WCLA MCLE 8 10 11 AMA Guides Section








- Slides: 71
WCLA MCLE 8 -10 -11 • AMA Guides: Section 8. 1 b, Fundamentals & Case Study • Wednesday August 10, 2011 from 11: 45 am to 1: 15 pm • Dr. David Fetter, M. D. • James R. Thompson Center Auditorium, Chicago, IL • 1. 5 Hours General MCLE Credit
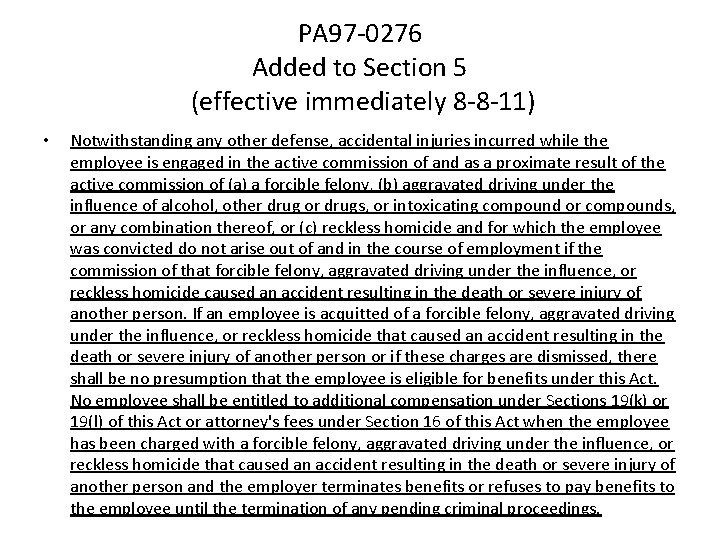
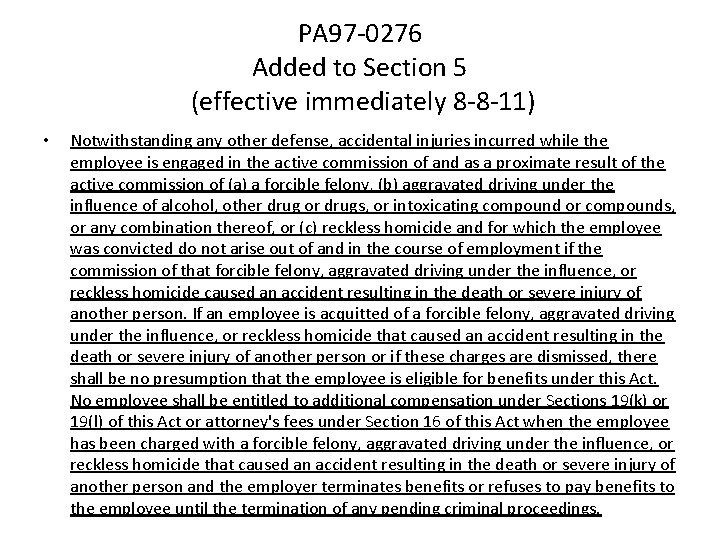
PA 97 -0276 Added to Section 5 (effective immediately 8 -8 -11) • Notwithstanding any other defense, accidental injuries incurred while the employee is engaged in the active commission of and as a proximate result of the active commission of (a) a forcible felony, (b) aggravated driving under the influence of alcohol, other drug or drugs, or intoxicating compound or compounds, or any combination thereof, or (c) reckless homicide and for which the employee was convicted do not arise out of and in the course of employment if the commission of that forcible felony, aggravated driving under the influence, or reckless homicide caused an accident resulting in the death or severe injury of another person. If an employee is acquitted of a forcible felony, aggravated driving under the influence, or reckless homicide that caused an accident resulting in the death or severe injury of another person or if these charges are dismissed, there shall be no presumption that the employee is eligible for benefits under this Act. No employee shall be entitled to additional compensation under Sections 19(k) or 19(l) of this Act or attorney's fees under Section 16 of this Act when the employee has been charged with a forcible felony, aggravated driving under the influence, or reckless homicide that caused an accident resulting in the death or severe injury of another person and the employer terminates benefits or refuses to pay benefits to the employee until the termination of any pending criminal proceedings.
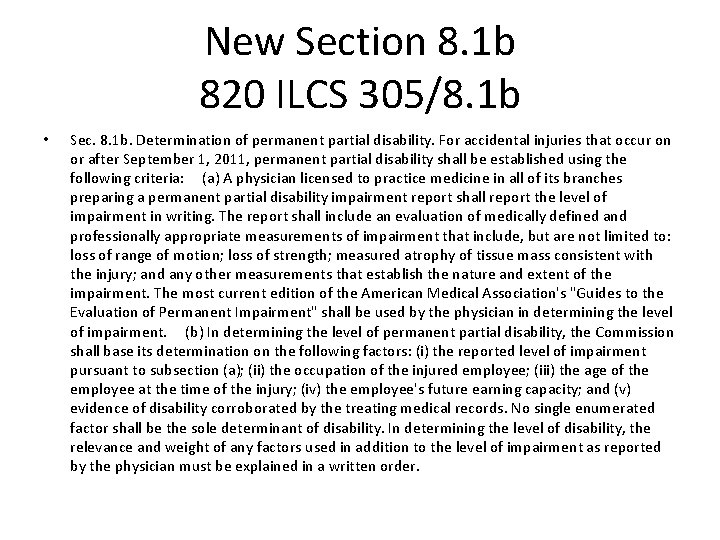
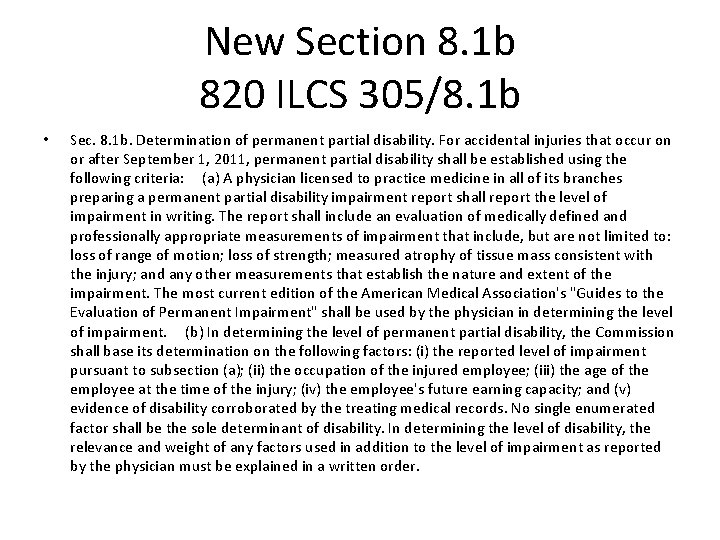
New Section 8. 1 b 820 ILCS 305/8. 1 b • Sec. 8. 1 b. Determination of permanent partial disability. For accidental injuries that occur on or after September 1, 2011, permanent partial disability shall be established using the following criteria: (a) A physician licensed to practice medicine in all of its branches preparing a permanent partial disability impairment report shall report the level of impairment in writing. The report shall include an evaluation of medically defined and professionally appropriate measurements of impairment that include, but are not limited to: loss of range of motion; loss of strength; measured atrophy of tissue mass consistent with the injury; and any other measurements that establish the nature and extent of the impairment. The most current edition of the American Medical Association's "Guides to the Evaluation of Permanent Impairment" shall be used by the physician in determining the level of impairment. (b) In determining the level of permanent partial disability, the Commission shall base its determination on the following factors: (i) the reported level of impairment pursuant to subsection (a); (ii) the occupation of the injured employee; (iii) the age of the employee at the time of the injury; (iv) the employee's future earning capacity; and (v) evidence of disability corroborated by the treating medical records. No single enumerated factor shall be the sole determinant of disability. In determining the level of disability, the relevance and weight of any factors used in addition to the level of impairment as reported by the physician must be explained in a written order.
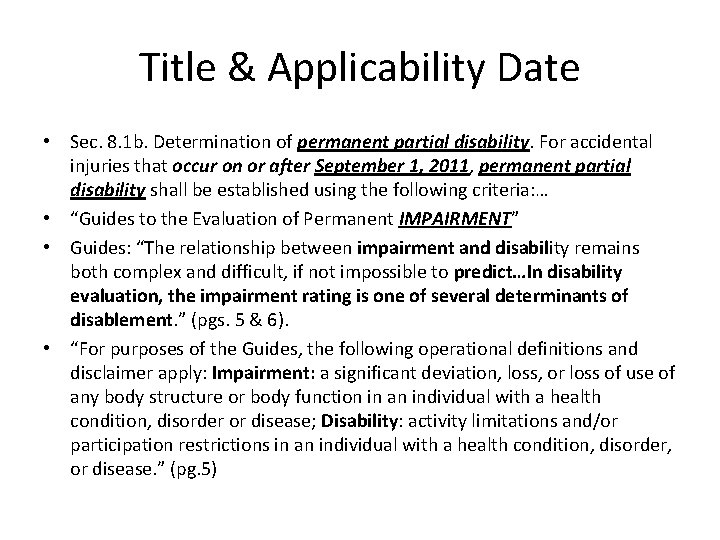
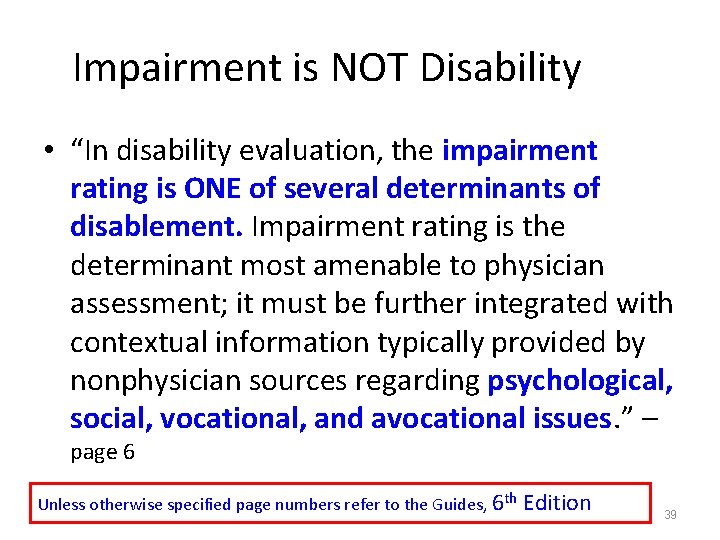
Title & Applicability Date • Sec. 8. 1 b. Determination of permanent partial disability. For accidental injuries that occur on or after September 1, 2011, permanent partial disability shall be established using the following criteria: … • “Guides to the Evaluation of Permanent IMPAIRMENT” • Guides: “The relationship between impairment and disability remains both complex and difficult, if not impossible to predict…In disability evaluation, the impairment rating is one of several determinants of disablement. ” (pgs. 5 & 6). • “For purposes of the Guides, the following operational definitions and disclaimer apply: Impairment: a significant deviation, loss, or loss of use of any body structure or body function in an individual with a health condition, disorder or disease; Disability: activity limitations and/or participation restrictions in an individual with a health condition, disorder, or disease. ” (pg. 5)
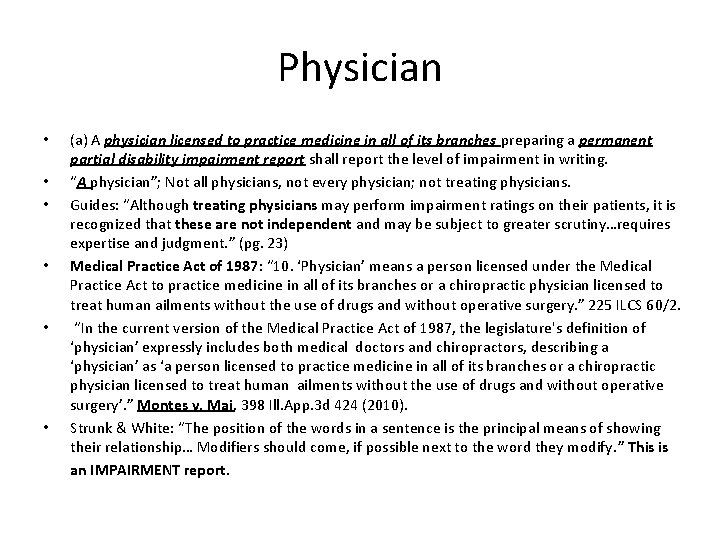
Physician • • • (a) A physician licensed to practice medicine in all of its branches preparing a permanent partial disability impairment report shall report the level of impairment in writing. “A physician”; Not all physicians, not every physician; not treating physicians. Guides: “Although treating physicians may perform impairment ratings on their patients, it is recognized that these are not independent and may be subject to greater scrutiny…requires expertise and judgment. ” (pg. 23) Medical Practice Act of 1987: “ 10. ‘Physician’ means a person licensed under the Medical Practice Act to practice medicine in all of its branches or a chiropractic physician licensed to treat human ailments without the use of drugs and without operative surgery. ” 225 ILCS 60/2. “In the current version of the Medical Practice Act of 1987, the legislature's definition of ‘physician’ expressly includes both medical doctors and chiropractors, describing a ‘physician’ as ‘a person licensed to practice medicine in all of its branches or a chiropractic physician licensed to treat human ailments without the use of drugs and without operative surgery’. ” Montes v. Mai, 398 Ill. App. 3 d 424 (2010). Strunk & White: “The position of the words in a sentence is the principal means of showing their relationship… Modifiers should come, if possible next to the word they modify. ” This is an IMPAIRMENT report.
Impairment Report • The report shall include an evaluation of medically defined and professionally appropriate measurements of impairment that include, but are not limited to: loss of range of motion; loss of strength; measured atrophy of tissue mass consistent with the injury; and any other measurements that establish the nature and extent of the impairment. The most current edition of the American Medical Association's "Guides to the Evaluation of Permanent Impairment" shall be used by the physician in determining the level of impairment. • Notice legislatures’s distinction between impairment vs. disability • “Loss of range of motion”? Is this in Guides? • “Any other measurements that establish nature & extent”? Does “any other” include measurements not in Guides? Must evaluator go outside of Guides to comply with this requirement? • “Most current” is 6 th Edition, Second printing
Factors • (b) In determining the level of permanent partial disability, the Commission shall base its determination on the following factors: • Notice legislature’s distinction between impairment and disability • Notice seemingly mandatory language: “shall base” • Notice use of word “factors”: one of five elements in ultimate determination of PPD
Factors Impairment • “(i) the reported level of impairment pursuant to subsection (a)” • What if no “reported” impairment? Guides cannot be considered: decisions “shall be based exclusively on evidence in the record. ” New(? ) standards of conduct. • Must comply with paragraph (a); done under AMA Guides • Are Impairment Reports (IR) automatically admissible? No! Blatant hearsay at least; no exception made for IR; legislature knows how to make things automatically admissible; See Section 16 • Section 16: “does not apply to reports prepared by treating providers for use in litigation. ” IR’s are just this! • Section 12? 48 hour rule?
Factors Occupation; Age; Earning Capacity • “(ii) the occupation of the injured employee” When? DA or later? • (iii) age of the employee at the time of the injury” Why at the time of the injury? Cuts both ways: young live with it longer; old recover poorly • “(iv) the employee’s future earning capacity” Consider 8(d)1 wage differential or 8(d)2 PAW
Factors Evidence of Disability • “and: evidence of disability corroborated by the treating medical records. ” • “Corroborated by”: supported by; credibility • “Treating medical records”: who cares what IME says about evidence of disability? • “Evidence of disability”: PPD shall be based on disability! Still! • What is evidence of disability?
Factors Evidence of Disability • Commission decisions: “conclusions of law set out in such decisions shall be regarded as precedents by Arbitrators” Section 19(e) • 81 IIC 1: “evaluate the effect of a disability on the life of the particular worker before it. Several factors are relevant…” • “Occupation; age; inability to engage in certain kinds of work or activities; loss of income; skill; training; pain; stiffness; weakness; cramps; numbness; inflammation; spasms; limitation of motion; tenderness; atrophy; lack of coordination; soreness; diminished reflexes; the need for assistance devices such as braces, orthotics and glasses; the need for medication and ongoing medical care. ” • Still a question of fact for reviewing courts

Factors No Sole Determinant • “No single enumerated factor shall be the sole determinant of disability. ” • “No single”: one alone • “enumerated”: (i) through and including (v) • “shall be the sole”: contrary to law if violated • “determinant”: decisive factor • “of disability”: Still PPD! Get it yet? !
Factors Weight • “In determining the level of disability, the relevance and weight of any factors used in addition to the level of impairment as reported by the physician must be explained in writing. ” • Notice disability v. impairment • Notice no special weight given to any one factor (i) through (v) • Notice relevance: irrelevant evidence in record? • Notice weight: “ Arbitrator assigns great weight to Petitioner’s credible complaints of pain as corroborated by the treating medical records. ” • Written order: Decision

Is This Right? • Compare to previous versions (See SB 1349 Mc. Carter: (c) In determining the level of disability, the Commission shall base their determination on the level of impairment as certified by the physician. The Commission may deviate from the level of impairment only using the following additional factors…) • “Illinois will not be a strict AMA Guides state” • Positions of interested parties: labor, ITLA, Chamber, CAT • No change in minimum permanency compensation (amputations, organs etc. ) • New carpal tunnel provision: recognition that disability is different from impairment • NCCI: No premium reduction for this provision because, “PPD award is based on determination of disability by the WCC using other subjective factors. ” (8. 8% reduction altogether)

AMA Guides, 6 th Edition It’s Changed Coming SOON to Illinois Workers’ Compensation
Why are you listening to me? ? • 820 ILCS 305/8. 1 B (NEW) – For accidental injuries that occurs on or after September 1, 2011, permanent partial impairment shall be established by the following criteria: a. A Physician licensed to practice medicine in all of its branches preparing a permanent partial disability report shall report the level of impairment in writing. …. The most current edition of the American Medical Association’s “Guides to the Evaluation of Permanent “Guides Impairment: shall be used by the physician in determining the level of impairment.
Why are you listening to me? ? • 820 ILCS 305/8. 1 B (NEW) – b. In determining the level of permanent partial disability, the Commission shall base its determination of the following factors: – – – (i) the reported level of impairment pursuant to subsection (a) (ii) the occupation of the injured employee (iii) the age of the employee at the time of the injury (iv) the employee’s future earning capacity (v) evidence of disability corroborated by the treating medical records. • In determining the level of disability, the relevance and weight of any factors used in addition to the level of impairment as reported by the physician must be explained in a written order.
JAMA Feb 15, 1958 The Musculoskeletal System 12 other “Guides” published over the next 12 years in Issues of JAMA. 18
AMA Guides – Work in Progress Gradual, Incremental Change 19
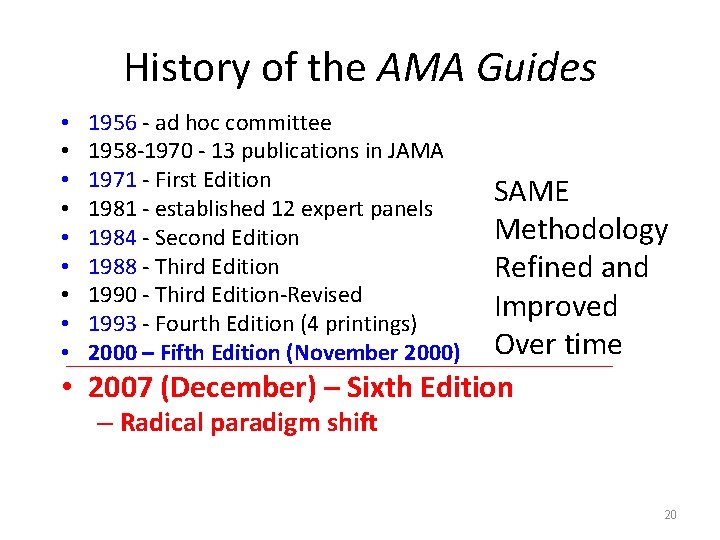
History of the AMA Guides • • • 1956 - ad hoc committee 1958 -1970 - 13 publications in JAMA 1971 - First Edition 1981 - established 12 expert panels 1984 - Second Edition 1988 - Third Edition 1990 - Third Edition-Revised 1993 - Fourth Edition (4 printings) 2000 – Fifth Edition (November 2000) SAME Methodology Refined and Improved Over time • 2007 (December) – Sixth Edition – Radical paradigm shift 20
The Color: Purple Date of publication December 24, 2007 Merry Christmas 21
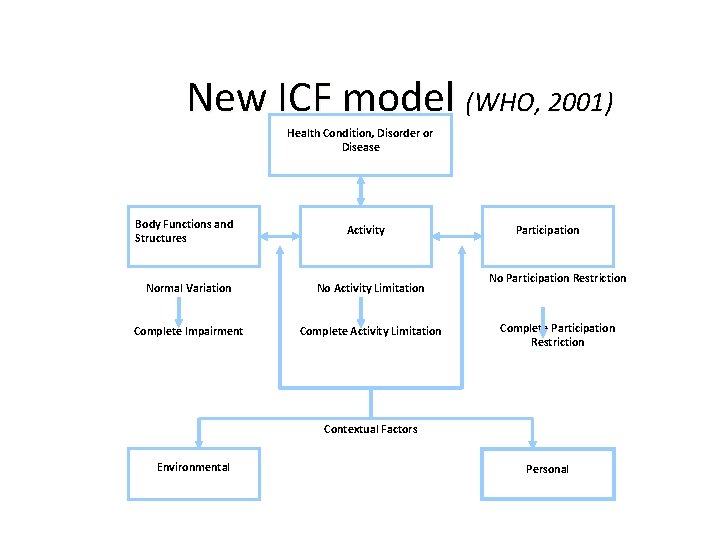
Axiom 1: • The AMA Guides must adopt the terminology and conceptual framework of disablement as put forward by the International Classification of Functioning, Disability and Health (ICF). (WHO, 2001)

23
We are all to some degree DISABLED ? ICF Model is INTENDED to blur CAUSATION, so we focus on the individual’s handicap, NOT on Causation. 24
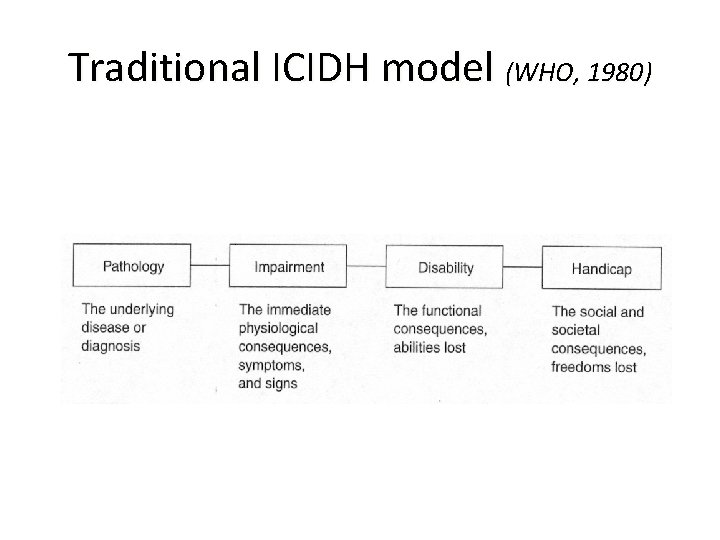
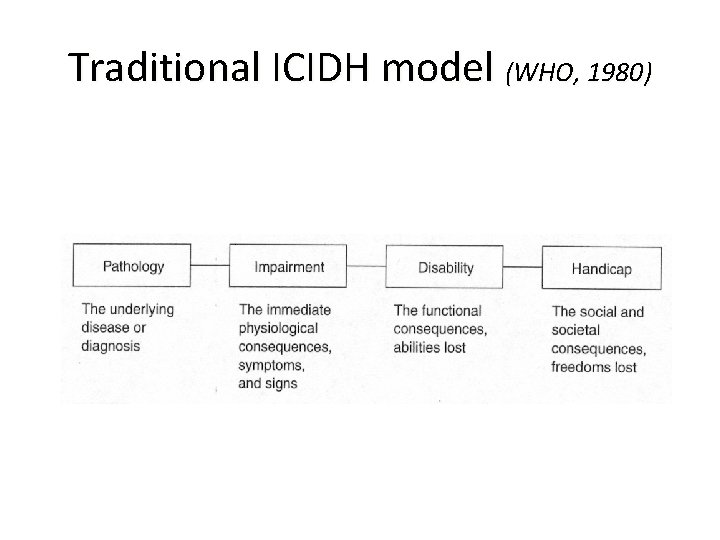
Traditional ICIDH model (WHO, 1980)
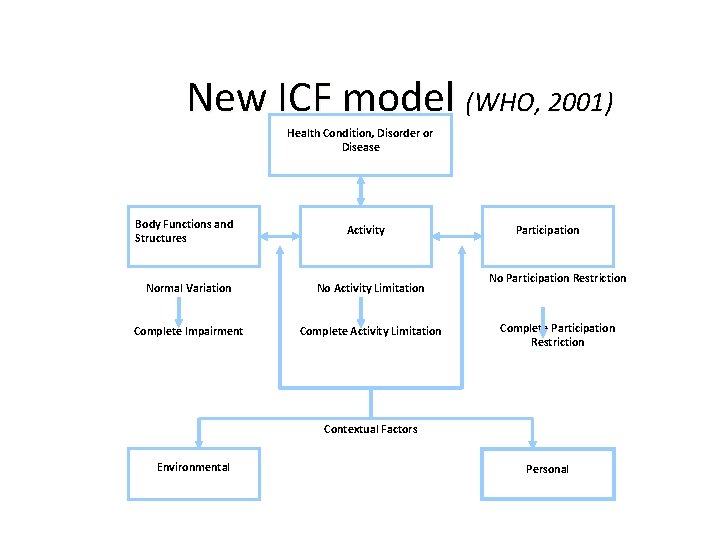
New ICF model (WHO, 2001) Health Condition, Disorder or Disease Body Functions and Structures Activity Normal Variation No Activity Limitation Complete Impairment Complete Activity Limitation Participation No Participation Restriction Complete Participation Restriction Contextual Factors Environmental Personal
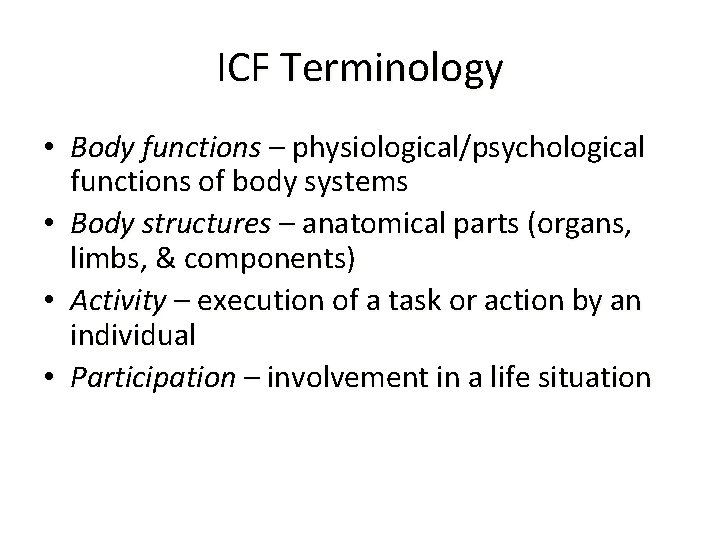
ICF Terminology • Body functions – physiological/psychological functions of body systems • Body structures – anatomical parts (organs, limbs, & components) • Activity – execution of a task or action by an individual • Participation – involvement in a life situation
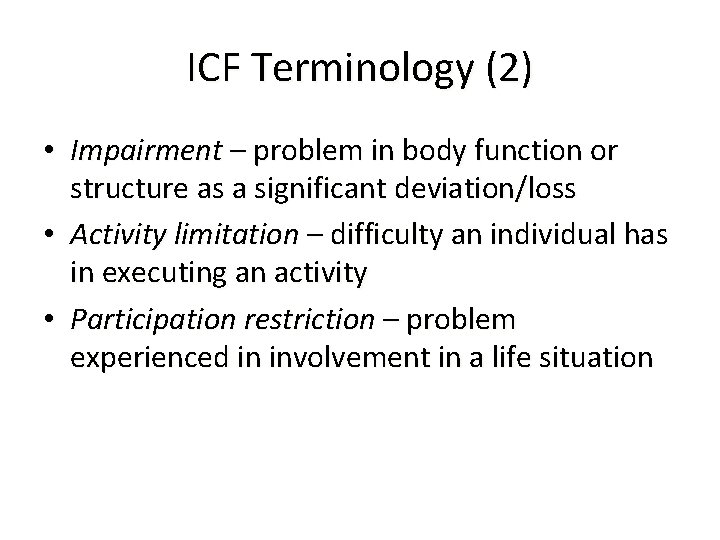
ICF Terminology (2) • Impairment – problem in body function or structure as a significant deviation/loss • Activity limitation – difficulty an individual has in executing an activity • Participation restriction – problem experienced in involvement in a life situation
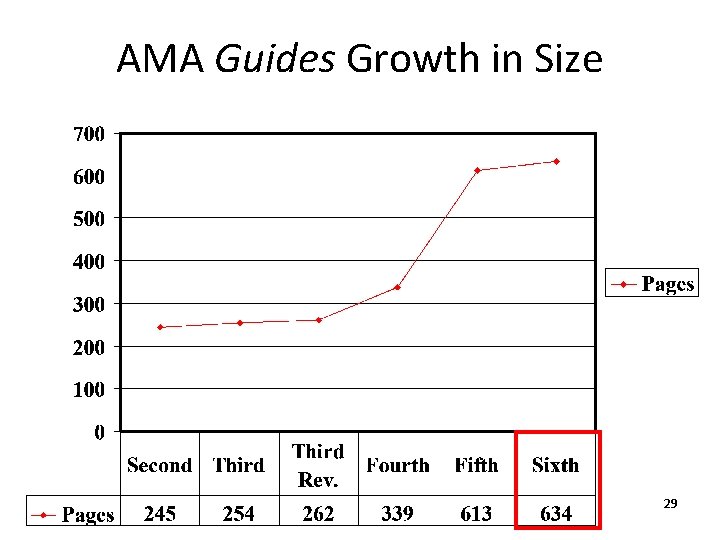
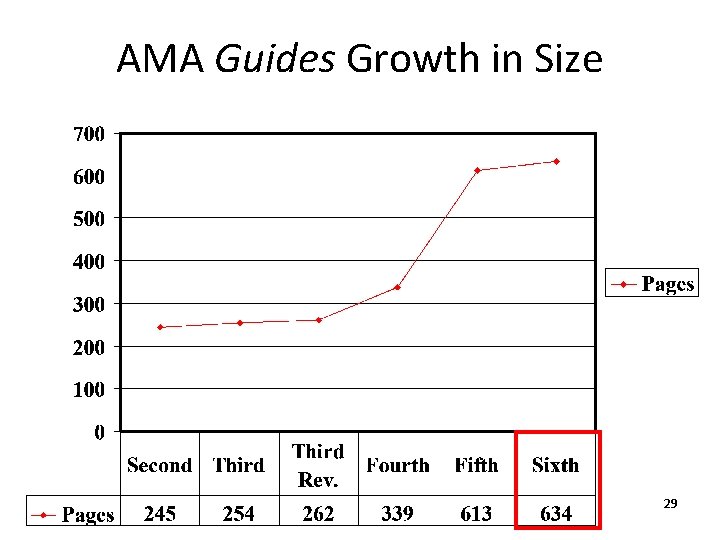
AMA Guides Growth in Size 29
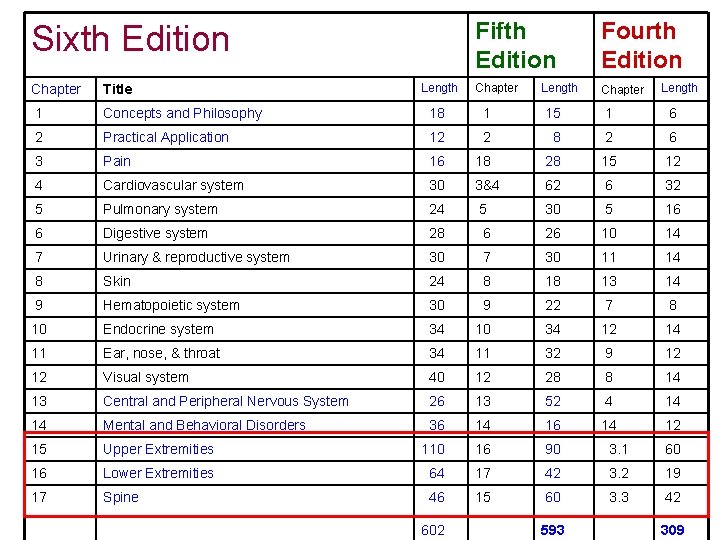
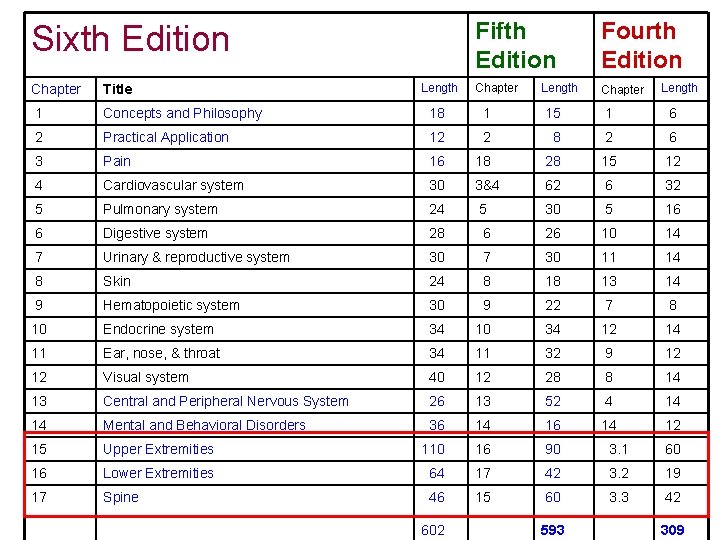
Sixth Edition Length Fifth Edition Fourth Edition Chapter Length Chapter Title 1 Concepts and Philosophy 18 1 15 1 6 2 Practical Application 12 2 8 2 6 3 Pain 16 18 28 15 12 4 Cardiovascular system 30 3&4 62 6 32 5 Pulmonary system 24 5 30 5 16 6 Digestive system 28 6 26 10 14 7 Urinary & reproductive system 30 7 30 11 14 8 Skin 24 8 18 13 14 9 Hematopoietic system 30 9 22 7 8 10 Endocrine system 34 10 34 12 14 11 Ear, nose, & throat 34 11 32 9 12 12 Visual system 40 12 28 8 14 13 Central and Peripheral Nervous System 26 13 52 4 14 14 Mental and Behavioral Disorders 36 14 12 15 Upper Extremities 110 16 90 3. 1 60 16 Lower Extremities 64 17 42 3. 2 19 17 Spine 46 15 60 3. 3 42 602 593 309

Impairment Rating Does NOT • Determine Medical Care • Comment on causation • “Impairment evaluations are usually performed not to establish academic facts or to make treatment decisions but, rather, to establish the financial obligations of payers to individuals, or, conversely, the entitlement of individuals to monetary rewards. – Guides, 5 th Edition page 569 32
Impairment Rating: 6 th Edition • “… to translate objective clinical findings into a percentage of the whole person. Typically this number is used to measure the residual deficit, a loss – a number that is then converted to a monetary award to the injured party. ” – page 20 • The Guides is not intended to be used for direct estimates of work participation restrictions. Impairment percentages derived according to the Guides criteria do NOT directly measure work participation restrictions. ” – Page 6, 6 th Edition – Page 13, 5 th Edition 33
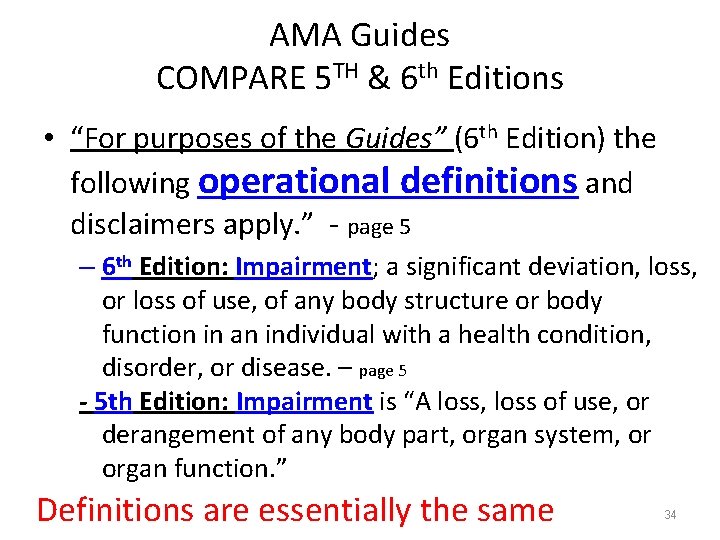
AMA Guides COMPARE 5 TH & 6 th Editions • “For purposes of the Guides” (6 th Edition) the following operational definitions and disclaimers apply. ” - page 5 – 6 th Edition: Impairment; a significant deviation, loss, or loss of use, of any body structure or body function in an individual with a health condition, disorder, or disease. – page 5 - 5 th Edition: Impairment is “A loss, loss of use, or derangement of any body part, organ system, or organ function. ” Definitions are essentially the same 34
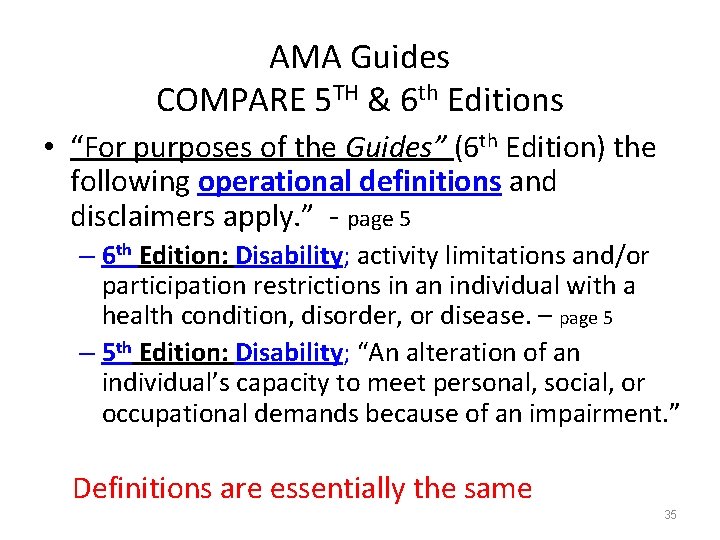
AMA Guides COMPARE 5 TH & 6 th Editions • “For purposes of the Guides” (6 th Edition) the following operational definitions and disclaimers apply. ” - page 5 – 6 th Edition: Disability; activity limitations and/or participation restrictions in an individual with a health condition, disorder, or disease. – page 5 – 5 th Edition: Disability; “An alteration of an individual’s capacity to meet personal, social, or occupational demands because of an impairment. ” Definitions are essentially the same 35
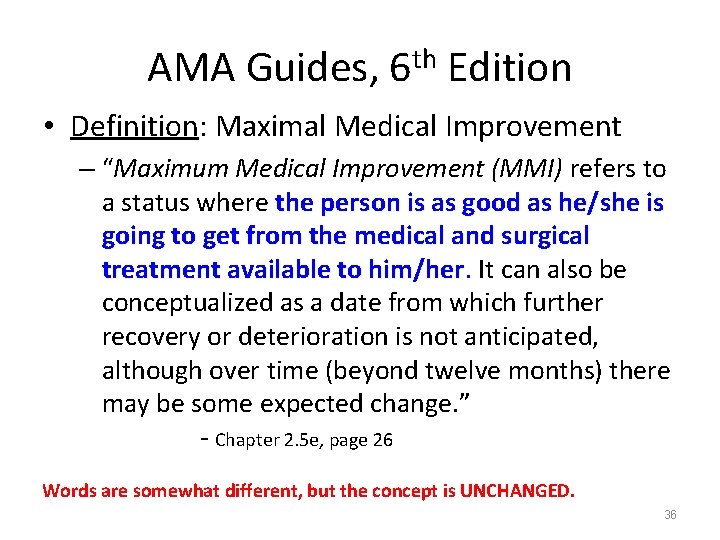
AMA Guides, 6 th Edition • Definition: Maximal Medical Improvement – “Maximum Medical Improvement (MMI) refers to a status where the person is as good as he/she is going to get from the medical and surgical treatment available to him/her. It can also be him/her conceptualized as a date from which further recovery or deterioration is not anticipated, although over time (beyond twelve months) there may be some expected change. ” - Chapter 2. 5 e, page 26 Words are somewhat different, but the concept is UNCHANGED. 36
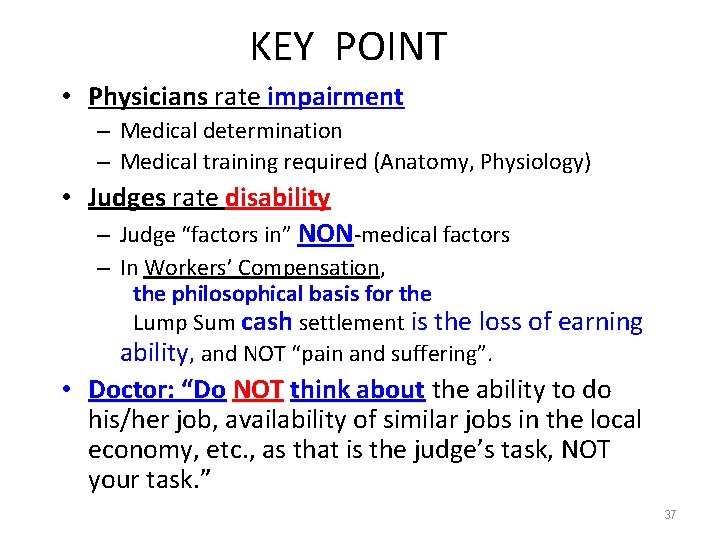
KEY POINT • Physicians rate impairment – Medical determination – Medical training required (Anatomy, Physiology) • Judges rate disability – Judge “factors in” NON-medical factors – In Workers’ Compensation, the philosophical basis for the Lump Sum cash settlement is the loss of earning ability, and NOT “pain and suffering”. • Doctor: “Do NOT think about the ability to do his/her job, availability of similar jobs in the local economy, etc. , as that is the judge’s task, NOT your task. ” 37

Impairment DOES NOT equal Disability • Example: both a lawyer and a pianist sustain an amputation of the non-dominant little finger. – Both have the same impairment • 100% of the digit, 10% of the hand, 9% of the upper extremity, 5% whole person – The lawyer has no disability – The pianist is unable to perform his occupation • Totally disabled for his occupation • Fully capable of many jobs • Physician’s role: Determine IMPAIRMENT 38
Impairment is NOT Disability • “In disability evaluation, the impairment rating is ONE of several determinants of disablement. Impairment rating is the determinant most amenable to physician assessment; it must be further integrated with contextual information typically provided by nonphysician sources regarding psychological, social, vocational, and avocational issues. ” – page 6 Unless otherwise specified page numbers refer to the Guides, 6 th Edition 39
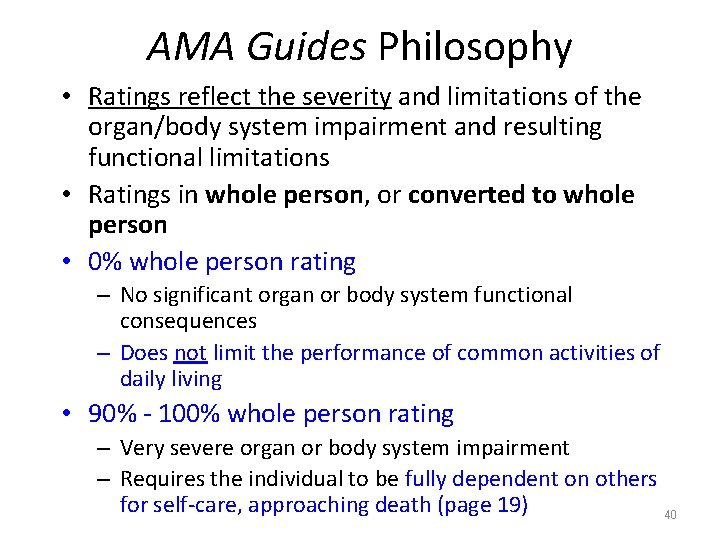
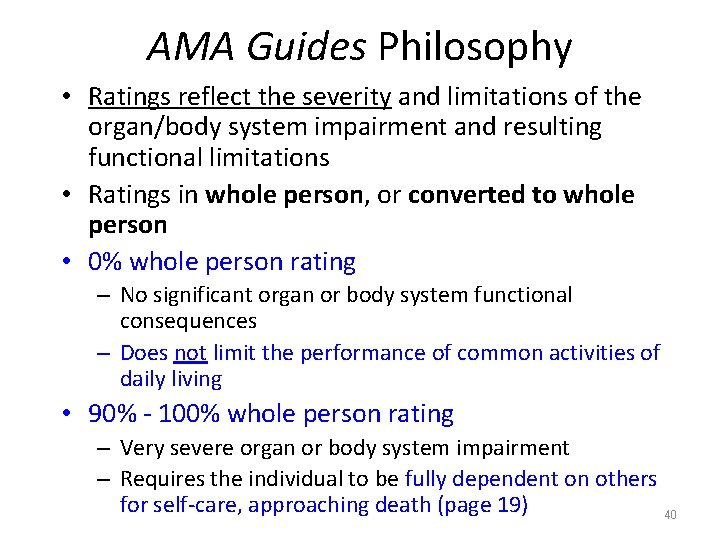
AMA Guides Philosophy • Ratings reflect the severity and limitations of the organ/body system impairment and resulting functional limitations • Ratings in whole person, or converted to whole person • 0% whole person rating – No significant organ or body system functional consequences – Does not limit the performance of common activities of daily living • 90% - 100% whole person rating – Very severe organ or body system impairment – Requires the individual to be fully dependent on others for self-care, approaching death (page 19) 40
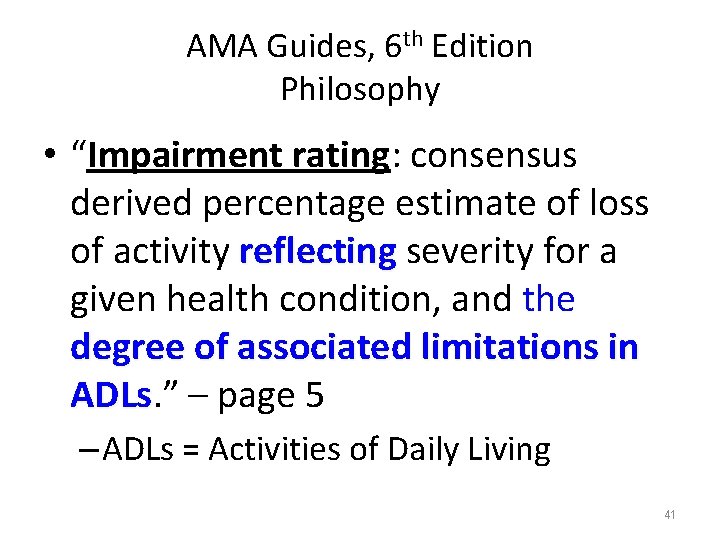
AMA Guides, 6 th Edition Philosophy • “Impairment rating: consensus derived percentage estimate of loss of activity reflecting severity for a reflecting given health condition, and the degree of associated limitations in ADLs. ” – page 5 ADLs – ADLs = Activities of Daily Living 41
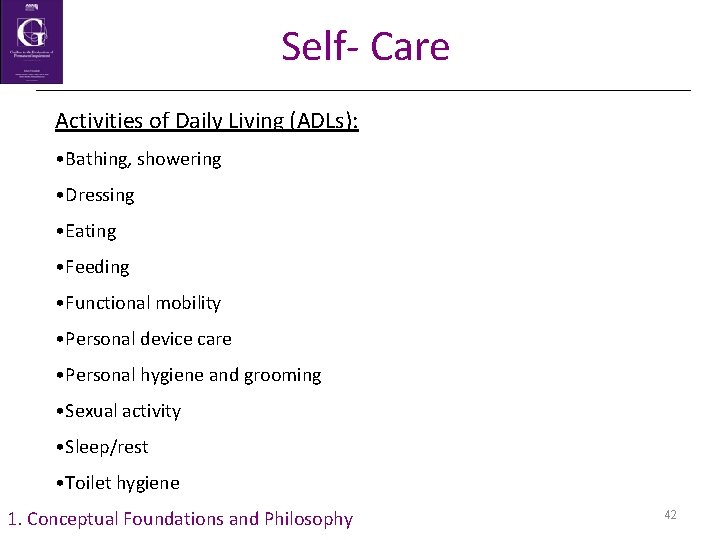
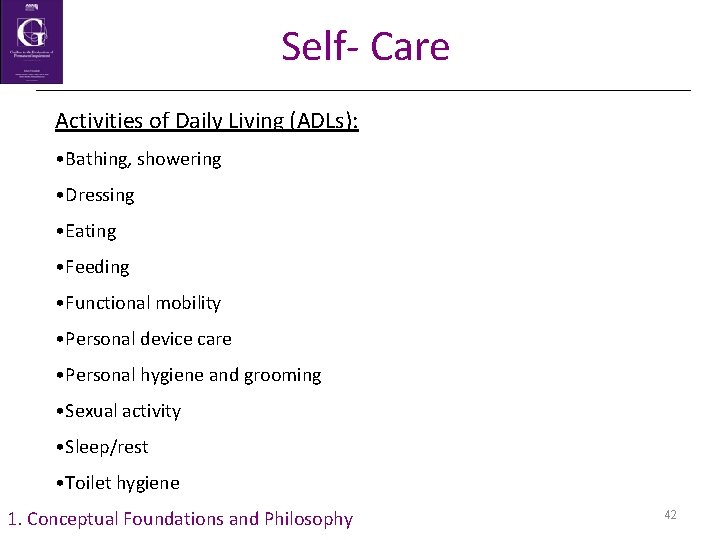
Self- Care Activities of Daily Living (ADLs): • Bathing, showering • Dressing • Eating • Feeding • Functional mobility • Personal device care • Personal hygiene and grooming • Sexual activity • Sleep/rest • Toilet hygiene 1. Conceptual Foundations and Philosophy 42
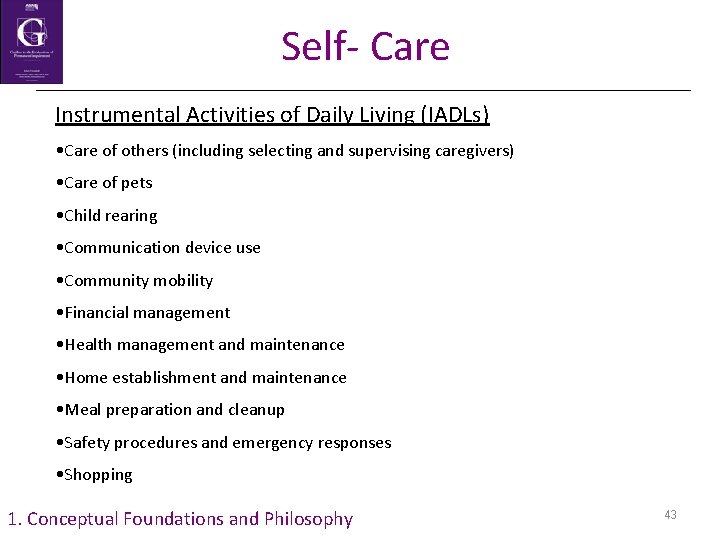
Self- Care Instrumental Activities of Daily Living (IADLs) • Care of others (including selecting and supervising caregivers) • Care of pets • Child rearing • Communication device use • Community mobility • Financial management • Health management and maintenance • Home establishment and maintenance • Meal preparation and cleanup • Safety procedures and emergency responses • Shopping 1. Conceptual Foundations and Philosophy 43
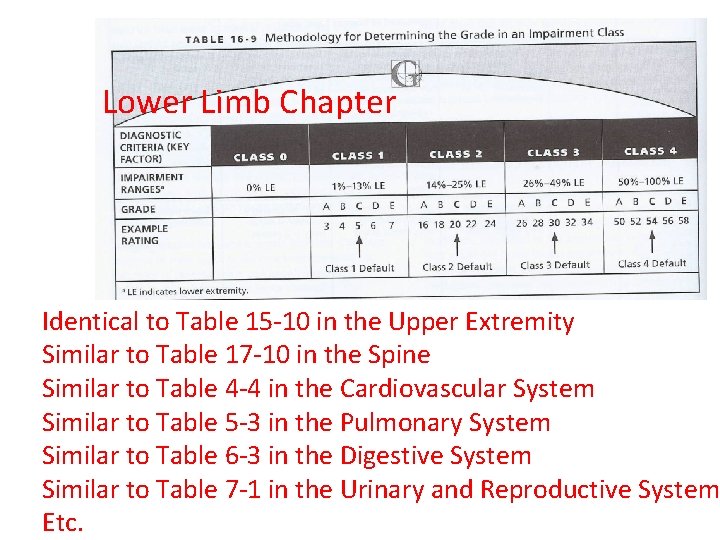
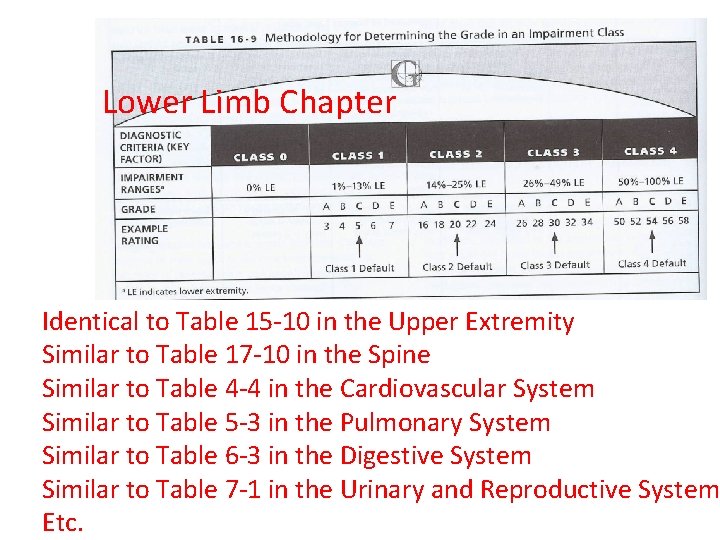
Lower Limb Chapter Identical to Table 15 -10 in the Upper Extremity Similar to Table 17 -10 in the Spine Similar to Table 4 -4 in the Cardiovascular System Similar to Table 5 -3 in the Pulmonary System Similar to Table 6 -3 in the Digestive System Similar to Table 7 -1 in the Urinary and Reproductive System 44 Etc.
Essential Elements of Physician Assessment & Reporting: OR How one Doctor talks to another about a case • What is the clinical problem (diagnosis)? • What difficulties does the patient report (symptoms; functional loss)? • What are the physical examination findings? • What are the results of clinical studies? • These same steps are involved in rating impairment using the 6 th Edition methodology.
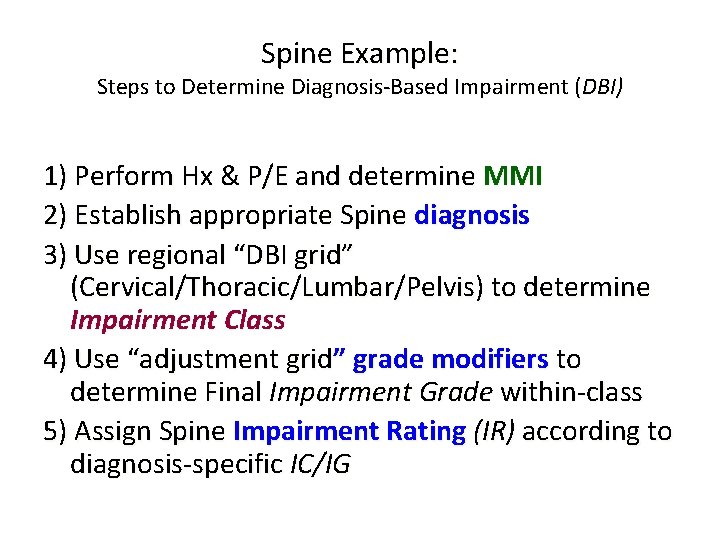
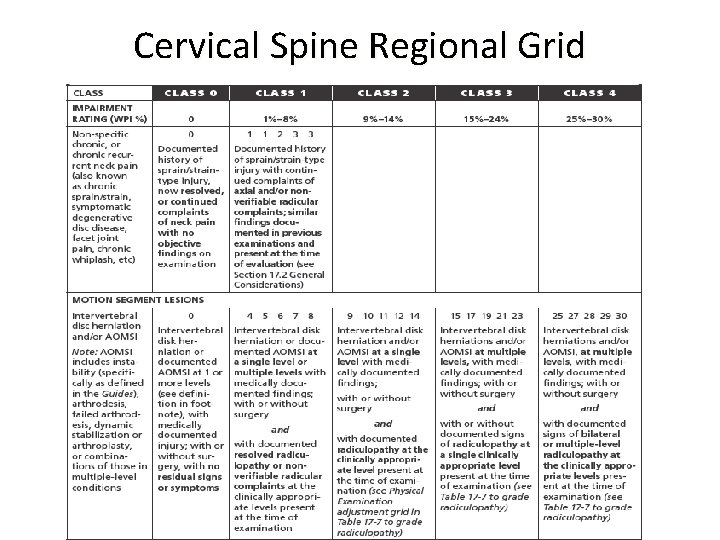
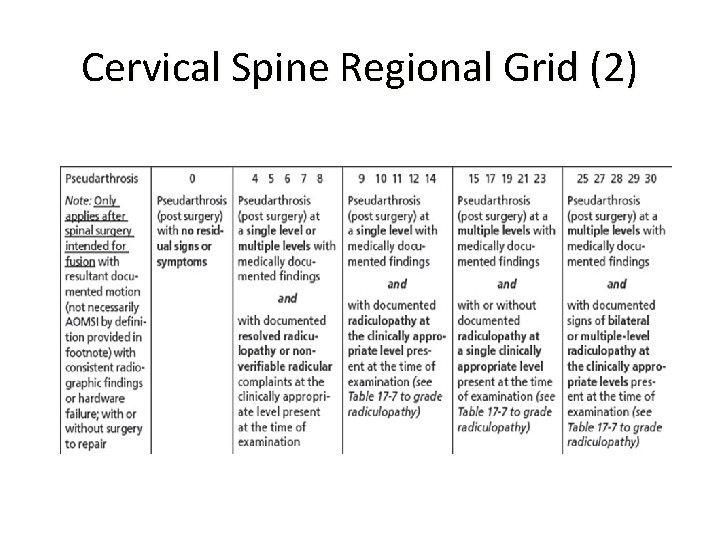
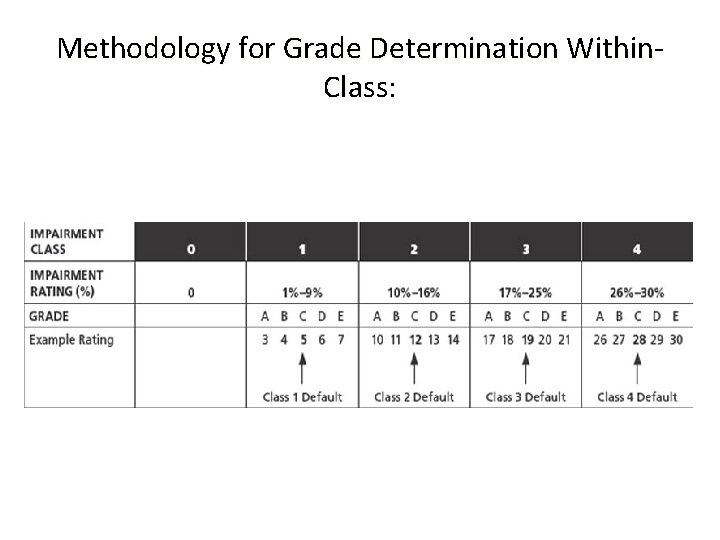
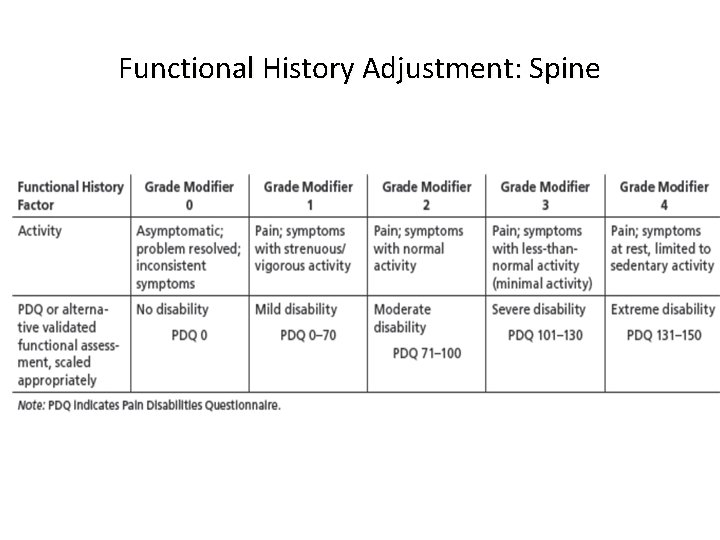
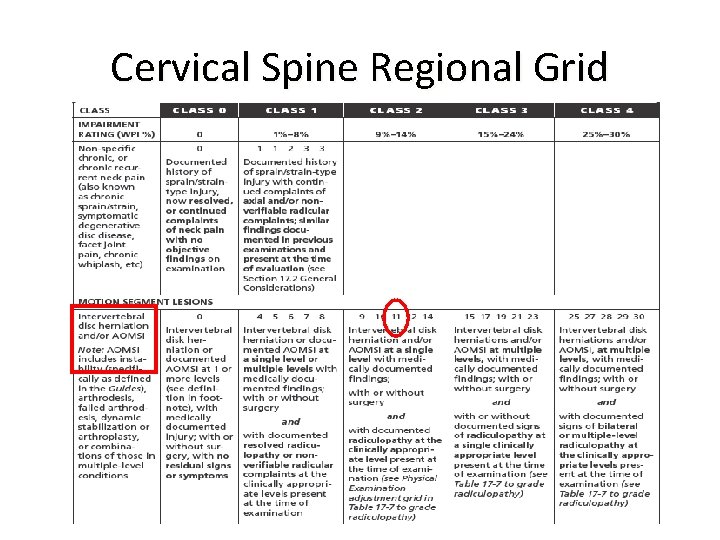
Spine Example: Steps to Determine Diagnosis-Based Impairment (DBI) 1) Perform Hx & P/E and determine MMI 2) Establish appropriate Spine diagnosis 3) Use regional “DBI grid” (Cervical/Thoracic/Lumbar/Pelvis) to determine Impairment Class 4) Use “adjustment grid” grade modifiers to determine Final Impairment Grade within-class 5) Assign Spine Impairment Rating (IR) according to diagnosis-specific IC/IG
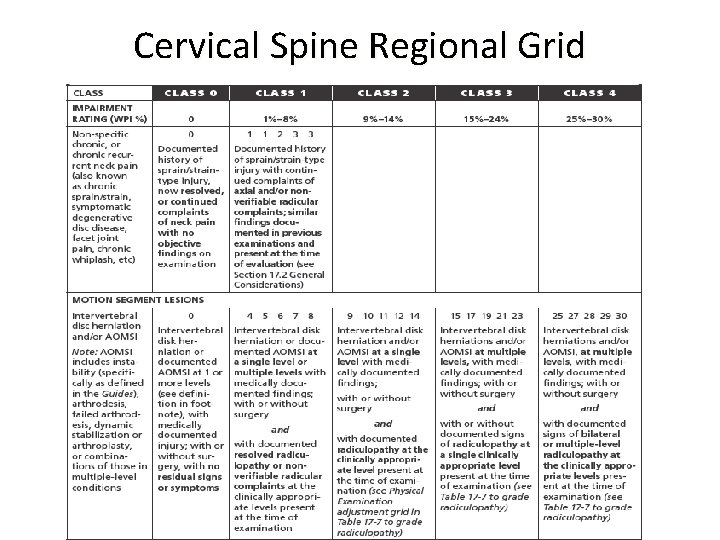
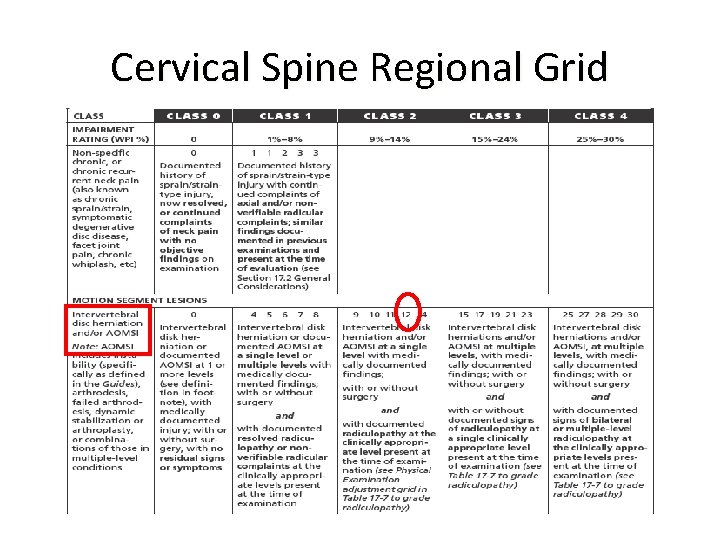
Cervical Spine Regional Grid
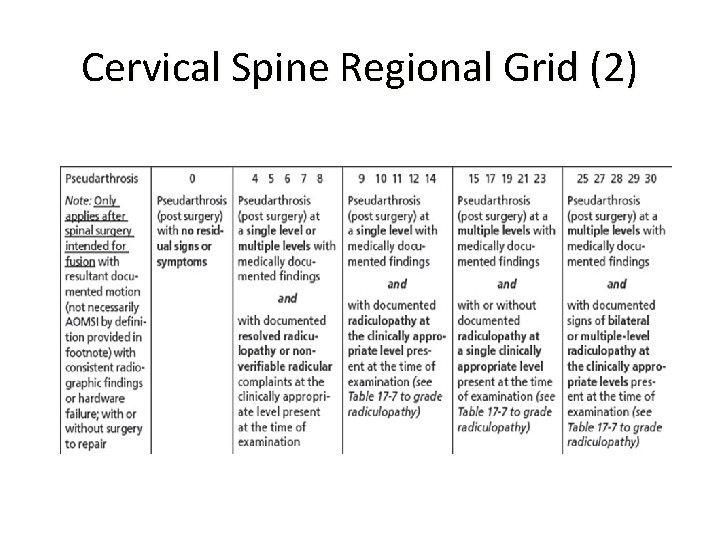
Cervical Spine Regional Grid (2)
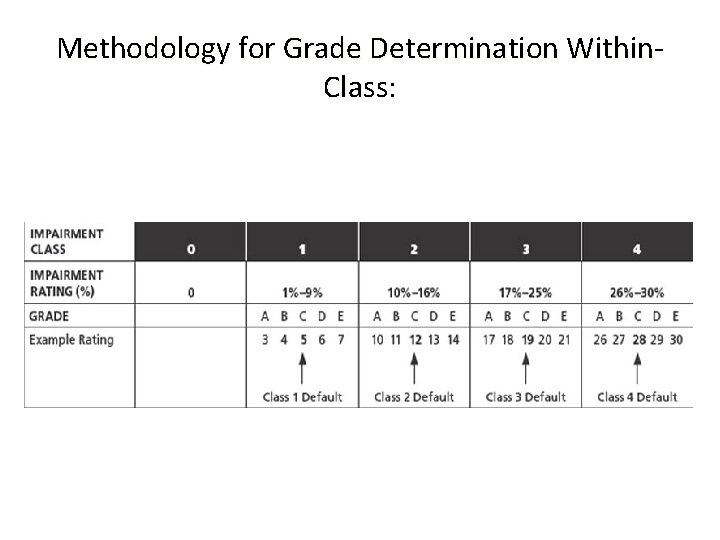
Methodology for Grade Determination Within. Class:

Adjustment Grid Summary
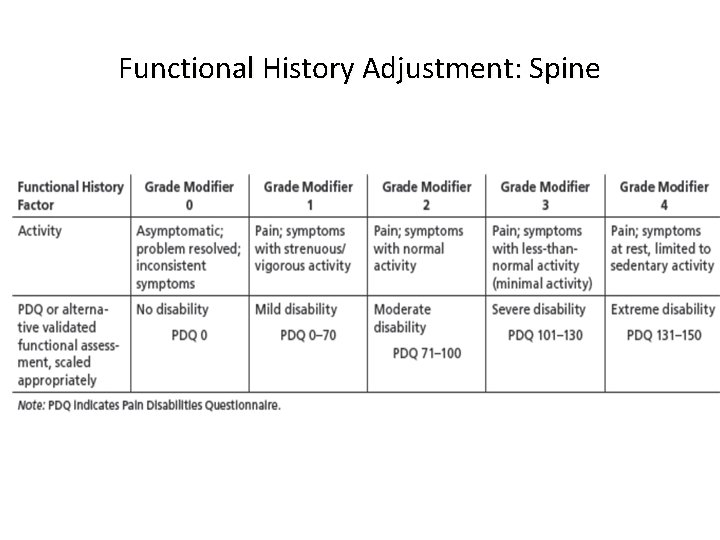
Functional History Adjustment: Spine
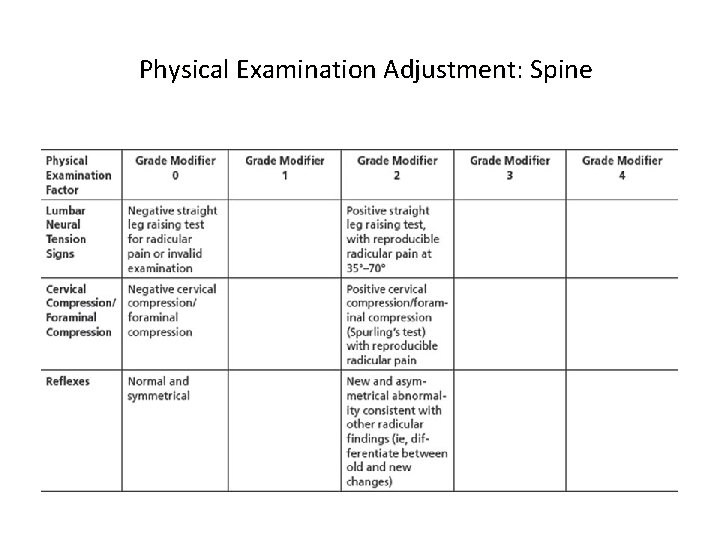
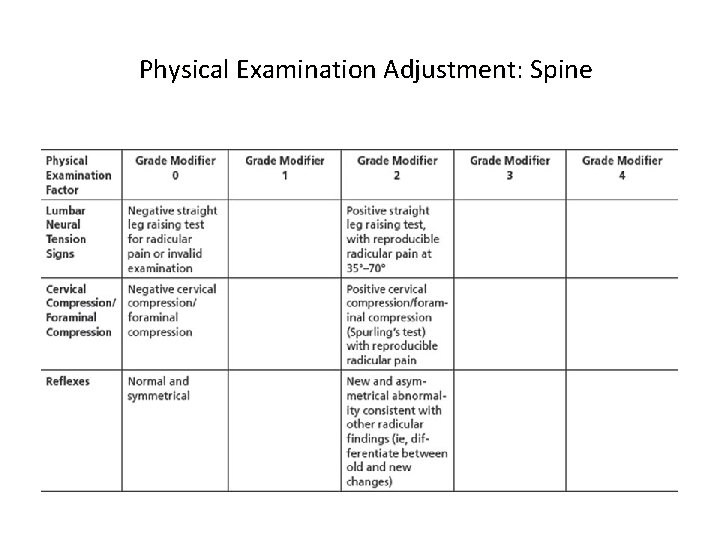
Physical Examination Adjustment: Spine
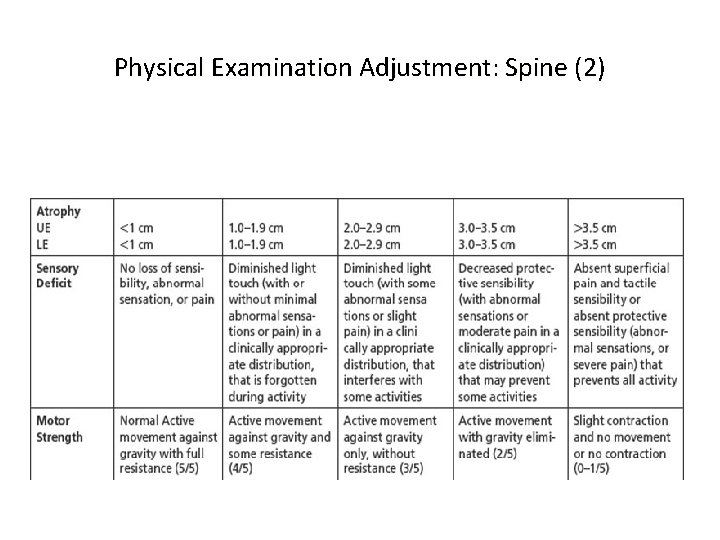
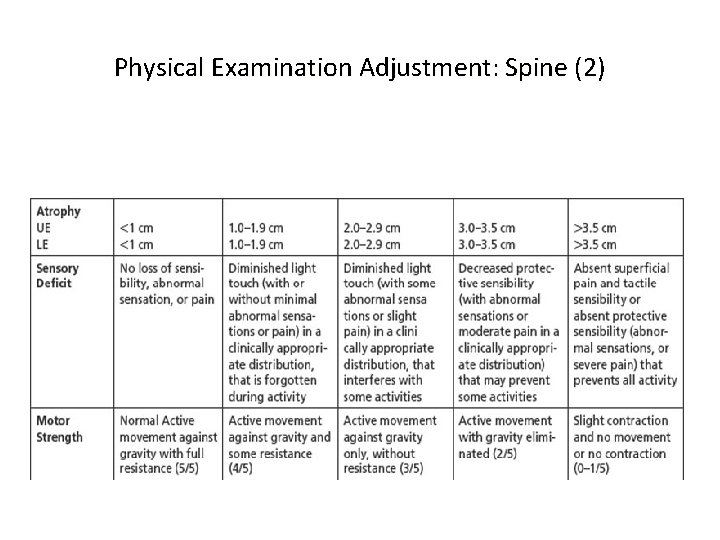
Physical Examination Adjustment: Spine (2)
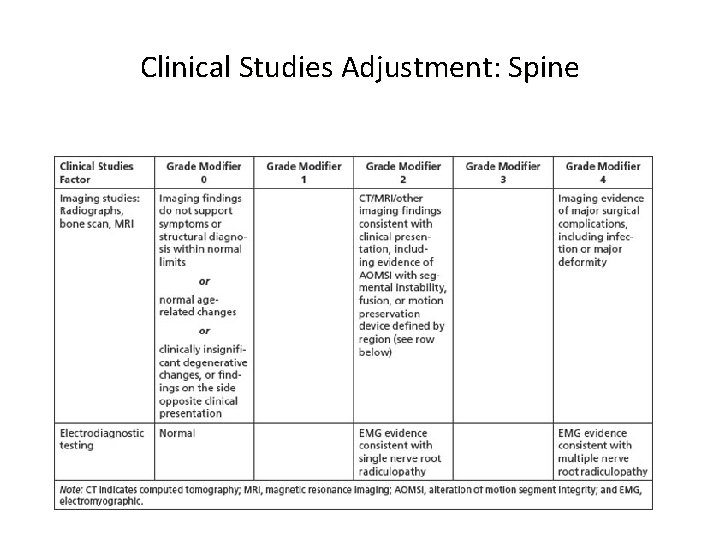
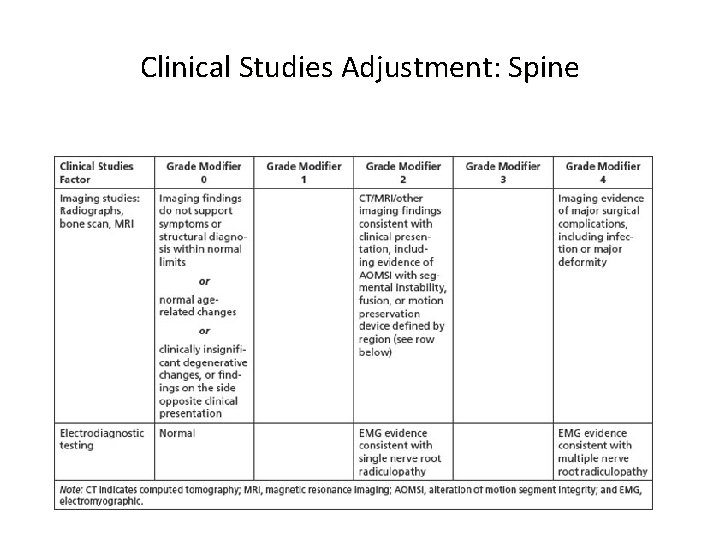
Clinical Studies Adjustment: Spine
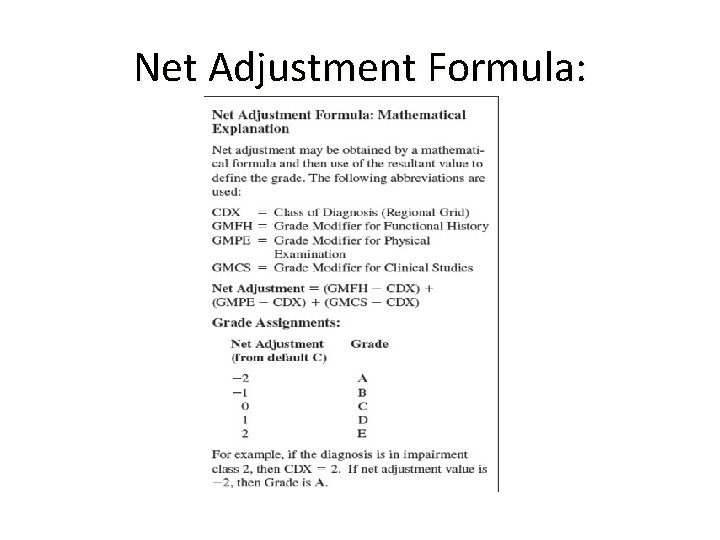
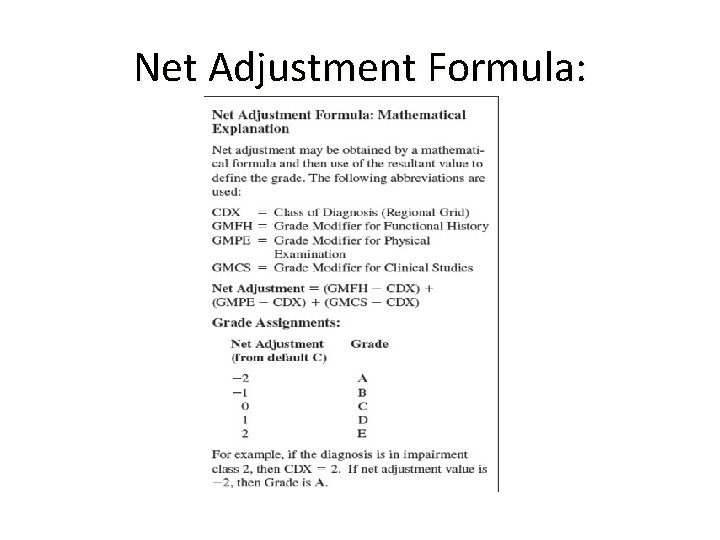
Net Adjustment Formula:
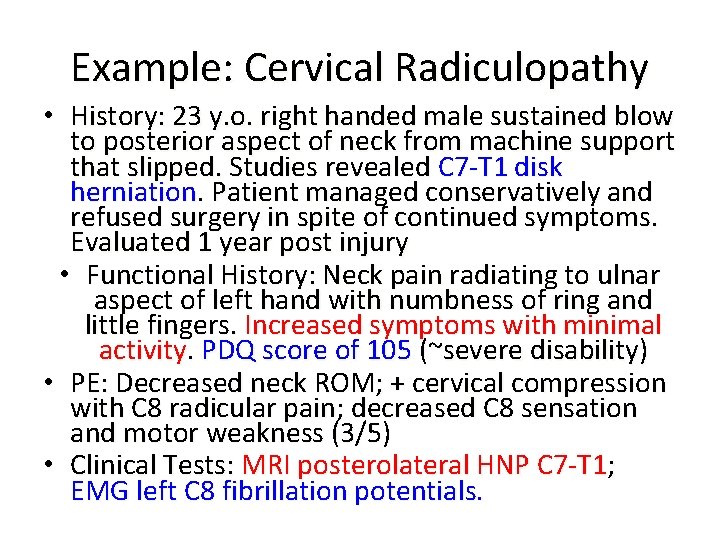
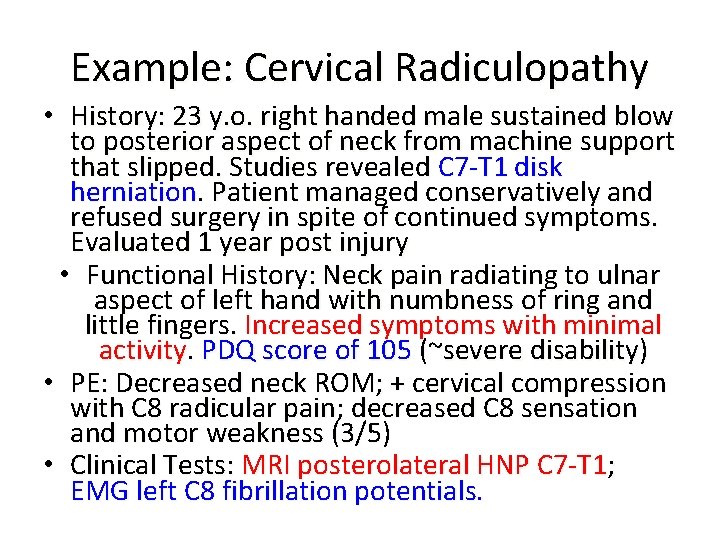
Example: Cervical Radiculopathy • History: 23 y. o. right handed male sustained blow to posterior aspect of neck from machine support that slipped. Studies revealed C 7 -T 1 disk herniation. Patient managed conservatively and refused surgery in spite of continued symptoms. Evaluated 1 year post injury • Functional History: Neck pain radiating to ulnar aspect of left hand with numbness of ring and little fingers. Increased symptoms with minimal activity. PDQ score of 105 (~severe disability) • PE: Decreased neck ROM; + cervical compression with C 8 radicular pain; decreased C 8 sensation and motor weakness (3/5) • Clinical Tests: MRI posterolateral HNP C 7 -T 1; EMG left C 8 fibrillation potentials.
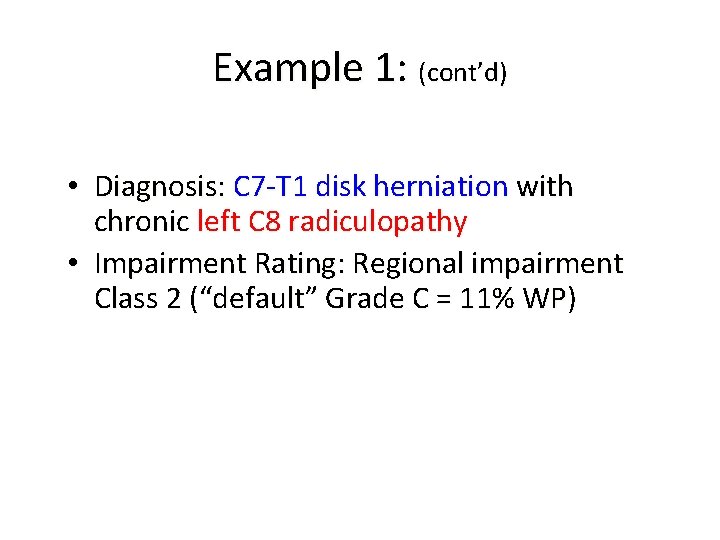
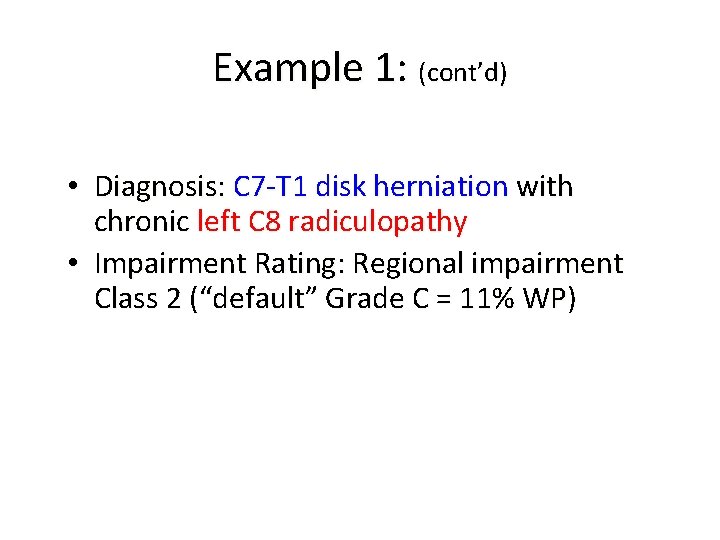
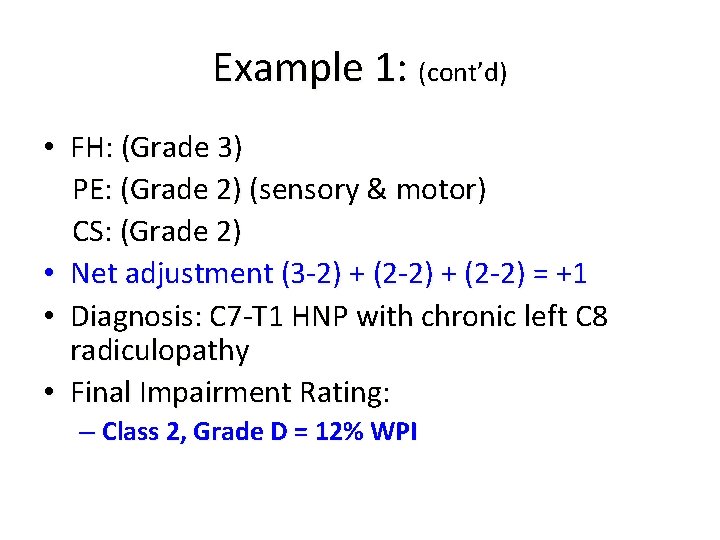
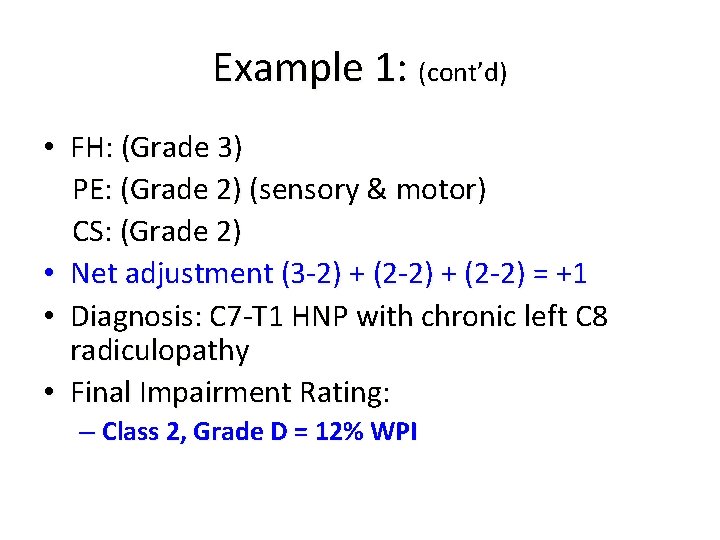
Example 1: (cont’d) • Diagnosis: C 7 -T 1 disk herniation with chronic left C 8 radiculopathy • Impairment Rating: Regional impairment Class 2 (“default” Grade C = 11% WP)
Cervical Spine Regional Grid
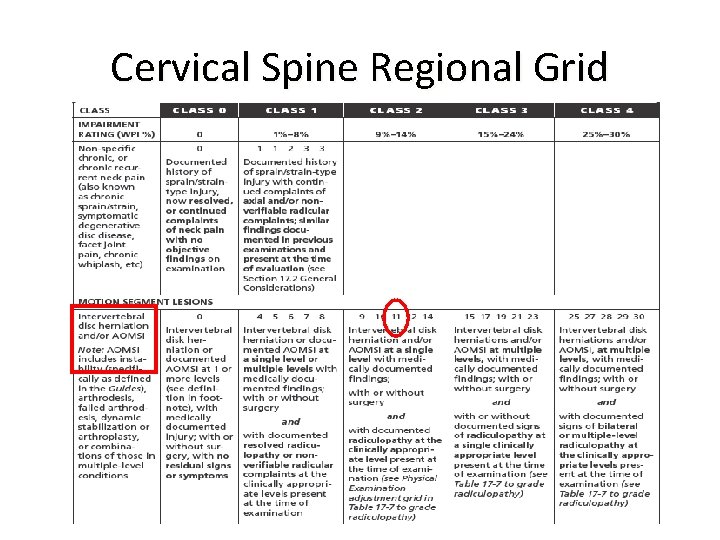
Example 1: (cont’d) • FH: (Grade 3) PE: (Grade 2) (sensory & motor) CS: (Grade 2) • Net adjustment (3 -2) + (2 -2) = +1 • Diagnosis: C 7 -T 1 HNP with chronic left C 8 radiculopathy • Final Impairment Rating: – Class 2, Grade D = 12% WPI
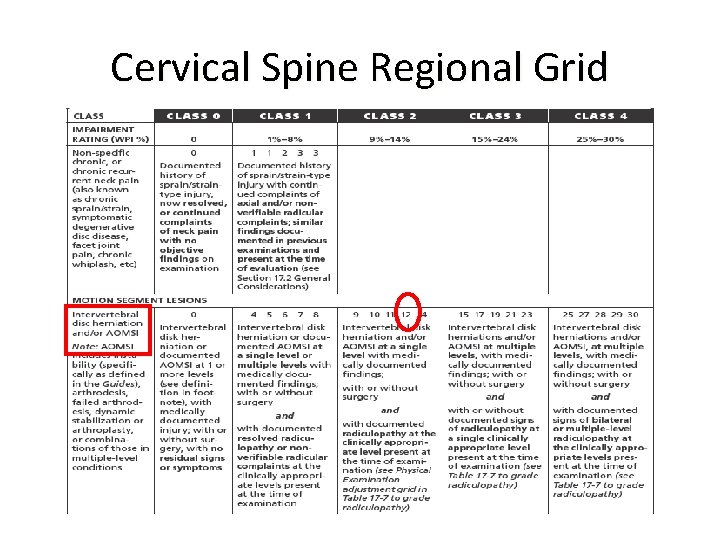
Cervical Spine Regional Grid

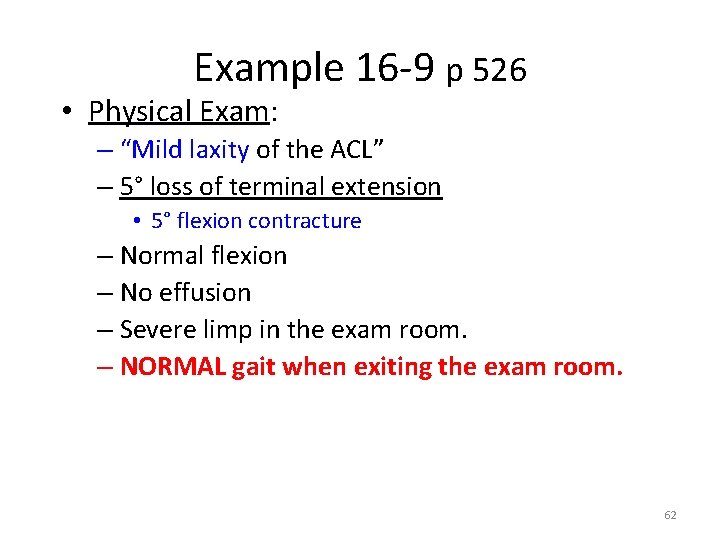
Example 16 -9 p 526 • Subject: 52 year old man • History: Twisting injury – s/p ACL reconstruction and medial meniscal repair – Severe pain and “nearly total functional loss of his extremity” 61
Example 16 -9 p 526 • Physical Exam: – “Mild laxity of the ACL” – 5° loss of terminal extension • 5° flexion contracture – Normal flexion – No effusion – Severe limp in the exam room. – NORMAL gait when exiting the exam room. 62
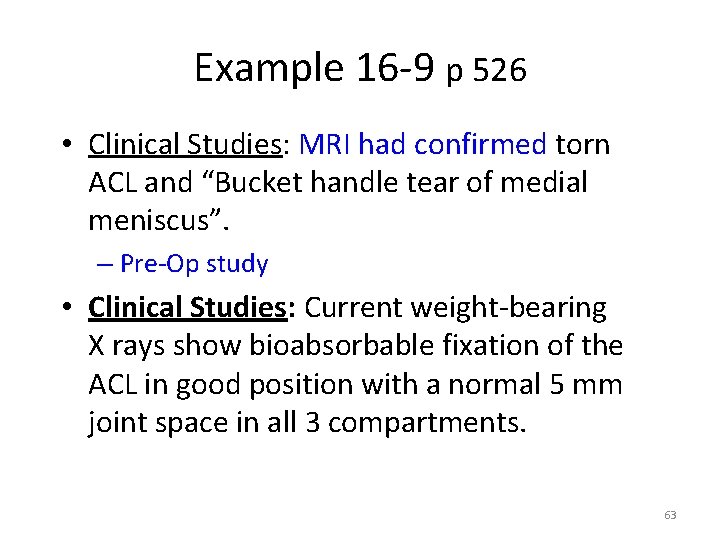
Example 16 -9 p 526 • Clinical Studies: MRI had confirmed torn ACL and “Bucket handle tear of medial meniscus”. – Pre-Op study • Clinical Studies: Current weight-bearing X rays show bioabsorbable fixation of the ACL in good position with a normal 5 mm joint space in all 3 compartments. 63
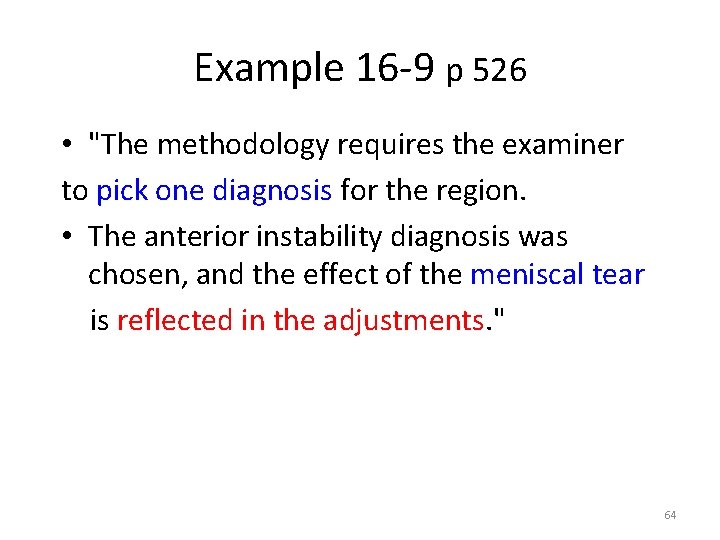
Example 16 -9 p 526 • "The methodology requires the examiner to pick one diagnosis for the region. • The anterior instability diagnosis was chosen, and the effect of the meniscal tear is reflected in the adjustments. " 64
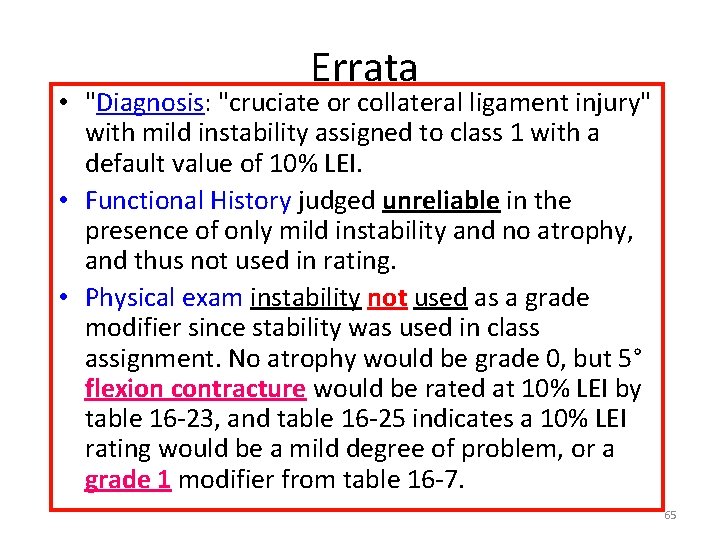
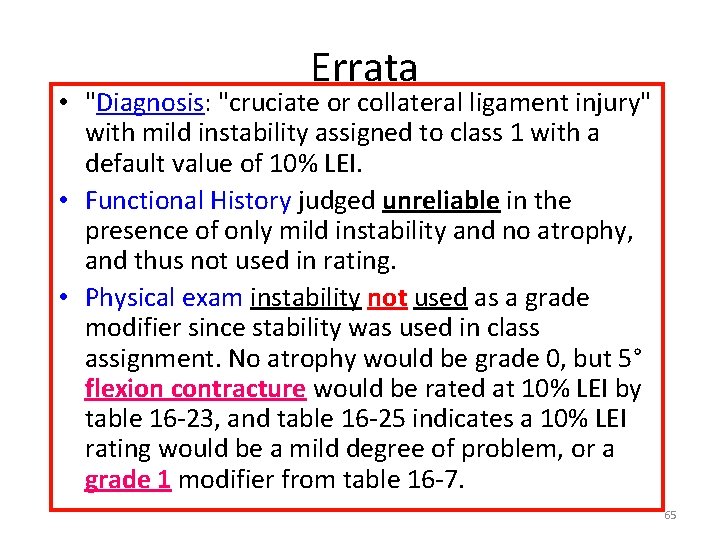
Errata • "Diagnosis: "cruciate or collateral ligament injury" with mild instability assigned to class 1 with a default value of 10% LEI. • Functional History judged unreliable in the presence of only mild instability and no atrophy, and thus not used in rating. • Physical exam instability not used as a grade modifier since stability was used in class assignment. No atrophy would be grade 0, but 5° flexion contracture would be rated at 10% LEI by table 16 -23, and table 16 -25 indicates a 10% LEI rating would be a mild degree of problem, or a grade 1 modifier from table 16 -7. 65
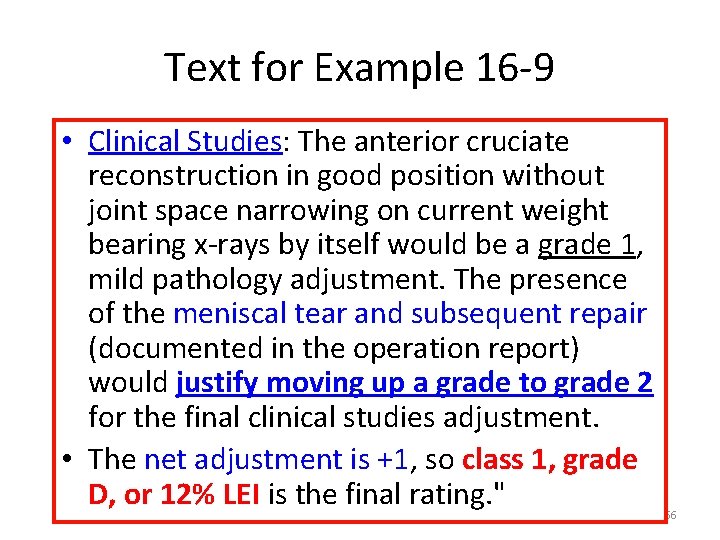
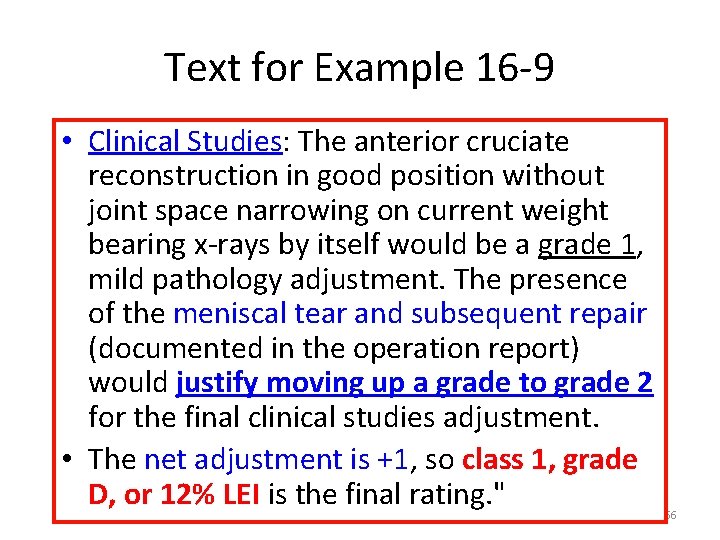
Text for Example 16 -9 • Clinical Studies: The anterior cruciate reconstruction in good position without joint space narrowing on current weight bearing x-rays by itself would be a grade 1, mild pathology adjustment. The presence of the meniscal tear and subsequent repair (documented in the operation report) would justify moving up a grade to grade 2 for the final clinical studies adjustment. • The net adjustment is +1, so class 1, grade D, or 12% LEI is the final rating. " 66
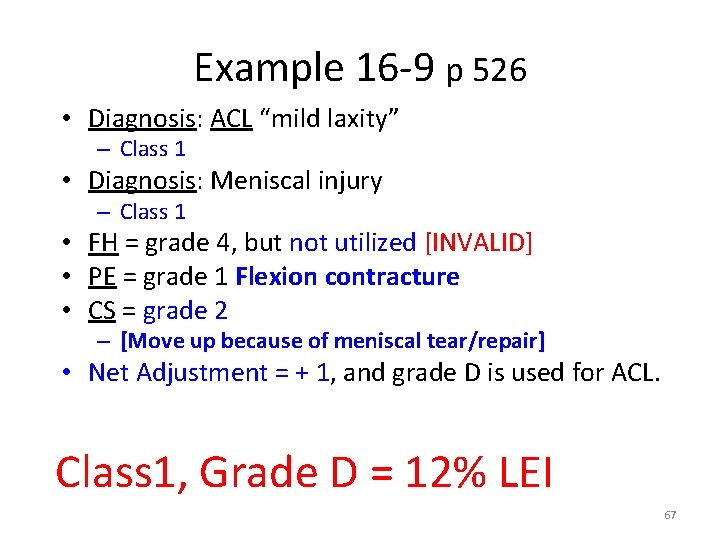
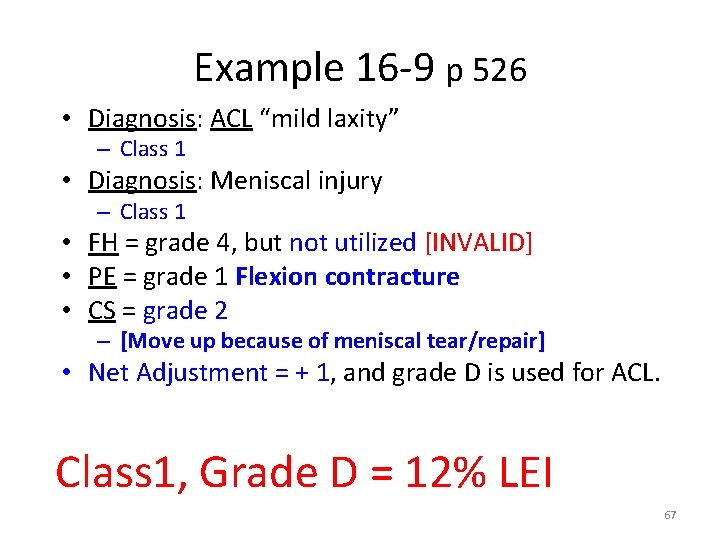
Example 16 -9 p 526 • Diagnosis: ACL “mild laxity” – Class 1 • Diagnosis: Meniscal injury – Class 1 • FH = grade 4, but not utilized [INVALID] • PE = grade 1 Flexion contracture • CS = grade 2 – [Move up because of meniscal tear/repair] • Net Adjustment = + 1, and grade D is used for ACL. Class 1, Grade D = 12% LEI 67
Features of AMA Guides 6 th ed: • ICF Model of Disablement (WHO 2001) replaces outdated ICIDH model (WHO 1980) • AMA Guides is regularly updated with latest, evidence-based diagnostic information • AMA Guides is increasingly diagnosis-based, hence physician-friendly and easy to learn and to use
Features of AMA Guides 6 th ed: (2) • AMA Guides is internally-consistent, hence easy to apply across multiple organ systems • AMA Guides is functionally-based to help capture impact of impairment upon ADLs • AMA Guides has high precision and resolution of impairment ratings • AMA Guides is transparent and promotes • greater inter-rater reliability and agreement
Conclusions • Many of the more meaningful changes were for spine-related diagnoses that resulted in surgery. • Diagnoses not previously ratable (e. g. soft tissue) may result in small impairments. • Consistent process should result in improved inter-rater reliability.
Thanks For Your Attention 71 71