Total Laryngectomy and Neck Dissection in the Setting
- Slides: 25
Total Laryngectomy and Neck Dissection in the Setting of Supraglottic Squamous Cell Carcinoma Major Case Study Presented by Veronica Chocron, MS, Dietetic Intern February 1, 2015
Objectives 1) Overview of laryngeal cancer 2) Review medical interventions for supraglottic cancer 3) Interpret nutrition interventions s/p laryngectomy 4) Analyze complications and risks associated with initiation of PO
Introduction to GD 63 yo. WM, married, well groomed, social Dx w/supraglottic mass consistent with squamous cell carcinoma Admitted 12/01/14 for elective total laryngectomy, left level II-IV neck dissection and tracheoesophageal prosthesis (TEP) D/c 12/11/14 3 RD visits
Biometrics and Needs Measurements Ht: 175. 3 cm/69” Wt: 93 kg/205# BMI: 30. 2 kg/M 2, obese class I Physical appearance: overweight, abdominal adiposity, well nourished IBW: 73 kg/ 160#, 128%IBW Estimated needs 1825 kcals (25 kcals/kg IBW) 146 gm pro (2. 0 gm/kg IBW) Fluids per team
Medical History PMHx: cataract surgery (06/2014), nasal blockage, congestion and hearing loss, asthma, heart attack, hernia repair, tonsillectomy and microlaryngoscopy Current medical concerns Hoarseness of voice (1 -2 yrs) Choking Dysphagia Coughing Difficulty clearing airway and wheezing
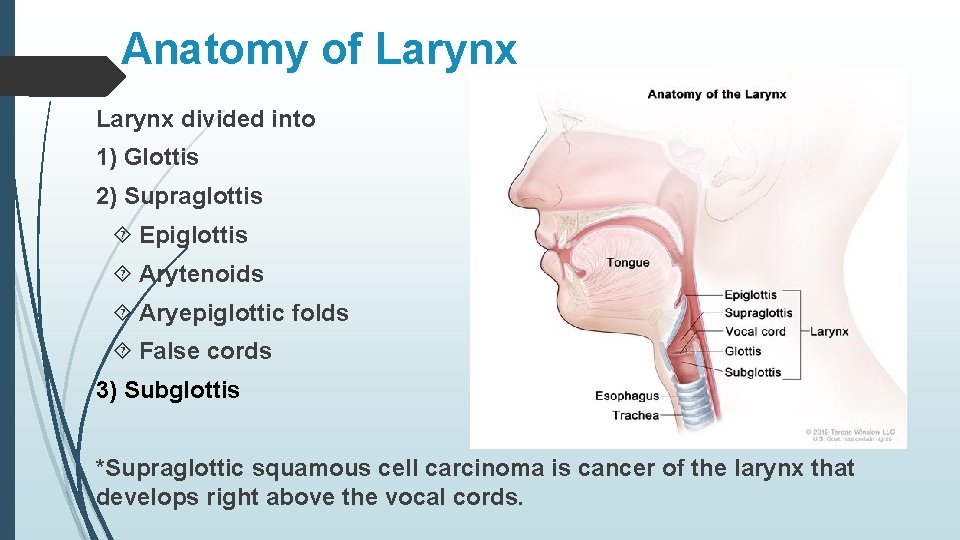
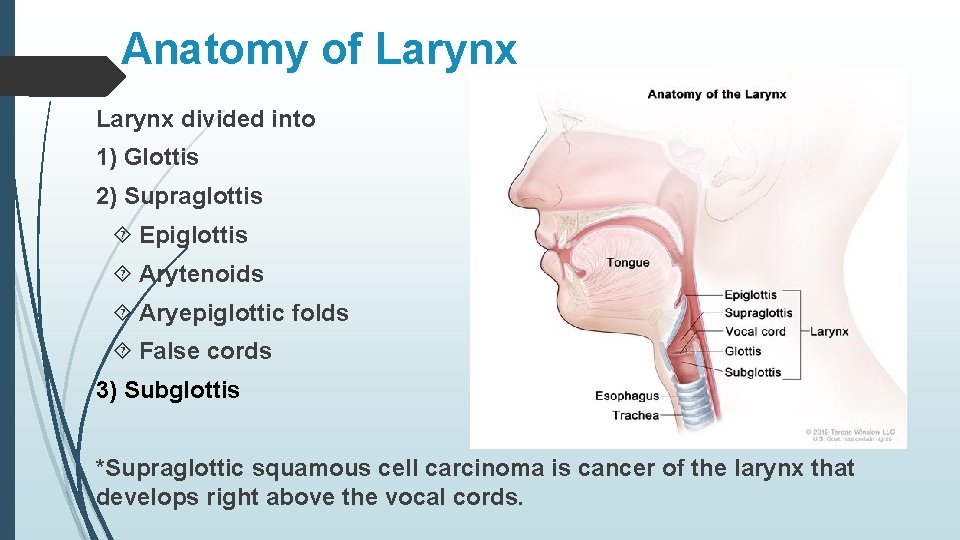
Anatomy of Larynx divided into 1) Glottis 2) Supraglottis Epiglottis Arytenoids Aryepiglottic folds False cords 3) Subglottis *Supraglottic squamous cell carcinoma is cancer of the larynx that develops right above the vocal cords.
Laryngeal Cancer Statistics 2 nd most common type of head & neck ca worldwide 12, 500 new cases/yr in U. S ~160, 000 cases of laryngeal cancer and 90, 000 deaths worldwide (2002) SCC 30 x more in men than women Associated with smoking & alcohol (can increase the risk by >100!) Supraglottis vs. glottis tumors > risk of lymphogenous metastasis greater vascularity later presentation fewer symptoms
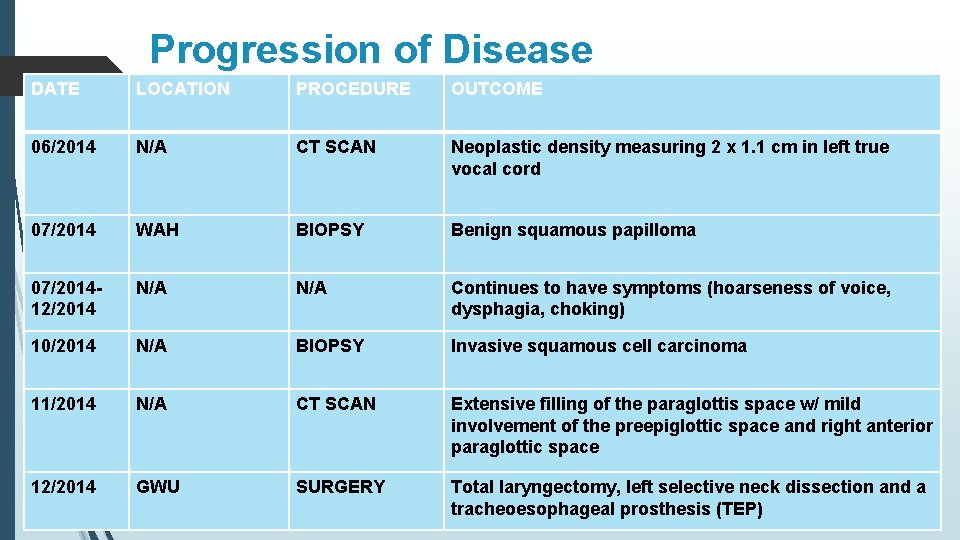
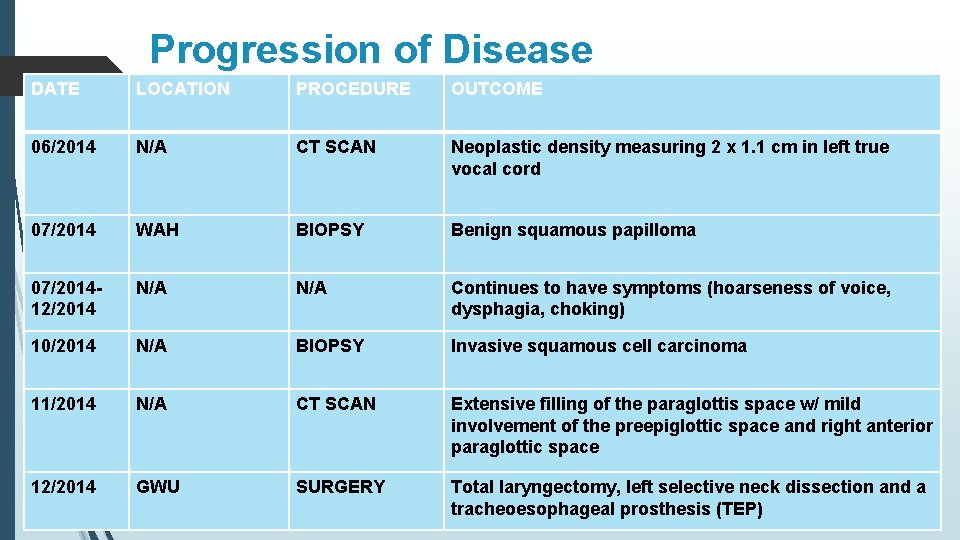
Progression of Disease DATE LOCATION PROCEDURE OUTCOME 06/2014 N/A CT SCAN Neoplastic density measuring 2 x 1. 1 cm in left true vocal cord 07/2014 WAH BIOPSY Benign squamous papilloma 07/201412/2014 N/A Continues to have symptoms (hoarseness of voice, dysphagia, choking) 10/2014 N/A BIOPSY Invasive squamous cell carcinoma 11/2014 N/A CT SCAN Extensive filling of the paraglottis space w/ mild involvement of the preepiglottic space and right anterior paraglottic space 12/2014 GWU SURGERY Total laryngectomy, left selective neck dissection and a tracheoesophageal prosthesis (TEP)
Treatment Options for Supraglottic SCC Chemotherapy Radiation Therapy Surgical intervention of mass Total laryngectomy GD’s treatment plan: e/o minor thyroid cartilage involvement (higher risk for recurrence using chemo/radiation) total laryngectomy.
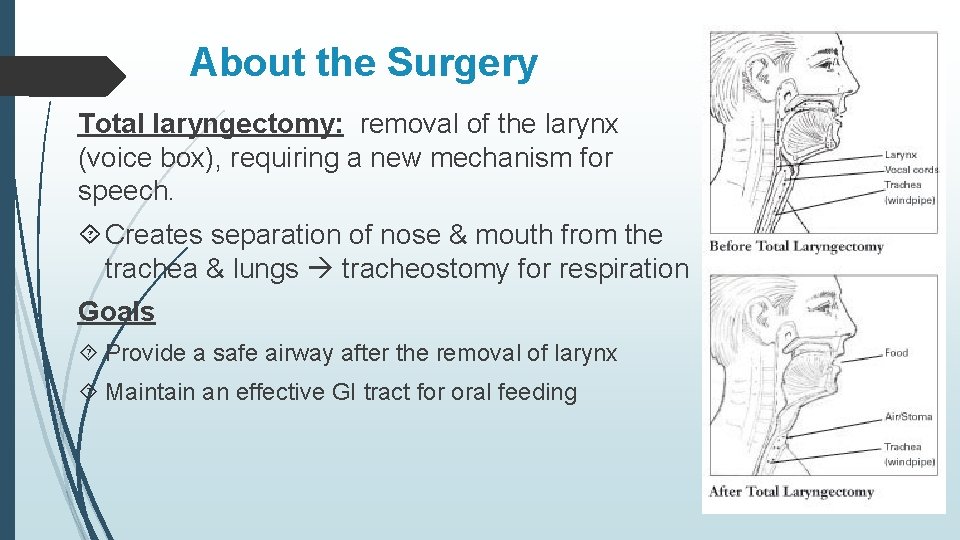
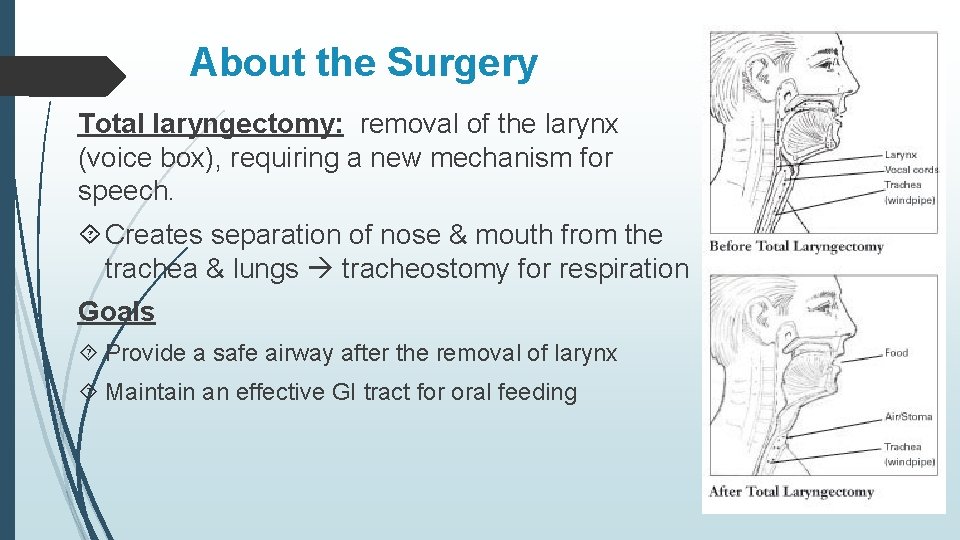
About the Surgery Total laryngectomy: removal of the larynx (voice box), requiring a new mechanism for speech. Creates separation of nose & mouth from the trachea & lungs tracheostomy for respiration Goals Provide a safe airway after the removal of larynx Maintain an effective GI tract for oral feeding
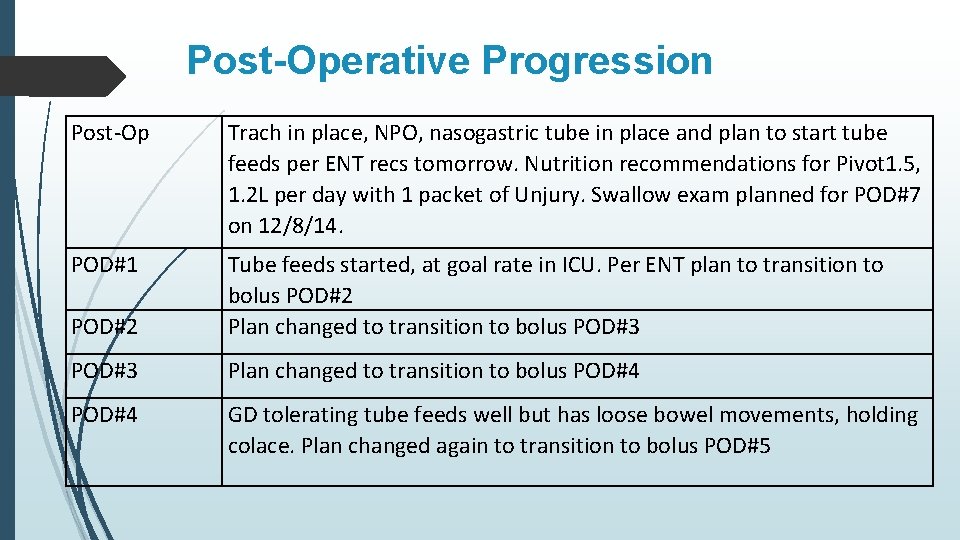
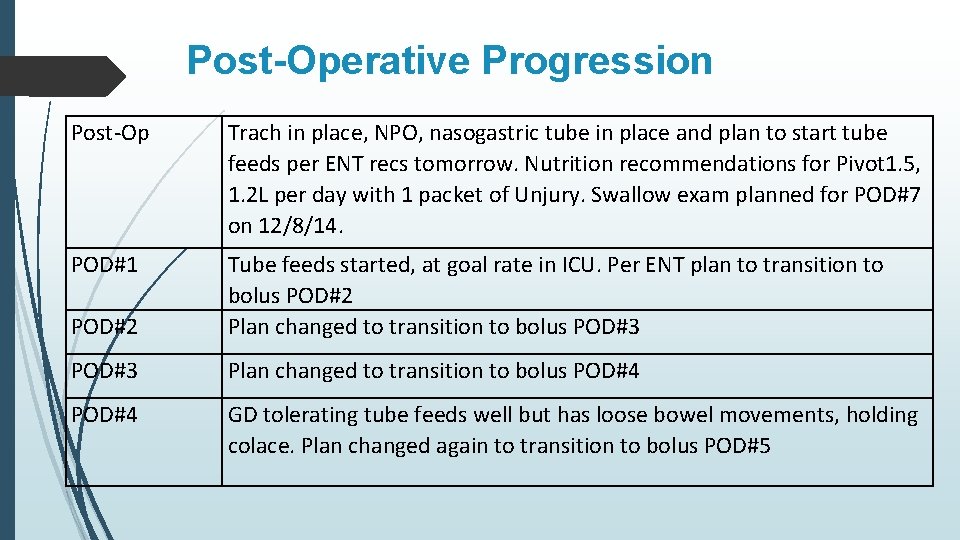
Post-Operative Progression Post-Op Trach in place, NPO, nasogastric tube in place and plan to start tube feeds per ENT recs tomorrow. Nutrition recommendations for Pivot 1. 5, 1. 2 L per day with 1 packet of Unjury. Swallow exam planned for POD#7 on 12/8/14. POD#1 POD#2 Tube feeds started, at goal rate in ICU. Per ENT plan to transition to bolus POD#2 Plan changed to transition to bolus POD#3 Plan changed to transition to bolus POD#4 GD tolerating tube feeds well but has loose bowel movements, holding colace. Plan changed again to transition to bolus POD#5
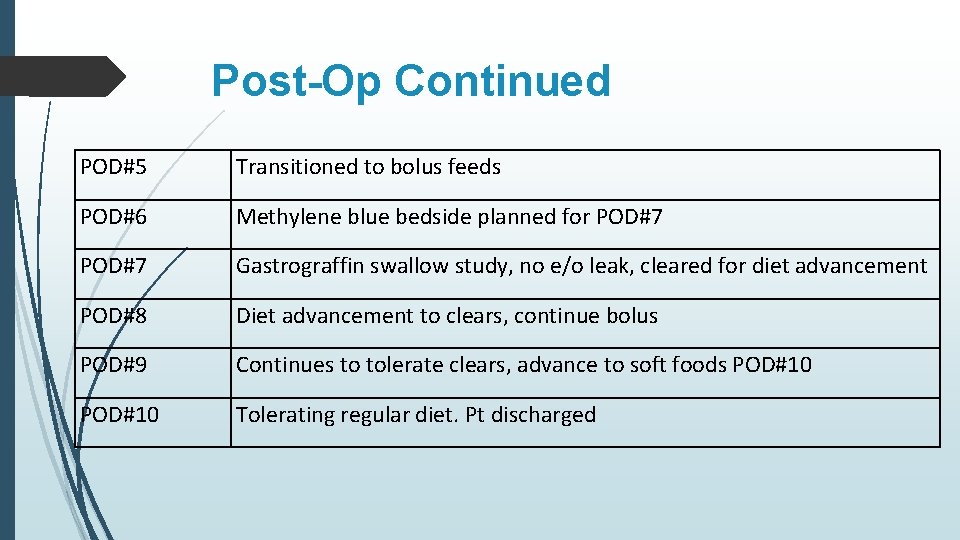
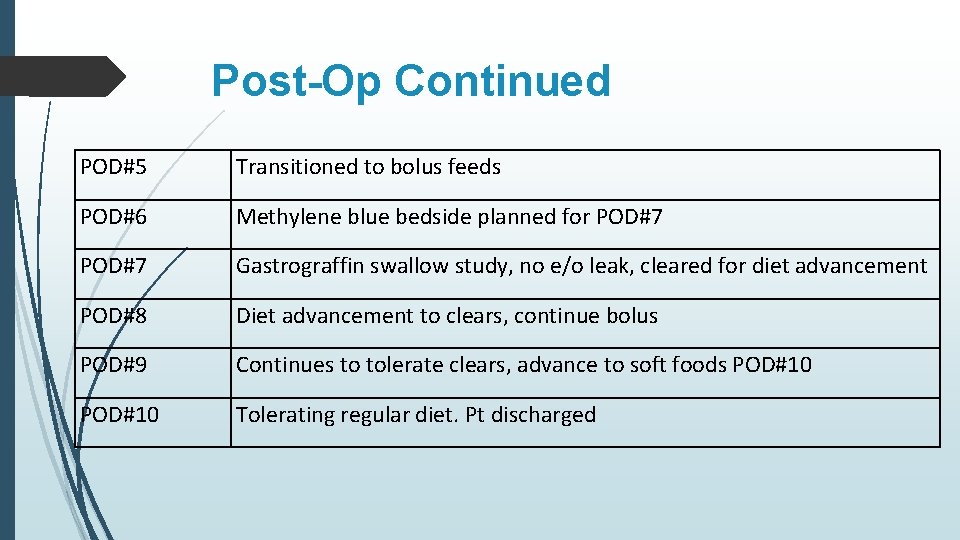
Post-Op Continued POD#5 Transitioned to bolus feeds POD#6 Methylene blue bedside planned for POD#7 Gastrograffin swallow study, no e/o leak, cleared for diet advancement POD#8 Diet advancement to clears, continue bolus POD#9 Continues to tolerate clears, advance to soft foods POD#10 Tolerating regular diet. Pt discharged
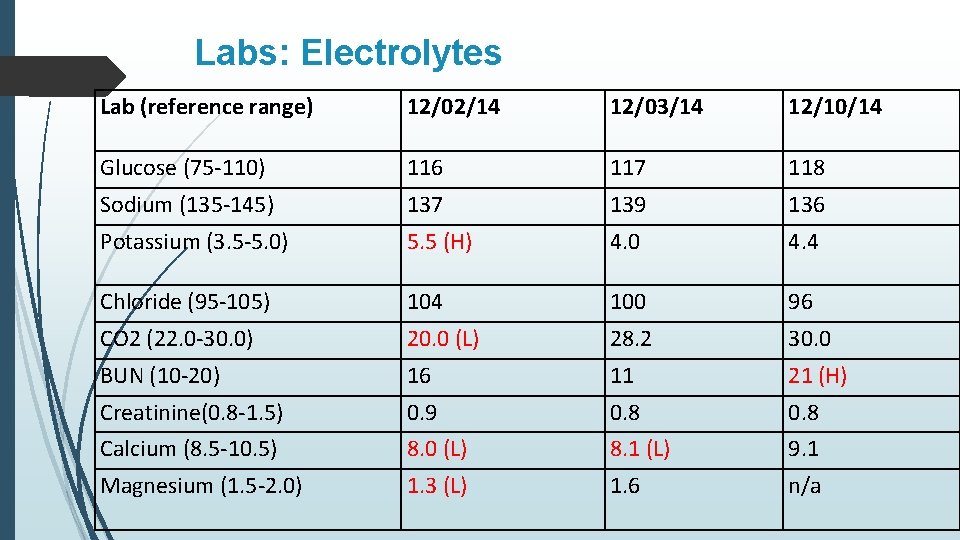
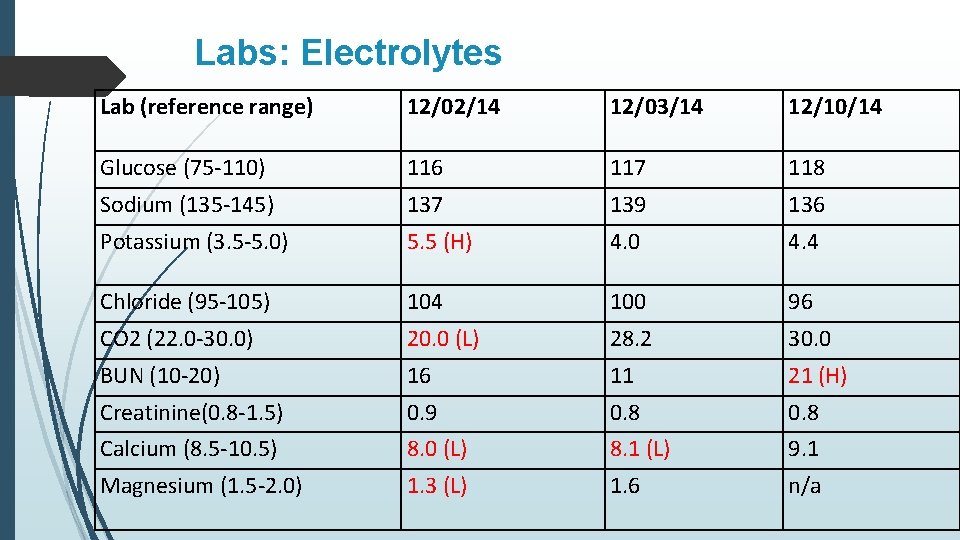
Labs: Electrolytes Lab (reference range) 12/02/14 12/03/14 12/10/14 Glucose (75 -110) 116 117 118 Sodium (135 -145) 137 139 136 Potassium (3. 5 -5. 0) 5. 5 (H) 4. 0 4. 4 Chloride (95 -105) 104 100 96 CO 2 (22. 0 -30. 0) 20. 0 (L) 28. 2 30. 0 BUN (10 -20) 16 11 21 (H) Creatinine(0. 8 -1. 5) 0. 9 0. 8 Calcium (8. 5 -10. 5) 8. 0 (L) 8. 1 (L) 9. 1 Magnesium (1. 5 -2. 0) 1. 3 (L) 1. 6 n/a
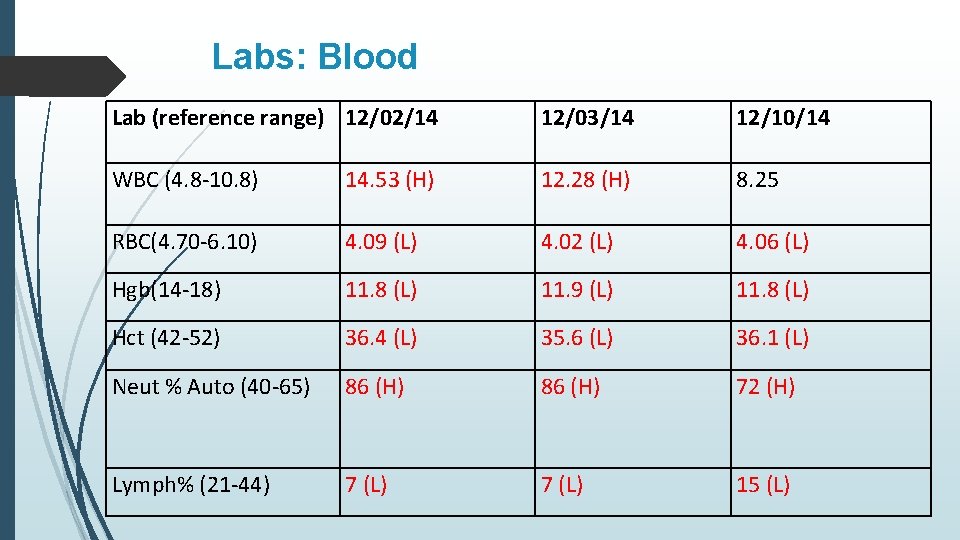
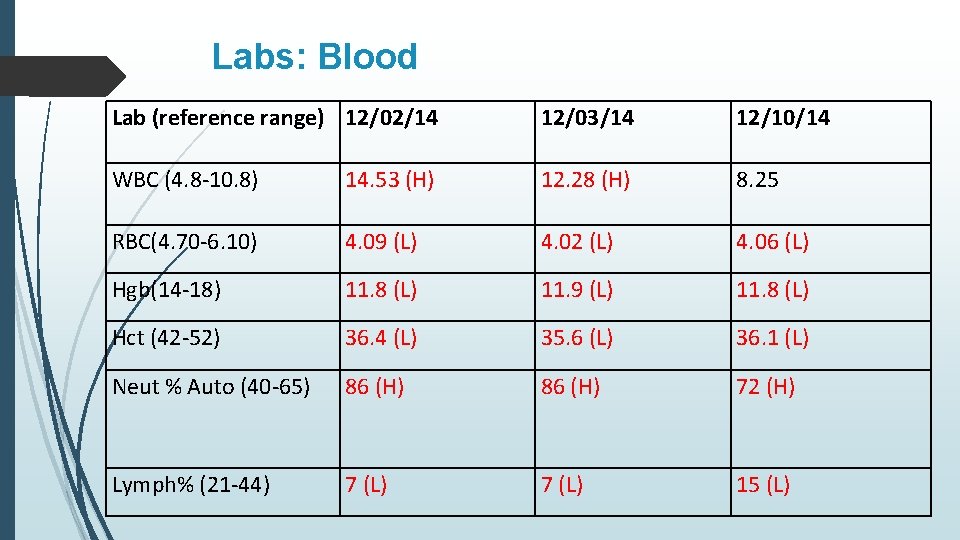
Labs: Blood Lab (reference range) 12/02/14 12/03/14 12/10/14 WBC (4. 8 -10. 8) 14. 53 (H) 12. 28 (H) 8. 25 RBC(4. 70 -6. 10) 4. 09 (L) 4. 02 (L) 4. 06 (L) Hgb(14 -18) 11. 8 (L) 11. 9 (L) 11. 8 (L) Hct (42 -52) 36. 4 (L) 35. 6 (L) 36. 1 (L) Neut % Auto (40 -65) 86 (H) 72 (H) Lymph% (21 -44) 7 (L) 15 (L)
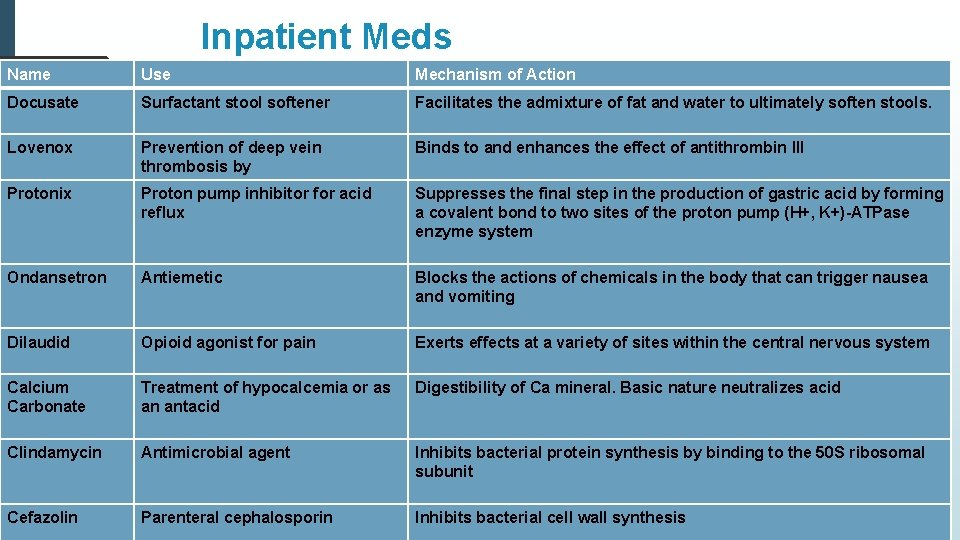
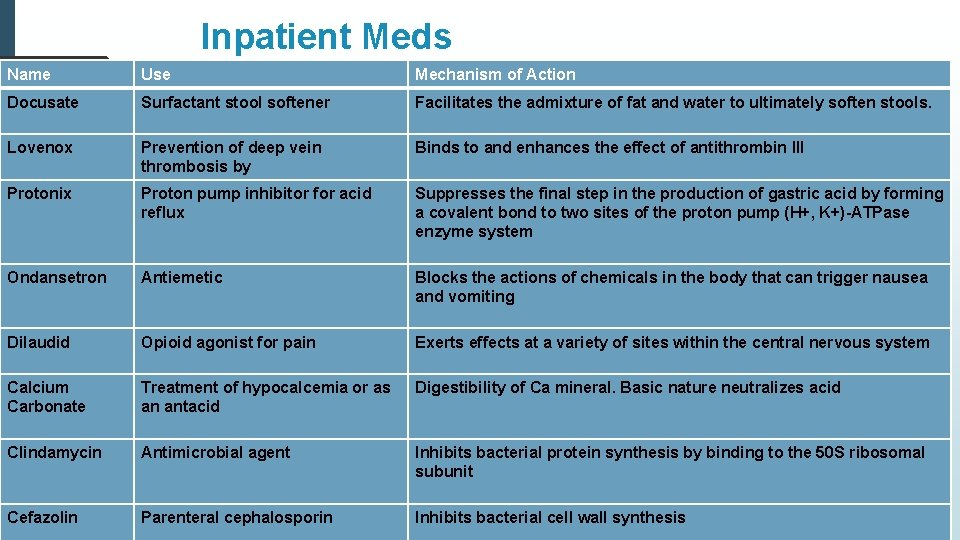
Inpatient Meds Name Use Mechanism of Action Docusate Surfactant stool softener Facilitates the admixture of fat and water to ultimately soften stools. Lovenox Prevention of deep vein thrombosis by Binds to and enhances the effect of antithrombin III Protonix Proton pump inhibitor for acid reflux Suppresses the final step in the production of gastric acid by forming a covalent bond to two sites of the proton pump (H+, K+)-ATPase enzyme system Ondansetron Antiemetic Blocks the actions of chemicals in the body that can trigger nausea and vomiting Dilaudid Opioid agonist for pain Exerts effects at a variety of sites within the central nervous system Calcium Carbonate Treatment of hypocalcemia or as an antacid Digestibility of Ca mineral. Basic nature neutralizes acid Clindamycin Antimicrobial agent Inhibits bacterial protein synthesis by binding to the 50 S ribosomal subunit Cefazolin Parenteral cephalosporin Inhibits bacterial cell wall synthesis
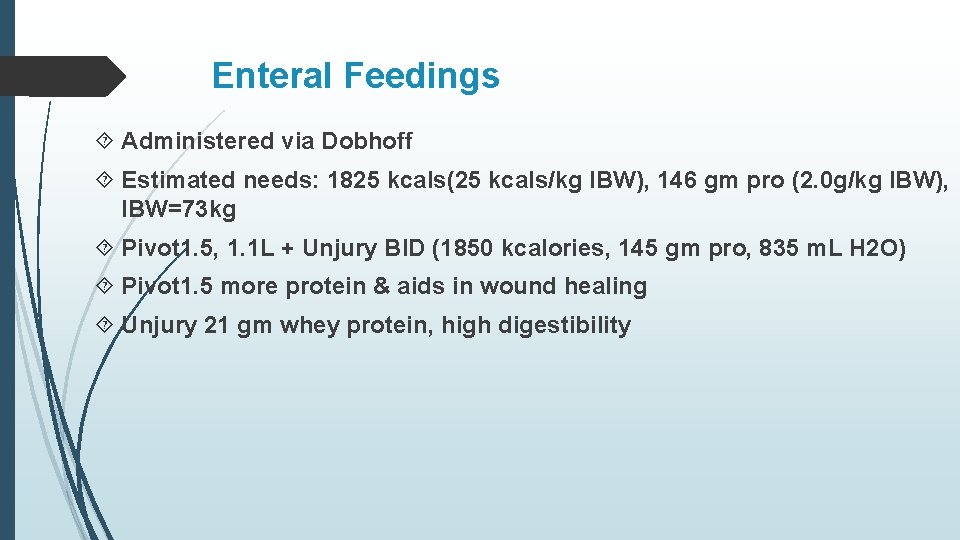
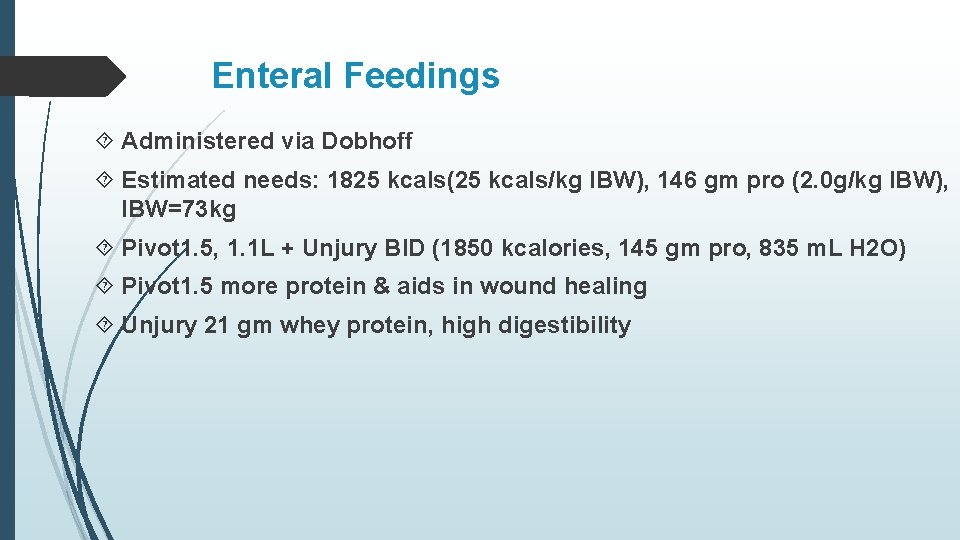
Enteral Feedings Administered via Dobhoff Estimated needs: 1825 kcals(25 kcals/kg IBW), 146 gm pro (2. 0 g/kg IBW), IBW=73 kg Pivot 1. 5, 1. 1 L + Unjury BID (1850 kcalories, 145 gm pro, 835 m. L H 2 O) Pivot 1. 5 more protein & aids in wound healing Unjury 21 gm whey protein, high digestibility
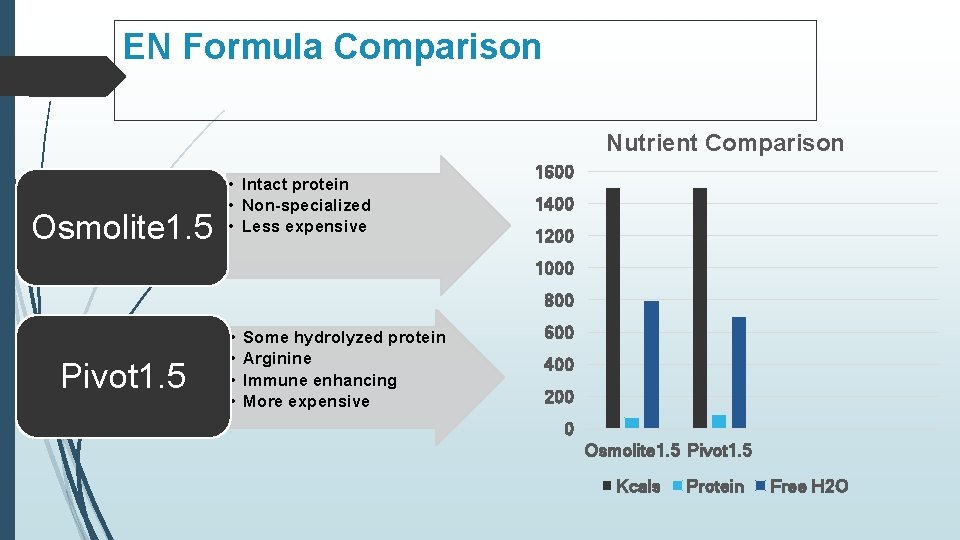
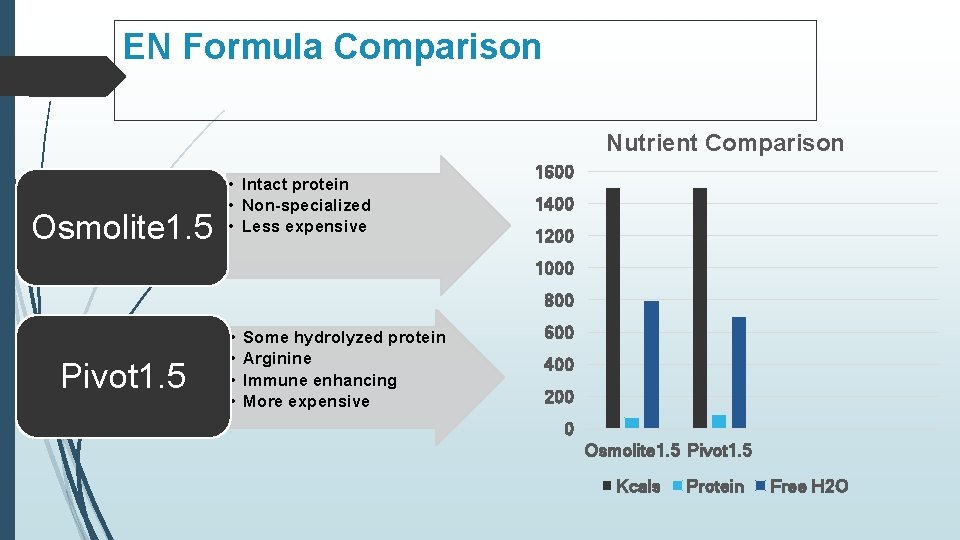
EN Formula Comparison Nutrient Comparison Osmolite 1. 5 • Intact protein • Non-specialized • Less expensive 1600 1400 1200 1000 800 Pivot 1. 5 • • Some hydrolyzed protein Arginine Immune enhancing More expensive 600 400 200 0 Osmolite 1. 5 Pivot 1. 5 Kcals Protein Free H 2 O
Adult Nutrition Initial Assessment Plan 12/02/14 POD#1 in ICU Pt seen at bedside +Trach w/ trach shield DHT in place, awaiting d/w ENT re: EN initiation Pt able to nod yes/no, write on paper Abd. Soft/NT/ND Nutrition Dx: Swallowing difficulty r/t recent tracheostomy a/e/b NPO; necessity of EN support to meet needs at present. Goals: EN infusing at goal rate High risk, f/u 2 -4 days
Adult Nutrition Reassessment Plan 12/04/14 POD#3 Pt seen at bedside, in good spirits, active conversationalist DHT in place, running at goal rate 50 m. L/hr, tolerating well No N/V/abdominal pain Loose stool and painful swallowing D/w pt re: transition to bolus feeds, pt agreeable. Zofran PRN Nutrition Dx: Swallowing difficult r/t recent tracheostomy a/e/b NPO; necessity of EN support to meet needs (ongoing). Goals: Tolerance of bolus feeds (4 x 275 m. L), d/c bowel regimen Moderate risk, f/u 5 -7 days
Adult Nutrition Reassessment Plan 12/09/14 POD #8 Interval Hx: s/p gastrograffin swallow exam, no e/o leak Pt seen pleasantly consuming clear liquids Tolerating bolus w/ mild discomfort No N/V/D/abd pain Nutrition Dx: Inadequate oral intake r/t recent tracheostomy a/e/b necessity of EN support to meet needs (revised). Goals: Cont. tolerance to bolus, consume 75 -100% CLD, 1 -2 Ensure Clears daily High Risk, f/u 2 -4 days
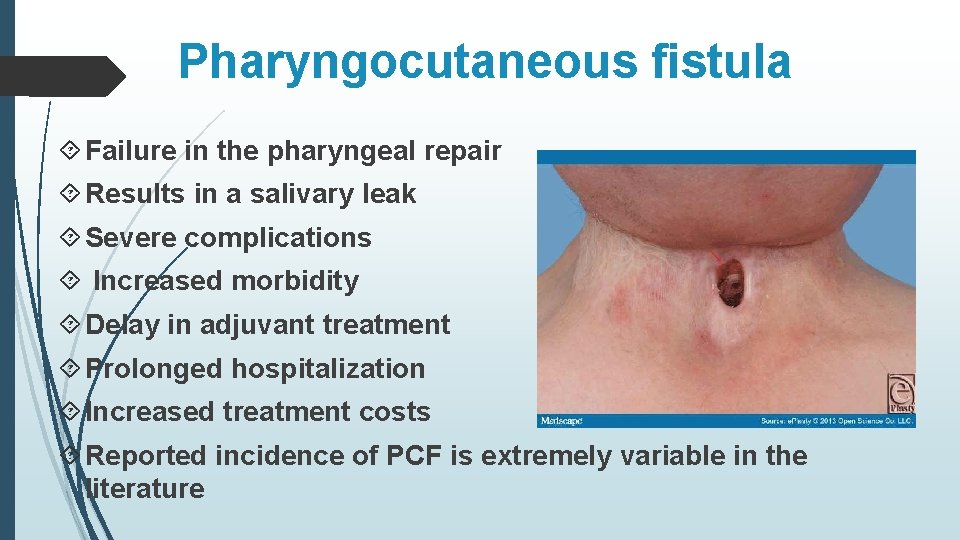
Initiation of Oral Intake Usually at least POD#7 Must have exam (gastrograffin) to evaluate for leaks Complications can occur if pharyngeal suture line is not healed Pharyngocutaneous fistula occurrence…debatable
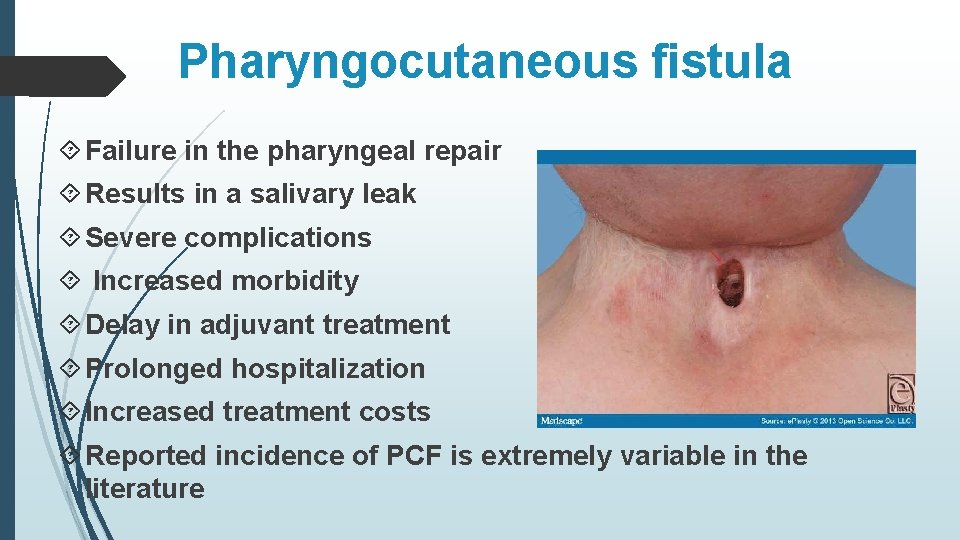
Pharyngocutaneous fistula Failure in the pharyngeal repair Results in a salivary leak Severe complications Increased morbidity Delay in adjuvant treatment Prolonged hospitalization Increased treatment costs Reported incidence of PCF is extremely variable in the literature
Interdisciplinary History Prior to Discharge 12/10/14 ENT-advanced to mechanical soft diet 12/10/14 SLP- ready for diet advancement 12/11/14 A. M. - tolerating mech. softs, advanced to regular diet. Ready for d/c 12/11/14 P. M. -d/c on regular diet Outpatient Rx Percocet for pain Colace for constipation Bacitracin ointment at surgical site
Outpatient Progress POD#17 SLP trialed thin and nectar thick liquids no e/o leakage POD#36 SLP trialed thin liquids trace leakage through TEP 1/5 -1/6 trials plans for readjustment of TEP
Well Done GD! Thank you to the wonderful and talented registered dietitians at GWU that have taught me so much and have been an inspiration throughout this process! Mary Gergely, RD, LD, CNM Mary Baginsky, MS, RD, LD, CNCS Elaine Ferrel, RD, LD Lauren Trahan, MS, RD, LD Sarah Swaintek, RD, LD Leah,