SCE questions mostly physiology and lung function testing
- Slides: 31
SCE questions – mostly physiology and lung function testing Joseph Kibbler Respiratory Sp. R Teaching 20/05/2020
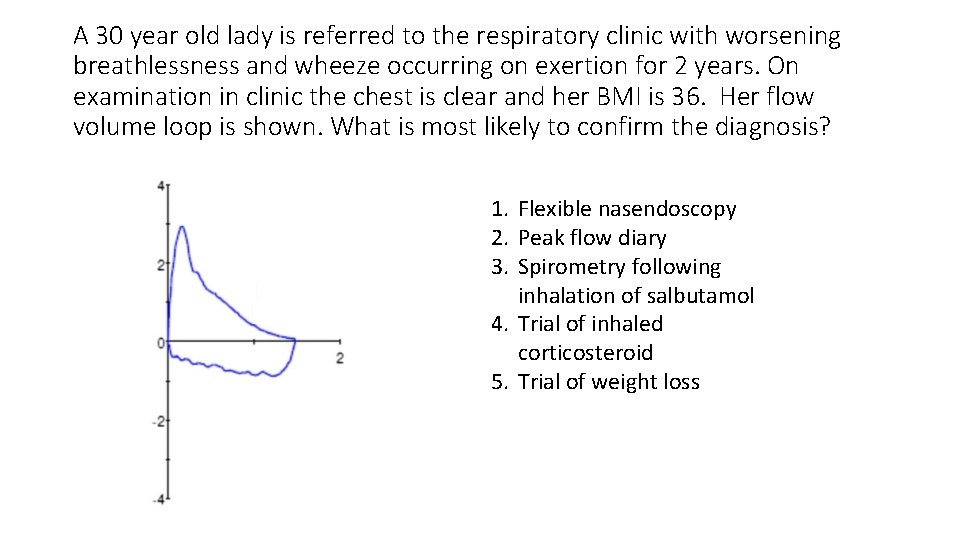
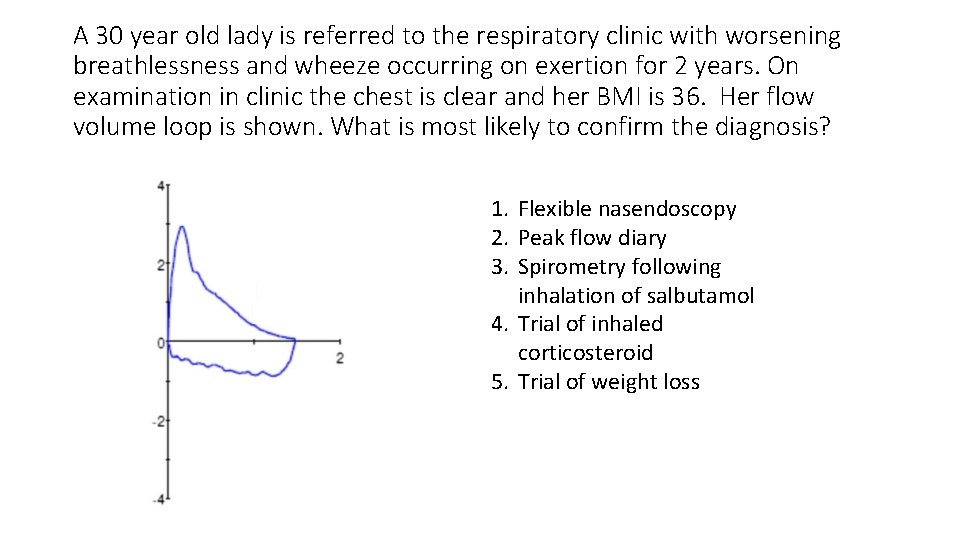
A 30 year old lady is referred to the respiratory clinic with worsening breathlessness and wheeze occurring on exertion for 2 years. On examination in clinic the chest is clear and her BMI is 36. Her flow volume loop is shown. What is most likely to confirm the diagnosis? 1. Flexible nasendoscopy 2. Peak flow diary 3. Spirometry following inhalation of salbutamol 4. Trial of inhaled corticosteroid 5. Trial of weight loss
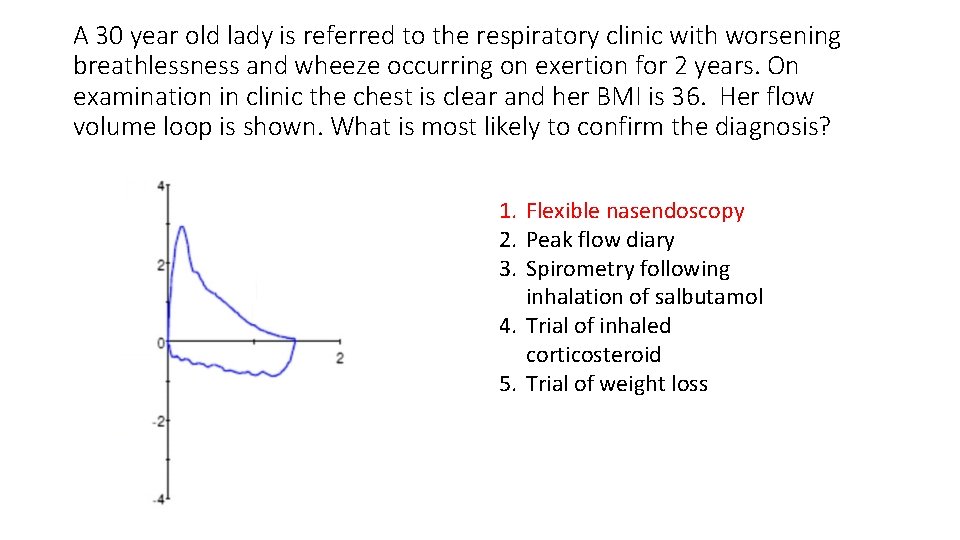
A 30 year old lady is referred to the respiratory clinic with worsening breathlessness and wheeze occurring on exertion for 2 years. On examination in clinic the chest is clear and her BMI is 36. Her flow volume loop is shown. What is most likely to confirm the diagnosis? 1. Flexible nasendoscopy 2. Peak flow diary 3. Spirometry following inhalation of salbutamol 4. Trial of inhaled corticosteroid 5. Trial of weight loss
Flow-volume loop in vocal cord dysfunction • Flow volume loop shows flattening of inspiratory portion • Would also be seen in laryngomalacia, polychondritis, mobile tumours • Hence need for nasendoscopy • Saw tooth pattern may also be seen • A degree of lower airway obstruction suggested by expiratory portion but inspiratory abnormality much starker
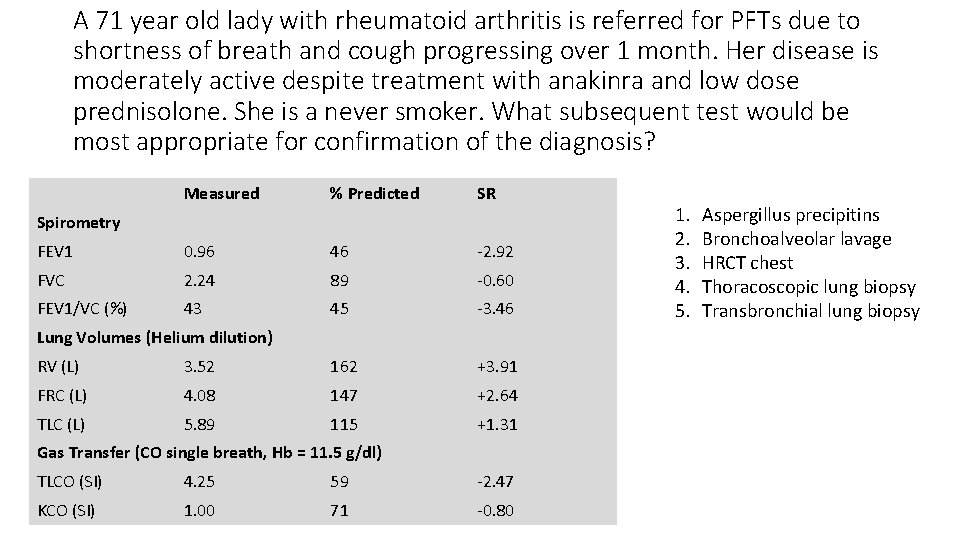
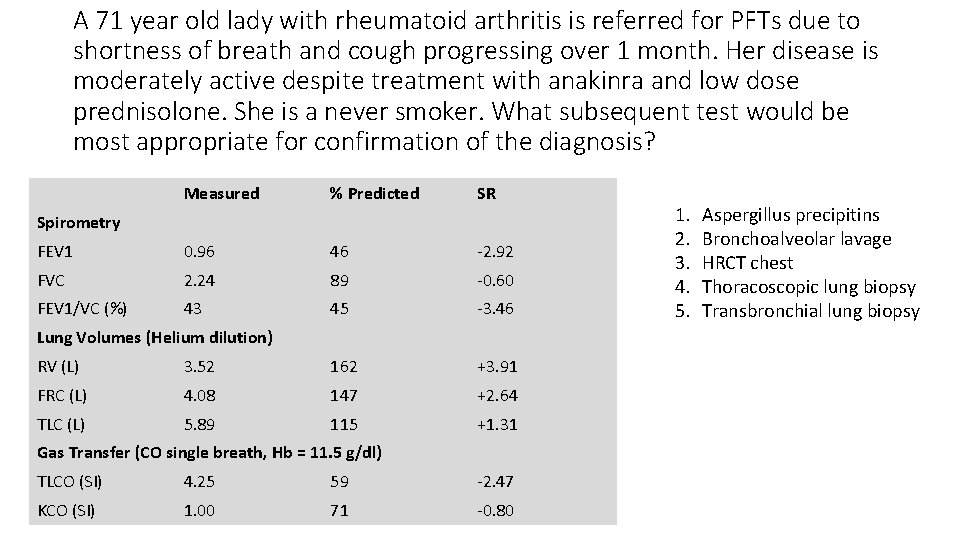
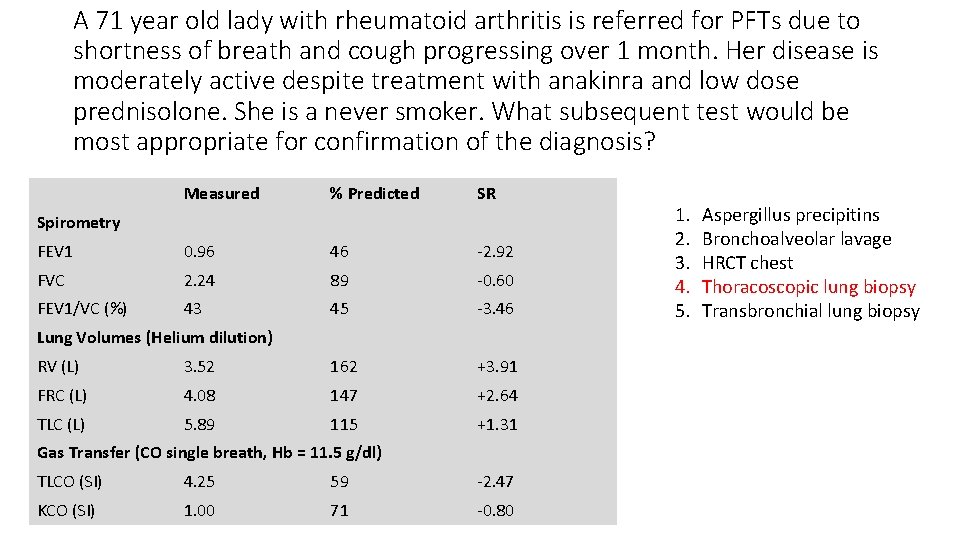
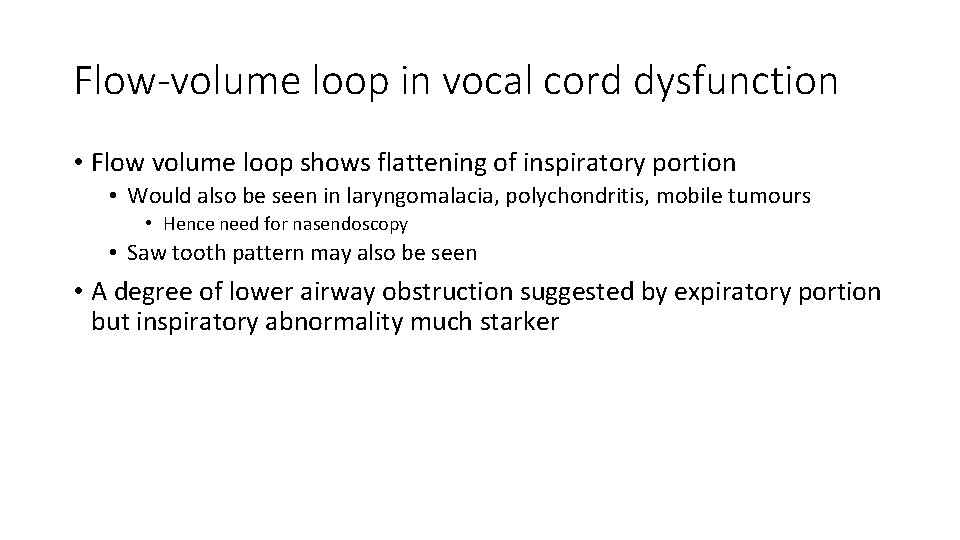
A 71 year old lady with rheumatoid arthritis is referred for PFTs due to shortness of breath and cough progressing over 1 month. Her disease is moderately active despite treatment with anakinra and low dose prednisolone. She is a never smoker. What subsequent test would be most appropriate for confirmation of the diagnosis? Measured % Predicted SR FEV 1 0. 96 46 ‐ 2. 92 FVC 2. 24 89 ‐ 0. 60 FEV 1/VC (%) 43 45 ‐ 3. 46 Spirometry Lung Volumes (Helium dilution) RV (L) 3. 52 162 +3. 91 FRC (L) 4. 08 147 +2. 64 TLC (L) 5. 89 115 +1. 31 Gas Transfer (CO single breath, Hb = 11. 5 g/dl) TLCO (SI) 4. 25 59 ‐ 2. 47 KCO (SI) 1. 00 71 ‐ 0. 80 1. 2. 3. 4. 5. Aspergillus precipitins Bronchoalveolar lavage HRCT chest Thoracoscopic lung biopsy Transbronchial lung biopsy
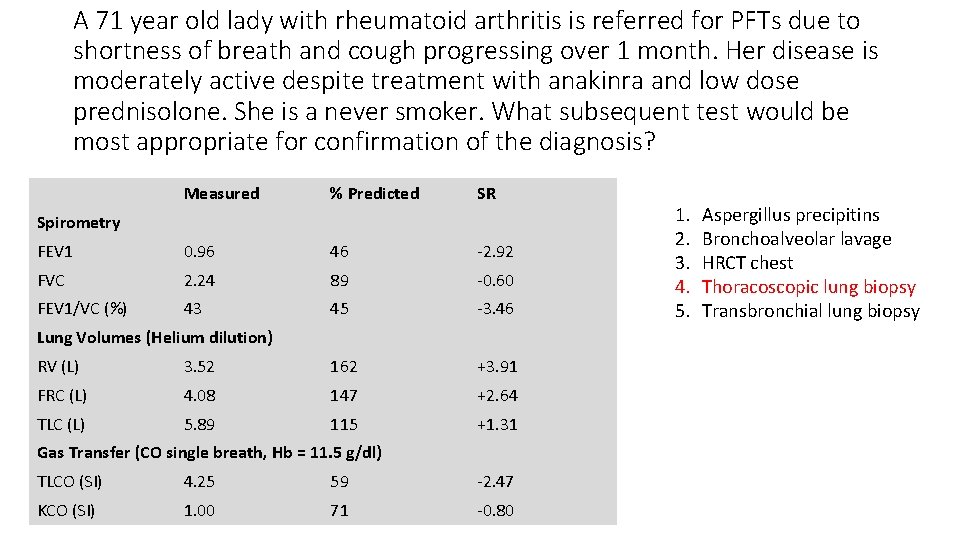
A 71 year old lady with rheumatoid arthritis is referred for PFTs due to shortness of breath and cough progressing over 1 month. Her disease is moderately active despite treatment with anakinra and low dose prednisolone. She is a never smoker. What subsequent test would be most appropriate for confirmation of the diagnosis? Measured % Predicted SR FEV 1 0. 96 46 ‐ 2. 92 FVC 2. 24 89 ‐ 0. 60 FEV 1/VC (%) 43 45 ‐ 3. 46 Spirometry Lung Volumes (Helium dilution) RV (L) 3. 52 162 +3. 91 FRC (L) 4. 08 147 +2. 64 TLC (L) 5. 89 115 +1. 31 Gas Transfer (CO single breath, Hb = 11. 5 g/dl) TLCO (SI) 4. 25 59 ‐ 2. 47 KCO (SI) 1. 00 71 ‐ 0. 80 1. 2. 3. 4. 5. Aspergillus precipitins Bronchoalveolar lavage HRCT chest Thoracoscopic lung biopsy Transbronchial lung biopsy
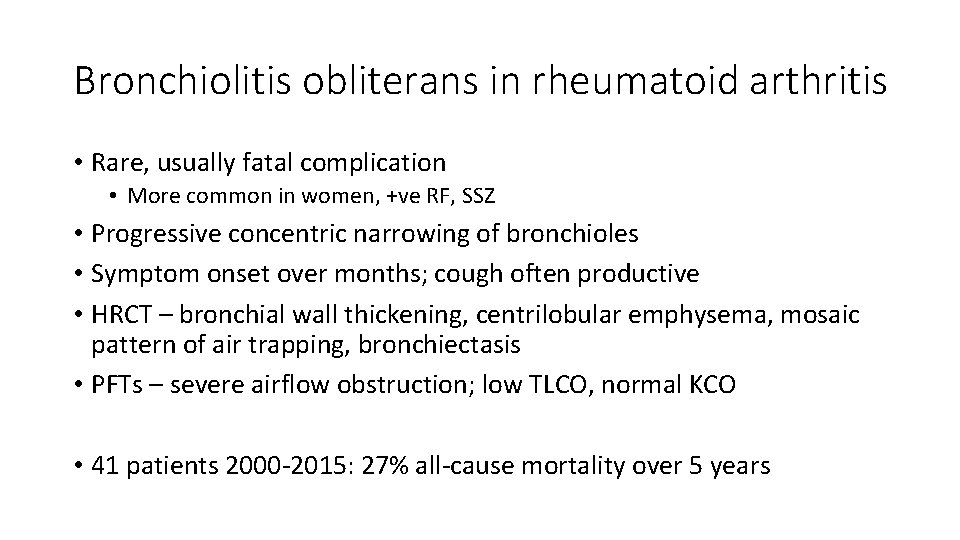
Bronchiolitis obliterans in rheumatoid arthritis • Rare, usually fatal complication • More common in women, +ve RF, SSZ • Progressive concentric narrowing of bronchioles • Symptom onset over months; cough often productive • HRCT – bronchial wall thickening, centrilobular emphysema, mosaic pattern of air trapping, bronchiectasis • PFTs – severe airflow obstruction; low TLCO, normal KCO • 41 patients 2000‐ 2015: 27% all‐cause mortality over 5 years
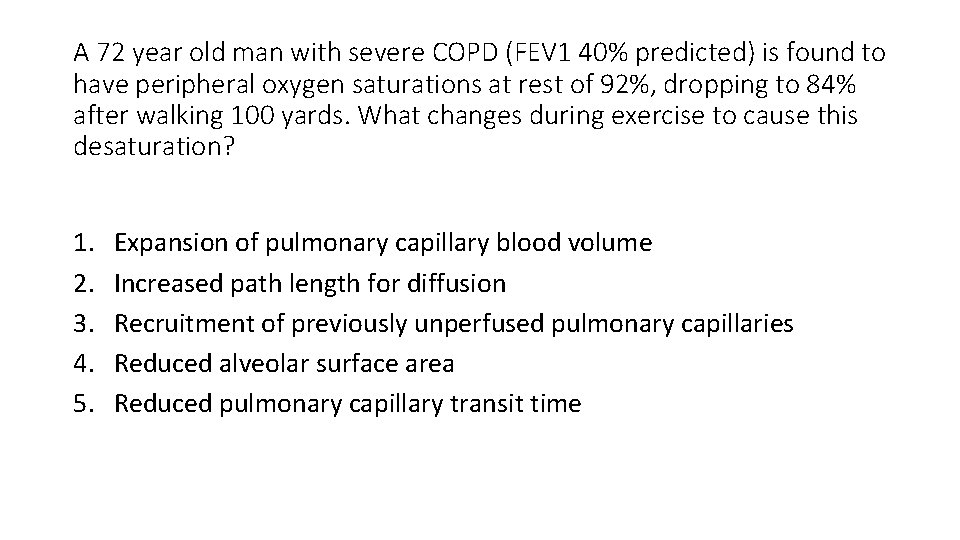
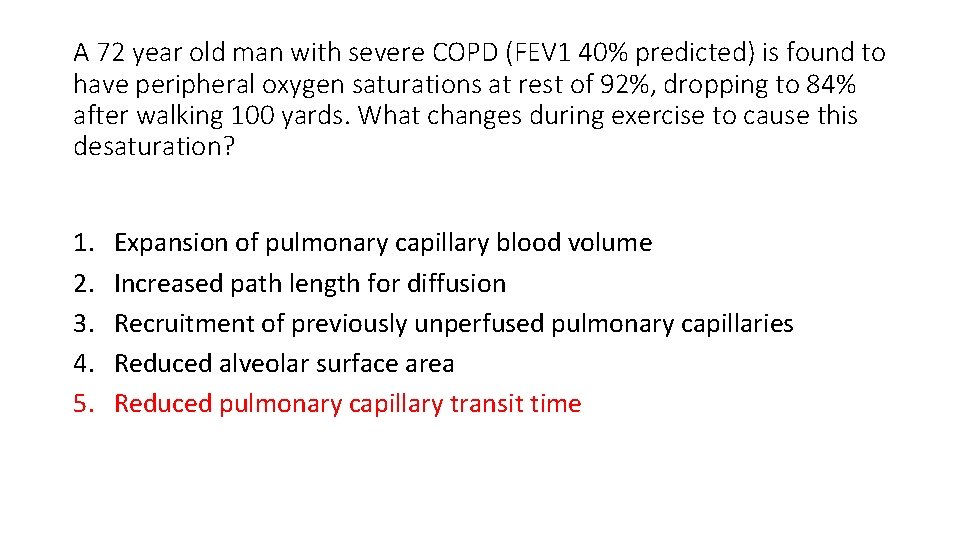
A 72 year old man with severe COPD (FEV 1 40% predicted) is found to have peripheral oxygen saturations at rest of 92%, dropping to 84% after walking 100 yards. What changes during exercise to cause this desaturation? 1. 2. 3. 4. 5. Expansion of pulmonary capillary blood volume Increased path length for diffusion Recruitment of previously unperfused pulmonary capillaries Reduced alveolar surface area Reduced pulmonary capillary transit time
A 72 year old man with severe COPD (FEV 1 40% predicted) is found to have peripheral oxygen saturations at rest of 92%, dropping to 84% after walking 100 yards. What changes during exercise to cause this desaturation? 1. 2. 3. 4. 5. Expansion of pulmonary capillary blood volume Increased path length for diffusion Recruitment of previously unperfused pulmonary capillaries Reduced alveolar surface area Reduced pulmonary capillary transit time
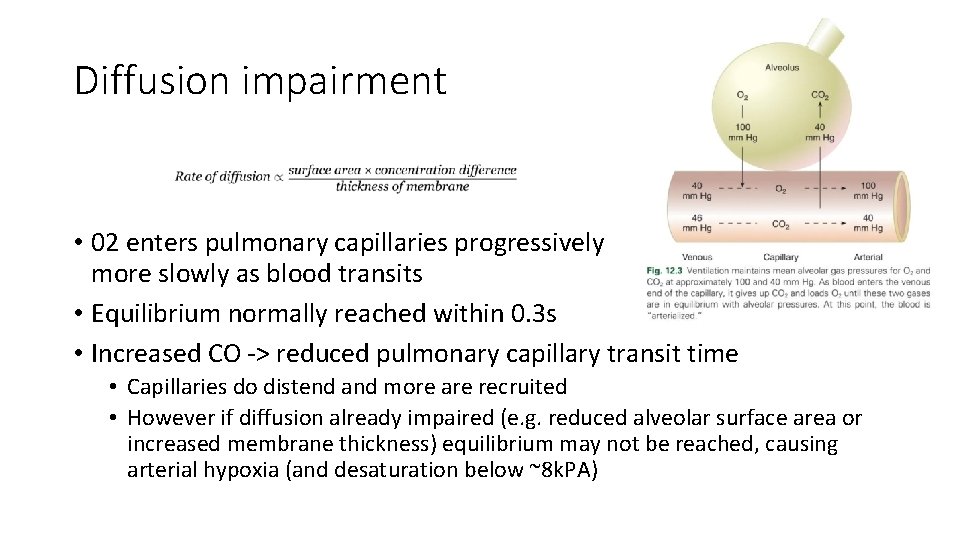
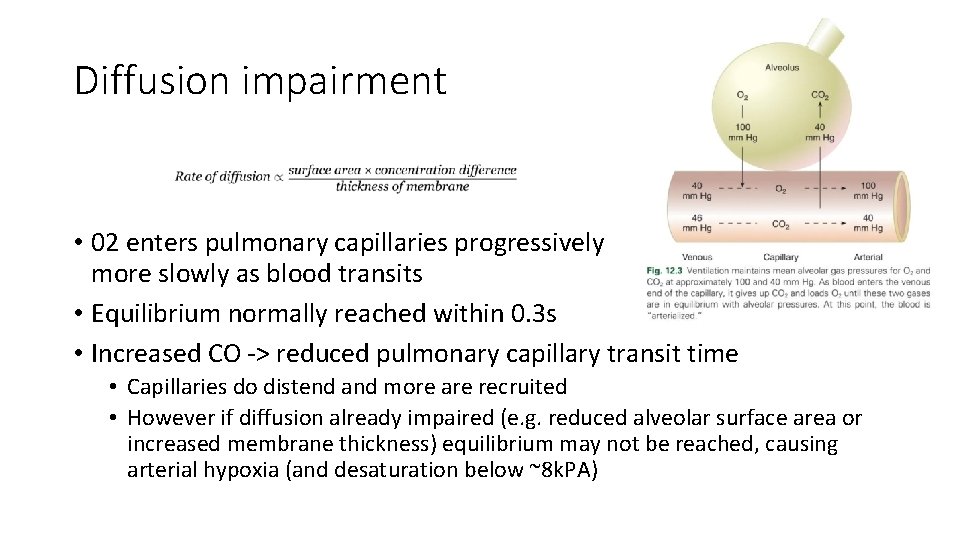
Diffusion impairment • 02 enters pulmonary capillaries progressively more slowly as blood transits • Equilibrium normally reached within 0. 3 s • Increased CO ‐> reduced pulmonary capillary transit time • Capillaries do distend and more are recruited • However if diffusion already impaired (e. g. reduced alveolar surface area or increased membrane thickness) equilibrium may not be reached, causing arterial hypoxia (and desaturation below ~8 k. PA)
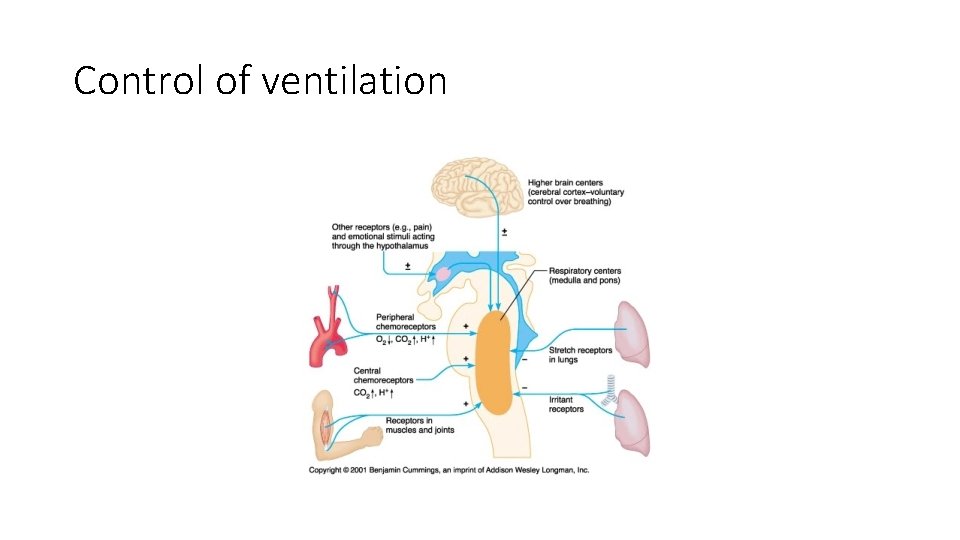
Regarding ventilatory control, which of the following is false? 1. Inadequate ventilation produces a change in the timing and amplitude of neural stimuli passing through the phrenic nerve 2. Peripheral chemoreceptors at the junction of the external and common carotid arteries do not discharge until Pa. O 2 falls below 8 k. Pa 3. An increase in arterial Pa. CO 2 increases central chemoreceptor firing rate 4. Acid‐base compensation within the cerebrospinal fluid is an important determinant of the effect of raised Pa. CO 2 5. The size of the effect of changes in Pa. O 2 and Pa. CO 2 changes in different stages of sleep
Regarding ventilatory control, which of the following is false? 1. Inadequate ventilation produces a change in the timing and amplitude of neural stimuli passing through the phrenic nerve 2. Peripheral chemoreceptors at the junction of the external and common carotid arteries do not discharge until Pa. O 2 falls below 8 k. Pa 3. An increase in arterial Pa. CO 2 increases central chemoreceptor firing rate 4. Acid‐base compensation within the cerebrospinal fluid is an important determinant of the effect of raised Pa. CO 2 5. The size of the effect of changes in Pa. O 2 and Pa. CO 2 changes in different stages of sleep
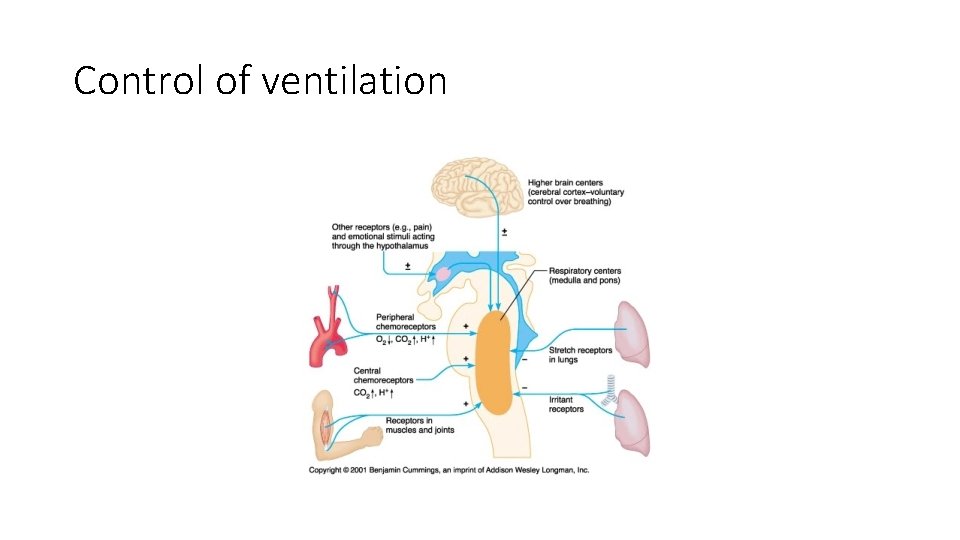
Control of ventilation
Which of the following statements about maximal inspiratory pressure (MIP) is true? 1. It is generated by a combination of inspiratory muscle force and elastic recoil of the chest wall at total lung capacity 2. It is generated by a combination of inspiratory muscle force and elastic recoil of the chest wall from functional residual capacity 3. It is generated by a combination of inspiratory muscle force and elastic recoil of the chest wall from residual volume 4. It is generated by a combination of inspiratory muscle force and elastic recoil of the lungs from functional residual capacity 5. It is generated by a combination of inspiratory muscle force and elastic recoil of the lungs from residual volume
Which of the following statements about maximal inspiratory pressure (MIP) is true? 1. It is generated by a combination of inspiratory muscle force and elastic recoil of the chest wall at total lung capacity 2. It is generated by a combination of inspiratory muscle force and elastic recoil of the chest wall from functional residual capacity 3. It is generated by a combination of inspiratory muscle force and elastic recoil of the chest wall from residual volume 4. It is generated by a combination of inspiratory muscle force and elastic recoil of the lungs from functional residual capacity 5. It is generated by a combination of inspiratory muscle force and elastic recoil of the lungs from residual volume
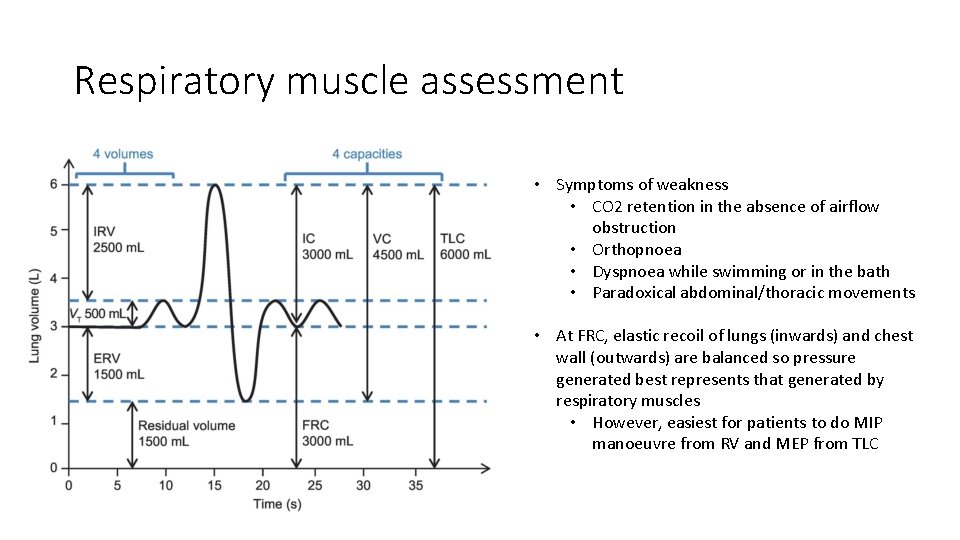
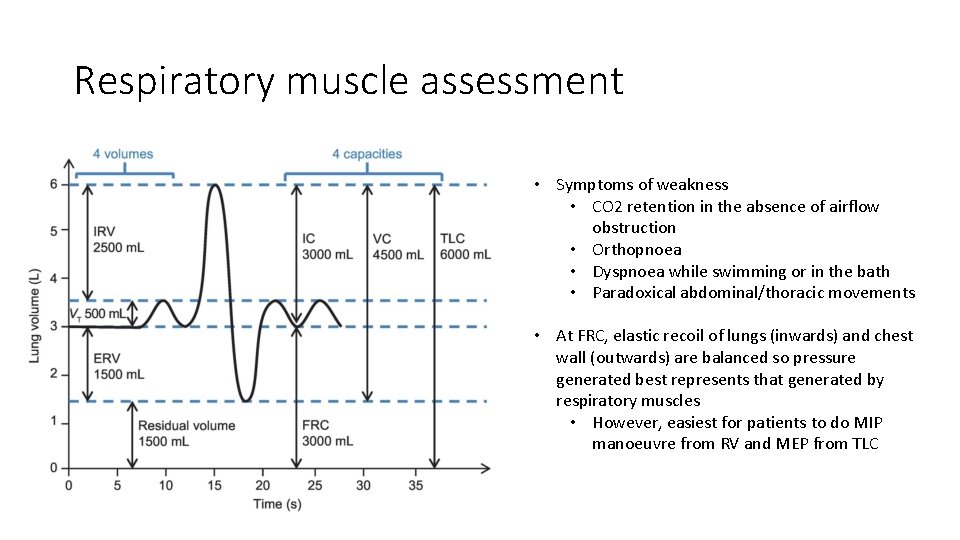
Respiratory muscle assessment • Symptoms of weakness • CO 2 retention in the absence of airflow obstruction • Orthopnoea • Dyspnoea while swimming or in the bath • Paradoxical abdominal/thoracic movements • At FRC, elastic recoil of lungs (inwards) and chest wall (outwards) are balanced so pressure generated best represents that generated by respiratory muscles • However, easiest for patients to do MIP manoeuvre from RV and MEP from TLC
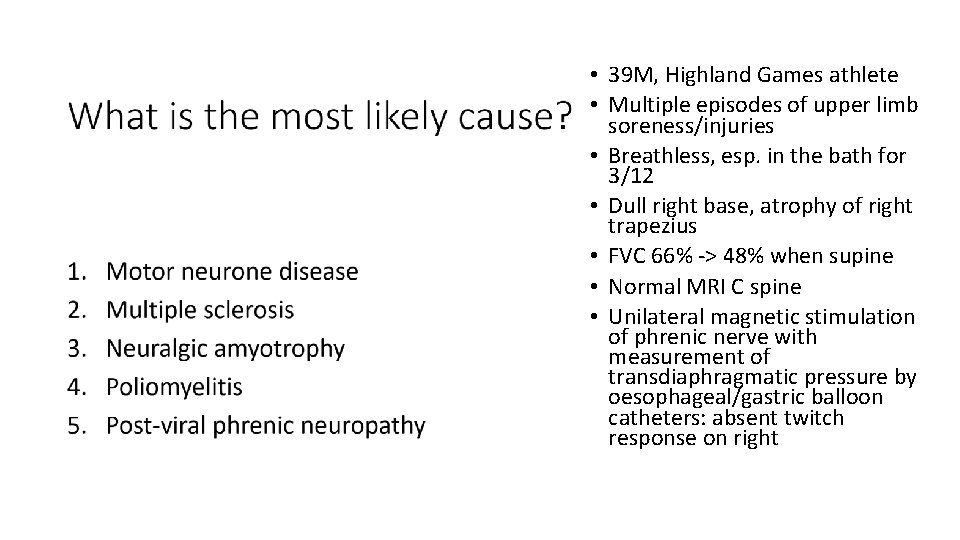
• 39 M, Highland Games athlete • Multiple episodes of upper limb soreness/injuries • Breathless, esp. in the bath for 3/12 • Dull right base, atrophy of right trapezius • FVC 66% ‐> 48% when supine • Normal MRI C spine • Unilateral magnetic stimulation of phrenic nerve with measurement of transdiaphragmatic pressure by oesophageal/gastric balloon catheters: absent twitch response on right
What is the most likely cause? 1. 2. 3. 4. 5. Motor neurone disease Multiple sclerosis Neuralgic amyotrophy Poliomyelitis Post‐viral phrenic neuropathy
Which of the following does not describe a mechanism by which inhaled helium-oxygen (Heliox) reduces work of breathing in patients with upper airway obstruction? 1. 2. 3. 4. It allows laminar flow to be established in larger airways It reduces the density of the gas flowing through the bronchial tree It reduces the proportion of gas that is flowing turbulently It reduces the Reynold’s number of the gas flowing through the bronchial tree 5. It reduces the viscosity of the gas flowing through the bronchial tree
Which of the following does not describe a mechanism by which inhaled helium-oxygen (Heliox) reduces work of breathing in patients with upper airway obstruction? 1. 2. 3. 4. It allows laminar flow to be established in larger airways It reduces the density of the gas flowing through the bronchial tree It reduces the proportion of gas that is flowing turbulently It reduces the Reynold’s number of the gas flowing through the bronchial tree 5. It reduces the viscosity of the gas flowing through the bronchial tree
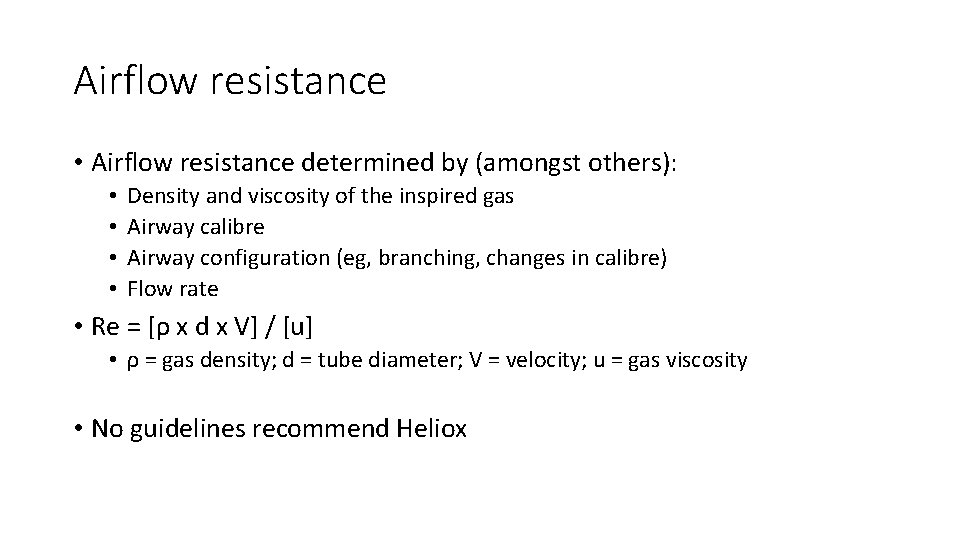
Airflow resistance • Airflow resistance determined by (amongst others): • • Density and viscosity of the inspired gas Airway calibre Airway configuration (eg, branching, changes in calibre) Flow rate • Re = [ρ x d x V] / [u] • ρ = gas density; d = tube diameter; V = velocity; u = gas viscosity • No guidelines recommend Heliox
In established interstitial lung disease, which of the following is typically true of the mechanics of the lungs? 1. 2. 3. 4. 5. Airflow for a given lung volume is normal or increased Chest wall compliance is reduced Functional residual capacity is increased Lung compliance is increased Lung recoil is reduced
In established interstitial lung disease, which of the following is typically true of the mechanics of the lungs? 1. 2. 3. 4. 5. Airflow for a given lung volume is normal or increased Chest wall compliance is reduced Functional residual capacity is increased Lung compliance is increased Lung recoil is reduced
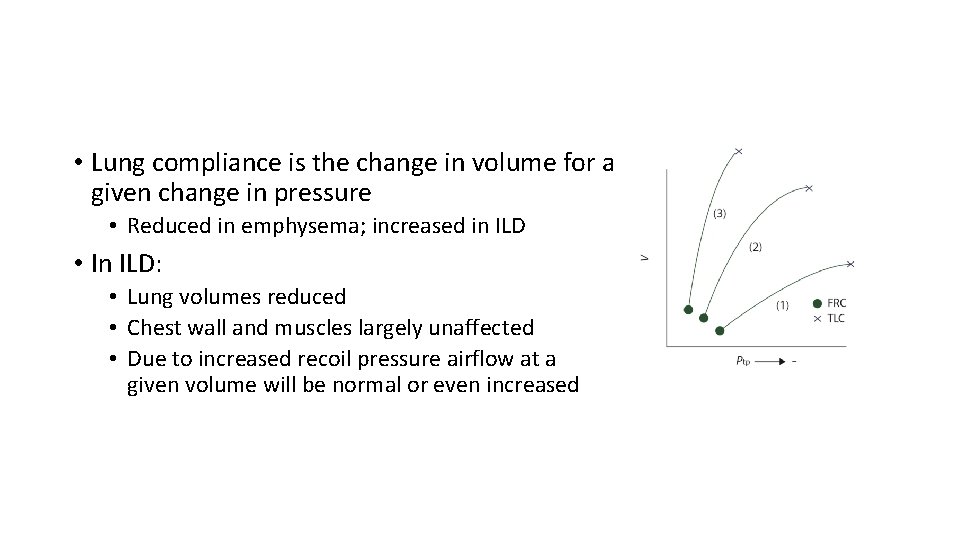
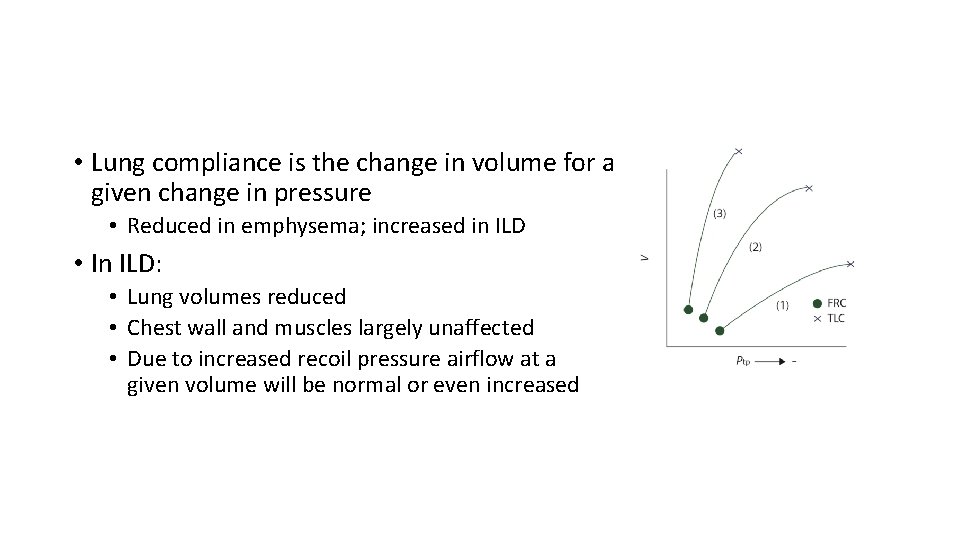
• Lung compliance is the change in volume for a given change in pressure • Reduced in emphysema; increased in ILD • In ILD: • Lung volumes reduced • Chest wall and muscles largely unaffected • Due to increased recoil pressure airflow at a given volume will be normal or even increased
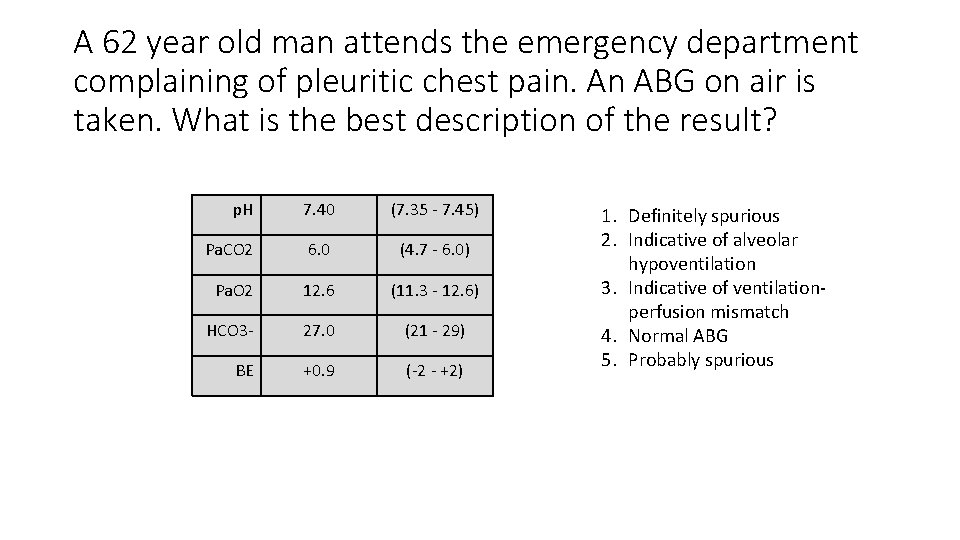
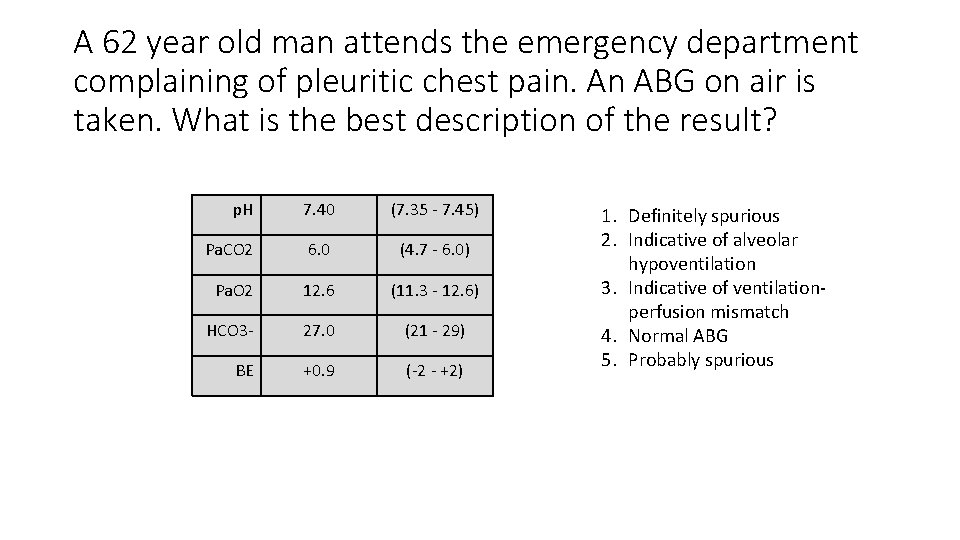
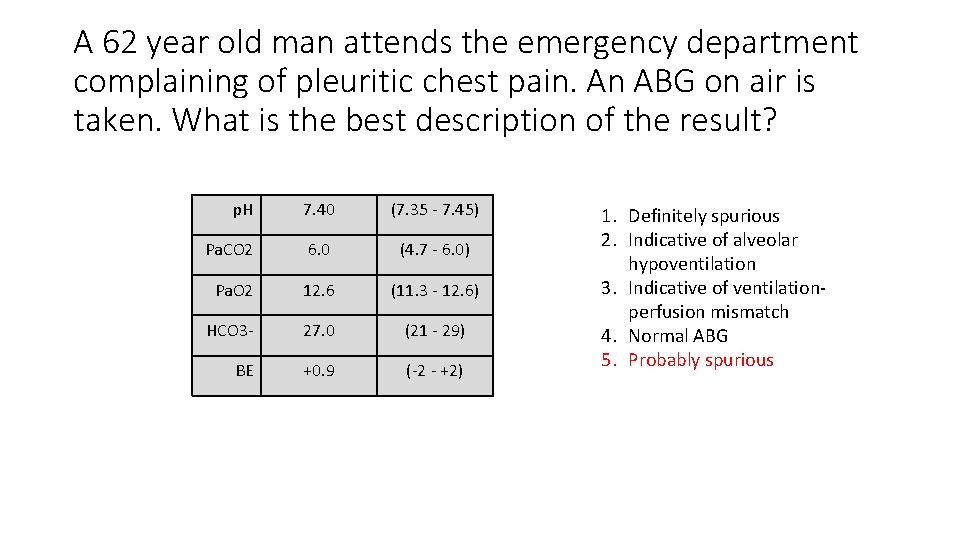
A 62 year old man attends the emergency department complaining of pleuritic chest pain. An ABG on air is taken. What is the best description of the result? p. H 7. 40 (7. 35 ‐ 7. 45) Pa. CO 2 6. 0 (4. 7 ‐ 6. 0) Pa. O 2 12. 6 (11. 3 ‐ 12. 6) HCO 3‐ 27. 0 (21 ‐ 29) BE +0. 9 (‐ 2 ‐ +2) 1. Definitely spurious 2. Indicative of alveolar hypoventilation 3. Indicative of ventilation‐ perfusion mismatch 4. Normal ABG 5. Probably spurious
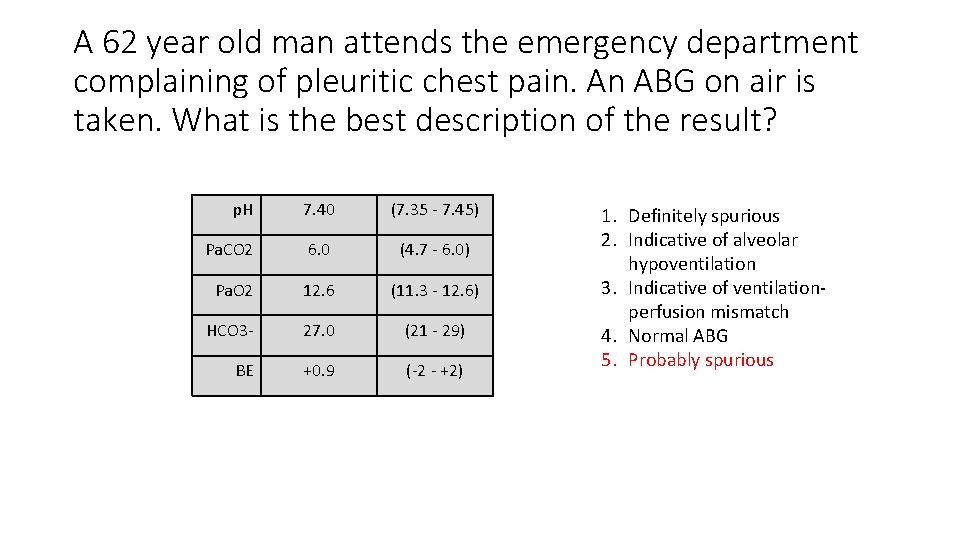
A 62 year old man attends the emergency department complaining of pleuritic chest pain. An ABG on air is taken. What is the best description of the result? p. H 7. 40 (7. 35 ‐ 7. 45) Pa. CO 2 6. 0 (4. 7 ‐ 6. 0) Pa. O 2 12. 6 (11. 3 ‐ 12. 6) HCO 3‐ 27. 0 (21 ‐ 29) BE +0. 9 (‐ 2 ‐ +2) 1. Definitely spurious 2. Indicative of alveolar hypoventilation 3. Indicative of ventilation‐ perfusion mismatch 4. Normal ABG 5. Probably spurious
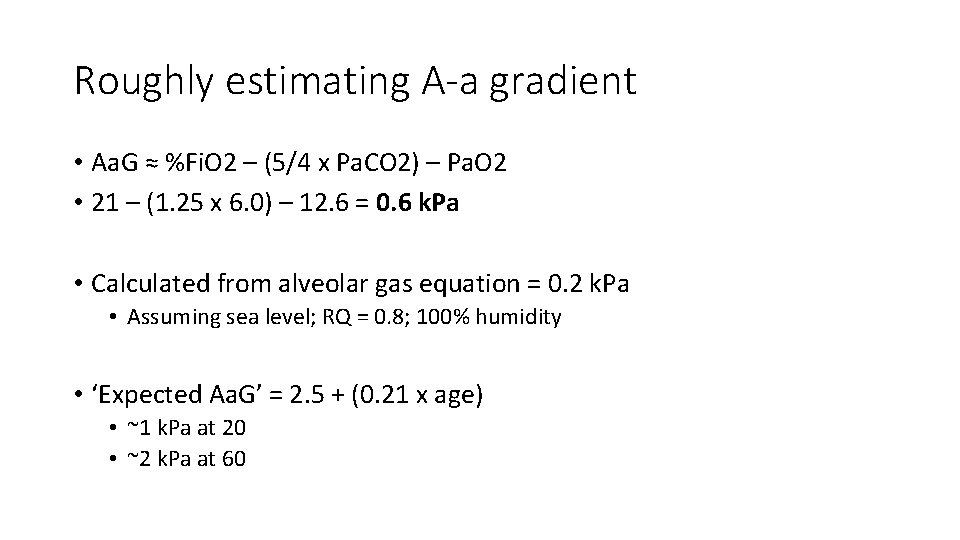
Roughly estimating A-a gradient • Aa. G ≈ %Fi. O 2 – (5/4 x Pa. CO 2) – Pa. O 2 • 21 – (1. 25 x 6. 0) – 12. 6 = 0. 6 k. Pa • Calculated from alveolar gas equation = 0. 2 k. Pa • Assuming sea level; RQ = 0. 8; 100% humidity • ‘Expected Aa. G’ = 2. 5 + (0. 21 x age) • ~1 k. Pa at 20 • ~2 k. Pa at 60
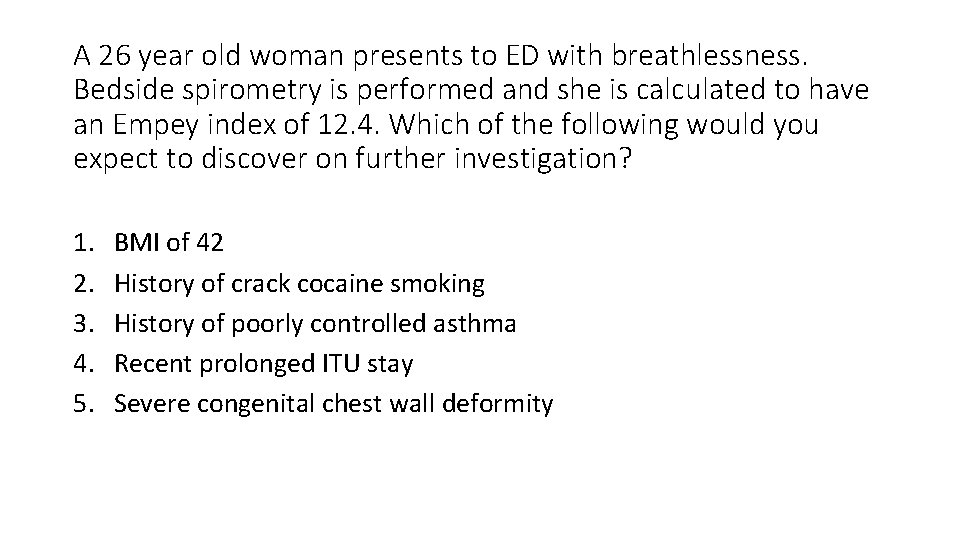
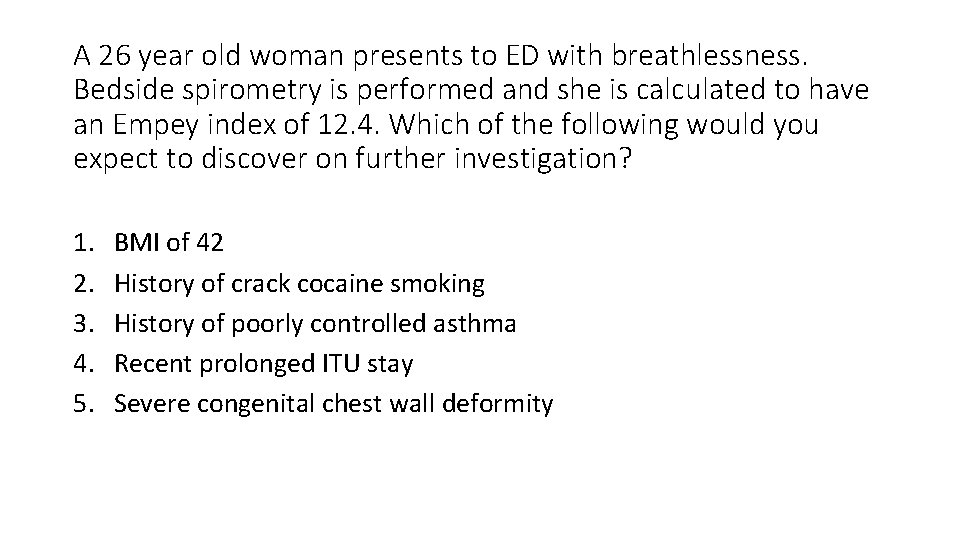
A 26 year old woman presents to ED with breathlessness. Bedside spirometry is performed and she is calculated to have an Empey index of 12. 4. Which of the following would you expect to discover on further investigation? 1. 2. 3. 4. 5. BMI of 42 History of crack cocaine smoking History of poorly controlled asthma Recent prolonged ITU stay Severe congenital chest wall deformity
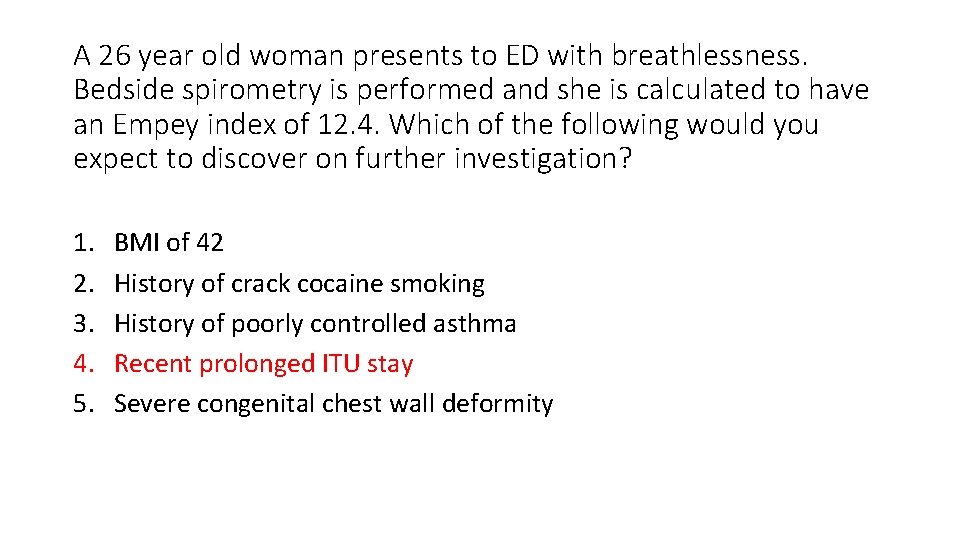
A 26 year old woman presents to ED with breathlessness. Bedside spirometry is performed and she is calculated to have an Empey index of 12. 4. Which of the following would you expect to discover on further investigation? 1. 2. 3. 4. 5. BMI of 42 History of crack cocaine smoking History of poorly controlled asthma Recent prolonged ITU stay Severe congenital chest wall deformity
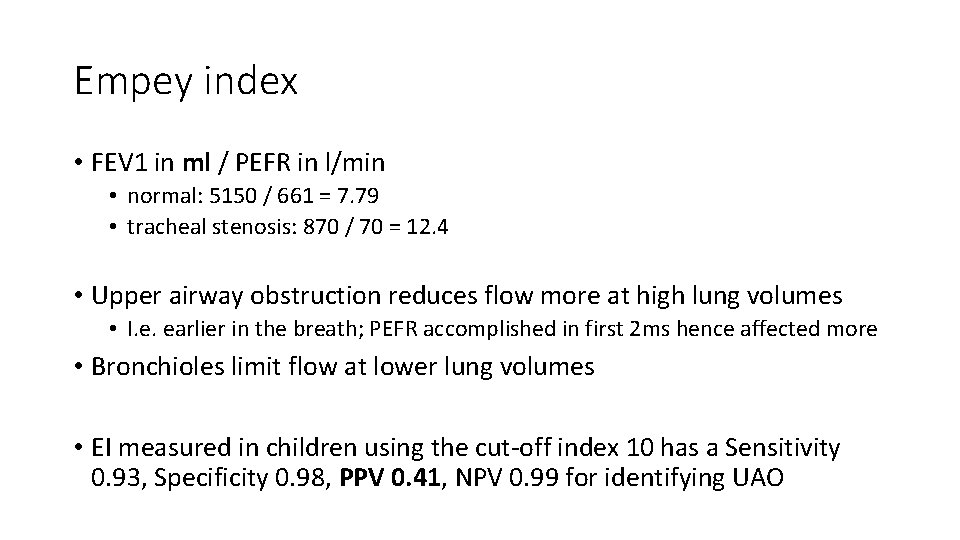
Empey index • FEV 1 in ml / PEFR in l/min • normal: 5150 / 661 = 7. 79 • tracheal stenosis: 870 / 70 = 12. 4 • Upper airway obstruction reduces flow more at high lung volumes • I. e. earlier in the breath; PEFR accomplished in first 2 ms hence affected more • Bronchioles limit flow at lower lung volumes • EI measured in children using the cut‐off index 10 has a Sensitivity 0. 93, Specificity 0. 98, PPV 0. 41, NPV 0. 99 for identifying UAO
References • Vocal cord dysfunction: a functional cause of respiratory distress • Weinberger, Doshi, 2017; Breathe • Characterisation of severe obliterative bronchiolitis in rheumatoid arthritis • Devouassoux et al, 2009; ERJ • https: //www. msdmanuals. com/en-gb/medical-calculators/AAGradient. htm • Clinical use of the Empey index in the emergency department • France, Thomas, 2004; Emergency Medicine Journal • Lung function testing • Gosselink, 2005; ERS Monographs • Physiology and clinical use of Heliox • www. uptodate. com • Physiology of the lungs in idiopathic pulmonary fibrosis • Plantier et al, 2018; ERJ