RESPIRATORY SYSTEM Ass Prof Dr Emre Hamurtekin EMU

- Slides: 13
RESPIRATORY SYSTEM Ass. Prof. Dr. Emre Hamurtekin EMU Faculty of Pharmacy
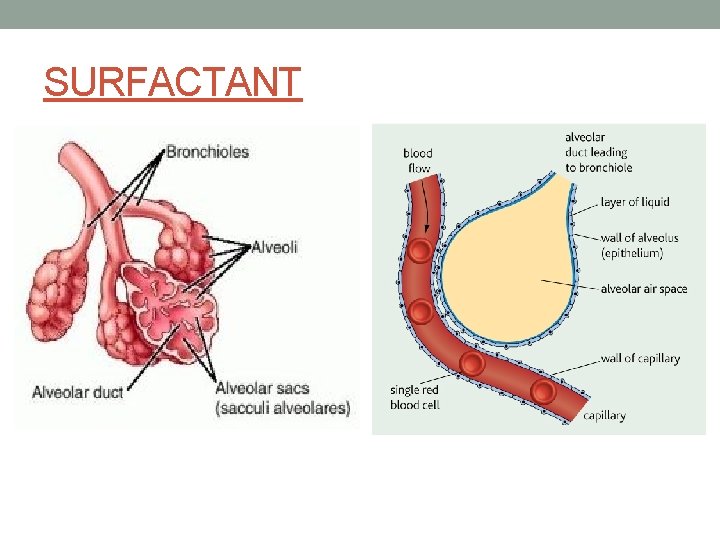
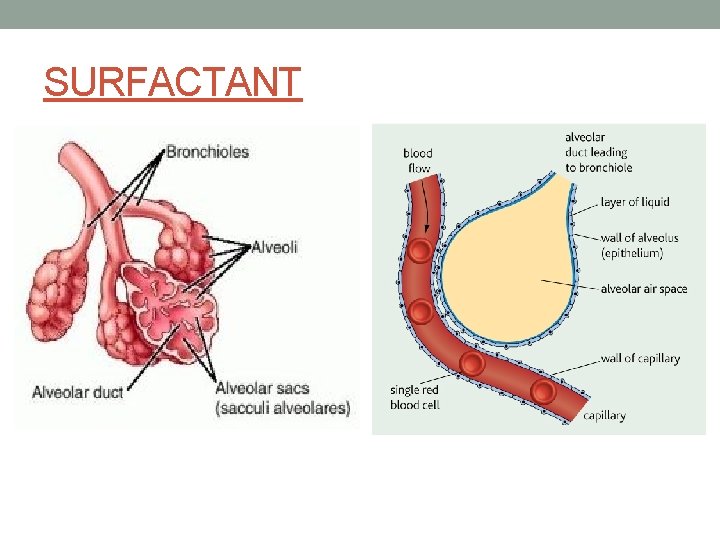
SURFACTANT
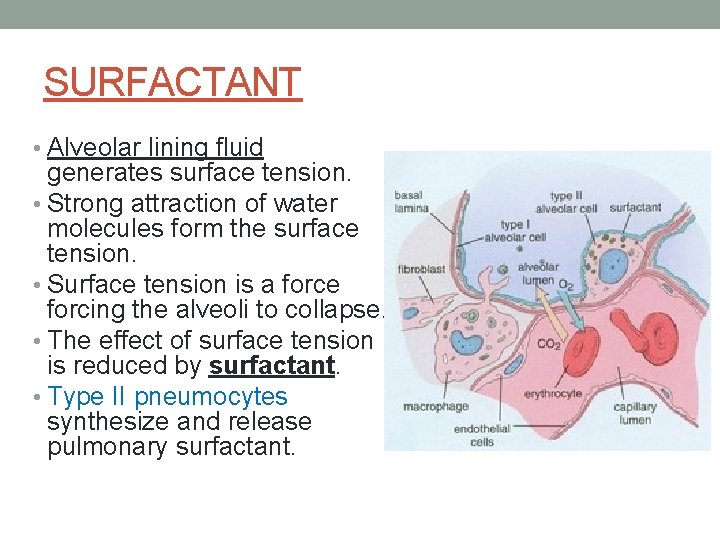
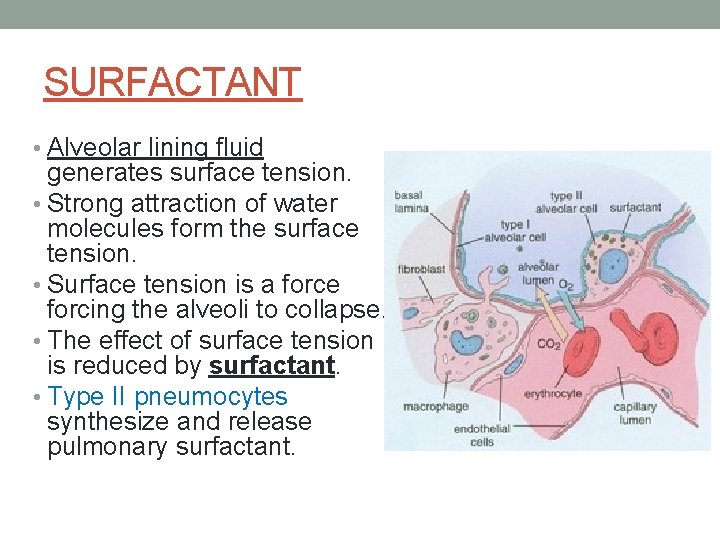
SURFACTANT • Alveolar lining fluid generates surface tension. • Strong attraction of water molecules form the surface tension. • Surface tension is a force forcing the alveoli to collapse. • The effect of surface tension is reduced by surfactant. • Type II pneumocytes synthesize and release pulmonary surfactant.
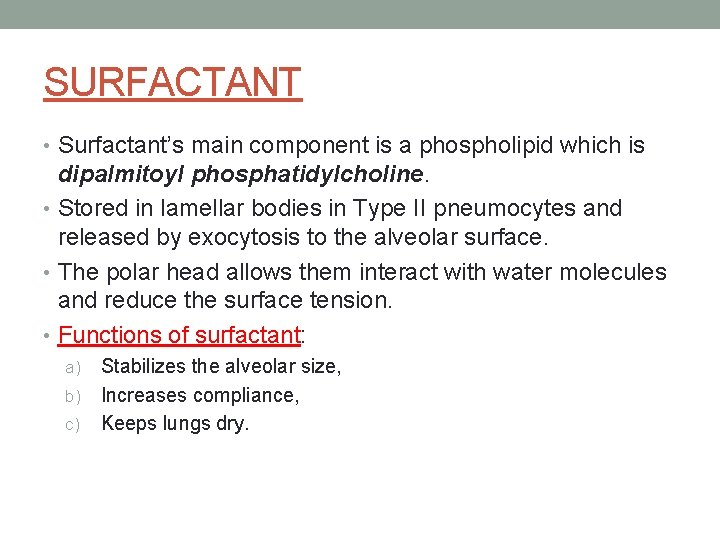
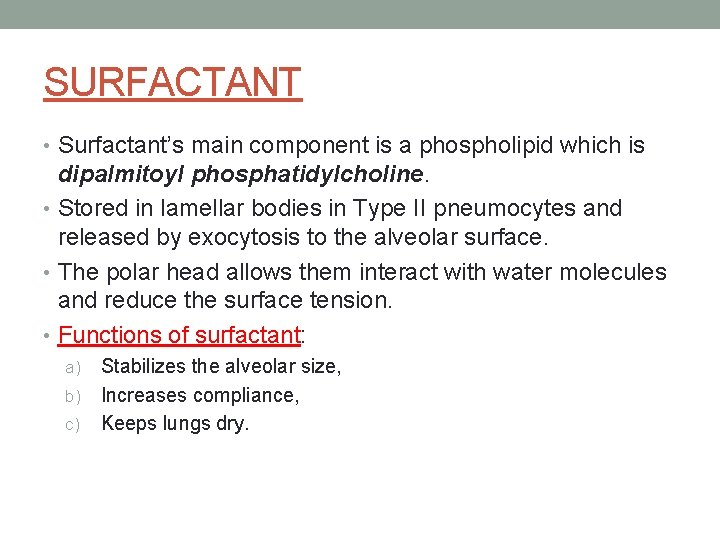
SURFACTANT • Surfactant’s main component is a phospholipid which is dipalmitoyl phosphatidylcholine. • Stored in lamellar bodies in Type II pneumocytes and released by exocytosis to the alveolar surface. • The polar head allows them interact with water molecules and reduce the surface tension. • Functions of surfactant: a) b) c) Stabilizes the alveolar size, Increases compliance, Keeps lungs dry.
SURFACTANT a) Stabilizes the alveolar size: v. Decrease in alveolar volume decreases surface area and concentrates surfactant molecules which helps reducing the surface tension, v. This prevents the collapse of alveoli. v. Increase in alveolar volume decreases the density of surfactant and allows surface tension. b) Increasing compliance: v. Lung compliance: Amount of pressure needed to inflate lungs to a given volume. v. Surface tension decreases lung compliance. v. Surfactant decreases the effort to inflate the lungs. c) Keeping lungs dry: v. The surface tension produce a driving force for the interstitial fluid to drain into the alveoli. v. Surfactant reduces the pressure gradient and helps keeping the lungs dry (prevent from pulmonay edema).
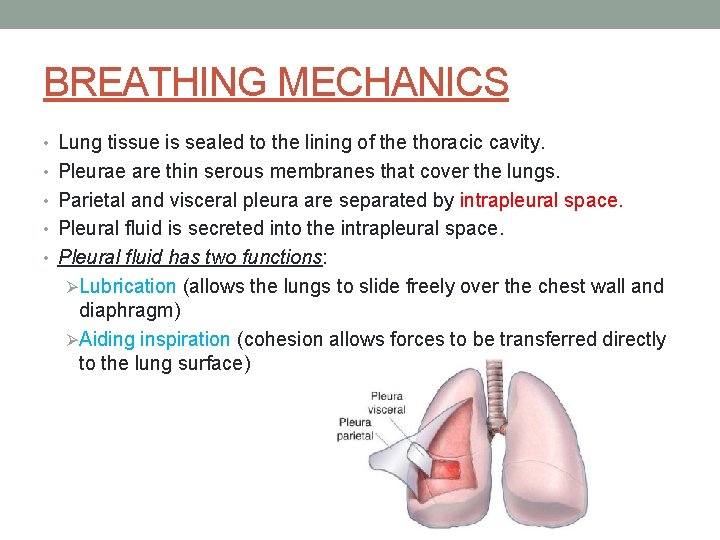
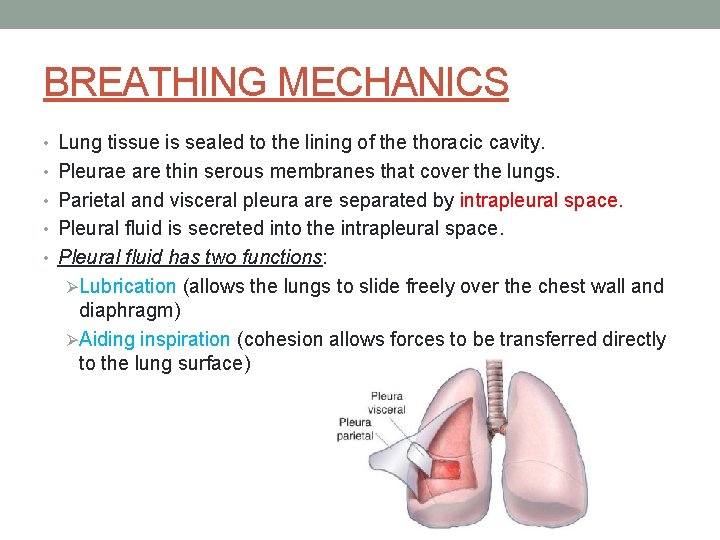
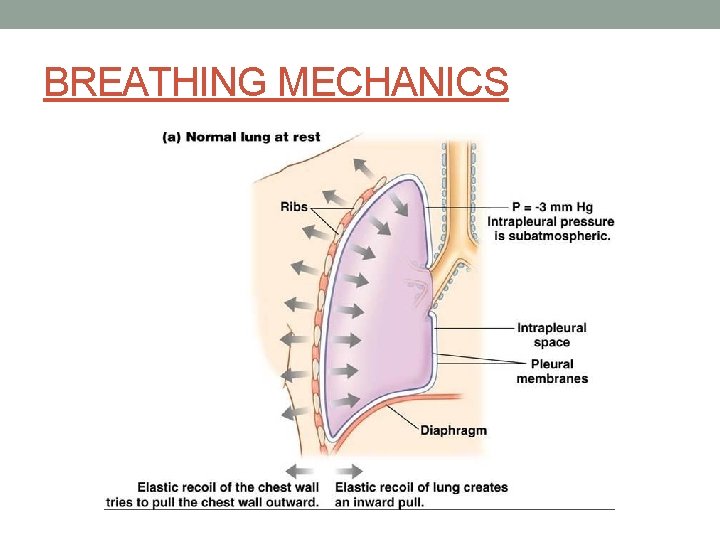
BREATHING MECHANICS • Lung tissue is sealed to the lining of the thoracic cavity. • Pleurae are thin serous membranes that cover the lungs. • Parietal and visceral pleura are separated by intrapleural space. • Pleural fluid is secreted into the intrapleural space. • Pleural fluid has two functions: ØLubrication (allows the lungs to slide freely over the chest wall and diaphragm) ØAiding inspiration (cohesion allows forces to be transferred directly to the lung surface)
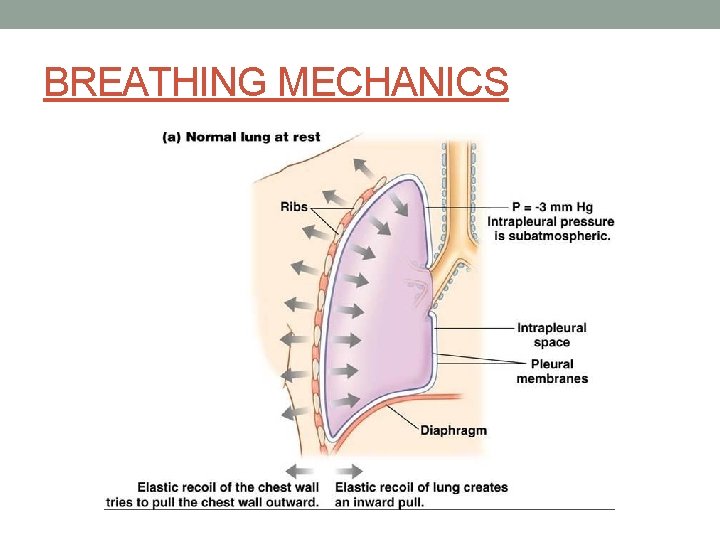
BREATHING MECHANICS
BREATHING MECHANICS INSPIRATION: • Inspiration is an active process. • When diaphragm contracts, intrathoracic volume increases. • Diaphragm contraction: ü pushes downward of the abdominal contents and increases the vertical dimensions of thoracic cavity ü causes the ribs to rise and cross-sectional area increases. EXPIRATION: • Expiration is generally a passive process and is driven by; v. Surface tension v. Elastic recoil
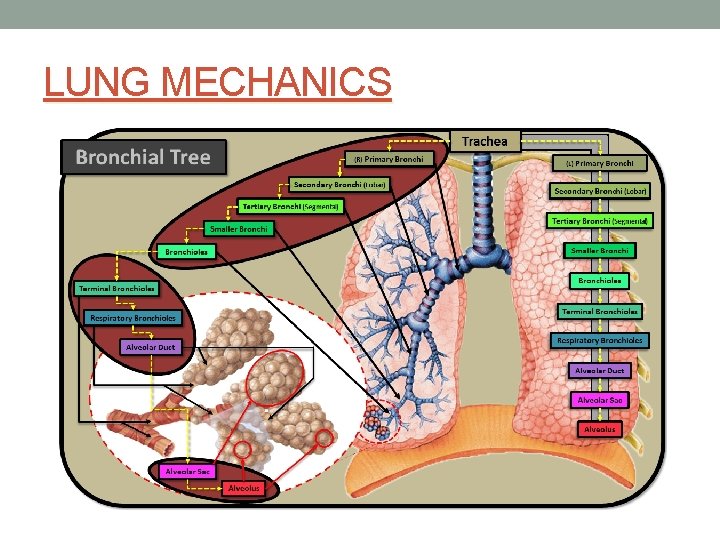
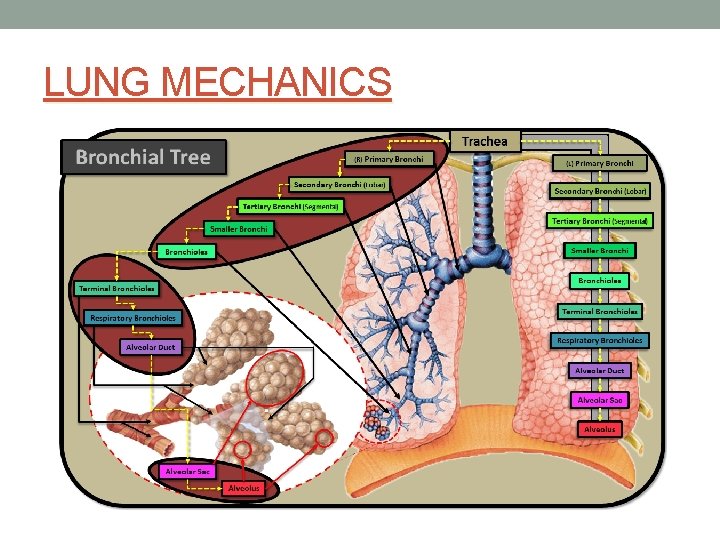
LUNG MECHANICS
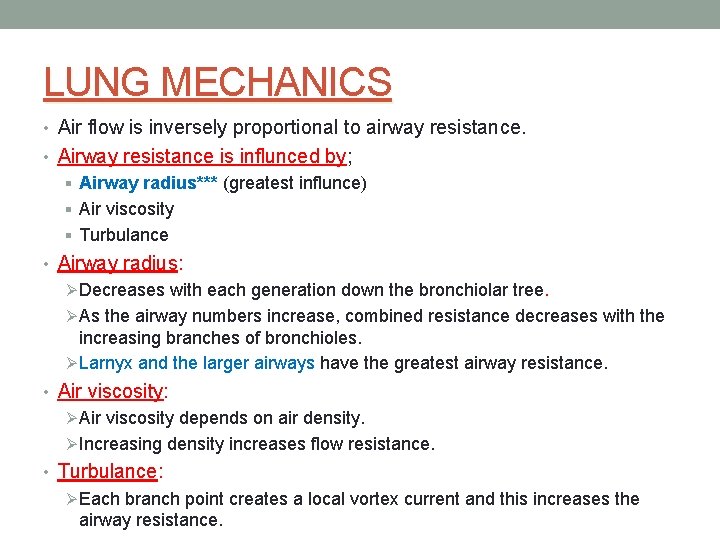
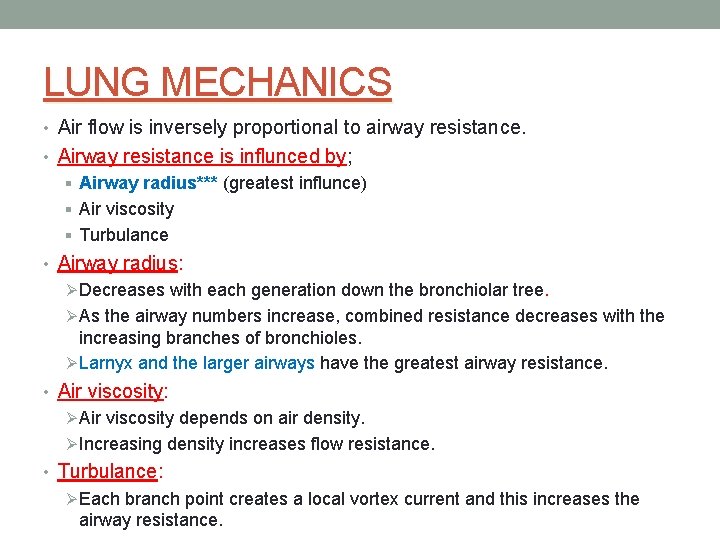
LUNG MECHANICS • Air flow is inversely proportional to airway resistance. • Airway resistance is influnced by; § Airway radius*** (greatest influnce) § Air viscosity § Turbulance • Airway radius: Ø Decreases with each generation down the bronchiolar tree. Ø As the airway numbers increase, combined resistance decreases with the increasing branches of bronchioles. Ø Larnyx and the larger airways have the greatest airway resistance. • Air viscosity: Ø Air viscosity depends on air density. Ø Increasing density increases flow resistance. • Turbulance: Ø Each branch point creates a local vortex current and this increases the airway resistance.
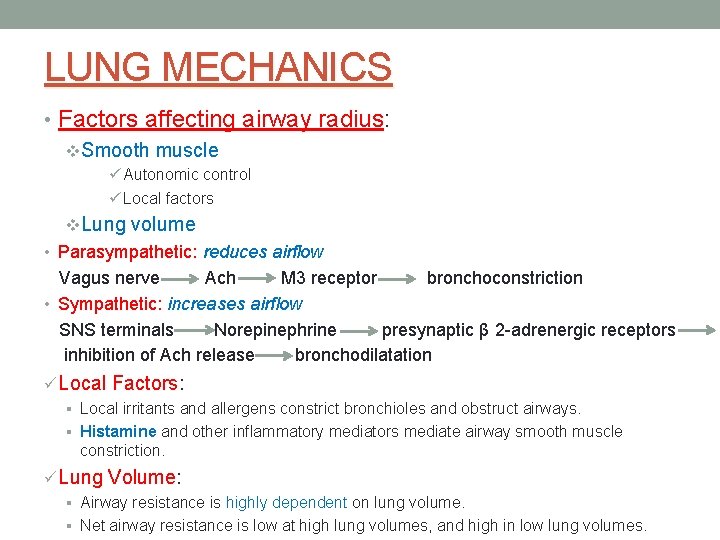
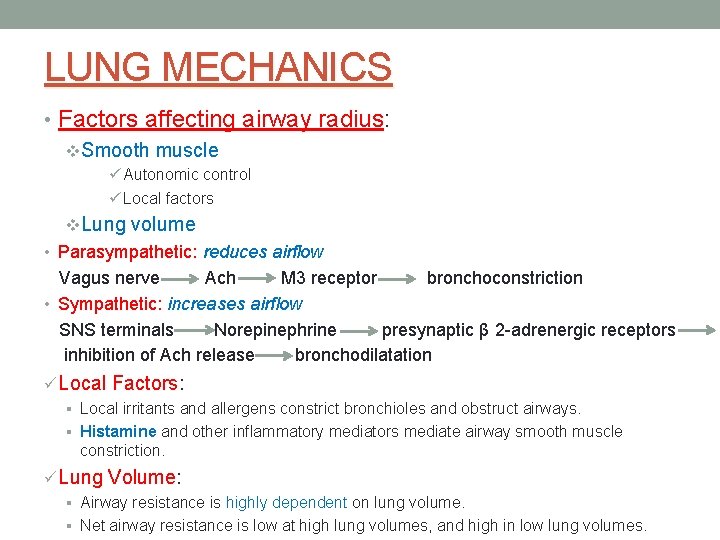
LUNG MECHANICS • Factors affecting airway radius: v. Smooth muscle ü Autonomic control ü Local factors v. Lung volume • Parasympathetic: reduces airflow Vagus nerve Ach M 3 receptor bronchoconstriction • Sympathetic: increases airflow SNS terminals Norepinephrine presynaptic β 2 -adrenergic receptors inhibition of Ach release bronchodilatation ü Local Factors: § Local irritants and allergens constrict bronchioles and obstruct airways. § Histamine and other inflammatory mediators mediate airway smooth muscle constriction. ü Lung Volume: § Airway resistance is highly dependent on lung volume. § Net airway resistance is low at high lung volumes, and high in low lung volumes.
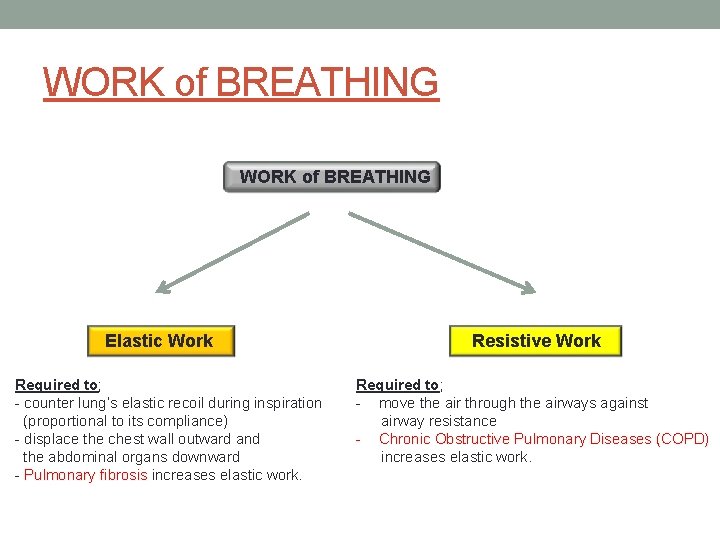
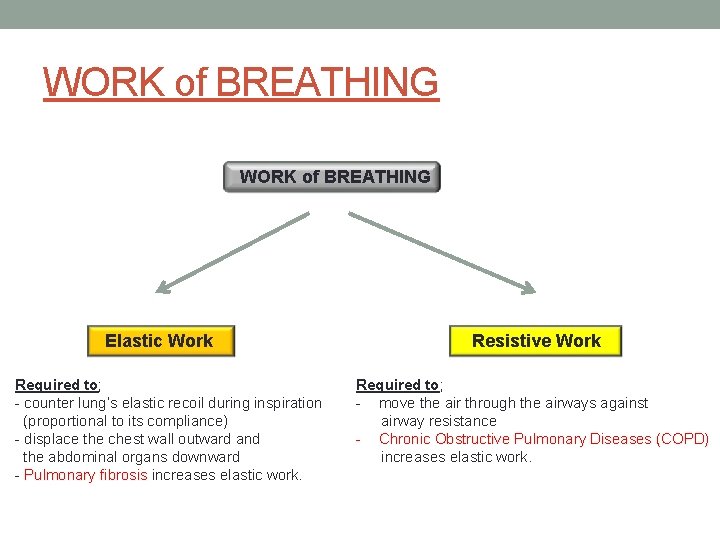
WORK of BREATHING Elastic Work Required to; - counter lung’s elastic recoil during inspiration (proportional to its compliance) - displace the chest wall outward and the abdominal organs downward - Pulmonary fibrosis increases elastic work. Resistive Work Required to; - move the air through the airways against airway resistance - Chronic Obstructive Pulmonary Diseases (COPD) increases elastic work.
