Respiratory System KNH 411 Respiratory System Nutritional status





- Slides: 19
Respiratory System KNH 411
Respiratory System Nutritional status and pulmonary function are interdependent Macronutrients fueled using oxygen and carbon dioxide Malnutrition can evolve from pulmonary disorders And can contribute to declining pulmonary status

Nutrition and Pulmonary Health Protein-energy malnutrition- PEM, using up so much energy to try breathe- COPD, emph, reduction of lung capacity, respiratory infection- eat up calories Antioxidants and lung function- Vit C, E, beta-carotene, selenium Cigarette smokers- increase Vit C DRI + 35 mg- diet not huge concerns for them Early satiety, anorexia, weight loss, cough, dyspnea- SOB during eating- want small meals
Bronchopulmonary Dysplasia (BPD) Growth failure d/t decreased nutrient intake, increased requirements, hypoxemia, delayed skeletal mineralization and osteopenia
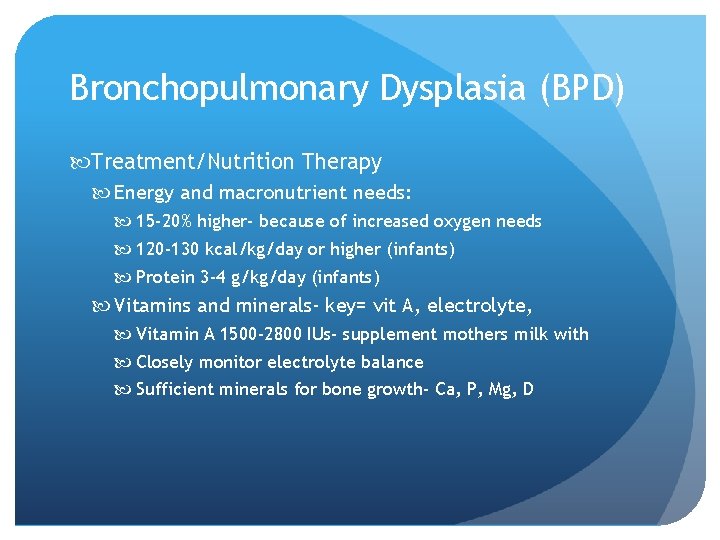
Bronchopulmonary Dysplasia (BPD) Treatment/Nutrition Therapy Energy and macronutrient needs: 15 -20% higher- because of increased oxygen needs 120 -130 kcal/kg/day or higher (infants) Protein 3 -4 g/kg/day (infants) Vitamins and minerals- key= vit A, electrolyte, Vitamin A 1500 -2800 IUs- supplement mothers milk with Closely monitor electrolyte balance Sufficient minerals for bone growth- Ca, P, Mg, D
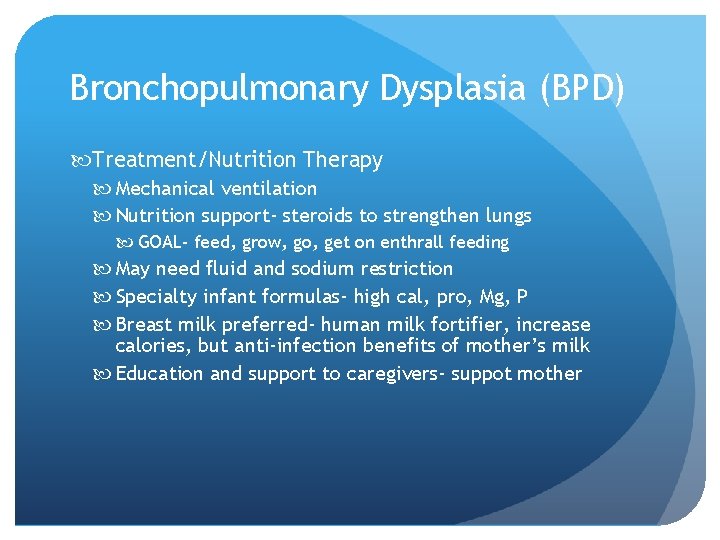
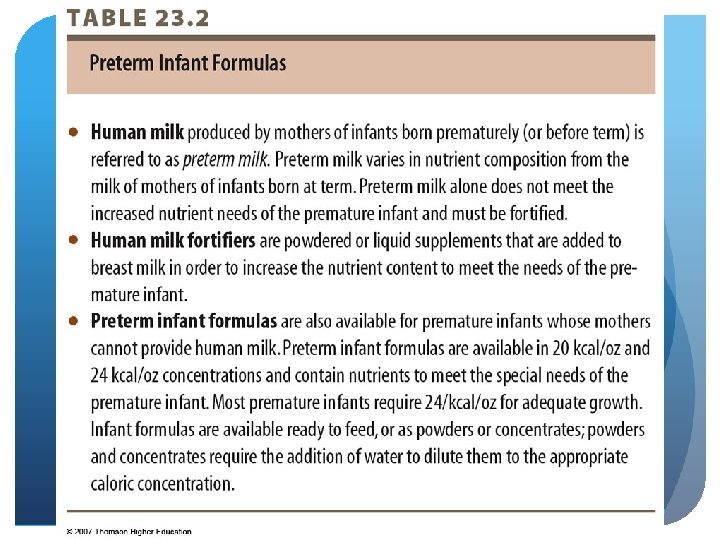
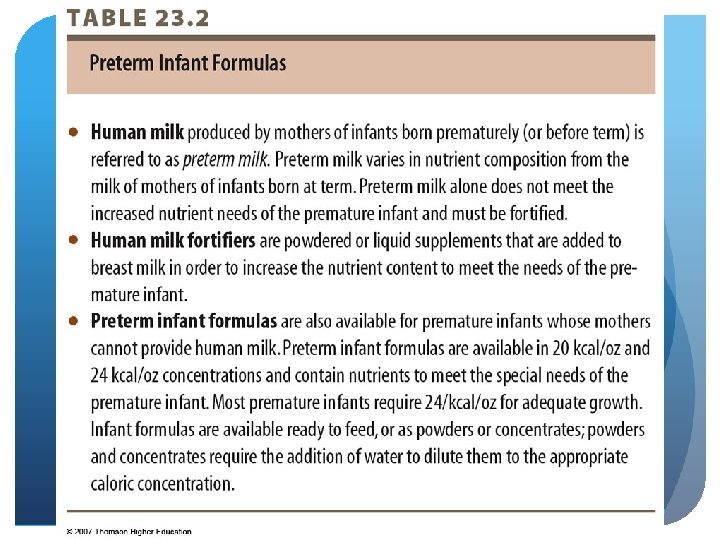
Bronchopulmonary Dysplasia (BPD) Treatment/Nutrition Therapy Mechanical ventilation Nutrition support- steroids to strengthen lungs GOAL- feed, grow, go, get on enthrall feeding May need fluid and sodium restriction Specialty infant formulas- high cal, pro, Mg, P Breast milk preferred- human milk fortifier, increase calories, but anti-infection benefits of mother’s milk Education and support to caregivers- suppot mother
© 2007 Thomson - Wadsworth
Chronic Obstructive Pulmonary Disease COPD – progressive disease which limits airflow through inflammation of bronchial tubes (bronchitis) Primary risk factor – smoking, get them to quit smoking, lifestyle Decrease to less than half and be able to function Ob of airflow to bronchial tubes Destruction of the alveoli Or both
COPD Nutrition Therapy Low dietary intake Deceased appetite- disease state, depressed Altered taste perceptions and appetite- trying to get air in Elevated REE- BECAUSE OF BREATHING Increased inflammation of the area
COPD Nutrition Therapy - Interventions Maintain optimal energy balance, maintain body weight!! 125 -156% of REE above- 25 -35 calories/ kilogram BW (based on weight) HB equation add 25 -50% of that Protein 1. 2 - 1. 7 g/kg BW Very hard to meet these needs! Overfeeding concern with ventilation Glucose >5 mg/kg/min increases CO 2 production Must look at composition and macronutrients Carbs can compromise- so want higher fat/pro intake 45 -50% carbs Commercial formulas - low CHO (30%) and higher lipid (50%) Pulmicare- one brand
COPD Nutrition Therapy - Interventions Supplement antioxidants- vit C, A, E, betac Monitor serum phosphate Compromised Phosphate level, essential for ATP, need to check Monitor status of calcium and vit. D 1200 -1500 mg Ca, 400 IU vit D per day Identify specific nutrition problems Low estrogen levels, decrease BMI, vit D, decreased mobility, PA, good nutrition, osteoporosis Manage weight

Cystic Fibrosis Nutrition Poor digestion, absorption, malnutrition d/t pancreatic insufficiency, poor digestion of fat, Vit ADEK, malnutrition related to pan insufficiency Abnormal growth Risk for osteopenia (impaired bone growth/ function) and osteoporosis Malabsorp- Ca, P, Mg, Vit D/K- compounded by cortical steroids Increased pro and calories at night

Cystic Fibrosis Nutrition Assessment- multidiseplinary approach National CF Foundation consensus guidelines - nutrition guidelines Special attention to poor growth: Early detection Birth-12 years of age, prepubesence (stunted growth)
Cystic Fibrosis Pancreatic enzyme therapy- no lipase, amylase, protiase secretion (they cannot secrete on their own) Given with food and beverages Individualized (need to follow on their own path) Adequate kcal for normal growth based on weight gain patterns Higher fat intake (35 -45% kcal) MCT- medium chain triglycerides (easy to digest) 6 -12 carbons, shorter in length than long chain, water soluble= less bile Because they malabsorb fat and are underweight Glucose intolerance common- will convert to a diabetic in teen years, type 2

Cystic Fibrosis Monitor vitamin & mineral status Monitor sodium levels- know they are not fluid overloaded Assess iron and zinc status- CF a mineral losing disease state, steroids can take away iron Recommend breast feeding- more kilocalories, immune fighting properties Developmentally appropriate recommendations COULD HAVE TROBLUE NURSING Could have trouble with hand-mouth coordination Weight status, head circumference, height in length Formulas or nutritional supplements 110% of kilocalories 24, 27, 30 calories per ounce- formula, make more calorie dense

Respiratory Failure Nutrition Meet nutrition need- preserve lean body mass (particularly their respiratory muscle) Energy needs vary widely; may be hypermetabolic Avoid overfeeding- avoid overfeeding carbohydrates (up protein and fat for calories) Indirect calorimetry is the preferred method- ICU setting, 25 calories per kilogram body weight or 130% REE- 1. 2 -1. 5 grams Preserve and restore LBM; respiratory muscle mass
Respiratory Failure Nutrition Maintain fluid balance Facilitate weaning from ventilation- key Specialty formulas available EPA and GLA can reduce severity of inflammation (fish oils beneficial to respiratory status, another nutrient that decreases inflammation) Supplementation with antioxidants (Vit, C, beta carotene, prevent slow, oxidative damage) Phosphate supplementation (helps with normal contraction of the diaphragm, essential for respiratory function)
 Nutritional status assessment
Nutritional status assessment Optimal nutritional status definition
Optimal nutritional status definition Advantages of clinical assessment of nutritional status
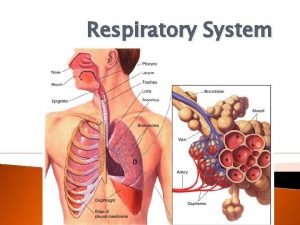
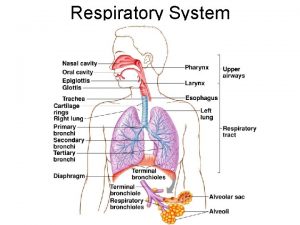
Advantages of clinical assessment of nutritional status Respiratory system maintain homeostasis
Respiratory system maintain homeostasis Knh
Knh Knh
Knh Respiratory zone
Respiratory zone Site:slidetodoc.com
Site:slidetodoc.com Nutrition 411
Nutrition 411 Mgt 411
Mgt 411 Ece 411
Ece 411 Csce 411
Csce 411 Comp 411
Comp 411 Anwar mamat umd
Anwar mamat umd Ncp nutrition care process
Ncp nutrition care process Ada 411
Ada 411 Ist 411
Ist 411 Csce 411
Csce 411 Csce 411
Csce 411 Cpsc 411
Cpsc 411