The Menopausal Woman Professor Hassan Nasrat FRCS FRCOG



- Slides: 43
The Menopausal Woman Professor Hassan Nasrat FRCS, FRCOG Professor of Obstetrics and Gynecology Faculty of Medicine King Abdulaziz University
Definition and Terminology Pathphysiology Do we have a real problem? Symptoms and Signs (Consequences of E deprivation) Long Term Risk of E deprivation Management HRT and The Controversy
The Menopause and The Perimenopause The Menopause: Permanent cessation of menstruation resulting from the loss of ovarian follicles (WHO). Is a retrospective diagnosis. Perimenopause: Is the period of time women, usually in their forties, menstruating, experience symptoms deficiency due to declining ovarian years) when normal and usually of oestrogen function (1 -9 This group has been termed the “Sandwich generation” caring for their immediate families, aging parents as well as having career commitment.
The Perimenopause Ø Gametogenic failure followed by. Ø Ovarian hormonal failure Cessation of Estrogen. The Biochemical markers are unreliable in diagnosis of the perimenopause because of irregularity hormonal levels.
Ovarian gametogenic Failure: • Failure in quantity: Accelerated Loss of Follicles Decreased Fertility Rate • Failure in quality: – Embryonic chromosomal anomalies e. g. Trisomies. – Increased spontaneous miscarriage
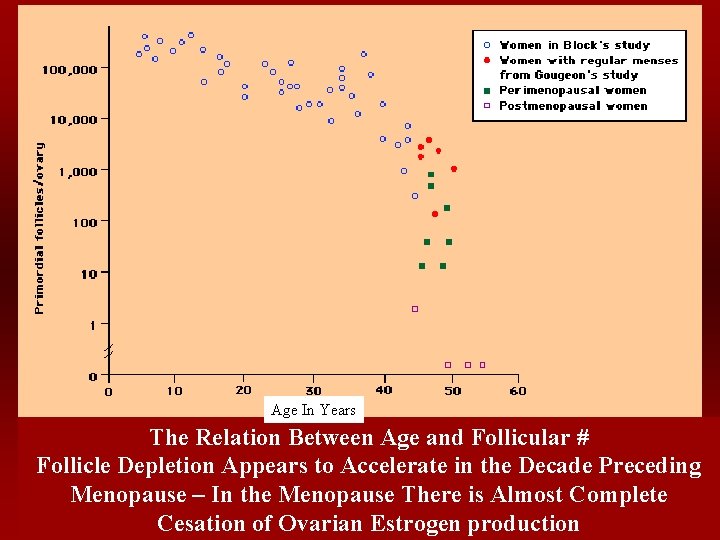
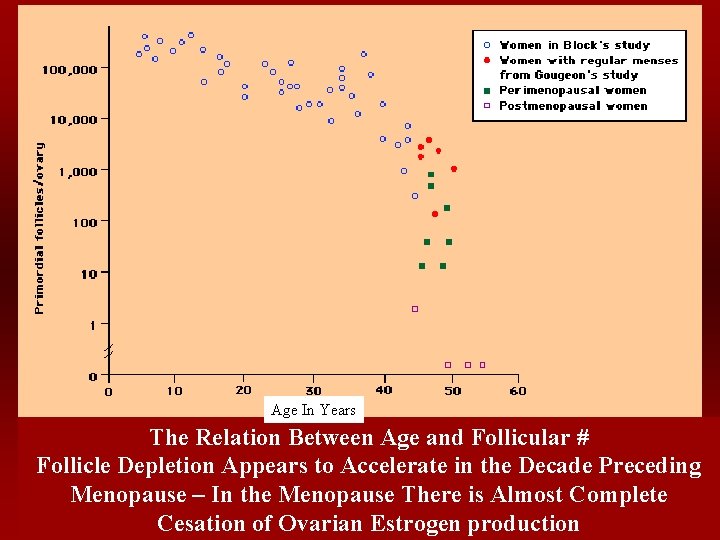
Age In Years The Relation Between Age and Follicular # Follicle Depletion Appears to Accelerate in the Decade Preceding Menopause – In the Menopause There is Almost Complete Cesation of Ovarian Estrogen production

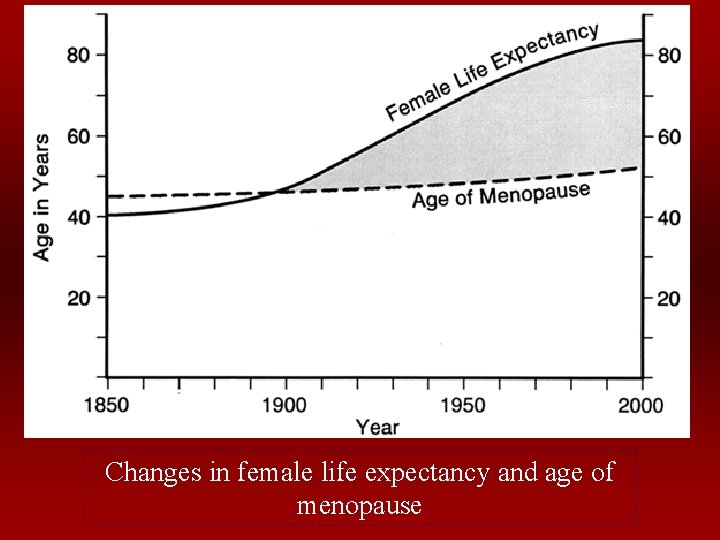
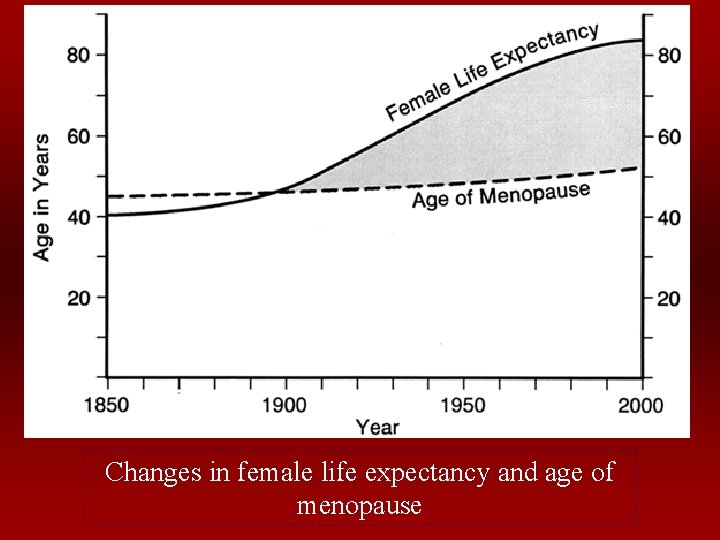
Changes in female life expectancy and age of menopause
Definition and Terminology Pathphysiology Do we have a real problem? Symptoms and Signs (Consequences of E deprivation) Long Term Risk of E deprivation Management HRT and The Controversy
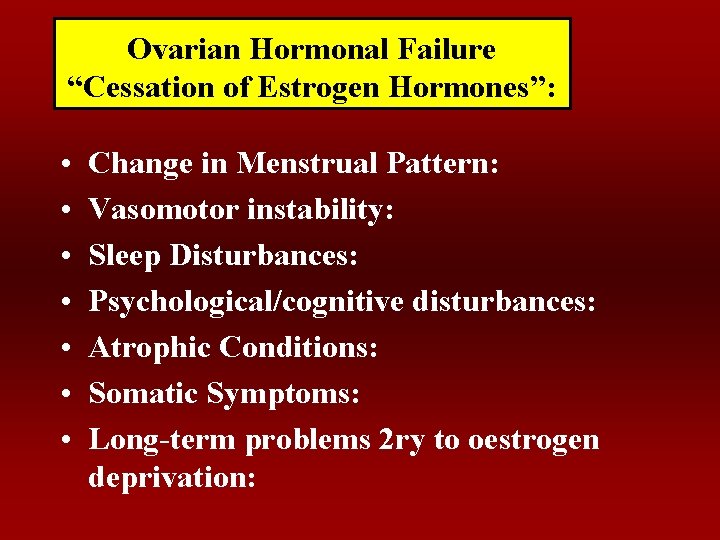
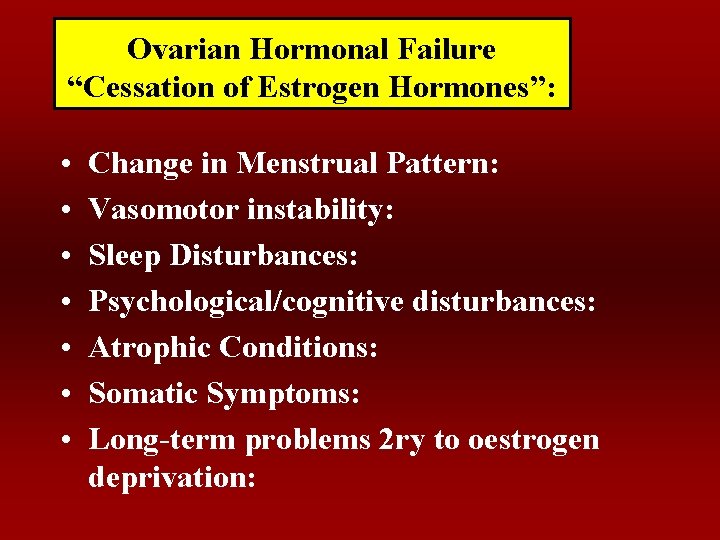
Ovarian Hormonal Failure “Cessation of Estrogen Hormones”: • • Change in Menstrual Pattern: Vasomotor instability: Sleep Disturbances: Psychological/cognitive disturbances: Atrophic Conditions: Somatic Symptoms: Long-term problems 2 ry to oestrogen deprivation:
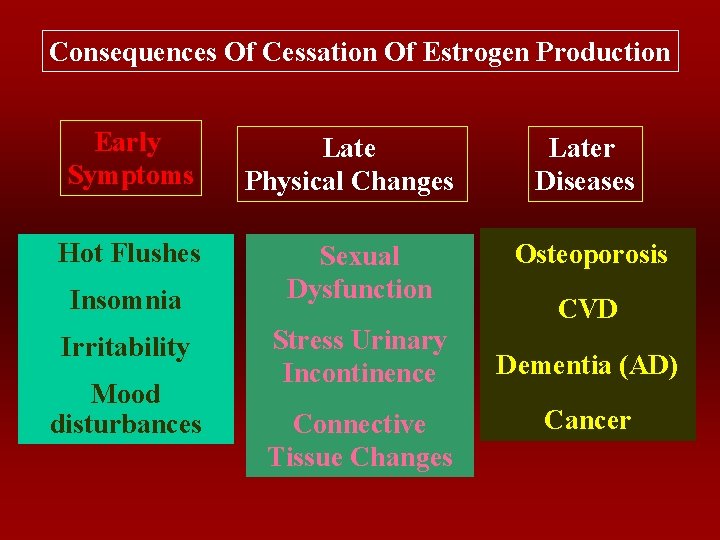
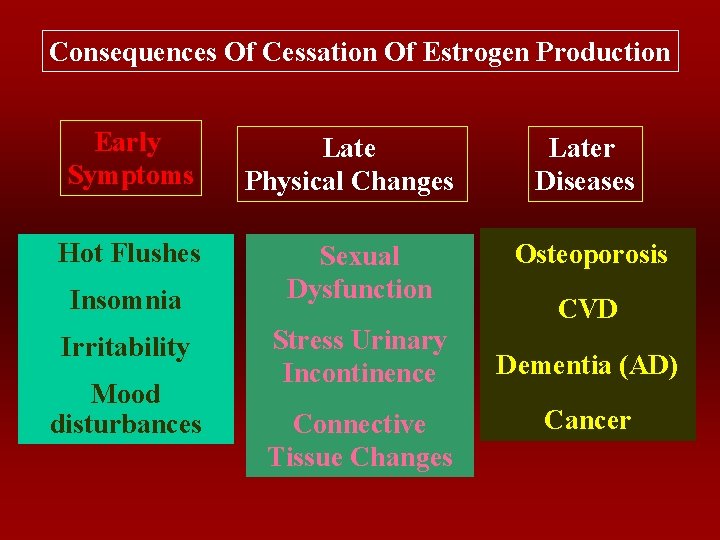
Consequences Of Cessation Of Estrogen Production Early Symptoms Hot Flushes Insomnia Irritability Mood disturbances Late Physical Changes Sexual Dysfunction Stress Urinary Incontinence Connective Tissue Changes Later Diseases Osteoporosis CVD Dementia (AD) Cancer
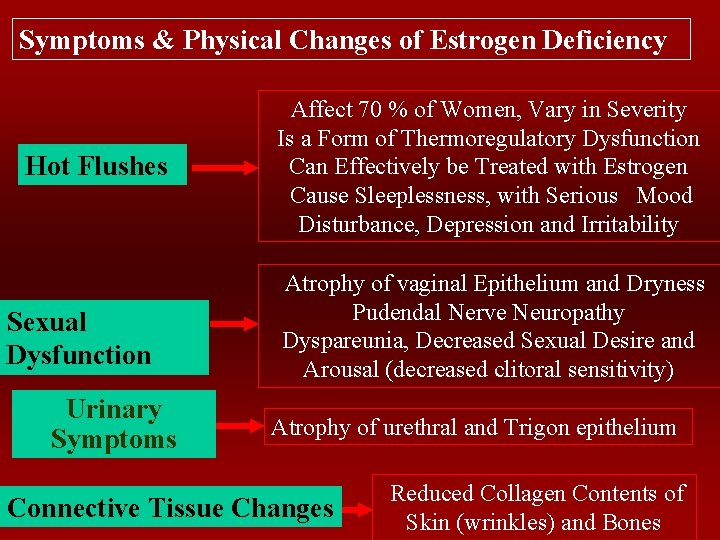
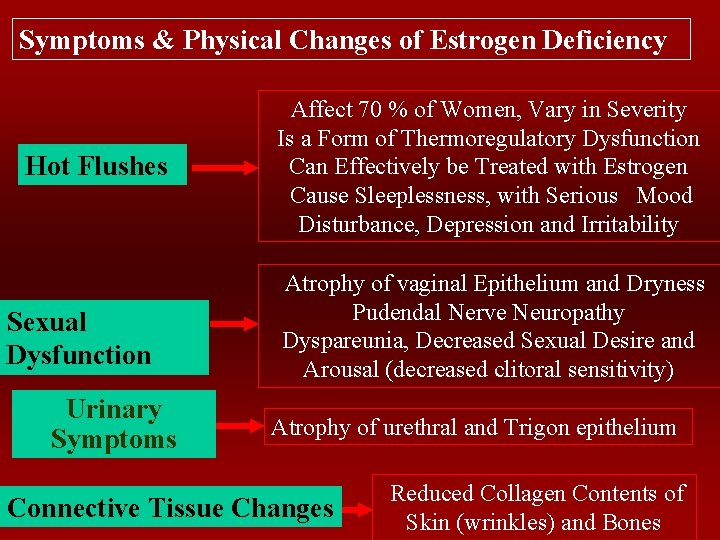
Symptoms & Physical Changes of Estrogen Deficiency Hot Flushes Sexual Dysfunction Urinary Symptoms Affect 70 % of Women, Vary in Severity Is a Form of Thermoregulatory Dysfunction Can Effectively be Treated with Estrogen Cause Sleeplessness, with Serious Mood Disturbance, Depression and Irritability Atrophy of vaginal Epithelium and Dryness Pudendal Nerve Neuropathy Dyspareunia, Decreased Sexual Desire and Arousal (decreased clitoral sensitivity) Atrophy of urethral and Trigon epithelium Connective Tissue Changes Reduced Collagen Contents of Skin (wrinkles) and Bones
Osteoporosis
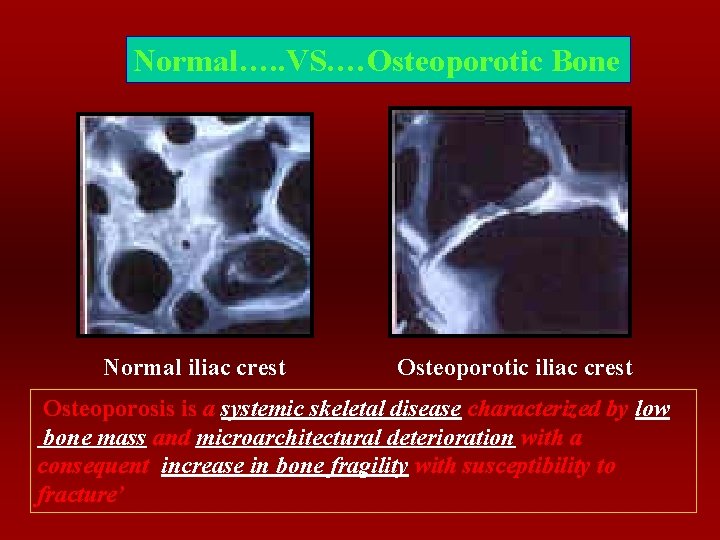
Osteoporosis ‘a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration with a consequent increase in bone fragility with susceptibility to fracture’
Estrogen and The Skeletal System: With Acute Estrogen Deficiency After The Menopause, There Is Accelerated Bone Loss Which Mounts To About 1 -1. 5% Loss Of Total Bone Mass/Year. For The First 20 Years After Cessation Of Menses, Menopause Related Bone Loss Results In 50% Reduction In Trabecular Bone And 30 % Reduction In Cortical Bone.
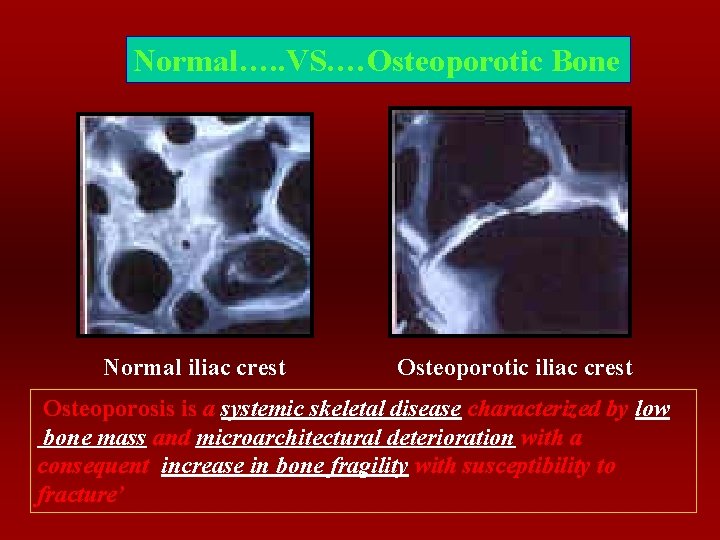
Normal…. . VS. …Osteoporotic Bone Normal iliac crest Osteoporotic iliac crest Osteoporosis is a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration with a consequent increase in bone fragility with susceptibility to fracture’
Oestrogen and The Skeletal System: The Precise mechanism of action of Oestrogen on the skeletal system is unknown. It seems to acts at different sites: - Increase efficiency of calcium absorption (enhance availability of Vit. D, 1, 25 dihydroxy vit. D) - Direct action on Osteoblasts - Through stimulation of estrogen dependant growth factors. - Promote the synthesis of Calcitonin.
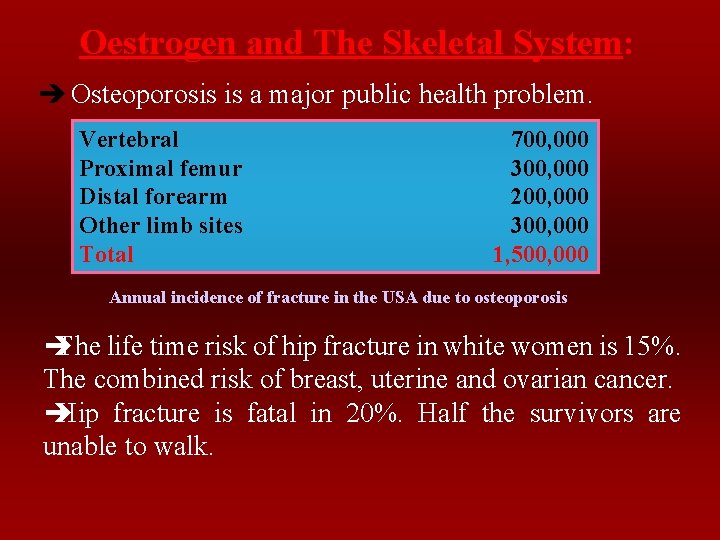
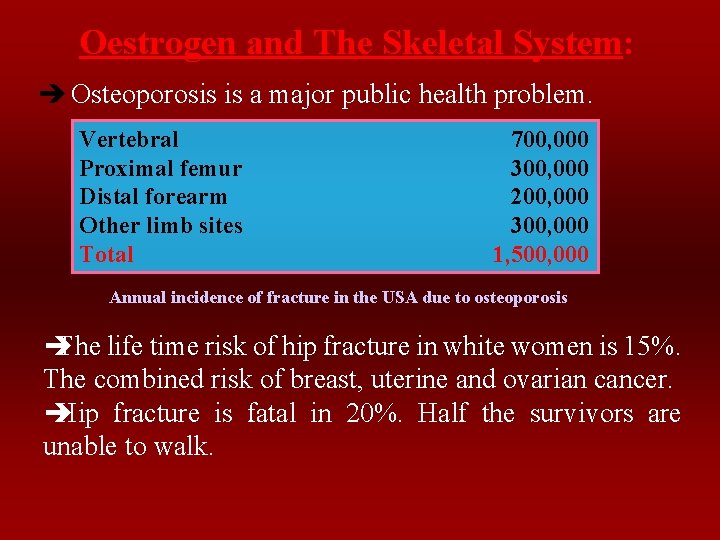
Oestrogen and The Skeletal System: è Osteoporosis is a major public health problem. Vertebral Proximal femur Distal forearm Other limb sites Total 700, 000 300, 000 200, 000 300, 000 1, 500, 000 Annual incidence of fracture in the USA due to osteoporosis è The life time risk of hip fracture in white women is 15%. The combined risk of breast, uterine and ovarian cancer. è Hip fracture is fatal in 20%. Half the survivors are unable to walk.
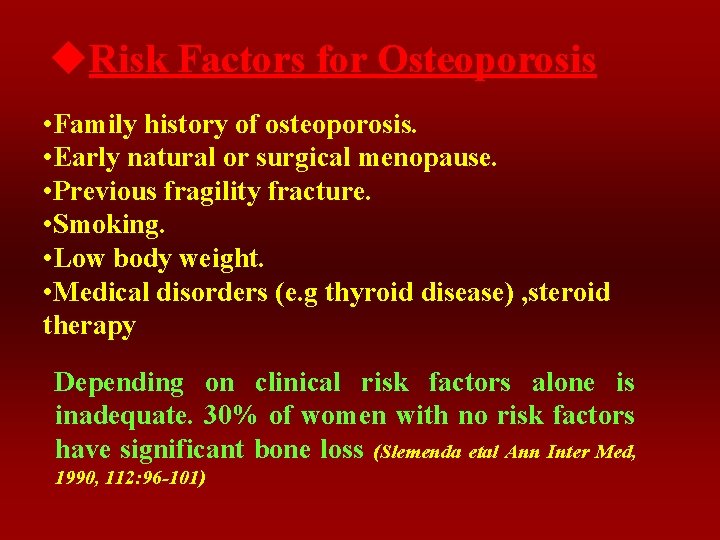
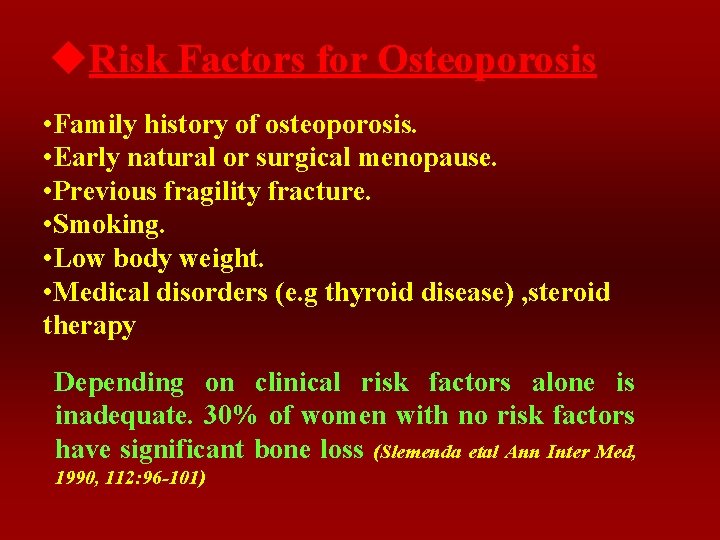
u. Risk Factors for Osteoporosis • Family history of osteoporosis. • Early natural or surgical menopause. • Previous fragility fracture. • Smoking. • Low body weight. • Medical disorders (e. g thyroid disease) , steroid therapy Depending on clinical risk factors alone is inadequate. 30% of women with no risk factors have significant bone loss (Slemenda etal Ann Inter Med, 1990, 112: 96 -101)
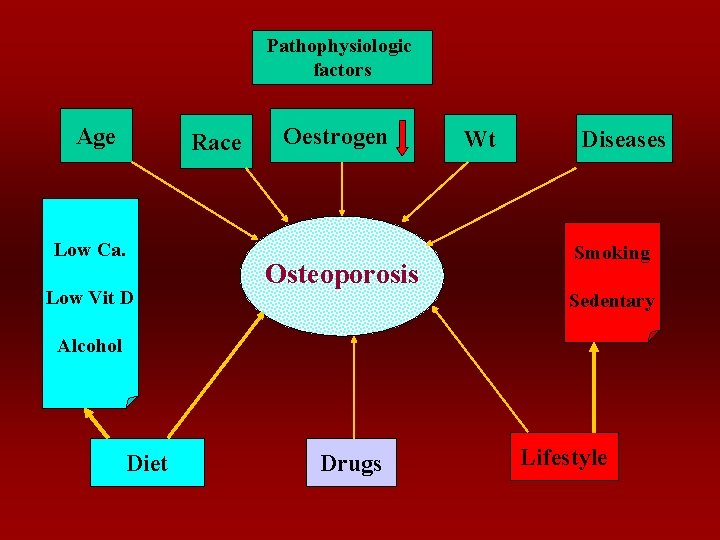
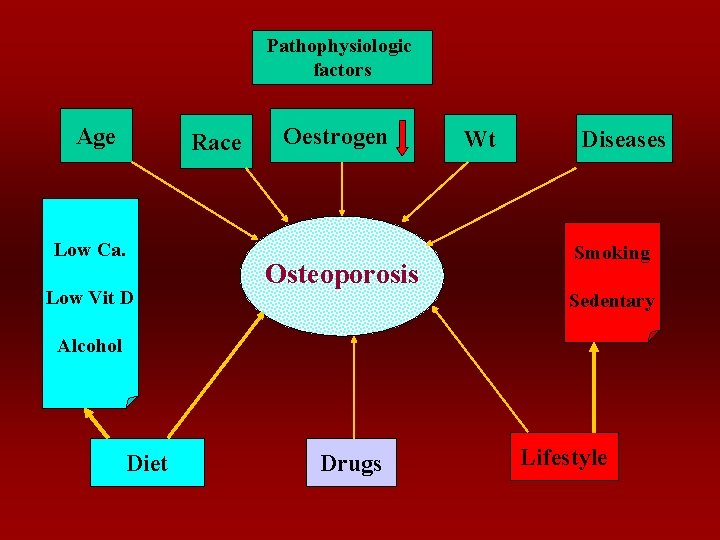
Pathophysiologic factors Age Race Low Ca. Low Vit D Oestrogen Osteoporosis Wt Diseases Smoking Sedentary Alcohol Diet Drugs Lifestyle
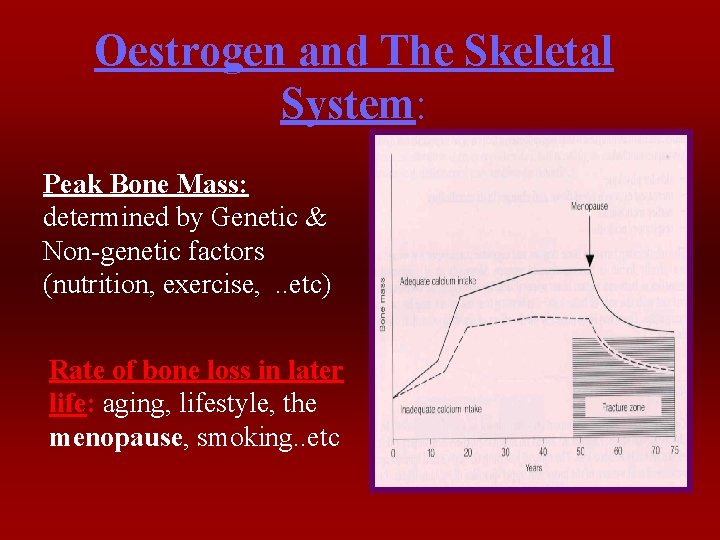
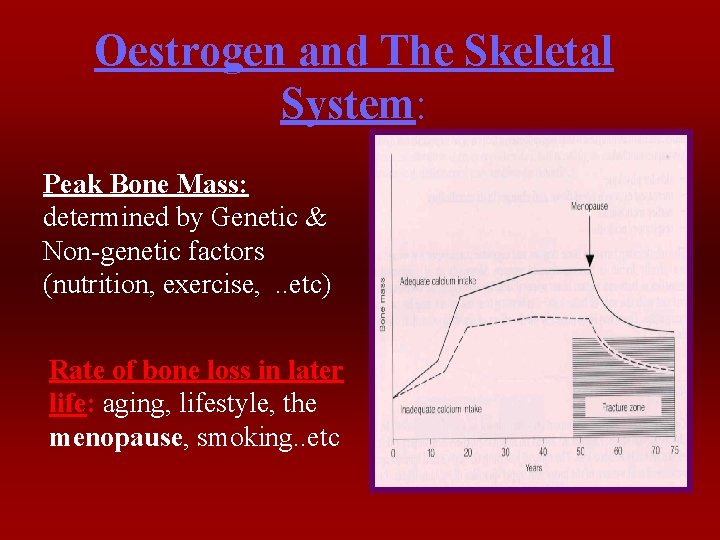
Oestrogen and The Skeletal System: Peak Bone Mass: determined by Genetic & Non-genetic factors (nutrition, exercise, . . etc) Rate of bone loss in later life: aging, lifestyle, the menopause, smoking. . etc
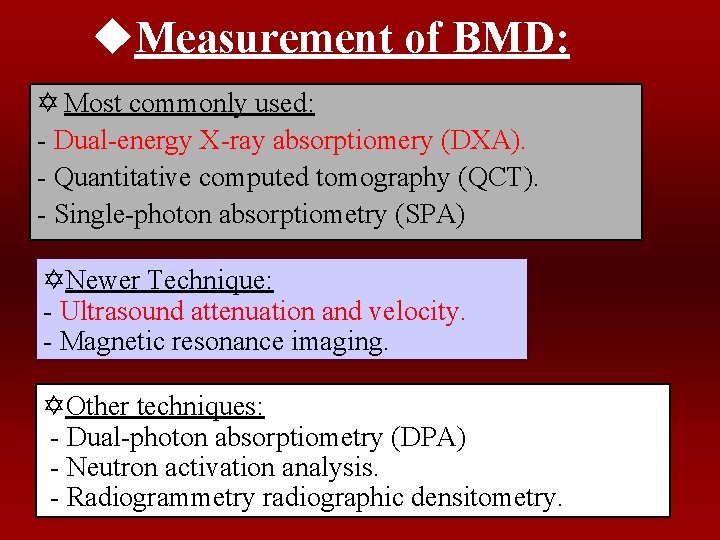
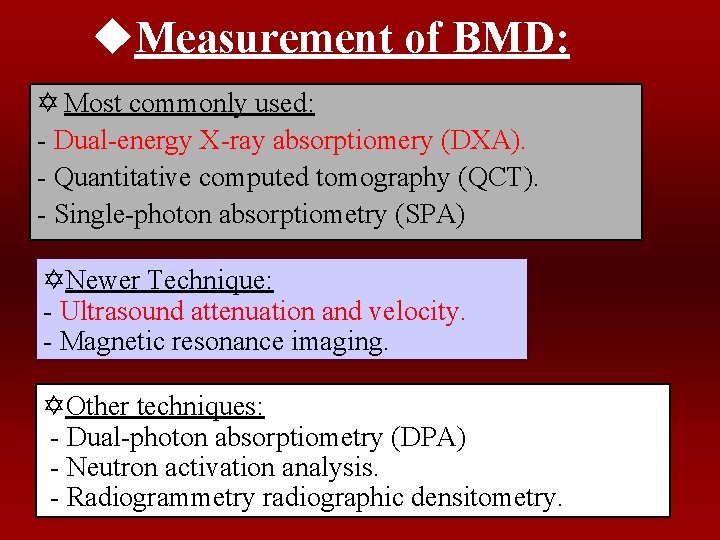
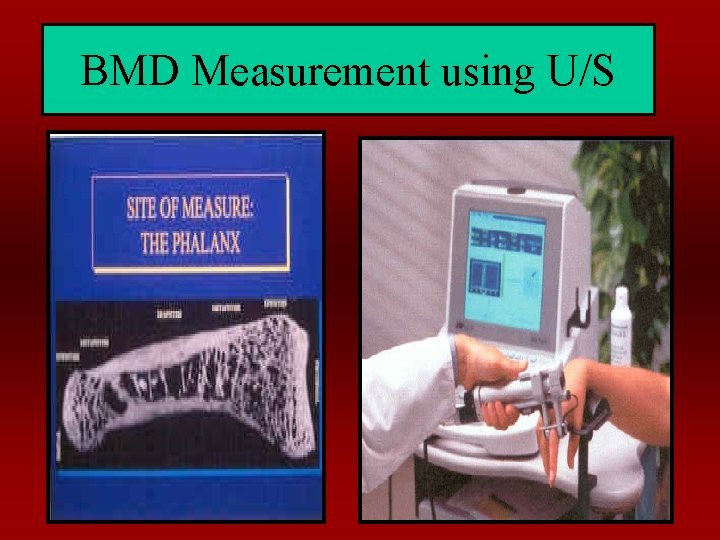
u. Measurement of BMD: Y Most commonly used: - Dual-energy X-ray absorptiomery (DXA). - Quantitative computed tomography (QCT). - Single-photon absorptiometry (SPA) YNewer Technique: - Ultrasound attenuation and velocity. - Magnetic resonance imaging. YOther techniques: - Dual-photon absorptiometry (DPA) - Neutron activation analysis. - Radiogrammetry radiographic densitometry.
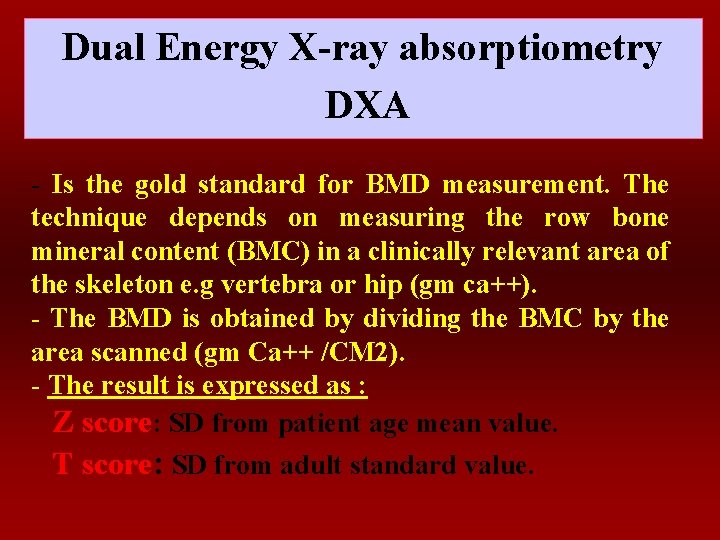
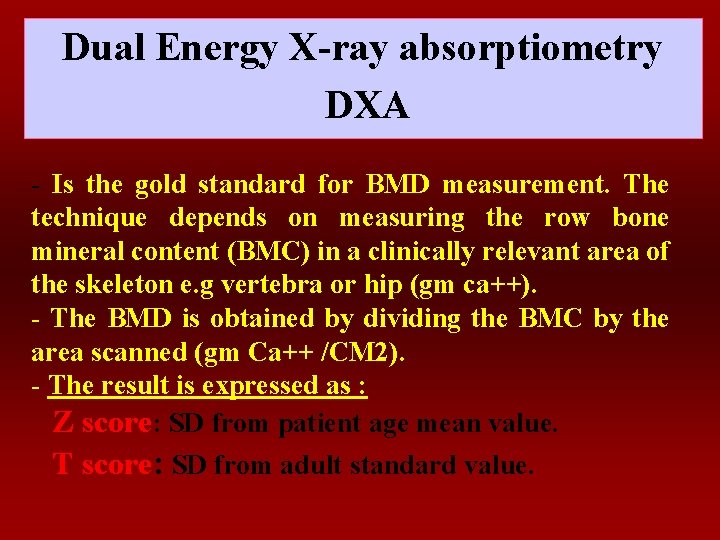
Dual Energy X-ray absorptiometry DXA - Is the gold standard for BMD measurement. The technique depends on measuring the row bone mineral content (BMC) in a clinically relevant area of the skeleton e. g vertebra or hip (gm ca++). - The BMD is obtained by dividing the BMC by the area scanned (gm Ca++ /CM 2). - The result is expressed as : Z score: SD from patient age mean value. T score: SD from adult standard value.
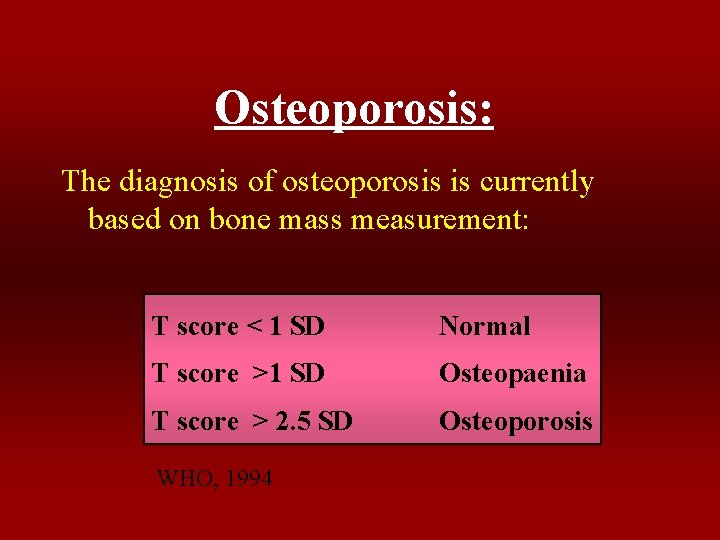
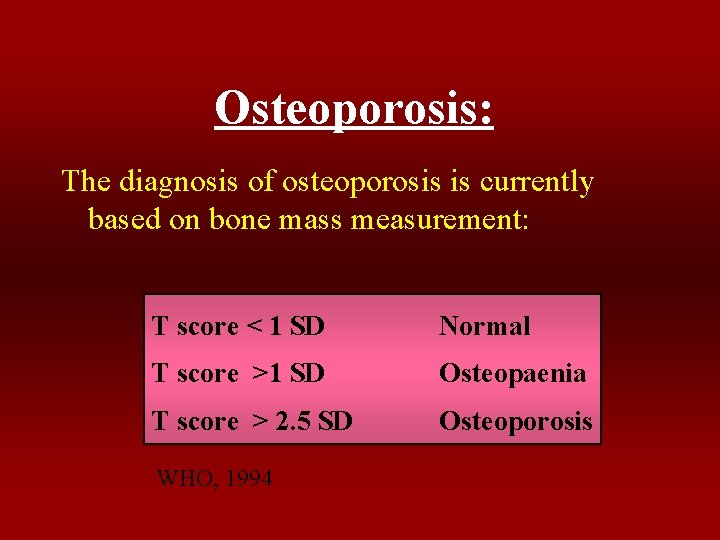
Osteoporosis: The diagnosis of osteoporosis is currently based on bone mass measurement: T score < 1 SD Normal T score >1 SD Osteopaenia T score > 2. 5 SD Osteoporosis WHO, 1994
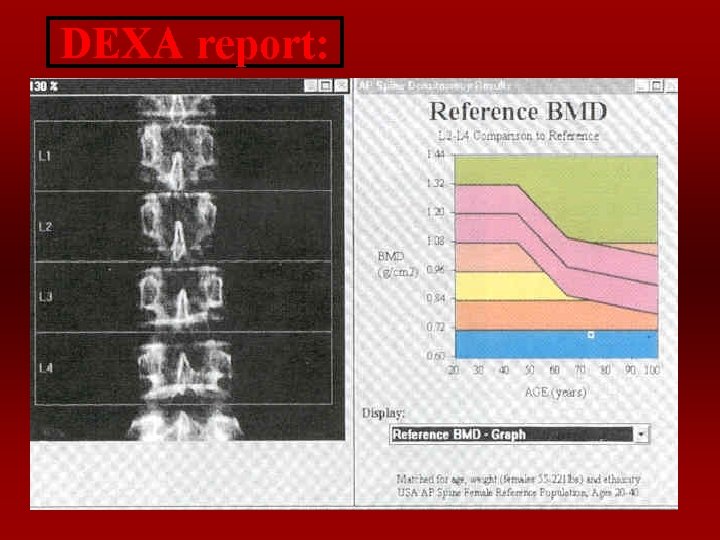
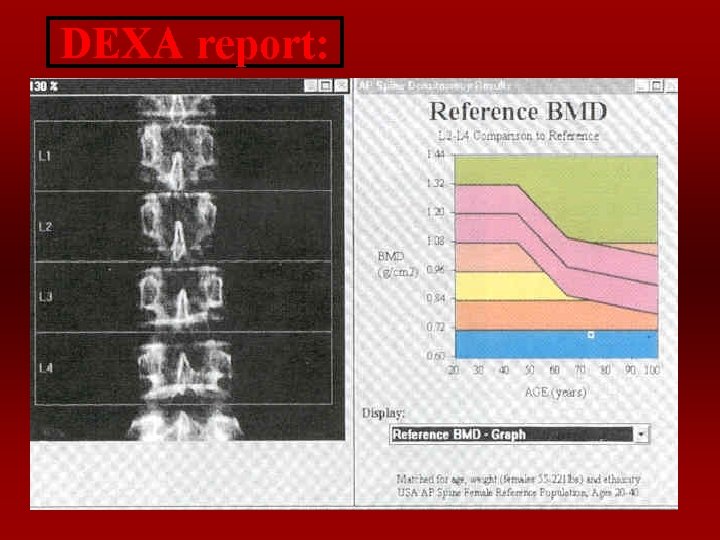
DEXA report:
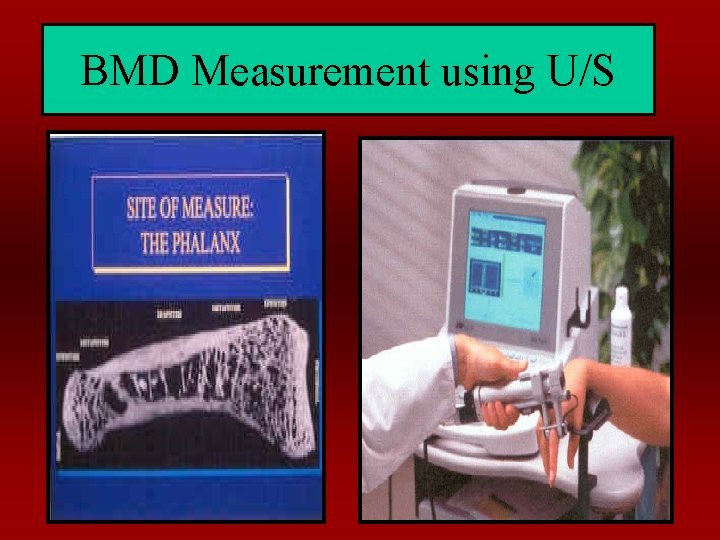
BMD Measurement using U/S
Oestrogen and the CVS
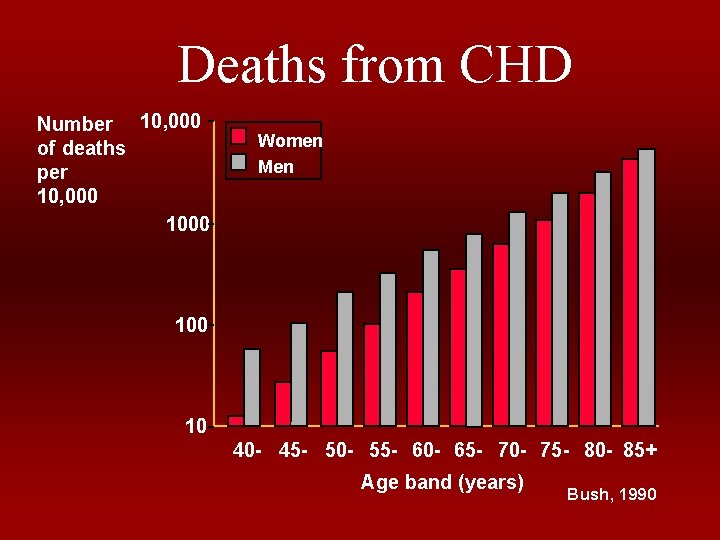
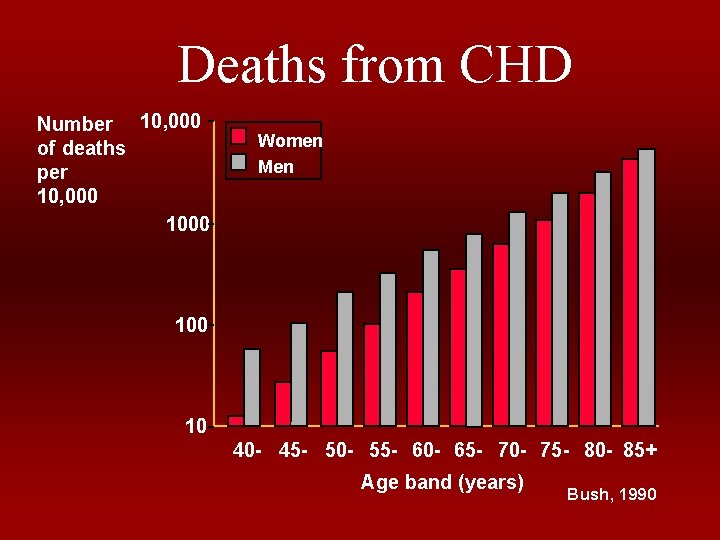
Deaths from CHD Number 10, 000 of deaths per 10, 000 1000 Women Men 100 10 40 - 45 - 50 - 55 - 60 - 65 - 70 - 75 - 80 - 85+ Age band (years) Bush, 1990
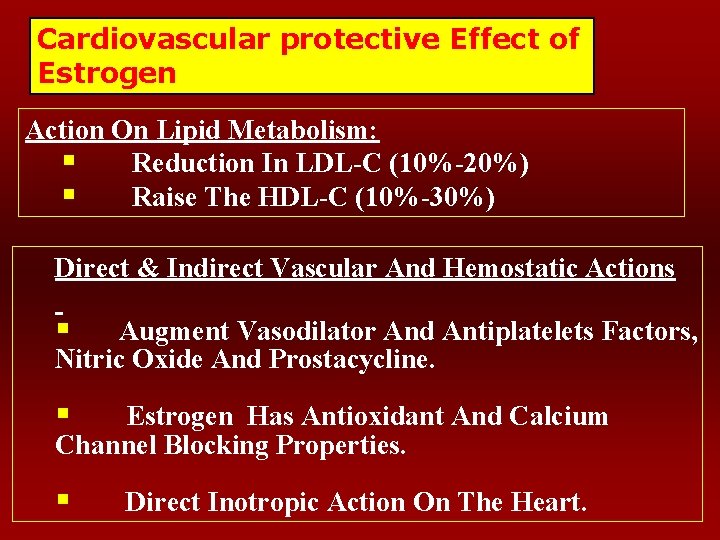
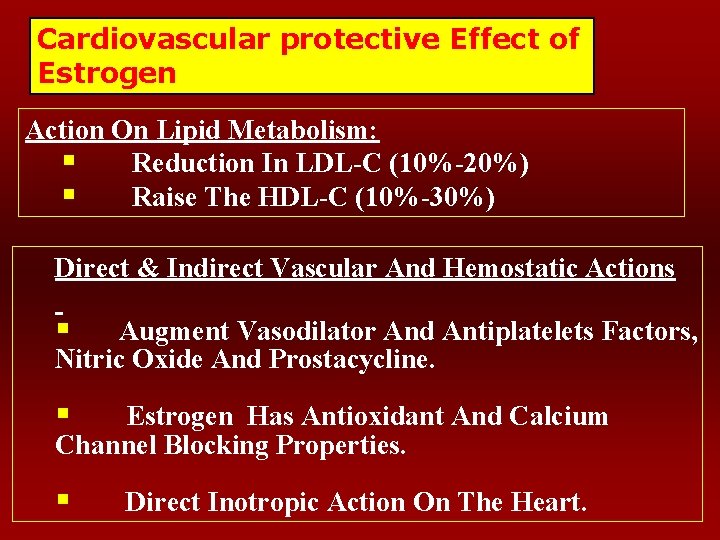
Cardiovascular protective Effect of Estrogen Action On Lipid Metabolism: § Reduction In LDL-C (10%-20%) § Raise The HDL-C (10%-30%) Direct & Indirect Vascular And Hemostatic Actions § Augment Vasodilator And Antiplatelets Factors, Nitric Oxide And Prostacycline. § Estrogen Has Antioxidant And Calcium Channel Blocking Properties. § Direct Inotropic Action On The Heart.
Management of the Menopause
• History: – symptoms of Estrogen deficiency – History of relevant medical or surgical conditions (e. g. diabetes, CVD, Thrombosis, Cancer…etc. ) in patient and family. – History of Relevant medications: e. g. steroid. – Family history of Cancer (breast or ovarian) • Examination And Investigations: – General: – Local: including Pap Smear – BMD – Mammography
• Counseling and Advice: – Life Style (Diet, exercise…etc. ) • Medications: – HRT – Calcium – Vit. D – SERM – Other specific agents for osteoporosis
Management of Early Consequences of Estrogen Deficiency: Hot Flashes, Vaginal Dryness, Urinary Symptoms, And Emotional Liability… etc Estrogen Treatment Is The Available Menopausal Symptoms Most For Effective Relief Of
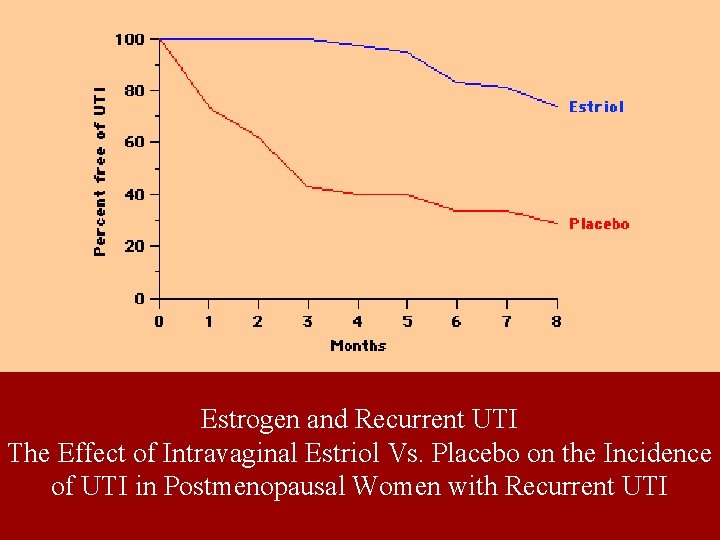
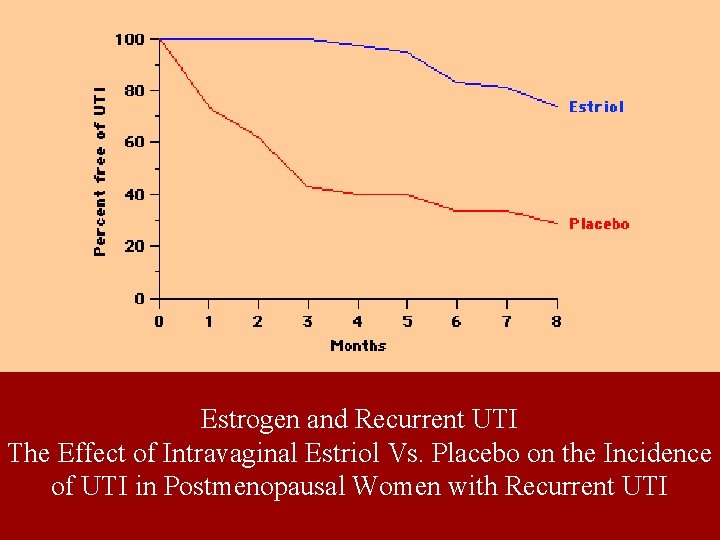
Estrogen and Recurrent UTI The Effect of Intravaginal Estriol Vs. Placebo on the Incidence of UTI in Postmenopausal Women with Recurrent UTI
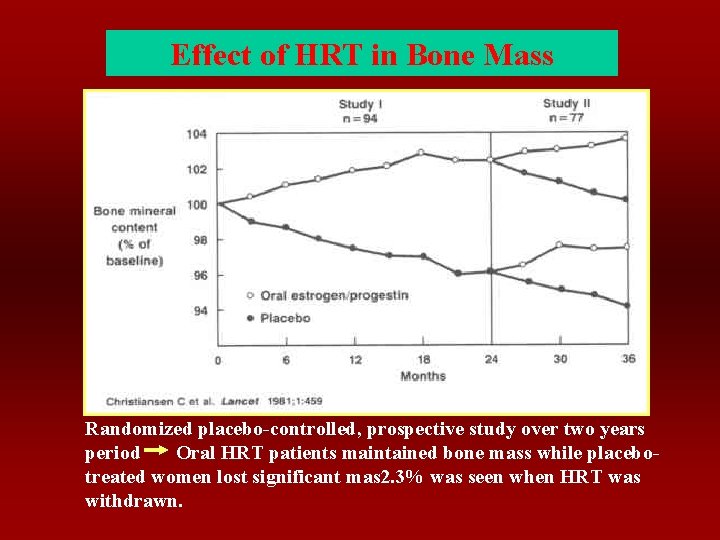
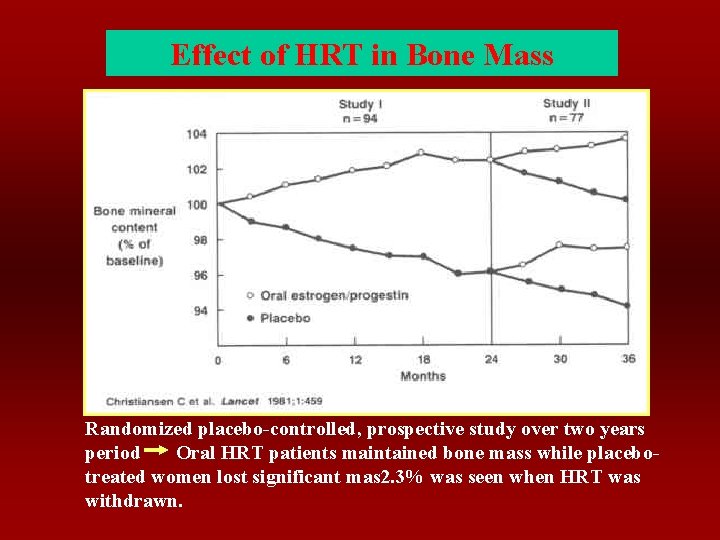
Effect of HRT in Bone Mass Randomized placebo-controlled, prospective study over two years period Oral HRT patients maintained bone mass while placebotreated women lost significant mas 2. 3% was seen when HRT was withdrawn.

Estrogen Replacement Therapy “ERT” • Type of Estrogen: • Route of Administration: • Combined Preparation “HRT” • Duration of treatment: • Risks of HRT

Estrogen Replacement Therapy ’ERT’ Oral Oestrogen Transdermal Oestrogen Gel Containing oestrogen Estrogen Implants Vaginal Oestrogen
Combined Preparation “HRT” - In Women With Intact Uteri Progesterone Preparation Should be Added. - It Has Virtually Eliminated The Risk Of Endometrial Cancer. .
Risks Associated with HRT: General and Metabolic Risks: Venous thrombosis gallbladder diseases liver diseases. Endometrial Neoplasia: Breast Cancer:
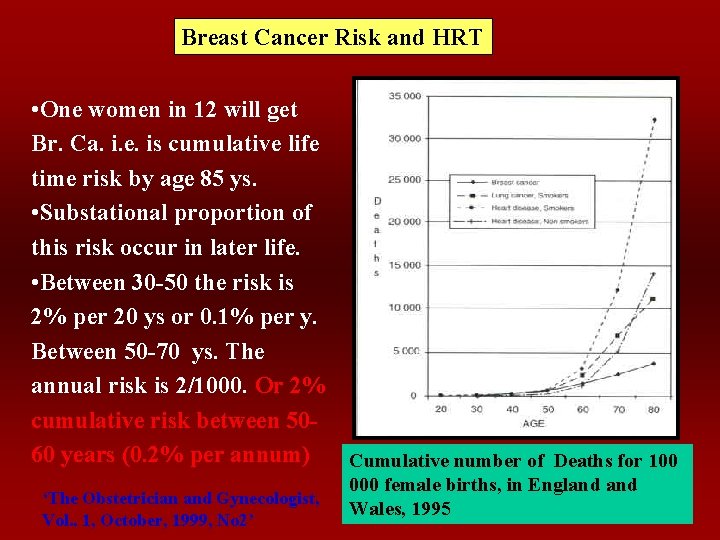
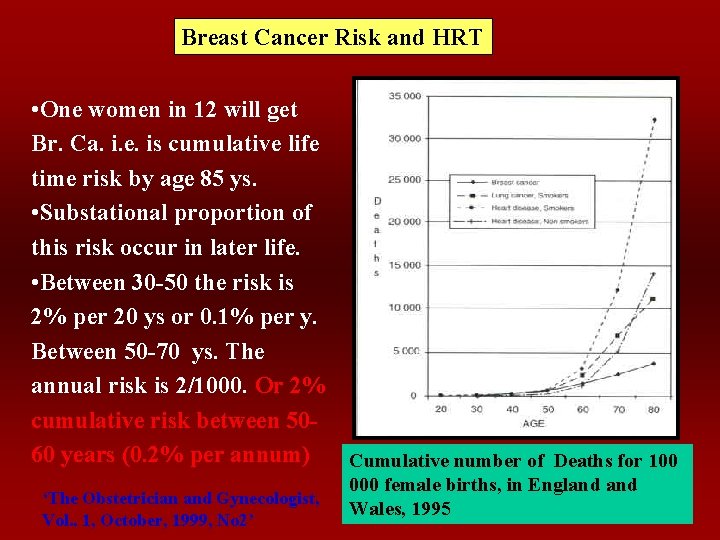
Breast Cancer Risk and HRT • One women in 12 will get Br. Ca. i. e. is cumulative life time risk by age 85 ys. • Substational proportion of this risk occur in later life. • Between 30 -50 the risk is 2% per 20 ys or 0. 1% per y. Between 50 -70 ys. The annual risk is 2/1000. Or 2% cumulative risk between 5060 years (0. 2% per annum) Cumulative number of Deaths for 100 ‘The Obstetrician and Gynecologist, Vol. . 1, October, 1999, No 2’ 000 female births, in England Wales, 1995
Ostrogen Hormone and Breast Cancer Analysis of world literature. Collaborative group on hormonal factors in breast cancer, Lancet 350: 1997 • There is a small but significant increase in risk beyond 5 years of HRT use. The relative risk is about 1. 3 at 15 years. (i. e. in the decade 50 -60 the HRT user for 5 -15 years may be considered to have an annual risk of 1. 3 0. 2% per annum of developing breast cancer). • The risk persists for 5 years after the end of therapy but not beyond that. The Obstetrician and Gynecologist, Vol. 1, 1999, No 2
Selective Estrogen Receptors Modulators ‘SERM’ Are group of antiestrogens that possess: Oestrogen Agonistic activity at desired targets: on bone and on lipoproteins. And Antagonistic action on the breast and the endometrium
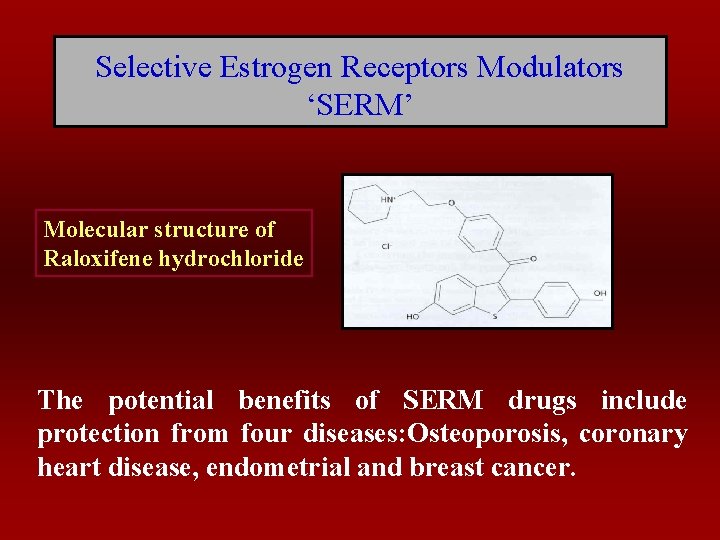
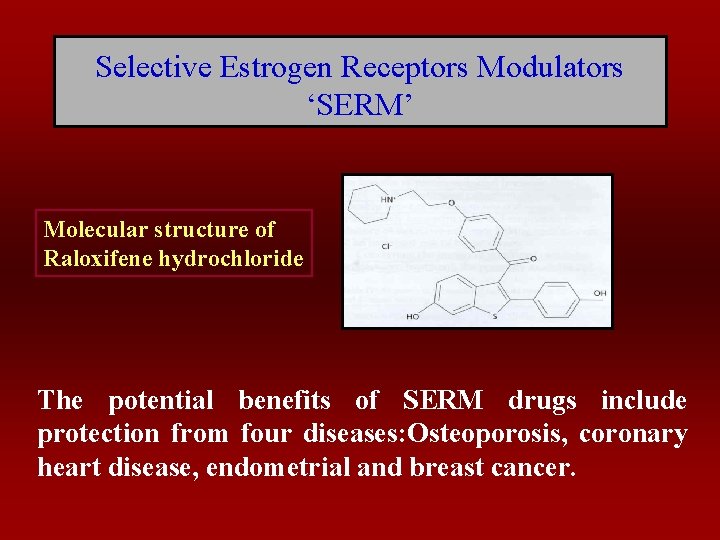
Selective Estrogen Receptors Modulators ‘SERM’ Molecular structure of Raloxifene hydrochloride The potential benefits of SERM drugs include protection from four diseases: Osteoporosis, coronary heart disease, endometrial and breast cancer.
 Postmenopausal endo thickness
Postmenopausal endo thickness Nasrat gyno
Nasrat gyno Frcs general surgery questions
Frcs general surgery questions Frcsed meaning
Frcsed meaning Titul frcs(t)
Titul frcs(t) Promotion from assistant to associate professor
Promotion from assistant to associate professor Once upon a time there lived a family of bears
Once upon a time there lived a family of bears Face recognition
Face recognition A woman travels in a lift. the mass of the woman is 50 kg
A woman travels in a lift. the mass of the woman is 50 kg Cones and rods are to vision as ____ are to audition
Cones and rods are to vision as ____ are to audition Hassan hadith
Hassan hadith Hassan akbari
Hassan akbari Caracterizarea lui pasa hassan
Caracterizarea lui pasa hassan Junaid hassan
Junaid hassan Hassan sayyadi
Hassan sayyadi Muhammad hasmi abu hassan asaari
Muhammad hasmi abu hassan asaari Hassan takabi
Hassan takabi Comparati baladele pasa hassan
Comparati baladele pasa hassan Hassan ben moussa
Hassan ben moussa Juxtra glomerular apparatus
Juxtra glomerular apparatus Dr hassan abdalla
Dr hassan abdalla Dr uzma hassan
Dr uzma hassan Junaid hassan
Junaid hassan Amanda hassan
Amanda hassan Hassan tout
Hassan tout Hassan foroosh
Hassan foroosh Mahmood ul hassan islamic aid
Mahmood ul hassan islamic aid Anhar hassan
Anhar hassan Assef kite runner
Assef kite runner Mohsen hassan
Mohsen hassan Yasir drabu
Yasir drabu Ent université hassan 2
Ent université hassan 2 Olu the wave
Olu the wave Sameera hassan
Sameera hassan Ayaz ul hassan
Ayaz ul hassan Dr hassan abdalla
Dr hassan abdalla Hassan chafi oracle
Hassan chafi oracle Sulamerica saude
Sulamerica saude Triploblast
Triploblast Marwan hassan mustafa
Marwan hassan mustafa Marcet boiler
Marcet boiler Hassan peerhossaini
Hassan peerhossaini Hassan makki
Hassan makki Dr mona idris
Dr mona idris