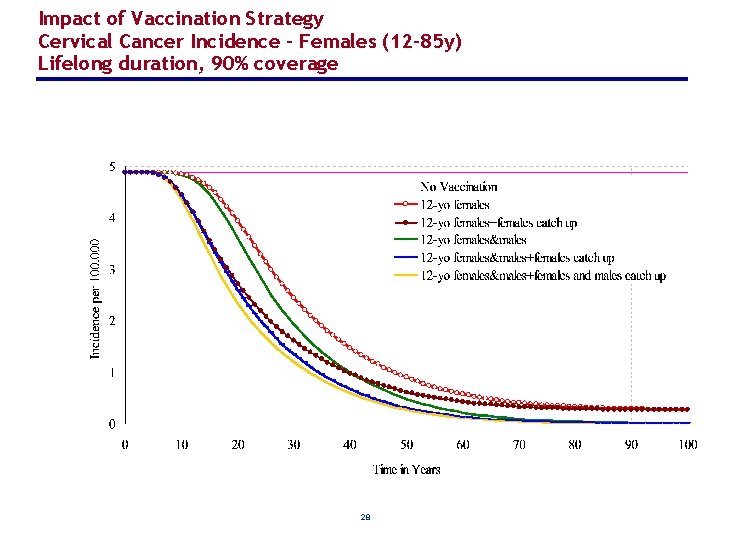
Impact of Vaccination Strategy Cervical Cancer Incidence - Females (12– 85 y) Lifelong duration, 90% coverage 28
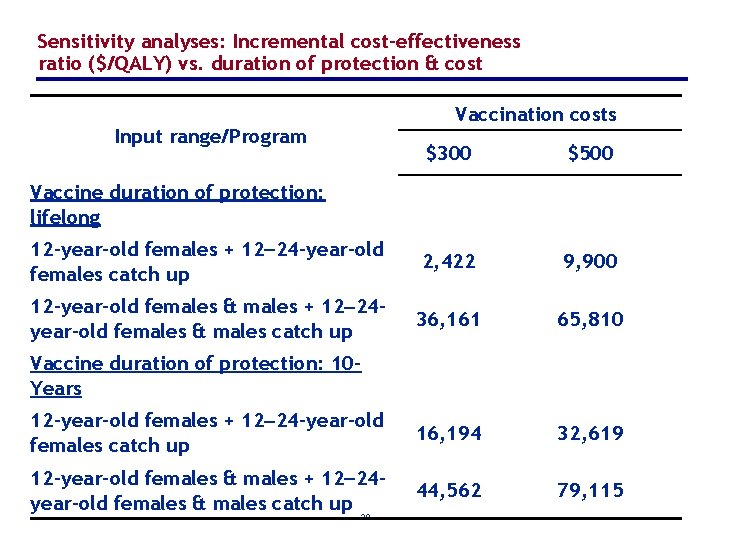
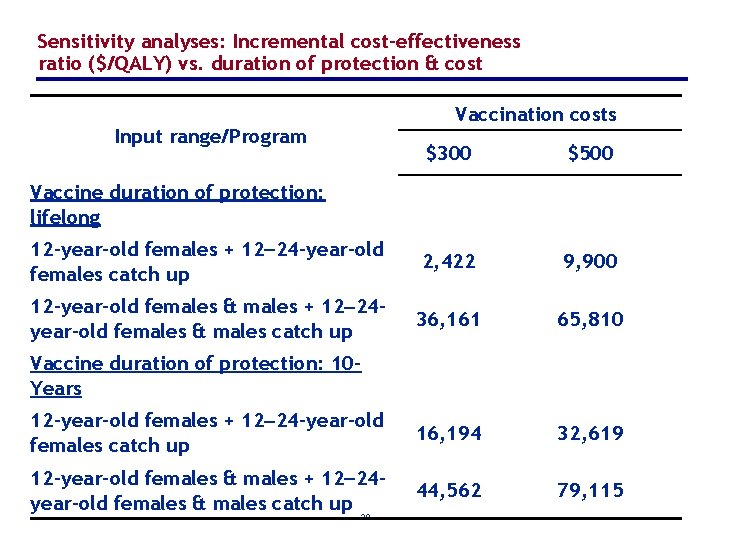
Sensitivity analyses: Incremental cost-effectiveness ratio ($/QALY) vs. duration of protection & cost Vaccination costs Input range/Program $300 $500 12 -year-old females + 12 24 -year-old females catch up 2, 422 9, 900 12 -year-old females & males + 12 24 year-old females & males catch up 36, 161 65, 810 12 -year-old females + 12 24 -year-old females catch up 16, 194 32, 619 12 -year-old females & males + 12 24 year-old females & males catch up 44, 562 79, 115 Vaccine duration of protection: lifelong Vaccine duration of protection: 10 Years 29
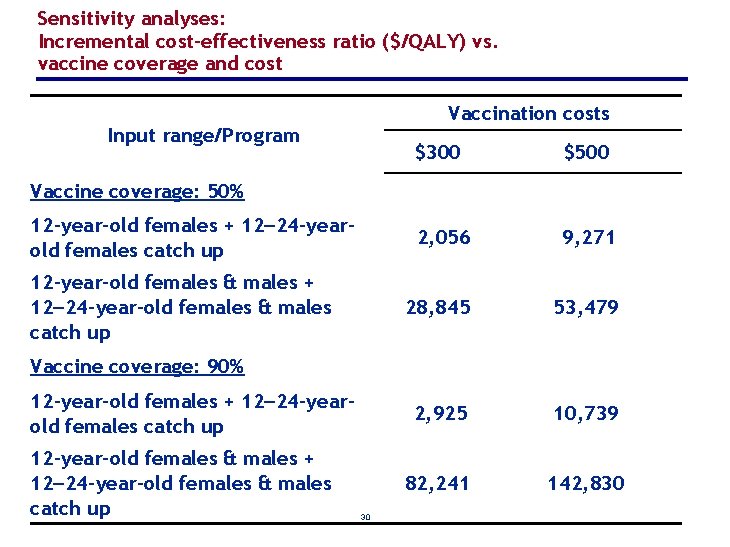
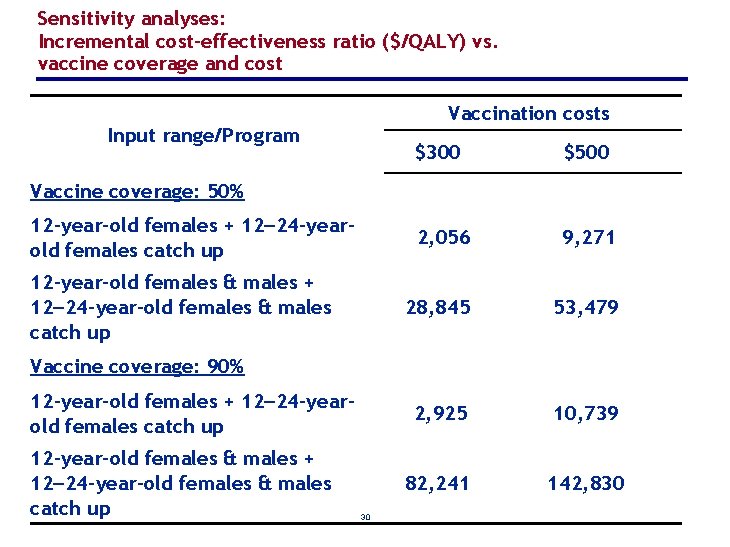
Sensitivity analyses: Incremental cost-effectiveness ratio ($/QALY) vs. vaccine coverage and cost Vaccination costs Input range/Program $300 $500 2, 056 9, 271 28, 845 53, 479 2, 925 10, 739 82, 241 142, 830 Vaccine coverage: 50% 12 -year-old females + 12 24 -yearold females catch up 12 -year-old females & males + 12 24 -year-old females & males catch up Vaccine coverage: 90% 12 -year-old females + 12 24 -yearold females catch up 12 -year-old females & males + 12 24 -year-old females & males catch up 30
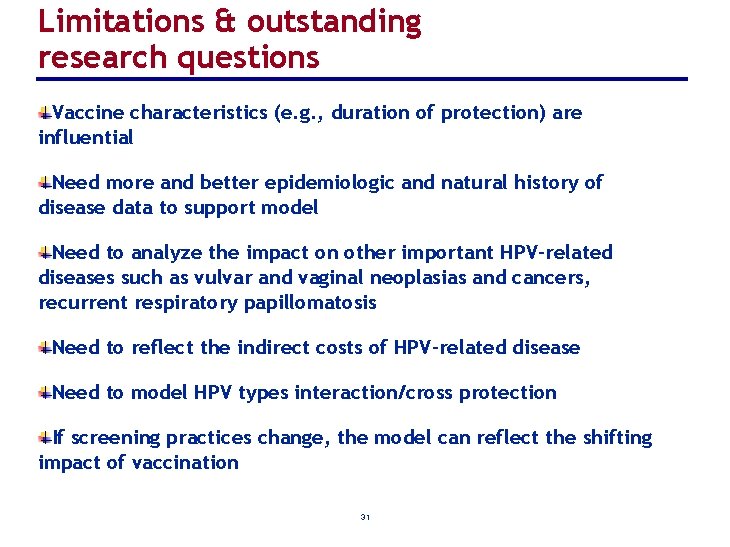
Limitations & outstanding research questions Vaccine characteristics (e. g. , duration of protection) are influential Need more and better epidemiologic and natural history of disease data to support model Need to analyze the impact on other important HPV-related diseases such as vulvar and vaginal neoplasias and cancers, recurrent respiratory papillomatosis Need to reflect the indirect costs of HPV-related disease Need to model HPV types interaction/cross protection If screening practices change, the model can reflect the shifting impact of vaccination 31
Summary A prophylactic quadrivalent HPV vaccine can substantially reduce the incidence of cervical cancer, CIN, and genital warts Catch up vaccination can provide earlier and greater reductions in HPV-related disease Vaccinating males and females before age 12 combined with a temporary 12 24 -year olds catch up program can be cost-effective and efficiently added to current screening programs 32
Acknowledgement Erik J. Dasbach, Ph. D Ralph P. Insinga, Ph. D Merck Research Laboratories, USA 33
 Hpv test for men
Hpv test for men Hpv oral cancer
Hpv oral cancer Hpv vaccine schedule adults
Hpv vaccine schedule adults Hpv cancer prevention
Hpv cancer prevention Hpv testi nasıl yapılır
Hpv testi nasıl yapılır Triage sort
Triage sort Does hpv go away
Does hpv go away Paplloma
Paplloma Hpv type 16 and 18
Hpv type 16 and 18 Hpv type 16 and 18
Hpv type 16 and 18 Cervixabrasio
Cervixabrasio 9 valanlı hpv aşısı
9 valanlı hpv aşısı Histologia
Histologia Cancerscreening.gov.au
Cancerscreening.gov.au Hpv cervical cancer
Hpv cervical cancer Metrorragia
Metrorragia Hpv cervical cancer
Hpv cervical cancer Low grade squamous intraepithelial lesion
Low grade squamous intraepithelial lesion Hpv dna testi
Hpv dna testi Cervixcancer
Cervixcancer Hpv
Hpv Genital warts
Genital warts Prevention hpv
Prevention hpv Hpv
Hpv Hpv infection
Hpv infection Epidermal dysplasia verruciformis
Epidermal dysplasia verruciformis Ahcc hpv
Ahcc hpv Hpv discret test
Hpv discret test Hpv
Hpv Human vs non human bones
Human vs non human bones Human needs and human development chapter 8
Human needs and human development chapter 8 Chapter 8 human needs and human development
Chapter 8 human needs and human development Gni definition ap human geography
Gni definition ap human geography Non human nouns
Non human nouns