Supporting and developing organisational change for personcentred coordinated

![Overview of session [1] Background: our P 3 C programme of work [2] Background: Overview of session [1] Background: our P 3 C programme of work [2] Background:](https://slidetodoc.com/presentation_image_h/098d9446347a6397af33f04c49eb0d54/image-2.jpg)
![[1] Shared Understanding: Domains and sub-domains of P 3 C My goals • Goal [1] Shared Understanding: Domains and sub-domains of P 3 C My goals • Goal](https://slidetodoc.com/presentation_image_h/098d9446347a6397af33f04c49eb0d54/image-8.jpg)
![[2] Evaluation of P 3 C. Multi level, Multi Perspective Measurements of Change: Complex [2] Evaluation of P 3 C. Multi level, Multi Perspective Measurements of Change: Complex](https://slidetodoc.com/presentation_image_h/098d9446347a6397af33f04c49eb0d54/image-10.jpg)


- Slides: 33

Supporting and developing organisational change for personcentred coordinated care (P 3 C) using a practice-based tool (P 3 C-OCT) Dr James Close, Ben Fosh, Dr Helen Lloyd
![Overview of session 1 Background our P 3 C programme of work 2 Background Overview of session [1] Background: our P 3 C programme of work [2] Background:](https://slidetodoc.com/presentation_image_h/098d9446347a6397af33f04c49eb0d54/image-2.jpg)
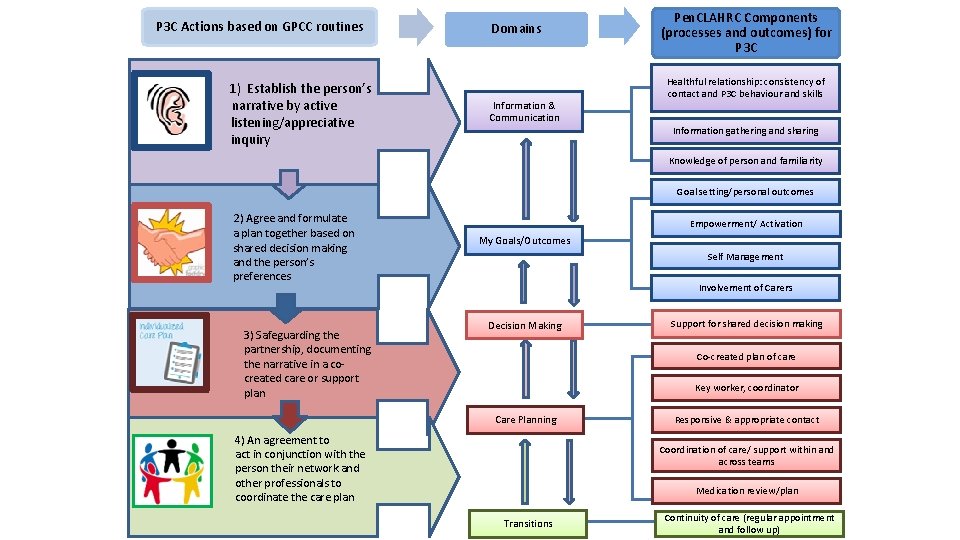
Overview of session [1] Background: our P 3 C programme of work [2] Background: measuring change using our consistent evaluation framework • • • Patients: P 3 C-EQ Our portal for patient-reported measures: P 3 c. org. uk Practitioners: P 3 C-Practitioner Organisations: P 3 C-OCT [3] Development and design of the P 3 C-OCT ~Interlude~ Workshop participants will fill out “mini P 3 C-OCT” for 10 minutes [4] P 3 C-OCT in context: Somerset Practice Quality Scheme (SPQS) [5] Ben Fosh: P 3 C-OCT dashboard demonstration (Ben Fosh) Workshop participant feedback on P 3 C-OCT Dashboard Workshop participant facilitation with “mini P 3 C-OCT”
The Context of the P 3 C Programme CLAHRCs • • 13 CLAHRCs ‘the research arm of the NHS’ Essential functions: • • Translate research findings into improved outcomes for patients Address applied and relevant issues to improve the process and function of statutory services Core team: Dr Helen Lloyd, Professor Richard Byng, Ben Fosh, Debra Westlake, James Close, Felix Gradginger, Julian Elston. SWAHSN: Richard Blackwell, Louise Witts, Louise Hall and Caroline Powell. Wider partners: Dr Mark Pearson and Professors José Valderas, Sheena Asthana, Nicky Britten and Rod Sheaff. AHSNs • 15 AHSNs aim to improve health and economic growth, seed innovation into practice, connect academics, researchers, the public and industry Services we work with: Somerset CCG, NEW Devon, Cornwall and Exeter. Links to organisations throughout the UK: Health Foundation, NHSE, C 4 CC, Do. H, West Midlands CLAHRC, Universities of Warwick, Birmingham & Kent.
Person Centred Coordinated Care (P 3 C) ‘Care and support that is guided by and organised effectively around the needs and preferences of the individuals’ • Challenge of long-term conditions (LTCs) & multimorbidity • Individuals with complex health and social care needs continue to experience fragmented care • New models of care • 5 YFV and the GPFV
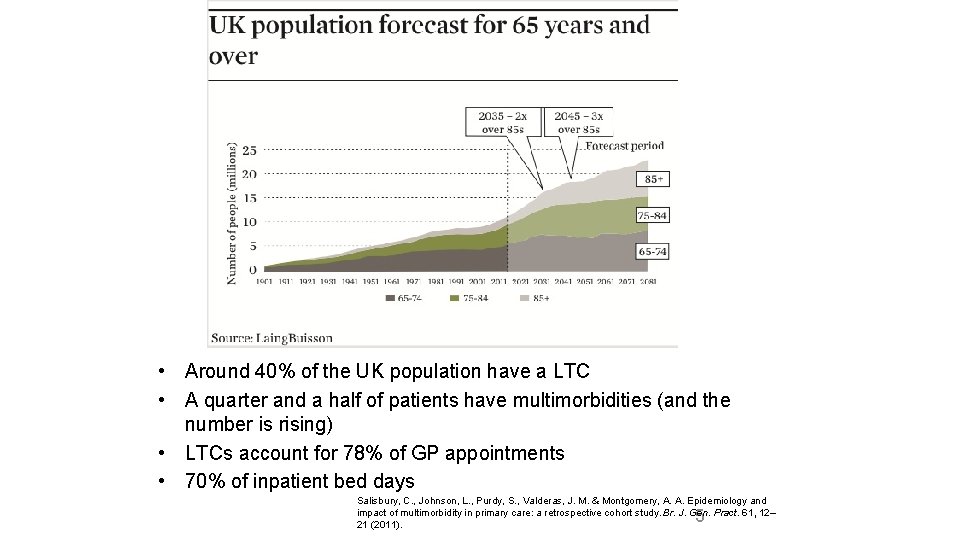
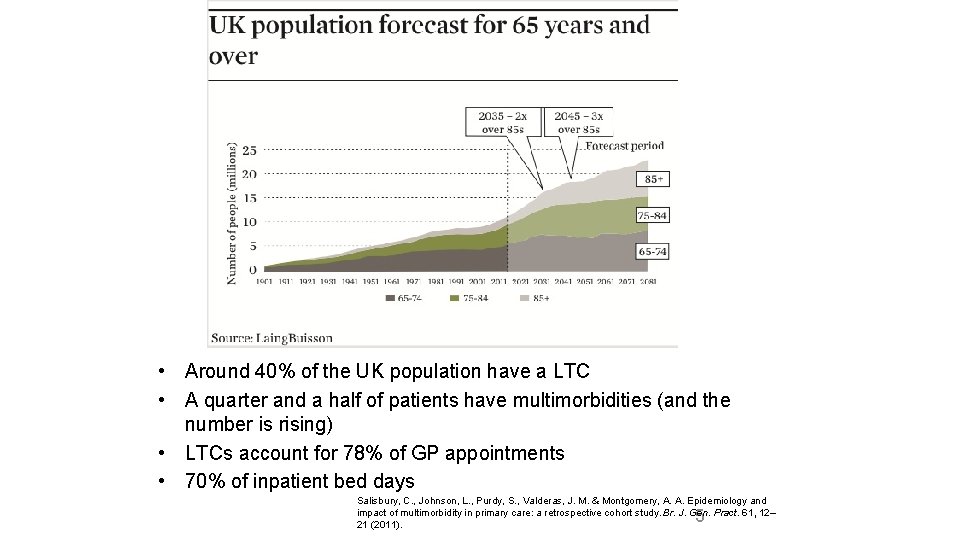
• Around 40% of the UK population have a LTC • A quarter and a half of patients have multimorbidities (and the number is rising) • LTCs account for 78% of GP appointments • 70% of inpatient bed days Salisbury, C. , Johnson, L. , Purdy, S. , Valderas, J. M. & Montgomery, A. A. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br. J. Gen. Pract. 61, 12– 21 (2011). 5
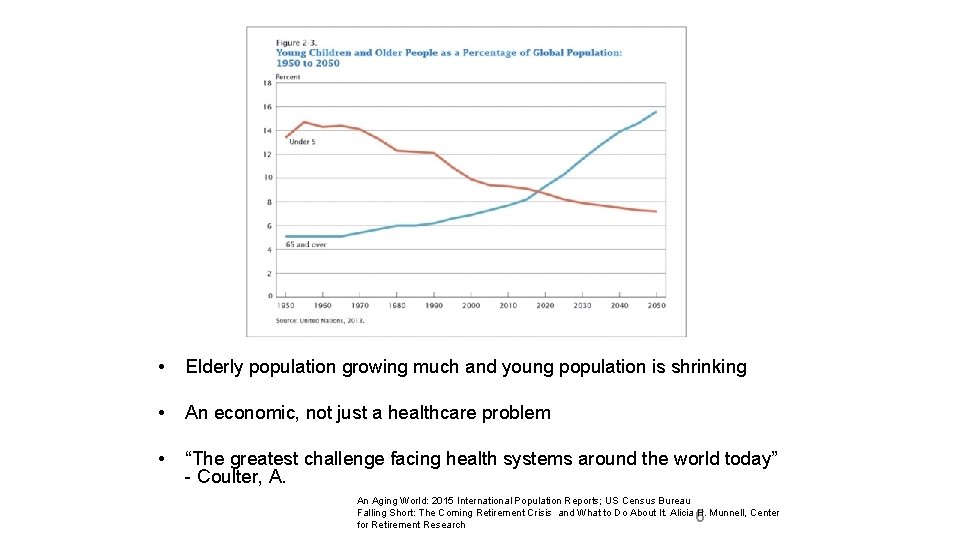
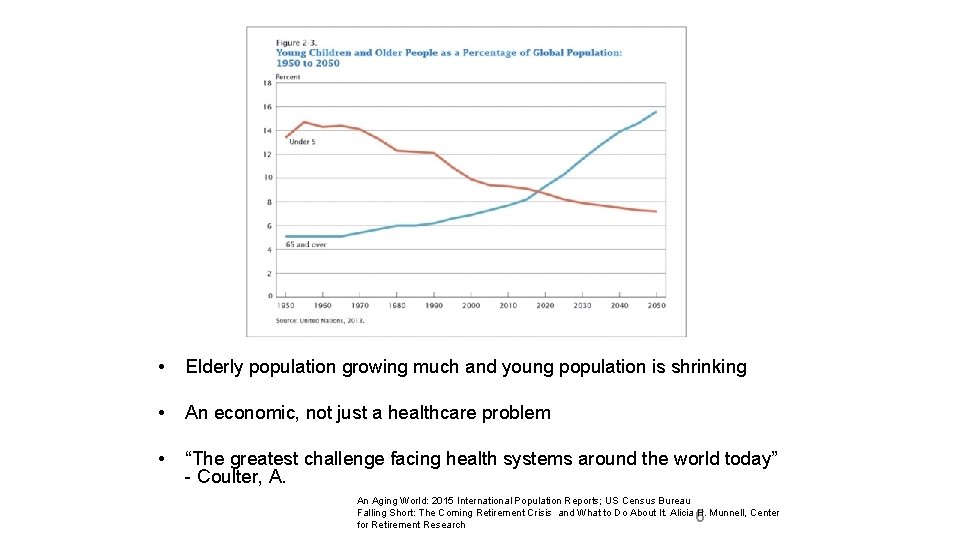
• Elderly population growing much and young population is shrinking • An economic, not just a healthcare problem • “The greatest challenge facing health systems around the world today” - Coulter, A. An Aging World: 2015 International Population Reports; US Census Bureau Falling Short: The Coming Retirement Crisis and What to Do About It. Alicia H. Munnell, Center for Retirement Research 6
Our Work: The P 3 C Programme Overarching aims of the programme • • Support services to develop Person Centred Coordinated approaches. Work with them to understand if they work, for whom they work and why they work. Specific aims of the programme [1] Developing a ‘Shared Understanding’ of P 3 C [2] A consistent framework of evaluation and measurement: a multi perspective, multi level approach with sufficient depth and breadth to handle complexity and build theory across localities trialling new initiatives: a) Organisational change b) Experience of patients and practitioners c) Process of care – crises, contacts, cost [3] Collaborative: learning together with services as they develop, using logic models, identifying barriers, supporting iterative and on going change through feedback cycles.
![1 Shared Understanding Domains and subdomains of P 3 C My goals Goal [1] Shared Understanding: Domains and sub-domains of P 3 C My goals • Goal](https://slidetodoc.com/presentation_image_h/098d9446347a6397af33f04c49eb0d54/image-8.jpg)
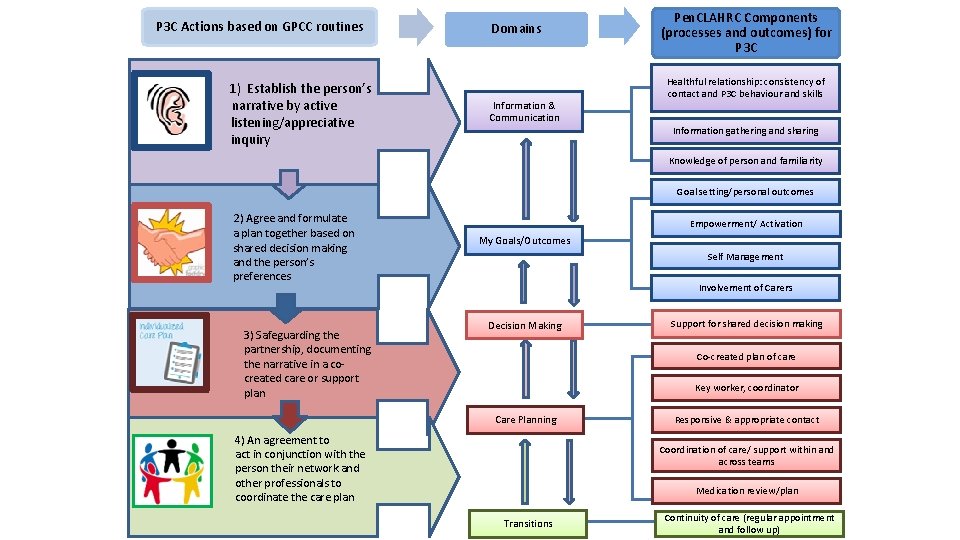
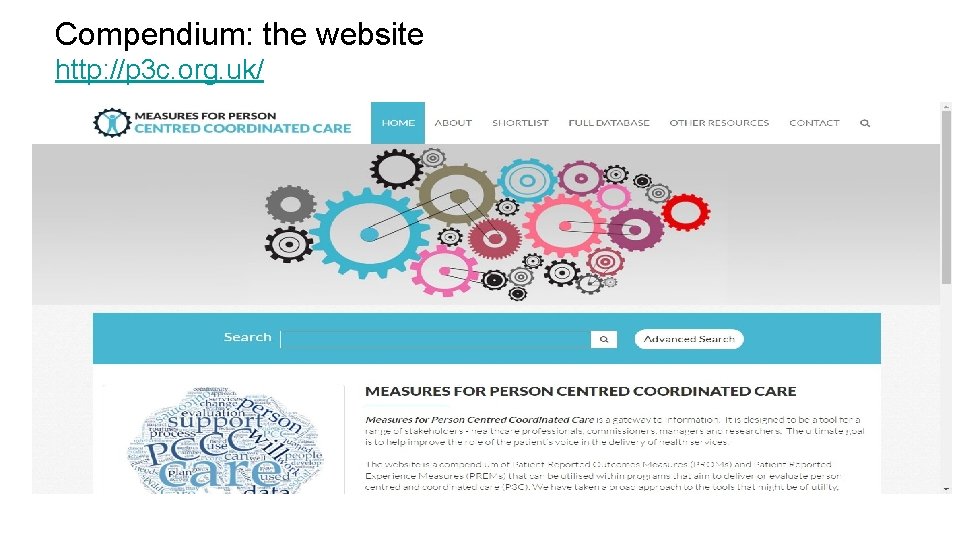
[1] Shared Understanding: Domains and sub-domains of P 3 C My goals • Goal setting • Empowerment & Activation • Self-management • Carer support Decision Making Care Planning • The care plan • Case management • Single point of contact • Care coordination (within teams and across teams ) Information & Communication • Relational continuity • Information gathering/sharing • Knowledge of Evidence for this model was derived from: patient/familiarity • Key literature: e. g. Ed Harding - ‘State of Play in PCC’, lead reviews etc. . • House of Care • National voices I statements • Gothenburg Model (GPCC) • Our work • Involvement in decision making Transitions • Continuity of care Organisational Process Activities • Valuing physical & mental health equally • Proactive case management • Experience of care • Longer appointment times • Staff training • Supporting people to stay at home
P 3 C Actions based on GPCC routines 1) Establish the person’s narrative by active listening/appreciative inquiry Domains Information & Communication Pen. CLAHRC Components (processes and outcomes) for P 3 C Healthful relationship: consistency of contact and P 3 C behaviour and skills Information gathering and sharing Knowledge of person and familiarity Goal setting/personal outcomes 2) Agree and formulate a plan together based on shared decision making and the person’s preferences 3) Safeguarding the partnership, documenting the narrative in a cocreated care or support plan Empowerment/ Activation My Goals/Outcomes Self Management Involvement of Carers Decision Making Support for shared decision making Co-created plan of care Key worker, coordinator Care Planning 4) An agreement to act in conjunction with the person their network and other professionals to coordinate the care plan Responsive & appropriate contact Coordination of care/ support within and across teams Medication review/plan Transitions Continuity of care (regular appointment and follow up)
![2 Evaluation of P 3 C Multi level Multi Perspective Measurements of Change Complex [2] Evaluation of P 3 C. Multi level, Multi Perspective Measurements of Change: Complex](https://slidetodoc.com/presentation_image_h/098d9446347a6397af33f04c49eb0d54/image-10.jpg)
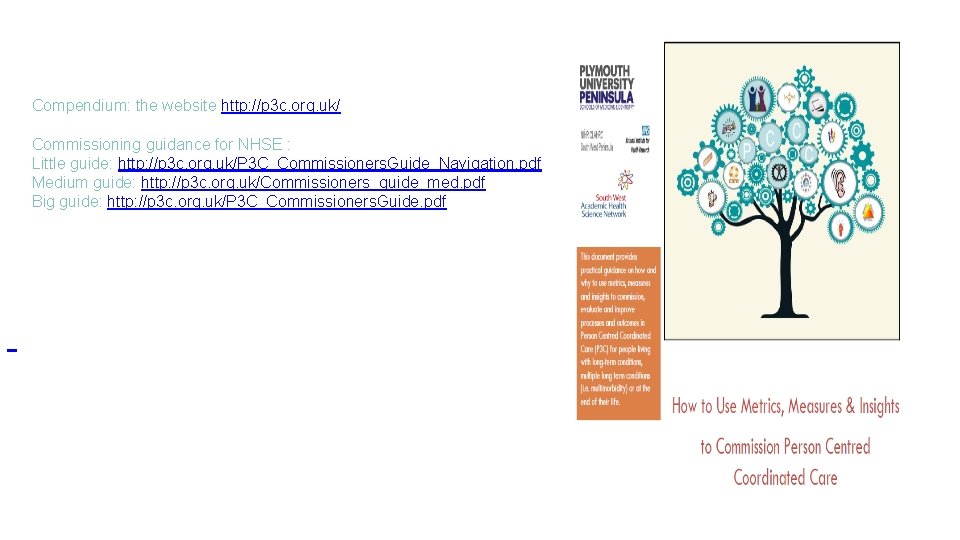
[2] Evaluation of P 3 C. Multi level, Multi Perspective Measurements of Change: Complex P 3 C Interventions Linking data bases across services Systems, IT, agreements etc. cost Annual P 3 C-OCT Practitioner activities: Qualitative approaches Patient activities Mortality Morbidity Quality of life Edinburgh Warwick Practitioner Survey Activation Annual measure – Patient Activation Measure (PAM) Practitioner experience and satisfaction Patient & Carer Experience of care Annual PEQ
Compendium: the website http: //p 3 c. org. uk/
Compendium: the website http: //p 3 c. org. uk/ Commissioning guidance for NHSE : Little guide: http: //p 3 c. org. uk/P 3 C_Commissioners. Guide_Navigation. pdf Medium guide: http: //p 3 c. org. uk/Commissioners_guide_med. pdf Big guide: http: //p 3 c. org. uk/P 3 C_Commissioners. Guide. pdf
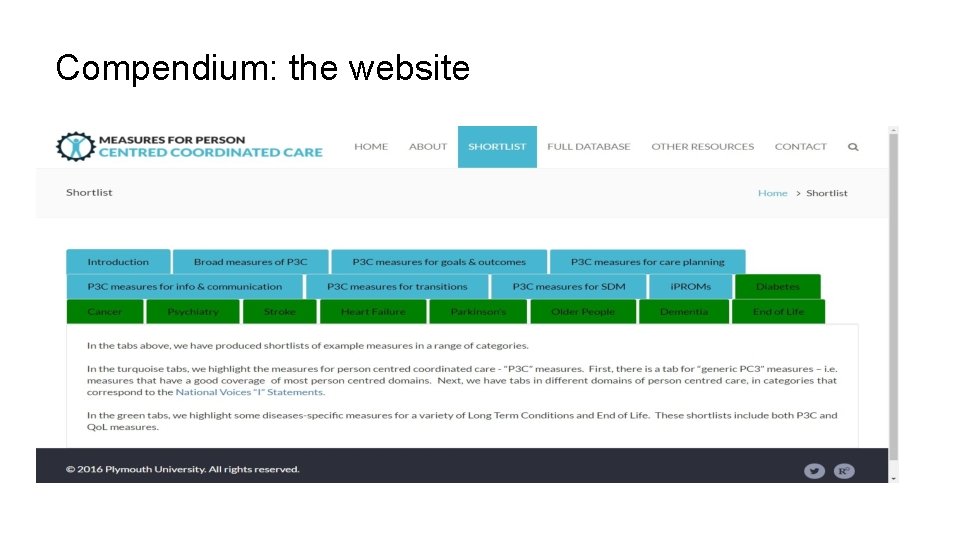
Compendium: the website

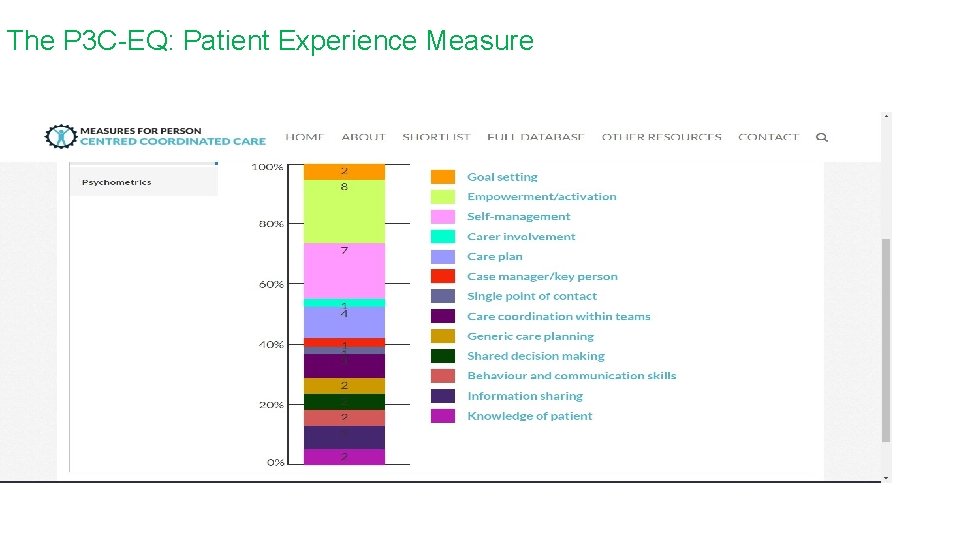
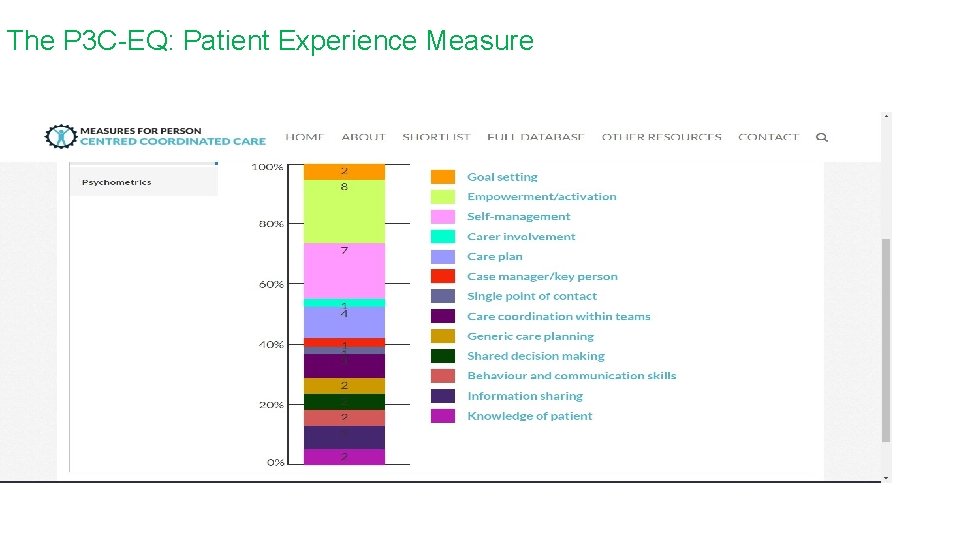
The P 3 C-EQ: Patient Experience Measure
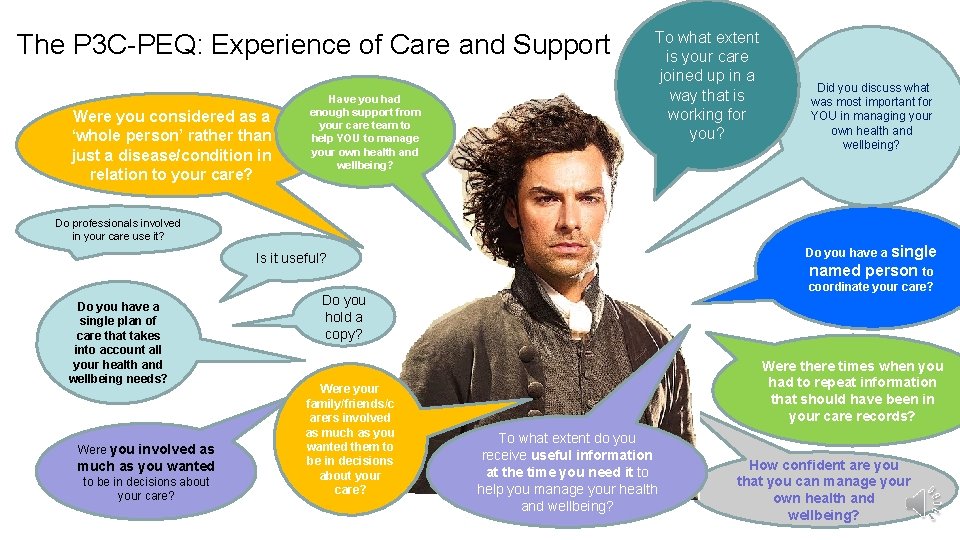
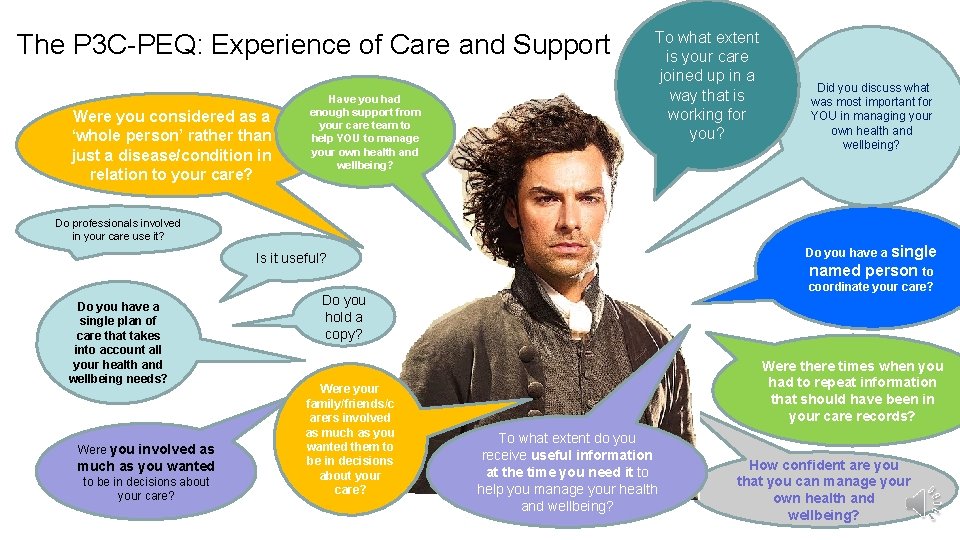
The P 3 C-PEQ: Experience of Care and Support Were you considered as a ‘whole person’ rather than just a disease/condition in relation to your care? Have you had enough support from your care team to help YOU to manage your own health and wellbeing? To what extent is your care joined up in a way that is working for you? Do professionals involved in your care use it? Do you have a single Is it useful? Do you have a single plan of care that takes into account all your health and wellbeing needs? Were you involved as much as you wanted to be in decisions about your care? named person to coordinate your care? Do you hold a copy? Were your family/friends/c arers involved as much as you wanted them to be in decisions about your care? Did you discuss what was most important for YOU in managing your own health and wellbeing? Were there times when you had to repeat information that should have been in your care records? To what extent do you receive useful information at the time you need it to help you manage your health and wellbeing? How confident are you that you can manage your own health and wellbeing?
Creating and Measuring Organisational Change The Development of the Person Centred Coordinated Care Organisational Change Tool (P 3 COCT).
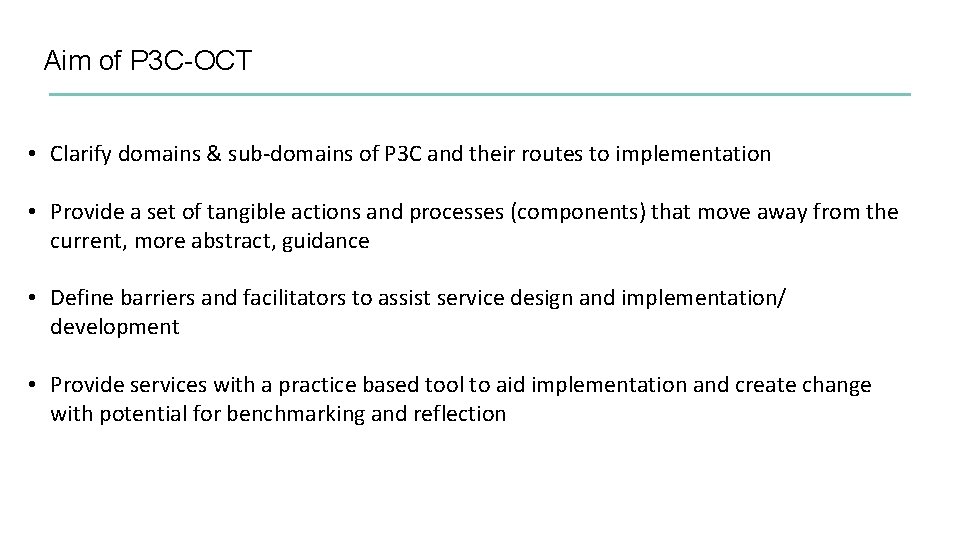
Aim of P 3 C-OCT • Clarify domains & sub-domains of P 3 C and their routes to implementation • Provide a set of tangible actions and processes (components) that move away from the current, more abstract, guidance • Define barriers and facilitators to assist service design and implementation/ development • Provide services with a practice based tool to aid implementation and create change with potential for benchmarking and reflection
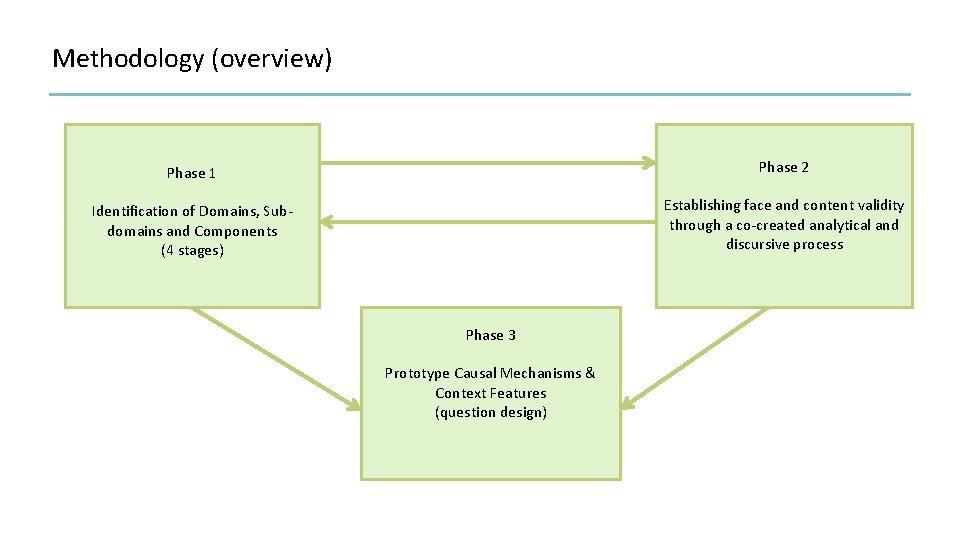
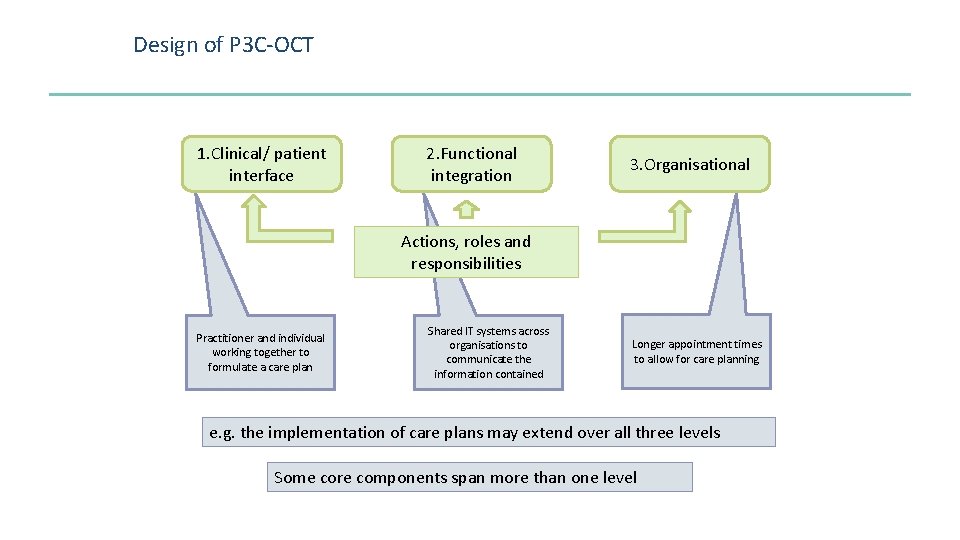
Methodology (overview) Phase 1 Phase 2 Identification of Domains, Subdomains and Components (4 stages) Establishing face and content validity through a co-created analytical and discursive process Phase 3 Prototype Causal Mechanisms & Context Features (question design)
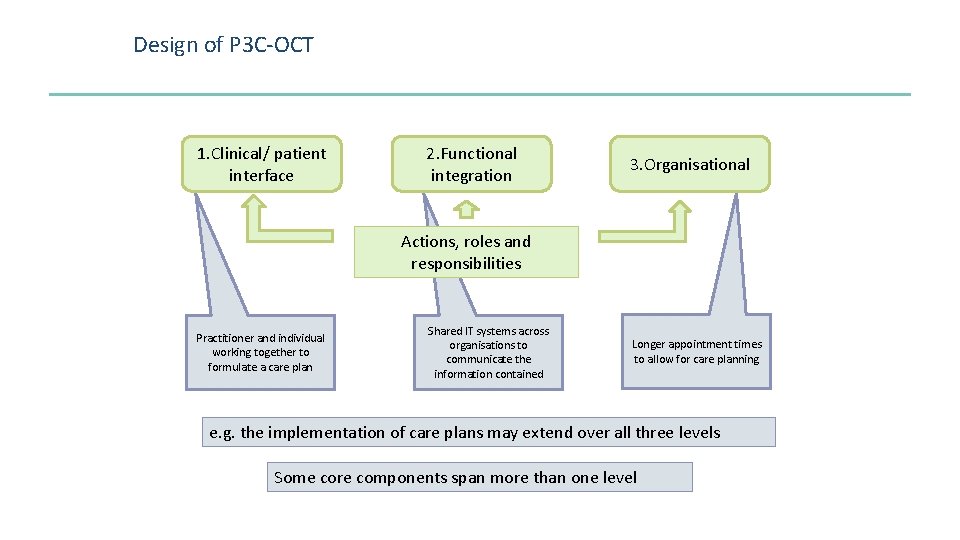
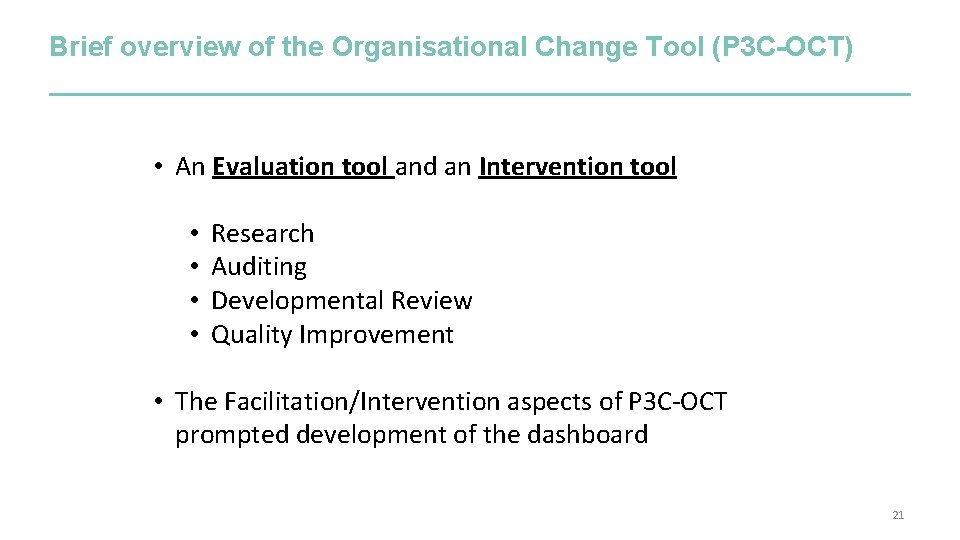
Design of P 3 C-OCT 1. Clinical/ patient interface 2. Functional integration 3. Organisational Actions, roles and responsibilities Practitioner and individual working together to formulate a care plan Shared IT systems across organisations to communicate the information contained Longer appointment times to allow for care planning e. g. the implementation of care plans may extend over all three levels Some core components span more than one level
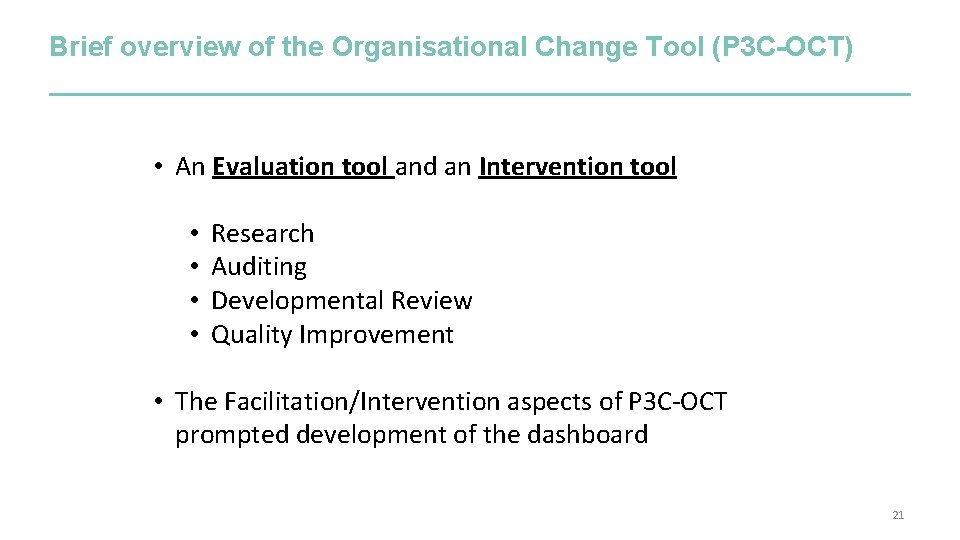
Brief overview of the Organisational Change Tool (P 3 C-OCT) • An Evaluation tool and an Intervention tool • • Research Auditing Developmental Review Quality Improvement • The Facilitation/Intervention aspects of P 3 C-OCT prompted development of the dashboard 21
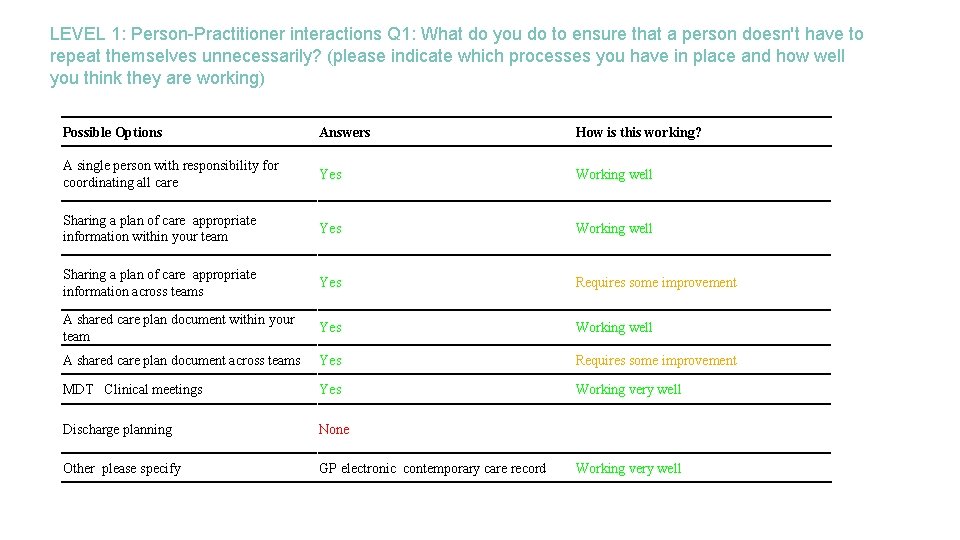
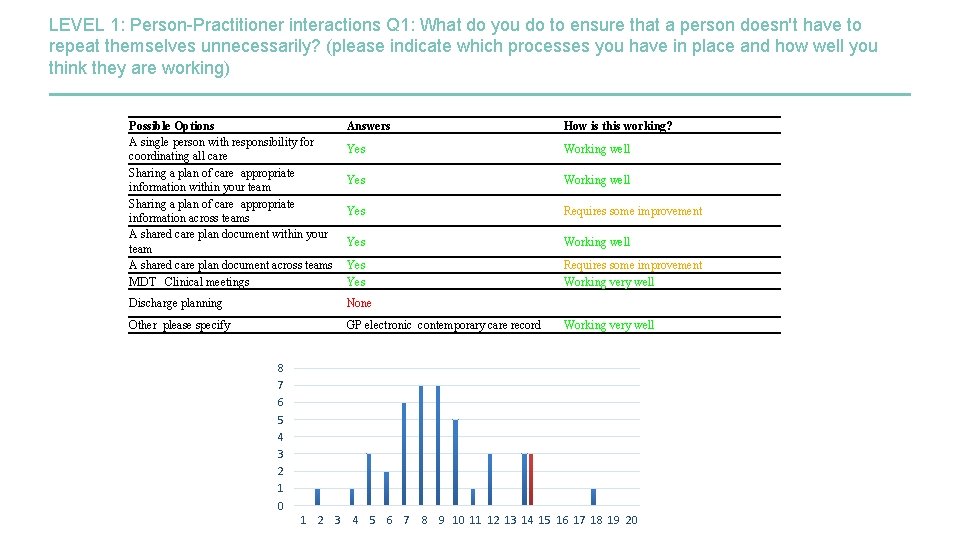
LEVEL 1: Person-Practitioner interactions Q 1: What do you do to ensure that a person doesn't have to repeat themselves unnecessarily? (please indicate which processes you have in place and how well you think they are working) Possible Options Answers How is this working? A single person with responsibility for coordinating all care Yes Working well Sharing a plan of care appropriate information within your team Yes Working well Sharing a plan of care appropriate information across teams Yes Requires some improvement A shared care plan document within your team Yes Working well A shared care plan document across teams Yes Requires some improvement MDT Clinical meetings Yes Working very well Discharge planning None Other please specify GP electronic contemporary care record Working very well
~Session Intermission~ • Ten minute break to fill out “Care Plan” questions from the P 3 C-OCT – Q 3, Q 4, Q 15, Q 29 • Please respond to the questions by following link below: – bit. ly/2 x. At. I 4 d • For a full version of the P 3 C-OCT, please see the demo version here: – bit. ly/2 hpt. GWK
OCT Scoring • There are 29 core questions on the OCT, with over 500 response codes • Scores on the P 3 C-OCT are given out of a total of 20 points • All of the 29 main questions of the OCT are weighted equally, and points are allocated equally for: • objective activities (e. g. processes being done to deliver P 3 C) • subjective responses (e. g. how well they thought these were working) • A score of 20 is theoretical maximum. Such as score is probably not attainable (or desirable), and could only be achieved with: • full P 3 C activity (as measured by the P 3 C-OCT) • all activities subjectively rated as “working very well” • A low relative score does not necessarily indicate poor performance for person centred care – instead, it will often be related to systemic factors (e. g. practice size; interoperability and governance; P 3 C solutions that are not appropriate for your organisational structure etc. ) 24
LEVEL 1: Person-Practitioner interactions Q 1: What do you do to ensure that a person doesn't have to repeat themselves unnecessarily? (please indicate which processes you have in place and how well you think they are working) Possible Options A single person with responsibility for coordinating all care Sharing a plan of care appropriate information within your team Sharing a plan of care appropriate information across teams A shared care plan document within your team A shared care plan document across teams MDT Clinical meetings Answers How is this working? Yes Working well Yes Requires some improvement Working very well Discharge planning None Other please specify GP electronic contemporary care record Working very well 8 7 6 5 4 3 2 1 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20
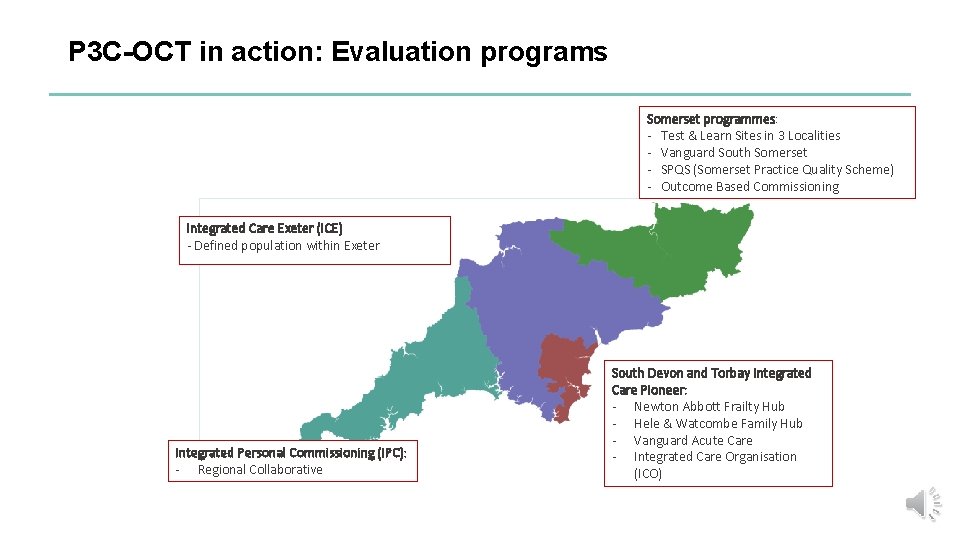
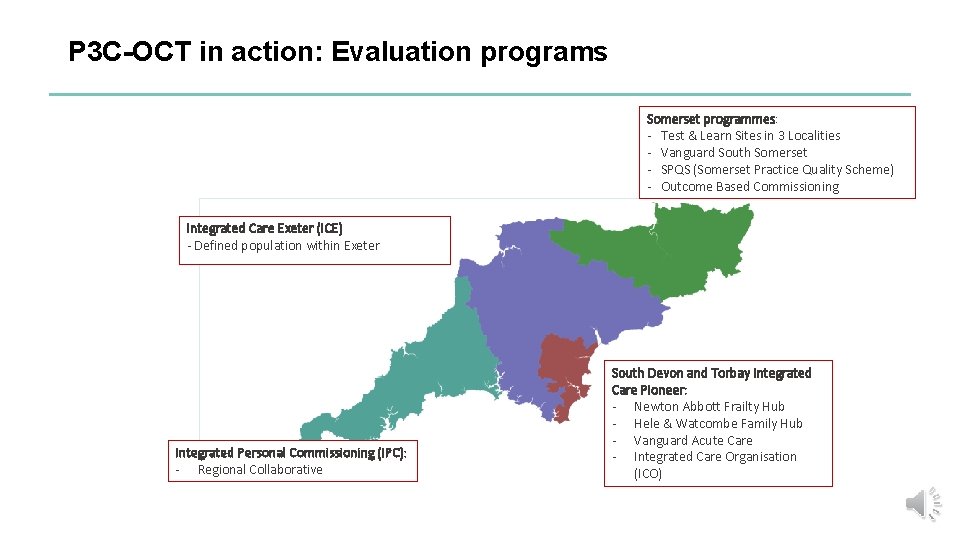
P 3 C-OCT in action: Evaluation programs Somerset programmes: - Test & Learn Sites in 3 Localities - Vanguard South Somerset - SPQS (Somerset Practice Quality Scheme) - Outcome Based Commissioning Integrated Care Exeter (ICE) - Defined population within Exeter Integrated Personal Commissioning (IPC): - Regional Collaborative South Devon and Torbay Integrated Care Pioneer: - Newton Abbott Frailty Hub - Hele & Watcombe Family Hub - Vanguard Acute Care - Integrated Care Organisation (ICO)
Introduction to Somerset Practice Quality Scheme (SPQS) • SPQS is a de-incentivisation of QOF in Somerset • SPQS arose due to criticism that QOF does not appropriately incentivise clinical care for people with complex conditions who require person centred and coordinated care • Began in June 2014, with 55 of the 75 practices in Somerset participating. • Perhaps best understood as a “system lever” to free up time/resources and allow greater involvement with schemes such as Test & Learn, Health Connections Mendip etc. 27

SPQS Phase II Evaluation • Somerset Practice Quality Scheme 28
SPQS: Methods / Our Evaluation Framework • We performed a comprehensive mixed-methods evaluation of SPQS using our consistent evaluation framework, including: Quantitative methods: • A triangulation of questionnaires: – Patient experience (P 3 C-EQ) – Practitioner perspective (P 3 C-Practitioner) – Organisational change (P 3 C-OCT) • Analysis of admissions data Qualitative methods: • Semi-structured interviews with practitioners • Observation of consultations • Facilitation workshops with practices 29
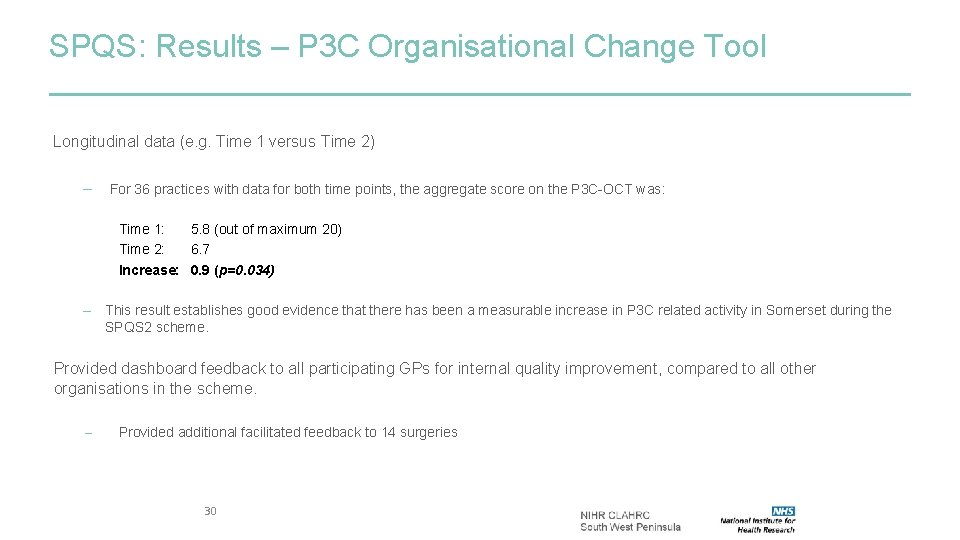
SPQS: Results – P 3 C Organisational Change Tool Longitudinal data (e. g. Time 1 versus Time 2) – For 36 practices with data for both time points, the aggregate score on the P 3 C-OCT was: Time 1: 5. 8 (out of maximum 20) Time 2: 6. 7 Increase: 0. 9 (p=0. 034) – This result establishes good evidence that there has been a measurable increase in P 3 C related activity in Somerset during the SPQS 2 scheme. Provided dashboard feedback to all participating GPs for internal quality improvement, compared to all other organisations in the scheme. – Provided additional facilitated feedback to 14 surgeries 30
Changes in P 3 C detected by the OCT in the SPQS evaluation • • Every domain of P 3 C showed improvement on P 3 C-OCT during the SPQS evaluation. Most significant improvements observed in: My Goals Decision Making Organisational Process Activities • Due to increased score in the underlying questions: – – – Q 9 b: Feedback of PAM scores into practice Q 9 a: Support tailored to ability/motivation Q 23: P 3 C training/support Q 8: Supporting social goals Q 25: Interventions to reduce hospitalisation
Summary of P 3 C-OCT • First tool of this kind • First tool that measures implementation of RCGP toolkit for personalised care and support planning • SPQS evaluation has validated P 3 C-OCT as a tool that is sensitive to organisational improvements in P 3 C, thus validating its use for: – Research – Benchmarking – Developmental review/audit for e. g. • Quality improvements • PDSA cycles make it meaningful.
Ben Fosh P 3 C-OCT Demonstration example. p 3 c. org. uk/T 1/Index. html or bit. ly/2 g. Vqgd. J Please use Google Chrome if possible!