SUPERIOR MESENTERIC ARTERY SYNDROME Dr ST Hung Princess

- Slides: 39
SUPERIOR MESENTERIC ARTERY SYNDROME Dr. ST Hung Princess Margaret Hospital
History F/73 Past Health: Metastatic CA breast ( Lung, Mediastinal LN ), on Femara® (letrozole) since 6/2012 for palliative intent Admit for repeated bilious vomiting for days • abdominal distension • BO once every 2 -3 days • Decrease intake & weight loss
Physical Examinations • Cachexic • Afebrile, BP/ P stable • Abdomen: grossly distended, succusion splash+, no mass or hernia • PR: No mass, brownish stool
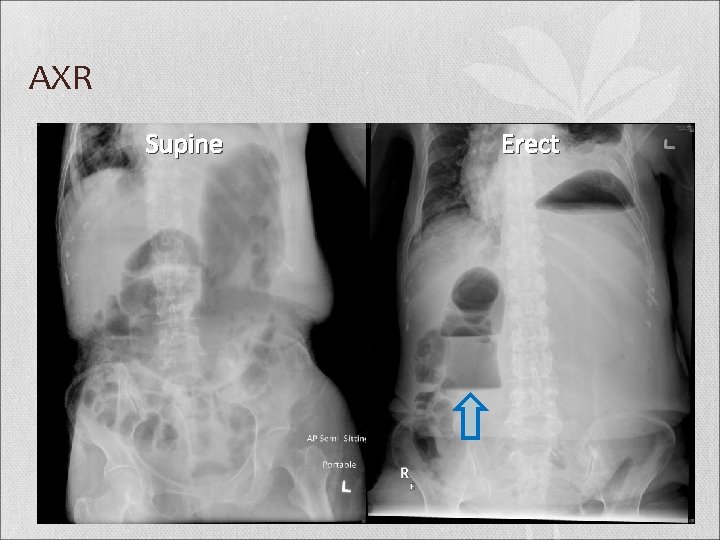
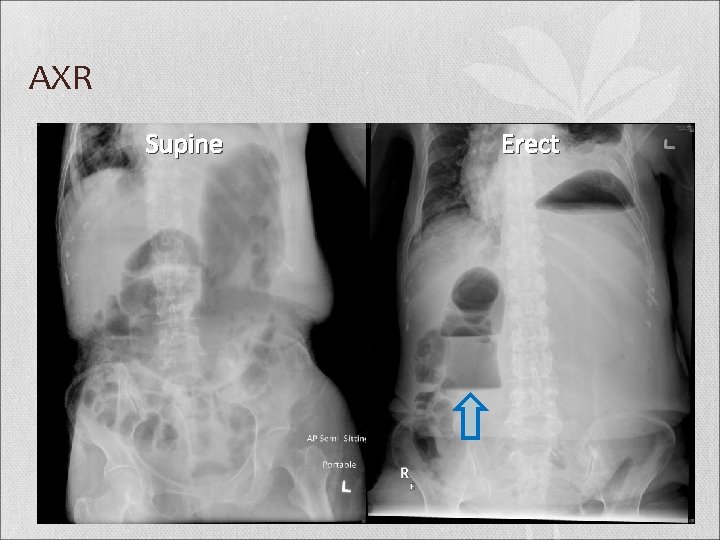
AXR Supine Erect
CT abdomen & Pelvis with Contrast

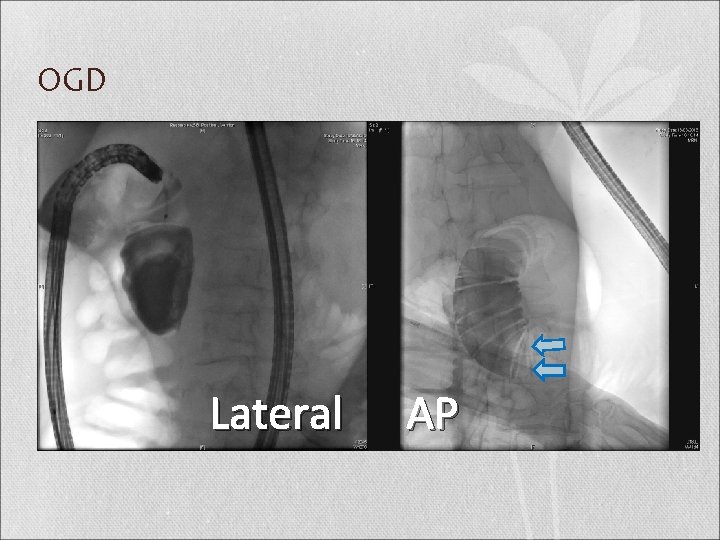
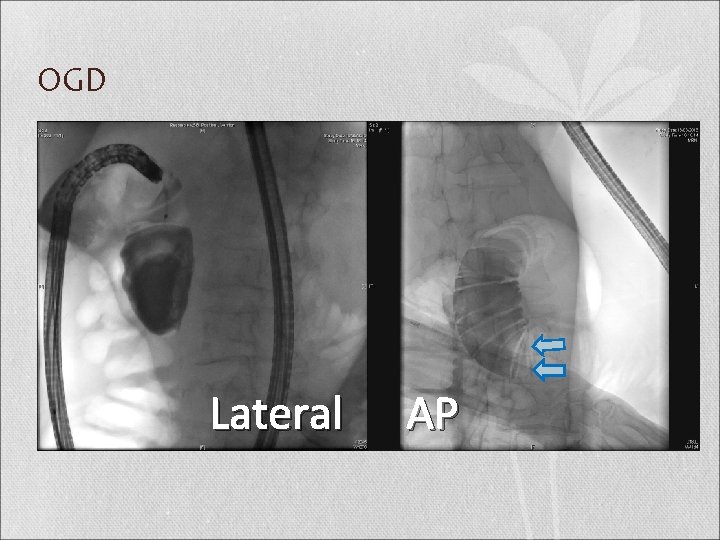
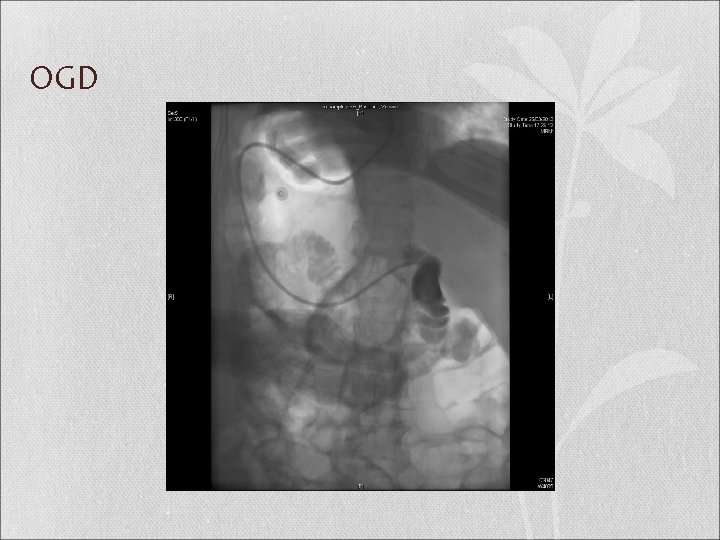
OGD Lateral AP
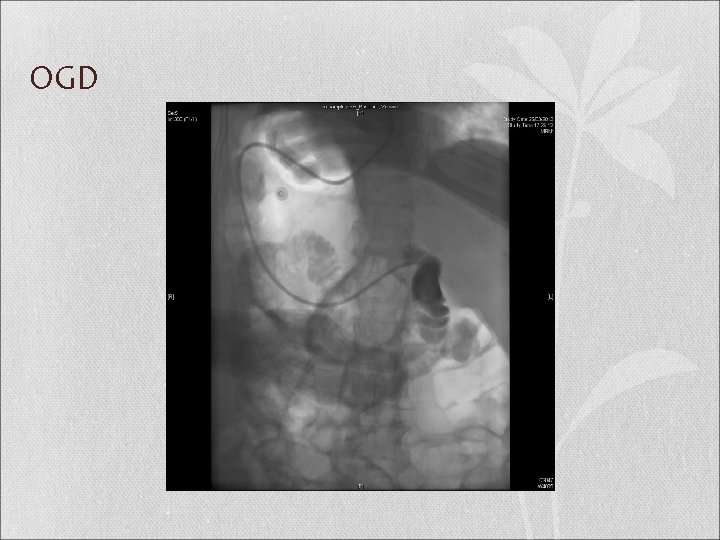
OGD
Superior Mesenteric Artery Syndrome (SMAS)
Introduction • The superior mesenteric artery syndrome is defined as vascular compression of the third part of the duodenum in the angle between the aorta and the superior mesenteric artery. • First described by Austrian Professor Carl Freiherr von Rokitansky in 1842 • Wilkie published the first comprehensive series of 75 patients, after which the eponym “Wilkie’s Syndrome” emerged • Other names: arteriomesenteric duodenal compression syndrome, chronic duodenal ileus and cast syndrome
Epidemiology • Unknown incidence; roughly estimated to be around 0. 013 to 0. 3% in general population • Females are more commonly affected, in ratio of 3: 2 • About two thirds of patients are in age group between 10 -39 • Cases described in preterm male of 23 weeks & 86 years old man • No racial difference
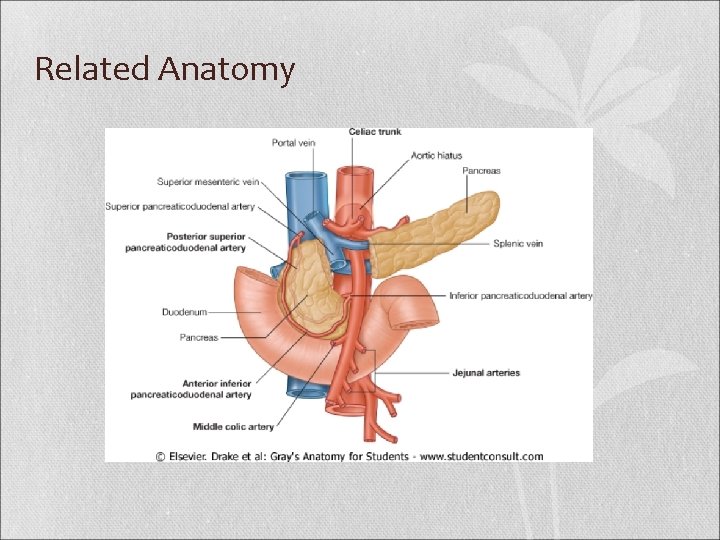
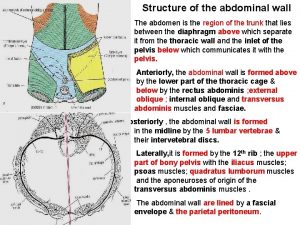
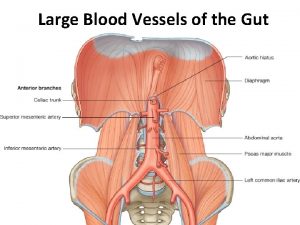
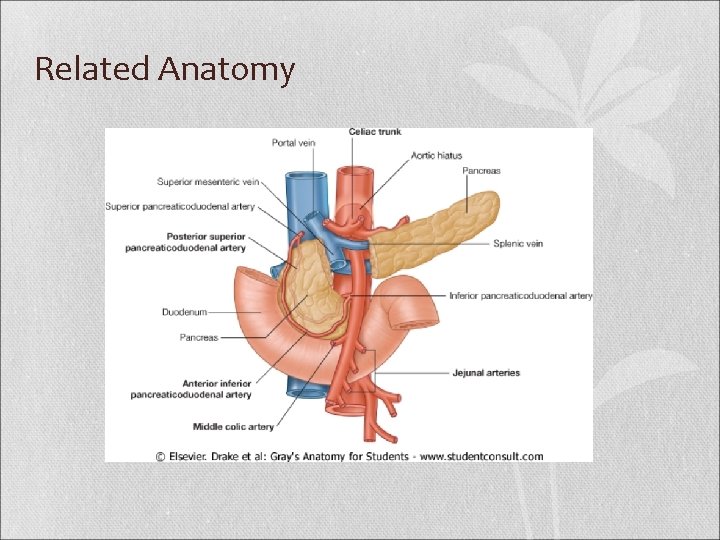
Related Anatomy
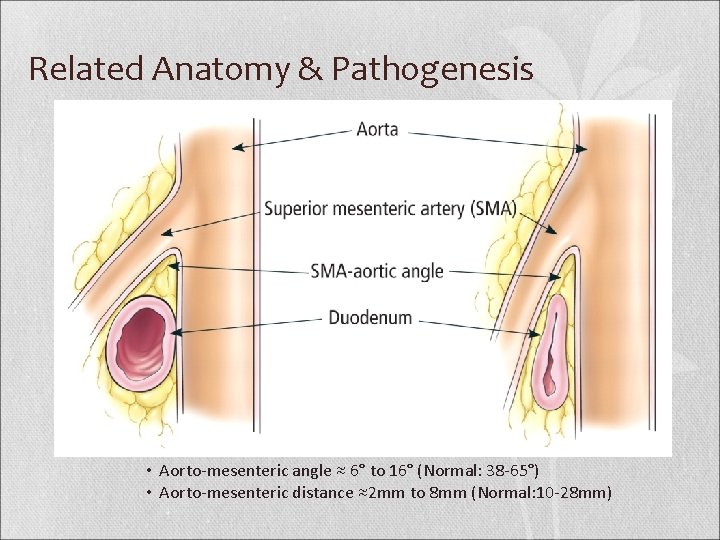
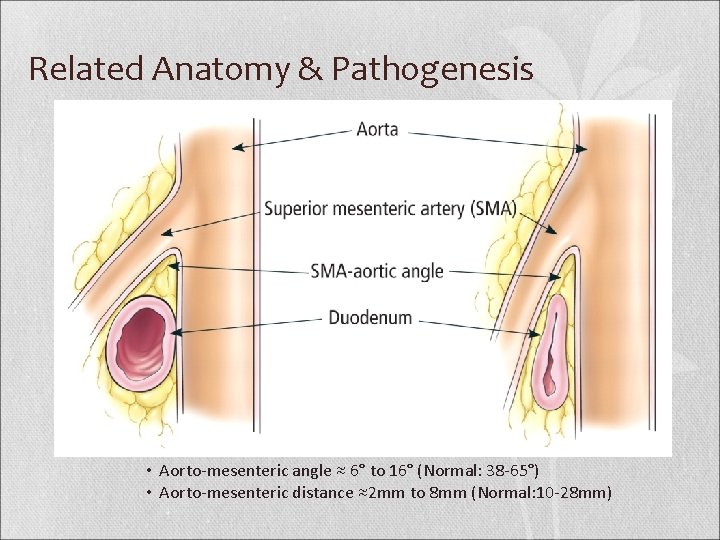
Related Anatomy & Pathogenesis • Aorto-mesenteric angle ≈ 6° to 16° (Normal: 38 -65°) • Aorto-mesenteric distance ≈2 mm to 8 mm (Normal: 10 -28 mm)
Etiology Congenital Vs Acquired
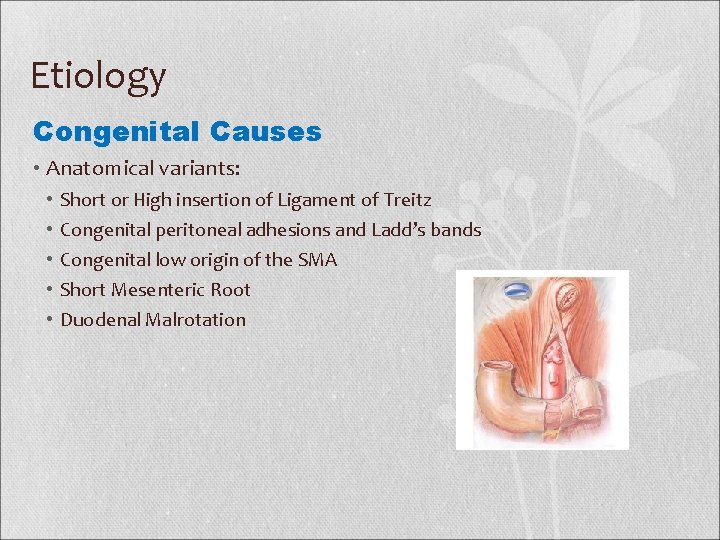
Etiology Congenital Causes • Anatomical variants: • • • Short or High insertion of Ligament of Treitz Congenital peritoneal adhesions and Ladd’s bands Congenital low origin of the SMA Short Mesenteric Root Duodenal Malrotation
Etiology Acquired Causes Chronic Wasting Disease e. g. Malignancy, paraplegia, AIDS Trauma e. g. Polytrauma, burn injury, brain and spinal cord injury Dietary Disorders e. g. Malabsorption syndrome, anorexia nervosa Postoperative States e. g. IPAA, scoliosis surgery, Cast syndrome Local pathology e. g. Neoplastic growth in mesenteric root, dissecting aortic aneurysm
Clinical Features • Depend on the cause and grade of duodenal compression • Chronic abdominal complaints with intermittent exacerbation • Rarely, rapid evolving upper intestinal ileus • Intermittent or postprandial abdominal pain (59 -81%)* followed by bilious vomiting • Epigastric pain is relieved by a prone, knee-chest, left lateral decubitus position or Hayes maneuver that all reduce small bowel mesenteric tension at aortomesenteric angle • Early satiety with a sensation of fullness, food intolerance, anorexia that trigger a vicious cycle resulting in weight loss *Ylinen P, Kinnunen J, Hockerstedt K: Superior mesenteric artery syndrome. A follow up study of 16 operated patients. J Clin Gastroenterol 1989; 11: 386– 391.
Complications Because of the frequent delay in the diagnosis of SMAS, it can result in life threatening complications* • Pancreatitis secondary to abnormal pancreaticoduodenal reflux within the closed intestinal loop • Gastroparesis is frequently encountered after correction surgery for SMAS • Esophageal tear • Peptic ulcer and perforation of stomach • Aspiration pneumonia, cardiovascular collapse, metabolic alkalosis, electrolyte imbalance *M. T. Mandarry, L. Zhao, C. Zhang, Z. Q. Wei. A comprehensive review of superior mesenteric artery syndrome. Eur Surg (2010) 42/5: 229– 236
Investigations and Diagnosis • Diagnosis is difficult and is often delayed because of incomplete obstruction and non-specific symptoms • Diagnosis by exclusion; thus requires high index of suspicious • Rosa Jimenez et al. advocated that the diagnosis should be based on clinical symptoms and radiologic evidences of obstruction* *U¨ nal B, Aktas� A, Kemal G, et al. Superior Mesenteric artery syndrome: CT and ultrasonography findings. Diagn Interv Radiol 2005; 11: 90– 5.
Investigations and Diagnosis Radiographic criteria 1. 2. 3. 4. 5. Dilatation of the 1 st and 2 nd part of the duodenum +/- gastric dilatation Abrupt vertical and oblique compression of the mucosal folds Antiperistaltic flow of contrast medium (barium) proximal to obstruction, producing to and fro movements Delay of 4 to 6 hours in gastroduodenojejunal transit time Relief of the obstruction when the patient is placed in a prone, knee-chest or left lateral positions Dietz UA, Debus ES, Heuko-Valiati L, Valiati W, Friesen A, Fuchs KH, Malafaia O, Thiede A: Aorto-mesenteric artery compression syndrome. Chirurg 2000; 71: 1345– 1351. Hines JR, Gore RM, Ballantyne GH: Superior mesenteric artery syndrome. Diagnostic criteria and therapeutic approaches. Am J Surg 1984; 148: 630– 632.
Radiographic Diagnostic Tools • Plain radiograph • Conventional barium studies • Hypotonic duodenography barium study • Computed tomography (CT) scan • Conventional angiography • 3 -Dimensional CT angiography • Magnetic resonance angiography • Ultrasonography • Endoscopy
Radiographic Diagnostic Tools Conventional barium studies • Classic diagnostic technique; cheap, easy but non-specific • A dilated proximal duodenum with an abrupt linear cut off at the 3 rd part of the duodenum and a collapsed small bowel distal to the crossing SMA • Retention of barium within the duodenum Hypotonic duodenography barium study • Duodenal peristalsis was suppressed by anti-cholinergics like propantheline bromide
Radiographic Diagnostic Tools Computed tomography (CT) scan • can clearly demonstrate the aortomesenteric angle and distance accurately • the gastric and proximal duodenal dilatation, the duodenal obstruction (site of vascular compression of the duodenum) • local pathologies e. g. aneurysm or neoplasm, etc. • Provide an overall assessment of the abdominal cavity as well as the amount of retroperitoneal fat
Radiographic Diagnostic Tools 3 -Dimensional CT & MR angiography • Most popular; rapid, non-invasive, eliminate erroneous diagnoses that originate from the angulations of SMA • Calculating the aortomesenteric angle and distance precisely • Can demonstrate the direct pressure of SMA on the entrapped duodenum Conventional angiography • Gold standard modality in the past • Invasive, time-consuming
Radiographic Diagnostic Tools Ultrasound color doppler • Advocate for detection of reduced aortomesenteric angle Upper gastrointestinal endoscopy • To rule out intraluminal obstruction and gastric or duodenal ulcer disease that might be secondary to reflux or as a primary pathology mimicking SMAS • Fluid retention in stomach, a dilated proximal duodenum, a pulsatile mass in the third part of duodenum precluding the passage of the scope • Not indicate the diagnosis
Differential Diagnosis Mechanical obstruction e. g. Pancreatic cysts or neoplasms, paraaortic lymphadenopathy, duodenumal tumor, adhesion, malrotation and Crohn’s disease Familial neuropathic disease e. g. megaduodenum Postoperative paralytic ileus e. g. general anesthesia, analgesic, electrolyte imbalance or greater splanchnic nerve injury during anterior spinal Recurrent biliary pancreatitis Gastroparesis in Type I Diabetes Psychogenic vomiting Rare causes with decreased peristalsis e. g. dermatomyositis, SLE, myxoedema, amyloidosis, myotonic dystrophy or chronic idiopathic intestinal pseudo-obstruction
Treatment • Medical Treatment to Surgical Treatment
Medical Treatment • In absence of displacement by an abdominal mass, an aneurysm or another pathologic condition that requires immediate surgical exploration, the treatment of the SMAS usually begins with conservative approaches • Aim: Reversal of weight loss; promote the restoration of retroperitoneal fat tissue which consequently increases the aortomesenteric angle* *Jawad NH, Al-Sanae A, Al-Qabandi W. Superior mesenteric artery syndrome: An uncommon cause of intestinal obstruction; report of two cases and review of literature. Kuwait Med J 2006; 38: 241– 4.
Medical Treatment • Nil by mouth • Nasogastric tube with regular aspiration • Correction of fluid and electrolyte balance • Enteral jejunal tube feeding, parental nutrition • Posturing maneuvers • Prokinetic drugs like metoclopramide or cisapride may be used to enhance stomach emptying by improving motility
Medical Treatment • No clear time limit for medical treatment • Relief of symptoms has been observed from 2 to 12 days; nevertheless, it has been also reported up to 169 days* and even up to 7 months in different cases *Lee CS, Mangla JC: Superior mesenteric artery compression syndrome. Am J Gastroenterol 1978; 70: 141– 150.
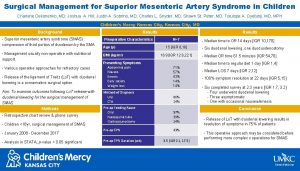
Surgical Treatment Indications for surgical intervention (Berner and Sherman, 1963) are: • Failed conservative treatment • Longstanding disease with progressive weight loss and duodenal dilatation with stasis • Complicated peptic ulcer disease and pancreatitis secondary to biliary stasis and reflux • Local pathology requiring laparotomy • Patients’ preference
Surgical Procedures • Duodenojejunostomy • Gastrojejunostomy • Strong’s operation • Laparoscopic duodenojejunostomy • Robotic assisted intestinal bypass surgery • Anterior transposition of the third part of duodenum • Transposition of the SMA to the infrarenal aorta • Duodenal circular drainage
Surgical Procedure Strong’s procedure • Mobilization of the duodenum by division of the ligament of Trietz, allowing the duodenum to fall away from the aorta • Avoids anastomosis thus, is less invasive, quicker, safer procedure, and with early postoperative recovery • Failure rate of 25%* presumably due to • • Short branches of the inferior pancreaticoduodenal artery not permitting the duodenum to fall inferiorly Adhesion resulting in difficult dissection *Lee CS, Mangla JC: Superior mesenteric artery compression syndrome. Am J Gastroenterol 1978; 70: 141– 150.
Surgical Procedure Gastrojejunostomy • Adequate gastric decompression • Fail to completely release duodenal obstruction leading to persistence of symptoms that necessitated duodenojejunostomy in some cases* • Persisting obstruction may lead to blind loop syndrome, gastric bile reflux and ulceration** *Lee CS, Mangla JC: Superior mesenteric artery compression syndrome. Am J Gastroenterol 1978; 70: 141– 150. **Geer MA. Superior mesenteric artery syndrome. Mil Med 1990; 155: 321– 323
Surgical Procedure Duodenojejunostomy • Was first performed by Stavely in 1910 • The most frequent surgical procedure with a success rate of about 90% * • Lee and Mangla * concluded after reviewing 146 cases operated after 1963 that duodenojejunostomy revealed the best results in severe cases and was significantly better compared to gastrojejunostomy and Strong’s procedure *Lee CS, Mangla JC: Superior mesenteric artery compression syndrome. Am J Gastroenterol 1978; 70: 141– 150.
Surgical Procedure Laparoscopic duodenojejunostomy • Gersin and Heniford reported the first successful laparoscopic duodenojejunostomy case in 1998 • Small series have reported success rates of 75 -100% with laparoscopic division of the ligament of Treitz or laparoscopic duodenojejunostomy using a retrocolic stapled anastomosis.
Surgical Procedure Others • World’s first robotically assisted intestinal bypass surgery for SMAS: was reported in July 2008 at London Health Services Centre • Anterior transposition of the third part of duodenum • Billroth II gastrectomy • Transposition of the SMA to the infrarenal aorta • Duodenal circular drainage
Conclusion • SMAS is a very rare entity which has been associated with a wide range of predisposing factors, presenting with features of upper GIT obstruction and a recent abrupt weight loss. • An early recognition of the condition, institution of the appropriate conservative measures and proper timely selection of a definite surgical method are critical to prevent the development of severe complications. M. T. Mandarry et al. A comprehensive review of superior mesenteric artery syndrome. Eur Surg (2010) 42/5: 229– 236
Thank You
 Superior mesenteric artery origin
Superior mesenteric artery origin Upper mesenteric artery
Upper mesenteric artery Inferior mesenteric artery
Inferior mesenteric artery Superior epigastric artery
Superior epigastric artery Pyramidal lobe
Pyramidal lobe Internal vs external intercostal muscles
Internal vs external intercostal muscles Inferior pancreaticoduodenal artery
Inferior pancreaticoduodenal artery Cruciate anastomosis of thigh
Cruciate anastomosis of thigh Deep artery of the arm
Deep artery of the arm Diverticulosis
Diverticulosis Mesenteric angiogram
Mesenteric angiogram Gastric ligaments
Gastric ligaments The radial and ulnar veins merge to form the
The radial and ulnar veins merge to form the Mesenteric arteriogram
Mesenteric arteriogram Hepatorenal recess
Hepatorenal recess Iliac nodes
Iliac nodes Hopital avicenne
Hopital avicenne Supracolic compartment organs
Supracolic compartment organs Causes of superior vena cava syndrome
Causes of superior vena cava syndrome Superior canal dehiscence syndrome symptoms
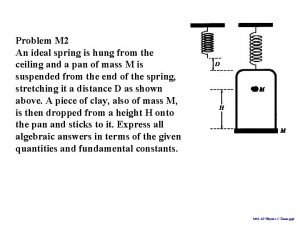
Superior canal dehiscence syndrome symptoms A spring is hung from the ceiling
A spring is hung from the ceiling Hung yi lee
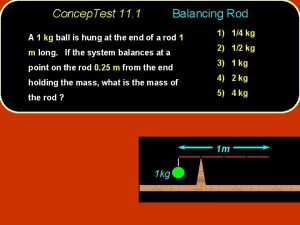
Hung yi lee When two objects of unequal mass are hung vertically
When two objects of unequal mass are hung vertically Patellar reflex definition
Patellar reflex definition Hungyi lee
Hungyi lee A loose spiral spring is hung from the ceiling
A loose spiral spring is hung from the ceiling Tranh đền hùng
Tranh đền hùng Anh hùng lấy thân làm giá súng
Anh hùng lấy thân làm giá súng Whats a hung jury
Whats a hung jury Hãy kể những điều em biết về các vua hùng
Hãy kể những điều em biết về các vua hùng Vua hùng
Vua hùng Samantha hung
Samantha hung Phùng hưng
Phùng hưng Substantv
Substantv John tyndall fiber optics
John tyndall fiber optics Hung bui
Hung bui Felling a hung up tree
Felling a hung up tree Hung yi lee
Hung yi lee Hungyi lee
Hungyi lee Up hair hush ooze
Up hair hush ooze