2017 National Training Program Medigap Helpline Services Medicare


- Slides: 62

2017 National Training Program Medigap Helpline Services. Medicare Supplement Insurance Policies; Medicare Advantage Plans; Other Insurance Coverages. August 16, 2017
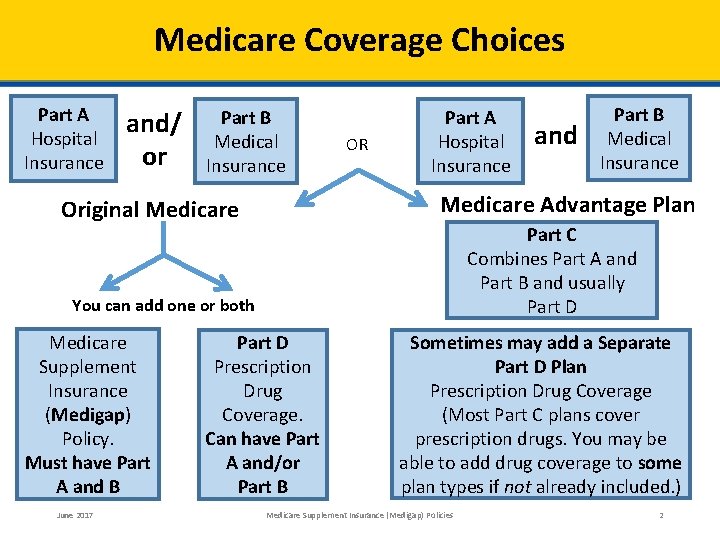
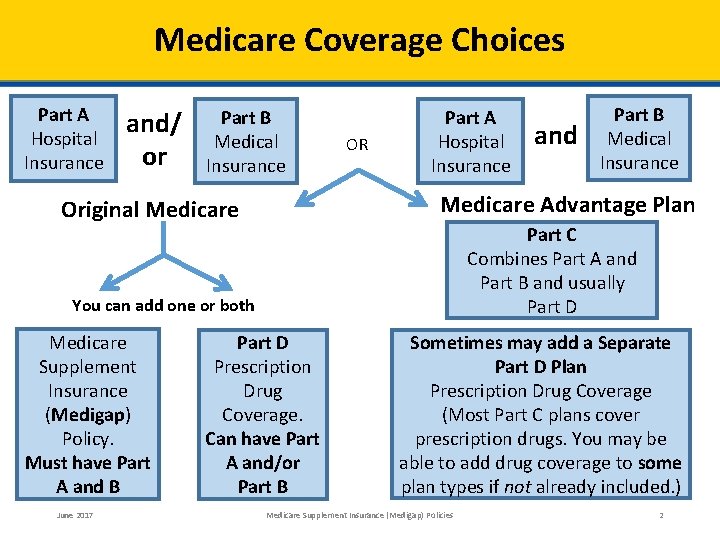
Medicare Coverage Choices Part A Hospital Insurance and/ or Part B Medical Insurance OR Part A Hospital Insurance Medicare Advantage Plan Original Medicare Part C Combines Part A and Part B and usually Part D You can add one or both Medicare Supplement Insurance (Medigap) Policy. Must have Part A and B June 2017 and Part B Medical Insurance Part D Prescription Drug Coverage. Can have Part A and/or Part B Sometimes may add a Separate Part D Plan Prescription Drug Coverage (Most Part C plans cover prescription drugs. You may be able to add drug coverage to some plan types if not already included. ) Medicare Supplement Insurance (Medigap) Policies 2
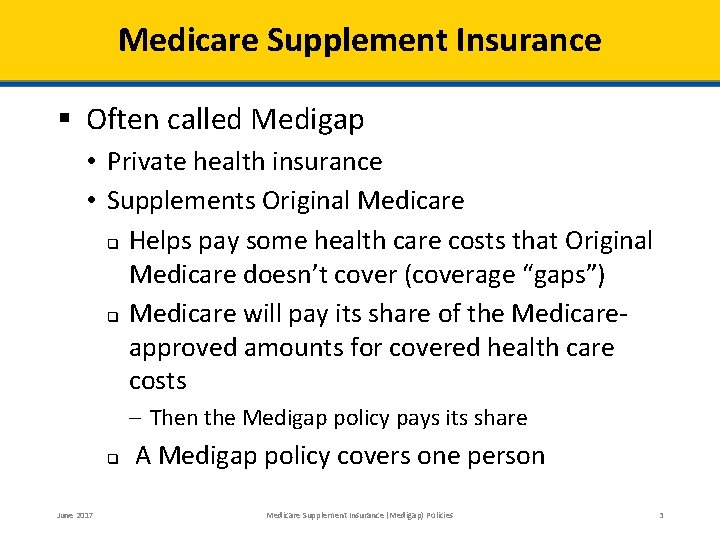
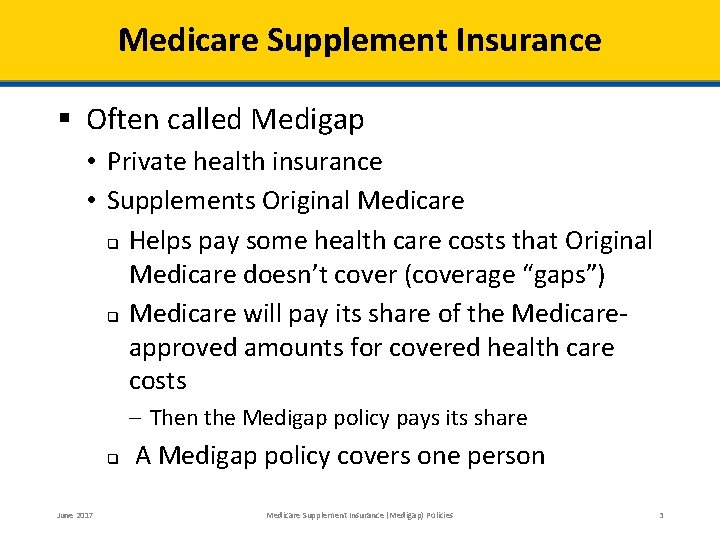
Medicare Supplement Insurance § Often called Medigap • Private health insurance • Supplements Original Medicare q Helps pay some health care costs that Original Medicare doesn’t cover (coverage “gaps”) q Medicare will pay its share of the Medicareapproved amounts for covered health care costs – Then the Medigap policy pays its share q June 2017 A Medigap policy covers one person Medicare Supplement Insurance (Medigap) Policies 3
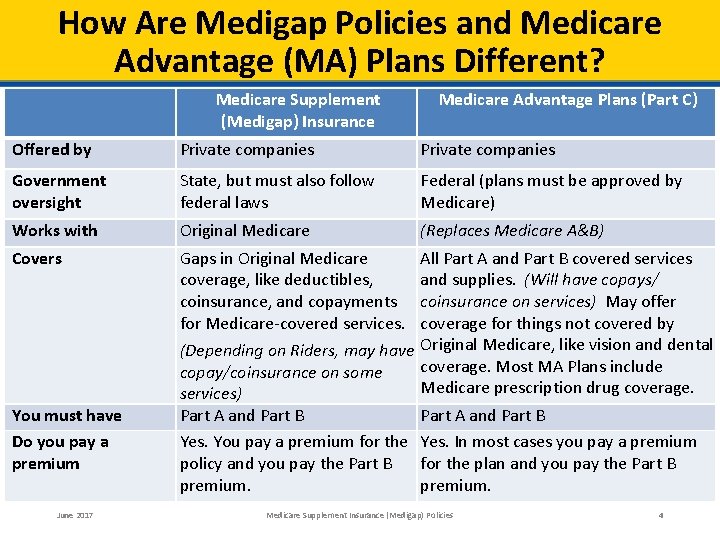
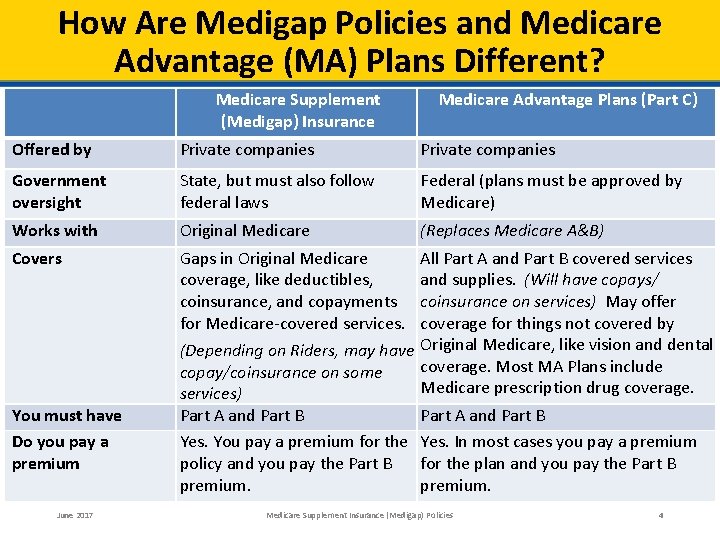
How Are Medigap Policies and Medicare Advantage (MA) Plans Different? Medicare Supplement (Medigap) Insurance Medicare Advantage Plans (Part C) Offered by Private companies Government oversight State, but must also follow federal laws Federal (plans must be approved by Medicare) Works with Original Medicare (Replaces Medicare A&B) Covers Gaps in Original Medicare coverage, like deductibles, coinsurance, and copayments for Medicare-covered services. You must have Do you pay a premium Part A and Part B Yes. You pay a premium for the policy and you pay the Part B premium. June 2017 All Part A and Part B covered services and supplies. (Will have copays/ coinsurance on services) May offer coverage for things not covered by (Depending on Riders, may have Original Medicare, like vision and dental coverage. Most MA Plans include copay/coinsurance on some Medicare prescription drug coverage. services) Part A and Part B Yes. In most cases you pay a premium for the plan and you pay the Part B premium. Medicare Supplement Insurance (Medigap) Policies 4
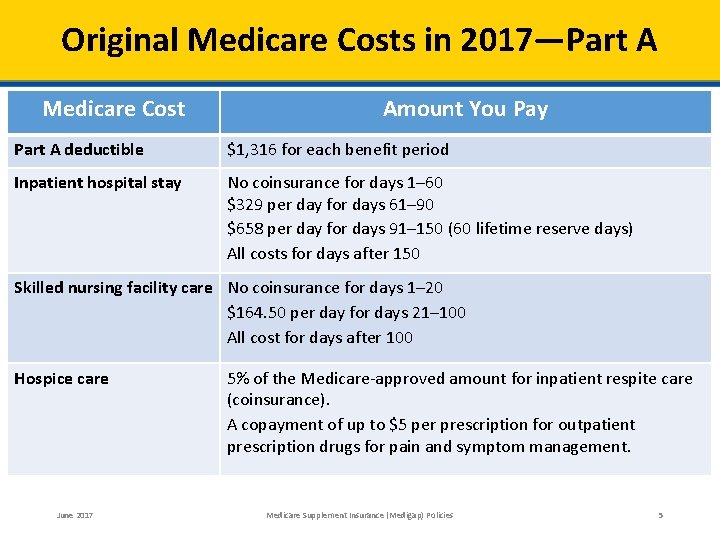
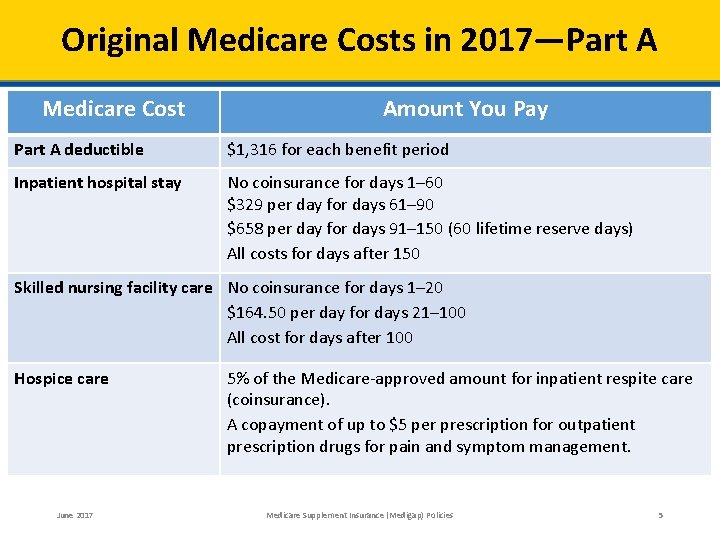
Original Medicare Costs in 2017—Part A Medicare Cost Amount You Pay Part A deductible $1, 316 for each benefit period Inpatient hospital stay No coinsurance for days 1– 60 $329 per day for days 61– 90 $658 per day for days 91– 150 (60 lifetime reserve days) All costs for days after 150 Skilled nursing facility care No coinsurance for days 1– 20 $164. 50 per day for days 21– 100 All cost for days after 100 Hospice care June 2017 5% of the Medicare-approved amount for inpatient respite care (coinsurance). A copayment of up to $5 per prescription for outpatient prescription drugs for pain and symptom management. Medicare Supplement Insurance (Medigap) Policies 5
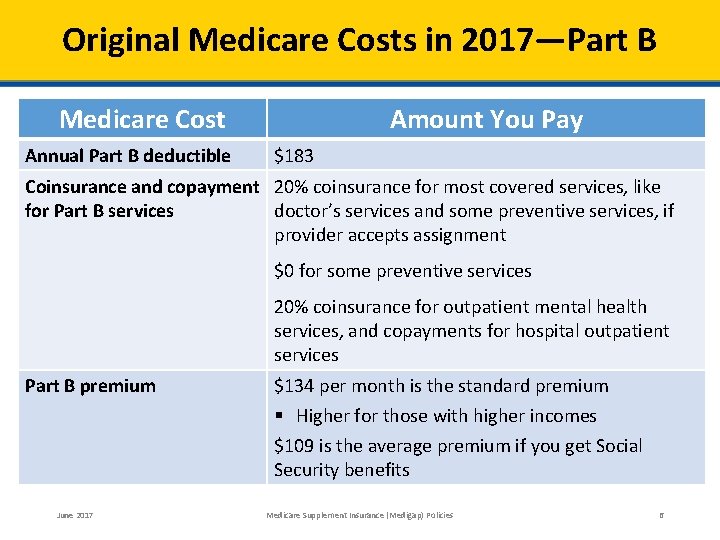
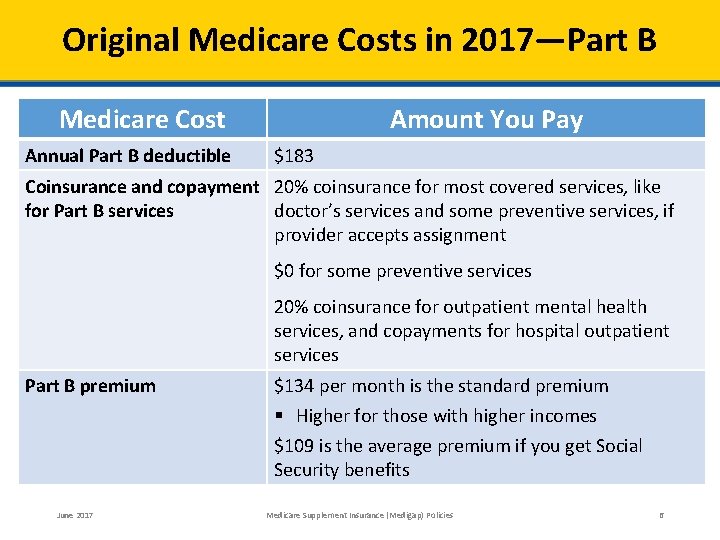
Original Medicare Costs in 2017—Part B Medicare Cost Annual Part B deductible Amount You Pay $183 Coinsurance and copayment 20% coinsurance for most covered services, like for Part B services doctor’s services and some preventive services, if provider accepts assignment $0 for some preventive services 20% coinsurance for outpatient mental health services, and copayments for hospital outpatient services Part B premium $134 per month is the standard premium § Higher for those with higher incomes $109 is the average premium if you get Social Security benefits June 2017 Medicare Supplement Insurance (Medigap) Policies 6
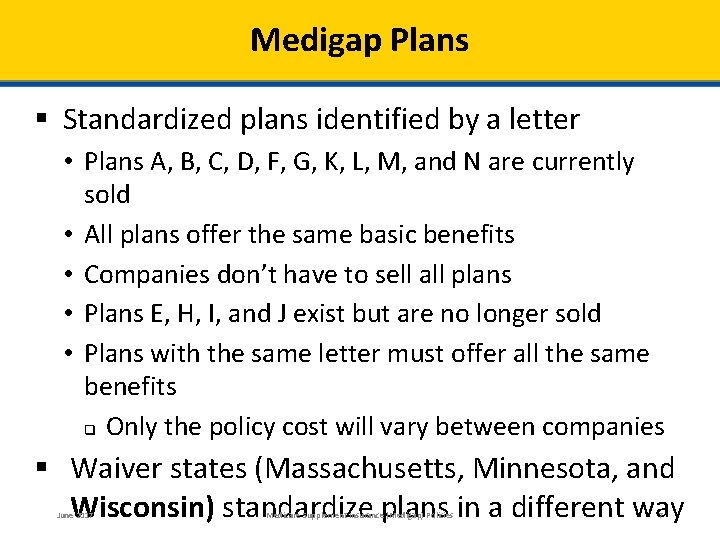
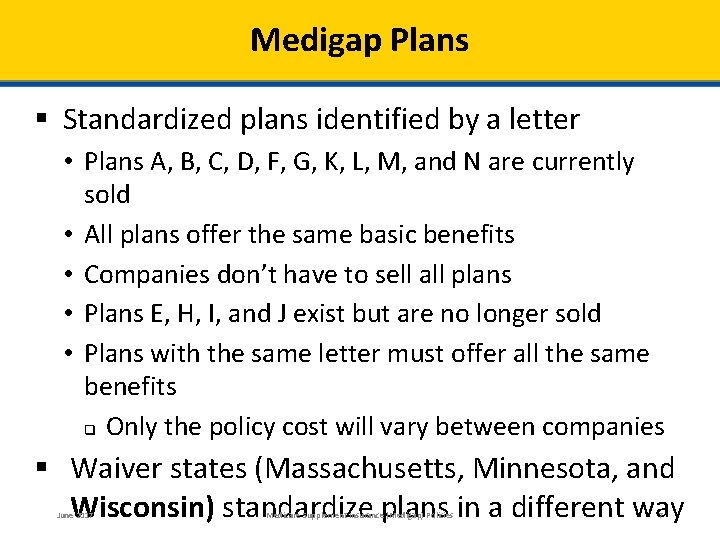
Medigap Plans § Standardized plans identified by a letter • Plans A, B, C, D, F, G, K, L, M, and N are currently sold • All plans offer the same basic benefits • Companies don’t have to sell all plans • Plans E, H, I, and J exist but are no longer sold • Plans with the same letter must offer all the same benefits q Only the policy cost will vary between companies § Waiver states (Massachusetts, Minnesota, and Wisconsin) standardize plans in a different way June 2017 Medicare Supplement Insurance (Medigap) Policies 7
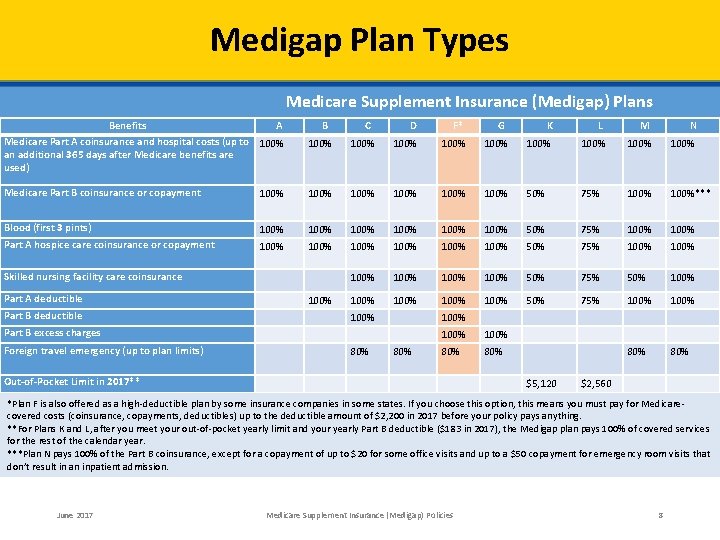
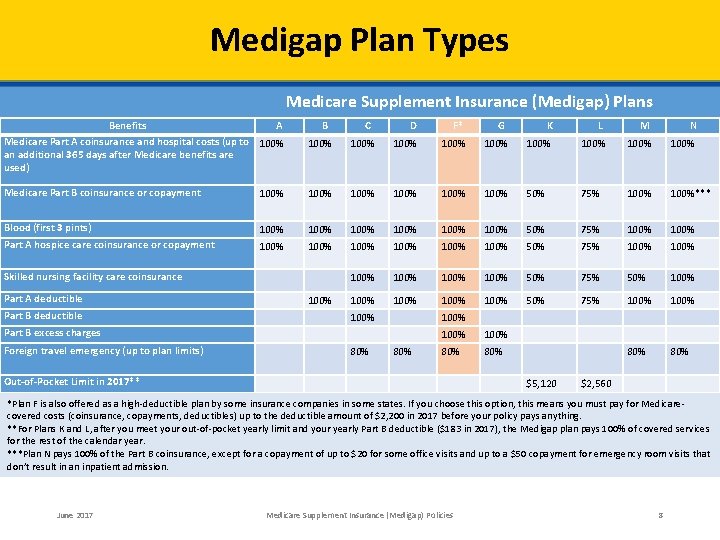
Medigap Plan Types Medicare Supplement Insurance (Medigap) Plans Benefits A Medicare Part A coinsurance and hospital costs (up to 100% an additional 365 days after Medicare benefits are used) B 100% Medicare Part B coinsurance or copayment 100% Blood (first 3 pints) Part A hospice care coinsurance or copayment D F* 100% 100% 100% Skilled nursing facility care coinsurance Part A deductible Part B deductible 100% C K L M N 100% 100% 50% 75% 100%*** 100% 100% 50% 75% 100% 100% 100% 50% 75% 50% 100% 100% 50% 75% 100% 80% 100% Part B excess charges Foreign travel emergency (up to plan limits) 80% G 80% 100% 80% Out-of-Pocket Limit in 2017** $5, 120 $2, 560 *Plan F is also offered as a high-deductible plan by some insurance companies in some states. If you choose this option, this means you must pay for Medicarecovered costs (coinsurance, copayments, deductibles) up to the deductible amount of $2, 200 in 2017 before your policy pays anything. **For Plans K and L, after you meet your out-of-pocket yearly limit and your yearly Part B deductible ($183 in 2017), the Medigap plan pays 100% of covered services for the rest of the calendar year. ***Plan N pays 100% of the Part B coinsurance, except for a copayment of up to $20 for some office visits and up to a $50 copayment for emergency room visits that don’t result in an inpatient admission. June 2017 Medicare Supplement Insurance (Medigap) Policies 8
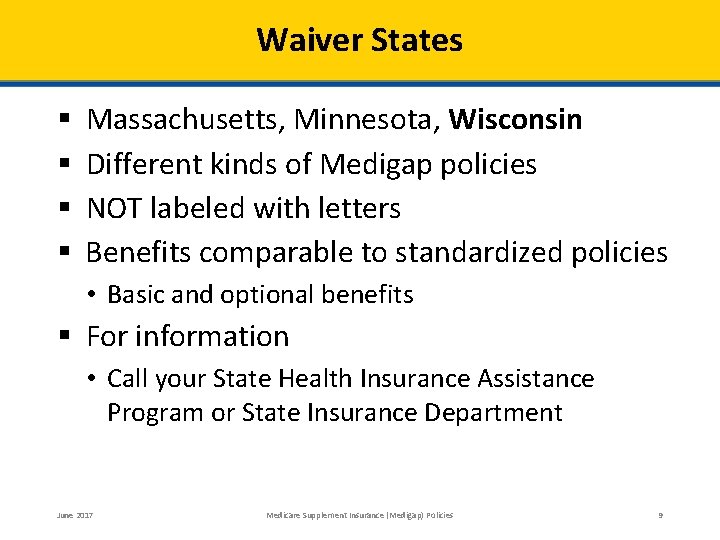
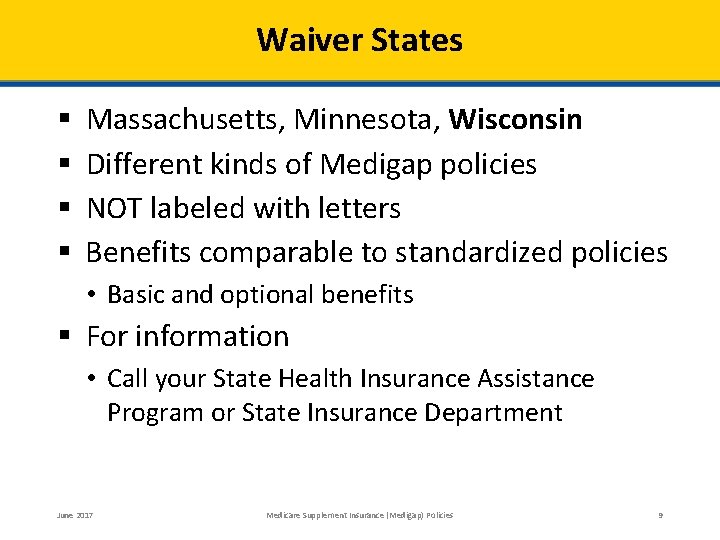
Waiver States § § Massachusetts, Minnesota, Wisconsin Different kinds of Medigap policies NOT labeled with letters Benefits comparable to standardized policies • Basic and optional benefits § For information • Call your State Health Insurance Assistance Program or State Insurance Department June 2017 Medicare Supplement Insurance (Medigap) Policies 9
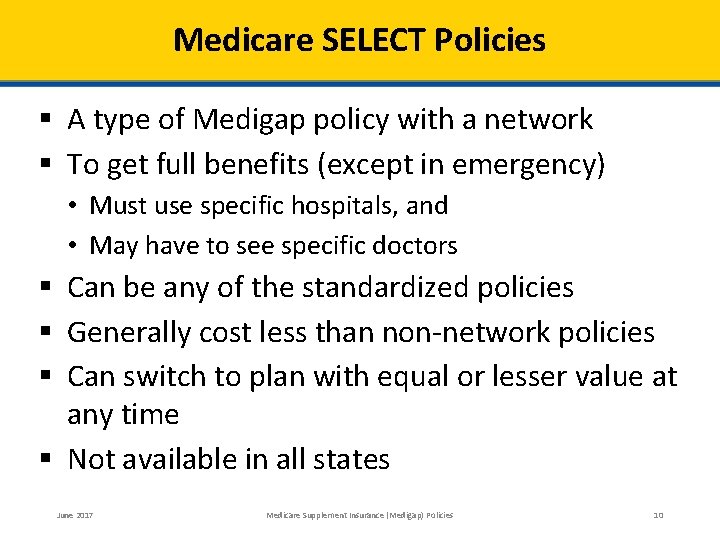
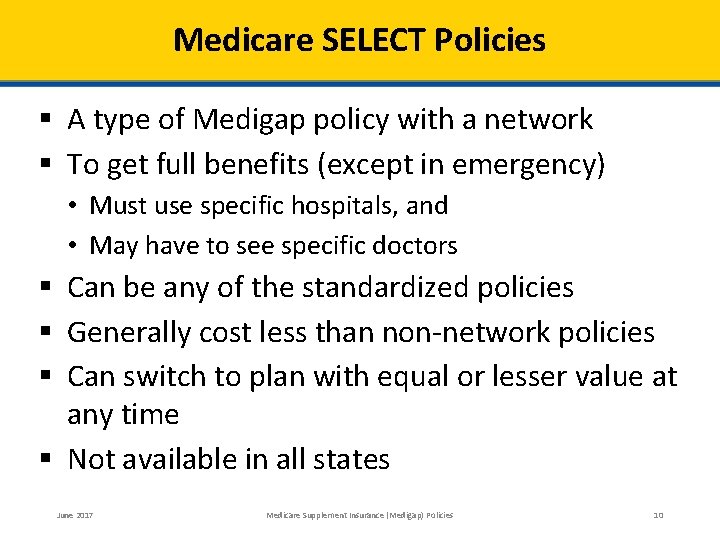
Medicare SELECT Policies § A type of Medigap policy with a network § To get full benefits (except in emergency) • Must use specific hospitals, and • May have to see specific doctors § Can be any of the standardized policies § Generally cost less than non-network policies § Can switch to plan with equal or lesser value at any time § Not available in all states June 2017 Medicare Supplement Insurance (Medigap) Policies 10
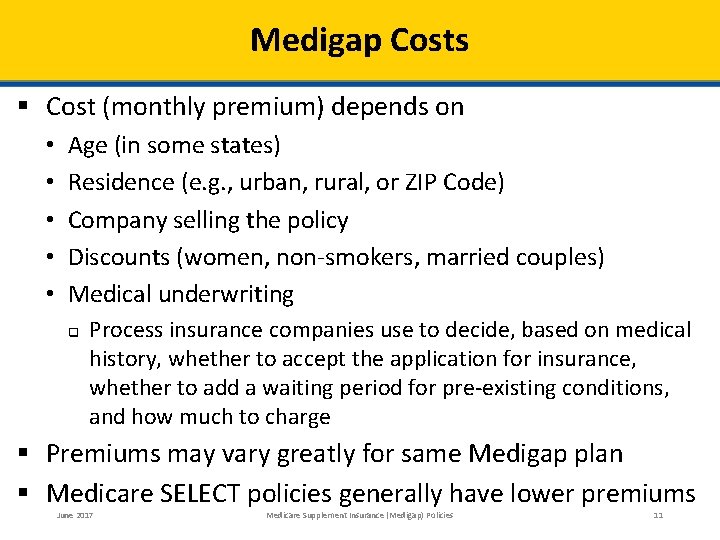
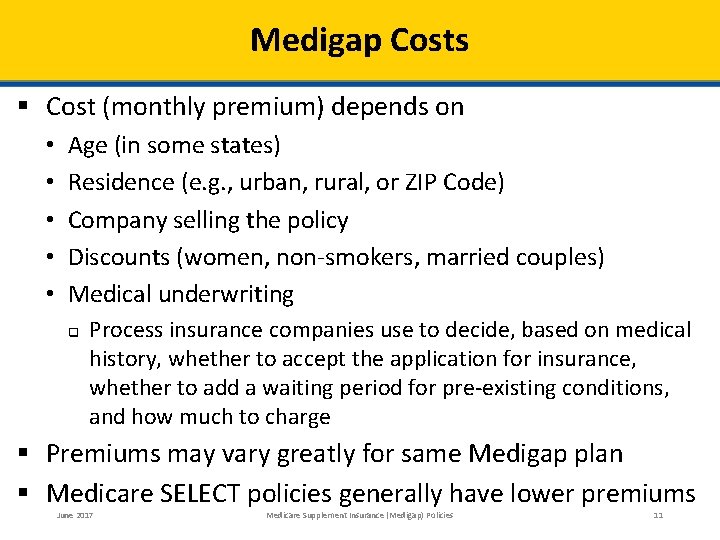
Medigap Costs § Cost (monthly premium) depends on • • • Age (in some states) Residence (e. g. , urban, rural, or ZIP Code) Company selling the policy Discounts (women, non-smokers, married couples) Medical underwriting q Process insurance companies use to decide, based on medical history, whether to accept the application for insurance, whether to add a waiting period for pre-existing conditions, and how much to charge § Premiums may vary greatly for same Medigap plan § Medicare SELECT policies generally have lower premiums June 2017 Medicare Supplement Insurance (Medigap) Policies 11
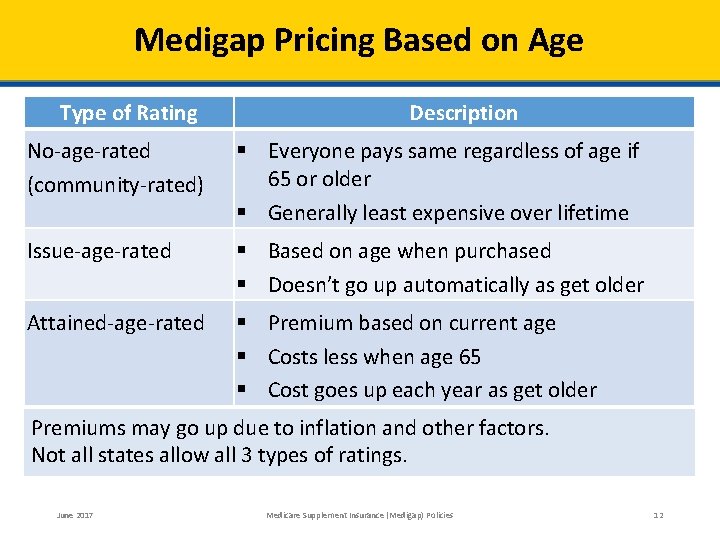
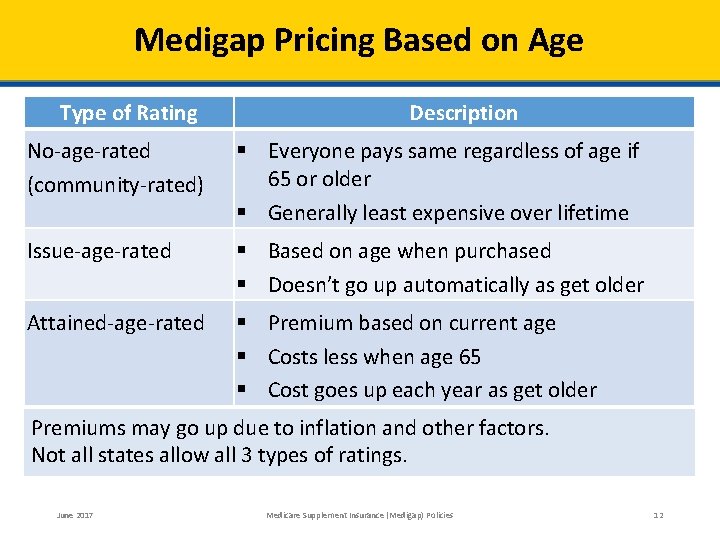
Medigap Pricing Based on Age Type of Rating Description No-age-rated (community-rated) § Everyone pays same regardless of age if 65 or older § Generally least expensive over lifetime Issue-age-rated § Based on age when purchased § Doesn’t go up automatically as get older Attained-age-rated § Premium based on current age § Costs less when age 65 § Cost goes up each year as get older Premiums may go up due to inflation and other factors. Not all states allow all 3 types of ratings. June 2017 Medicare Supplement Insurance (Medigap) Policies 12
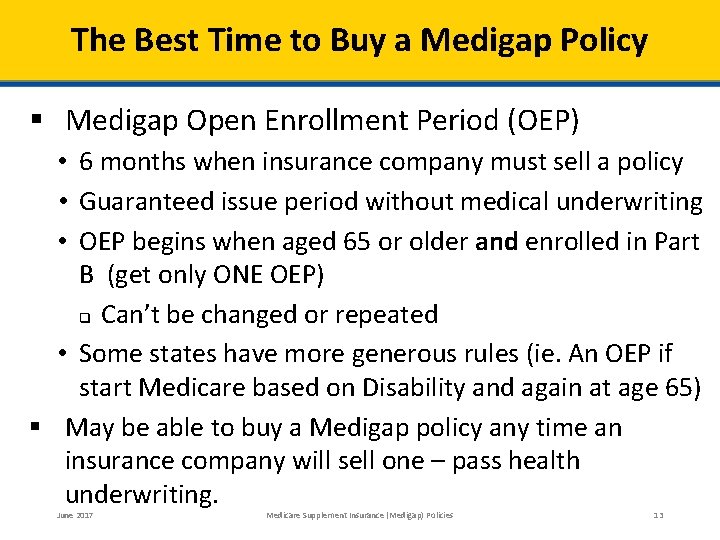
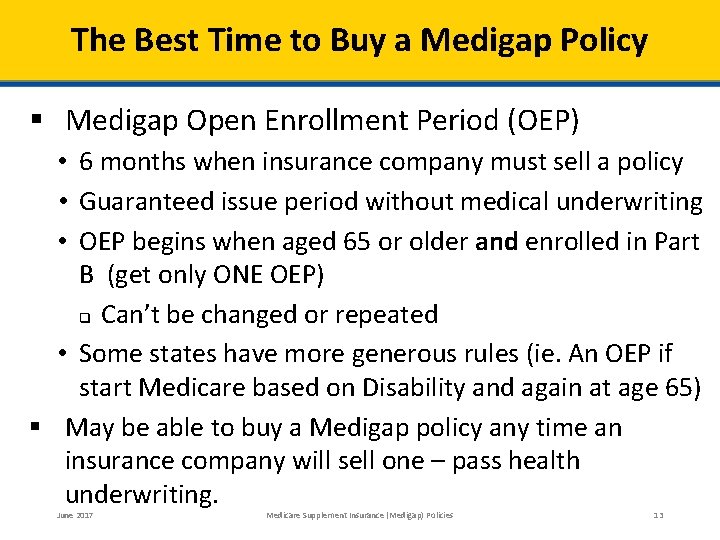
The Best Time to Buy a Medigap Policy § Medigap Open Enrollment Period (OEP) • 6 months when insurance company must sell a policy • Guaranteed issue period without medical underwriting • OEP begins when aged 65 or older and enrolled in Part B (get only ONE OEP) q Can’t be changed or repeated • Some states have more generous rules (ie. An OEP if start Medicare based on Disability and again at age 65) § May be able to buy a Medigap policy any time an insurance company will sell one – pass health underwriting. June 2017 Medicare Supplement Insurance (Medigap) Policies 13
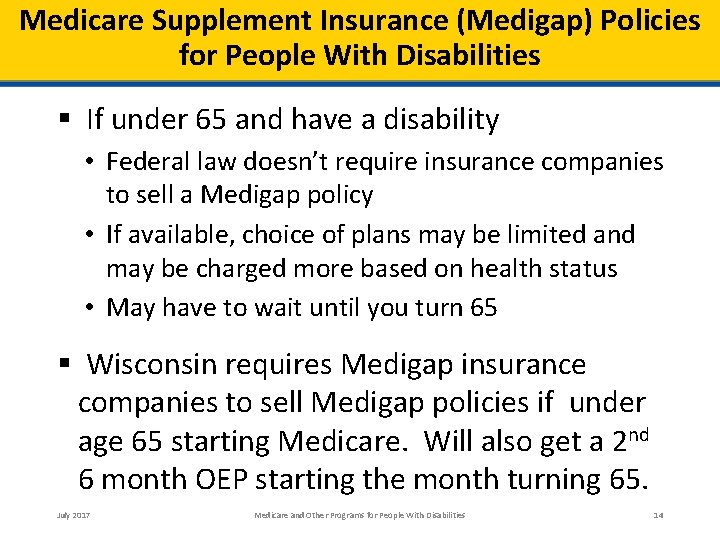
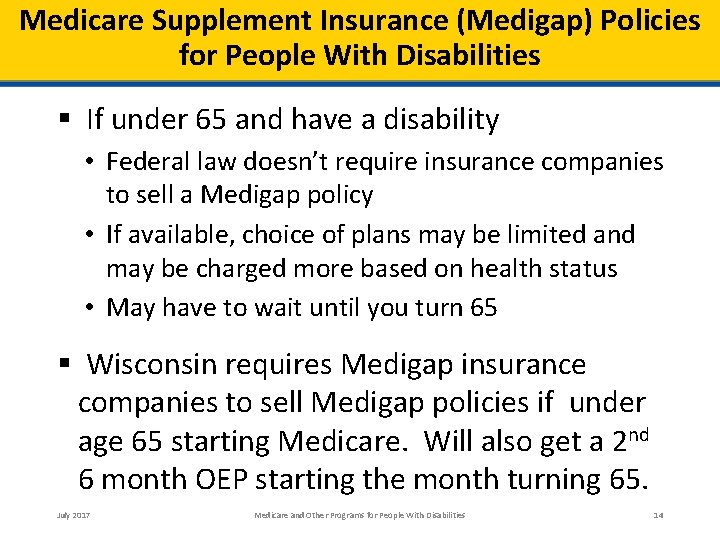
Medicare Supplement Insurance (Medigap) Policies for People With Disabilities § If under 65 and have a disability • Federal law doesn’t require insurance companies to sell a Medigap policy • If available, choice of plans may be limited and may be charged more based on health status • May have to wait until you turn 65 § Wisconsin requires Medigap insurance companies to sell Medigap policies if under age 65 starting Medicare. Will also get a 2 nd 6 month OEP starting the month turning 65. July 2017 Medicare and Other Programs for People With Disabilities 14
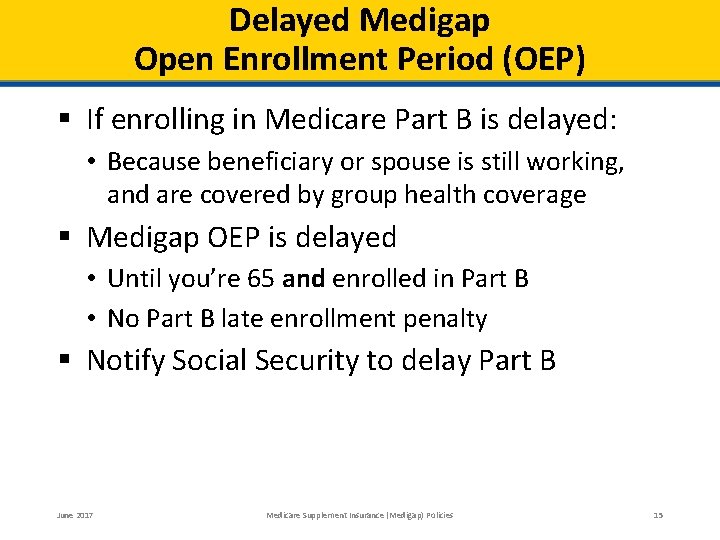
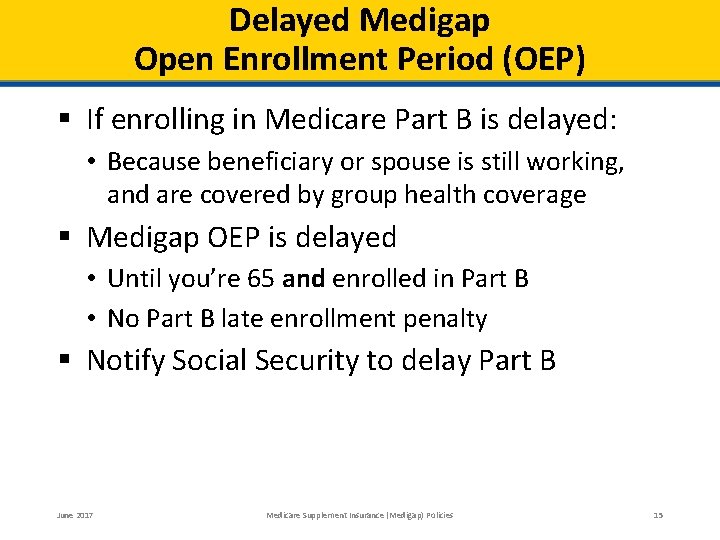
Delayed Medigap Open Enrollment Period (OEP) § If enrolling in Medicare Part B is delayed: • Because beneficiary or spouse is still working, and are covered by group health coverage § Medigap OEP is delayed • Until you’re 65 and enrolled in Part B • No Part B late enrollment penalty § Notify Social Security to delay Part B June 2017 Medicare Supplement Insurance (Medigap) Policies 15
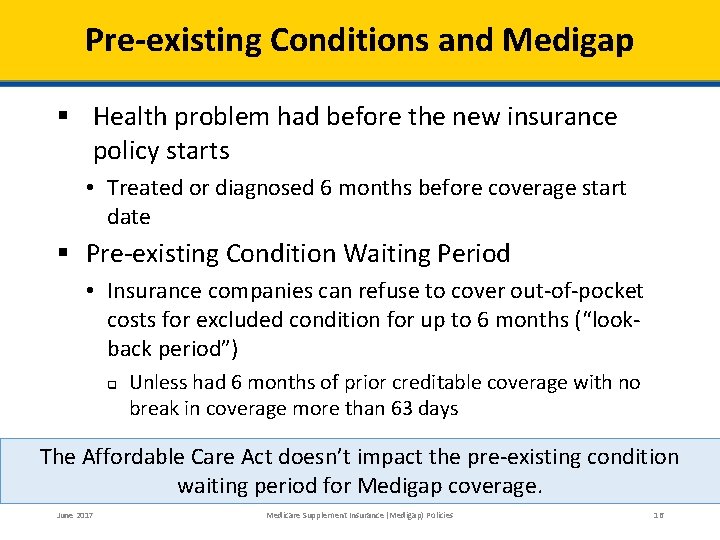
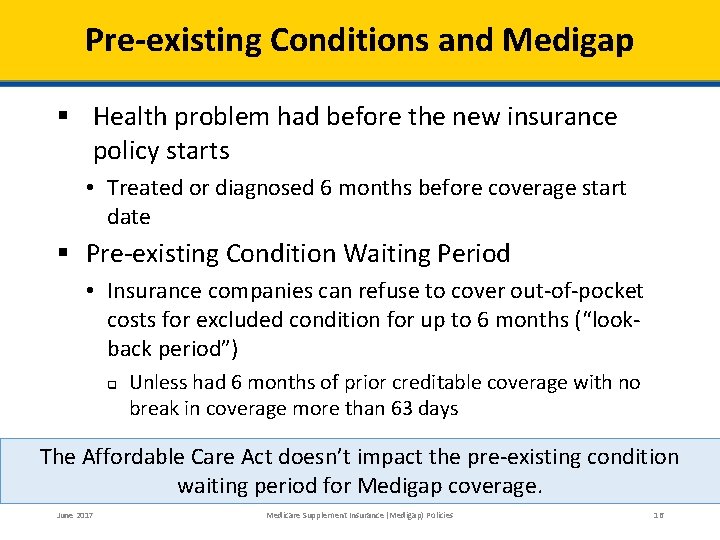
Pre-existing Conditions and Medigap § Health problem had before the new insurance policy starts • Treated or diagnosed 6 months before coverage start date § Pre-existing Condition Waiting Period • Insurance companies can refuse to cover out-of-pocket costs for excluded condition for up to 6 months (“lookback period”) q Unless had 6 months of prior creditable coverage with no break in coverage more than 63 days The Affordable Care Act doesn’t impact the pre-existing condition waiting period for Medigap coverage. June 2017 Medicare Supplement Insurance (Medigap) Policies 16
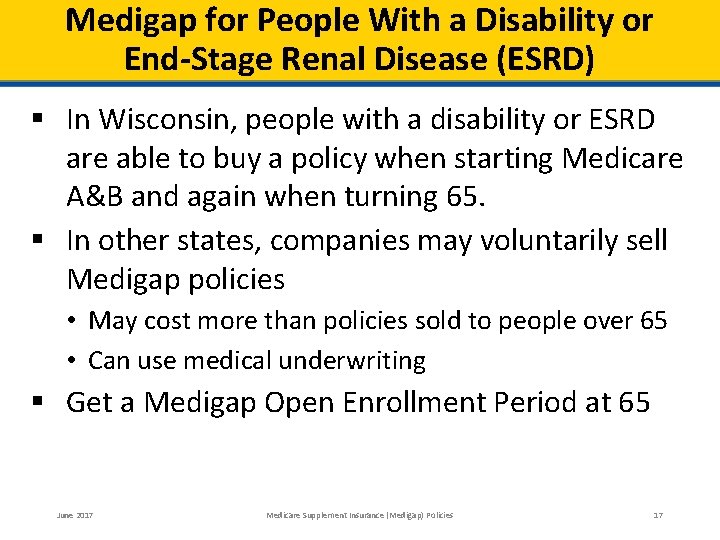
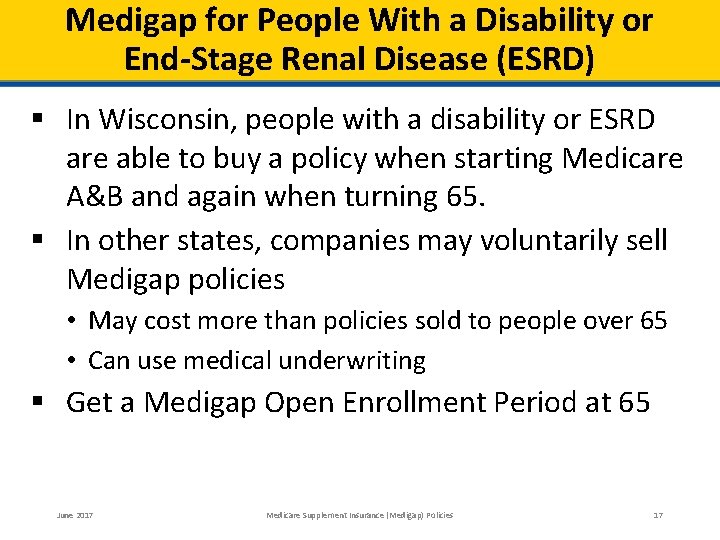
Medigap for People With a Disability or End-Stage Renal Disease (ESRD) § In Wisconsin, people with a disability or ESRD are able to buy a policy when starting Medicare A&B and again when turning 65. § In other states, companies may voluntarily sell Medigap policies • May cost more than policies sold to people over 65 • Can use medical underwriting § Get a Medigap Open Enrollment Period at 65 June 2017 Medicare Supplement Insurance (Medigap) Policies 17
Steps to Buy a Medigap Policy STEP 1: STEP 2: STEP 3: STEP 4: June 2017 Decide which benefits/riders are wanted, then decide which of the Medigap policies meets those needs. Get a listing of the insurance companies selling Medigap policies in the state. Compare costs of the Medigap Policies sold by those insurance companies Buy the Medigap policy Medicare Supplement Insurance (Medigap) Policies 18
Switching Medigap Policies § Might switch policies if: • • • Want to change insurance companies Find a cheaper policy May pay more for the new policy There will be medical underwriting Could have a delay in coverage for a pre-existing condition § When you buy a new Medigap policy • You’ll have a 30 -day “free-look period” q You’ll need to pay both Medigap policy premiums June 2017 Medicare Supplement Insurance (Medigap) Policies 19
Medigap Guaranteed Issue Rights § Federal protections in certain situations • • Companies must sell a Medigap policy All pre-existing conditions must be covered Can’t be charged a higher premium Must apply within 63 days of date other coverage ends § Wisconsin has added Consumer Protections • Loss of Medicaid (Full Medicaid, QMB, MAPP) Wisconsin gives Guarantee Issue. June 2017 Medicare Supplement Insurance (Medigap) Policies 20
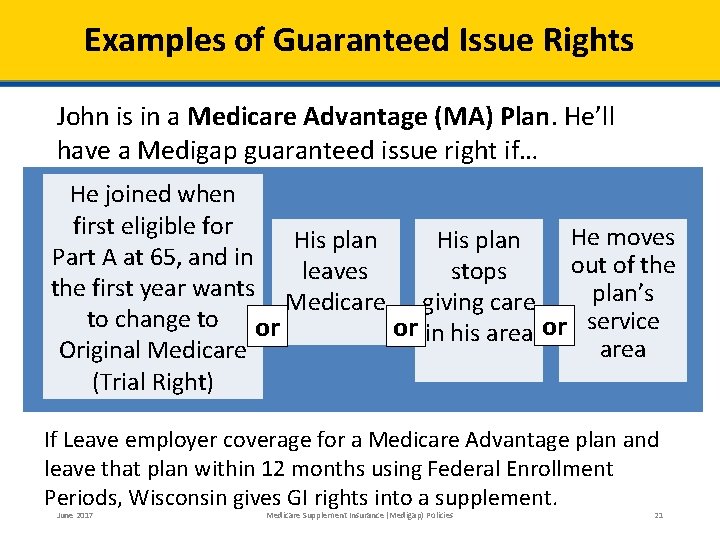
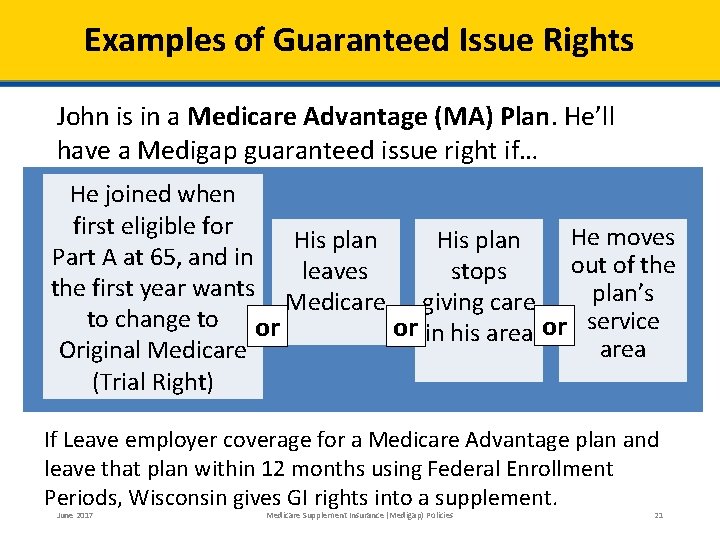
Examples of Guaranteed Issue Rights John is in a Medicare Advantage (MA) Plan. He’ll have a Medigap guaranteed issue right if… He joined when first eligible for He moves His plan Part A at 65, and in out of the leaves stops the first year wants plan’s Medicare giving care to change to or or in his area or service area Original Medicare (Trial Right) If Leave employer coverage for a Medicare Advantage plan and leave that plan within 12 months using Federal Enrollment Periods, Wisconsin gives GI rights into a supplement. June 2017 Medicare Supplement Insurance (Medigap) Policies 21
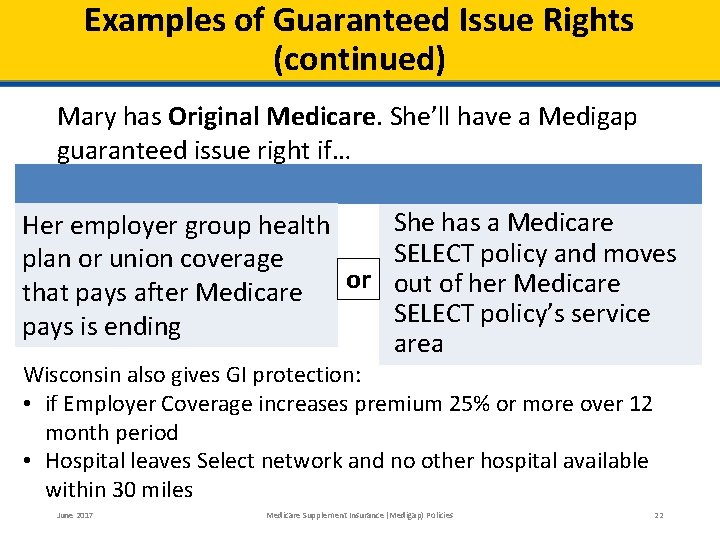
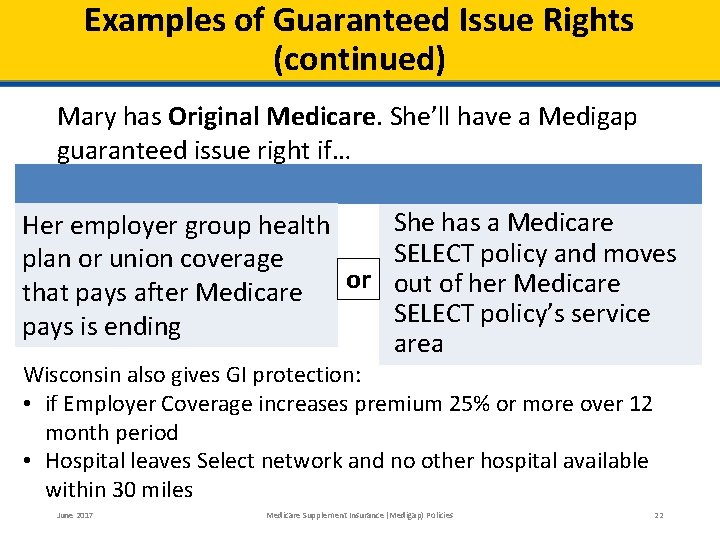
Examples of Guaranteed Issue Rights (continued) Mary has Original Medicare. She’ll have a Medigap guaranteed issue right if… She has a Medicare Her employer group health SELECT policy and moves plan or union coverage or out of her Medicare that pays after Medicare SELECT policy’s service pays is ending area Wisconsin also gives GI protection: • if Employer Coverage increases premium 25% or more over 12 month period • Hospital leaves Select network and no other hospital available within 30 miles June 2017 Medicare Supplement Insurance (Medigap) Policies 22
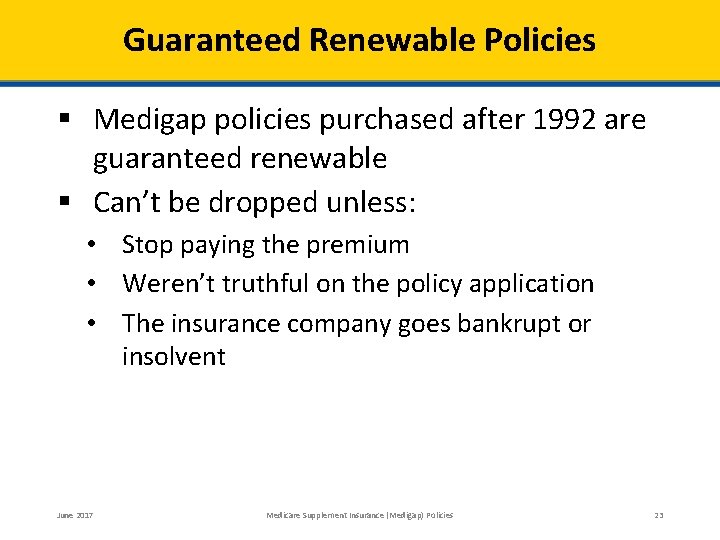
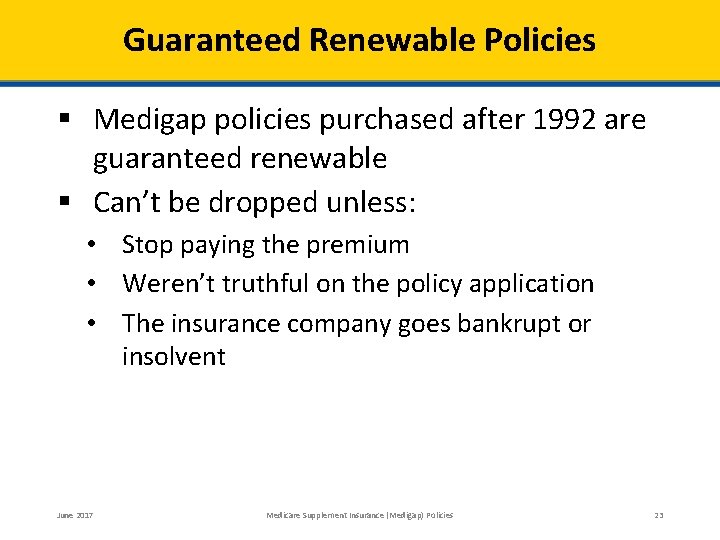
Guaranteed Renewable Policies § Medigap policies purchased after 1992 are guaranteed renewable § Can’t be dropped unless: • Stop paying the premium • Weren’t truthful on the policy application • The insurance company goes bankrupt or insolvent June 2017 Medicare Supplement Insurance (Medigap) Policies 23
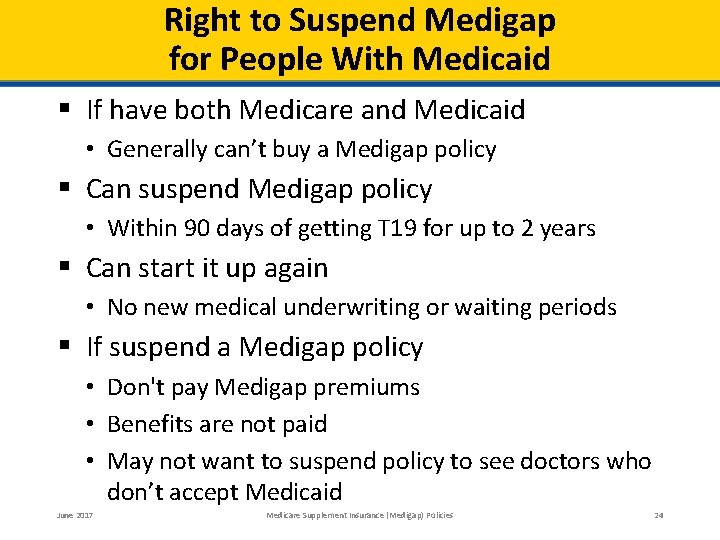
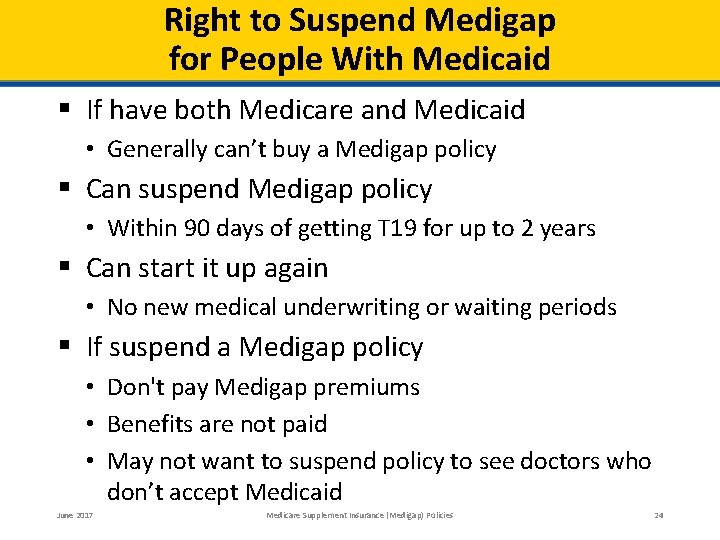
Right to Suspend Medigap for People With Medicaid § If have both Medicare and Medicaid • Generally can’t buy a Medigap policy § Can suspend Medigap policy • Within 90 days of getting T 19 for up to 2 years § Can start it up again • No new medical underwriting or waiting periods § If suspend a Medigap policy • Don't pay Medigap premiums • Benefits are not paid • May not want to suspend policy to see doctors who don’t accept Medicaid June 2017 Medicare Supplement Insurance (Medigap) Policies 24
Right to Suspend Medigap for People Under 65 § Can suspend Medigap policy if under 65 • While enrolled in own or spouse’s employer group health plan § Get Medigap policy back at any time • Must notify insurer within 90 days of losing employer plan • No waiting period June 2017 Medicare Supplement Insurance (Medigap) Policies 25
Medicare Advantage Plans § Health plans run by private companies that provide Part A and Part B benefits • • Part of the Medicare Program Approved by Medicare Most plans include prescription drug coverage—Part D May provide vision and dental services (other non. Medicare services) § Sometimes called Part C § Available across the country May 2017 Medicare Advantage and Other Health Plans 26
Medicare Advantage Plans § Medicare pays the plan every month to provide coverage (on average over $800 a month unless on dialysis) • Provides Medicare-covered benefits • Have Medicare rights and protections § May have to use in-network doctors/ hospitals § May differ from Original Medicare—cost sharing (copays/coinsurance) § If the plan leaves Medicare, will have Consumer protections: • Join another MA Plan, or • Return to Original Medicare (GI for a Medigap) May 2017 Medicare Advantage and Other Health Plans 27
Medicare Advantage Plan Costs § Need to pay the monthly Part B premium • A few plans may pay all or part of Part B premium • State assistance is available for some § May pay an additional monthly premium to the plan § Plan deductibles, coinsurance, and copayments • Different from Original Medicare • Vary from plan to plan • May have higher costs if out-of-network May 2017 Medicare Advantage and Other Health Plans 28
Joining a Medicare Advantage Plan § To be eligible, the beneficiary must Be enrolled in Medicare Part A (Hospital Insurance) Be enrolled in Medicare Part B (Medical Insurance) Live in the plan’s service area Be a United States (U. S. ) citizen or lawfully present in the U. S. • Not be incarcerated • • § To join must also • Provide necessary information to the plan • Follow the plan’s rules • Only belong to one plan at a time May 2017 Medicare Advantage and Other Health Plans 29
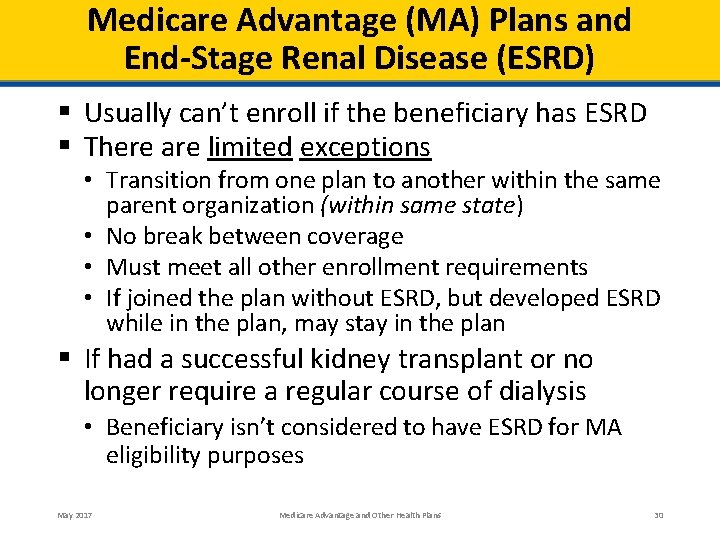
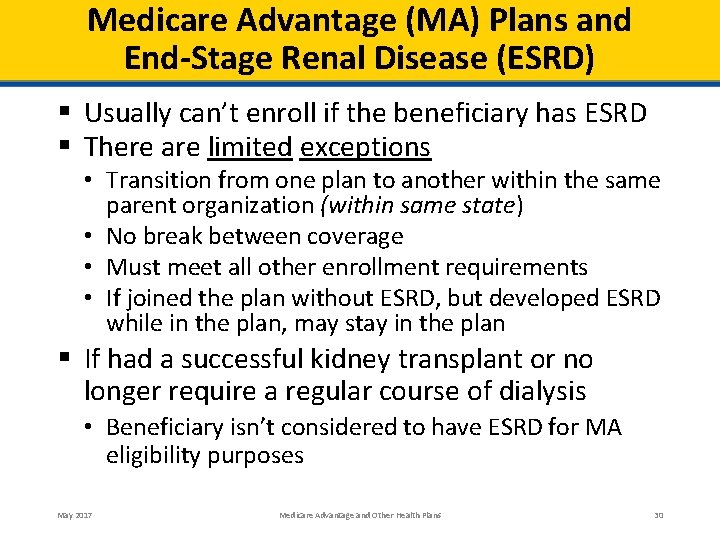
Medicare Advantage (MA) Plans and End-Stage Renal Disease (ESRD) § Usually can’t enroll if the beneficiary has ESRD § There are limited exceptions • Transition from one plan to another within the same parent organization (within same state) • No break between coverage • Must meet all other enrollment requirements • If joined the plan without ESRD, but developed ESRD while in the plan, may stay in the plan § If had a successful kidney transplant or no longer require a regular course of dialysis • Beneficiary isn’t considered to have ESRD for MA eligibility purposes May 2017 Medicare Advantage and Other Health Plans 30
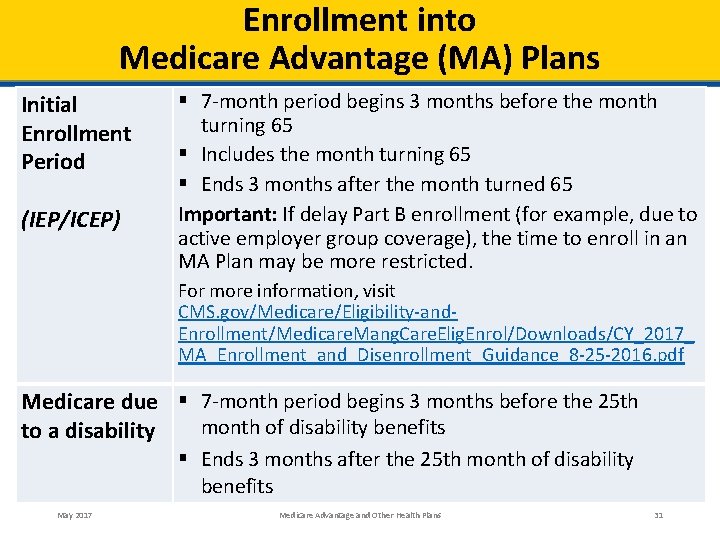
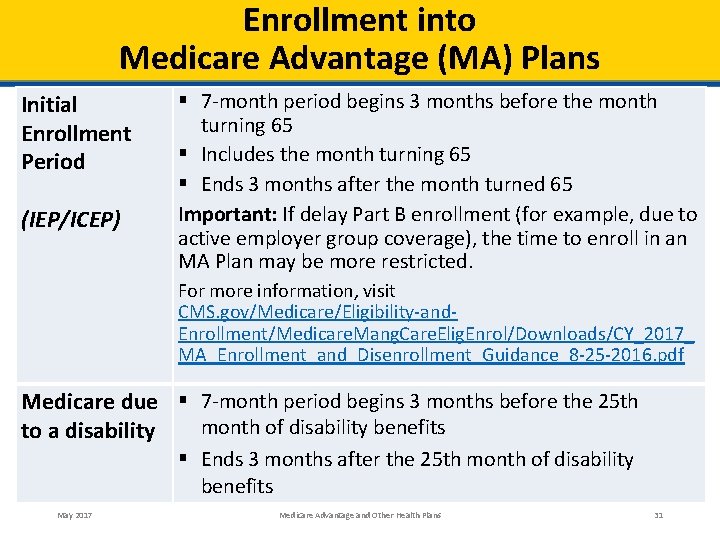
Enrollment into Medicare Advantage (MA) Plans Initial Enrollment Period (IEP/ICEP) § 7 -month period begins 3 months before the month turning 65 § Includes the month turning 65 § Ends 3 months after the month turned 65 Important: If delay Part B enrollment (for example, due to active employer group coverage), the time to enroll in an MA Plan may be more restricted. For more information, visit CMS. gov/Medicare/Eligibility-and. Enrollment/Medicare. Mang. Care. Elig. Enrol/Downloads/CY_2017_ MA_Enrollment_and_Disenrollment_Guidance_8 -25 -2016. pdf Medicare due § 7 -month period begins 3 months before the 25 th month of disability benefits to a disability § Ends 3 months after the 25 th month of disability benefits May 2017 Medicare Advantage and Other Health Plans 31
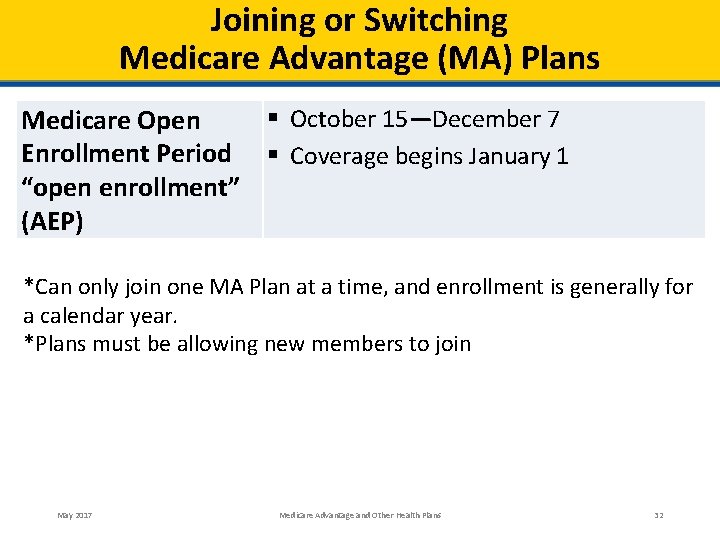
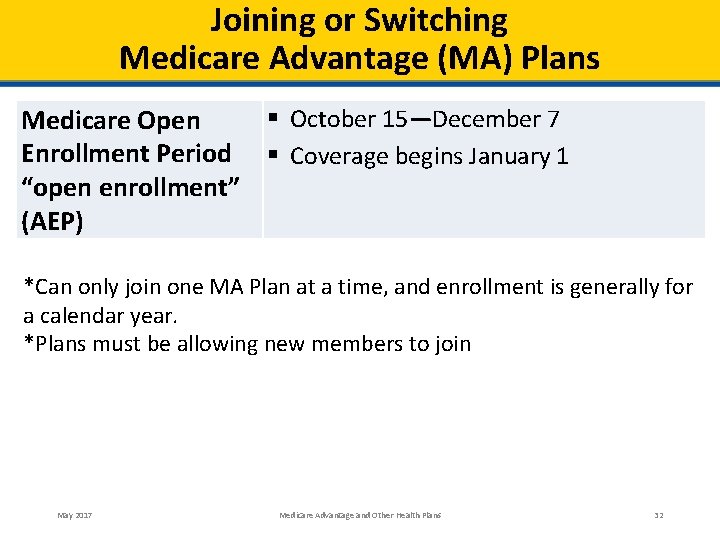
Joining or Switching Medicare Advantage (MA) Plans § October 15—December 7 Medicare Open Enrollment Period § Coverage begins January 1 “open enrollment” (AEP) *Can only join one MA Plan at a time, and enrollment is generally for a calendar year. *Plans must be allowing new members to join May 2017 Medicare Advantage and Other Health Plans 32
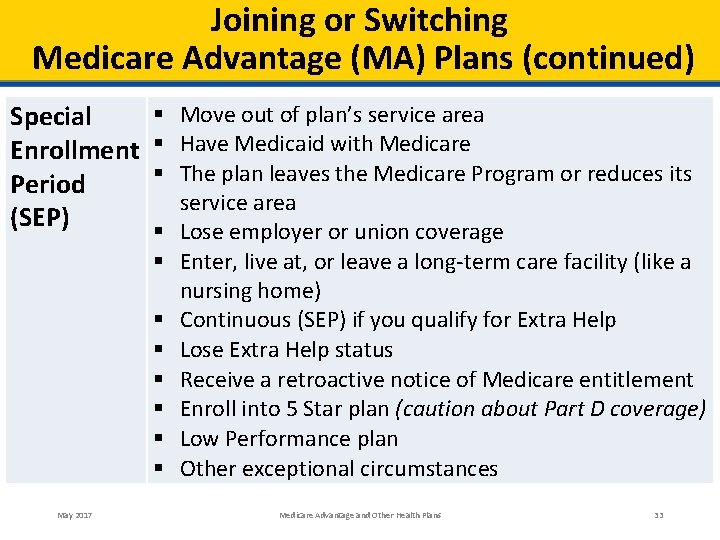
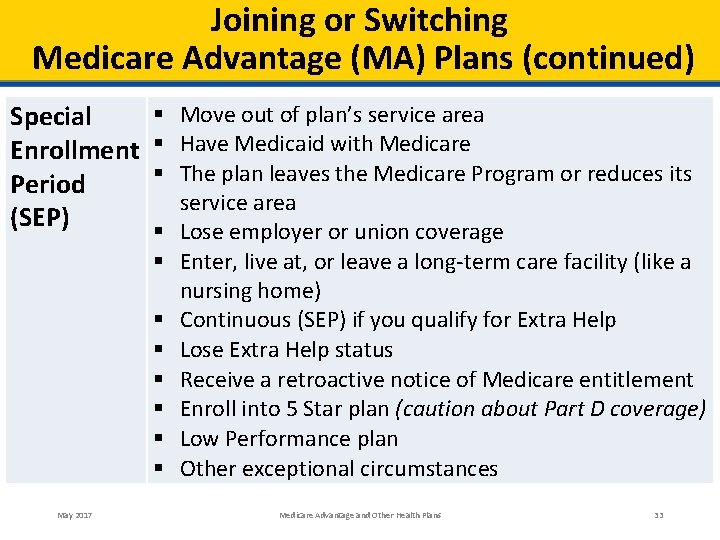
Joining or Switching Medicare Advantage (MA) Plans (continued) Special Enrollment Period (SEP) May 2017 § Move out of plan’s service area § Have Medicaid with Medicare § The plan leaves the Medicare Program or reduces its service area § Lose employer or union coverage § Enter, live at, or leave a long-term care facility (like a nursing home) § Continuous (SEP) if you qualify for Extra Help § Lose Extra Help status § Receive a retroactive notice of Medicare entitlement § Enroll into 5 Star plan (caution about Part D coverage) § Low Performance plan § Other exceptional circumstances Medicare Advantage and Other Health Plans 33
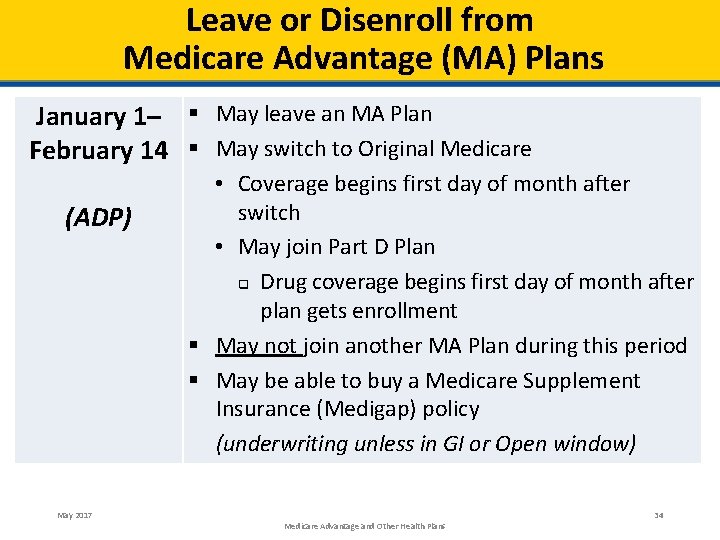
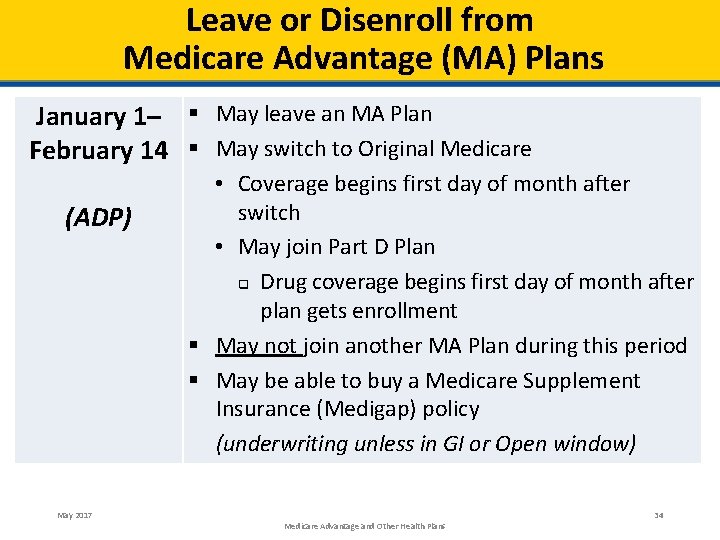
Leave or Disenroll from Medicare Advantage (MA) Plans January 1– § May leave an MA Plan February 14 § May switch to Original Medicare (ADP) May 2017 • Coverage begins first day of month after switch • May join Part D Plan q Drug coverage begins first day of month after plan gets enrollment § May not join another MA Plan during this period § May be able to buy a Medicare Supplement Insurance (Medigap) policy (underwriting unless in GI or Open window) Medicare Advantage and Other Health Plans 34
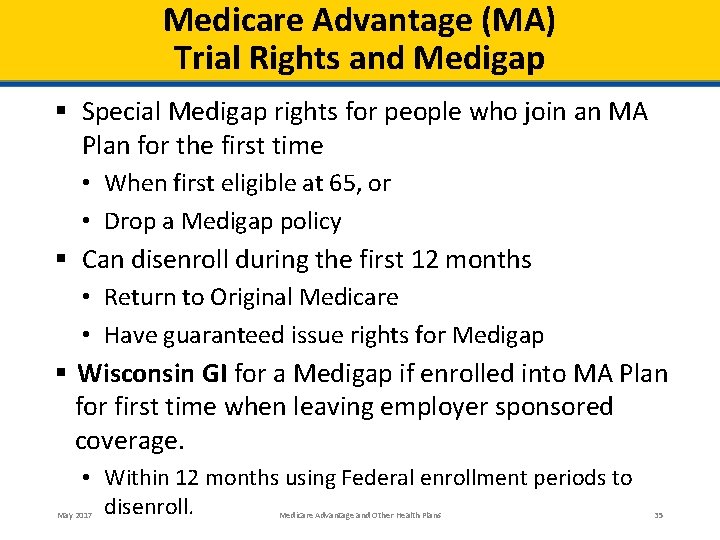
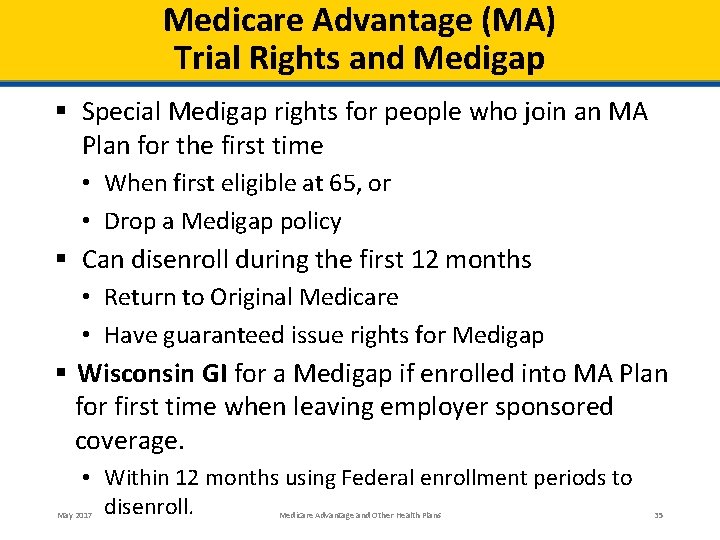
Medicare Advantage (MA) Trial Rights and Medigap § Special Medigap rights for people who join an MA Plan for the first time • When first eligible at 65, or • Drop a Medigap policy § Can disenroll during the first 12 months • Return to Original Medicare • Have guaranteed issue rights for Medigap § Wisconsin GI for a Medigap if enrolled into MA Plan for first time when leaving employer sponsored coverage. • Within 12 months using Federal enrollment periods to disenroll. May 2017 Medicare Advantage and Other Health Plans 35
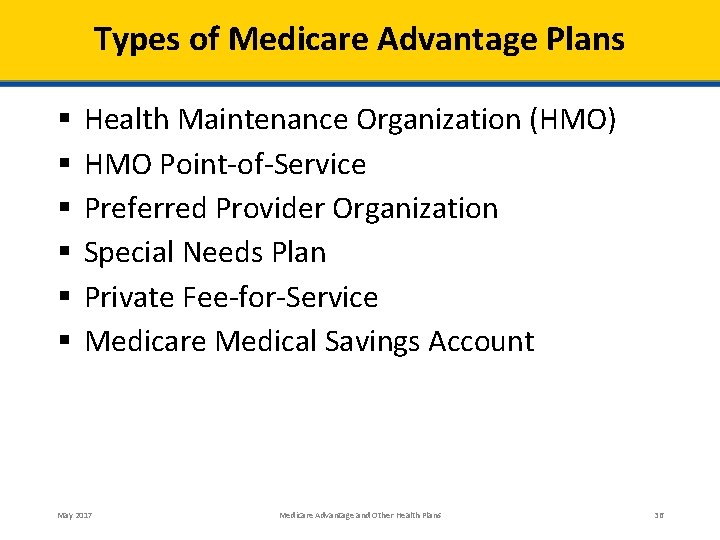
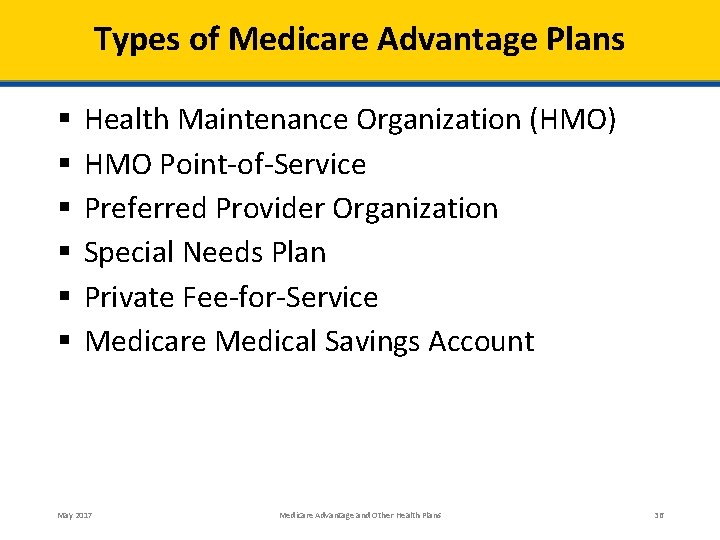
Types of Medicare Advantage Plans § § § Health Maintenance Organization (HMO) HMO Point-of-Service Preferred Provider Organization Special Needs Plan Private Fee-for-Service Medicare Medical Savings Account May 2017 Medicare Advantage and Other Health Plans 36
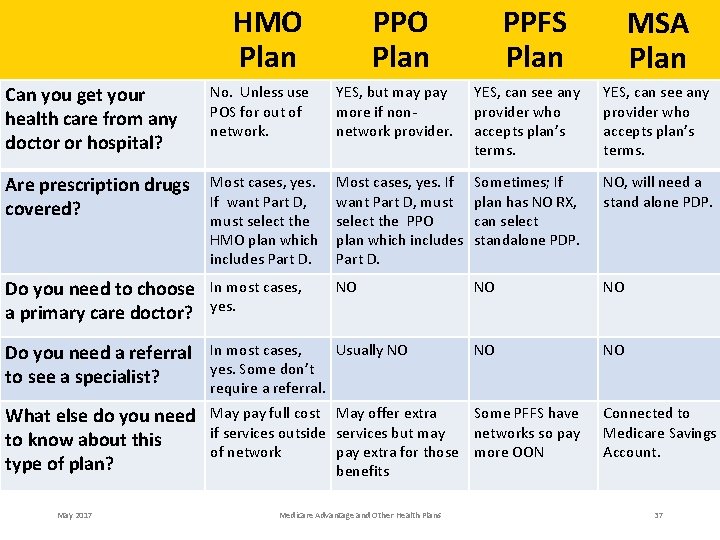
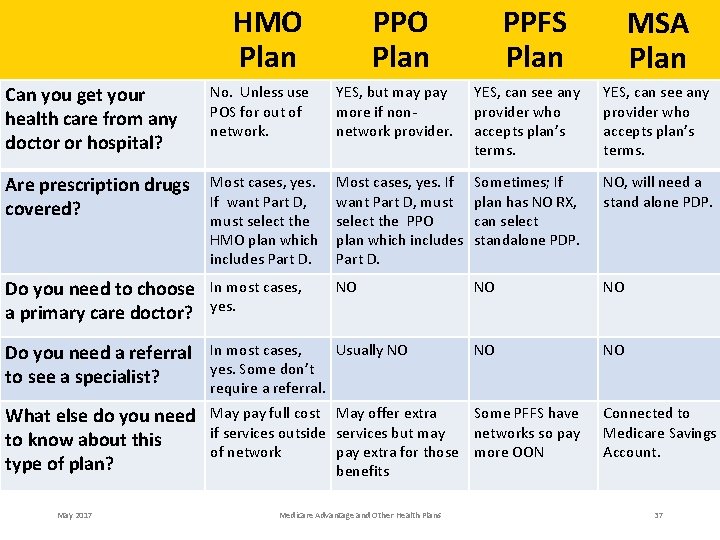
PPO Plan HMO Plan PPFS Plan MSA Plan Can you get your health care from any doctor or hospital? No. Unless use POS for out of network. YES, but may pay more if nonnetwork provider. YES, can see any provider who accepts plan’s terms. Are prescription drugs covered? Most cases, yes. If want Part D, must select the HMO plan which includes Part D. Most cases, yes. If want Part D, must select the PPO plan which includes Part D. Sometimes; If plan has NO RX, can select standalone PDP. NO, will need a stand alone PDP. Do you need to choose a primary care doctor? In most cases, yes. NO NO NO Do you need a referral to see a specialist? In most cases, Usually NO yes. Some don’t require a referral. NO NO What else do you need to know about this type of plan? May pay full cost May offer extra Some PFFS have if services outside services but may networks so pay of network pay extra for those more OON benefits May 2017 Medicare Advantage and Other Health Plans Connected to Medicare Savings Account. 37
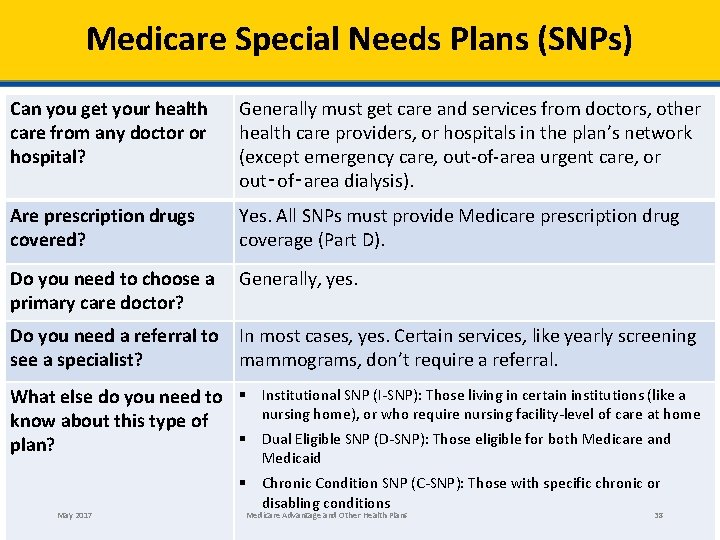
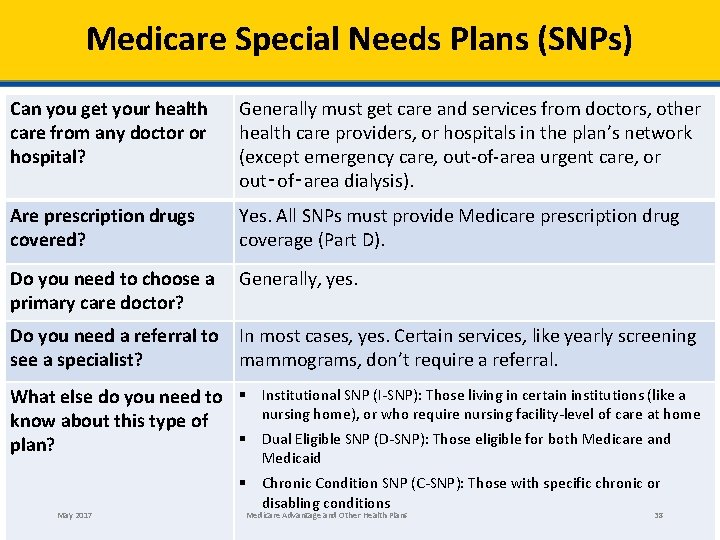
Medicare Special Needs Plans (SNPs) Can you get your health care from any doctor or hospital? Generally must get care and services from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out‑of‑area dialysis). Are prescription drugs covered? Yes. All SNPs must provide Medicare prescription drug coverage (Part D). Do you need to choose a primary care doctor? Generally, yes. Do you need a referral to see a specialist? In most cases, yes. Certain services, like yearly screening mammograms, don’t require a referral. What else do you need to § know about this type of § plan? May 2017 Institutional SNP (I-SNP): Those living in certain institutions (like a nursing home), or who require nursing facility-level of care at home Dual Eligible SNP (D-SNP): Those eligible for both Medicare and Medicaid § Chronic Condition SNP (C-SNP): Those with specific chronic or disabling conditions Medicare Advantage and Other Health Plans 38
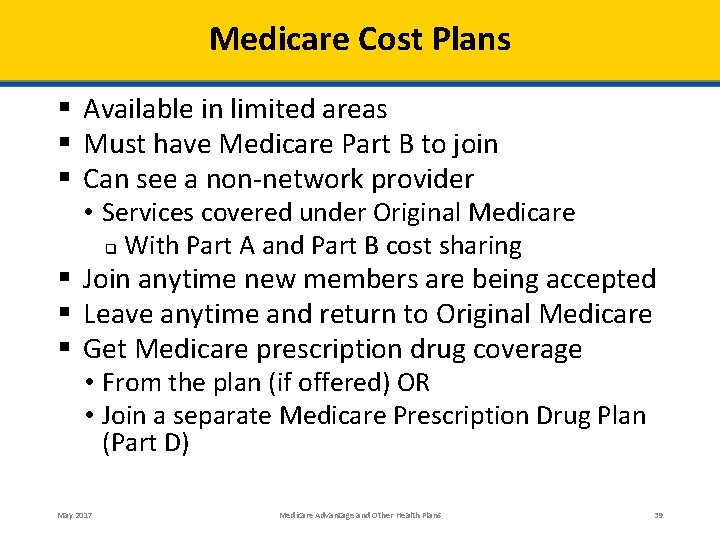
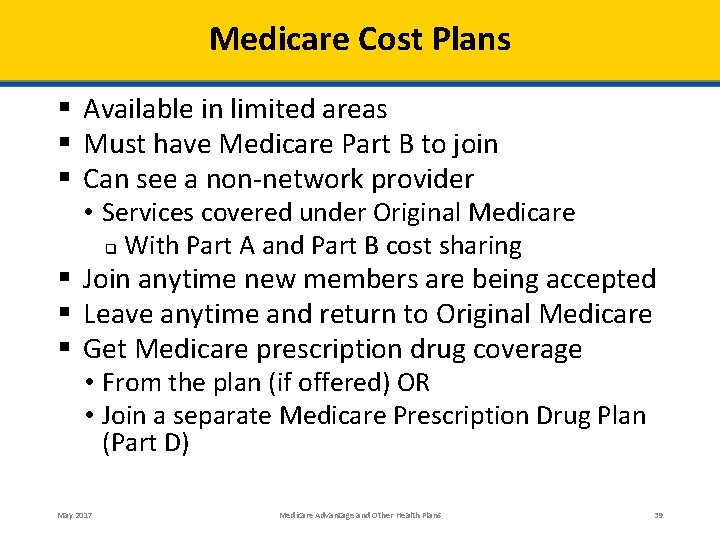
Medicare Cost Plans § Available in limited areas § Must have Medicare Part B to join § Can see a non-network provider • Services covered under Original Medicare q With Part A and Part B cost sharing § Join anytime new members are being accepted § Leave anytime and return to Original Medicare § Get Medicare prescription drug coverage • From the plan (if offered) OR • Join a separate Medicare Prescription Drug Plan (Part D) May 2017 Medicare Advantage and Other Health Plans 39
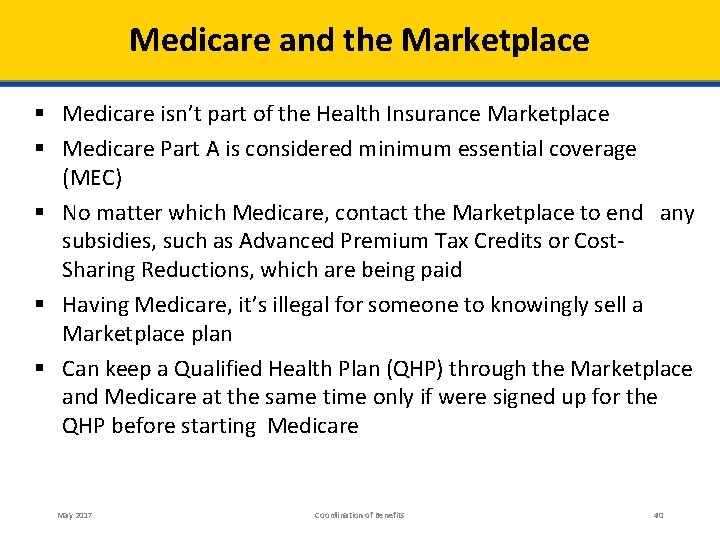
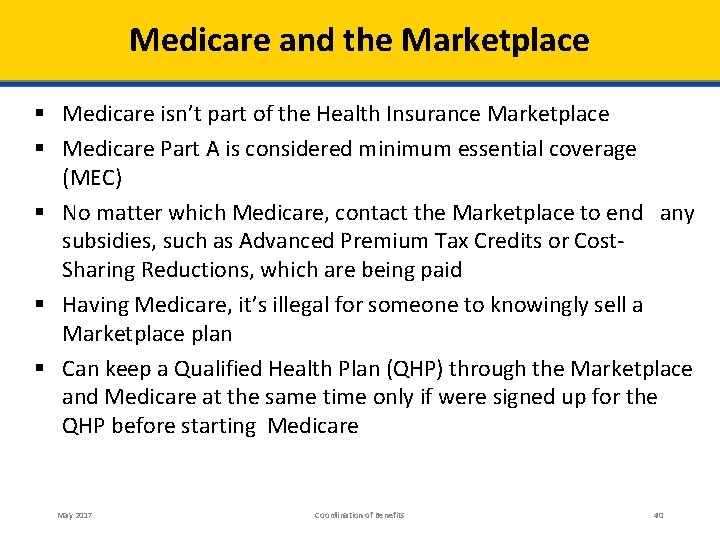
Medicare and the Marketplace § Medicare isn’t part of the Health Insurance Marketplace § Medicare Part A is considered minimum essential coverage (MEC) § No matter which Medicare, contact the Marketplace to end any subsidies, such as Advanced Premium Tax Credits or Cost. Sharing Reductions, which are being paid § Having Medicare, it’s illegal for someone to knowingly sell a Marketplace plan § Can keep a Qualified Health Plan (QHP) through the Marketplace and Medicare at the same time only if were signed up for the QHP before starting Medicare May 2017 Coordination of Benefits 40
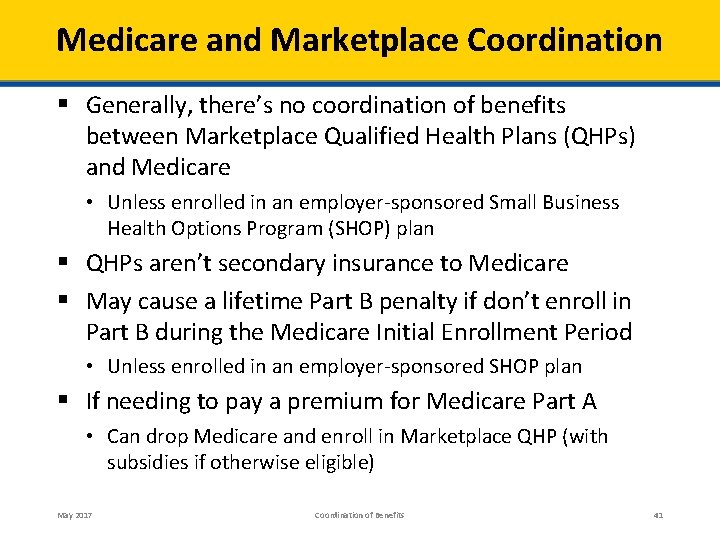
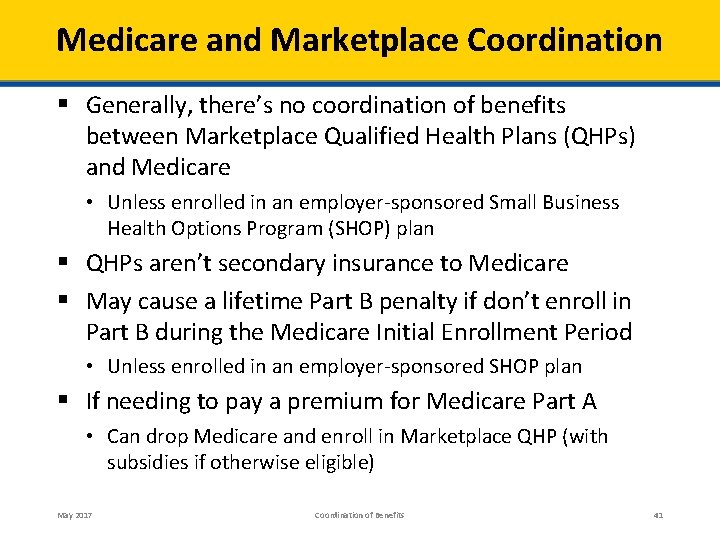
Medicare and Marketplace Coordination § Generally, there’s no coordination of benefits between Marketplace Qualified Health Plans (QHPs) and Medicare • Unless enrolled in an employer-sponsored Small Business Health Options Program (SHOP) plan § QHPs aren’t secondary insurance to Medicare § May cause a lifetime Part B penalty if don’t enroll in Part B during the Medicare Initial Enrollment Period • Unless enrolled in an employer-sponsored SHOP plan § If needing to pay a premium for Medicare Part A • Can drop Medicare and enroll in Marketplace QHP (with subsidies if otherwise eligible) May 2017 Coordination of Benefits 41
Consumers Who Have Premium-Free Medicare Part A, But Not Part B § Consumers who receive a PDM (Periodic Data Matching) notice may have a special opportunity to sign up for Medicare Part B • Must visit their local Social Security office by September 30, 2017, to request enrollment in Medicare Part B o Must show their Medicare PDM notice Note: This opportunity will expire September 30, 2017 July 2017 Medicare and the Marketplace 42
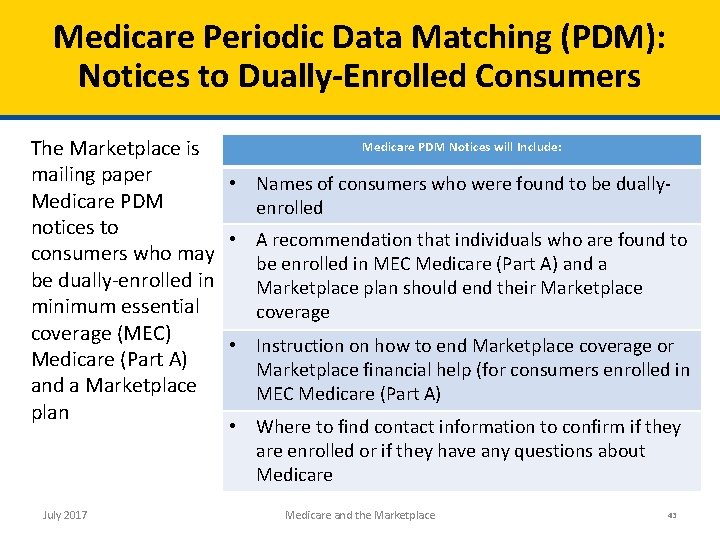
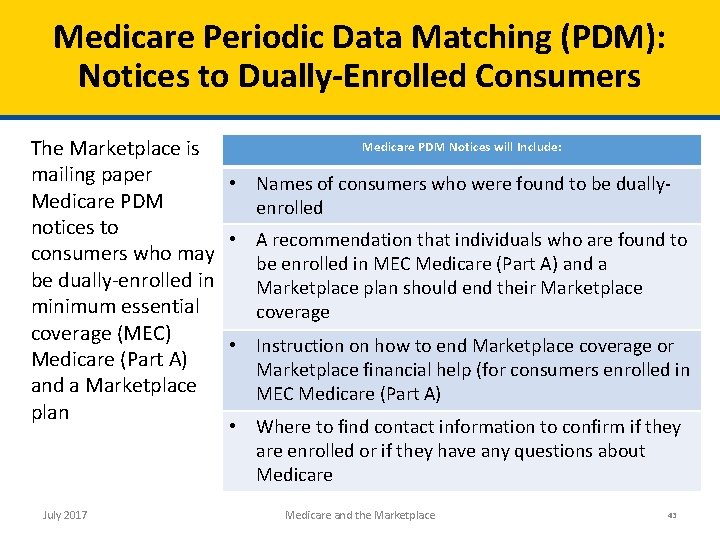
Medicare Periodic Data Matching (PDM): Notices to Dually-Enrolled Consumers Medicare PDM Notices will Include: The Marketplace is mailing paper • Names of consumers who were found to be dually. Medicare PDM enrolled notices to • A recommendation that individuals who are found to consumers who may be enrolled in MEC Medicare (Part A) and a be dually-enrolled in Marketplace plan should end their Marketplace minimum essential coverage (MEC) • Instruction on how to end Marketplace coverage or Medicare (Part A) Marketplace financial help (for consumers enrolled in and a Marketplace MEC Medicare (Part A) plan • Where to find contact information to confirm if they are enrolled or if they have any questions about Medicare July 2017 Medicare and the Marketplace 43
Premium-Free Medicare Part A and Part B—Late Enrollment Penalty Reduction/Removal (Limited) § Consumers who received a PDM notice may be eligible to request that their late enrollment penalty be reduced or removed • Must be currently or previously dually enrolled in Marketplace coverage (with or without APTC) and Medicare Part A and Part B • Must visit their local Social Security office by September 30, 2017, to request removal or reduction of their Medicare Part B penalty o Must show their Medicare PDM notice Note: This opportunity expires September 30, 2017 July 2017 Medicare and the Marketplace 44
Important Retiree Coverage Considerations § Most retiree plans offer generous medical and prescription drug coverage for the entire family • Employer/union must disclose how its plan works with Medicare drug coverage • Talk to your benefits administrator for more information § If you lose your creditable prescription drug coverage, you have 63 days to enroll in a Part D plan without penalty § People who drop retiree drug coverage may • Lose other health coverage • Not be able to get it back • Cause family members to lose their coverage May 2017 Coordination of Benefits 45
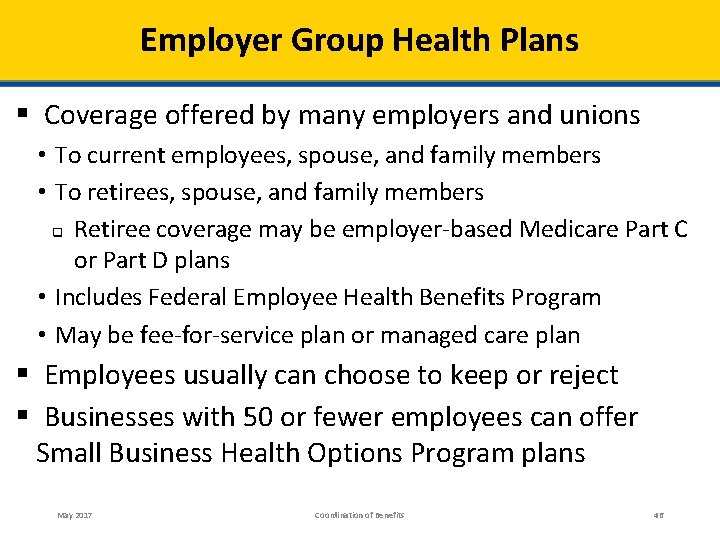
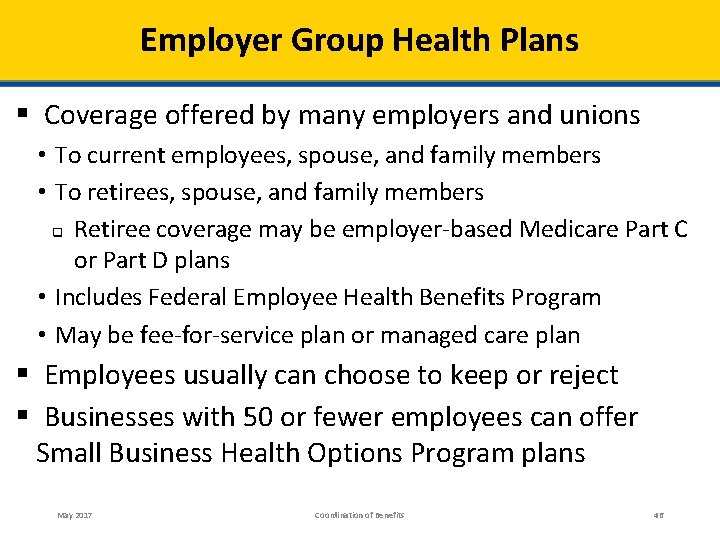
Employer Group Health Plans § Coverage offered by many employers and unions • To current employees, spouse, and family members • To retirees, spouse, and family members q Retiree coverage may be employer-based Medicare Part C or Part D plans • Includes Federal Employee Health Benefits Program • May be fee-for-service plan or managed care plan § Employees usually can choose to keep or reject § Businesses with 50 or fewer employees can offer Small Business Health Options Program plans May 2017 Coordination of Benefits 46
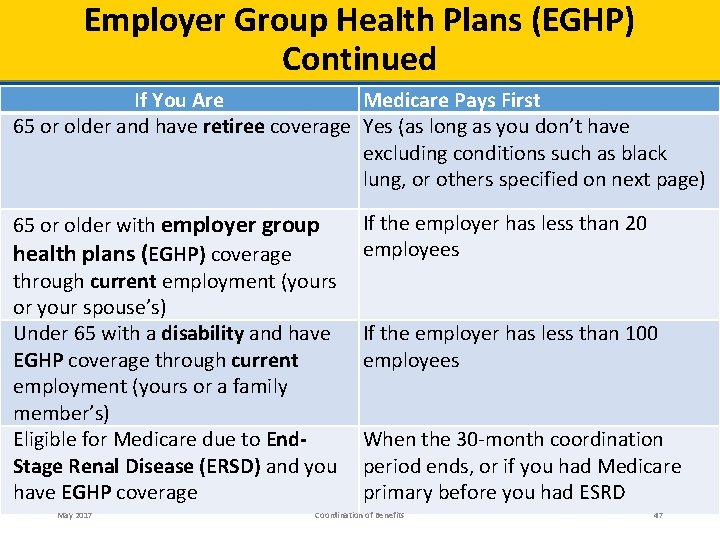
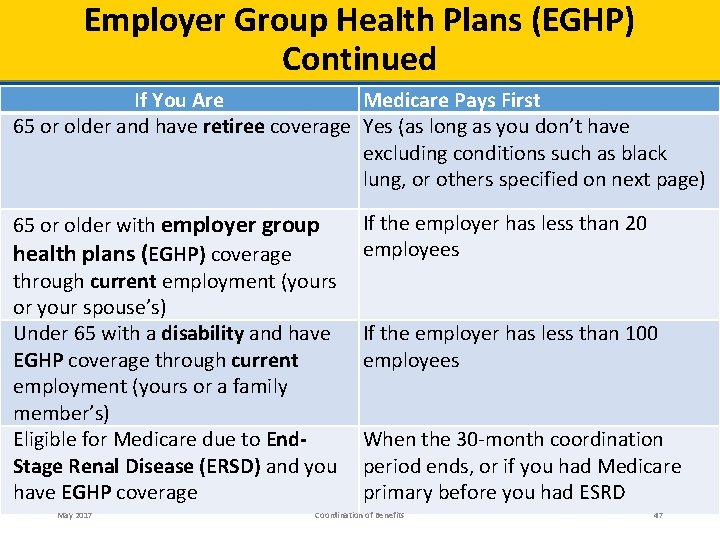
Employer Group Health Plans (EGHP) Continued If You Are Medicare Pays First 65 or older and have retiree coverage Yes (as long as you don’t have excluding conditions such as black lung, or others specified on next page) 65 or older with employer group health plans (EGHP) coverage through current employment (yours or your spouse’s) Under 65 with a disability and have EGHP coverage through current employment (yours or a family member’s) Eligible for Medicare due to End. Stage Renal Disease (ERSD) and you have EGHP coverage May 2017 If the employer has less than 20 employees If the employer has less than 100 employees When the 30 -month coordination period ends, or if you had Medicare primary before you had ESRD Coordination of Benefits 47
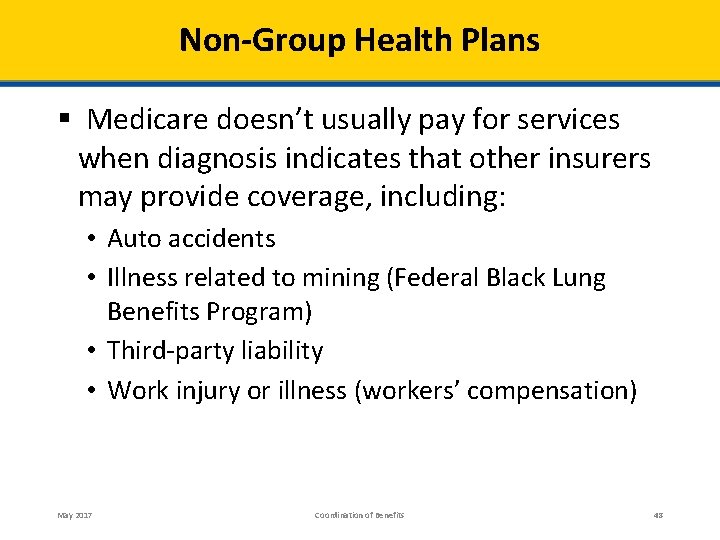
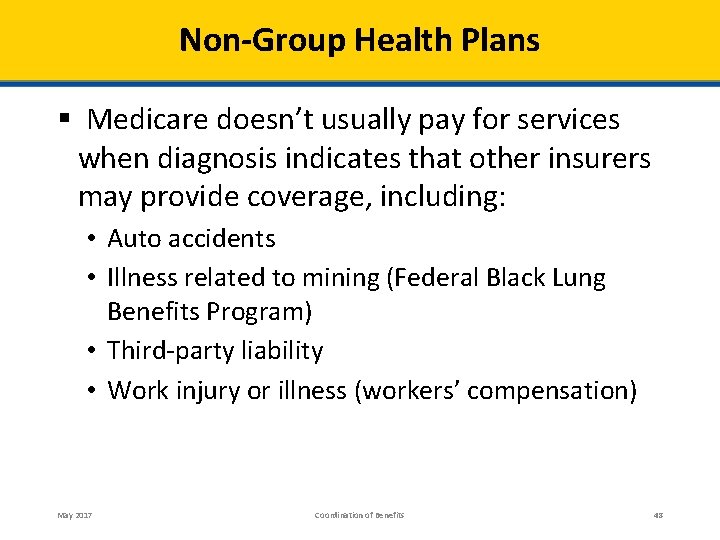
Non-Group Health Plans § Medicare doesn’t usually pay for services when diagnosis indicates that other insurers may provide coverage, including: • Auto accidents • Illness related to mining (Federal Black Lung Benefits Program) • Third-party liability • Work injury or illness (workers’ compensation) May 2017 Coordination of Benefits 48
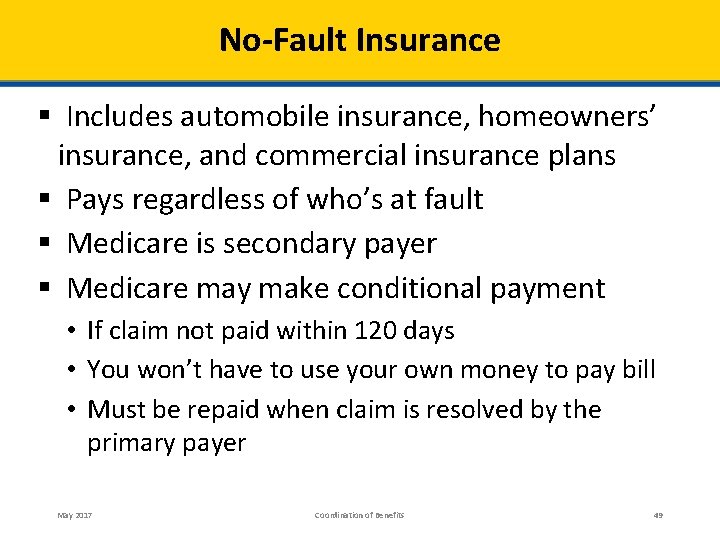
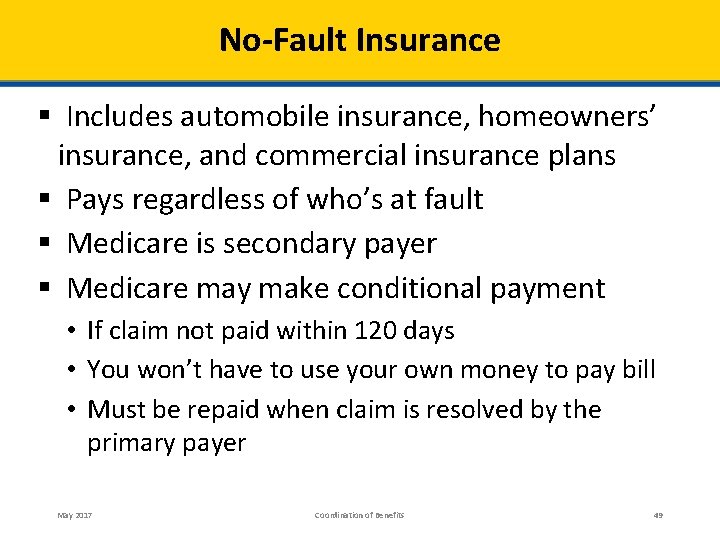
No-Fault Insurance § Includes automobile insurance, homeowners’ insurance, and commercial insurance plans § Pays regardless of who’s at fault § Medicare is secondary payer § Medicare may make conditional payment • If claim not paid within 120 days • You won’t have to use your own money to pay bill • Must be repaid when claim is resolved by the primary payer May 2017 Coordination of Benefits 49
Liability Insurance § Protects against certain claims • Negligence, inappropriate action, or inaction § Medicare is secondary payer • Providers must attempt to collect before billing Medicare § Medicare may make conditional payment • If the liability insurer won’t pay promptly (within 120 days) • Must be repaid when claim is resolved by the primary payer May 2017 Coordination of Benefits 50
Workers’ Compensation § Medicare won’t pay for health care related to workers’ compensation claims § If workers’ compensation claim is denied, claim may be filed for Medicare payment § Workers' compensation claims can be resolved by settlements, judgments, awards, or other payments May 2017 Coordination of Benefits 51
Workers’ Compensation Medicare Set-Aside Arrangement (WCMSA) § Funds to be set aside to pay for future medical or prescription drug services § Funds must be used for the injury, illness, or disease covered by workers’ compensation § Only used for Medicare-covered services § Medicare pays for Medicare-covered services after WCMSA funds are used up May 2017 Coordination of Benefits 52
Federal Black Lung Benefits Program § Covers lung disease/conditions caused by coal mining § Services under this program • Considered workers’ compensation claims • Not covered by Medicare § For more information • Call 1 -800 -638 -7072 • TTY: 1 -877 -889 -5627 May 2017 Coordination of Benefits 53
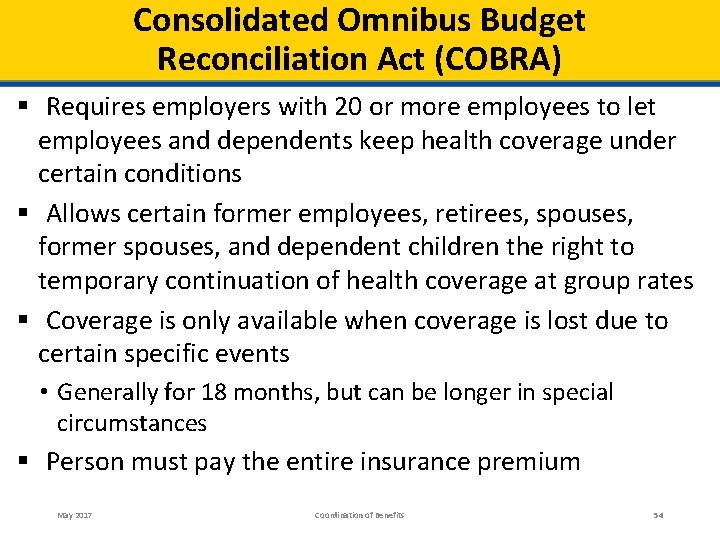
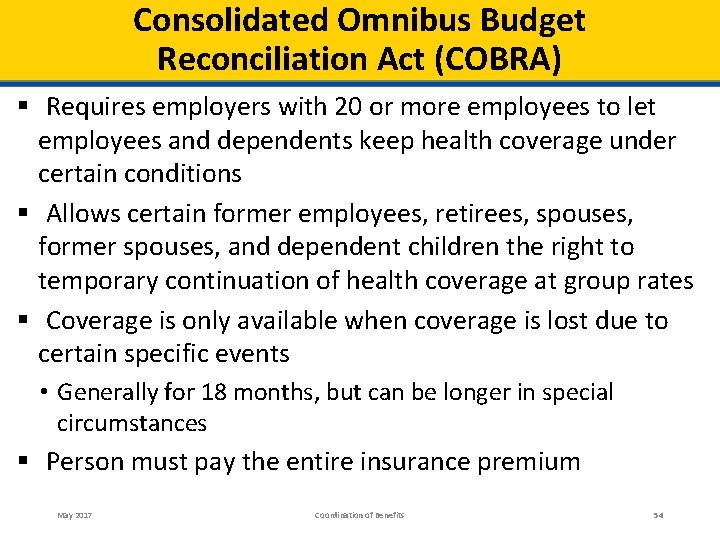
Consolidated Omnibus Budget Reconciliation Act (COBRA) § Requires employers with 20 or more employees to let employees and dependents keep health coverage under certain conditions § Allows certain former employees, retirees, spouses, former spouses, and dependent children the right to temporary continuation of health coverage at group rates § Coverage is only available when coverage is lost due to certain specific events • Generally for 18 months, but can be longer in special circumstances § Person must pay the entire insurance premium May 2017 Coordination of Benefits 54
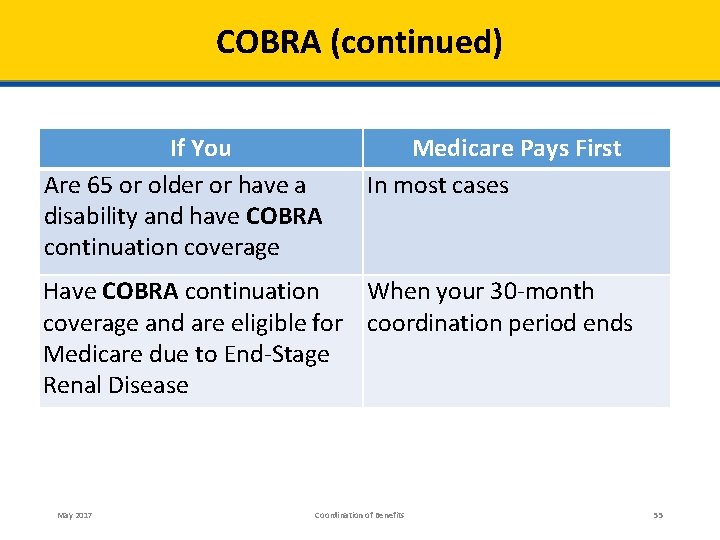
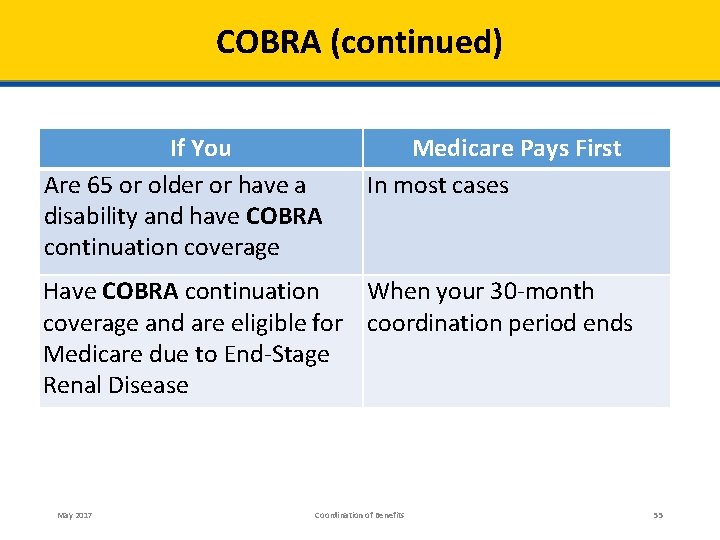
COBRA (continued) If You Are 65 or older or have a disability and have COBRA continuation coverage Medicare Pays First In most cases Have COBRA continuation When your 30 -month coverage and are eligible for coordination period ends Medicare due to End-Stage Renal Disease May 2017 Coordination of Benefits 55
Veterans Affairs (VA) Coverage § If you have Medicare and VA benefits • Can get treatment under either program § Medicare pays when you choose to get your benefits from Medicare § To receive services under VA benefits • You must get your health care at a VA facility, or • Have the VA authorize, or agree to pay for, services in a non-VA facility May 2017 Coordination of Benefits 56
TRICARE for Life Coverage (TFL) § Military retiree coverage for services covered by Medicare and TRICARE for Life (TFL) Medicare pays first/TFL pays remaining § For services covered by TFL but not Medicare • TFL pays first and Medicare pays nothing § For services you get in a military hospital or other federal provider • TFL pays first and Medicare generally pays nothing May 2017 Coordination of Benefits 57
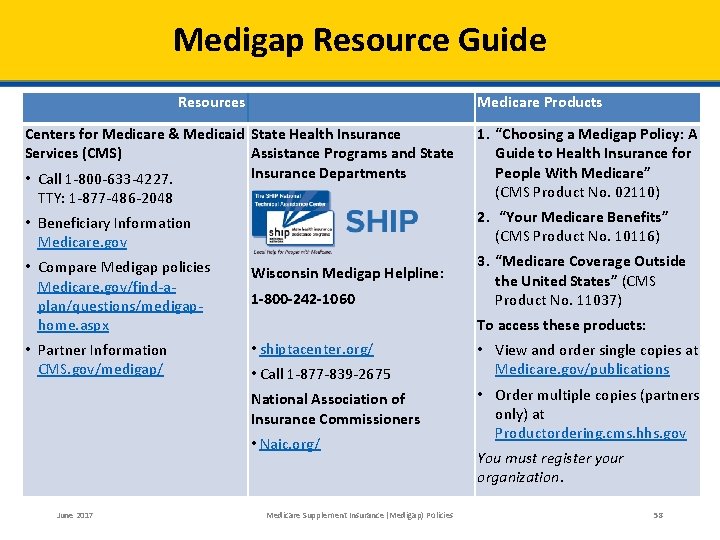
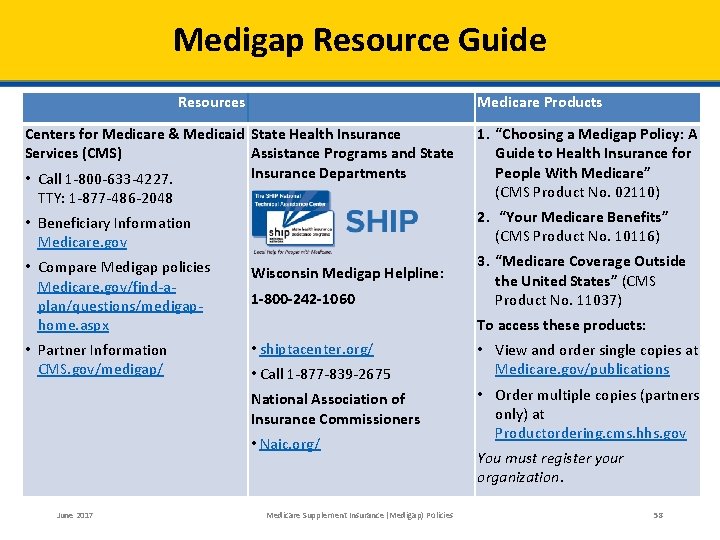
Medigap Resource Guide Resources Medicare Products Centers for Medicare & Medicaid State Health Insurance Services (CMS) Assistance Programs and State Insurance Departments • Call 1 -800 -633 -4227. 1. “Choosing a Medigap Policy: A Guide to Health Insurance for People With Medicare” (CMS Product No. 02110) • Beneficiary Information Medicare. gov 2. “Your Medicare Benefits” (CMS Product No. 10116) TTY: 1 -877 -486 -2048 • Compare Medigap policies Medicare. gov/find-aplan/questions/medigaphome. aspx Wisconsin Medigap Helpline: • Partner Information CMS. gov/medigap/ • shiptacenter. org/ 1 -800 -242 -1060 To access these products: • Call 1 -877 -839 -2675 National Association of Insurance Commissioners • Naic. org/ June 2017 3. “Medicare Coverage Outside the United States” (CMS Product No. 11037) Medicare Supplement Insurance (Medigap) Policies • View and order single copies at Medicare. gov/publications • Order multiple copies (partners only) at Productordering. cms. hhs. gov You must register your organization. 58
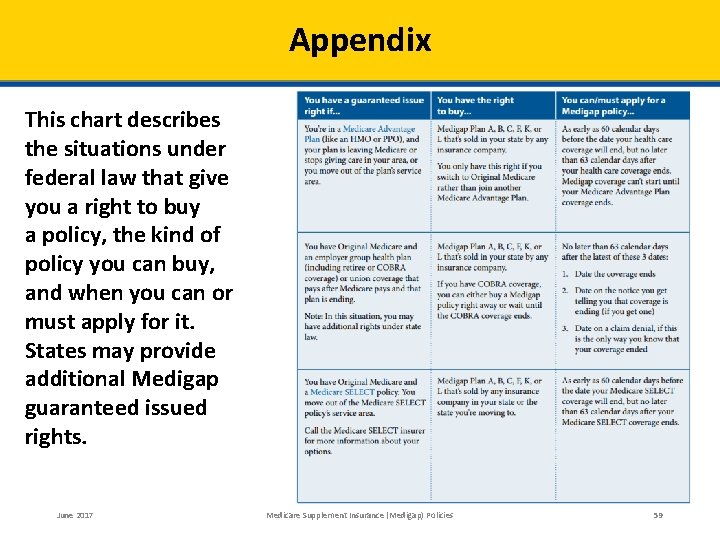
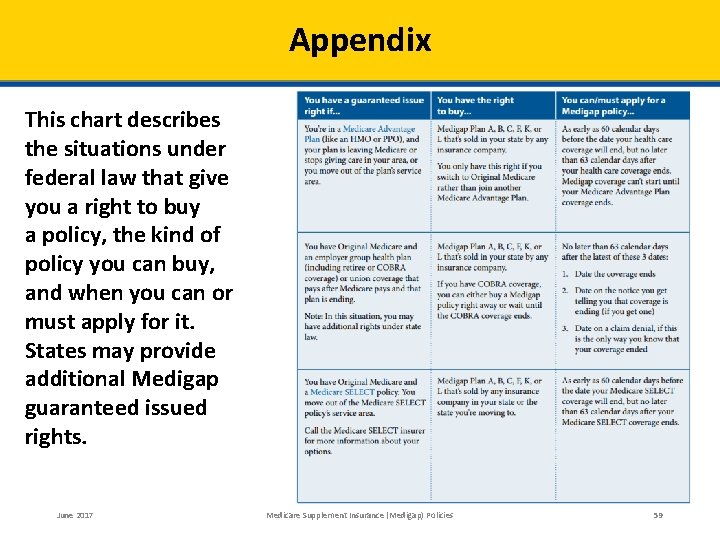
Appendix This chart describes the situations under federal law that give you a right to buy a policy, the kind of policy you can buy, and when you can or must apply for it. States may provide additional Medigap guaranteed issued rights. June 2017 Medicare Supplement Insurance (Medigap) Policies 59
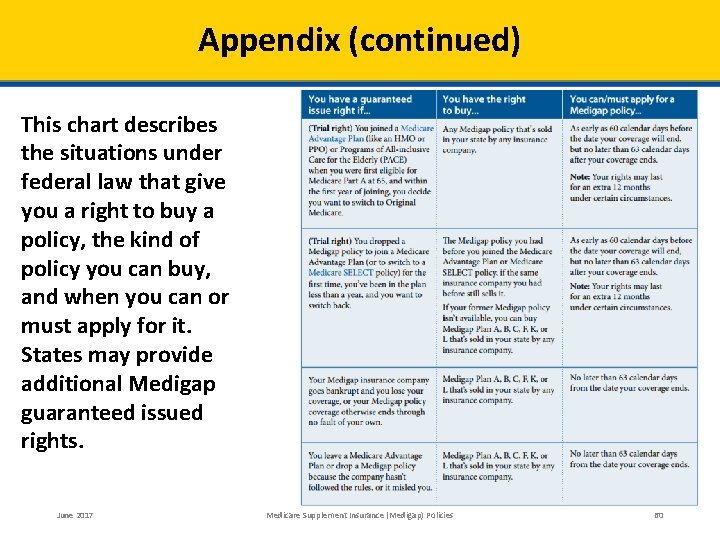
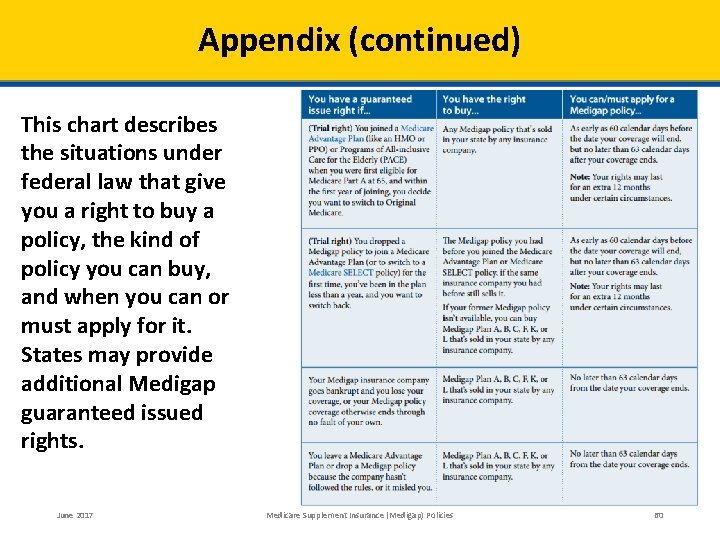
Appendix (continued) This chart describes the situations under federal law that give you a right to buy a policy, the kind of policy you can buy, and when you can or must apply for it. States may provide additional Medigap guaranteed issued rights. June 2017 Medicare Supplement Insurance (Medigap) Policies 60
Acronyms § CHIP Children’s Health Insurance Program § COBRA Consolidated Omnibus Budget Reconciliation Act § CMS Centers for Medicare & Medicaid Services § EGHP Employer Group Health Plan § ESRD End-Stage Renal Disease § HMO Health Maintenance Organization § MA Medicare Advantage § MA-PD Medicare Advantage Prescription Drug June 2017 NTP National Training Program OEP Open Enrollment Period PDP Prescription Drug Plan PPO Preferred Provider Organization § SSA Social Security Administration § SHIP State Health Insurance Assistance Program § TTY Teletypewriter/Text Telephone § § Medicare Supplement Insurance (Medigap) Policies 61

This Training is Provided by the CMS National Training Program (NTP) To view all available NTP training materials, or to subscribe to our email list, visit CMS. gov/outreach-andeducation/training/CMSNational. Training. Program. Stay connected. Contact us at training@cms. hhs. gov, or follow us @CMSGov #CMSNTP June 2017 Medicare Supplement Insurance (Medigap) Policies 62