Social Insurance updated Allen C Goodman 2013 Social














- Slides: 43
Social Insurance …updated © Allen C. Goodman, 2013

Social Insurance • Started in Germany, in 1880 s. • Originally employment-related. • United States was dragged in kicking and screaming with the Social Security Act of 1935. • Medicare and Medicaid were established in 1965.
Particularly good places for data • Center for Medicare and Medicaid Services • Kaiser Family Foundation • They update all of the data in this chapter faster than I can.
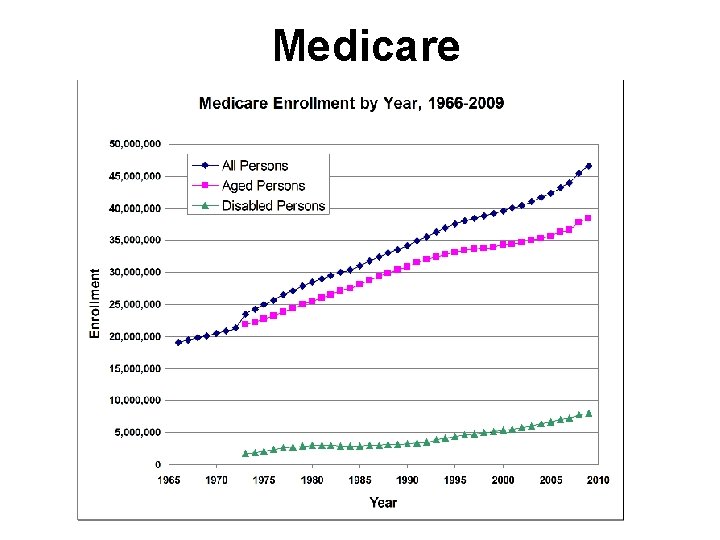
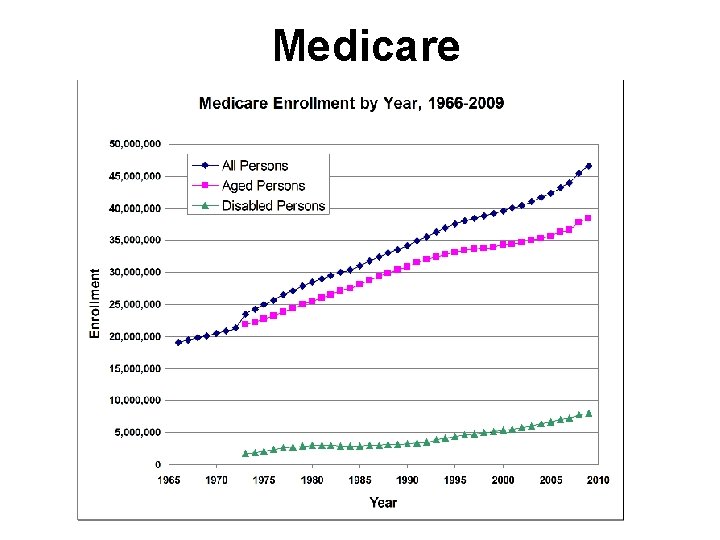
Medicare

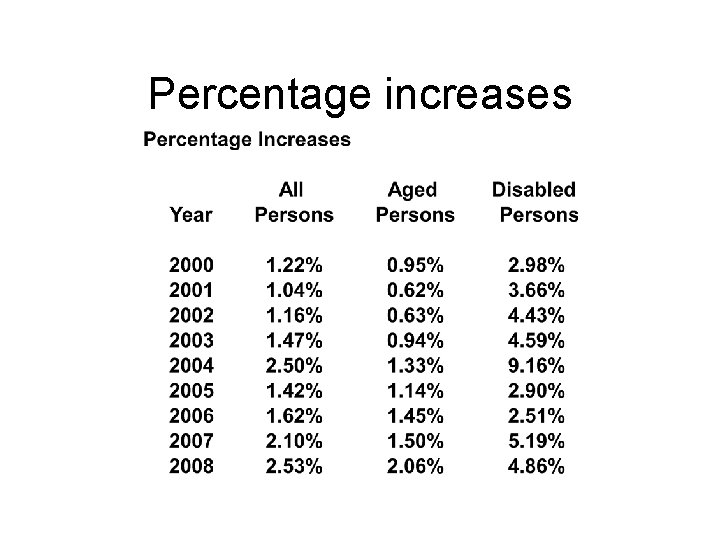
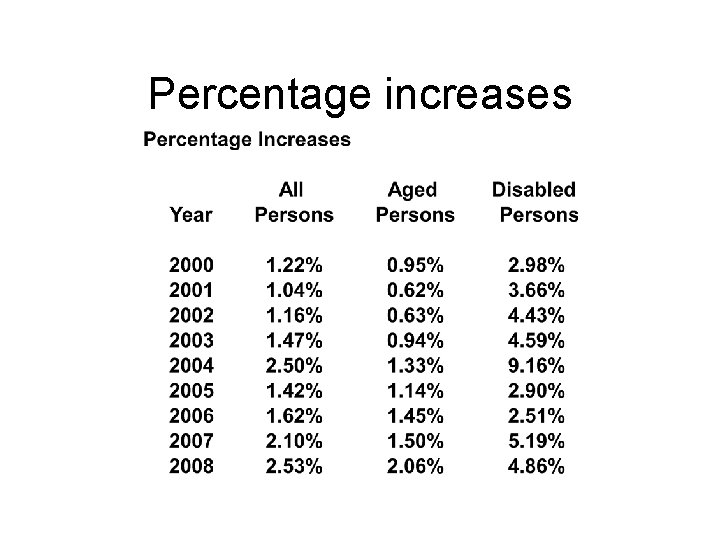
Percentage increases
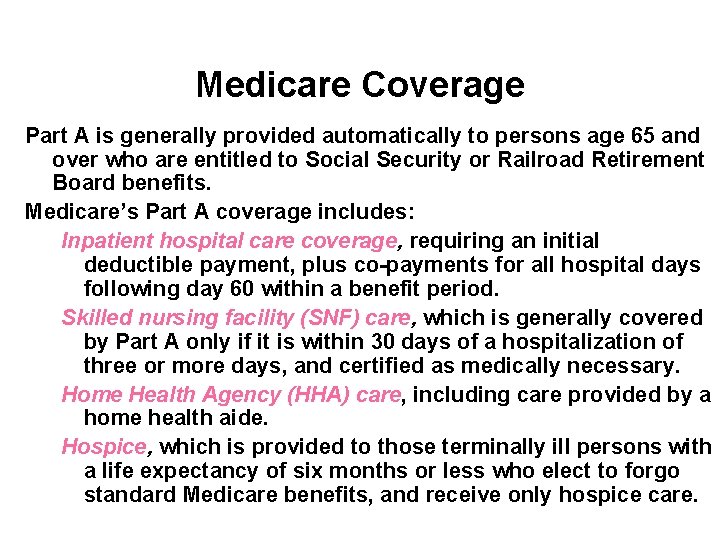
Medicare Coverage Part A is generally provided automatically to persons age 65 and over who are entitled to Social Security or Railroad Retirement Board benefits. Medicare’s Part A coverage includes: Inpatient hospital care coverage, requiring an initial deductible payment, plus co-payments for all hospital days following day 60 within a benefit period. Skilled nursing facility (SNF) care, which is generally covered by Part A only if it is within 30 days of a hospitalization of three or more days, and certified as medically necessary. Home Health Agency (HHA) care, including care provided by a home health aide. Hospice, which is provided to those terminally ill persons with a life expectancy of six months or less who elect to forgo standard Medicare benefits, and receive only hospice care.
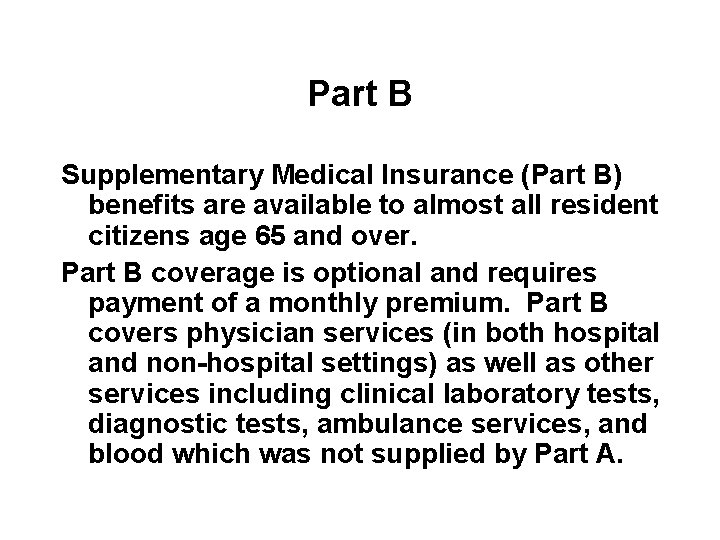
Part B Supplementary Medical Insurance (Part B) benefits are available to almost all resident citizens age 65 and over. Part B coverage is optional and requires payment of a monthly premium. Part B covers physician services (in both hospital and non-hospital settings) as well as other services including clinical laboratory tests, diagnostic tests, ambulance services, and blood which was not supplied by Part A.

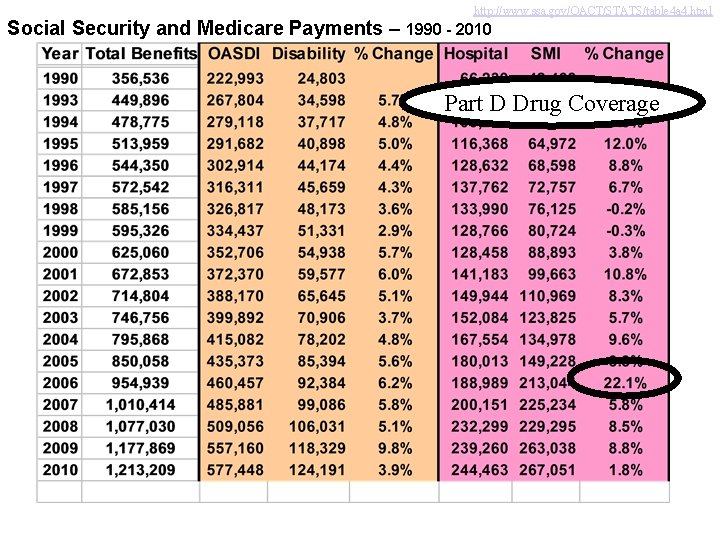
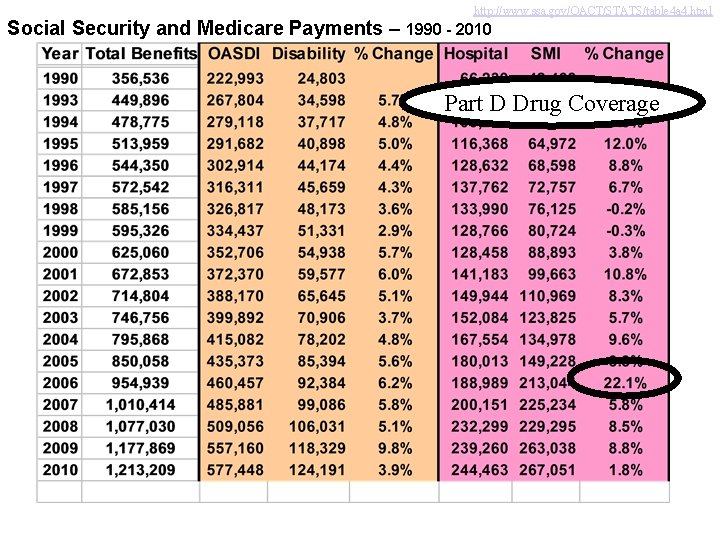
http: //www. ssa. gov/OACT/STATS/table 4 a 4. html Social Security and Medicare Payments – 1990 - 2010 Part D Drug Coverage

Program Financing The Medicare Part A program is financed primarily through a mandatory payroll deduction (FICA tax). The FICA tax is 1. 45% of earnings (paid by each employee and by the employer for each), as well as 2. 90% for self-employed persons. This tax is paid on all covered wages and self-employment income without limit.
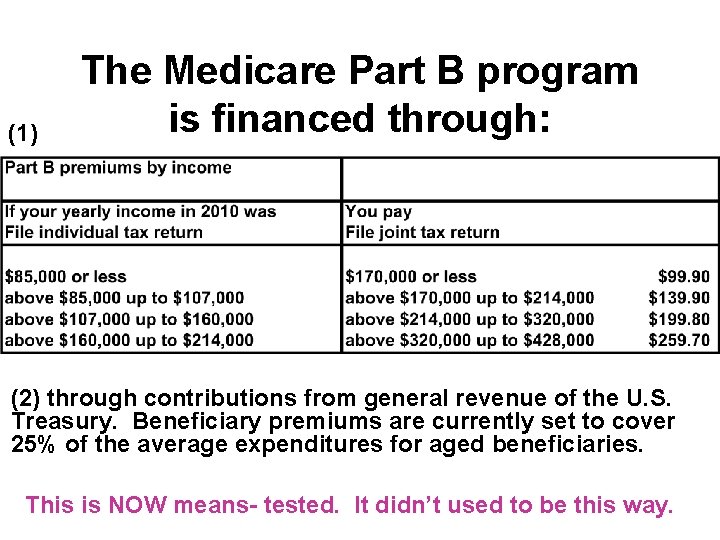
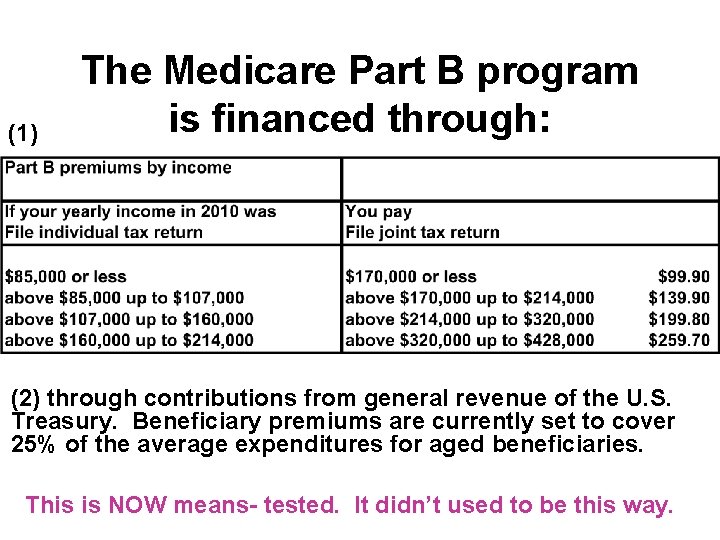
(1) The Medicare Part B program is financed through: (2) through contributions from general revenue of the U. S. Treasury. Beneficiary premiums are currently set to cover 25% of the average expenditures for aged beneficiaries. This is NOW means- tested. It didn’t used to be this way.
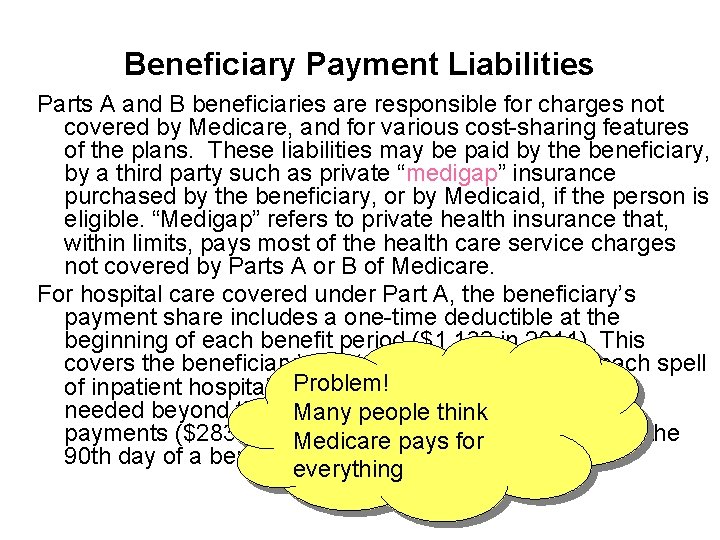
Beneficiary Payment Liabilities Parts A and B beneficiaries are responsible for charges not covered by Medicare, and for various cost-sharing features of the plans. These liabilities may be paid by the beneficiary, by a third party such as private “medigap” insurance purchased by the beneficiary, or by Medicaid, if the person is eligible. “Medigap” refers to private health insurance that, within limits, pays most of the health care service charges not covered by Parts A or B of Medicare. For hospital care covered under Part A, the beneficiary’s payment share includes a one-time deductible at the beginning of each benefit period ($1, 132 in 2011). This covers the beneficiary’s part of the first 60 days of each spell Problem! of inpatient hospital care. If continued inpatient care is needed beyond the 60 Many days, people additional thinkcoinsurance payments ($283 per day in 2011) arefor required through the Medicare pays 90 th day of a benefit period. everything
Beneficiary Payment Liabilities For Part B, the beneficiary’s payment share includes one annual deductible (in 2011, $162); the monthly premiums; the coinsurance payments for Part B services (usually 20% of the medically allowed charges); a deductible for blood; and payment for any services which are not covered by Medicare. For end-stage renal disease (ESRD) patients, Medicare Part B covers kidney dialysis and physician charges incurred by the patient and donor during the transplant and follow-up care.

Medicaid Overview Medicaid, referring to Title XIX of the Social Security Act, is a federal-state matching entitlement program that pays for medical assistance for certain vulnerable and needy individuals and families with low incomes and resources. This program is the largest source of funding for medical and health-related services for America’s poorest people. In 2007, it provided health care assistance to more than 50. 1 million persons on average, with a total of 62. 9 million people enrolled for at least one month. Total expenditures (including CHIP) for fiscal year 2009 were $380. 6 billion.
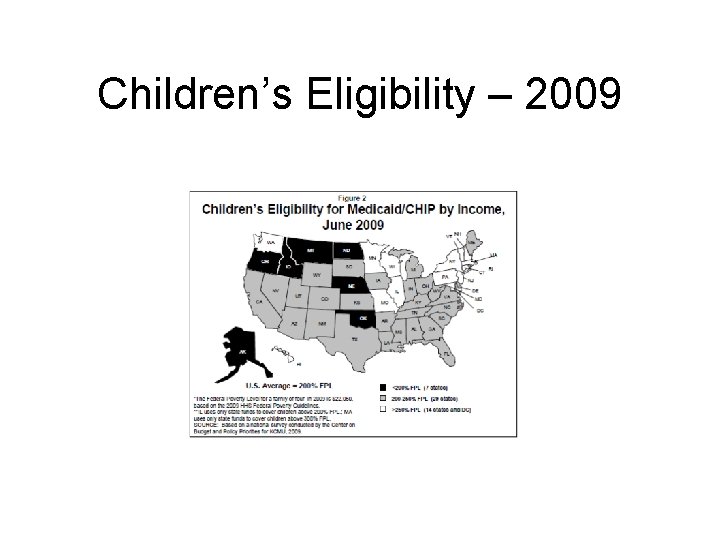
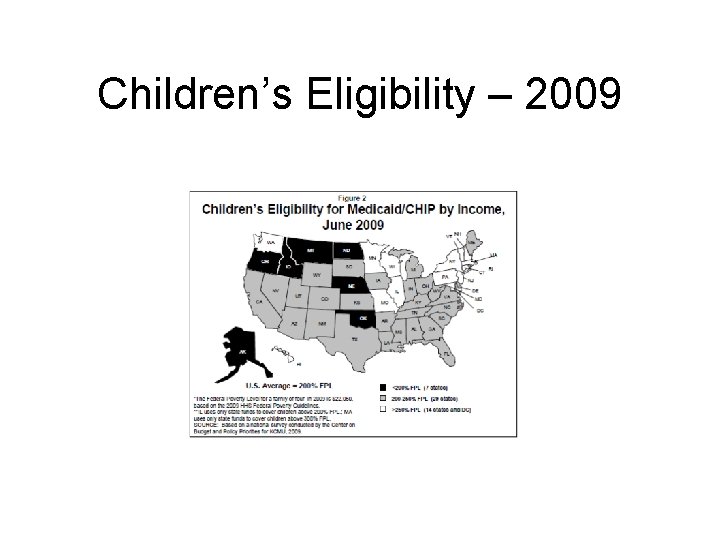
Children’s Eligibility – 2009

Children’s Eligibility – 2011
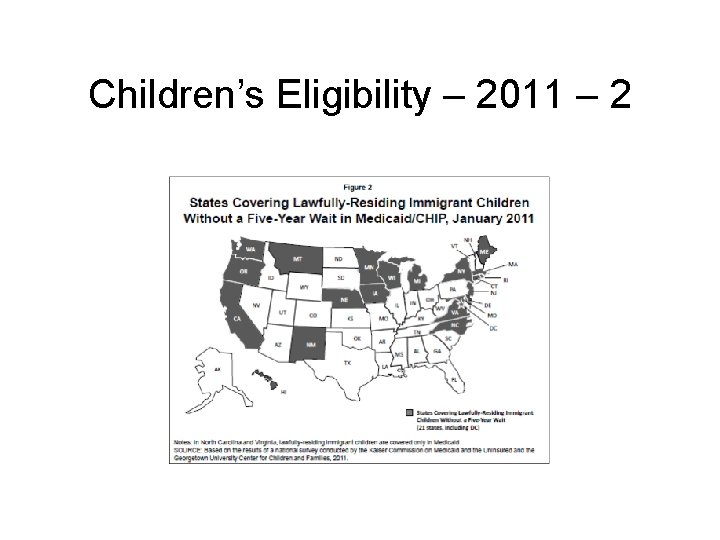
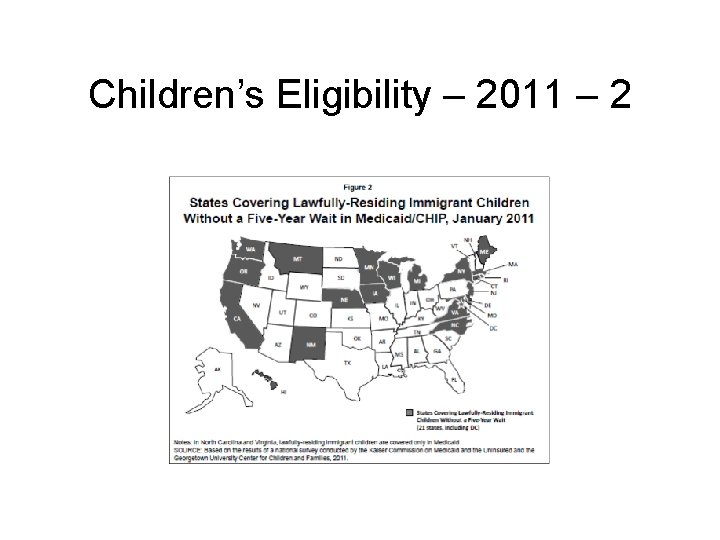
Children’s Eligibility – 2011 – 2
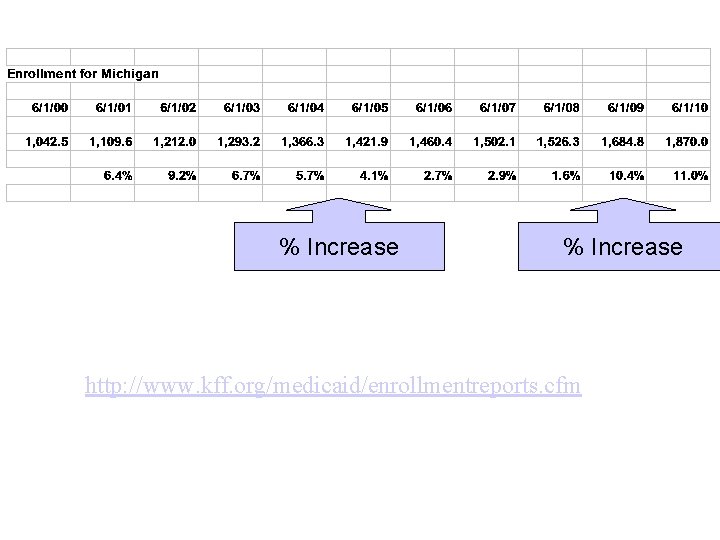
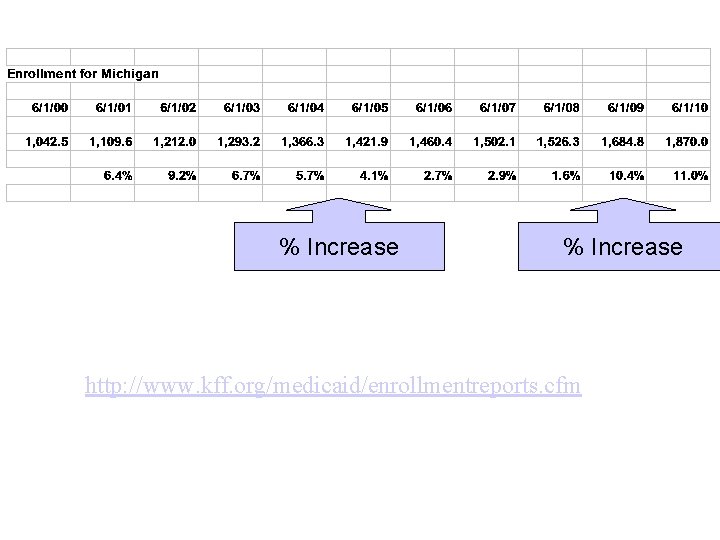
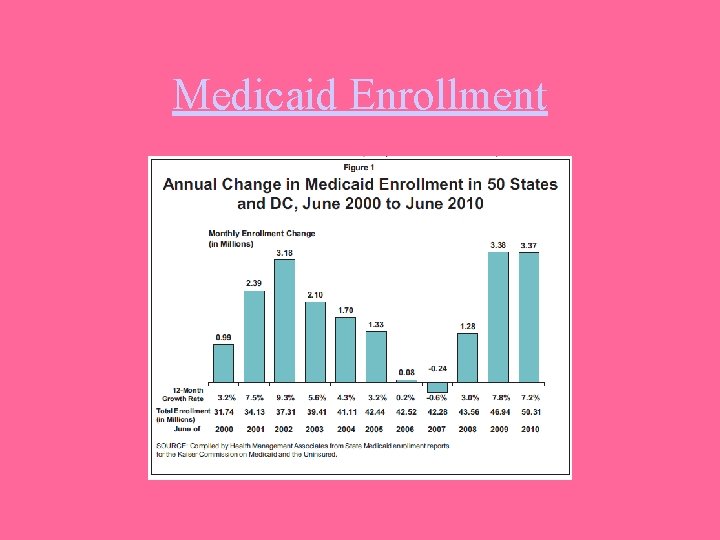
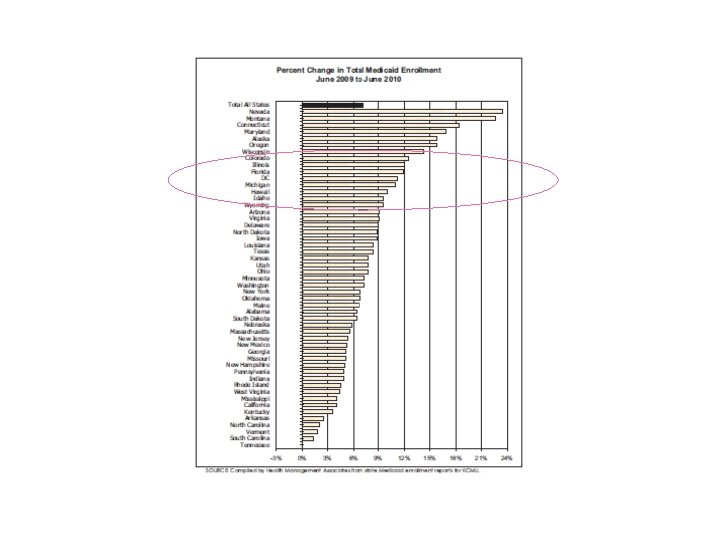
% Increase http: //www. kff. org/medicaid/enrollmentreports. cfm

Comes from the states Within broad national guidelines established by federal statutes, regulations and policies, each state: (1) establishes its own eligibility standards; (2) determines the type, amount, duration, and scope of services; (3) sets the rate of payment for services; and (4) administers its own program. Medicaid policies for eligibility, services, and payment vary considerably even among similar-sized and/or adjacent states. Thus, a person who is eligible for Medicaid in one state might not be eligible in another state; and the services provided by one state may differ.
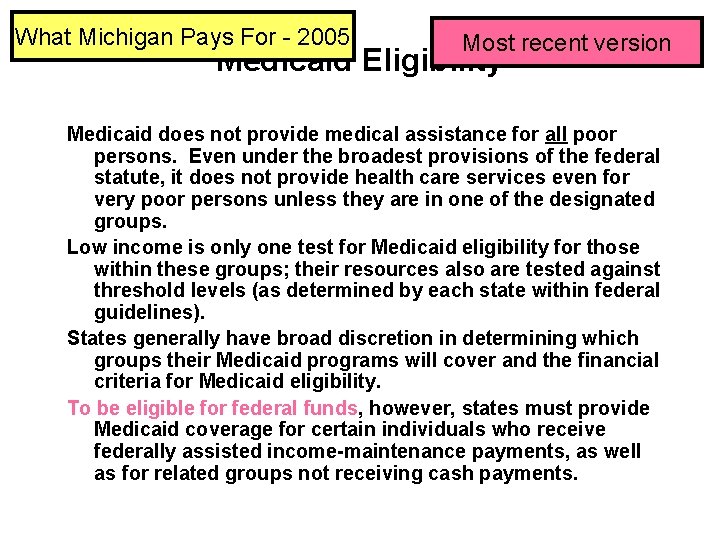
What Michigan Pays For - 2005 Most recent version Medicaid Eligibility Medicaid does not provide medical assistance for all poor persons. Even under the broadest provisions of the federal statute, it does not provide health care services even for very poor persons unless they are in one of the designated groups. Low income is only one test for Medicaid eligibility for those within these groups; their resources also are tested against threshold levels (as determined by each state within federal guidelines). States generally have broad discretion in determining which groups their Medicaid programs will cover and the financial criteria for Medicaid eligibility. To be eligible for federal funds, however, states must provide Medicaid coverage for certain individuals who receive federally assisted income-maintenance payments, as well as for related groups not receiving cash payments.

Payment for Medicaid Services States may impose nominal deductibles, coinsurance, or copayments on some Medicaid recipients for certain services, but certain Medicaid recipients, including pregnant women and children under age 18, are excluded from cost sharing. All Medicaid recipients must be exempt from copayments for emergency services and family planning services. Medicaid is a cost-sharing partnership between the federal government and the states. The federal government pays a share of the medical assistance expenditures under each state’s Medicaid program. That share, known as the Federal Medical Assistance Percentage (FMAP) is determined annually by a formula that compares the state’s average per capita income level with the national income average. States with higher per capita income levels are reimbursed smaller shares of their costs.

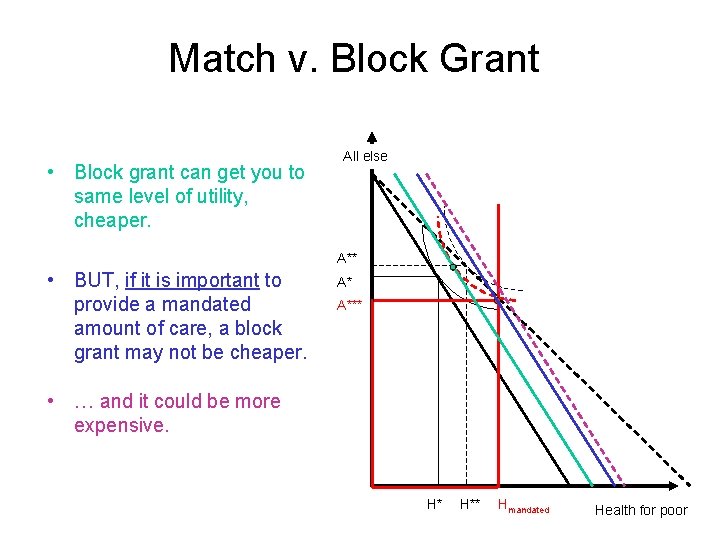
How the Medicaid match works … • Medicaid provides matching funds. • BUT federal mandates of program they cannot simply substitute Federal $ for State $. All else A** A* A*** • In particular, Medicaid has provided universal health insurance for children under age 18, whether states wanted it or not. • Probably a good thing. H* H** Hmandated Health for poor
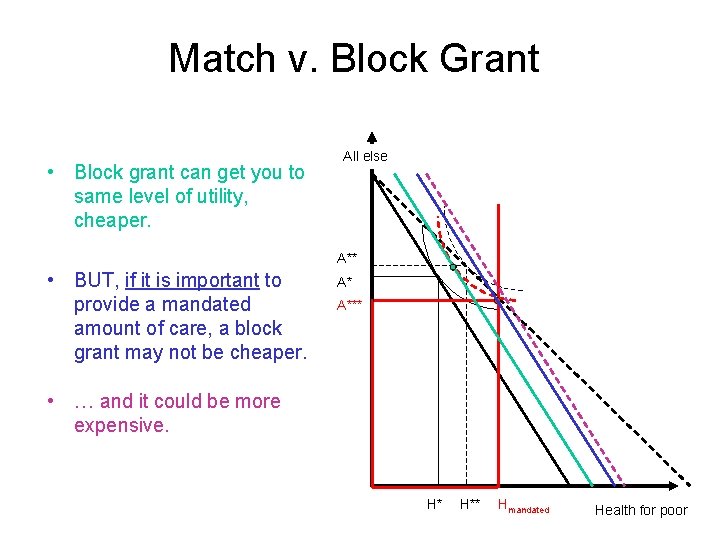
Match v. Block Grant • Block grant can get you to same level of utility, cheaper. All else A** • BUT, if it is important to provide a mandated amount of care, a block grant may not be cheaper. A* A*** • … and it could be more expensive. H* H** Hmandated Health for poor
States’ Decisions • States must raise taxes for matches. • Some have threatened to leave Medicaid, although they’ve not done it. • Others have threatened to reduce covered conditions.

Medicaid Summary • Most Medicaid recipients require relatively small average expenditures person each year. The 2009 data indicate that Medicaid payments for non-disabled children averaged about $2, 848 per child. Per capita spending for non-disabled children ($2, 848) and adults ($4, 123) was much lower than that for aged ($15, 678) and disabled beneficiaries ($16, 563). This reflects the differing health status and use of services by the members of these groups. • In 2008 Medicaid paid for 40. 6% of the total cost of nursing facility care and 34. 7% of or home health services care. With the elderly or disabled percentage of the population increasing faster than the younger groups, the need for long-term care is expected to increase.

The Medicaid — Medicare Relationship The Medicare and Medicaid programs work jointly for many beneficiaries. Medicare beneficiaries who have low incomes and limited resources may also receive help from the Medicaid program. For those eligible for full Medicaid coverage, the Medicare health care coverage is supplemented by services that are available under their state’s Medicaid program, according to eligibility category. These additional services may include, for example, nursing facility care beyond the 100 day limit covered by Medicare, prescription drugs, eyeglasses, and hearing aids. For persons enrolled in both programs, any services that are covered by Medicare paid for by the Medicare program before any payments are made by the Medicaid program, since Medicaid is always “payer of last resort. ”
The Medicaid — Medicare Relationship CMS estimates that Medicaid provided some supplemental health coverage for at least 8. 8 million persons who were Medicare beneficiaries. Medicare prescription drug benefit, started in 2006, includes all who previously received coverage from Medicaid.
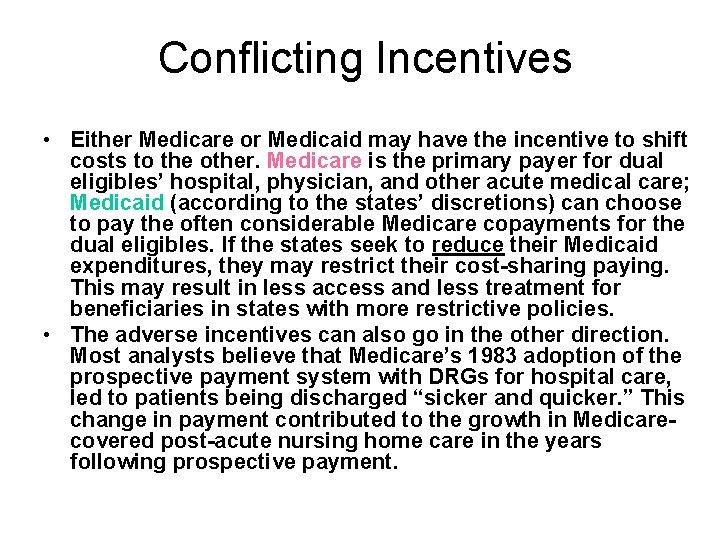
Conflicting Incentives • Either Medicare or Medicaid may have the incentive to shift costs to the other. Medicare is the primary payer for dual eligibles’ hospital, physician, and other acute medical care; Medicaid (according to the states’ discretions) can choose to pay the often considerable Medicare copayments for the dual eligibles. If the states seek to reduce their Medicaid expenditures, they may restrict their cost-sharing paying. This may result in less access and less treatment for beneficiaries in states with more restrictive policies. • The adverse incentives can also go in the other direction. Most analysts believe that Medicare’s 1983 adoption of the prospective payment system with DRGs for hospital care, led to patients being discharged “sicker and quicker. ” This change in payment contributed to the growth in Medicarecovered post-acute nursing home care in the years following prospective payment.
Conflicting Incentives – What to Do? • One possibility is to try to coordinate the two programs. • Second possibility – Shift financial responsibility of dual eligibles to federal government. Either Medicare, or some new program. • PPACA creates “office of the duals” to look at this.

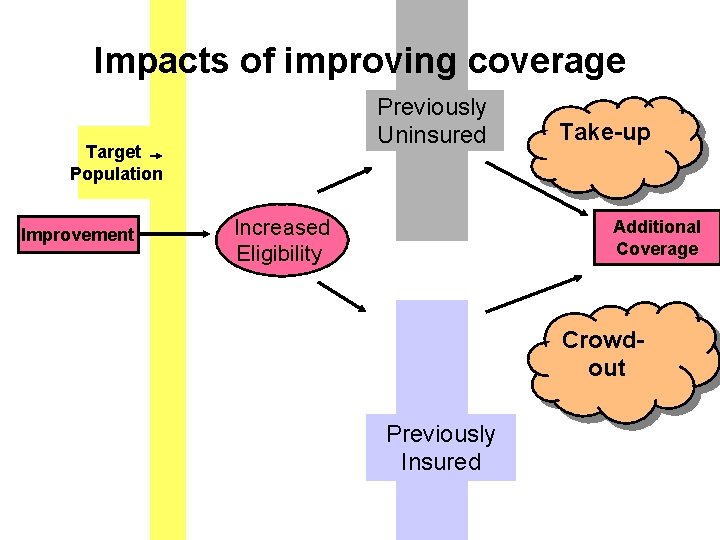
“Take-up” and “Crowd-out” • What are the net impacts of social insurance program implementation? • Are people now insured, who were previously uninsured (take-up), or are the new programs simply crowding out other forms of insurance?
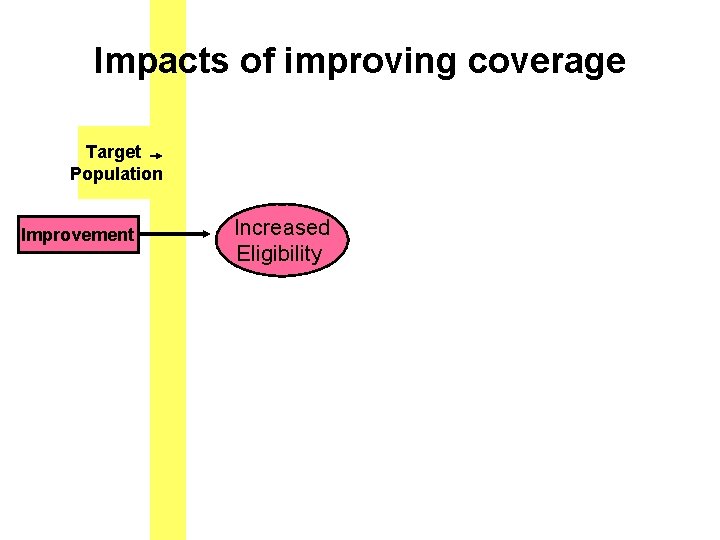
Impacts of improving coverage Target Population Improvement Increased Eligibility
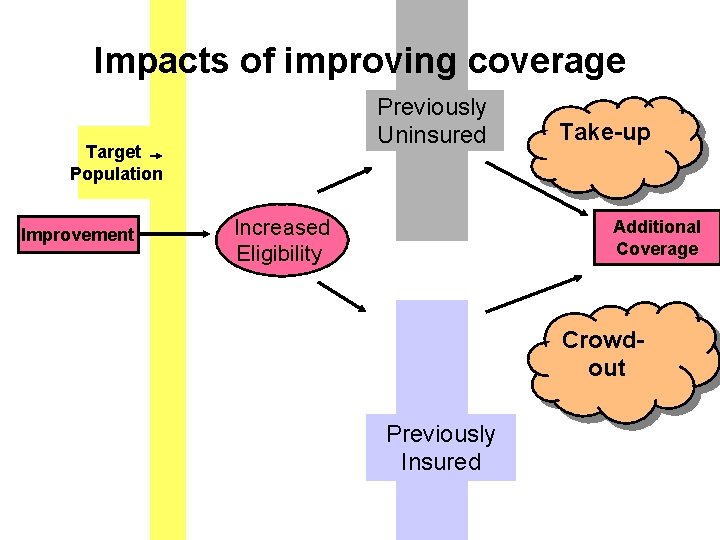
Impacts of improving coverage Previously Uninsured Target Population Improvement Increased Eligibility Take-up Additional Coverage Crowdout Previously Insured

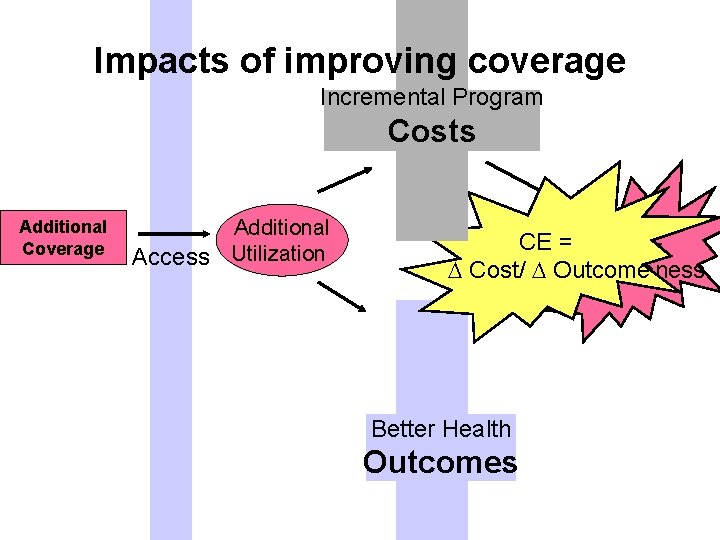
Impacts of improving coverage Additional Coverage Access Additional Utilization
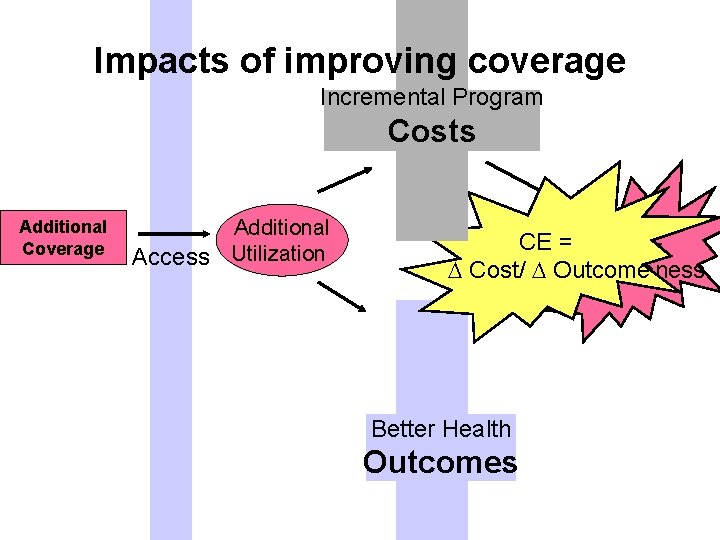
Impacts of improving coverage Incremental Program Costs Additional Coverage Additional Access Utilization CE = Cost/ Outcome Effectiveness Better Health Outcomes
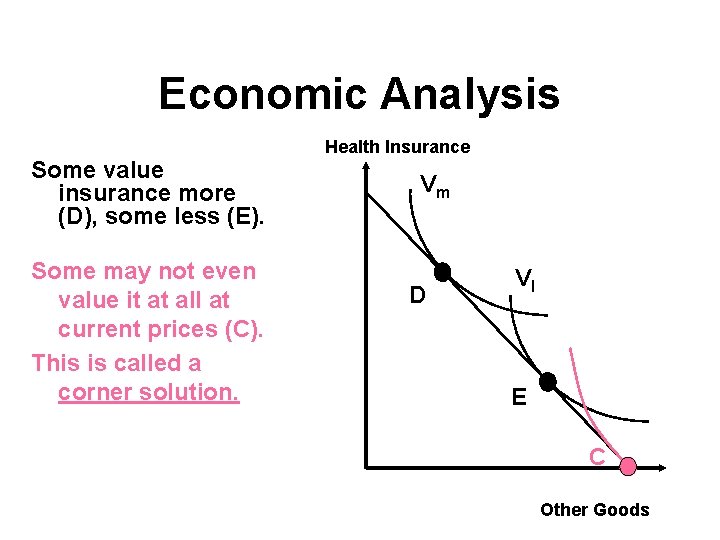
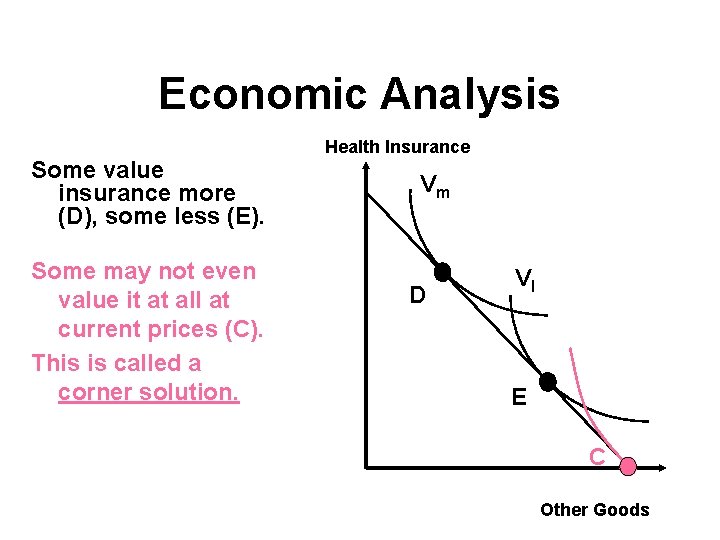
Economic Analysis Some value insurance more (D), some less (E). Some may not even value it at all at current prices (C). This is called a corner solution. Health Insurance Vm D Vl E C Other Goods
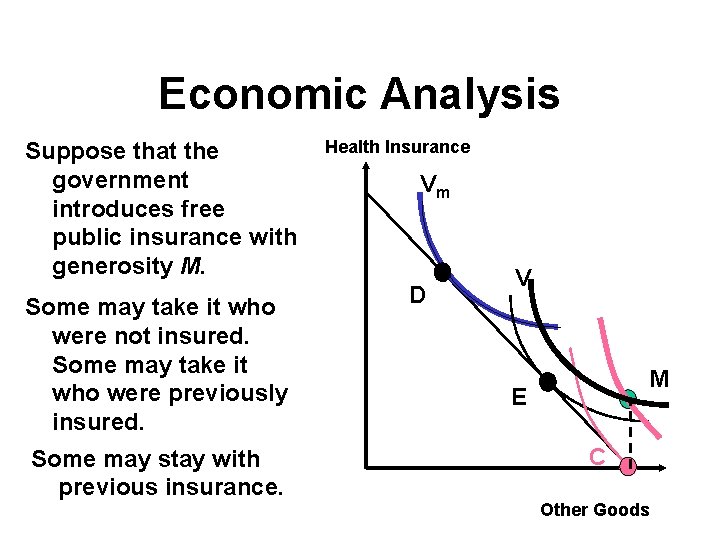
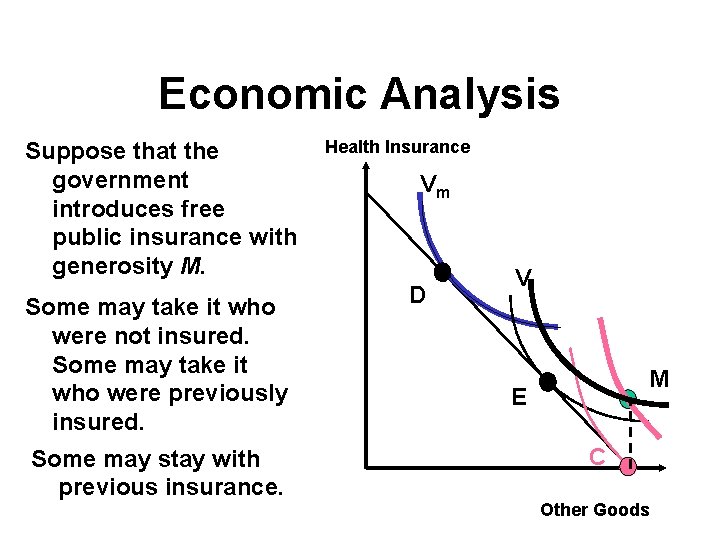
Economic Analysis Suppose that the government introduces free public insurance with generosity M. Some may take it who were not insured. Some may take it who were previously insured. Some may stay with previous insurance. Health Insurance Vm D Vl M E C Other Goods
Impacts • Cutler and Gruber estimate that under Medicaid expansions, about ½ of increase in eligibility has been associated with a reduction in private insurance coverage (crowd-out), and about ½ with take-up.
Supplemental
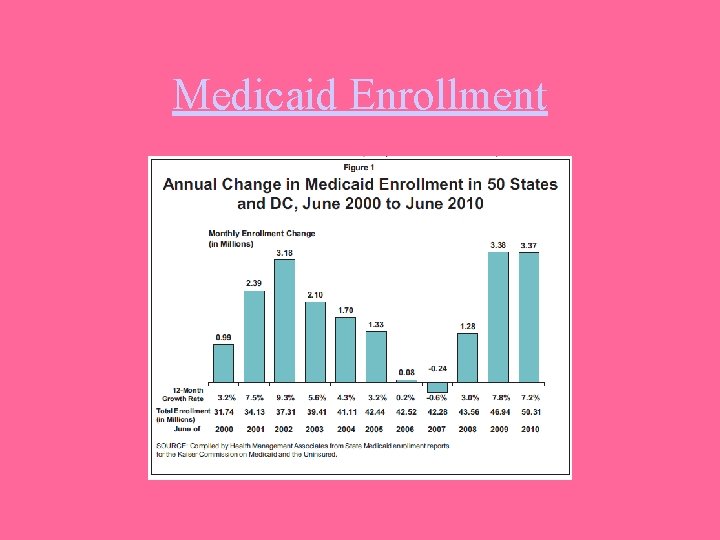
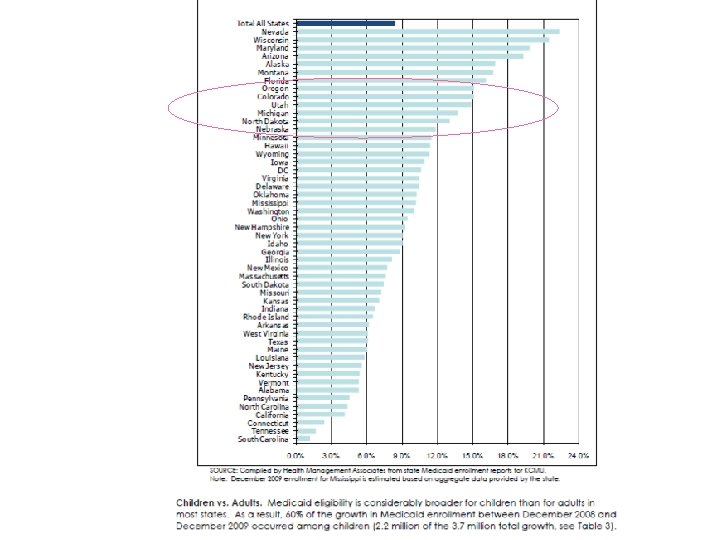
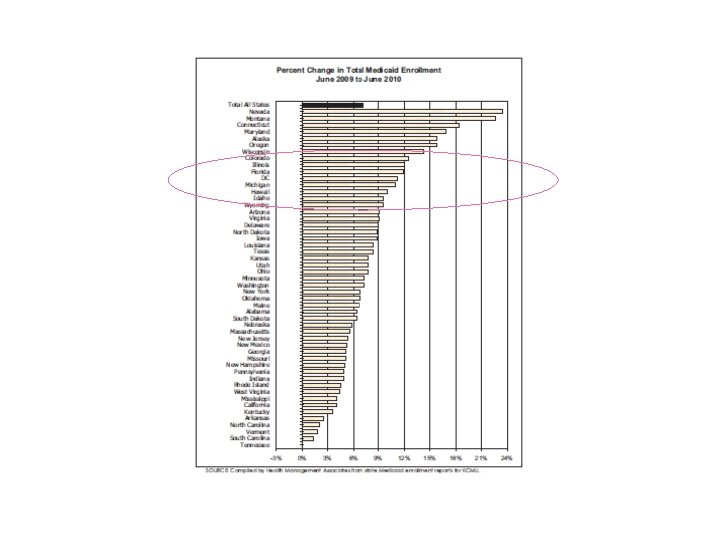
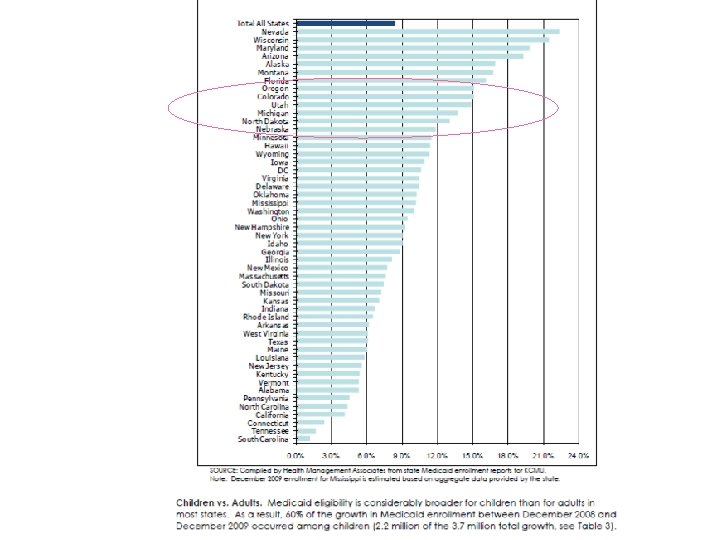
Medicaid Enrollment

Medicaid Enrollment
 Ein gleiches
Ein gleiches The symbol tsfa in alu operations include
The symbol tsfa in alu operations include Sample performance monitoring and coaching form
Sample performance monitoring and coaching form Nature of fire insurance
Nature of fire insurance Imagery in young goodman brown
Imagery in young goodman brown Young goodman brown theme
Young goodman brown theme Suki goodman
Suki goodman 17 miracle prayer by elisha goodman
17 miracle prayer by elisha goodman Young goodman brown theme
Young goodman brown theme Dr anthony goodman
Dr anthony goodman Debrisochina
Debrisochina Dünyanın en çok piercing takan adamı
Dünyanın en çok piercing takan adamı Elisha goodman biography
Elisha goodman biography Design against fluctuating load
Design against fluctuating load Goodman bacon decomposition
Goodman bacon decomposition Pagkilala sa mambabasa
Pagkilala sa mambabasa Historical context of young goodman brown
Historical context of young goodman brown Cta goodman elementary
Cta goodman elementary Young goodman brown exposition
Young goodman brown exposition Soderberg diyagramı
Soderberg diyagramı What does charlie accuse goodman of?
What does charlie accuse goodman of? Dark romanticism in young goodman brown
Dark romanticism in young goodman brown Goodman recycling
Goodman recycling Corrina martinez
Corrina martinez Gerard finbow
Gerard finbow Nathaniel hawthorne puritan background
Nathaniel hawthorne puritan background Gawen goodman portrait
Gawen goodman portrait Nathaniel hawthorne dark romanticism
Nathaniel hawthorne dark romanticism Livspace financials
Livspace financials Dr elizabeth goodman
Dr elizabeth goodman Samuel lopez lawyer
Samuel lopez lawyer Karin allen
Karin allen Peripheral iv antecubital
Peripheral iv antecubital Allen and gale 2000
Allen and gale 2000 Allen's test
Allen's test Poder judicial
Poder judicial Royal college of nursing v dhss (1981)
Royal college of nursing v dhss (1981) Whitely v chappel
Whitely v chappel Nicola allen knutsford
Nicola allen knutsford Burroughs allen waltrip
Burroughs allen waltrip Next in line effect psychology definition
Next in line effect psychology definition Ivan allen jr accomplishments
Ivan allen jr accomplishments Allen knutson
Allen knutson Record du monde corps humain
Record du monde corps humain