THINGS THE ENT RESIDENTS WANT YOU TO KNOW






- Slides: 58
THINGS THE ENT RESIDENTS WANT YOU TO KNOW ANDREA ZIEGLER PGY-5 8/16/2019
OUTLINE Tracheotomy Laryngectomy Epistaxis Angioedema Acute Invasive Fungal Sinusitis Mastoid effusions vs mastoiditis
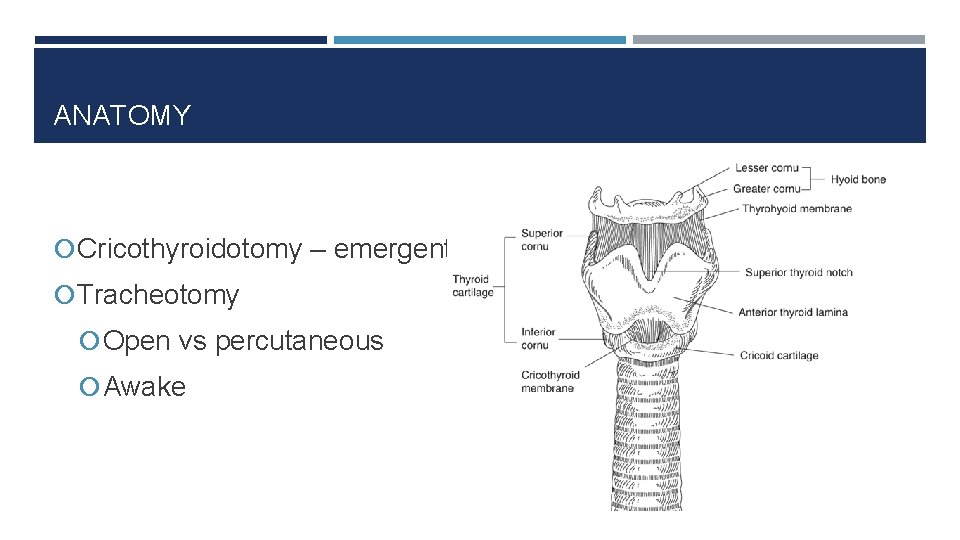
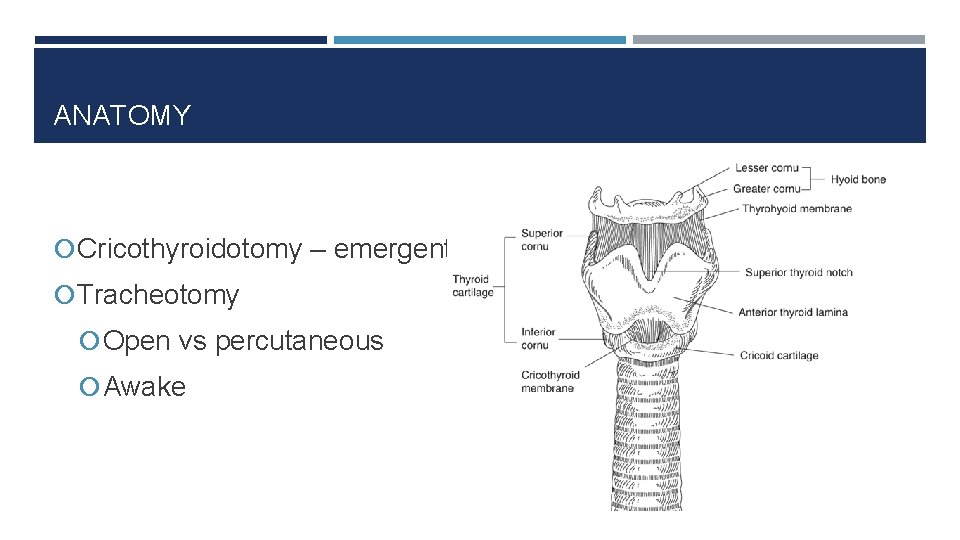
ANATOMY Cricothyroidotomy – emergent Tracheotomy Open vs percutaneous Awake
CRICOTHYROIDOTOMY • Emergent surgical airway needed, and tracheostomy not possible • Risk of damage to subglottis • Relative CI: peds < 12 yo, infected larynx, laryngeal cancer, laryngeal trauma • Revise early to avoid subglottic stenosis
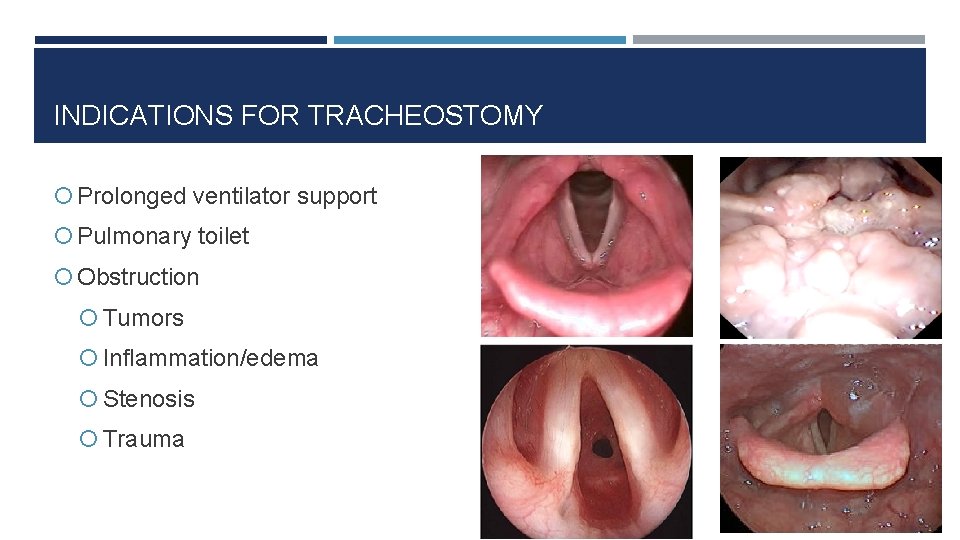
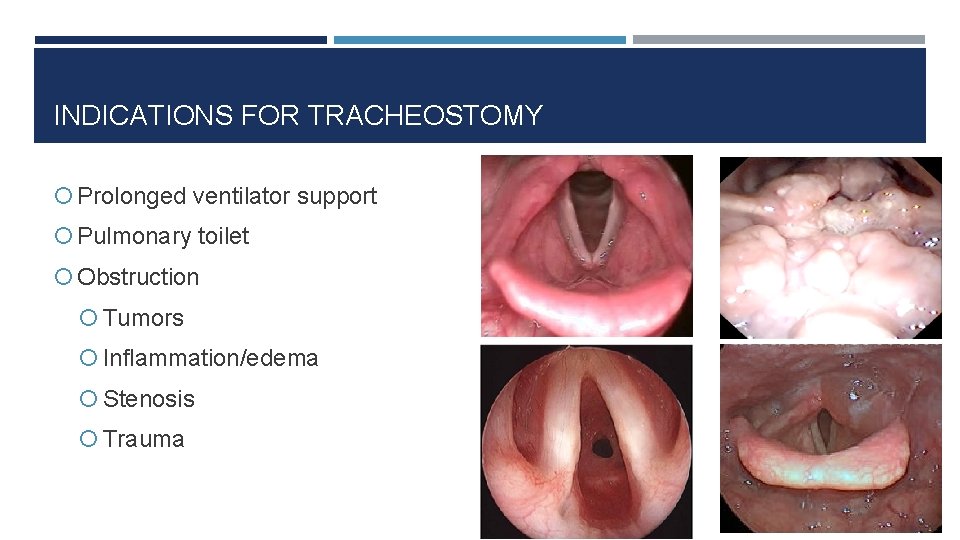
INDICATIONS FOR TRACHEOSTOMY Prolonged ventilator support Pulmonary toilet Obstruction Tumors Inflammation/edema Stenosis Trauma
PROLONGED RESPIRATORY SUPPORT • Rationale • 7 -10 days of intubation typically acceptable • Complications associated w/ longer intubation • Capillary perfusion pressure ≈ 30 cm H 2 O • Subglottis most susceptible (cricoid = complete ring) • Benefits • Lower sedation requirements • Ventilator weaning • Trach collar trials vs. re-intubation • Better pulmonary toilet
In adult patients with prolonged ventilation, early tracheostomy (within 7 -14 days), is associated with significant reduction in hospital acquired pneumonia, incidence of mortality, duration of mechanical ventilation, and length of stay in ICU

TRACHEOSTOMY CONSULTS • No imminent extubation or withdrawal of care • Preferences • Anticoagulants that can be held • No vasopressors/stable vasopressor requirements • Fi. O 2 ~ 40% • Family/patient discussion
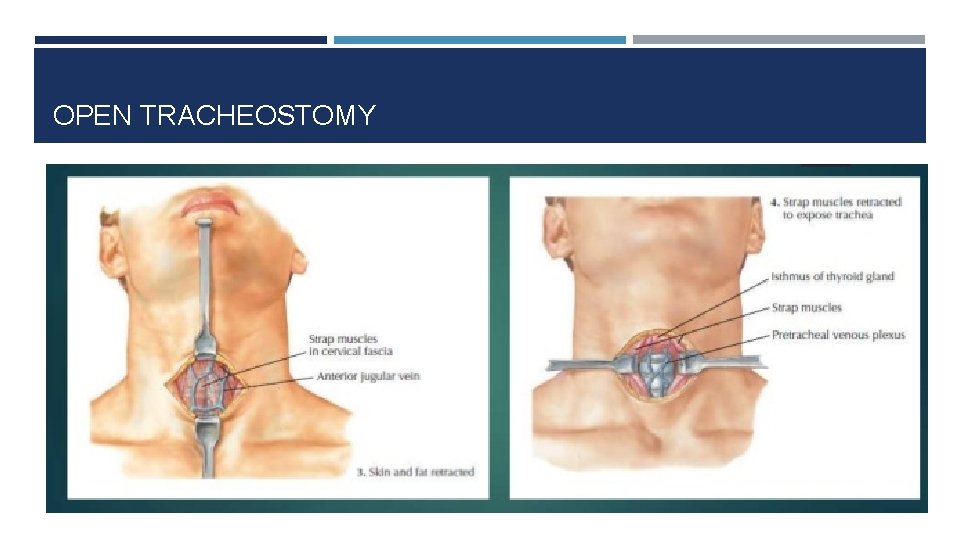
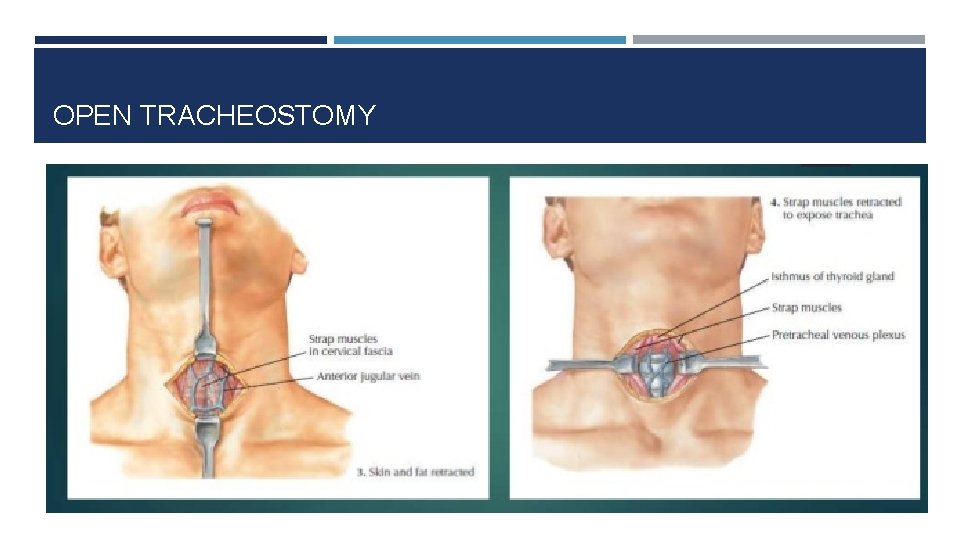
OPEN TRACHEOSTOMY
PERCUTANEOUS TRACHEOSTOMY • Less time, less expensive, bedside • Bronchoscopy required • Contraindications • • • Enlarged thyroid Previous neck surgery Obesity Calcified tracheal rings Non-intubated Pediatric patient (relative)
PERCUTANEOUS VS OPEN? No significant difference in minor or major complications Cadaver studies show significantly more mucosal and cartilage damage in percutaneous group Could translate to increased risk of subglottis stenosis and difficult decannulation but has not been shown in studies
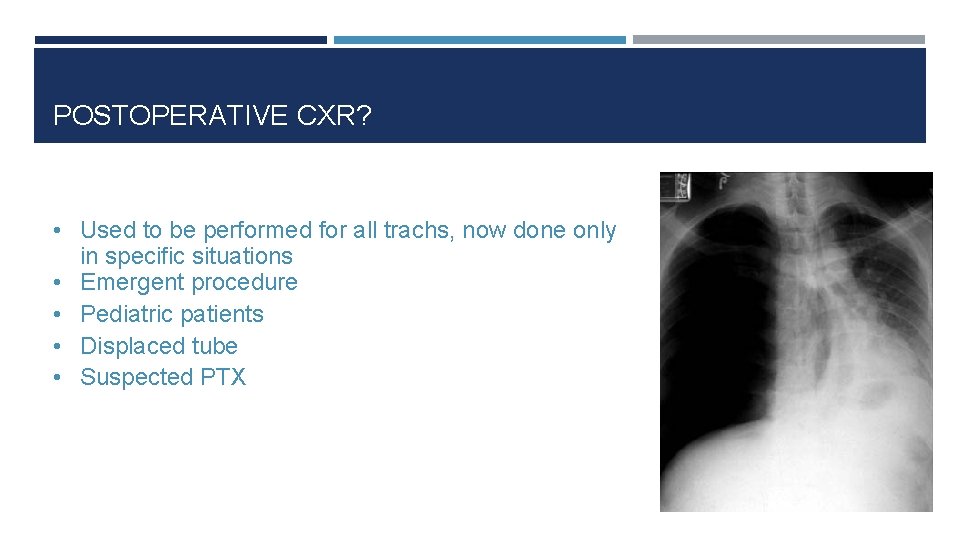
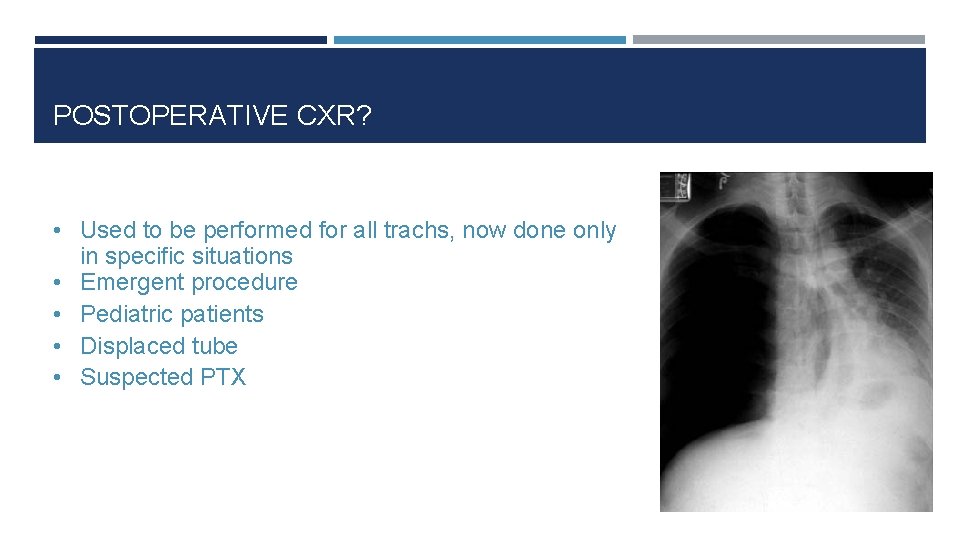
POSTOPERATIVE CXR? • Used to be performed for all trachs, now done only • • in specific situations Emergent procedure Pediatric patients Displaced tube Suspected PTX

PARTS OF A TRACH Obturator Inner cannula Cuffed trach Reading the faceplate Brand (Shiley, Portex, Bivona) Size (4, 6, 8) Type DCT = cuffed CFS= cuffless
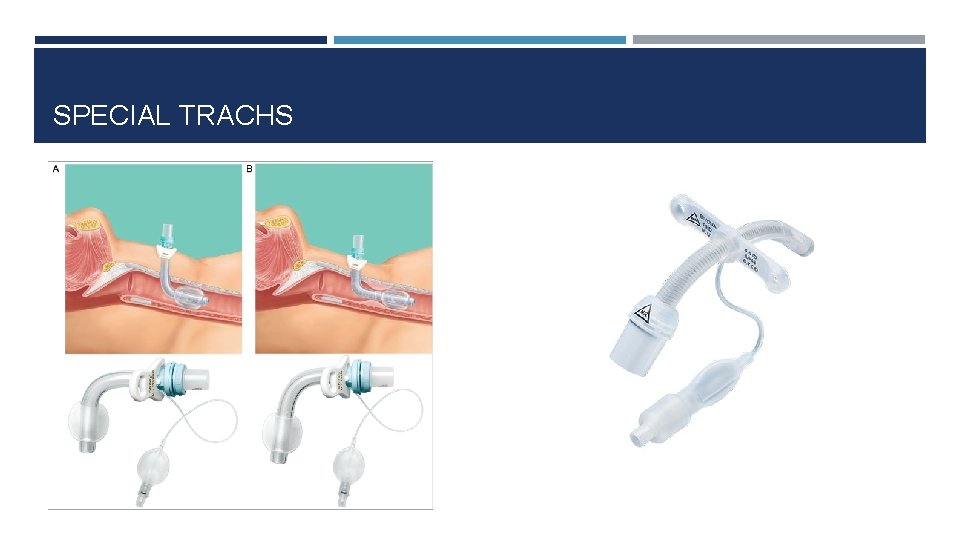
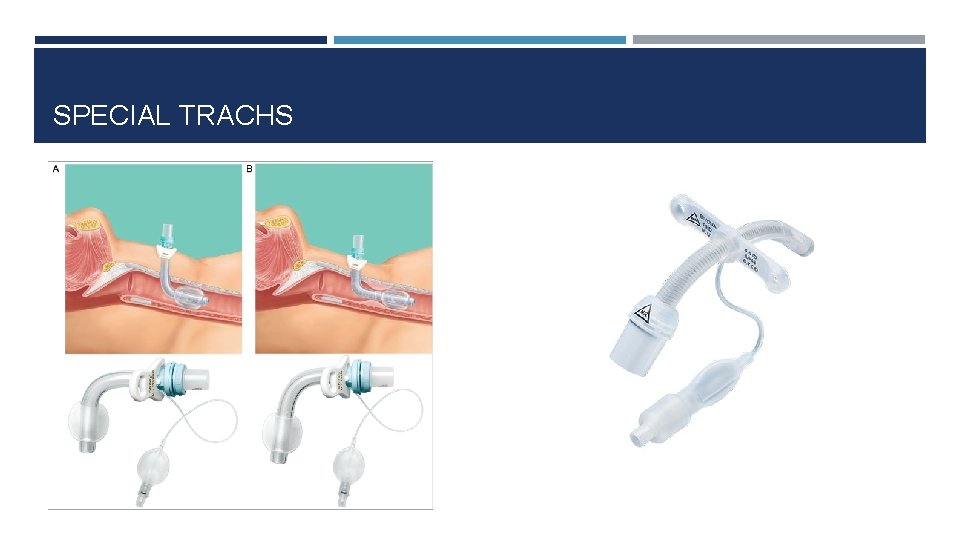
SPECIAL TRACHS
POSTOPERATIVE ORDERS • • • Extra tube to bedside Suction q 1 hrs and PRN Tape obturator above bed “Patient is neck breather” Clean/change inner cannula q 8 hrs and PRN
EARLY COMPLICATIONS • Tube obstruction (mucous plugs) • Humidification, frequent suctioning/irrigation • Accidental displacement/decannulation • Recognition and replacement • Post-obstructive pulmonary edema • Mechanical ventilation, PEEP, diuretics • Tracheitis • Regular trach changes, Ciprofloxacin
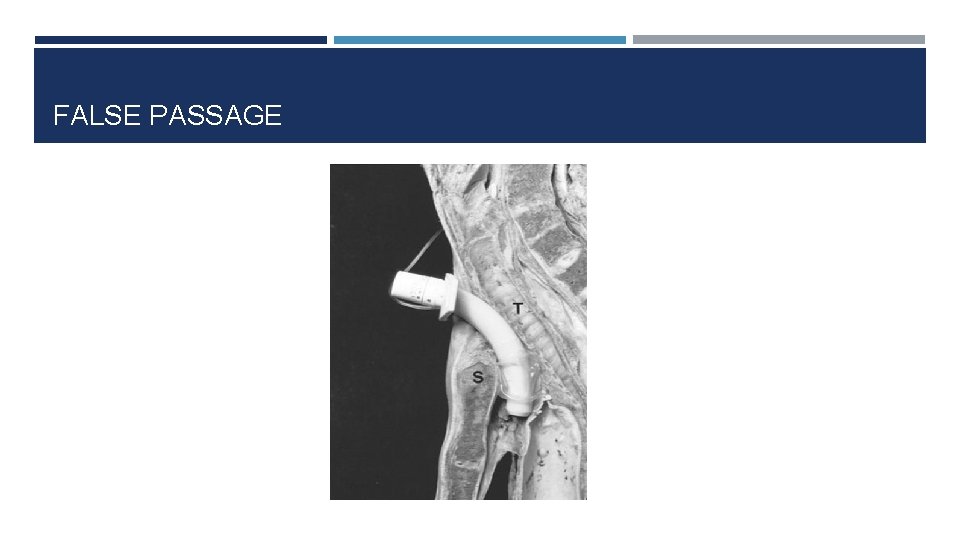
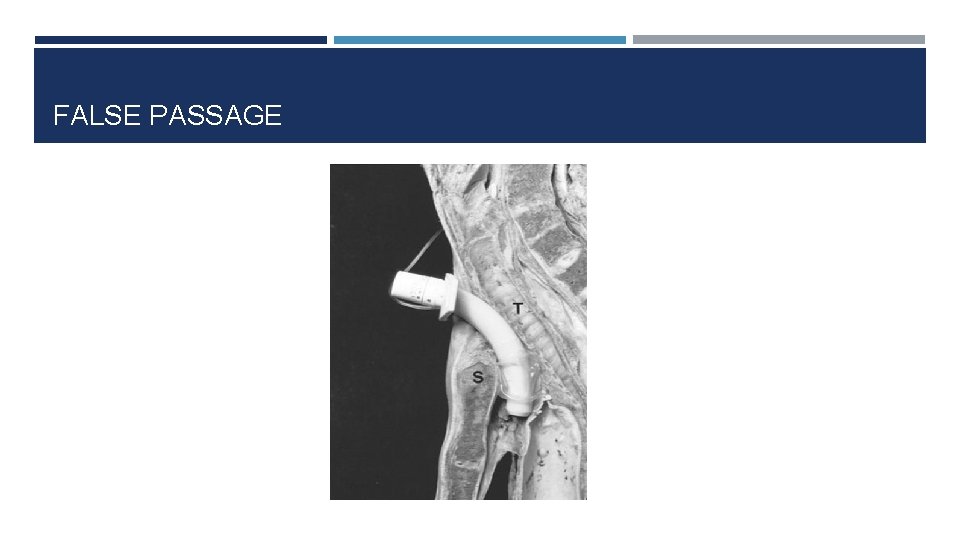
FALSE PASSAGE
DIFFICULTY VENTILATING • Call ENT • Assess tube patency: • Remove and replace inner cannula, suction • Check return volumes, auscultate chest • 100% oxygen • Bag mask • Deflate cuff • Bedside scope • False tract or decannulation • <5 days – caution • >5 days – attempt to replace • Endotracheal intubation
LONG TERM COMPLICATIONS • Stenosis • Goal cuff pressures < 25 cm H 2 O • Allow slight air leak or no cuff in kids • Granulation tissue • Bleeding • <48 h: usually incision • >48 h: r/o tracheoinnominate fistula (TIF) • Tracheocutaneous fistula (post-decannulation)
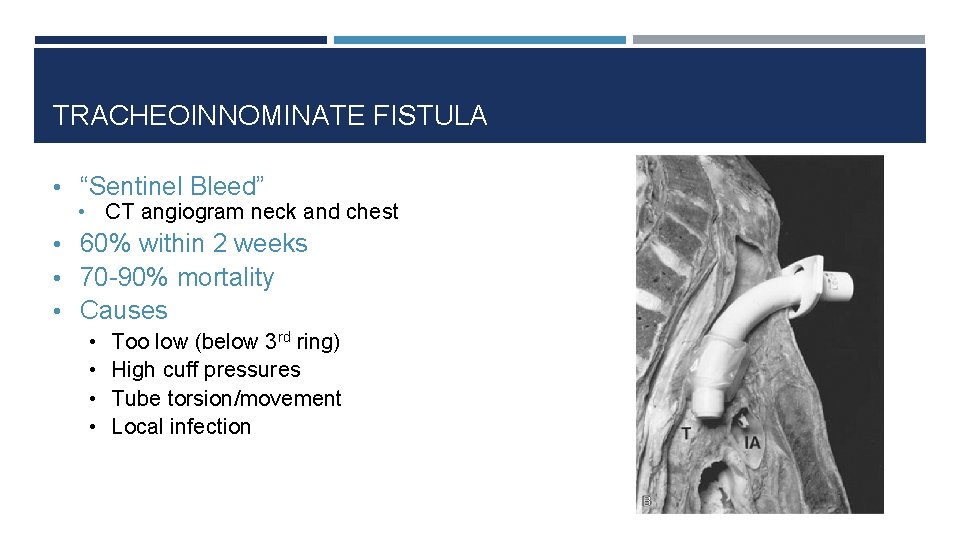
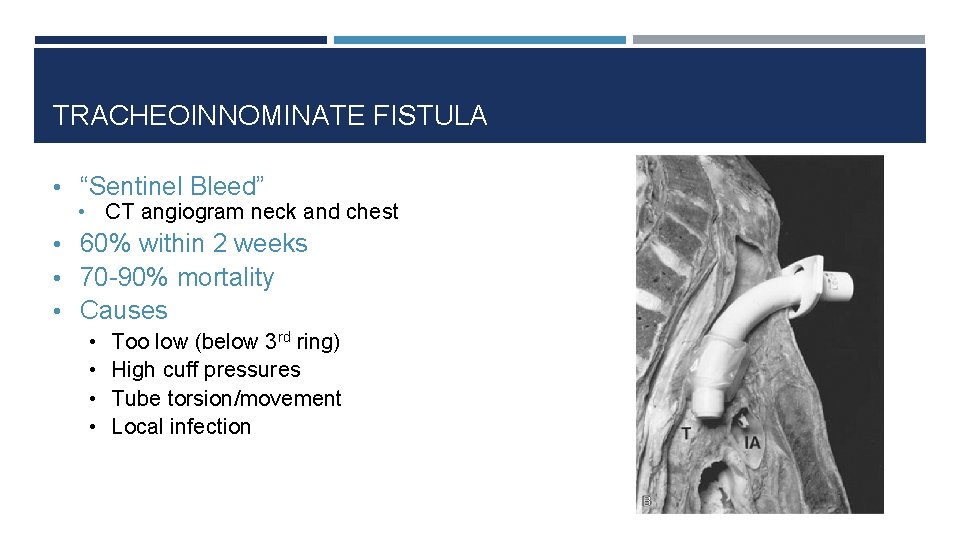
TRACHEOINNOMINATE FISTULA • “Sentinel Bleed” • CT angiogram neck and chest • 60% within 2 weeks • 70 -90% mortality • Causes • • Too low (below 3 rd ring) High cuff pressures Tube torsion/movement Local infection
MANAGEMENT OF TI FISTULA • • • ENT & Thoracic Surgery Overinflate cuff or… Pass ETT below level of bleed Compress innominate against sternum with finger anterior to trachea Definitive treatment: ligate innominate artery
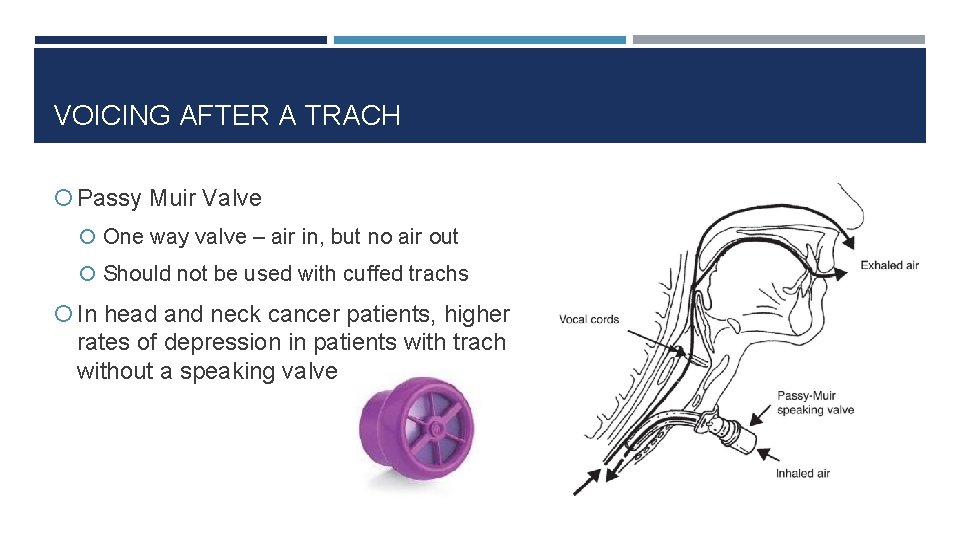
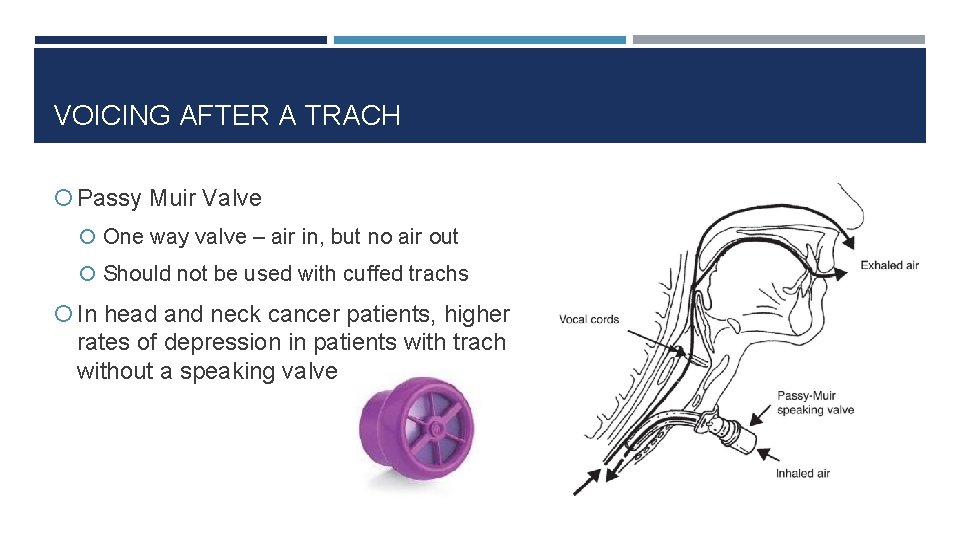
VOICING AFTER A TRACH Passy Muir Valve One way valve – air in, but no air out Should not be used with cuffed trachs In head and neck cancer patients, higher rates of depression in patients with trach without a speaking valve
PO INTAKE AFTER TRACH • Many patients will aspirate on VFSS test with new tracheostomy • Often easier for patient to eat once trach is downsized or cuff is deflated • Decannulation, capping, or PMV should be attempted in patients w/ trach to help with aspiration • Speech pathology will help in rehabilitation
DECANNULATION • Original indication for trach resolved • Including no additional planned treatment or procedures • No further need for aggressive pulmonary toilet • Capping trial • Decannulation • Tape (wound reinforcement) • Education (during speech, coughing) • Surgical closure for failures
PREVIOUSLY PLACED TRACHS If placed by another service, they should be notified first of any issues and we are available to help Can evaluate previously placed trachs if having issues
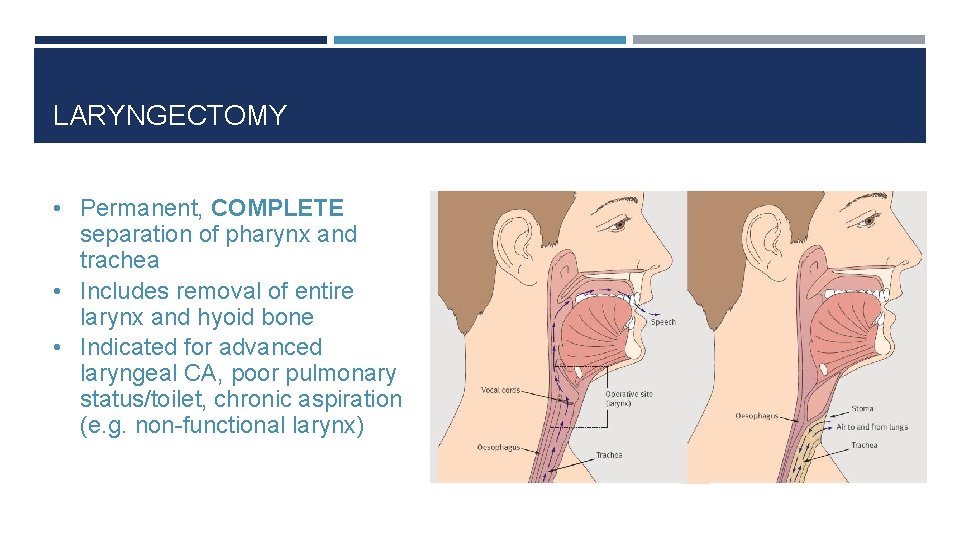
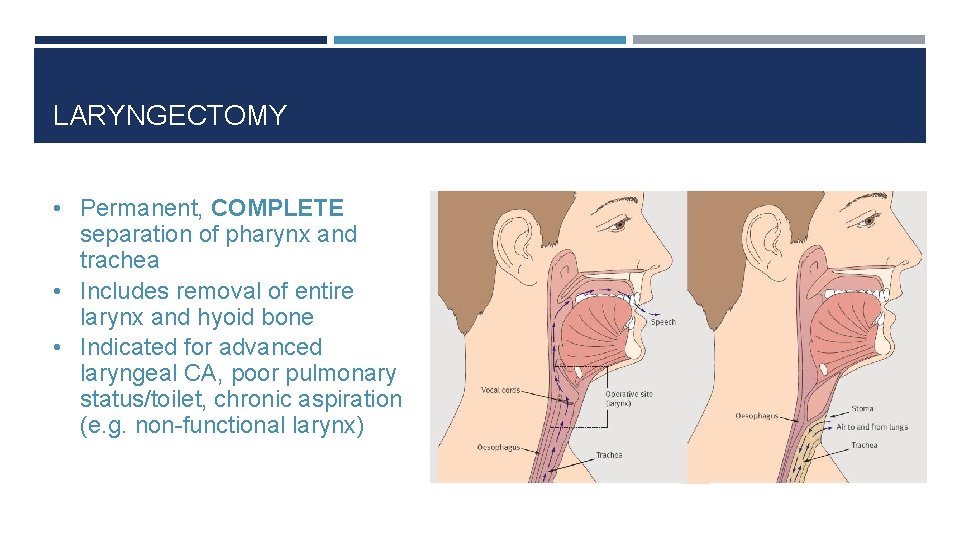
LARYNGECTOMY • Permanent, COMPLETE separation of pharynx and trachea • Includes removal of entire larynx and hyoid bone • Indicated for advanced laryngeal CA, poor pulmonary status/toilet, chronic aspiration (e. g. non-functional larynx)
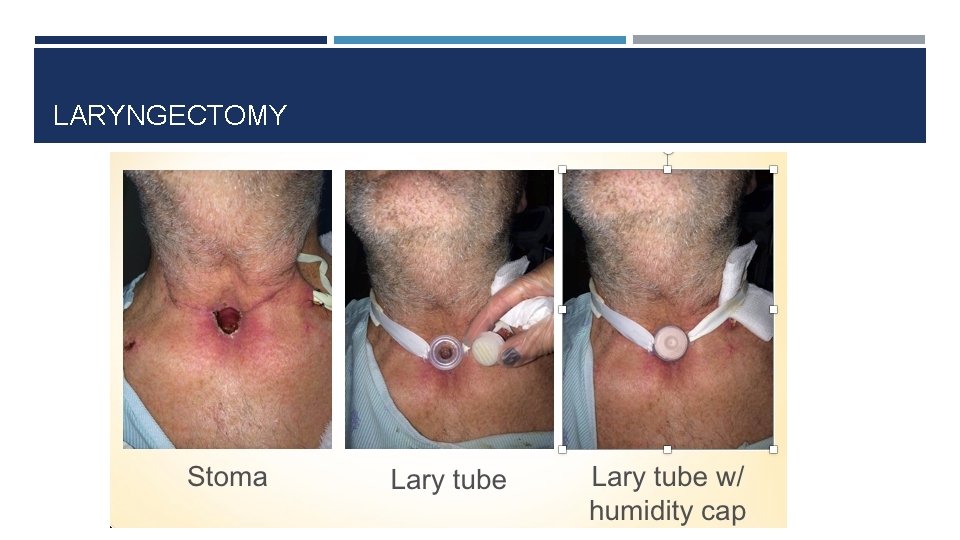
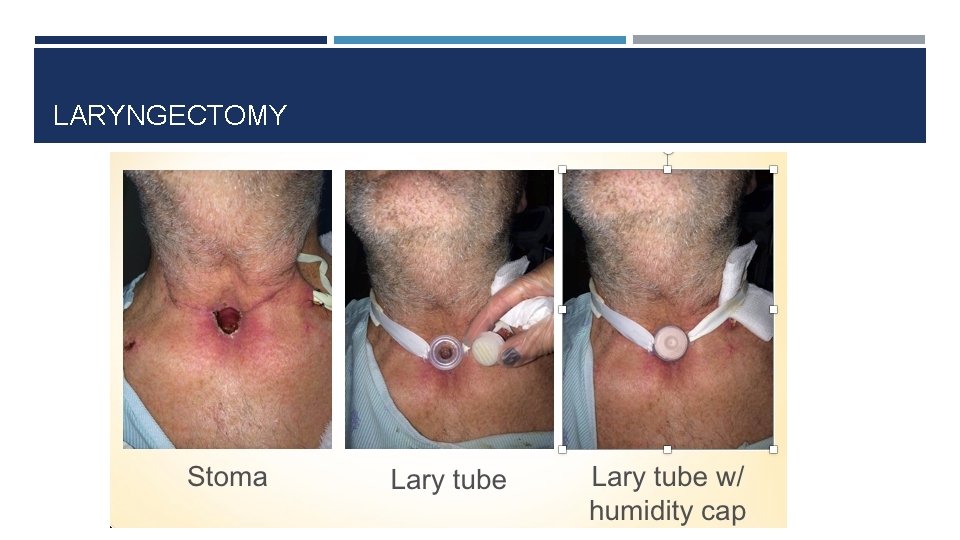
LARYNGECTOMY
LARYNGECTOMY PEARLS • Do not try to intubate through the mouth for any reason • Stomal intubation only • Humidification/trach collar (no nasal O 2) • Saline squirts • Suction (red rubber catheters) • These patients ARE NOT ASPIRATING


EPISTAXIS
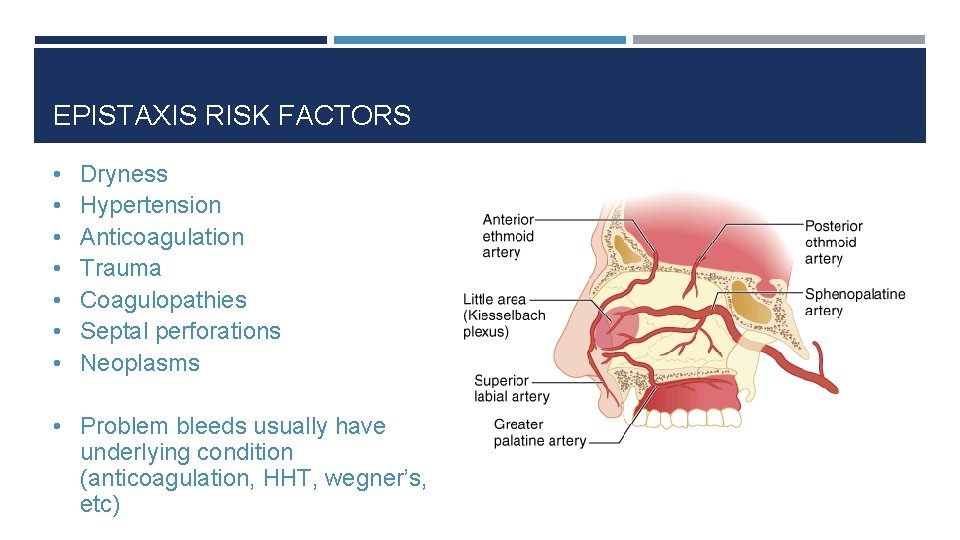
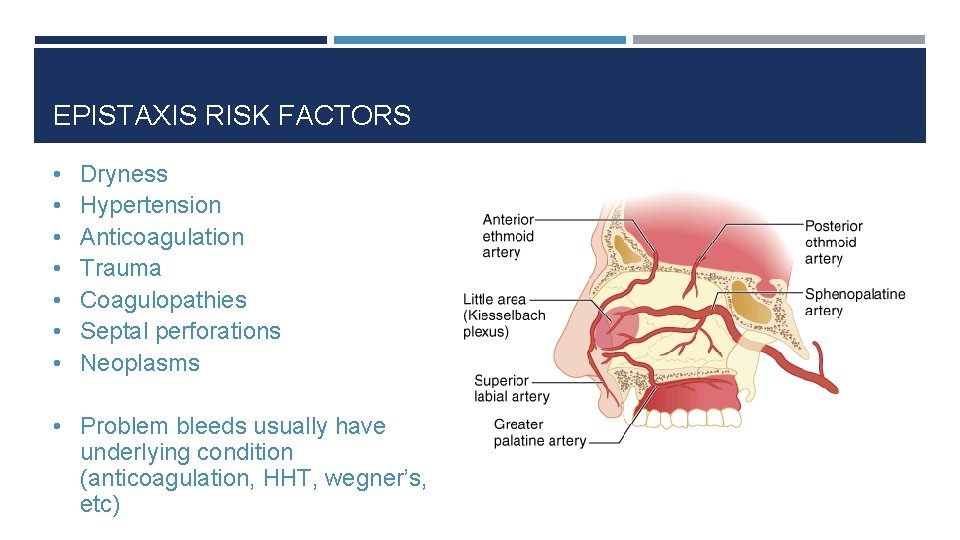
EPISTAXIS RISK FACTORS • • Dryness Hypertension Anticoagulation Trauma Coagulopathies Septal perforations Neoplasms • Problem bleeds usually have underlying condition (anticoagulation, HHT, wegner’s, etc)
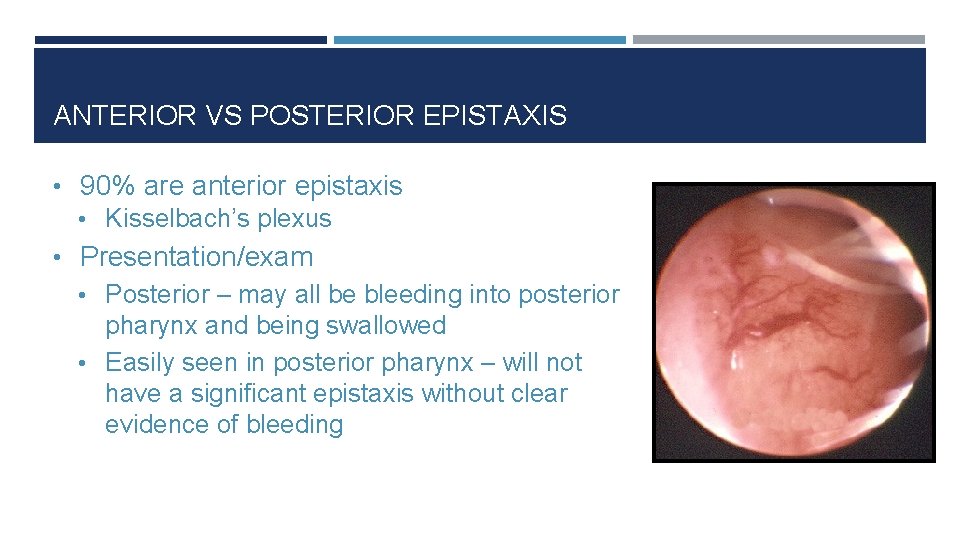
ANTERIOR VS POSTERIOR EPISTAXIS • 90% are anterior epistaxis • Kisselbach’s plexus • Presentation/exam • Posterior – may all be bleeding into posterior pharynx and being swallowed • Easily seen in posterior pharynx – will not have a significant epistaxis without clear evidence of bleeding
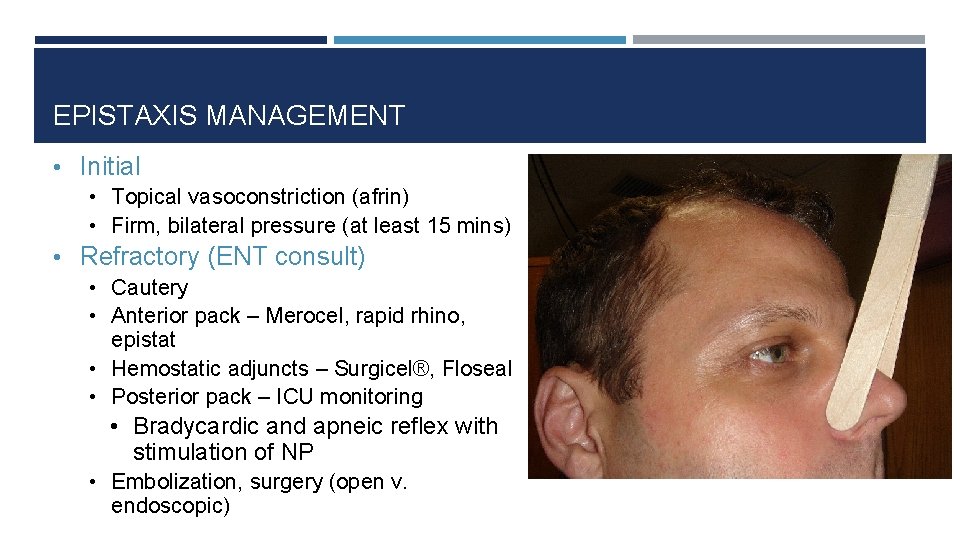
EPISTAXIS MANAGEMENT • Initial • Topical vasoconstriction (afrin) • Firm, bilateral pressure (at least 15 mins) • Refractory (ENT consult) • Cautery • Anterior pack – Merocel, rapid rhino, epistat • Hemostatic adjuncts – Surgicel®, Floseal • Posterior pack – ICU monitoring • Bradycardic and apneic reflex with stimulation of NP • Embolization, surgery (open v. endoscopic)

ADDITIONAL EPISTAXIS MANAGEMENT • Blood pressure • Coagulopathy • Fluid repletion • Transfusion • Antibiotics (packing) • Nasal saline spray QID, Vaseline to septum BID, humidifier
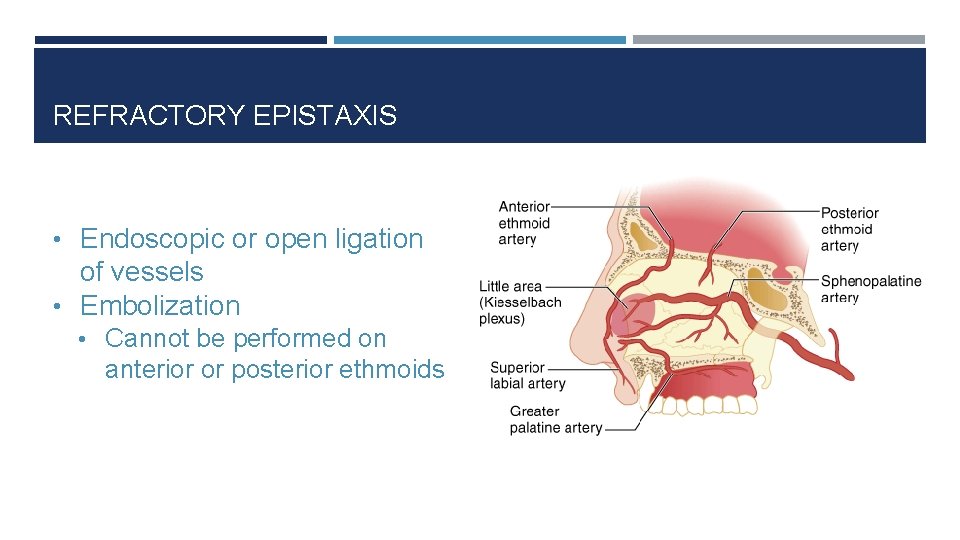
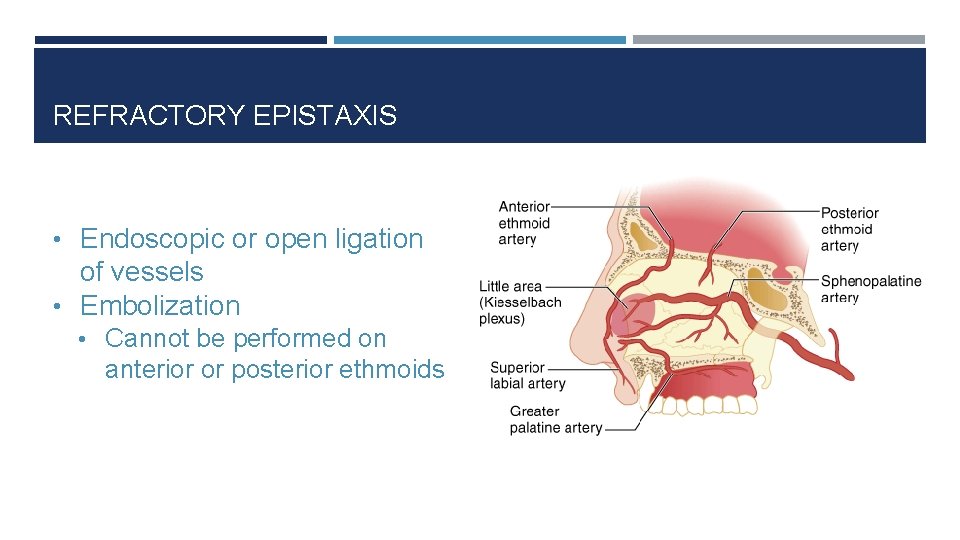
REFRACTORY EPISTAXIS • Endoscopic or open ligation of vessels • Embolization • Cannot be performed on anterior or posterior ethmoids
ANGIOEDEMA
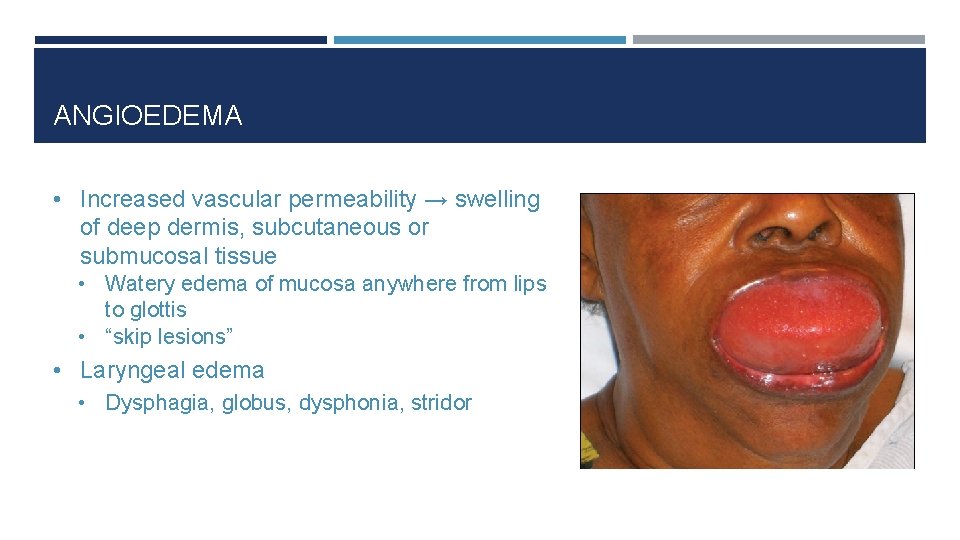
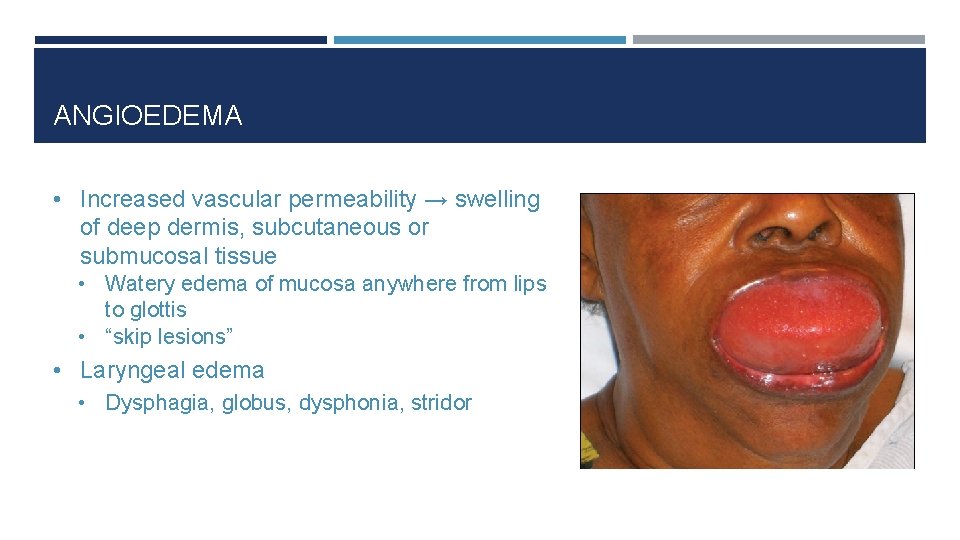
ANGIOEDEMA • Increased vascular permeability → swelling of deep dermis, subcutaneous or submucosal tissue • Watery edema of mucosa anywhere from lips to glottis • “skip lesions” • Laryngeal edema • Dysphagia, globus, dysphonia, stridor
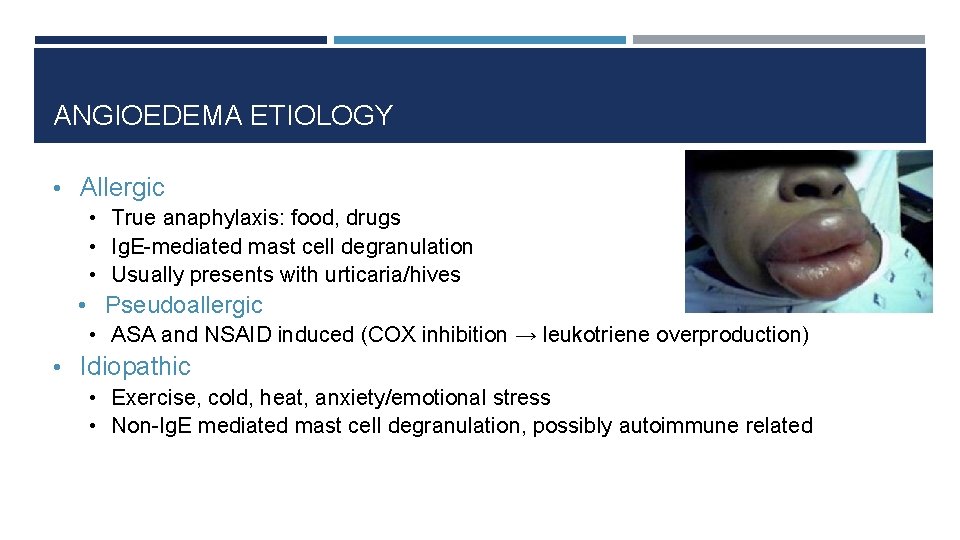
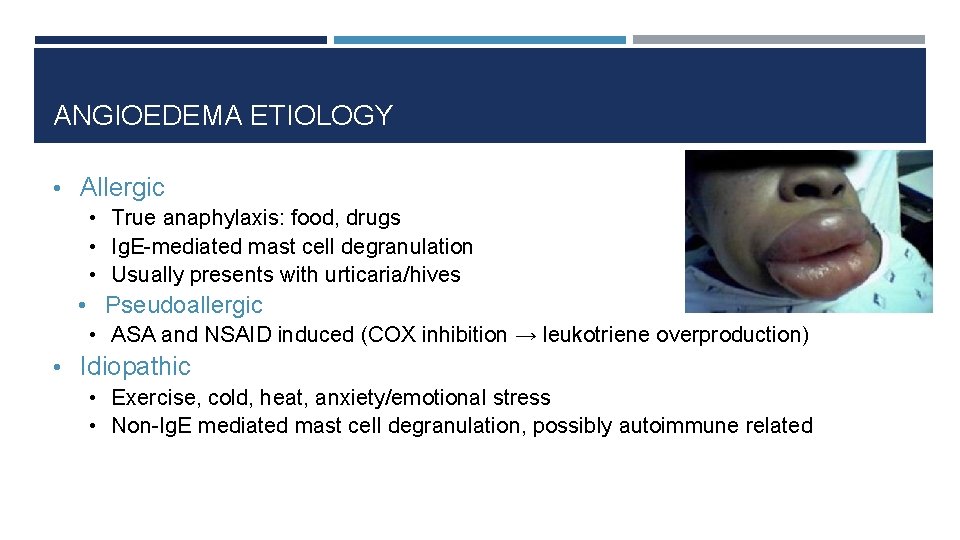
ANGIOEDEMA ETIOLOGY • Allergic • True anaphylaxis: food, drugs • Ig. E-mediated mast cell degranulation • Usually presents with urticaria/hives • Pseudoallergic • ASA and NSAID induced (COX inhibition → leukotriene overproduction) • Idiopathic • Exercise, cold, heat, anxiety/emotional stress • Non-Ig. E mediated mast cell degranulation, possibly autoimmune related
ANGIOEDEMA ETIOLOGY • Non-Allergic/drug induced: bradykinin mediated • ACE inhibitor-induced • Bradykinin = potent vasodilator, inactivated by ACE • ACE-I → increased bradykinin levels • African-Americans 3. 0 -4. 5 RR • Hereditary angioedema • decreased C 1 inhibitor production • Acquired angioedema • C 1 inhibitor auto-antibodies
TREATMENT • Evaluate and secure airway, NPO in case need to secure airway in the future • 0. 3 ml 1: 1, 000 IM or 0. 3 ml 1: 100, 000 IV epinephrine if acute life threatening • IV methylprednisolone (Solumedrol) 100 -125 mg IV once – works quickly • IV diphenhydramine • IV ranitidine or pepcid • IV decadron • FFP for hereditary type (contains C 1 inhibitor)
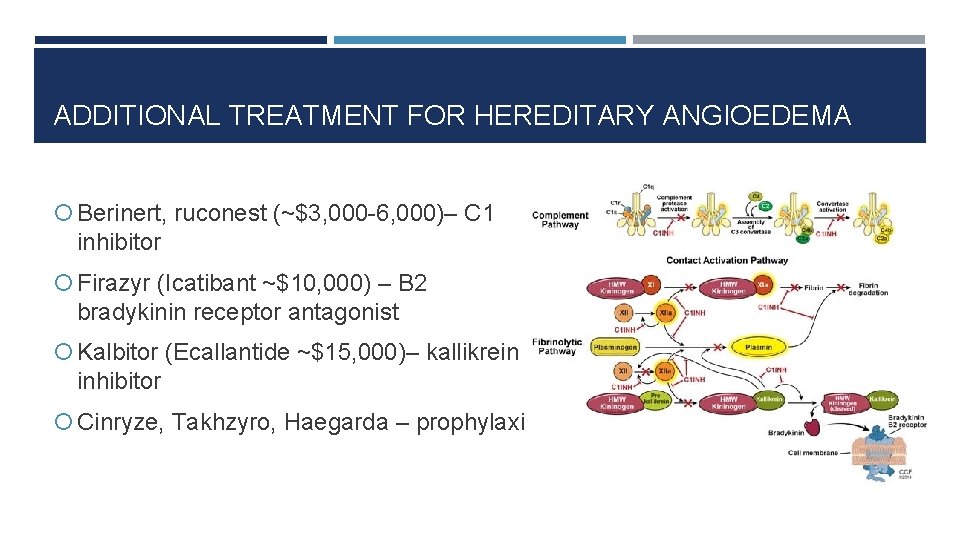
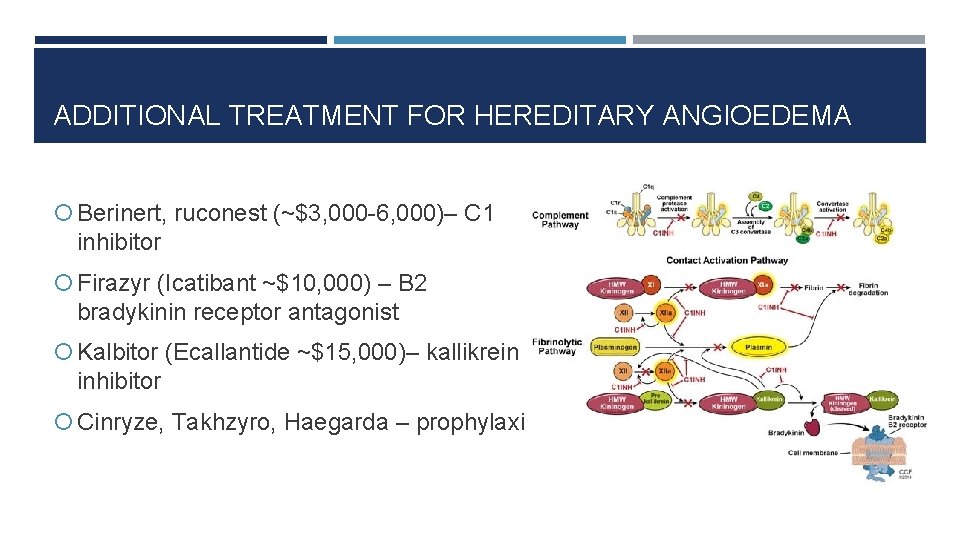
ADDITIONAL TREATMENT FOR HEREDITARY ANGIOEDEMA Berinert, ruconest (~$3, 000 -6, 000)– C 1 inhibitor Firazyr (Icatibant ~$10, 000) – B 2 bradykinin receptor antagonist Kalbitor (Ecallantide ~$15, 000)– kallikrein inhibitor Cinryze, Takhzyro, Haegarda – prophylaxis
TREATMENT Gen med obs for minor oral cavity involvement MICU for severe or laryngeal involvement Serial exams – look for improvement, not necessarily resolution before starting PO +/- steroid taper Allergy referral for recurrent episodes
INVASIVE FUNGAL SINUSITIS
INVASIVE FUNGAL SINUSITIS • No risk to immuno-competent host, always in immunocompromised • Characterized by fungal angioinvasion → ischemia and necrosis • Rapid tissue destruction • High mortality even with treatment (up to 50%)
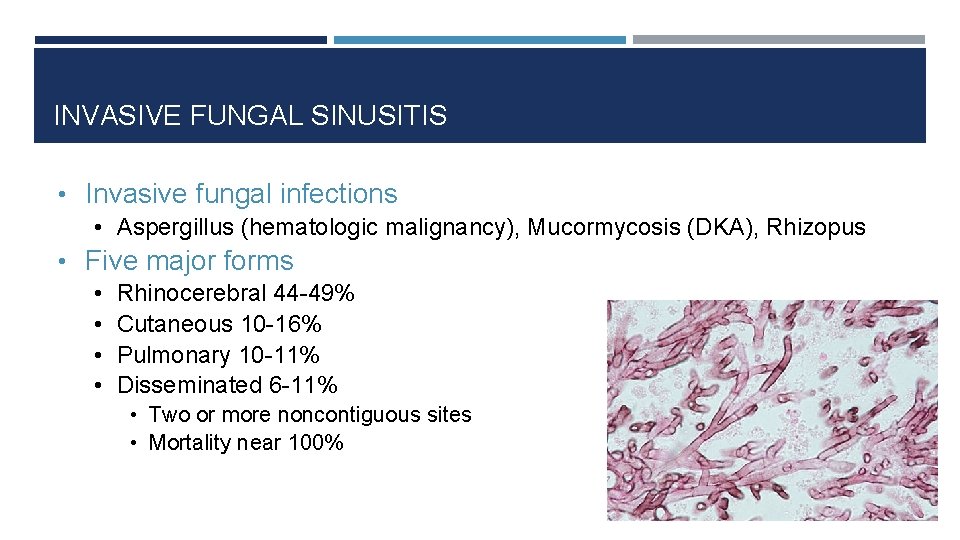
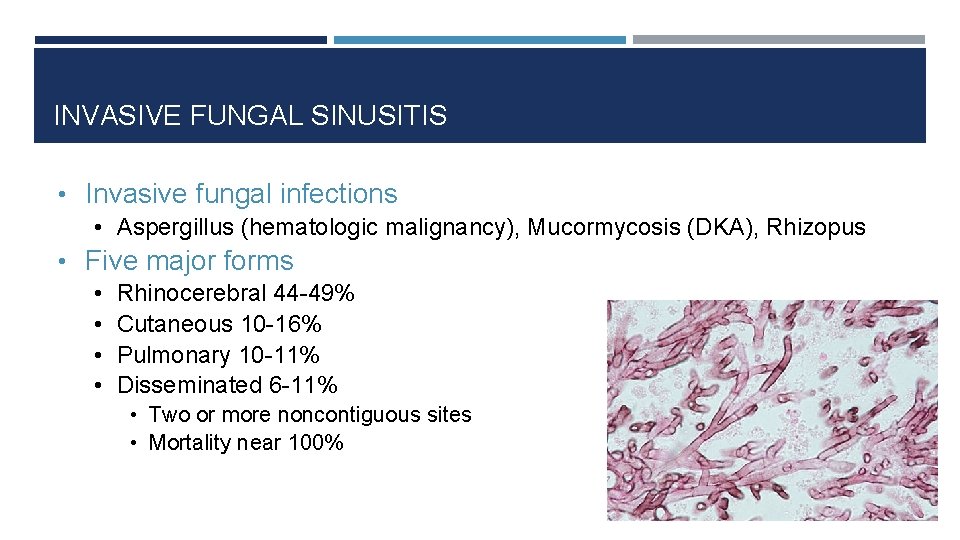
INVASIVE FUNGAL SINUSITIS • Invasive fungal infections • Aspergillus (hematologic malignancy), Mucormycosis (DKA), Rhizopus • Five major forms • • Rhinocerebral 44 -49% Cutaneous 10 -16% Pulmonary 10 -11% Disseminated 6 -11% • Two or more noncontiguous sites • Mortality near 100%
RISK FACTORS • • • Diabetes with metabolic acidosis High-dose systemic corticosteroids Patients w/ hematologic malignancy/transplantation Solid-organ transplantation Neutropenia AIDS
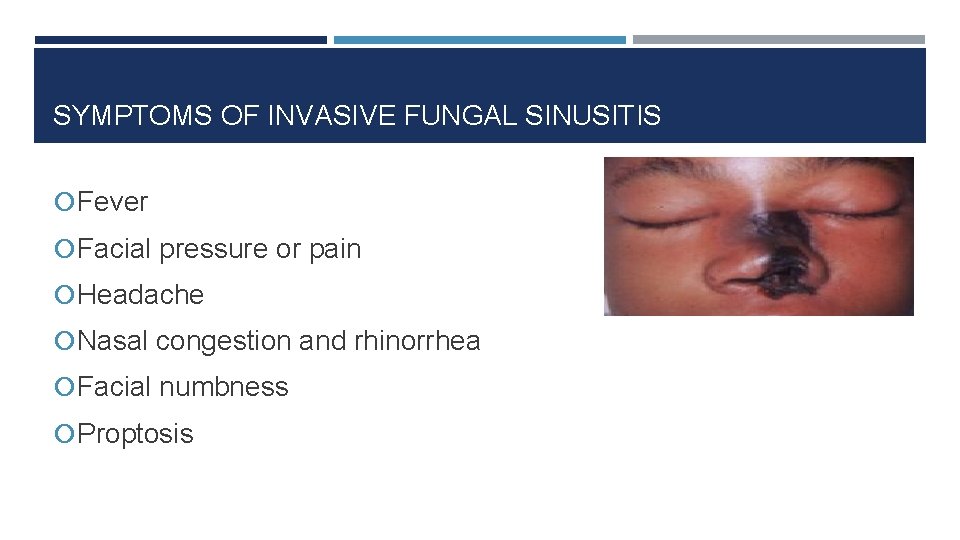
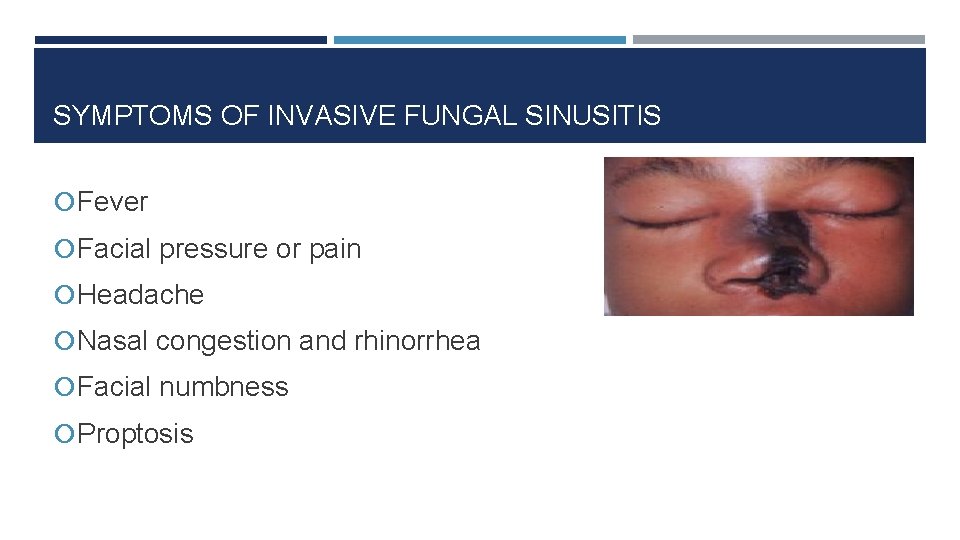
SYMPTOMS OF INVASIVE FUNGAL SINUSITIS Fever Facial pressure or pain Headache Nasal congestion and rhinorrhea Facial numbness Proptosis
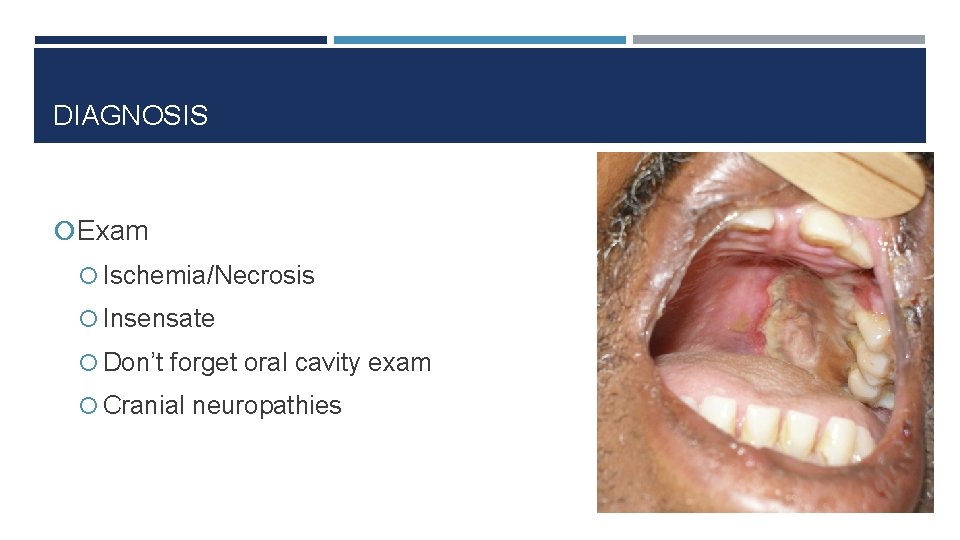
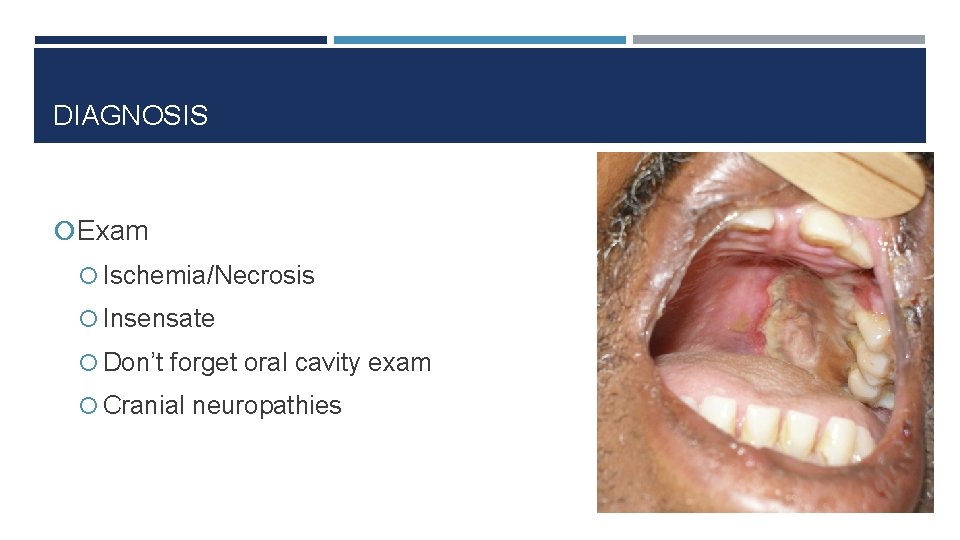
DIAGNOSIS Exam Ischemia/Necrosis Insensate Don’t forget oral cavity exam Cranial neuropathies
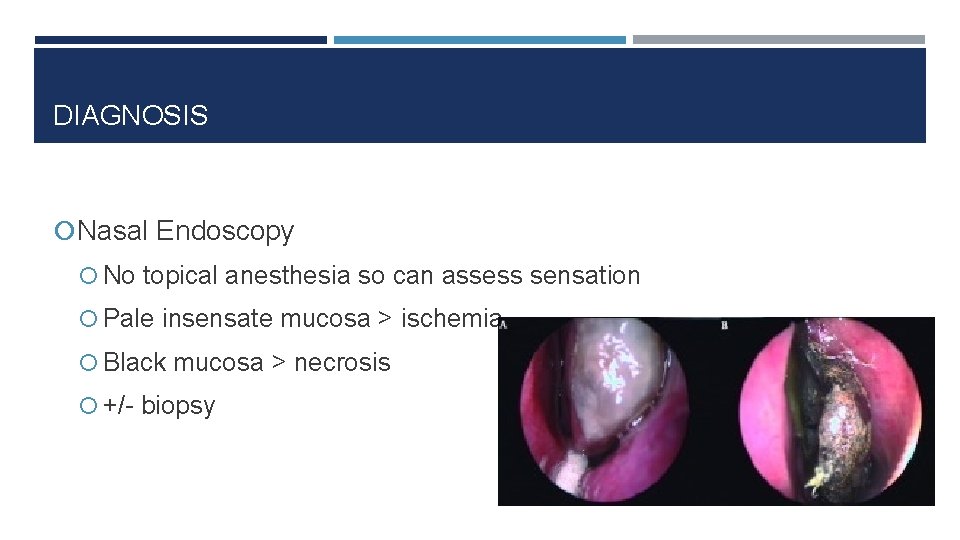
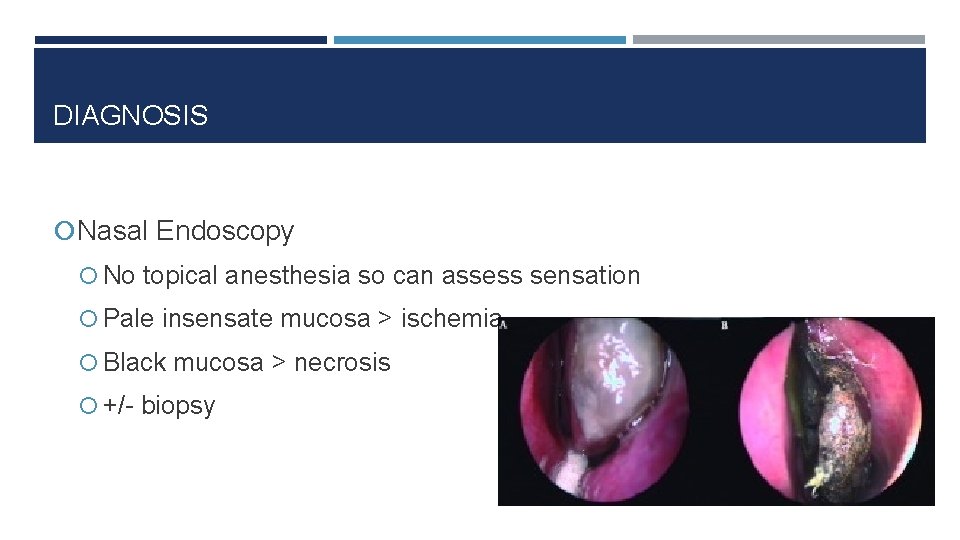
DIAGNOSIS Nasal Endoscopy No topical anesthesia so can assess sensation Pale insensate mucosa > ischemia Black mucosa > necrosis +/- biopsy
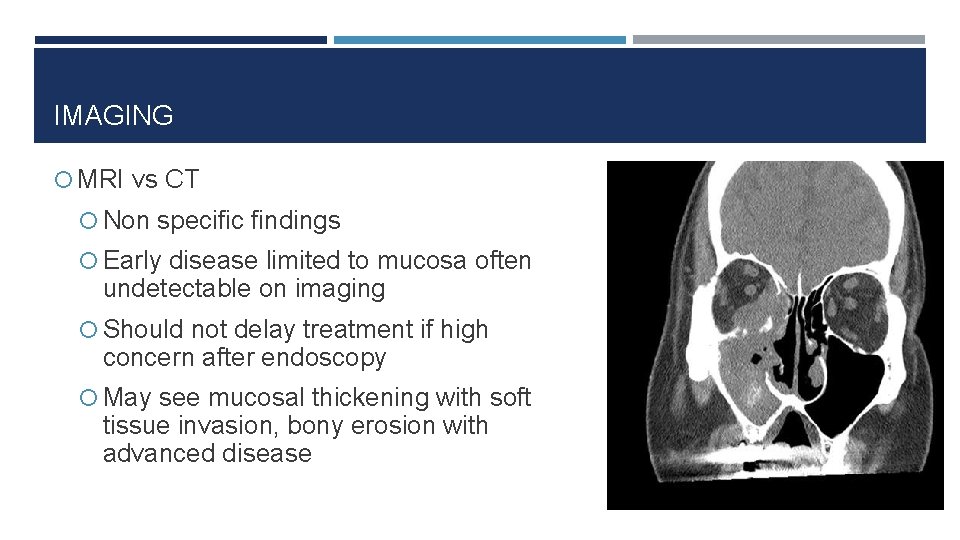
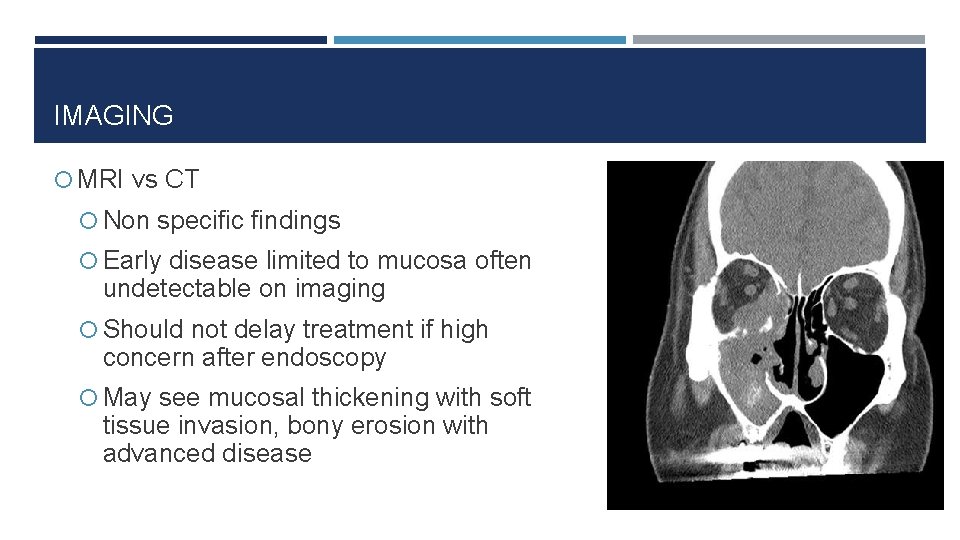
IMAGING MRI vs CT Non specific findings Early disease limited to mucosa often undetectable on imaging Should not delay treatment if high concern after endoscopy May see mucosal thickening with soft tissue invasion, bony erosion with advanced disease
TREATMENT Reversal of underlying condition when possible Tight glycemic control Normalize acidosis Hold steroids and immunosuppressants when able Urgent/emergent debridement Systemic antifungals

MASTOID EFFUSIONS VS MASTOIDITIS
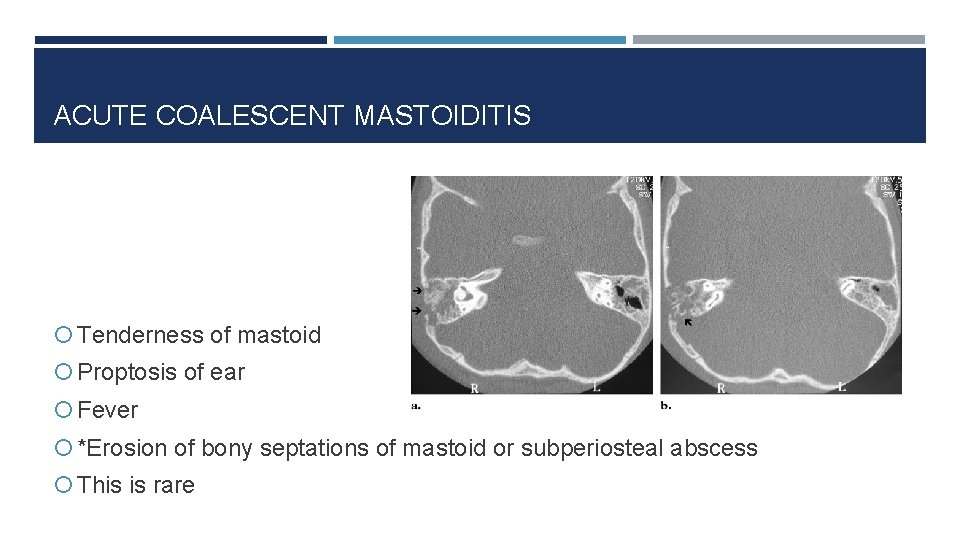
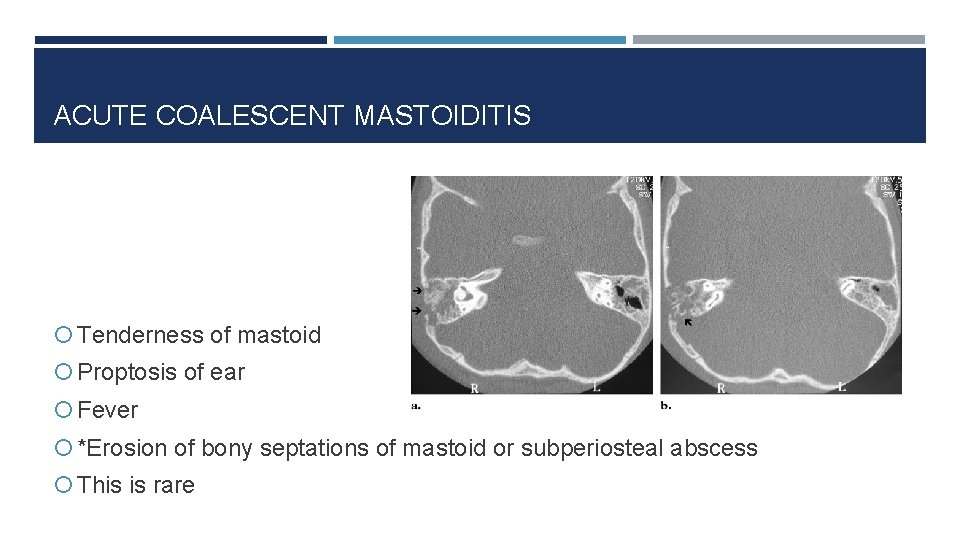
ACUTE COALESCENT MASTOIDITIS Tenderness of mastoid Proptosis of ear Fever *Erosion of bony septations of mastoid or subperiosteal abscess This is rare
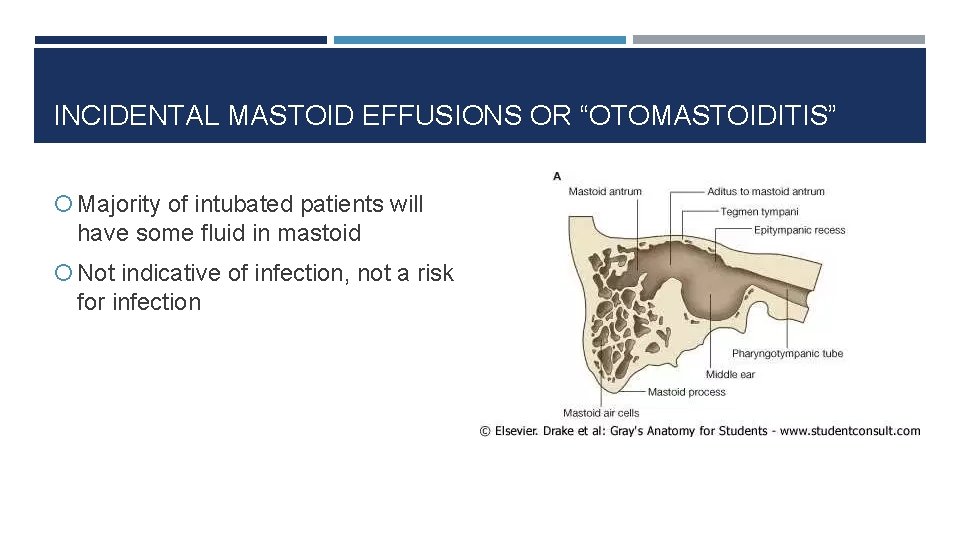
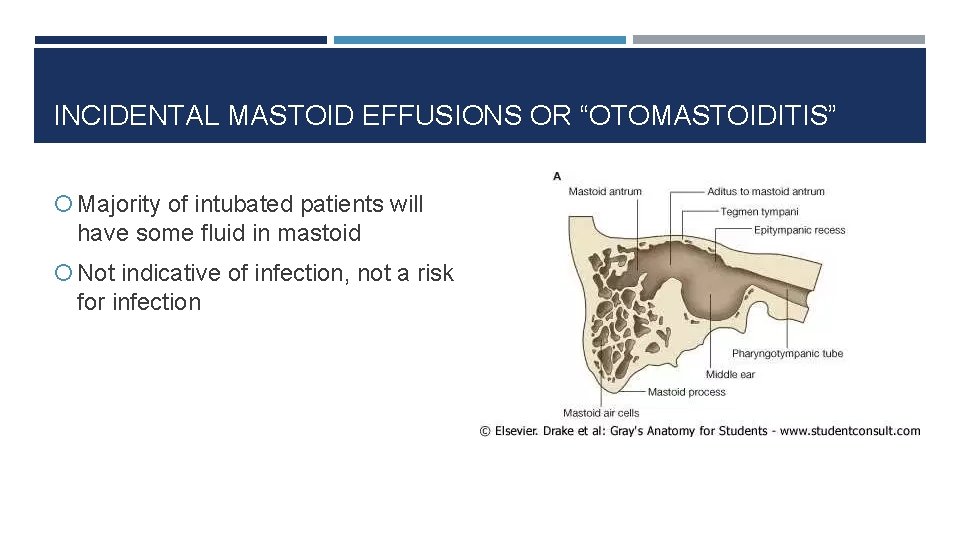
INCIDENTAL MASTOID EFFUSIONS OR “OTOMASTOIDITIS” Majority of intubated patients will have some fluid in mastoid Not indicative of infection, not a risk for infection
CALLING ENT CONSULTS Be patient with us and our OR nurses! We don’t have a true ”consult” resident. We will see emergencies when needed but please help us triage what can wait until later.
QUESTIONS?
 St louis family medicine residency
St louis family medicine residency Like a rushing wind jesus breathe within
Like a rushing wind jesus breathe within If you want to know me by noemia de sousa
If you want to know me by noemia de sousa 15 things every veteran wants you to know
15 things every veteran wants you to know Inquiry minds want to know
Inquiry minds want to know Curious minds want to know
Curious minds want to know Curious minds want to know
Curious minds want to know I want to know something about
I want to know something about Elements of spoken word poetry
Elements of spoken word poetry Know history know self
Know history know self Dilan gorur
Dilan gorur I know who goes before me i know who stands behind
I know who goes before me i know who stands behind So you think you know minecraft
So you think you know minecraft Happpy nod
Happpy nod Personification in the raven
Personification in the raven If you're blue and you don't know where to go
If you're blue and you don't know where to go Do asexual people have sex
Do asexual people have sex Do you know who you are
Do you know who you are I will follow you wherever you blank
I will follow you wherever you blank 2021 graduation songs
2021 graduation songs Michael levitt uw
Michael levitt uw Umass neurology residency
Umass neurology residency Vanderbilt neurology residency
Vanderbilt neurology residency Https://ncc-efm.org/game/efmgame.cfm
Https://ncc-efm.org/game/efmgame.cfm Uihc internal medicine residency
Uihc internal medicine residency Tufts anesthesiology residency
Tufts anesthesiology residency Dr finney unmc
Dr finney unmc Paro call stipend
Paro call stipend Post campaign analysis presentation
Post campaign analysis presentation Unm internal medicine
Unm internal medicine Uthscsa internal medicine residents
Uthscsa internal medicine residents Karl suure pealinn
Karl suure pealinn Tourism involving non-residents of the given area.
Tourism involving non-residents of the given area. Nutrition and hydration chapter 15
Nutrition and hydration chapter 15 Chapter 13 personal care skills
Chapter 13 personal care skills Famous yonkers residents
Famous yonkers residents Uf neurology residents
Uf neurology residents Five things we need to know about technological change
Five things we need to know about technological change Common things everyone should know
Common things everyone should know Get to.know you questions
Get to.know you questions Eoc biology test
Eoc biology test Whats an energy pyramid
Whats an energy pyramid What are the seven life processes
What are the seven life processes Will mandy have lunch with sue
Will mandy have lunch with sue Lirik lagu more more more we praise you
Lirik lagu more more more we praise you More more more i want more more more more we praise you
More more more i want more more more more we praise you Why do you want to work for us
Why do you want to work for us Unit 5 what do you want to do
Unit 5 what do you want to do Go con ing
Go con ing So you want to be a social worker
So you want to be a social worker It's everywhere you want to be slogan
It's everywhere you want to be slogan Plain folks persuasive technique examples
Plain folks persuasive technique examples Motivated last thing you want do
Motivated last thing you want do If u want to go fast go alone
If u want to go fast go alone Do you want to build a snowman english
Do you want to build a snowman english Omar hamdan lives in tabuk.
Omar hamdan lives in tabuk. Chris burden shoot
Chris burden shoot Do you want me to be honest
Do you want me to be honest Suppose you want to combine two types of fruit drink
Suppose you want to combine two types of fruit drink