STI diagnosis treatment Dr Jolle Turner Consultant in



- Slides: 28
STI diagnosis & treatment Dr Joëlle Turner Consultant in Sexual Health Luton Sexual Health 27 th February 2018
Overall objectives of session • Look at examples of presentations of STIs • How to assess a patient with a possible STI – history taking and examination • Testing for STIs • Consider differential diagnoses and appropriate referral • Treatment and follow up • Partner notification
Case 1 • 17 yr old female presents with intermenstrual bleeding • On COC pill – previously regular withdrawal bleed only • No discharge/dysuria/abdominal pain • No dyspareunia or postcoital bleeding • New boyfriend of 2 months, age 18
Differential diagnosis? • Breakthrough bleeding • Cervical ectopy or other pathology • STI • Examination: • Normal vulva and vagina, no discharge seen • Cervix – small area of ectopy, contact bleeding
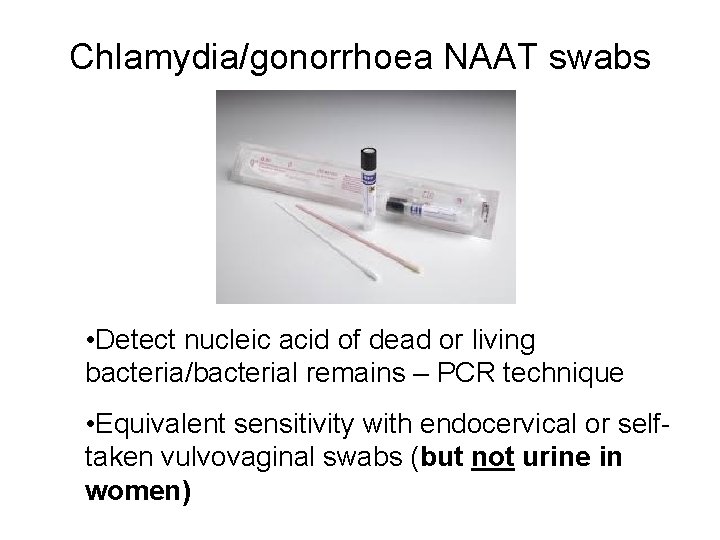
Chlamydia/gonorrhoea NAAT swabs • Detect nucleic acid of dead or living bacteria/bacterial remains – PCR technique • Equivalent sensitivity with endocervical or selftaken vulvovaginal swabs (but not urine in women)
Chlamydia NAAT positive • Treatment options: – Doxycycline 100 mg bd x 7 days (preferred if no pregnancy risk or other contraindication) – Azithromycin 1 g stat po • Other advice: – No sex (with or without condom, inc. oral/anal) until 7 days after treatment completion • Partner notification: – Recommend test & treat all partners from last 6 months – no sex until 7 days after treatment
Case 2 • 22 yr old man • Presents with right testicular pain and swelling – noted 3 hours ago on waking, gradually worsening • Moderate pain • Intermittent dysuria for 2 weeks
History • • No urethral discharge or recent diarrhoea No recent travel No previous UTI or catheterisation No associated abdo pain/N+V No recent trauma No PMHx, no medications Sexual history – 3 casual female partners in last 3 months – all unprotected vaginal and oral sex
Differential diagnosis? • • • Torsion Epididymo-orchitis Testicular mass Hydrocele Testicular infarction or rupture Scrotal cellulitis/Fournier’s gangrene

Examination findings • Right scrotum swollen and red • Right testicular and epididymal swelling and tenderness • Normal lie of testis • No urethral discharge • Abdomen soft, non tender
Investigations and referral • Urine dipstick + MSU • Urine for chlamydia and gonorrhoea NAAT test – First void urine – Plain (white top) bottle or NAAT tube – Virology form • Tests before treatment! • Offer blood test for HIV/syphilis • If any suspicion of torsion urgent urology review. • If no suspicion of torsion/torsion ruled out start Abx
Treatment • STI most likely if age <35 and no other features – Treat with doxycycline 100 mg bd x 14 days – if GC suspected (frank pus discharge, contact of GC) needs ceftriaxone 500 mg IM stat also • If UTI/enteric pathogen suspected – e. g. dipstick +ve, recent diarrhoea, previous UTI/catheter, age >35 – Ciprofloxacin 500 mg bd for 10 -14 days – Ofloxacin 200 -400 mg bd for 10 -14 days
Other advice • Scrotal support – folded up towel, briefs>boxers • Ice and analgesia • No sex until a week after abx complete • Partner notification – treat partner if STI suspected. • Follow up at 2 -3 weeks if sx persist
Case 3 • 26 yr old woman • Presents with 10 day history of pelvic pain and vaginal bleeding • Cramping pain, constant • Intermenstrual bleeding and post coital bleeding for last month. • Now heavy constant bleeding for 3 days
History • • Yellow PV discharge with odour No dysuria/frequency No bowel changes/N+V Deep dyspareunia for last 6 weeks • No previous medical history, no medications • LMP 5/52 ago, not using any contraception, last sexual intercourse 3/52 ago • Regular partner for last 6 months
Differential diagnosis? • • • Ectopic pregnancy Early miscarriage Appendicitis Pelvic inflammatory disease (PID) Ovarian cyst rupture Endometriosis
Examination findings • • Vulva NAD Vagina – thin white/yellow discharge Cervix – inflamed, mucoid discharge Bimanual – bilateral adnexal tenderness but no masses, mild cervical motion tenderness • Abdomen soft, no rebound/guarding, mild lower abdominal tenderness L>R

Tests • • Pregnancy test – negative Urine dip – trace leucocytes only Blood test for HIV/syphilis NAAT swab for chlamydia/gonorrhoea/TV (or charcoal swab for TV) – High vaginal – Self-taken vulvovaginal
Pathogens linked to PID • • Chlamydia & gonorrhoea BV-associated bacteria Other STIs e. g. mycoplasma genitalium Other non–STIs • STI detected in <one third of cases • ‘Translocation’ of vaginal bacteria
Treatment • Standard treatment for PID is with combination Abx: • Doxycycline 100 mg bd x 2/52 (consider alternative if risk of pregnancy) plus • Metronidazole 400 mg bd x 10 -14 days • +/- Ceftriaxone IM 500 mg stat if gonorrhoea suspected • No sex during treatment
Follow up • If complicated/severe PID suspected refer to sexual health same or next day • Ensure partner notification commenced • Important to do tests before antibiotics commenced • If fever/systemically unwell consider gynae admission for iv Abx and USS ? tubo-ovarian abscess • Review at 2 -3 weeks – Check completed abx – Repeat pregnancy test, review swab results – Check if sx/signs resolved – Ensure has abstained from sex and partner screened and treated • If signs and sx persist proceed to USS
Case 3 • 52 yr old woman • Presents with 3 day history of fever, swollen glands, myalgia • Also reports dysuria, difficulty passing urine and vulval soreness • Yellowish vaginal discharge • No pelvic pain, no bleeding (post menopausal) • Last sex 4 years ago • Oral intercourse with new partner – 1 week ago
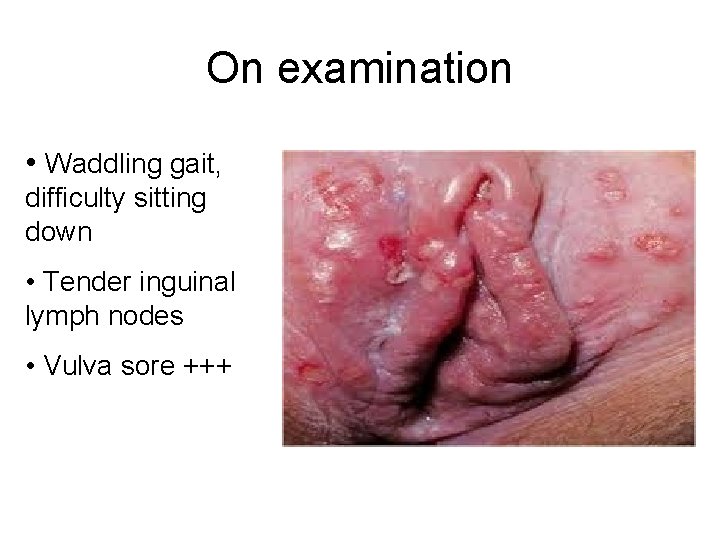
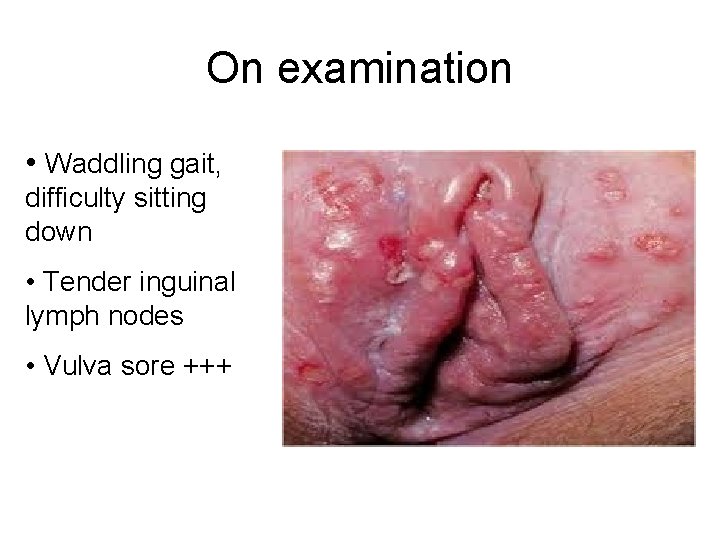
On examination • Waddling gait, difficulty sitting down • Tender inguinal lymph nodes • Vulva sore +++
Tests • Urine dip • Ensure can pass urine • Swab for HSV PCR • Blood test for HIV/syphilis • Do not attempt vaginal swabs or speculum examination – too painful
Treatment and referral • Start aciclovir 200 mg 5 x/day or 400 mg tds x 5/7 • Admission for catheterisation if urinary retention • Give topical lidocaine cream/gel (instillagel if nothing else available) for symptomatic relief • Advise analgesia, salt water bathing, pee in bath • Refer to sexual health esp. if no access to swab testing for confirmation of diagnosis, symptoms severe or not settling or if diagnosis unclear • If frequent recurrences can provide suppresiive treatment – Aciclovir 400 mg bd for 6 -12 months
Follow up • Review if not improving • Otherwise review after ulcers healed – Perform rest of STI screen (swabs/bloods) – Review swab results – Counsel about HSV – Advise about transmission to partners – Refer to Herpes Viruses Association for advice www. hva. org. uk

Luton Sexual Health opening hours • • Monday 9. 00 – 18. 30 Tuesday 9. 00 – 17. 30 Wednesday 9. 00 – 18. 30 Thursday 9. 00 – 18. 30 Friday 9. 00 – 13. 00 Saturday 9. 00 – 15. 00 Walk in clinics daily • Contact us if any advice needed • See www. lutonsexualhealth. org. uk
Resources • British Association for Sexual Health and HIV – www. bashh. org/guidelines • British HIV Association – www. bhiva. org/guidelines
 What is the nursing process
What is the nursing process Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Nursing diagnosis three parts
Nursing diagnosis three parts Nursing process and critical thinking
Nursing process and critical thinking Oral diagnosis and treatment planning ppt
Oral diagnosis and treatment planning ppt Charting identification chapter 28
Charting identification chapter 28 House palate classification
House palate classification Endodontic diagnosis and treatment planning
Endodontic diagnosis and treatment planning Sti
Sti Std
Std Dit-tik.upi.edu.akun
Dit-tik.upi.edu.akun Icares sti
Icares sti Greek and latin roots quiz
Greek and latin roots quiz Hycode sti
Hycode sti Sexual health adviser
Sexual health adviser Std vs sti
Std vs sti Dca to sti
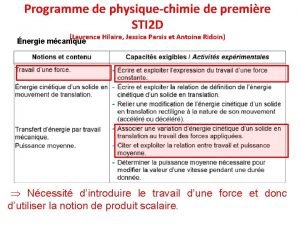
Dca to sti Programme première sti2d physique-chimie
Programme première sti2d physique-chimie Rails sti vs polymorphic
Rails sti vs polymorphic Peran manajer sti
Peran manajer sti Diomed biyoteknoloji san.tic.ltd.şti
Diomed biyoteknoloji san.tic.ltd.şti Dr swastika
Dr swastika Sti stands for
Sti stands for Pemti
Pemti Peran manajer sti
Peran manajer sti Sti university moscow
Sti university moscow I sti
I sti 17 year old penis
17 year old penis