Telemedicine in Nursing Homes Murthy Gokula M D








- Slides: 42
Telemedicine in Nursing Homes Murthy Gokula, M. D. , C. M. D Associate Professor/Program Director(Geriatrics fellowship) University of Toledo
Objectives • Understand telemedicine • Discuss telemedicine to reduce hospitalizations in the nursing home • Understand STAY HOME project • What will we be using?
What is Telemedicine? • Telecommunications technology + Medicine = Telemedicine
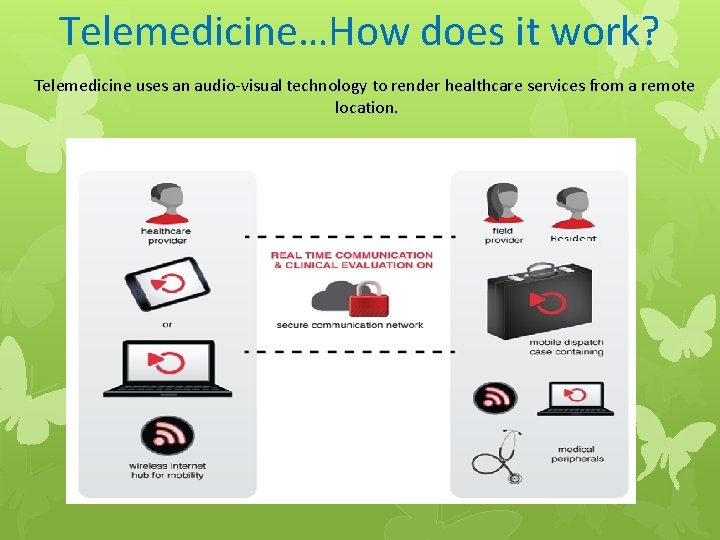
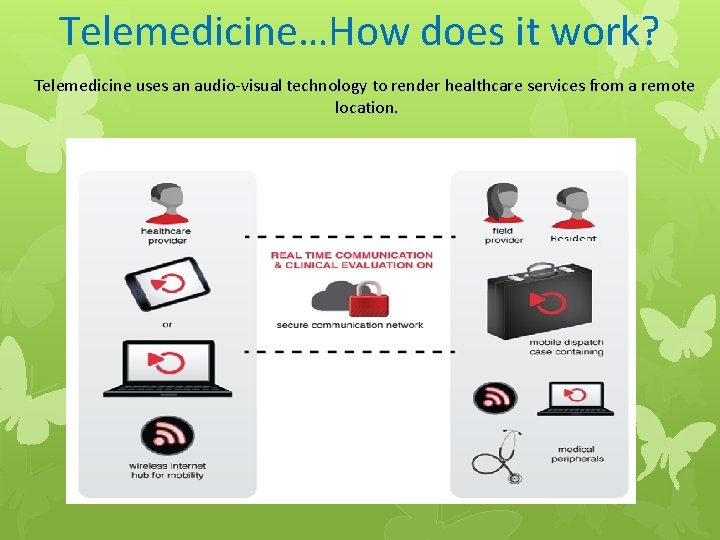
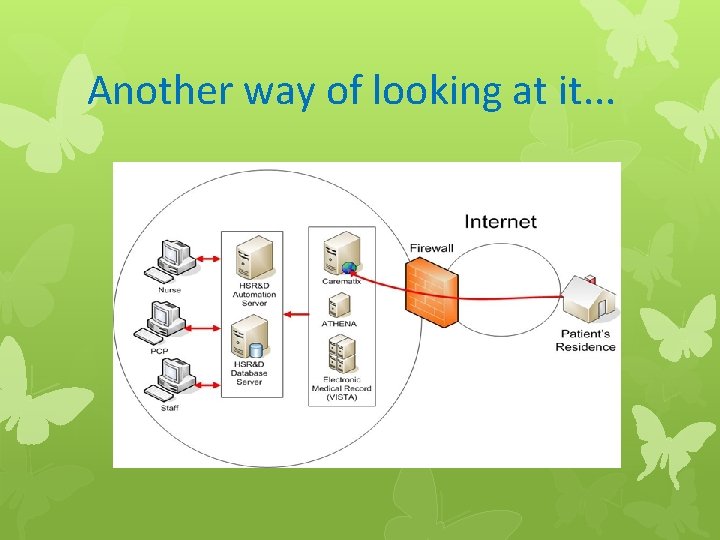
Telemedicine…How does it work? Telemedicine uses an audio-visual technology to render healthcare services from a remote location.
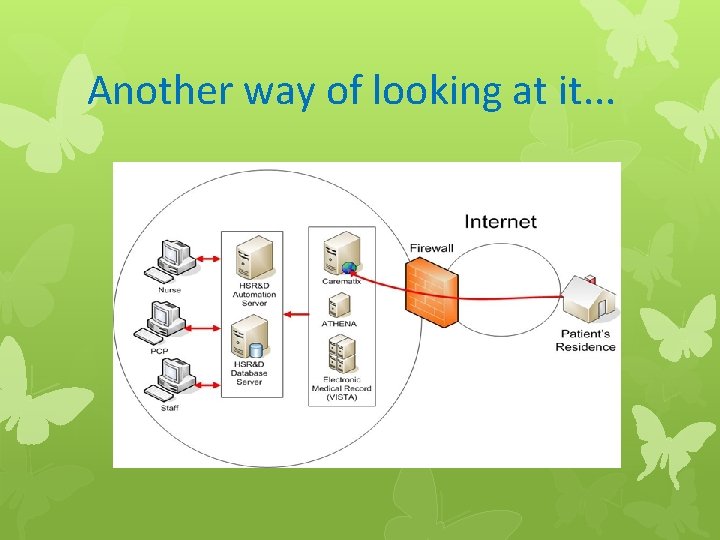
Another way of looking at it. . .
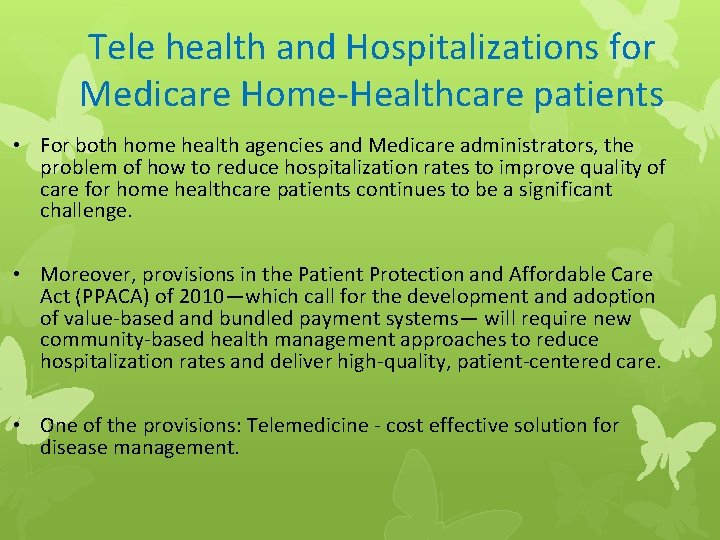
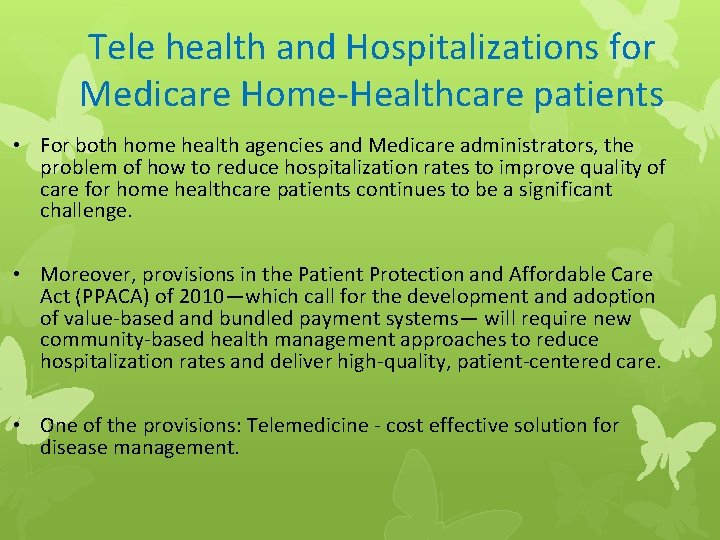
Tele health and Hospitalizations for Medicare Home-Healthcare patients • For both home health agencies and Medicare administrators, the problem of how to reduce hospitalization rates to improve quality of care for home healthcare patients continues to be a significant challenge. • Moreover, provisions in the Patient Protection and Affordable Care Act (PPACA) of 2010—which call for the development and adoption of value-based and bundled payment systems— will require new community-based health management approaches to reduce hospitalization rates and deliver high-quality, patient-centered care. • One of the provisions: Telemedicine - cost effective solution for disease management.
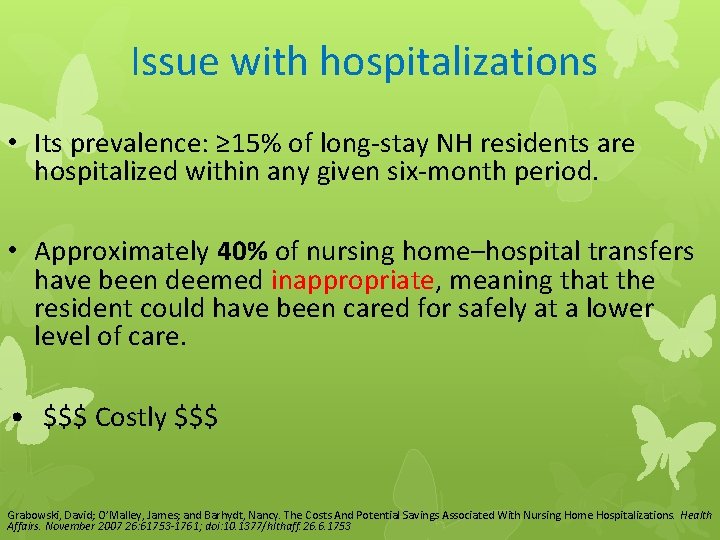
Issue with hospitalizations • Its prevalence: ≥ 15% of long-stay NH residents are hospitalized within any given six-month period. • Approximately 40% of nursing home–hospital transfers have been deemed inappropriate, meaning that the resident could have been cared for safely at a lower level of care. • $$$ Costly $$$ Grabowski, David; O’Malley, James; and Barhydt, Nancy. The Costs And Potential Savings Associated With Nursing Home Hospitalizations. Health Affairs. November 2007 26: 61753 -1761; doi: 10. 1377/hlthaff. 26. 6. 1753

More Issues with Hospitalizations They are often associated with negative health outcomes: • Falls • Incontinence • Dehydration • Adverse drug events • Iatrogenic disease • Delirium
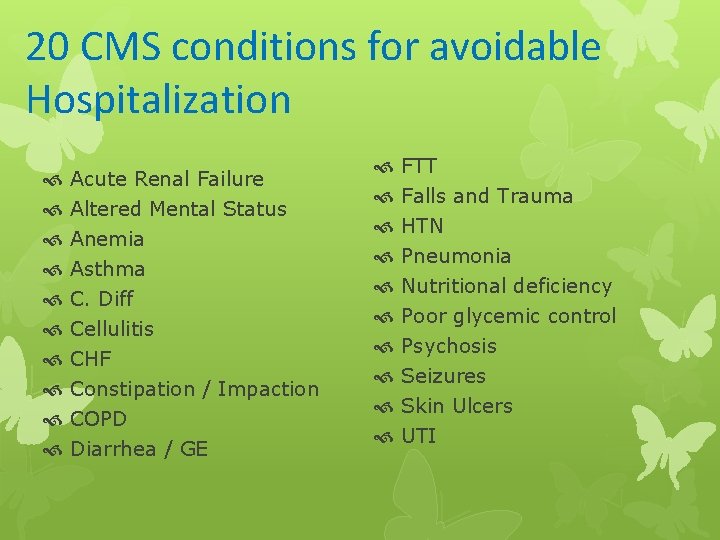
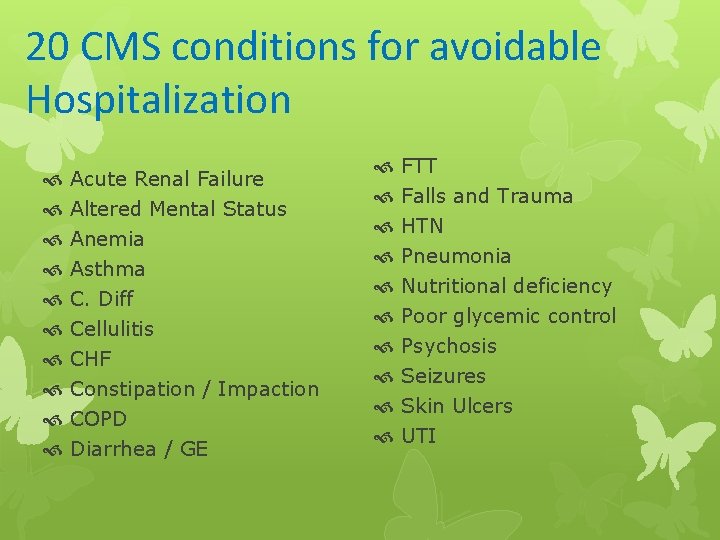
20 CMS conditions for avoidable Hospitalization Acute Renal Failure Altered Mental Status Anemia Asthma C. Diff Cellulitis CHF Constipation / Impaction COPD Diarrhea / GE FTT Falls and Trauma HTN Pneumonia Nutritional deficiency Poor glycemic control Psychosis Seizures Skin Ulcers UTI
Can telemedicine keep NH residents out of the hospital? • YES! It also reduces health care costs, according to a study in the Feb 2014 issue of Health Affairs. • Researchers from Harvard and Dartmouth universities studied 11 nursing homes in Massachusetts. They contracted with a telemedicine provider to cover urgent or emergent calls on weeknights and weekends. A medical secretary at the telemedicine service answered the after-hours calls and referred residents to a staff nurse, nurse practitioner or physician. Clinicians used 2 -way video conferencing and a high-resolution camera to examine residents and prescribe treatments. Researchers compared 2 years of outcomes from 6 nursing homes that used the telemedicine service and 5 nursing homes that did not. They also categorized nursing homes in the intervention group as “more engaged” or “less engaged, ” depending on how often they used the telemedicine service. Grabowski, David and O’Malley, James. THE CARE SPAN: Use Of Telemedicine Can Reduce Hospitalizations Of Nursing Home Residents and Generate
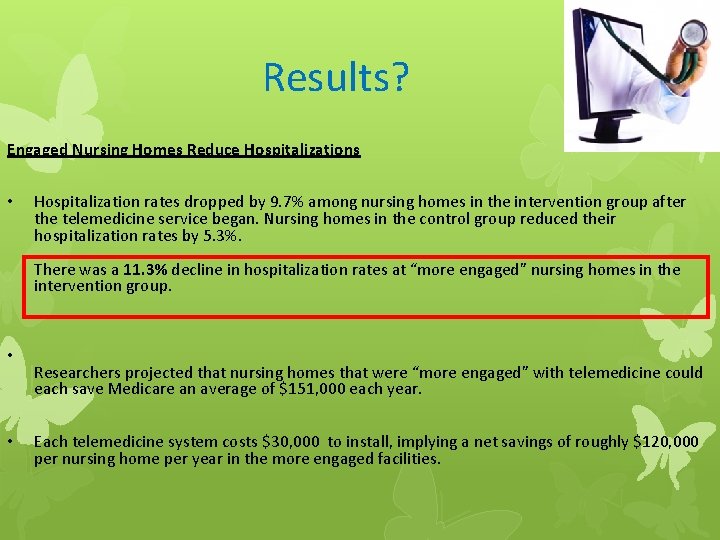
Results? Engaged Nursing Homes Reduce Hospitalizations • Hospitalization rates dropped by 9. 7% among nursing homes in the intervention group after the telemedicine service began. Nursing homes in the control group reduced their hospitalization rates by 5. 3%. There was a 11. 3% decline in hospitalization rates at “more engaged” nursing homes in the intervention group. • • Researchers projected that nursing homes that were “more engaged” with telemedicine could each save Medicare an average of $151, 000 each year. Each telemedicine system costs $30, 000 to install, implying a net savings of roughly $120, 000 per nursing home per year in the more engaged facilities.
Increasing Access to Specialty Care: A Pilot, Randomized Controlled Trial of Telemedicine for Parkinson’s Disease • A study evaluated the feasibility of providing subspecialty care via telemedicine for patients with Parkinson’s disease residing in a remote community located 130 miles from an academic movement disorders clinic. • 10 patients were randomized to receive telemedicine care with a movement disorder specialist (n=6) or their usual care (n=4). • Feasibility, as measured by the completion of telemedicine visits, was the primary outcome measure. Secondary measures were quality of life, patient satisfaction, and clinical outcomes. • Four nursing home patients were assigned to telemedicine. Those receiving telemedicine completed 97% (29 of 30) of their telemedicine visits as scheduled. • Compared with usual care, those randomized to telemedicine had significant improvements in quality of life (3. 4 point improvement vs. 10. 3 point worsening on the Parkinson’s Disease Questionnaire 39) and motor performance (0. 3 point improvement vs. 6. 5 point worsening on the Unified Parkinson’s Disease Rating Scale, motor subscale). • Relative to baseline, nursing home patients experienced trends toward improvement in quality of life and patient satisfaction. Providing subspecialty care via telemedicine for individuals with Parkinson’s disease living remotely is feasible. Dorsey, E. R. , Deuel, L. M. , Voss, T. S. , Finnigan, K. , George, B. P. , Eason, S. , Miller, D. , Reminick, J. I. , Appler, A. , Polanowicz, J. , Viti, L. , Smith, S. , Joseph, A. and Biglan, K. M. (2010), Increasing access to specialty care: A pilot, randomized controlled trial of telemedicine for Parkinson's disease. Mov. Disord. , 25: 1652– 1659. doi: 10. 1002/mds. 23145
ECHO-AGE: An Innovative Model of Geriatric Care for Long-Term Care Residents With Dementia and Behavioral Issues In another study, a remote case-based video-consultation program called ECHO-AGE was used. It linked experts in the management of behavior disorders in patients with dementia to nursing home care providers. Eleven long-term care sites in Massachusetts and Maine, presented challenging cases regarding residents with dementia and/or delirium related behavioral issues to specialists via video-conferencing. Baseline resident characteristics and follow-up data regarding compliance with ECHO-AGE recommendations, resident improvement, hospitalization, and mortality were collected from the long-term care sites. Results: Forty-seven residents, with a mean age of 82 years, were presented during the ECHO-AGE pilot period. Eighty-three percent of residents had a history of dementia and 44% were taking antipsychotic medications. The most common reasons for presentation were agitation, intrusiveness, and paranoia. Behavioral plans were recommended in 72. 3% of patients. Suggestions for medication adjustments were also frequent. ECHO-AGE recommendations were completely or partially followed in 88. 6% of residents. When recommendations were followed, sites were much more likely to report clinical improvement (74% vs 20%). Hospitalization was also less common among residents for whom recommendations were followed. TAKE HOME: case-based video-consultation program can be successful in improving the care of elders with dementia and/or delirium related behavioral issues by linking specialists with long-term care providers. Catic AG, Mattison ML, Bakaev I, Morgan M, Monti SM, Lipsitz L. ECHO-AGE: An Innovative Model of Geriatric Care for Long-Term Care Residents With Dementia and Behavioral Issues. J. Amer. Med. Dir. Assoc. [online before print], 2014
Effectiveness of telecare in elderly populations--a comparison of three settings • The primary aim of this study was to assess the level of satisfaction with 3 types of formal care systems of the elderly: – (1) a day care center, – (2) a nursing home, and – (3) telecare service in a group of oldest frail elderly, • The study involved a population of 162 oldest elderly. Study participants were asked to complete a questionnaire, investigating socio-demographic characteristics and degree of overall satisfaction with the service, as well as eliciting possible suggestions for improvement. • In our study, nearly all subjects using the telecare service were satisfied or very satisfied (98. 5%), as compared to 75. 3% of those residing in a nursing home, and 76. 5% of those attending the day care center. • This result confirms the findings of previous studies on elderly subjects' satisfaction with telecare services. Telecare, therefore, seems to be the service achieving the greatest levels of satisfaction, a service that can also be used by low-income subjects, by whom it is also perceived as a source of social support. Maria L. Onor, Marianna Trevisiol, Ornella Urciuoli, Shai Misan, Francesca Bertossi, Gabriella Tirone, Eugenio Aguglia, and Elisabetta Pascolo-Fabrici. Telemedicine and e. Health. March 2008, 14(2): 164 -169. doi: 10. 1089/tmj. 2007. 0028 .
Benefits of Telepsychiatry Consultation Service for Rural Nursing Home Residents • Psychiatric care for NH residents is difficult to obtain, especially in rural areas, and this deficiency may lead to significant morbidity or death. • Providing this service by videoconference may be a helpful, cost-effective, and acceptable alternative to face-to-face treatment. • A study analyzed data for 278 telepsychiatry encounters for 106 NH residents to estimate potential cost and time savings associated with this modality compared to in-person care (REFER TO TABLE): – A total of 843. 5 hours (105. 4 8 -hour work days) of travel time was saved compared to inperson consultation for each of the 278 encounters if they had occurred separately. – Travel distance saved was 43, 000 miles. – More than $3, 700 would be spent on gas for 278 separate encounters. – Personnel cost savings estimates ranged from $33, 739 to $67, 477. – Physician costs associated with additional travel time ranged from $84, 347 to $253, 040 for 278 encounters.

The point? • Although telemedicine applications for the general population are relatively widespread and numbers are increasing, less has been accomplished specific to elders, though they are a major target group for telemedicine interventions, who appear to benefit from and to be accepting of a telemedicine approach to their needs. • The tele psychiatry approach was enthusiastically accepted by virtually all residents, family members, and NH personnel, and led to successful patient management. • In addition, this approach will allow many nursing homes to provide essential care that would not otherwise be available. Terry Rabinowitz, Katharine M. Murphy, Judith L. Amour, Michael A. Ricci, Michael P. Caputo, and Paul A. Newhouse. Telemedicine and e-Health. January/February 2010, 16(1): 34 -40. doi: 10. 1089/tmj. 2009. 0088
Long term effect of home telehealth services on preventable hospitalization use • In this study, the longitudinal effect of a Department of Veterans Affairs (VA) patient -centered Care Coordination Home Telehealth (CCHT) program on preventable hospitalization use by veterans with diabetes mellitus (DM) at four VA medical centers was assessed. • All patients were followed for 4 years. • During the initial 18 months of follow-up, CCHT enrollees were less likely to be admitted for a preventable hospitalization than their non-enrollee counterparts, and this difference diminished during the rest of the 4 -year follow-up period. • The VA CCHT program for DM patients reduced preventable hospitalizations. These findings are some of the first that have systematically examined the extent to which home telehealth programs have a long-term effect on preventable hospitalization use. Jia, H; Chuang, HC; Wu, SS; Wang, X; Chumbler, NR. Long-term effect of home telehealth services on preventable hospitalization use. J Rehabil Res Dev. 2009; 46(5): 557 -66.
Today >16, 000+ patients enrolled in daily home telehealth with Health Buddy Over 100 programs for 30+ chronic conditions FEB 2006

This is new. . .
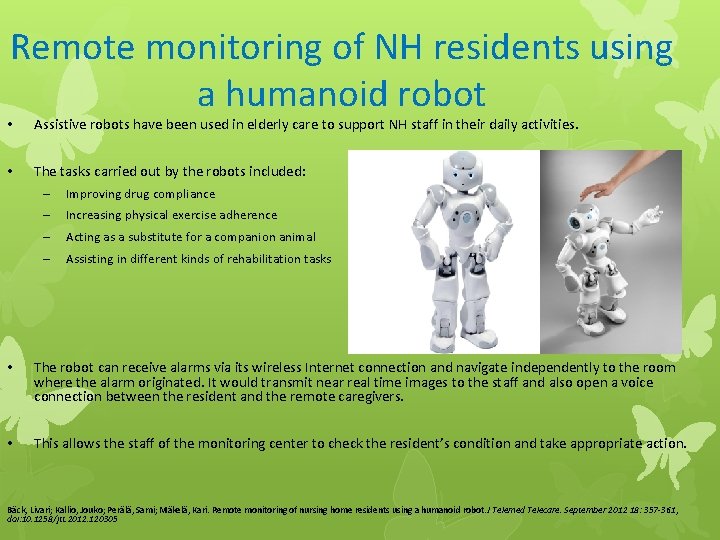
Remote monitoring of NH residents using a humanoid robot • Assistive robots have been used in elderly care to support NH staff in their daily activities. • The tasks carried out by the robots included: – Improving drug compliance – Increasing physical exercise adherence – Acting as a substitute for a companion animal – Assisting in different kinds of rehabilitation tasks • The robot can receive alarms via its wireless Internet connection and navigate independently to the room where the alarm originated. It would transmit near real time images to the staff and also open a voice connection between the resident and the remote caregivers. • This allows the staff of the monitoring center to check the resident’s condition and take appropriate action. Bäck, Livari; Kallio, Jouko; Perälä, Sami; Mäkelä, Kari. Remote monitoring of nursing home residents using a humanoid robot. J Telemed Telecare. September 2012 18: 357 -361, doi: 10. 1258/jtt. 2012. 120305
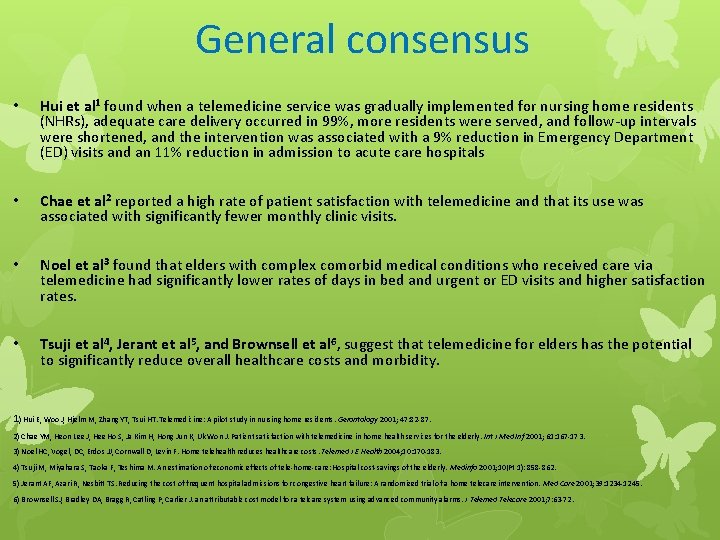
General consensus • Hui et al 1 found when a telemedicine service was gradually implemented for nursing home residents (NHRs), adequate care delivery occurred in 99%, more residents were served, and follow-up intervals were shortened, and the intervention was associated with a 9% reduction in Emergency Department (ED) visits and an 11% reduction in admission to acute care hospitals • Chae et al 2 reported a high rate of patient satisfaction with telemedicine and that its use was associated with significantly fewer monthly clinic visits. • Noel et al 3 found that elders with complex comorbid medical conditions who received care via telemedicine had significantly lower rates of days in bed and urgent or ED visits and higher satisfaction rates. • Tsuji et al 4, Jerant et al 5, and Brownsell et al 6, suggest that telemedicine for elders has the potential to significantly reduce overall healthcare costs and morbidity. 1) Hui E, Woo J, Hjelm M, Zhang YT, Tsui HT. Telemedicine: A pilot study in nursing home residents. Gerontology 2001; 47: 82 -87. 2) Chae YM, Heon Lee J, Hee Ho S, Ja Kim H, Hong Jun K, Uk Won J. Patient satisfaction with telemedicine in home health services for the elderly. Int J Med Inf 2001; 61: 167 -173. 3) Noel HC, Vogel, DC, Erdos JJ, Cornwall D, Levin F. Home telehealth reduces healthcare costs. Telemed J E Health 2004; 10: 170 -183. 4) Tsuji M, Miyahara S, Taoka F, Teshima M. An estimation of economic effects of tele-home-care: Hospital cost-savings of the elderly. Medinfo 2001; 10(Pt 1): 858 -862. 5) Jerant AF, Azari R, Nesbitt TS. Reducing the cost of frequent hospital admissions for congestive heart failure: A randomized trial of a home telecare intervention. Med Care 2001; 39: 1234 -1245. 6) Brownsell SJ, Bradley DA, Bragg R, Catling P, Carlier J. an attributable cost model for a telcare system using advanced community alarms. J Telemed Telecare 2001; 7: 63 -72.
STAY HOME Project – Background (Strategic Team Activity Yielding High Outcomes and Minimizing Expenditures) • Many avoidable ED visits and hospitalizations occur among NH residents • These visits lead to increased health care costs and affect the quality of care and life for the residents • The first step in addressing the problem is to determine the root cause
STAY HOME - Purpose • Purpose of this project was to determine the rate and characteristics of avoidable transfers of NH residents to acute care (hospitalization)
STAY HOME - Method • This project is the first phase of the STAY HOME project establishing baseline data • Two facilities provided transfer lists for each month (January -July 2014) • The data included reason for transfer from NH to acute care (hospitalization), date of transfer and the discharge diagnosis
STAY HOME - Methods (Contd. ) • Chart review was completed on 29% (N=44) of the 151 of these transfers using the INTERACT Quality Improvement Tool

INTERACT 3 Quality Tool
Results • 151 residents were transferred during the 7 month period at the 2 facilities (site 1 =87; site 2=64) • Over ¼ of the transferred residents were categorized as at-risk for transfer, as a result of multiple co-morbidities and polypharmacy
Results Unplanned hospitalization rates for the 2 facilities for the 7 month period was: • Site 1: 4. 42 admissions every 10 days • Site 2: 2. 55 admissions every 10 days
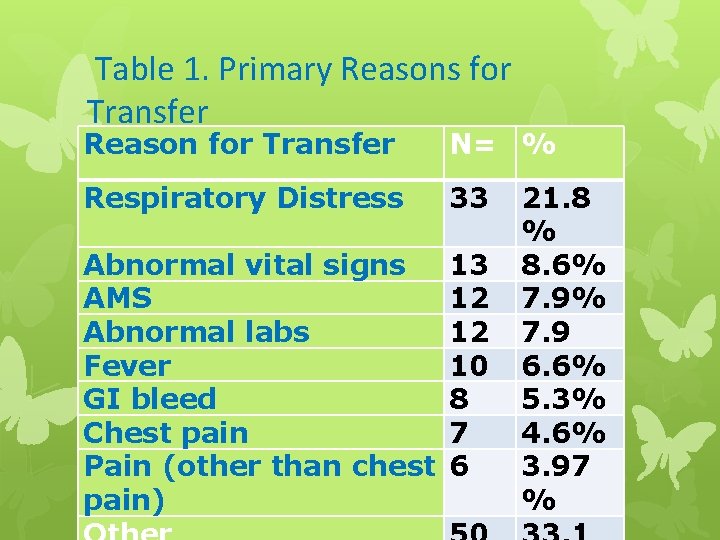
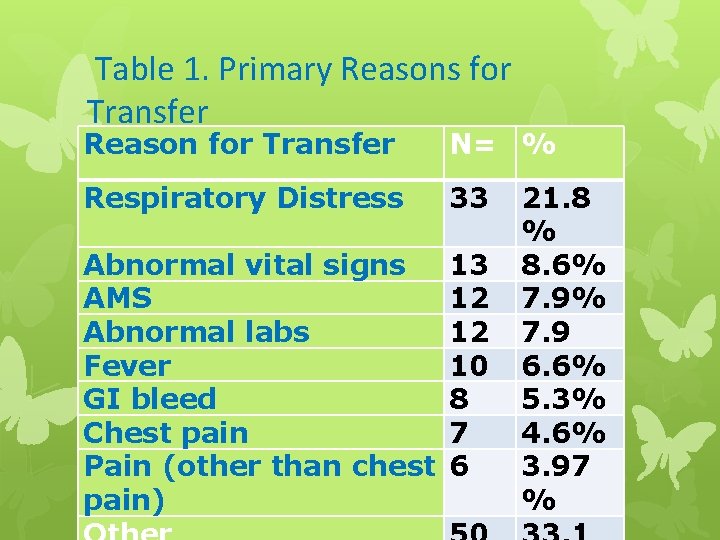
Table 1. Primary Reasons for Transfer Reason for Transfer N= % Respiratory Distress 33 Abnormal vital signs AMS Abnormal labs Fever GI bleed Chest pain Pain (other than chest pain) 13 12 12 10 8 7 6 21. 8 % 8. 6% 7. 9 6. 6% 5. 3% 4. 6% 3. 97 %
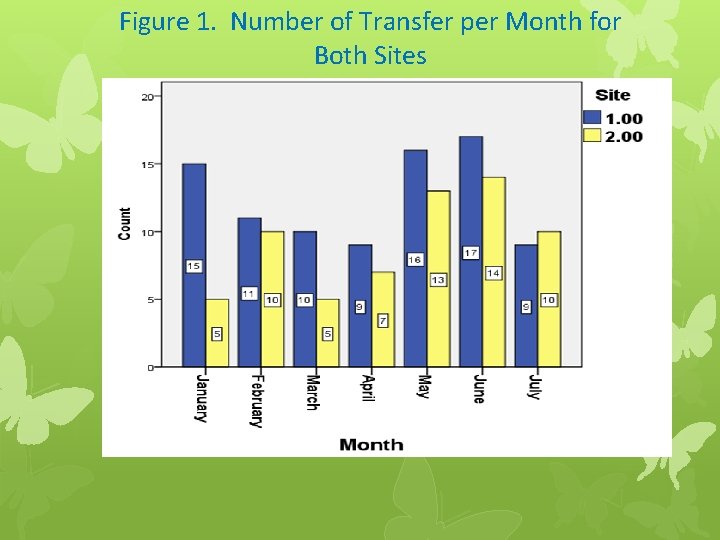
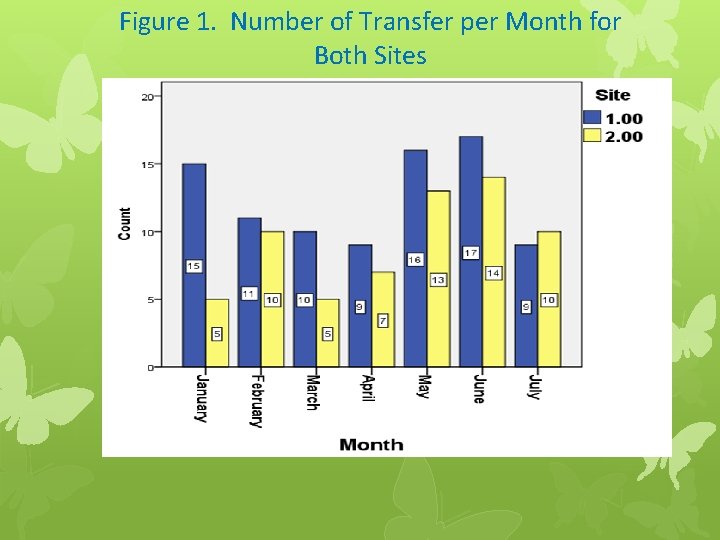
Figure 1. Number of Transfer per Month for Both Sites
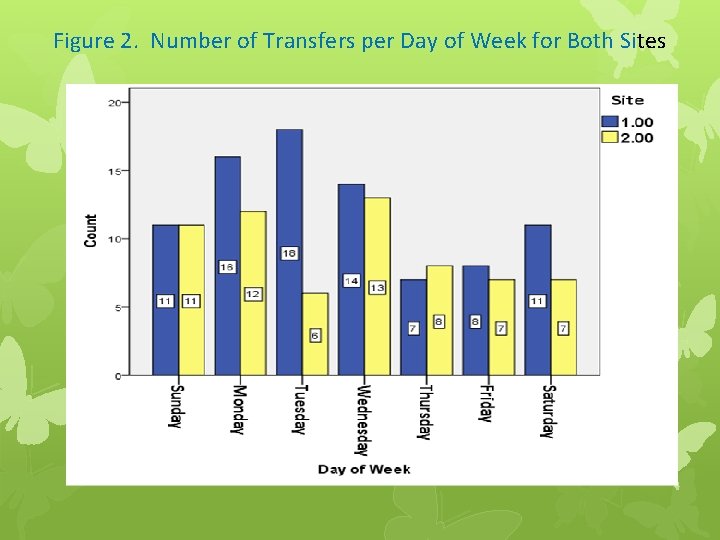
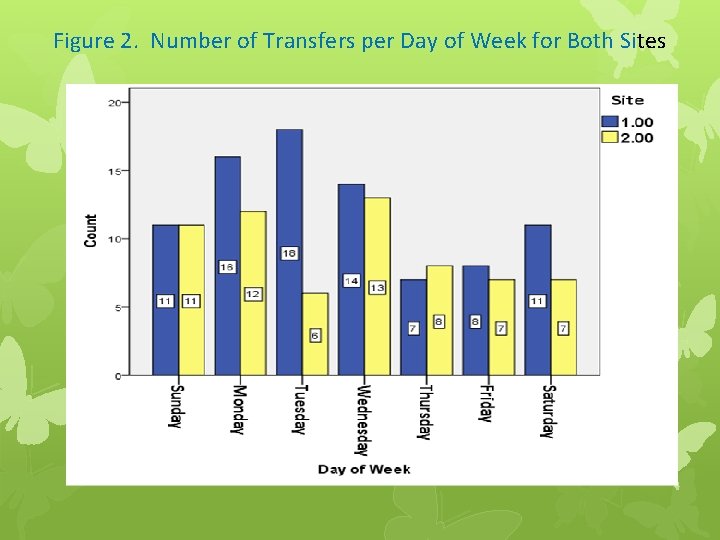
Figure 2. Number of Transfers per Day of Week for Both Sites
Conclusions • Further exploration of the potential use of tele-health for assessment and management of acute changes in condition is essential • Telemedicine is a feasible and potentially beneficial means for increasing access to specialty care for a large and growing population. • Future research should focus on how to adapt systems to the individual needs (deficit in cognitive function, physical limitation and comorbidities) and resources of elderly patients within the specific frameworks of the respective national healthcare systems

We will be using. . . HNC IT Support: 248 -926 -1661

Medical Peripherals include. . .
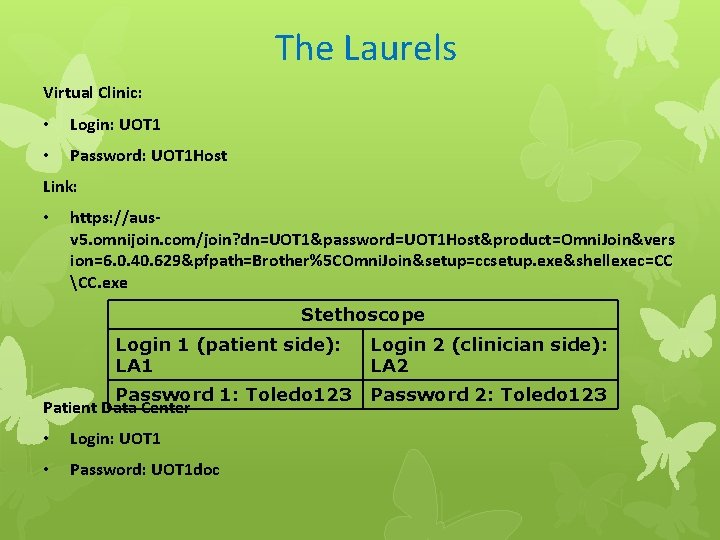
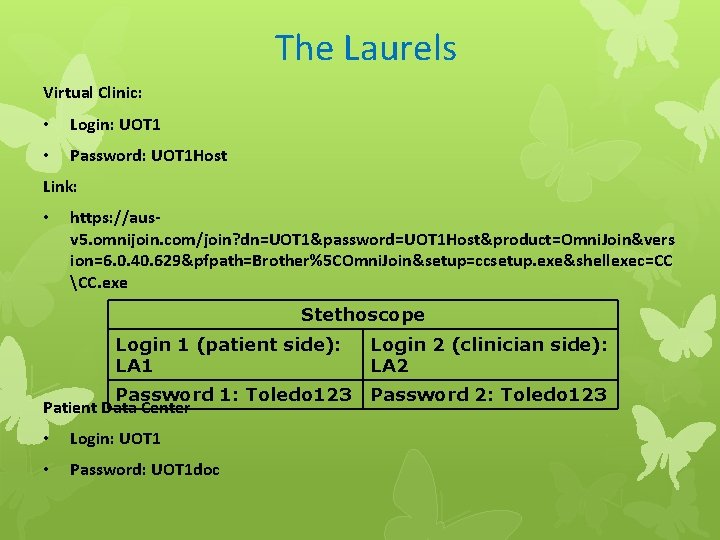
The Laurels Virtual Clinic: • Login: UOT 1 • Password: UOT 1 Host Link: • https: //ausv 5. omnijoin. com/join? dn=UOT 1&password=UOT 1 Host&product=Omni. Join&vers ion=6. 0. 40. 629&pfpath=Brother%5 COmni. Join&setup=ccsetup. exe&shellexec=CC CC. exe Stethoscope Login 1 (patient side): LA 1 Password 1: Toledo 123 Patient Data Center • Login: UOT 1 • Password: UOT 1 doc Login 2 (clinician side): LA 2 Password 2: Toledo 123
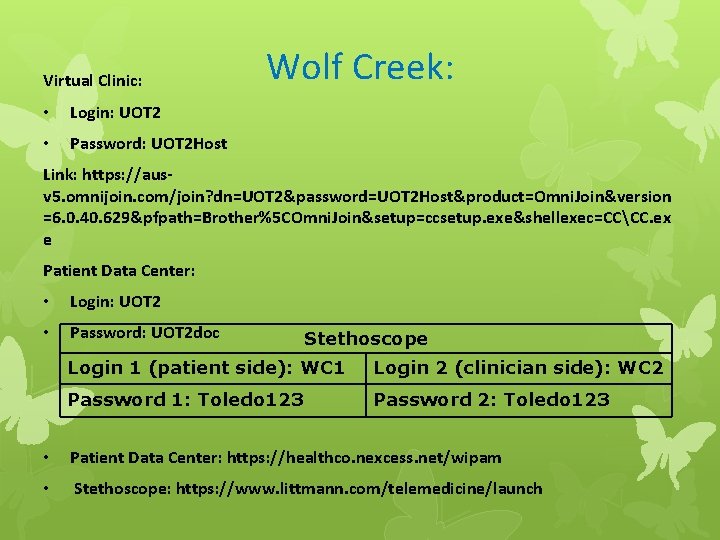
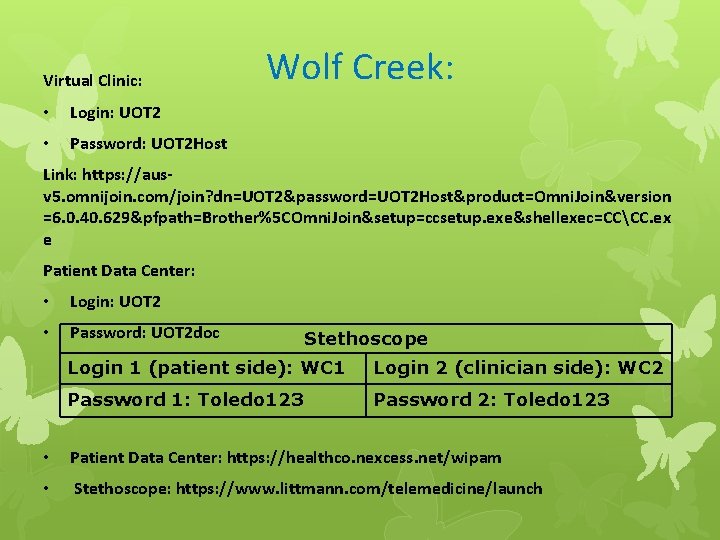
Virtual Clinic: • Login: UOT 2 • Password: UOT 2 Host Wolf Creek: Link: https: //ausv 5. omnijoin. com/join? dn=UOT 2&password=UOT 2 Host&product=Omni. Join&version =6. 0. 40. 629&pfpath=Brother%5 COmni. Join&setup=ccsetup. exe&shellexec=CCCC. ex e Patient Data Center: • Login: UOT 2 • Password: UOT 2 doc Stethoscope Login 1 (patient side): WC 1 Login 2 (clinician side): WC 2 Password 1: Toledo 123 Password 2: Toledo 123 • Patient Data Center: https: //healthco. nexcess. net/wipam • Stethoscope: https: //www. littmann. com/telemedicine/launch
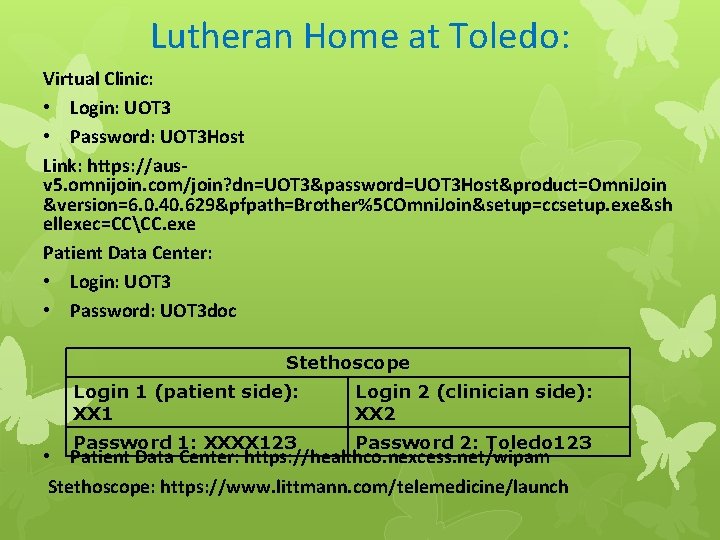
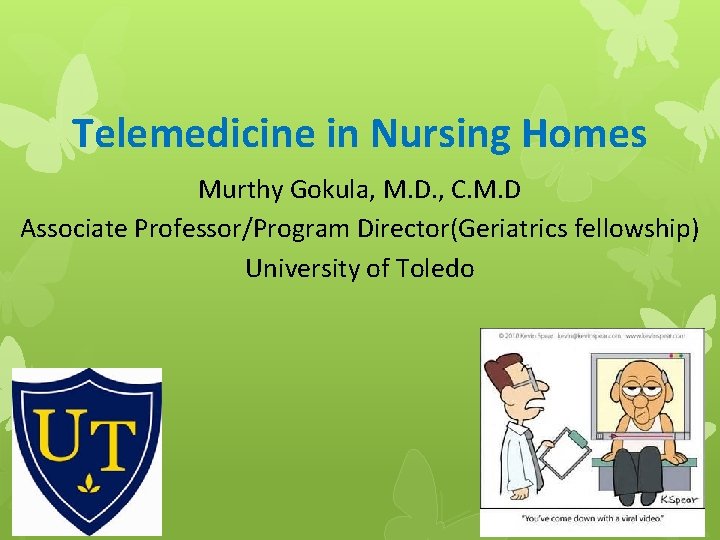
Lutheran Home at Toledo: Virtual Clinic: • Login: UOT 3 • Password: UOT 3 Host Link: https: //ausv 5. omnijoin. com/join? dn=UOT 3&password=UOT 3 Host&product=Omni. Join &version=6. 0. 40. 629&pfpath=Brother%5 COmni. Join&setup=ccsetup. exe&sh ellexec=CCCC. exe Patient Data Center: • Login: UOT 3 • Password: UOT 3 doc Stethoscope Login 1 (patient side): XX 1 Login 2 (clinician side): XX 2 Password 1: XXXX 123 Password 2: Toledo 123 • Patient Data Center: https: //healthco. nexcess. net/wipam Stethoscope: https: //www. littmann. com/telemedicine/launch
Discussion - Are you involved? • Audience - Any previous experiences with telehealth? • Reluctance - and reasons • Can our society afford not to bring telehealth into our healthcare management situations?

RESOURCES Telehealth Resource Centers Toolkits • http: //www. telehealthresourcecenter. org/toolbo x. php

Thank You
 Murthy gokula
Murthy gokula Sai gokula seva samsthe
Sai gokula seva samsthe Jln murthy advocate
Jln murthy advocate Shashi murthy
Shashi murthy Arun c murthy
Arun c murthy Ashlesh murthy
Ashlesh murthy K ramachandra murthy
K ramachandra murthy Pranav murthy
Pranav murthy Telehealth and telemedicine
Telehealth and telemedicine Bric telemedicine market
Bric telemedicine market Telemedicine basics
Telemedicine basics Vsee telemedicine kit
Vsee telemedicine kit Telemedicine wiki
Telemedicine wiki Telemedicine wikipedia
Telemedicine wikipedia Medisoft telemedicine pvt ltd
Medisoft telemedicine pvt ltd Telemedicine software
Telemedicine software Ethical hacking wikipedia
Ethical hacking wikipedia Drug diversion investigation checklist
Drug diversion investigation checklist Qapi template for nursing homes
Qapi template for nursing homes Nursing homes day out an
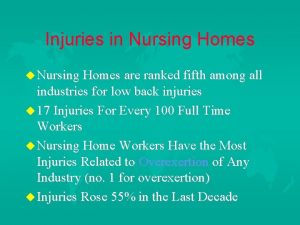
Nursing homes day out an Ergonomics
Ergonomics New yorkers spaces homes
New yorkers spaces homes Postmodern architecture homes
Postmodern architecture homes Timestatement
Timestatement What types of homes existed in salem
What types of homes existed in salem Who was the first state advisor of georgia nha
Who was the first state advisor of georgia nha Labana developers llp
Labana developers llp Tiny homes in las vegas
Tiny homes in las vegas Heatherman homes llc
Heatherman homes llc Enhanced health in care homes
Enhanced health in care homes Examples of homely remedies
Examples of homely remedies Wappetaw landing awendaw homes for sale
Wappetaw landing awendaw homes for sale Abu bakr homes
Abu bakr homes Homes-for-sale.file?login_id=
Homes-for-sale.file?login_id= Eastern woodland tools
Eastern woodland tools Snugbug homes
Snugbug homes Ancient greek homes
Ancient greek homes 11245 lantern road fishers in 46038
11245 lantern road fishers in 46038 Gabrielino tribe shelter
Gabrielino tribe shelter Chelsea modular homes
Chelsea modular homes Middle colonies homes
Middle colonies homes Homes with purpose
Homes with purpose Homes for sale knightstown
Homes for sale knightstown